Abstract
Background
Foreign body aspiration (FBA) is a serious condition with high morbidity and mortality rates. Although chest radiography is generally the first radiologic modality used in diagnosis, a substantial percentage of foreign bodies are radiolucent in adults with diagnosis challenging.
Methods
Retrospective review of adult patients with FBA diagnosed by flexible electronic bronchoscopy from 2012 to 2022 collecting demographics, history, hospital presentation, radiographic, and operative details. Risk factors associated with radiolucent foreign body inhalation in adults were explored using appropriate statistical methods.
Results
Between 1 January 2012 and 1 January 2022, 114 adult patients diagnosed with FBA were enrolled. The median age of participants was 65 years (IQR 52–74). Multidetector computed tomography (MDCT) examinations identified 28 cases (25%) showing direct visualization of the foreign body (defined as the radiopaque group) and 86 cases (75%) in the radiolucent group. Multivariable stepwise linear regression analysis showed increased odds of radiolucent foreign body inhalation in adults associated with pneumonic patches in MDCT (OR 6.99; 95% CI 1.80–27.22; P = 0.005) and plants/meat foreign bodies (OR 6.17; 95% CI 1.12–33.96; P = 0.04). A witnessed choking history (OR 0.02; 95% CI 0–0.14; P < 0.001) was a protective factor of radiolucent foreign body inhalation in adults.
Conclusions
Unlike radiopaque FBA, in those presenting with a suspected radiolucent foreign body aspiration, the diagnosis is far more challenging. Risk factors such as lacking a choking history, non-resolving pneumonia (pneumonic patches) in MDCT findings, and plants/meat foreign bodies may help in the early diagnosis of radiolucent foreign body inhalation in adults. Further prospective multicenter studies should be conducted to validate the findings.
Similar content being viewed by others
Background
Foreign body aspiration (FBA) is an uncommon but potentially life-threatening event [1, 2]. Symptoms typically consist of a choking event followed by cough and dyspnea [3, 4]. Although both adults and children tend to inhale foreign bodies, it is more common in children than in adults [4]. Several observational studies report a low rate of FBA in adults (0.66 per 100,000) [5,6,7]. However, the presentations in adults are inconsistent and symptoms may mimic more chronic lung diseases such as asthma or chronic obstructive pulmonary disease [6, 8,9,10]. In addition, many cases of FBA in adults lack a history of choking and are often with no direct signs of airway foreign body in chest radiographs [4, 11].
The initial clues for FBA in adults are usually obscure or indirect [11, 12]. Reports have indicated that only 25–38% of adult patients who are found to have a lower airway foreign body remember a choking event [13, 14]. This is supported by a systematic literature review showing that often a history of aspiration is lacking in adults with FBA [15]. Although chest radiography is the primary imaging modality used to identify a foreign body in the lower airway, a study from Sehgal and colleagues showed that only 24.6% of foreign body inhalation in the adult population has the radiological manifestations of foreign body aspiration and direct visualization of the foreign body in the case of radiopaque foreign bodies [5]. Unlike radiopaque FBA, in those presenting with a suspected radiolucent foreign body aspiration, the diagnosis is far more challenging [16,17,18]. When a diagnosis is not established immediately, retained foreign bodies may lead to recurrent pneumonia, recurrent hemoptysis, bronchiectasis, or other complications [5].
In this study, we aimed to analyze retrospectively to determine risk factors that help in the early diagnosis of radiolucent foreign body inhalation in adults.
Study design and methods
Participants
All methods were carried out following relevant guidelines and regulations. With approval from the Ethics Committee of the Central Hospital of Wuhan, Hubei, China (Approval No.: WHZXKYL2022-052), a retrospective review was conducted at the Department of Pulmonary and Critical Care Medicine in the Central Hospital of Wuhan. All adult patients (age > 18 years) diagnosed with FBA from 1 January 2012 to 1 January 2022 were enrolled. They all underwent multi-detector Computed Tomography (MDCT) examinations followed by flexible bronchoscopy (details in Additional file 1: Methods).
Measures
Patient demographics, pre-hospital history, symptoms, radiographic presentations, operative details, bronchoscopic findings, and clinical course were collected from the medical records.
Patients underwent chest MDCT examinations in the supine position and with breath-holding following inspiration (GE Healthcare Optima) from the level of the thoracic inlet to the dome of the diaphragm. The CT examinations were performed with a rotation time of 0.6 s, a pitch ratio of 1.75, tube voltage of 120 kV, tube current adjust automatically, and a slice thickness of 1.25 mm for a whole chest scan. MDCT images were reconstructed with a 1.25-mm slice thickness on the workstation (GE ADW 2.0). These reconstructed axial images were processed. On the 3D page, the reconstructed multiplanar reformation (MPR) images were evaluated in the axial, sagittal, and coronal planes. MDCT examinations showing direct visualization of the foreign body are defined as radiopaque cases, while radiolucent cases are those foreign bodies that failed to be identified by 2 experienced radiologists. They reviewed the images independently in a consistent manner, with a conclusion reached by consensus when there was a discrepancy.
Statistical analysis
Categorical variables were expressed as n (%) and compared by χ2 test or Fisher's exact test if appropriate. Continuous variables were expressed as median (IQR, interquartile range), and compared using a two-sample t-test, Welch's two-sample t-test, or Mann–Whitney U test, if appropriate. Normality of distribution was assessed using the Shapiro–Wilk test. Because of the sample size, measurable variables with significant differences between groups were considered in subsequent univariate and multivariable logistic regression analyses [19,20,21,22,23,24]. A multivariable binary logistic regression analysis (backward stepwise method) was performed to identify the independent risk factors associated with radiolucent foreign body inhalation in adults. Cut off point was determined by the receiver operating characteristic curve. P values less than 0.05 were considered statistically significant. All data analyses and graphs were done in R (version 4.1.3).
Results
Patient characteristics
As shown in Table 1, between 1 January 2012 and 1 January 2022, 114 adult patients diagnosed with FBA were enrolled, of whom 71 were male (62%) and 43 females (38%), with a median age of 65 years (IQR 52 ~ 74). A witnessed choking history was observed in 19 (17%) patients. 49 cases (43%) were with a length of disease course of more than 60 days. 12 patients (11%) had been admitted to ICU, mainly due to airway obstruction, respiratory failure, and multiple organ dysfunction. 64 cases (56%) had been misdiagnosed as pneumonia and 5 cases (4%) as lung cancer.
80 patients (70%) had complications with 59 patients (52%) had a variety of chronic diseases requiring daily medication, including hypertension, coronary disease, and type 2 diabetes mellitus. 30 patients (26%) suffered chronic respiratory diseases presenting cough, expectoration, and dyspnea. 18 patients (16%) had post-stroke dysphagia, 3 patients (3%) with Alzheimer's disease, 2 patients (2%) with a history of throat surgery, and 1 patient with FBA during the dental operation.
For symptoms, coughing was the most common presentation of FBA (103 cases, 90%). Other presentations included purulent sputum (84 cases, 74%), chest tightness (49 cases, 43%), and hemoptysis (25 cases, 22%). In addition, a few patients presented symptoms as fever (9 cases, 8%), dyspnea (6 cases, 5%), chest pain (5 cases, 4%), and disturbance of consciousness (1 case, 1%). Physical examinations identified 24 cases (21%) presenting rales and 6 cases (5%) wheezing.
Comparisons in adult patients with radiolucent versus radiopaque FBA were done. A higher proportion of patients without a witnessed choking history was observed in radiolucent FBA cases when compared with those with radiopaque FBA (93% vs. 39%; P < 0.001). Patients diagnosed with radiolucent FBA also had a longer disease course (median 60 days, IQR 14–150; P < 0.001), with 44 cases (51%) having a length of disease course of more than 60 days (P = 0.004). 12 (14%) patients diagnosed with radiolucent FBA had been admitted to ICU, while no case was for those with radiopaque FBA (P = 0.04). 57 (66%) patients diagnosed with radiolucent FBA had been misdiagnosed as pneumonia compared to 7 (25%) for those with radiopaque FBA (P < 0.001). Details are summarized in Table 1.
Multidetector computed tomography (MDCT) presentations
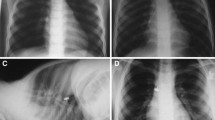
All patients (n = 114) underwent MDCT examinations followed by flexible bronchoscopy, with 28 cases (25%) showing direct visualization of the foreign body (defined as the radiopaque group, Fig. 1A) and 86 cases (75%) in the radiolucent group (Fig. 1B). In addition to the visualization of the foreign body, MDCT presentations for FBA included non-resolving pneumonia (pneumonic patch) in 80 cases (70%), airway stenosis in 18 cases (16%), atelectasis in 16 cases (14%), bronchiectasis in 15 cases (13%), thickening of the bronchial wall in 14 cases (12%), unilateral pleural effusion in 14 cases (12%), and consolidation in 13 cases (11%) (Table 2).
Representative radiographic presentations and bronchoscopic findings from foreign body aspiration cases. A A 68-year male patient inhaled a metal nail (red arrows) during dental implantation located at the LB8 in the radiopaque group. B A 78-year male patient inhaled a fish bone (red arrows) located at the RB2 in the radiolucent group. In B, the position of the fish bone was indicated retrospectively after a flexible bronchoscopy examination
When comparing adult patients with radiolucent versus radiopaque FBA, we noticed that a higher proportion of patients with radiolucent FBA showed non-resolving pneumonia (pneumonic patch) (81% vs. 36%; P < 0.001), thickening of the bronchial wall (16% vs. 0%; P = 0.02) and consolidation (15% vs. 0%; P = 0.04) (Table 2).
Flexible bronchoscopy findings
In total, 112 cases (98%) of the foreign bodies were successfully removed by flexible bronchoscopy with 85 cases (75%) achieved by a single operation and 29 cases (25%) needing more than 2 operations. 85 cases (75%) were operated on under local anesthesia and 29 cases (25%) under general anesthesia. Granulomas under bronchoscopy were observed in 50 cases (44%) and ulcers in 9 cases (8%). 85 cases (75%) required a single surgical tool to remove foreign bodies while 29 cases (25%) with more than 2 different types of tools. During operations, 20 cases (18%) presented active bleeding. For operation time, 79 cases (69%) were finished within 30 min and 35 cases (31%) above 30 min. Interestingly, adult patients with radiolucent FBA seemed to require a fewer number of operations (P = 0.03) (Table 3).
The foreign bodies successfully removed were mostly located in the right main bronchus (34 cases, 30%) and right lower lobe bronchus (25 cases, 22%). Other locations included the left lower lobe bronchus (12 cases, 11%), right middle lobe bronchus (10 cases, 9%), left upper lobe bronchus (7 cases, 6%), left main bronchus (6 cases, 5%), right upper lobe bronchus (5 cases, 4%), glottis (3 cases, 3%), and trachea (windpipe) (2 cases, 2%). Foreign bodies in 10 cases (9%) had multiple locations (Fig. 2A).
A variety of foreign bodies were detected, including 58 cases (51%) of bones (chicken bone, fish bone, crayfish shell), 34 cases (30%) of plants/meat (vegetable, beans, nuts, food scrap mixed with rice, vegetable, and meat), medicine pills (2 cases, 2%), metal (2 cases, 2%), plastic films (2 cases, 2%), and dentures (2 cases, 2%). 11 subjects (10%) were not identifiable (Table 4). We then classified metal, plastic films, and dentures as inorganics, while bones, medicine pills, and plants/meat as organics. In this cohort, 97 cases (85%) were organic foreign bodies (Additional file 1: Table S1).
When comparing adult patients with radiolucent versus radiopaque FBA, we noticed the differences in the site (P = 0.005) and type of foreign bodies (P = 0.03) (Table 4). The top 2 locations for radiolucent foreign bodies were the right lower lobe bronchus (22 cases, 26%) and right main bronchus (19 cases, 22%) (Fig. 2B), while the majority of radiopaque foreign bodies located at the right main bronchus (15 cases, 53%) (Fig. 2C). Regarding the type of foreign bodies, radiolucent foreign bodies were mainly bones (38 cases, 44%) and plants/meat (31 cases, 36%) (Table 4).
Risk factors associated with radiolucent foreign body inhalation in adults
To explore the risk factors associated with radiolucent foreign body inhalation in adults, univariate and multivariable logistic regression models were used. In univariate analysis, without a witnessed choking history, a longer disease course, MDCT showing pneumonic patches, located at the right lower lobe bronchus, and plants/meat foreign bodies were associated with radiolucent foreign body inhalation in adults (all P < 0.05; Additional file 1: Table S2).
We then identified MDCT showing pneumonic patches (OR 6.99; 95% CI 1.80–27.22; P = 0.005) and plants/meat foreign bodies (OR 6.17; 95% CI 1.12–33.96; P = 0.04) as independent risk factors of radiolucent foreign body inhalation in adults in the multivariable analysis (Table 5; Additional file 1: Table S3). A witnessed choking history (OR 0.02; 95% CI 0–0.14; P < 0.001) was a protective factor of radiolucent foreign body inhalation in adults in this multivariable analysis (Table 5; Additional file 1: Table S3).
Discussion
FBA may present a life-threatening emergency, which requires early diagnosis and urgent removal of foreign bodies by bronchoscopy to avoid complications [9, 12, 25, 26]. However, the presentations and symptoms of FBA in adults are inconsistent and diverse [6, 8,9,10]. In this retrospective study, with coughing as the most common presentation as expected, other presentations, such as purulent sputum, chest tightness, hemoptysis, and dyspnea, were also recorded. Occasionally, several patients presented symptoms such as fever, chest pain, and disturbance of consciousness.
In addition, foreign body inhalation in adults is often with no direct signs of airway foreign body in chest radiographs [12, 27]. In our cohort, all adult patients underwent MDCT examinations followed by flexible bronchoscopy. There were 75% of patients without direct visualization of the foreign bodies (radiolucent). Within this group, a majority of patients (93%) denied a witnessed choking history. All these factors resulted in a challenging/delayed diagnosis in adults with radiolucent foreign body inhalation. This led to a higher proportion of patients with misdiagnosis, a longer disease course, and being admitted to ICU. These findings were also reflected by the MDCT examinations showing that in the radiolucent group, patients often manifested non-resolving pneumonia (pneumonic patches), thickening of the bronchial wall, and consolidation, indicating recurrent airway inflammation. Taken together, identifying risk factors (predictors) that help in the early diagnosis of radiolucent foreign body inhalation in adults is urgently demanded.
A previous study by Boyd and colleagues suggested that risk factors of FBA in adults include loss of consciousness, age-related slowing in the swallowing mechanism, use of medications (those impair the ability to cough and swallow), post-stroke dysphagia, and numerous neurodegenerative diseases such as Alzheimer's or Parkinson's disease [27]. When comparing adult patients with radiolucent versus radiopaque FBA, no differences were found among the aforementioned risk factors.
To explore the risk factors associated with radiolucent foreign body inhalation in adults, robust and appropriate statistical methods were adopted. We identified MDCT showing pneumonic patches and plants/meat foreign bodies as independent risk factors of radiolucent foreign body inhalation in adults, and a witnessed choking history as a protective factor. This is consistence with earlier discussions indicating that a majority of radiolucent FBA cases in adults show evidence of recurrent airway inflammation as well as lacking a choking event.
Studies showed that the nature of the inhaled foreign bodies is highly variable ranging from organic to inorganic materials in adults [25, 28, 29]. The type of food aspirated varies with local traditions and/or ethnic background [30, 31]. Our study showed that 85% of foreign bodies were organic, including plants/meat and bones from different food. Although chest MDCT is more sensitive to detect radiopaque foreign bodies than X-rays [32], many organic foreign bodies, such as bones and plants/meat are radiolucent under MDCT [33,34,35,36]. A study suggested that a plant foreign body is a risk factor for lower respiratory tract infection in children [33]. Some plants, such as nuts, can cause inflammation, granulation tissue formation, and airway stenosis; while beans, seeds, and sweetcorn seeds can absorb water, leading to swelling which causes partial obstruction to a complete obstruction [37]. Multiple medication pills can also cause severe airway inflammation and ulceration [38]. The reason for the false-negative MDCT findings under these conditions could be a consequence of local lung infections resulting in a failed visualization of the foreign body.
The most common site of aspiration in adults is the right bronchus, in particular the mainstem or divisions of the right lower lobe bronchus. This is because compared to the left bronchus, the right one is more vertical and with a slightly larger diameter [39, 40]. This is also true in our cohort, with a majority of foreign bodies located in the right main bronchus and right lower lobe bronchus. Interestingly, the top location for radiolucent foreign bodies is the right lower lobe bronchus compared to the right main bronchus as the top location for radiopaque foreign bodies.
This study has several limitations. As a bronchoscopy and endoscopy center in central China, referral bias can influence the results of this study. Additionally, the details for foreign bodies, such as sharpness, hardness, and stability, were not recorded, which may be associated with different levels of airway inflammation and consequently MDCT presentations. Lastly, interpretation of our findings might be limited by the sample size. Despite these limitations, to our knowledge, this is the largest retrospective study to date on the risk factors associated with radiolucent foreign body inhalation in adults.
Conclusion
Unlike radiopaque FBA, in those presenting with a suspected radiolucent foreign body aspiration, the diagnosis is far more challenging. This study identifies a few risk factors that have the potential to facilitate an early diagnosis of radiolucent foreign body inhalation in adults. Further prospective multicenter studies should be conducted to validate the findings.
Availability of data and materials
The data that support the findings of this study are available from Xioafan Liu upon reasonable request and with permission of The Central Hospital of Wuhan, Hubei, China.
Abbreviations
- FBA:
-
Foreign body aspiration
- MDCT:
-
Multi-detector Computed Tomography
References
Salih AM, Alfaki M, Alam-Elhuda DM. Airway foreign bodies: a critical review for a common pediatric emergency. World J Emerg Med. 2016;7(1):5–12.
Gregori D, Salerni L, Scarinzi C, et al. Foreign bodies in the upper airways causing complications and requiring hospitalization in children aged 0–14 years: results from the ESFBI study. Eur Arch Otorhinolaryngol. 2008;265(8):971–8.
Na’ara S, Vainer I, Amit M, Gordin A. Foreign body aspiration in infants and older children: a comparative study. Ear Nose Throat J. 2020;99(1):47–51.
Ulas AB, Aydin Y, Eroglu A. Foreign body aspirations in children and adults. Am J Surg. 2022. https://doi.org/10.1016/j.amjsurg.2022.05.032.
Sehgal IS, Dhooria S, Ram B, et al. Foreign body inhalation in the adult population: experience of 25,998 bronchoscopies and systematic review of the literature. Respir Care. 2015;60(10):1438–48.
Baharloo F, Veyckemans F, Francis C, Biettlot MP, Rodenstein DO. Tracheobronchial foreign bodies: presentation and management in children and adults. Chest. 1999;115(5):1357–62.
Hsu W, Sheen T, Lin C, Tan C, Yeh T, Lee S. Clinical experiences of removing foreign bodies in the airway and esophagus with a rigid endoscope: a series of 3217 cases from 1970 to 1996. Otolaryngol Head Neck Surg. 2000;122(3):450–4.
Hewlett JC, Rickman OB, Lentz RJ, Prakash UB, Maldonado F. Foreign body aspiration in adult airways: therapeutic approach. J Thorac Dis. 2017;9(9):3398–409.
Limper AH, Prakash UB. Tracheobronchial foreign bodies in adults. Ann Intern Med. 1990;112(8):604–9.
Lin L, Lv L, Wang Y, Zha X, Tang F, Liu X. The clinical features of foreign body aspiration into the lower airway in geriatric patients. Clin Interv Aging. 2014;9:1613–8.
Kosutova P, Mikolka P. Aspiration syndromes and associated lung injury: incidence, pathophysiology and management. Physiol Res. 2021;70(Suppl4):S567–83.
Chen CH, Lai CL, Tsai TT, Lee YC, Perng RP. Foreign body aspiration into the lower airway in Chinese adults. Chest. 1997;112(1):129–33.
Mise K, JurcevSavicevic A, Pavlov N, Jankovic S. Removal of tracheobronchial foreign bodies in adults using flexible bronchoscopy: experience 1995–2006. Surg Endosc. 2009;23(6):1360–4.
Donado Una JR, de Miguel PE, Casado Lopez ME, Alfaro Abreu JJ. Fiber optic bronchoscopy in extraction of tracheo-bronchial foreign bodies in adults. Arch Bronconeumol. 1998;34(2):76–81.
Ben-Dov I, Aelony Y. Foreign body aspiration in the adult: an occult cause of chronic pulmonary symptoms. Postgrad Med J. 1989;65(763):299–301.
Reyad HM, El-Deeb ME, Abbas AM, Sherief D, Elagamy OA. Foreign body aspiration in Egyptian children clinical, radiological and bronchoscopic findings. J Multidiscip Healthc. 2021;14:2299–305.
Sersar SI, Rizk WH, Bilal M, et al. Inhaled foreign bodies: presentation, management and value of history and plain chest radiography in delayed presentation. Otolaryngol Head Neck Surg. 2006;134(1):92–9.
Ibrahim Sersar S, Hamza UA, AbdelHameed WA, et al. Inhaled foreign bodies: management according to early or late presentation. Eur J Cardiothorac Surg. 2005;28(3):369–74.
Courvoisier DS, Combescure C, Agoritsas T, Gayet-Ageron A, Perneger TV. Performance of logistic regression modeling: beyond the number of events per variable, the role of data structure. J Clin Epidemiol. 2011;64(9):993–1000.
Agoritsas T, Merglen A, Shah ND, O’Donnell M, Guyatt GH. Adjusted analyses in studies addressing therapy and harm: users’ guides to the medical literature. JAMA. 2017;317(7):748–59.
Wu X, Liu X, Zhou Y, et al. 3-month, 6-month, 9-month, and 12-month respiratory outcomes in patients following COVID-19-related hospitalisation: a prospective study. Lancet Respir Med. 2021;9(7):747–54.
Liu X, Zhou H, Zhou Y, et al. Risk factors associated with disease severity and length of hospital stay in COVID-19 patients. J Infect. 2020;81(1):e95–7.
Wu X, Wang T, Zhou Y, et al. Different laboratory abnormalities in COVID-19 patients with hypertension or diabetes. Virol Sin. 2020;35(6):853–6.
Liu X, Zhou H, Zhou Y, et al. Temporal radiographic changes in COVID-19 patients: relationship to disease severity and viral clearance. Sci Rep. 2020;10(1):10263.
Ramos MB, Fernandez-Villar A, Rivo JE, et al. Extraction of airway foreign bodies in adults: experience from 1987–2008. Interact Cardiovasc Thorac Surg. 2009;9(3):402–5.
Lan RS. Non-asphyxiating tracheobronchial foreign bodies in adults. Eur Respir J. 1994;7(3):510–4.
Boyd M, Chatterjee A, Chiles C, Chin R Jr. Tracheobronchial foreign body aspiration in adults. South Med J. 2009;102(2):171–4.
Sancho-Chust JN, Molina V, Vanes S, Pulido AM, Maestre L, Chiner E. Utility of flexible bronchoscopy for airway foreign bodies removal in adults. J Clin Med. 2020. https://doi.org/10.3390/jcm9051409.
Hsu AA. Endoscopic intervention of lower airway foreign matter in adults-a different perspective. J Thorac Dis. 2015;7(10):1870–7.
Choroomi S, Curotta J. Foreign body aspiration and language spoken at home: 10-year review. J Laryngol Otol. 2011;125(7):719–23.
Gendeh BS, Gendeh HS, Purnima S, Comoretto RI, Gregori D, Gulati A. Inhaled foreign body impaction: a review of literature in malaysian children. Indian J Pediatr. 2019;86(Suppl 1):20–4.
Zissin R, Shapiro-Feinberg M, Rozenman J, Apter S, Smorjik J, Hertz M. CT findings of the chest in adults with aspirated foreign bodies. Eur Radiol. 2001;11(4):606–11.
Zhong B, Sun SL, Du JT, et al. Risk factors for lower respiratory tract infection in children with tracheobronchial foreign body aspiration. Medicine (Baltimore). 2019;98(10): e14655.
Piovesan A, Vancauwenberghe V, Van De Looverbosch T, Verboven P, Nicolai B. X-ray computed tomography for 3D plant imaging. Trends Plant Sci. 2021;26(11):1171–85.
Marin-Diez E, Landeras Alvaro RM, Lamagrande Obregon A, Pelaz Esteban M, Gallardo AE. Ultrasonography of subcutaneous foreign bodies: differences depending on their nature, complications, and potential diagnostic errors. Radiologia (Engl Ed). 2020;62(1):3–12.
Dindar H, Konkan R, Cakmak M, Barlas M, Gokcora H, Yucesan S. A bronchopleurocutaneous fistula caused by an unusual foreign body aspiration simulating acute abdomen. Eur J Pediatr. 1994;153(2):136–7.
Freiman MA, McMurray JS. Unique presentation of a bronchial foreign body in an asymptomatic child. Ann Otol Rhinol Laryngol. 2001;110(6):495–7.
Mehta AC, Khemasuwan D. A foreign body of a different kind: pill aspiration. Ann Thorac Med. 2014;9(1):1–2.
Blanco Ramos M, Botana-Rial M, Garcia-Fontan E, Fernandez-Villar A, Gallas TM. Update in the extraction of airway foreign bodies in adults. J Thorac Dis. 2016;8(11):3452–6.
Mi W, Zhang C, Wang H, et al. Measurement and analysis of the tracheobronchial tree in Chinese population using computed tomography. PLoS ONE. 2015;10(4): e0123177.
Acknowledgements
We acknowledge all the patients involved in this study. For the purpose of open access, the authors have applied a CC-BY public copyright license to any Author Accepted Manuscript version arising from this submission.
Funding
YW was funded by the UK Medical Research Council (MR/S025480/1) and the UK Royal Society (IEC\NSFC\191030). CS was funded by the National Natural Science Foundation of China (81800064), Science project of the Wuhan Bureau of Science and Technology (2020020601012322), and Science project of the Wuhan Health Commission (WX20Q11). The funding bodies and sponsors had no role in the design and conduct of the study; collection, management, analysis, or interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
YW, YH, and XL had the idea for and designed the study. All authors had full access to the data and had final responsibility for the decision to submit it for publication. YW, YH, XL, FN, TG, and FJ drafted the paper. TG, FJ, XL, FN, YH, and YW did the analysis and all authors critically revised the manuscript for important intellectual content and gave final approval for the version to be published. XL, FN, YJ, CS, MYuan, ZT, MYe, JX, YingW, and QQ collected the data. All authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Ethics Committee of the Central Hospital of Wuhan, Hubei, China (Approval No.: WHZXKYL2022-052). Informed consent was not deemed necessary owing to the retrospective nature of the study.
Consent for publications
Not applicable.
Competing interests
The authors declare that they have no conflicts of interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Methods.
Flexible bronchoscopy. Table S1. Bronchoscopy findings. Table S2. Univariate logistic regression analysis for risk factors associated with radiolucent FBA in adults. Table S3. Multivariable logistic regression analysis for risk factors associated with radiolucent FBA in adults.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Liu, X., Ni, F., Guo, T. et al. Risk factors associated with radiolucent foreign body inhalation in adults: a 10-year retrospective cohort study. Respir Res 23, 238 (2022). https://doi.org/10.1186/s12931-022-02165-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12931-022-02165-9