Abstract
Background
Bronchial Thermoplasty (BT) is an endoscopic treatment for severe asthma using radiofrequency energy to target airway remodeling including smooth muscle. The correlation of pulmonary function tests and BT response are largely unknown. Forced Oscillation Technique (FOT) is an effort-independent technique to assess respiratory resistance (Rrs) by using pressure oscillations including small airways.
Aim
To investigate the effect of BT on pulmonary function, assessed by spirometry, bodyplethysmography and FOT and explore associations between pulmonary function parameters and BT treatment response.
Methods
Severe asthma patients recruited to the TASMA trial were analyzed in this observational cohort study. Spirometry, bodyplethysmography and FOT measurements were performed before and 6 months after BT. Asthma questionnaires (AQLQ/ACQ-6) were used to assess treatment response.
Results
Twenty-four patients were analyzed. AQLQ and ACQ improved significantly 6 months after BT (AQLQ 4.15 (±0.96) to 4.90 (±1.14) and ACQ 2.64 (±0.60) to 2.11 (±1.04), p = 0.004 and p = 0.02 respectively). Pulmonary function parameters remained stable. Improvement in FEV1 correlated with AQLQ change (r = 0.45 p = 0.03). Lower respiratory resistance (Rrs) at baseline (both 5 Hz and 19 Hz) significantly correlated to AQLQ improvement (r = − 0.52 and r = − 0.53 respectively, p = 0.01 (both)). Borderline significant correlations with ACQ improvement were found (r = 0.30 p = 0.16 for 5 Hz and r = 0.41 p = 0.05 for 19 Hz).
Conclusion
Pulmonary function remained stable after BT. Improvement in FEV1 correlated with asthma questionnaires improvement including AQLQ. Lower FOT-measured respiratory resistance at baseline was associated with favorable BT response, which might reflect targeting of larger airways with BT.
Trial registration
ClinicalTrials.gov Identifier: NCT02225392; Registered 26 August 2014.
Similar content being viewed by others
Introduction
Bronchial Thermoplasty (BT) is an endoscopic treatment for patients with severe asthma. It uses radiofrequency energy delivered to the medium and larger airways to reduce airway smooth muscle (ASM) mass [1,2,3,4,5]. Several studies have shown an improvement in asthma quality of life, asthma control, and a reduction in exacerbations after BT [6,7,8]. The exact mechanism of action however is still incompletely understood and patient responder profile remains under debate.
Pulmonary function measurements before and after BT have shown various results and correlations with treatment response have not been explored comprehensively. The large clinical trials and long term follow up studies thereafter showed a stable one-second forced expiratory volume (FEV1) up to 5 years after BT with only the RISA trial showing an improvement in FEV1 6 months after BT [6,7,8].
Forced Oscillation Technique (FOT) is an effort-independent technique using various pressure oscillations to assess the relation between flow and pressure in the respiratory system [9]. It has been postulated that FOT is more accurate in detecting small airways disease than conventional tests such as spirometry [10, 11]. Additionally, while with bodyplethysmography the airway resistance is calculated by combining the flow with alveolar pressure, FOT measures the resistance of the entire respiratory system including the surrounding tissue and small airways [12].
This study hypothesized that the BT-induced reduction of ASM in the larger airways influences the mechanical properties of the asthmatic airways. The aims of this trial are (1) to assess the effect of BT on pulmonary function parameters as assessed by spirometry, bodyplethysmography-determined airway resistance and FOT; (2) to evaluate whether pulmonary function parameters are related to BT response.
Methods
Subjects
Patients fulfilling the World Health Organization (WHO) and Innovative Medicine Initiative (IMI) criteria for severe refractory asthma and scheduled for BT and pulmonary function tests including FOT between December 2014 and September 2018 were included (Clinical trials.gov NCT02225392) [13, 14]. Ethical approval was provided by the Medical Ethics Committee of the Academic Medical Center Amsterdam (NL45394.018.13) and written informed consent was obtained. Asthma medication remained stable during the study period.
Bronchial thermoplasty
Patients were treated with BT according to current guidelines using the Alair System (Boston Scientific, USA) [15,16,17] and under conscious sedation (remifentanil/propofol) [18] or general anesthesia. Prednisolone 50 mg was started 3 days before treatment, on the day itself and 1 day thereafter.
Methods of measurement
All pulmonary function tests were performed in the morning and conducted by experienced staff according to ERS/ATS standards using Jaeger Masterlab software (Erich Jaeger GmbH, Wurtzburg, Germany). The measurements were performed during two visits: one visit before and one visit 6 months after treatment. During the visits, short acting bronchodilators were stopped for at least 6 hours. Long acting beta agonists (LABA) were continued. Spirometry, bodyplethysmography and FOT measurements were performed both before and after administration of 400 μg salbutamol. FOT was performed in an upright position with the Resmon Pro device using a pseudorandom noise signal (Restech, Italy). The subjects received a nose-clip and patients were instructed to support their cheeks with their hands while breathing tidal for 3 min. This measurement was performed twice and the average was used in the analysis.
Outcome parameters
The main outcome parameter of this study was the change in pulmonary function assessed by spirometry, bodyplethysmography and FOT. Other outcome parameters were the correlations between baseline and change in pulmonary function parameters and baseline and change in asthma quality of life questionnaires (AQLQ) and asthma control (ACQ-6) [19, 20]. Changes in pulmonary function parameters or asthma questionnaires were defined as post-BT minus pre-BT values. A decrease of 0.5 points on AQLQ and an increase of 0.5 points on ACQ-6 is designated as clinically relevant.
Statistical analysis
GraphPad Prism version 5.01 (GraphPad Software Inc., San Diego, CA, USA) was used for the analysis. Grouped data were reported as mean with standard deviation or median with interquartile ranges, as appropriate. Within group analyses were performed with paired t-tests or Wilcoxon signed rank tests. Correlation analyses were performed with Spearman’s rho coefficient. P-values were two sided and a statistical significance was set at p < 0.05.
Results
Subjects and clinical outcome
BT and pulmonary function tests including FOT were performed in 26 patients. Two patients were excluded from analyses due to lost to follow up at the 6 months visit. Baseline characteristics of the included 24 patients are shown in Table 1. Due to claustrophobia one patient was excluded from bodyplethysmography analyses. In FOT analysis, one patient was excluded due to extreme coughing and in one other patient only post-bronchodilator measurements were performed. BT significantly improved quality of life and asthma control. AQLQ questionnaires improved from 4.15 (±0.96) to 4.90 (±1.14) (p = 0.004) and ACQ questionnaires improved from 2.64 (±0.60) to 2.11 (±1.04) (p = 0.02).
Pulmonary function measurements
The effect of BT on spirometry and bodyplethysmography parameters are shown in Table 2. FEV1 did not significantly change after BT. FVC (% of predicted, pre-bronchodilator) was slightly increased after BT, with a stable FEV1 resulting in a reciprocal decrease in FEV1/FVC. Additionally, a minimal increase in post bronchodilator airway resistance was found (before BT 0.15 (0.14;0.21) kPa*s/L versus after BT 0.23 (0.16;0.24) kPa*s/L (p < 0.05)).
Total group analyses of FOT measurements did not show a change in respiratory resistance (Rrs) and reactance (Xrs) after BT for both 5 Hz and 19 Hz (Table 3).
Correlation analyses
Associations between asthma questionnaires and pulmonary function parameters were explored.
Asthma questionnaires and spirometry parameters
No significant correlations were found at baseline before BT between asthma questionnaires and spirometry parameters. After BT, improvements in AQLQ and ACQ showed a correlation with baseline FEV1 reversibility (for AQLQ r = 0.42 p = 0.05 and for ACQ r = − 0.45 p = 0.03) but not with baseline FEV1. Additionally, after BT improvements in asthma questionnaires were correlated with improvements in pre-bronchodilator FEV1 (% predicted) (r = 0.45 p = 0.03 for AQLQ and r = − 0.37 p = 0.08 for ACQ) (Fig. 1a and b) but not with post-bronchodilator FEV1.
Correlation between asthma questionnaire AQLQ and ACQ-6 changes and pre-BD FEV1(% predicted) change after BT. An improvement in AQLQ (n = 22) (a) and ACQ (n = 23) (b) is correlated with post-BT change in FEV1 (%) pre-BD. FEV1, forced expiratory volume in 1 s; BD, bronchodilation; BT, Bronchial Thermoplasty; AQLQ, asthma quality of life questionnaire; ACQ, asthma control questionnaire
Asthma questionnaires and bodyplethysmography
Regarding bodyplethysmography, a correlation was found between baseline AQLQ and baseline airway resistance (Raw) (n = 23, r = 0.56 for both pre-BD and post-BD; p < 0.01). Baseline measurements of airway resistance were not correlated with baseline ACQ. No correlations were found between changes in AQLQ and ACQ questionnaires and airway resistance measured with bodyplethysmography.
Asthma questionnaires and respiratory resistance
Similar correlations were found for respiratory resistance measured with FOT at both 5hz and 19 Hz. Baseline AQLQ scores showed a significant positive correlation with respiratory resistance at 19 Hz (r = 0.67 p = 0.0005 for pre-bronchodilator Rrs and r = 0.57 p = 0.005 for post-bronchodilator Rrs) and a trend between baseline AQLQ and pre-bronchodilator respiratory resistance at 5 Hz (r = 0.36; p = 0.09). Baseline ACQ scores were not correlated to baseline FOT measurements.
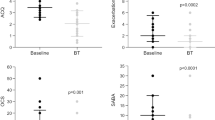
Next the correlation between changes in asthma questionnaires and baseline respiratory resistance were analyzed. AQLQ improvement was negatively correlated with baseline pre-bronchodilator respiratory resistance (Rrs at 5 Hz r = − 0.52 p = 0.01; Rrs at 19 Hz r = − 0.53 p = 0.01) (Fig. 2a-b) and baseline post-bronchodilator respiratory resistance (Rrs at 5hz r = − 0.43 p = 0.04; Rrs at 19 Hz r = − 0.55 p = 0.01). A positive trend was found between ACQ improvement and baseline pre-bronchodilator respiratory resistance at both 5 Hz (r = 0.30 p = 0.16) and 19 Hz (r = 0.41 p = 0.05) (Fig. 2c-d).
Associations between asthma questionnaire AQLQ and ACQ-6 changes and respiratory resistance measured with FOT at baseline (5 Hz and 19 Hz). A negative correlation was found between AQLQ improvement and baseline respiratory resistance at both 5 Hz (a) and 19 Hz (b). A positive correlation was seen between ACQ improvement and baseline respiratory resistance at both 5 Hz (c) and 19 Hz (d). FOT, forced oscillation technique; AQLQ, asthma quality of life questionnaire; ACQ, asthma control questionnaire; Rrs, respiratory resistance in cmH2O.s/L; BT, bronchial thermoplasty; BD, bronchodilation
Asthma questionnaires and airway reactance
Correlations between asthma questionnaires and reactance measurements were only found for AQLQ and reactance at 5 Hz: baseline AQLQ was negatively correlated with airway reactance (r = − 0.42; p = 0.05) and improvement of AQLQ was correlated with a higher reactance at baseline (r = 0.48; p = 0.02). No significant correlation between baseline / change ACQ and airway reactance was found.
Discussion
This study aimed to investigate the effect of BT on pulmonary function and to explore whether these pulmonary function parameters were associated with BT response. An improvement in asthma control and quality of life was found while overall pulmonary function parameters remained stable. More importantly, this is the first study showing that a low respiratory resistance, measured with FOT, correlated to BT-response. These results can contribute to improved patient selection for BT.
Comparable to previously published larger trials [8, 21], spirometry parameters overall remained stable. A slight increase in pre-bronchodilator FVC (% predicted) and decrease in post-bronchodilator FEV1/FVC after BT were found, although significantly different, the clinical relevance of these small differences is questionable. For the first time however, correlations were found between asthma questionnaire (AQLQ and ACQ) changes and FEV1 change. Although the differences were small, these data suggest that spirometry might improve after BT as previously shown in the RISA trial [7]. In our study, this improvement in FEV1 was only visible in the patients that responded well to BT. This correlation was also explored, but not found in an Australian cohort of severe asthma patients [22]. An explanation can be the difference in baseline characteristics between both cohorts, with a more obstructive asthma phenotype in the Australian cohort compared to the present study (FEV1 (% predicted) of 55% compared to 88%).
When taking all patient data into account a significant increase was found after BT in post-bronchodilator bodyplethysmography airway resistance. This increase is mainly caused by one patient, who gained 7 kg during follow-up, which could explain this outcome. Similar to Langton et al. [23] no significant differences in FOT measurements were found after BT in our study. However, a positive correlation was found between airway and respiratory resistance measured with both bodyplethysmography and FOT and AQLQ questionnaires at baseline. For ACQ this correlation was not present. The mechanism underlying this result needs to be further explored.
An important finding of this study is the correlation between improvements on AQLQ and ACQ and respiratory resistance measured with FOT. In this study, patients with a higher respiratory resistance at baseline showed less improvements on both questionnaires after BT compared to patients with a lower resistance. Conventional spirometry and bodyplethysmography-determined airway resistance did not show this correlation. A possible explanation for this difference might be that FOT measures the respiratory resistance of the entire respiratory system, including smaller airways and surrounding tissue. Non-responding patients might be the patients with a higher resistance in surrounding tissue, potentially in the smaller distal airways which are not reached by the BT catheter. Consequently, patients with lower respiratory resistance at baseline might be the patients to select for BT treatment.
An improvement in the respiratory resistance was not observed. Other recently published studies however did show an improvement of ventilation homogeneity after BT [24] and effects of BT on airtrapping parameters with pulmonary function tests [22] and Computed Tomography [25,26,27] indicating a BT-effect in the peripheral parts of the airways. To measure the resistance in the smaller airways, FOT alone is probably not sufficient. The assessment of small airways disease and/or the effect on the smaller airways of BT might be more accurate when combining multiple techniques together such as CT, FOT and/or impulse oscillometry (IOS) as currently investigated by the Atlantis study group [28].
There are limitations to this study that need to be addressed. The results in this study are part of the TASMA study, a multicenter study, however FOT measurements were only performed in one center. Therefore the present study included patients from one center only. Although single center results, the included group was clinically heterogeneous with allergic, eosinophilic and non-allergic/non-eosinophilic patients included. Additionally, patients were referred to this center from all parts of the Netherlands, thereby decreasing the effect of environmental factors on the outcome. Another limitation is the relatively small number of included patients. Although results need to be confirmed in larger trials, this study does offer important insights that may help to improve patient selection in the future. Strong points of this study are using not only conventional methods to assess lung function parameters but also use FOT, a method known to give a more reliable result on peripheral airway resistance. Also by keeping the medication use stable during follow up, and not start tapering down, which could influence the results, strengthens the observed measurements.
Conclusion
Pulmonary function parameters, including FOT, remained stable after BT. Correlations were found between FEV1 improvement and asthma questionnaires improvement including AQLQ. Additionally, a lower respiratory resistance at baseline, measured with FOT, was associated with a favorable BT-response, which might reflect the main targeting of BT on the larger airways. These results add to understanding the mechanism of action of BT and might contribute to improved patient selection for this treatment.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ACQ:
-
Asthma control questionnaire
- AQLQ:
-
Asthma quality of life questionnaire
- ASM:
-
Airway smooth muscle
- BT:
-
Bronchial thermoplasty
- CT:
-
Computed tomography
- FEV1:
-
Forced expiratory volume in 1 s
- FOT:
-
Forced oscillation technique
- FVC:
-
Forced vital capacity
- IMI:
-
Innovative medicine initiative
- IQR:
-
Interquartile range
- Rrs:
-
Respiratory resistance
- WHO:
-
World health organization
- Xrs:
-
Reactance
References
Pretolani M, Dombret MC, Thabut G, Knap D, Hamidi F, Debray MP, et al. Reduction of airway smooth muscle mass by bronchial thermoplasty in patients with severe asthma. Am J Respir Crit Care Med. 2014;190:1452–4.
Denner DR, Doeing DC, Hogarth DK, Dugan K, Naureckas ET, White SR. Airway inflammation after bronchial thermoplasty for severe asthma. Ann Am Thorac Soc. 2015;12:1302–9.
Chakir J, Haj-Salem I, Gras D, Joubert P, Beaudoin EL, Biardel S, et al. Effects of bronchial thermoplasty on airway smooth muscle and collagen deposition in asthma. Ann Am Thorac Soc. 2015;12:1612–8.
Pretolani M, Bergqvist A, Thabut G, Dombret MC, Knapp D, Hamidi F, et al. Effectiveness of bronchial thermoplasty in patients with severe refractory asthma: clinical and histopathologic correlations. J Allergy Clin Immunol. 2017;139:1176–85.
d’Hooghe JNS, Goorsenberg AWM, ten Hacken NHT, Weersink EJM, Roelofs JJTH, Mauad D, et al. Airway smooth muscle reduction after bronchial thermoplasty in severe asthma correlates with FEV1. Clin Exp Immunol. 2019;49(4):541–4.
Cox G, Thomson NC, Rubin AS, Niven RM, Corris PA, Siersted HC, et al. Asthma control during the year after bronchial thermoplasty. N Engl J Med. 2007;356:1327–37.
Pavord ID, Cox G, Thomson NC, Rubin AS, Corris PA, Niven RM, et al. Safety and efficacy of bronchial thermoplasty in symptomatic, severe asthma. Am J Respir Crit Care Med. 2007;176:1185–91.
Castro M, Rubin AS, Laviolette M, Fiterman J, De Andrade LM, Shah PL, et al. Effectiveness and safety of bronchial thermoplasty in the treatment of severe asthma: a multicenter, randomized, double-blind, sham-controlled clinical trial. Am J Respir Crit Care Med. 2010;181:116–24.
Oostveen E, MacLeod D, Lorino H, Farre R, Hantos Z, Desager K, et al. The forced oscillation technique in clinical practice: methodology, recommendations and future developments. Eur Respir J. 2003;22:1026–41.
McNulty W, Usmani OS. Techniques of assessing small airways dysfunction. Eur Clin Respir J. 2014. https://doi.org/10.3402/ecrj.v1.25898.
Anderson WJ, Zajda E, Lipworth BJ. Are we overlooking persistent small airways dysfunction in community-managed asthma? Ann Allergy Asthma Immunol. 2012;109(3):185–9.
Kaminsky DA, Bates JHT. Breathing In and Out: Airway Resistance. In: Kaminsky DA, Irvin CG, editors. Pulmonary Function Testing. Principles and Practice. Cham: Humana press; 2018. p. 127–50.
Bousquet J, Mantzouranis E, Cruz, Ait-Khaled N, Baena-Cagnani CE, Bleecker ER, et al. Uniform definition of asthma severity, control, and exacerbations: document presented for the World Health Organization Consultation on Severe Asthma. J Allergy Clin Immunol. 2010;126:926–38.
Bel EH, Sousa A, Fleming L, Bush A, Chung KF, Versnel J, et al. Diagnosis and definition of severe refractory asthma: an international consensus statement from the innovative medicine initiative (IMI). Thorax. 2011;66:910–7.
Cox G, Miller JD, McWilliams A, Fitzgerald JM, Lam S. Bronchial thermoplasty for asthma. Am J Respir Crit Care Med. 2006;173:965–9.
d’Hooghe JNS, Ten Hacken NHT, Weersink EJM, Sterk PJ, Annema JT, Bonta PI. Emerging understanding of the mechanism of action of bronchial thermoplasty in asthma. Pharmacol Ther. 2018;181:101–7.
Bonta PI, Chanez P, Annema JT, Shah PL, Niven R. Bronchial thermoplasty in severe asthma: best practice recommendations from an expert panel. Respiration. 2018;95(5):289–300.
d’Hooghe JN, Eberl S, Annema JT, Bonta PI. Propofol and remifentanil sedation for bronchial thermoplasty: a prospective cohort trial. Respiration. 2017;93:58–64.
Juniper EF, O'Byrne PM, Guyatt GH, Ferrie PJ, King DR. Development and validation of a questionnaire to measure asthma control. Eur Respir J. 1999;14(4):902–7.
Juniper EF, Buist AS, Cox FM, Ferrie PJ, King DR. Validation of a standardized version of the asthma quality of life questionnaire. Chest. 1999;115:1265–70.
Chupp G, Laviolette M, Cohn L, McEvoy C, Bansal S, Shifren A, et al. Long-term outcomes of bronchial thermoplasty in subjects with severe asthma: a comparison of 3-year follow-up results from two prospective multicentre studies. Eur Respir J. 2017;(2):50. https://doi.org/10.1183/13993003.00017-2017.
Langton D, Ing A, Bennetts K, Wang W, Farah C, Peters M, et al. Bronchial thermoplasty reduces gas trapping in severe asthma. BMC Pulm Med. 2018;18:155.
Langton D, Ing A, Sha J, Bennetts K, Hersch N, Kwok M, et al. Measuring the effects of bronchial thermoplasty using oscillometry. Respirology. 2018;24(5):431–6.
Donovan GM, Elliot JG, Green FHY, James AL, Noble PB. Unravelling a clinical paradox – why does bronchial thermoplasty work in asthma? Am J Respir Cell Mol Biol. 2018;59:355–62.
Zanon M, Strieder DL, Rubin AS, Watte G, Marchiori E, Cardoso PFG, et al. Use of MDCT to assess the results of bronchial Thermoplasty. Am J Roentgenol. 2017;209(4):752–6.
Konietzke P, Weinheimer O, Wielputz MO, Wagner WL, Kaukel P, Eberhardt R, et al. Quantitative CT detects changes in airway dimensions and air-trapping after bronchial thermoplasty for severe asthma. Eur J Radiol. 2018;107:33–8.
Ishii S, Iikura M, Shimoda Y, Izumi S, Hojo M, Sugiyama H. Evaluation of expiratory capacity with severe asthma following bronchial thermoplasty. Respirol Case Rep. 2018;7(1):e00387.
Postma DS, Brightling C, Baldi S, Van den Berge M, Fabbri LM, Gagnatelli A, et al. Exploring the relevance and extent of small airways dysfunction in asthma (ATLANTIS): baseline data form a prospective cohort study. Lancet Respir Med. 2019;7(5):402–16.
Acknowledgements
Not applicable.
Funding
The TASMA study is funded by the Dutch Lung Foundation (grant number 5.2.13.064JO), the Netherlands Organization for Health Research and Development (ZonMw) (grant number 90713477) and Boston Scientific. The sponsors had no role in the design of the study, the data collection and analysis or the preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
JNSdH, PIB and JTA conceived and designed the study. AWMG and JNSdH acquired the data. AWMG analyzed the data and drafted the manuscript. AMS and JGvdA contributed substantially with the interpretation of the data. All authors revised the manuscript for important intellectual content and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval was provided by the Medical Ethics Committee of the Academic Medical Center Amsterdam (NL45394.018.13) and informed consent obtained from all participants.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Data from this article have been partly presented during the European Respiratory Society international congress in Paris, September 18th 2018.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Goorsenberg, A.W.M., d’Hooghe, J.N.S., Slats, A.M. et al. Resistance of the respiratory system measured with forced oscillation technique (FOT) correlates with bronchial thermoplasty response. Respir Res 21, 52 (2020). https://doi.org/10.1186/s12931-020-1313-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12931-020-1313-6