Abstract
Background
Although reduced function of the respiratory system limits peak oxygen uptake in diseases affecting the lungs or airways, the healthy respiratory system is thought to have a spare capacity for oxygen transport and uptake, and is not considered a limiting factor for peak oxygen uptake in healthy people. However, lung function declines with age and could theoretically limit peak oxygen uptake in elderly. We examined the association between peak oxygen uptake and lung function indices in an elderly population with the hypothesis that lung function indices would be associated with VO2peak up to a threshold value situated above the lower limits of normal lung function for our population.
Methods
Spirometry, gas diffusion tests and incremental work tests were performed in 1443 subjects (714 women) aged 69–77 years. Association between lung function indices and peak oxygen uptake was studied with hockey-stick regression.
Results
Forced expiratory volume in 1 s (FEV1) had a positive association with peak oxygen uptake up to, but not above, a threshold value of 2.86 l for men, and 2.13 l for women (lower limit of normal 2.73 and 1.77 l respectively). A corresponding threshold was found for diffusing capacity of the lung for carbon monoxide (DLCO) for men at 9.18 mmol/min/kPa (lower limit of normal 6.84 mmol/min/kPa). DLCO for women and DLCO divided by alveolar volume (DLCO/VA) for both sexes had a significant linear relationship to VO2peak (p < 0.05), but no significant threshold value was found in these associations.
Conclusions
Threshold values for FEV1 for both sexes and DLCO for men were identified. These lung function indices had a positive association with VO2peak up to these threshold values, but not above. The identified threshold values were above lower limits of normal for FEV1 and DLCO.
Similar content being viewed by others
Background
It is generally accepted that maximal cardiac output is the principal limiting factor for peak oxygen uptake (VO2peak) in healthy individuals exercising at sea-level. By contrast the respiratory system has been considered to be structurally overbuilt both with respect to dynamic lung function and diffusion capacity, and is therefore believed not to restrict oxygen uptake even during maximal exercise in non-endurance athletes [1, 2]. Reduced lung function limits VO2peak in patients with pulmonary disease [3–7], but the association with VO2peak for lung function indices within the normal range is little studied.
In healthy ageing there is a steady decline of dynamic lung volumes. Expiratory flow is reduced and the flow-volume curve may resemble what is found in patients with chronic obstructive pulmonary disease [8]. The capacity of the lung for gas diffusion is also reduced with age [9]. Elderly have an increased dead space to tidal volume ventilation ratio compared to younger individuals and develop a marked alveolar to arterial oxygen gradient during exercise [10]. The spare capacity of the respiratory system is possibly reduced in elderly compared to middle-aged and young people, and both dynamic lung function and the diffusion capacity of the lungs may therefore be associated with reduced oxygen uptake even in healthy elderly people. This has previously not been examined in population based studies.
Given that the healthy respiratory system is overbuilt with respect to requirements for oxygen uptake, one would observe an association between lung function and VO2peak only when the capacity of the respiratory system is reduced below a threshold value which is below the lower limits of normal lung function. However, if the spare capacity of lung function is reduced with increasing age, this threshold may be found within the range of normal lung function in an elderly population, in that case suggesting that VO2peak may be limited by lung function in many healthy elderly. The present study examined the association between VO2peak and parameters from spirometry and gas diffusion tests in a large population based sample of elderly men and women.
We wanted to investigate if lung function indices were associated with VO2peak up to a threshold value above which further increase in lung function would not be associated with increasing VO2peak. If a threshold value were identified, we hypothesized that this threshold would be above the LLN (lower limits of normal) for lung function, i.e. within the normal range of lung function for this population.
Methods
Study population
The ongoing Generation 100 Study invited all inhabitants in the city of Trondheim, Norway, born between 01 January 1936 and 31 December 1942 (n = 6966) to a randomized controlled trial on the effect of exercise intervention on morbidity and mortality in an ageing population [11]. Study subjects were included from August 2012 to June 2013 giving a study population aged 69–77 years. The present study includes baseline data of participants that were able to perform exercise testing and training. Participants with chronic communicable infectious diseases, dementia, uncontrolled hypertension, heart failure, cardiomyopathy, severe arrhythmia, participating in other studies conflicting with Generation 100, or with conditions or test results indicating that testing or training could be unsafe were excluded. The Generation 100 Study and the present sub-study were approved by the Regional Committee for Medical Research Ethics (REK 2012/381 B) and all participants gave written informed consents.
Examinations
A symptom-limited incremental work test on a treadmill was performed to measure VO2peak using MetaMax II (Cortex, Leipzig, Germany) or Oxycon Pro (Erich Jaeger, Hoechberg, Germany) as previously described [12]. Participants not able to perform the test on a treadmill due to poor balance or other reasons performed the test on a cycle ergometer. Load was increased 1 km/h or 2 % inclination on the treadmill approximately every 90 s until exhaustion, on the bicycle load was increased 10 W every 30 s. Testing of participants with suspected or previously diagnosed heart disease was supervised by a trained physician [13]. For simplicity the term VO2peak is used throughout this paper, even when referring to work by others that have reported maximum oxygen uptake. The participants reported average physical activity by answering three questions covering frequency, intensity and duration of physical activity. The answers were given different weights and a physical activity index was calculated as previously described [14].
Spirometry and gas diffusion test were performed with Sensormedics Vmax22 Encore (CareFusion, San Diego, USA) in accordance with the American Thoracic Society/European Respiratory Society recommendations [15, 16]. The spirometer was calibrated daily. The study participants performed up to a maximum of eight spirometry trials until forced expiratory volume at 1 s (FEV1) and forced vital capacity (FVC) showed <150 ml variation between the two highest results. The highest values for vital capacity (forced expiratory or inspiratory) and FEV1 were recorded. No reversibility test was performed. For the day of testing, participants were instructed to continue any medication as usual, including anti-obstructive treatment. Predicted values and lower limit of normal (LLN) were calculated from Norwegian reference equations using age, sex and height [17].
Diffusing capacity of the lung for carbon monoxide (DLCO) was measured by the single breath-method using a gas mixture containing 0.3 % carbon monoxide and 0.3 % methane. Estimated alveolar volume (VA) was calculated based on the dilution of methane from inspired to expired gas. The procedure was repeated with at least 4 min between each trial up to a maximum of 4 trials, until two tests of acceptable quality show DLCO within 1 mmol/min/kPa or within 10 % of the highest value and the mean of these values were recorded. Predicted values were calculated using equations developed for a comparable age group [18].
The spirometry and DLCO-test were administered by a pulmonary care nurse or medical doctor and all measurements were quality controlled.
Body-fat percentage was measured with bioelectric impedance analysis (Inbody 720, Seoul, South Korea). In addition to the clinical tests, the participants filled out health-related questionnaires.
Statistics
All analyses were stratified by sex. A statistical procedure called hockey-stick regression was applied [19]. It assumes that the effect of variable x is best fitted by two continuous linear functions; the slopes of both lines and also the change-point where the two lines meet are estimated. The resulting combined fitted line has one slope up to a change-point on the x-axis and a different slope after the change-point. Hockey-stick regressions with VO2peak (ml/min/kg) as the dependent variable were performed; FEV1, DLCO and DLCO adjusted for alveolar volume (DLCO/VA) were tested as variables with change-points in separate models. For comparison linear and curvilinear models were also fitted. In the linear models FEV1, DLCO and DLCO/VA were added as linear variables; and in the curvilinear models these measurements were added as both linear and squared variables. The analyses were controlled for age, physical activity index, resting heart rate and body-fat percentage, smoking status and self-reported heart disease. Covariates were chosen based on previous prediction models for VO2peak [14, 20]; self-reported heart disease was also added due to potential confounding in this age group. Control variables were continuous linear variables, except for current smoking (coded 1 or 0) and self-reported heart disease coded 1 for self-reported history of myocardial infarction, angina pectoris or atrial fibrillation, otherwise 0. Chow test with null-hypothesis that intercept and coefficient are equal before and after change point were used to test for structural break at change-point, and f-test were used to compare hockey-stick and curvilinear models to linear models. All calculations were performed with Stata 13.1 (StataCorp, Texas, USA); hockey-stick regressions were modelled with the “nl hockey” function.
Results
A total number of 1567 VO2peak-tests were completed; of these 47 on a cycle ergometer. Forty cases were omitted from the analyses due to submaximal effort (maximal self-reported value <15 on the 6-20 Borg scale); and 84 were omitted due to missing physical activity score, smoking status, body-fat percentage or valid spirometry data. Descriptive statistics for the 1443 participants included in the analyses are shown in Table 1, histograms showing the distribution of VO2peak, FEV1 and DLCO and DLCO/VA are shown in Additional file 1.
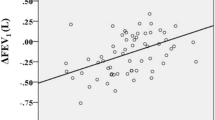
Significant change-points in the association with VO2peak were found for FEV1 for men at 2.86 l (LLN = 2.73 l) and for women at 2.13 l (LLN = 1.77 l) (Table 2). The association between FEV1 and VO2peak was positive up to these values, but not above. The change-points correspond to the 31st and 28th percentile of measured FEV1, for men and women respectively. A change-point was also found in the association between DLCO and VO2peak for men at 9.18 mmol/min/kPa (LLN = 6.84 mmol/min/kPa), corresponding to the 54th percentile. No significant change-point in the association between DLCO and VO2peak was found for women. Furthermore, no significant change-points were found in the association between DLCO/VA and VO2peak for either sex. Predicted effect plots for these hockey-stick regression models are shown in Fig. 1.
Predicted effect plots for hockey-stick models. In separate models forced expiratory volume in 1 s (FEV1) in litres, diffusing capacity of the lung for carbon monoxide (DLCO) in mmol/min/kPa and DLCO corrected for estimated alveolar volume (DLCO/VA) in mmol/min/kPa/l were added as variables with change points. Dependent variable is peak oxygen uptake in ml/min/kg. All models included age, self-reported physical activity, resting heart rate, body-fat percentage, self-reported history of heart disease and current smoking status as control variables. To illustrate the isolated effect of the lung function parameters, control variables were set to sample mean for these plots. Vertical lines mark change-points; dashed lines mark lower limit of normal; grey fields mark 95 % confidence interval for slopes; dots mark observations. Change-points were significant (p < 0.5) for FEV1 for both sexes and for DLCO for men, but not for DLCO for women and DLCO/VA for neither sex
Explained variance (adjusted R2) for VO2peak from the hockey stick models were compared to corresponding linear and curvilinear models (Table 3). For the association between FEV1 and VO2peak the hockey-stick model gave higher R2-values than the linear and curvilinear models (R2 = 0.433 (hockey-stick) vs. 0.423 (linear) and 0.429 (curvilinear) for men, and R2 = 0.460 (hockey-stick) vs. 0.452 (linear) and 0.456 (curvilinear) for women), supporting the choice of statistical model for this relationship. For DLCO the hockey-stick model was significantly better than the linear model for men (R2 = 0.450 vs. 0.440), but not for women (R2 = 0.470 vs. 0.469); and for both sexes R2-values from hockey-stick model were similar to R2 from curvilinear models (Table 3). For DLCO for women and for DLCO/VA for either sex, neither the hockey stick model nor the curvilinear model was significantly better than the linear model, suggesting linear relationships. Full descriptions of models are presented in Additional file 2.
To evaluate the effects of self-reported physical activity on the identified change-points, sub-group analyses were performed separately on those reporting high physical activity (physical activity index > = 15) and those reporting low activity (physical activity index < 15). A physical activity index score of 15 corresponds to reporting exercise once a week with high intensity and duration >30 min; or exercise 2–3 times per week with moderate intensity and duration >30 min; or exercise almost every day of moderate intensity and duration <30 min. This cut-point classifies 50.2 % of men and 44.7 % of women as reporting high physical activity. For men change-points for FEV1 were 2.90 l for those reporting high physical activity (LLN = 2.75 l) and 2.68 l for those reporting low activity (LLN = 2.73 l); the corresponding change-point localizations for DLCO were 11.0 mmol/min/kPa for high activity (LLN = 6.82 mmol/min/kPa) and 7.13 mmol/min/kPa for low activity (LLN = 6.85 mmol/min/kPa). For corresponding sub-groups of women the change-point values for FEV1 were 2.13 l for high activity (LLN = 1.78 l) and 2.12 l for low activity (LLN = 1.77 l).
To assess the effect of lung disease in our analyses, self-reported pulmonary disease (history of asthma, chronic bronchitis, emphysema or chronic obstructive pulmonary disease) were tested as an independent variable in the regression analyses. Self-reported pulmonary disease was not a significant predictor for VO2peak in the hockey-stick model for FEV1 for either sex, and did not increase R2 or affect the identified threshold value. In the hockey-stick model for DLCO for men, self-reported pulmonary disease was a significant predictor for VO2peak, but had only a minimal effect on the value, which decrease from 9.18 to 9.07 mmol/min/kPa.
Discussion
In this large population sample we have found evidence for a change-point in the association with VO2peak for FEV1 and DLCO in men and FEV1 in women. The associations between these variables and VO2peak were significant up to the change-points, but no significant associations were found above these values. This suggests that there may be a physiologic threshold for these lung function parameters, above which the lung function does not limit VO2peak. The identified threshold values are within the normal limits of lung function for this age group, which may suggest that lung function can be a limiting factor for maximal physical performance for many healthy elderly. A linear association with VO2peak was found for DLCO for women and DLCO/VA for both sexes, but no significant threshold was found for these parameters.
The identified change-points for FEV1 equals 86 % of predicted for men and 97 % for women when age and height are set to sample means; and are higher than calculated LLN at 2.73 l for men and 1.77 l for women. Predicted values and LLN were calculated using relevant Norwegian reference equations [17]. If instead using the 2012 Global Lung Function Initiative equations [21] the change-points would be 93 % of predicted FEV1 for men and 99 % for women, so using the Norwegian reference values is the more conservative approach. The threshold for DLCO for men corresponds to 95 % of predicted and is higher than LLN at 6.84 mmol/min/kPa. For the association between DLCO and VO2peak in women, neither the hockey-stick model nor the curvilinear model performed better than the multiple linear model; which may either be due to physiologic differences between sexes or to lack of statistical power to detect a levelling off of this relationship in women.
Several studies have shown that VO2peak is reduced in patients with lung disease and reduced lung function [3–6], but there are few studies on the relationship between pulmonary function measurements and VO2peak in healthy subjects. Babb et al. [22] reported a significant linear relationship between FEV1 and VO2peak in a small sample of asymptomatic volunteers selected to have a wide range of FEV1 (n = 11, age = 58 ± 8 years). Johnson et al. [23, 24] studying a group of active healthy older subjects (n = 30, age = 70 ± 1 years) found a correlation between % of predicted DLCO and VO2peak, and also showed that FEV1 were significantly higher in subjects with VO2peak above the median compared to those with VO2peak below the median. These studies had few participants and were not designed to study the association between lung function indices and VO2peak, and they do not allow general conclusions about this association. On the other hand, in an interventional study, Sue-Chu et al. [25] examined the effect of the bronchodilator salbutamol on VO2peak in non-asthmatic highly-trained cross-country skiers with high VO2peak. These subjects did not improve the VO2peak in spite of a significant improvement in FEV1, suggesting that even highly trained endurance athletes are not usually ventilatory limited with respect to VO2peak. A significant proportion of highly fit endurance athletes develops arterial hypoxemia during sub-maximal or maximal exercise [26]. This exercise-induced arterial hypoxemia limits VO2peak and this limitation can be reversed by supplemental oxygen during exercise [27, 28], suggesting that diffusion capacity could be a limiting factor in these subjects.
Physical exercise improves the capacity of the cardiovascular and locomotor systems to transport and utilize oxygen, while no such effect is evident on the respiratory system. An improvement in the maximal function of the circulatory and muscular systems from exercise would therefore increase the demand on the respiratory system for oxygen transport, reducing any spare capacity of this system. We would therefore expect that the association between lung function indices and VO2peak would be significant up to higher levels of FEV1 and DLCO in an exercise-trained population compared to a more sedate one. This is in accordance with the sub-group analyses in our study showing change-points at higher levels of lung function in men with high self-reported physical activity compared to low self-reported activity. This effect is particularly pronounced for the association between DLCO and VO2peak, suggesting that DLCO may represent a limiting factor for exercise capacity for men in this age group. For women, the location of the change point in the association between FEV1 and VO2peak is almost identical for those reporting high vs. low physical activity (2.13 vs. 2.12 l).
The findings in our study may be due to the age-related changes in the lung function of elderly people. With increasing age the lungs loose elastic recoil, the thorax wall gets stiffer and more restricted, respiratory muscle function is impaired, the alveolar surface area is reduced and there is increased ventilation-perfusion heterogeneity [29]. These changes cause expiratory flow limitation and reduced gas diffusion capacity in elderly compared to younger subjects. Even though there is a decline in the capacity for ventilation and gas exchange with age, there is also an age-related decline in the capacity of the other links of the oxygen uptake chain thus reducing the demands on the respiratory system. The margin between demand and capacity in the respiratory system decreases with age, but limitation of VO2peak due to demands exceeding the capacity is thought to be rare [30]. Our findings of an association with VO2peak for FEV1 and DLCO in the lower reference area may suggest that a reduced capacity of the respiratory system may be limiting for VO2peak for many elderly. The spare capacity of the lungs and airways seen in young healthy subjects may be fully eroded in many elderly, resulting in a limitation of VO2peak and maximal work rate by the respiratory system for these individuals.
The main strength of the present study is the population-based design and high number of subjects with directly measured VO2peak combined with spirometry and gas diffusion testing. To our knowledge, there are no other large studies examining the association between normal lung function and VO2peak. Even though known or plausible confounders were controlled for in our analyses, there might still be some residual confounding. Unrecognized pulmonary disease may contribute to residual confounding, but since pulmonary function is already included in the analyses, pulmonary disease would have to affect VO2peak independently of pulmonary function if pulmonary disease were to be a confounder for this relationship. We cannot test whether unrecognized pulmonary disease affects the results, but we can test this for those with self-reported pulmonary disease. Self-reported pulmonary disease is a significant predictor of VO2peak only when FEV1 is not included in the analyses, indicating that pulmonary disease is an up-stream variable of FEV1, and therefore not a relevant confounder in the analyses. Even though we have identified threshold levels in the associations between lung function indices and VO2peak on the population level for our subjects, the thresholds cannot be assumed to apply to individual subjects. Neither can we conclude that a subject having lung function below the threshold values has a pulmonary limitation of VO2peak. The physiologic basis for the observed change-point in the association between lung function indices and VO2peak may be age specific, and it cannot be assumed that the results in this study apply to younger or middle-aged populations. Ventilation-perfusion heterogeneity and widened alveolar-arterial oxygen pressure gradient are likely to be important factors for the limiting effect of the respiratory system on VO2peak; and measurements of blood oxygen concentration during exercise would likely have yielded further knowledge on this topic. Participants in this study were recruited to an exercise intervention study, and may be habitually physically active or at least more interested in exercise than the general population. This is a descriptive study with a cross-sectional design and it does not allow for conclusions on causality, and the results should therefore be interpreted with caution.
Conclusions
We have found evidence of a threshold in the association between lung function measurements and VO2peak in this elderly population. FEV1 for both sexes and for DLCO for men were positively associated with VO2peak only up to these threshold values. The identified threshold values are well within the normal range for these lung function parameters. DLCO for women and DLCO/VA for both sexes were linearly associated with VO2peak. A possible explanation for our findings could be that lung function even within the normal range may be a limiting factor for maximal oxygen uptake for many elderly.
References
Dempsey JA, McKenzie DC, Haverkamp HC, Eldridge MW. Update in the understanding of respiratory limitations to exercise performance in fit, active adults. Chest. 2008;134:613–22.
Romer LM, Sheel AW, Harms CA. The Respiratory System. In: Farrell PA, Joyner MJ, Caiozzo VJ, editors. ACSM’s Advanced Exercise Physiology. 2nd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2012. p. 242–96.
Carlson DJ, Ries AL, Kaplan RM. Prediction of maximum exercise tolerance in patients with COPD. Chest. 1991;100:307–11.
Babb TG, Viggiano R, Hurley B, Staats B, Rodarte JR. Effect of mild-to-moderate airflow limitation on exercise capacity. J Appl Physiol. 1991;70:223–30.
Cahalin L, Pappagianopoulos P, Prevost S, Wain J, Ginns L. The relationship of the 6-min walk test to maximal oxygen consumption in transplant candidates with end-stage lung disease. Chest. 1995;108:452–9.
Carter R, Holiday DB, Stocks J, Grothues C, Tiep B. Predicting oxygen uptake for men and women with moderate to severe chronic obstructive pulmonary disease. Arch Phys Med Rehabil. 2003;84:1158–64.
Chin RC, Guenette JA, Cheng S, Raghavan N, Amornputtisathaporn N, Cortes-Telles A, et al. Does the respiratory system limit exercise in mild chronic obstructive pulmonary disease? Am J Respir Crit Care Med. 2013;187:1315–23.
Hardie JA, Buist AS, Vollmer WM, Ellingsen I, Bakke PS, Morkve O. Risk of over-diagnosis of COPD in asymptomatic elderly never-smokers. Eur Respir J. 2002;20:1117–22.
Guenard H, Marthan R. Pulmonary gas exchange in elderly subjects. Eur Respir J. 1996;9:2573–7.
Venturelli M, Schena F, Scarsini R, Muti E, Richardson RS. Limitations to exercise in female centenarians: evidence that muscular efficiency tempers the impact of failing lungs. Age (Dordr). 2013;35:861–70.
Stensvold D, Viken H, Rognmo O, Skogvoll E, Steinshamn S, Vatten LJ, et al. A randomised controlled study of the long-term effects of exercise training on mortality in elderly people: study protocol for the Generation 100 study. BMJ Open. 2015;5:e007519.
Wisloff U, Stoylen A, Loennechen JP, Bruvold M, Rognmo O, Haram PM, et al. Superior cardiovascular effect of aerobic interval training versus moderate continuous training in heart failure patients: a randomized study. Circulation. 2007;115:3086–94.
Gibbons RJ, Balady GJ, Beasley JW, Bricker JT, Duvernoy WF, Froelicher VF, et al. ACC/AHA Guidelines for Exercise Testing. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Exercise Testing). J Am Coll Cardiol. 1997;30:260–311.
Nes BM, Janszky I, Vatten LJ, Nilsen TI, Aspenes ST, Wisloff U. Estimating V.O 2peak from a nonexercise prediction model: the HUNT Study, Norway. Med Sci Sports Exerc. 2011;43:2024–30.
Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, et al. Standardisation of spirometry. Eur Respir J. 2005;26:319–38.
Macintyre N, Crapo RO, Viegi G, Johnson DC, van der Grinten CP, Brusasco V, et al. Standardisation of the single-breath determination of carbon monoxide uptake in the lung. Eur Respir J. 2005;26:720–35.
Langhammer A, Johnsen R, Gulsvik A, Holmen TL, Bjermer L. Forced spirometry reference values for Norwegian adults: the Bronchial Obstruction in Nord-Trondelag Study. Eur Respir J. 2001;18:770–9.
Garcia-Rio F, Dorgham A, Galera R, Casitas R, Martinez E, Alvarez-Sala R, et al. Prediction equations for single-breath diffusing capacity in subjects aged 65 to 85 years. Chest. 2012;142:175–84.
Bacon DW, Watts DG. Estimating the Transition between Two Intersecting Straight Lines. Biometrika. 1971;58:525–34.
Jackson AS, Sui X, O’Connor DP, Church TS, Lee DC, Artero EG, et al. Longitudinal cardiorespiratory fitness algorithms for clinical settings. Am J Prev Med. 2012;43:512–9.
Quanjer PH, Stanojevic S, Cole TJ, Baur X, Hall GL, Culver BH, et al. Multi-ethnic reference values for spirometry for the 3-95-yr age range: the global lung function 2012 equations. Eur Respir J. 2012;40:1324–43.
Babb TG, Long KA, Rodarte JR. The relationship between maximal expiratory flow and increases of maximal exercise capacity with exercise training. Am J Respir Crit Care Med. 1997;156:116–21.
Johnson BD, Reddan WG, Pegelow DF, Seow KC, Dempsey JA. Flow limitation and regulation of functional residual capacity during exercise in a physically active aging population. Am Rev Respir Dis. 1991;143:960–7.
Johnson BD, Badr MS, Dempsey JA. Impact of the aging pulmonary system on the response to exercise. Clin Chest Med. 1994;15:229–46.
Sue-Chu M, Sandsund M, Helgerud J, Reinertsen RE, Bjermer L. Salmeterol and physical performance at -15 degrees C in highly trained nonasthmatic cross-country skiers. Scand J Med Sci Sports. 1999;9:48–52.
Dempsey JA, Wagner PD. Exercise-induced arterial hypoxemia. J Appl Physiol (1985). 1999;87:1997–2006.
Powers SK, Lawler J, Dempsey JA, Dodd S, Landry G. Effects of incomplete pulmonary gas exchange on VO2 max. J Appl Physiol (1985). 1989;66:2491–5.
Harms CA, McClaran SR, Nickele GA, Pegelow DF, Nelson WB, Dempsey JA. Effect of exercise-induced arterial O2 desaturation on VO2max in women. Med Sci Sports Exerc. 2000;32:1101–8.
Janssens JP, Pache JC, Nicod LP. Physiological changes in respiratory function associated with ageing. Eur Respir J. 1999;13:197–205.
Johnson BD, Dempsey JA. Demand vs. capacity in the aging pulmonary system. Exerc Sport Sci Rev. 1991;19:171–210.
Acknowledgements
The study was funded by The Kristian Gerhard Jebsen Foundation and Norwegian Health Association.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
EH, DS, TH, UW, AL and SS contributed substantially to the study design, acquisition or analysis of data, and the writing of the manuscript. All authors critically reviewed the manuscript and approved of the final version.
Additional files
Additional file 1:
Histograms showing the distribution of measured VO 2peak , FEV 1 , D LCO and D LCO /VA by sex. (JPG 547 kb)
Additional file 2:
Word document. Full description of models. Description of statistical models with coefficients. (DOCX 22 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Hassel, E., Stensvold, D., Halvorsen, T. et al. Association between pulmonary function and peak oxygen uptake in elderly: the Generation 100 study. Respir Res 16, 156 (2015). https://doi.org/10.1186/s12931-015-0317-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12931-015-0317-0