Abstract
Background
Although the endurance shuttle walk test (ESWT) has proven to be responsive to change in exercise capacity after pulmonary rehabilitation (PR) for COPD, the minimally important difference (MID) has not yet been established. We aimed to establish the MID of the ESWT in patients with severe COPD and chronic hypercapnic respiratory failure following PR.
Methods
Data were derived from a randomized controlled trial, investigating the value of noninvasive positive pressure ventilation added to PR. Fifty-five patients with stable COPD, GOLD stage IV, with chronic respiratory failure were included (mean (SD) FEV1 31.1 (12.0) % pred, age 62 (9) y). MID estimates of the ESWT in seconds, percentage and meters change were calculated with anchor based and distribution based methods. Six minute walking distance (6MWD), peak work rate on bicycle ergometry (Wpeak) and Chronic Respiratory Questionnaire (CRQ) were used as anchors and Cohen’s effect size was used as distribution based method.
Results
The estimated MID of the ESWT with the different anchors ranged from 186–199 s, 76–82% and 154–164 m. Using the distribution based method the MID was 144 s, 61% and 137 m.
Conclusions
Estimates of the MID for the ESWT after PR showed only small differences using different anchors in patients with COPD and chronic respiratory failure. Therefore we recommend using a range of 186–199 s, 76–82% or 154–164 m as MID of the ESWT in COPD patients with chronic respiratory failure. Further research in larger populations should elucidate whether this cut-off value is also valid in other COPD populations and with other interventions.
Trial registration
ClinicalTrials.Gov (ID NCT00135538).
Similar content being viewed by others
Background
Patients with severe Chronic Obstructive Pulmonary Disease (COPD) have an impaired exercise capacity, which is frequently associated with lower physical activity level [1] and, importantly, with lower quality of life [2,3] and higher mortality [4]. Therefore, enhancement of exercise capacity is an important goal of interventions such as pulmonary rehabilitation (PR) [5] and pharmacological treatment [6].
Exercise capacity can be assessed by maximal and submaximal tests, which reflect different pathobiological properties like sufficient aerobic enzyme systems, muscle strength, cardiovascular fitness and motivation. Maximal exercise capacity is commonly assessed with incremental cycle ergometry or treadmill walking, but these tests are not very responsive to interventions such as medication [7] or exercise training [8]. Field walking tests, such as the six-minute walking distance (6MWD) and endurance shuttle walk test (ESWT), might better reflect quality of life and activities of daily living, and therefore might be more relevant measurements in patients with severe COPD. The ESWT has a number of advantages compared to the 6MWD. Firstly, the ESWT has been shown to be very responsive to bronchodilation [9] and PR [10,11] and might be even more responsive to treatment than the 6MWD [11,12]. Secondly, the ESWT is less affected by motivation and pacing ability of the patient than the 6MWD because gate speed is imposed [13,14].
Unfortunately, at this moment it is not clear which size of change in ESWT could be considered as clinically relevant. This is important for developing new studies, for weighing results of interventions, and for clinicians in evaluating provided care. Until now, only one study provided some information about the minimally important difference (MID) of the ESWT [15]. In that study, the MID was investigated after bronchodilation and PR using an anchor based (global rating of change) and distribution based method (half a standard deviation (SD) of the changes in ESWT time or distance) [15]. The MID of the ESWT after treatment with salmeterol or ipratropium bromide was found to be 45–85 seconds. The anchor based MID of the ESWT after 7 weeks of PR, however, was not determined.
For this study we used the Chronic Respiratory Questionnaire (CRQ), peak work rate (Wpeak) and 6MWD as anchors in combination with a distribution based method. Those anchors were chosen because they are accepted outcomes of pulmonary rehabilitation and all in some way reflect exercise capacity or quality of life. The aim of the current study is to determine the MID of the ESWT in patients with severe, hypercapnic COPD (GOLD IV) following PR with or without nocturnal non-invasive intermittent positive pressure ventilation (NIPPV).
Methods
Study population
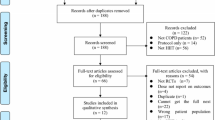
A total of 55 patients with stable COPD, GOLD stage IV, with chronic hypercapnic respiratory failure, were included in the current analyses. All these patients participated in a randomized controlled trial of which the results were published previously [16,17]. In this study the additional effect of NIPPV on the effects of PR was investigated. Seventy-two patients were included in the study, of which 56 patients completed the rehabilitation program of 12 weeks. Patients were assigned to rehabilitation with (n = 32) or without NIPPV (n = 24). Inclusion criteria were a stable clinical condition (no exacerbation in the four weeks prior to study participation), severe COPD (FEV1 < 50%pred), hypercapnia at rest (arterial carbon dioxide pressure PaCO2 > 6.0 kPa while breathing room air) and age between 40–80 years. Exclusion criteria were the presence of cardiac or neuromuscular diseases limiting exercise tolerance, exposure to NIPPV or PR in the previous 18 months, or the presence of obstructive sleep apnoea syndrome (apnoea/hypopnoea index ≥ 10/hour). The study was approved by the local Medical Ethics Committee of the University Medical Centre Groningen and was registered at ClinicalTrials.Gov (ID NCT00135538). All patients gave written informed consent to participate. In the current analysis only patients that completed all measurements (31 in the PR group and 24 in the PR + NIPPV group) at the start and directly after the rehabilitation program were included.
Study design
At baseline lung function, exercise tolerance and quality of life were assessed. Thereafter patients started a 12 week period of rehabilitation with or without NIPPV. The rehabilitation program consisted of strength training, cycling, walking, inspiratory muscle training, education and psychological and/or nutritional support if necessary as described in detail elsewhere [16,17]. The exercise training sessions were on three days per week. NIPPV was initiated in the hospital to train the patients to use the ventilatory support during the night as long as possible with a minimum duration of 6 hours. The adjustment process of NIPPV and the patient compliance afterwards were described in detail in previous publications [16,17]. After the intervention period of 12 weeks measurements of exercise tolerance and quality of life were repeated. Apnea/hypoapnea index was measured with overnight polygraphy prior to the study.
Measurements
All lung function measurements were performed after bronchodilation. Forced expiration volume in 1 second (FEV1) and forced vital capacity (FVC) were assessed by spirometry according to ERS criteria [18]. Total lung capacity (TLC) and residual volume (RV) were measured by body plethysmography [19].
Cycle ergometer tests were performed after optimal bronchodilation. First, daytime resting arterial blood gases on room air were taken from all patients while lying (Rapid lab type 865, Siemens, USA). The incremental cycle ergometer test was performed using a 1-minute incremental protocol, using 5 Watt increments. Patients were seated on the bicycle, respired through a mouth piece and wore a nose clip during the test. Minute ventilation, tidal volume, breathing frequency and oxygen uptake were measured continuously (Oxycon Pro Viasys, Bilthoven, the Netherlands). Maximal workload (Wpeak) was defined as the highest work level reached and maintained for at least 30 seconds.
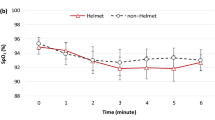
The ESWT was performed on a 10 m long course at a speed corresponding with 85% of VO2 peak, which was estimated from an earlier performed incremental shuttle walking test [20]. For both tests a practice walk was done during the run-in period of the study. Patients were instructed to walk as long as possible at the speed that was dictated by the auditory signal. The test was ended when a patient was more than 0.5 m away from the marker before the signal was given on two successive shuttles, or when he or she indicated to be exhausted.
The 6MWD was assessed indoors on a 40 m long course. Patients used their usual walking aids and, if applicable, their usual ambulatory oxygen therapy during the test. The test assistant gave standardized encouragements every 30 seconds and told the patient after 2 and after 4 minutes that he/she was 2 and 4 minutes on his/her way [21]. All patients performed a practice test first, the results of which were discarded.
During the walking tests supplemental oxygen was permitted, but conditions were the same at all tests. The walking tests were not stopped because of desaturation.
Quality of life was assessed with the interviewed version of the Chronic Respiratory Questionnaire [22]. The CRQ is a widely used disease specific questionnaire which has shown to be reliable and valid in COPD patients [23].
Minimal important difference calculation methods and statistical analysis
The minimal important difference can be estimated in various ways and generally a combination of methods is recommended [24]. In the current study we used both anchor based and distribution based methods. For the anchor based method we used three measures with an established MID: The 6MWD (25 m) [25], Wpeak (4 Watt) [26,27] and the CRQ (10 points in total score) [28]. Spearman’s correlations between improved ESWT on the one hand and improved 6MWD, Wpeak and CRQ on the other hand had to be > 0.30 allowing linear regression analyses. There is no consensus on what an appreciable association between the outcome variable and the anchor should be. However, a correlation of 0.30 is considered to be the lower limit [24,26,29]. Afterwards, the MID of the ESWT was derived from substituting the MID of the anchors in the regression line of ∆ESWT and ∆ anchor. A distribution-based method was used to compare the change in outcome variable with an arbitrary measure of variability, which in this study was the effect size, using the following equation: 0.5 *SD (ΔESWT). The analyses were performed on pooled treatment groups as the separate analyses of the two treatment arms (PR or PR + NIPPV) showed similar associations, thereby increasing statistical power. The MID of the ESWT was expressed as change in time, percentage change from baseline (time or meters) and change in meters.
All statistical analyses were performed using Scientific Package of Social Sciences (SPSS) version 18.0. P-values <0.05 were considered to be significant.
Results
The baseline characteristics of the 55 COPD patients (42% female) are shown in Table 1.
Correlates of ESWT change with change in anchors
For further analysis correlations >0.30 were used. These were shown for ESWT change in absolute time (ΔESWTs) and % change from baseline (ΔESWT%) with all three anchors, 6MWD, Wpeak and CRQ, and for ESWT change in meters (ΔESWTm) with the CRQ and Wpeak. (Table 2 and Additional file 1: Figure S1) The CRQ total score showed higher correlations with ESWT change than the CRQ subscales and therefore CRQ total score was used in the regression analysis.
Anchor based and distribution based estimates of the MID of the ESWT
Table 3 shows the MID estimates and 95% confidence intervals (in seconds, percentage and meters) derived from the linear regression equations of ΔESWT and Δanchor (Additional file 2: Table S1). The MID estimate of ESWTm using the 6MWD as an anchor was not calculated because ΔESWTm and Δ6MWD correlated <0.30. The MID estimates calculated with the distribution based method were 145 s for ΔESWTs, 61.4% for ΔESWT% and 137 m for ΔESWTm.
Discussion
In this population of patients with severe COPD and chronic hypercapnic respiratory failure, who followed PR (with or without NIPPV), we estimated the MID for the ESWT. Using three different anchors we found MID estimates ranging from 186–199 s, 76–82% and 154–164 m. The anchors Wpeak and 6MWD provided almost identical results. In contrast, the MID based on statistical variability of the effect size was somewhat lower: 61%, 145 s and 137 m.
All anchors used in our study meet the criteria of a good anchor [24]. These criteria, applied to this field, are firstly: the anchor should have an established MID derived from multiple high quality studies, including many well characterized COPD patients, using multiple methods, and agreeing about the final MID estimate. Secondly, the anchor should be derived from a comparable COPD population. Thirdly, the anchor should somehow reflect the perception of improved exercise capacity. Finally the anchor should correlate highly with changes in ESWT. The anchors used in this study will be discussed in this perspective.
The first anchor was the Chronic Respiratory Questionnaire. The CRQ has a widely accepted MID of 10 points on the total score (or 0.5 per question), which has been estimated with different methods [28,30,31]. In addition, the CRQ has served as an anchor for establishing MID’s of other measurement tools as well, such as the Hospital Anxiety and Depression Scale and the feeling thermometer [32,33]. Correlations of CRQ change and ESWT change showed rho values > 0.40 and the CRQ could therefore be used as an anchor. Although the CRQ does not reflect the exact same concept as the ESWT, it is a measure that reflects the patients perception of health status, which agrees with the MID concept.
The second anchor was Wpeak. Two studies estimated the MID for Wpeak using anchor based or distribution based methods and expert opinions. Both studies suggest a MID of 4 Watt. [26,27] Correlations of Wpeak change and ESWT change showed rho values > 0.50 suggesting that Wpeak could be used as an anchor. In addition, Wpeak reflects exercise capacity as does the ESWT, and in both tests patients reach a similar peak performance [34].
The 6MWD also seems a suitable anchor as its MID has been established in different subgroups of COPD patients using different interventions including a PR intervention. We chose to use the MID of 25 m, based on two studies, one in a slightly milder COPD population (age 70 y, FEV1 52% pred) after PR [25], and one in a more severe COPD population (age 66.4, FEV1 26.9% pred), showing an MID of 26 m after surgical lung volume reduction [26]. Another feature demonstrating the 6MWD to be a suitable anchor is that it reflects exercise capacity, as does the ESWT, though perhaps in a different way. Associations of 6MWD change with ESWT change were just high enough to use it as an anchor, therefore this estimation should be taken with some caution. On the other hand, the MID estimated using the 6MWD as anchor was very similar to the MID estimated using the CRQ and Wpeak.
To verify the MID values found with the anchor based method we also used a distribution based method. The latter method should only be used complementary to an anchor based method as it does not fit with the primary aim of the MID concept, which is to indentify an effect size that is relevant in the perception of the patient [24]. In our study the distribution based method showed lower values for the MID than the anchor based method. It has been shown before that distribution based methods tend to underestimate the MID when based on a single study [32].
The MID values estimated with the CRQ, Wpeak and 6MWD were very close to one another (see Table 3). The MID estimated with the distribution based method was somewhat lower (144 s, 61% and 137 m). In line with the literature we recommend to use MID values based on the anchor based method [24]. We prefer to use the MID estimates in seconds and %, and not meters as a change of 100 meters at a low speed has a different value in clinical perspective than a change of 100 m at a high speed.
The estimation of the MID of the ESWT after PR has been investigated in one other study in patients with less severe COPD (FEV1 48% pred). In this study, global rating of change was used as an anchor, comprising of one question. To our opinion, the anchors in our study were suitable as well because the CRQ, 6MWD and to a lesser degree Wpeak, are outcome measures with an established MID and showed correlations >0.30 with ESWT change. However, we realize that our anchors might not reflect exactly the same construct as the ESWT. Pepin et al. only used a distribution based method showing an MID of 186 seconds or 136%, because they decided that associations with the global rating of change were too low to be used to estimate an anchor based MID after PR.
Though we studied a different population than Pepin, our anchor based MID was surprisingly similar to their distribution based estimate, at least for the change in ESWT (s).
Of course we were very interested in how our results are in comparison to other PR intervention studies that used the ESWT as an outcome measure. Several studies were found and they all showed significant improvements in ESWT after intervention [10,35-39]. The studies included patients with quite similar mean age (60–75 years) and mean FEV1 (37.5–63.0% predicted) and demonstrated mean ESWT improvements between 138–378 seconds, 15–100% and 106–393 meters [10,35-39]. These change values were consistent with our MID estimates (ranging from 186–199 s, 76–82% and 154–164 m).
A major difference with the patients included in the present analysis is that the patients in the current analysis all suffered from chronic hypercapnic respiratory failure. Probably, the differences found in mean ESWT changes in these studies are due to differences in COPD population, study design and efficacy of the intervention.
A strong point of our study is that we used an anchor based method including three different anchors as well as a distribution based method to determine the MID of the ESWT. Another strong feature is that the correlations of the ESWT change with all anchors were above 0.30, allowing us to use the anchors in a meaningful way.
A limitation of this study might be the relatively small number of patients in the study and the fact that this was a very specific group of COPD patients, namely those with severe COPD and chronic respiratory failure. Therefore, it might not be appropriate to generalize our results straight to the entire COPD population as the MID might differ between populations with other phenotypes and disease stages. A remark should also be made about the confidence intervals for the MID estimates we found, which were quite wide. This hinders firm conclusions. Another limitation of this study is that we did not use a global rating of change as an anchor to estimate the MID of the ESWT. For example by asking the patient the question: ‘In comparison with your previous test, how would you rate your performance on the current test? Using a 7-point Likert scale to rate this performance.
Conclusions
In conclusion, in patients with severe hypercapnic COPD undergoing PR with or without NIPPV, the MID estimates for the ESWT ranged from 186–199 s, 76–82% and 154–164 m using different anchors (CRQ, Wpeak, 6MWD). Estimates of the MID of the ESWT using 6MWD and Wpeak as anchors provide almost identical results. This MID construct needs further validation in larger and different subgroups of COPD patients.
Abbreviations
- COPD:
-
Chronic Obstructive Pulmonary Disease
- 6MWD:
-
Six minute walking distance
- BMI:
-
Body mass index
- ESWT:
-
Endurance shuttle walk test
- MID:
-
Minimally important difference
- PR:
-
Pulmonary rehabilitation
- SD:
-
Standard deviation
- NIPPV:
-
Non-invasive intermittent positive pressure ventilation
- CRQ:
-
Chronic Respiratory Questionnaire
- Wpeak:
-
Peak work rate
- FEV1 :
-
Forced expiration volume in one second
- FVC:
-
Forced vital capacity
- ERS:
-
European Respiratory Society
- TLC:
-
Total lung capacity
- RV:
-
Residual volume
- SPSS:
-
Scientific Package of Social Sciences
- ∆ESWTs:
-
Change in endurance shuttle walk test in seconds
- ∆ESWT %:
-
Percentage change in endurance shuttle walk test
- ∆ESWT m:
-
Change in endurance shuttle walk test in meters
References
Bossenbroek L, de Greef MH, Wempe JB, Krijnen WP, Ten Hacken NH. Daily physical activity in patients with chronic obstructive pulmonary disease: a systematic review. COPD. 2011;8(4):306–19.
Stavem K, Boe J, Erikssen J. Health status, dyspnea, lung function and exercise capacity in patients with chronic obstructive pulmonary disease. Int J Tuberc Lung Dis. 1999;3(10):920–6.
Mangueira NM, Viega IL, Mangueira Mde A, Pinheiro AN, Costa Mdo R. Correlation between clinical parameters and health-related quality of life in women with COPD. J Bras Pneumol. 2009;35(3):248–55.
Cote CG, Pinto-Plata V, Kasprzyk K, Dordelly LJ, Celli BR. The 6-min walk distance, peak oxygen uptake, and mortality in COPD. Chest. 2007;132(6):1778–85.
Lacasse Y, Martin S, Lasserson TJ, Goldstein RS. Meta-analysis of respiratory rehabilitation in chronic obstructive pulmonary disease. A Cochrane systematic review. Eura Medicophys. 2007;43(4):475–85.
Liesker JJ, Wijkstra PJ, Ten Hacken NH, Koeter GH, Postma DS, Kerstjens HA. A systematic review of the effects of bronchodilators on exercise capacity in patients with COPD. Chest. 2002;121(2):597–608.
Oga T, Nishimura K, Tsukino M, Hajiro T, Ikeda A, Izumi T. The effects of oxitropium bromide on exercise performance in patients with stable chronic obstructive pulmonary disease. A comparison of three different exercise tests. Am J Respir Crit Care Med. 2000;161(6):1897–901.
Plankeel JF, McMullen B, MacIntyre NR. Exercise outcomes after pulmonary rehabilitation depend on the initial mechanism of exercise limitation among non-oxygen-dependent COPD patients. Chest. 2005;127(0012–3692; 1):110–6.
Brouillard C, Pepin V, Milot J, Lacasse Y, Maltais F. Endurance shuttle walking test: responsiveness to salmeterol in COPD. Eur Respir J. 2008;31(3):579–84.
Altenburg WA, de Greef MH, Ten Hacken NH, Wempe JB. A better response in exercise capacity after pulmonary rehabilitation in more severe COPD patients. Respir Med. 2012;106(5):694–700.
Eaton T, Young P, Nicol K, Kolbe J. The endurance shuttle walking test: a responsive measure in pulmonary rehabilitation for COPD patients. Chron Respir Dis. 2006;3(1479–9723; 1):3–9.
Pepin V, Brodeur J, Lacasse Y, Milot J, Leblanc P, Whittom F, et al. Six-minute walking versus shuttle walking: responsiveness to bronchodilation in chronic obstructive pulmonary disease. Thorax. 2007;62(4):291–8.
Solway S, Brooks D, Lacasse Y, Thomas S. A qualitative systematic overview of the measurement properties of functional walk tests used in the cardiorespiratory domain. Chest. 2001;119(1):256–70.
Eiser N, Willsher D, Dore CJ. Reliability, repeatability and sensitivity to change of externally and self-paced walking tests in COPD patients. Respir Med. 2003;97(4):407–14.
Pepin V, Laviolette L, Brouillard C, Sewell L, Singh SJ, Revill SM, et al. Significance of changes in endurance shuttle walking performance. Thorax. 2011;66(2):115–20.
Duiverman ML, Wempe JB, Bladder G, Vonk JM, Zijlstra JG, Kerstjens HA, et al. Two-year home-based nocturnal noninvasive ventilation added to rehabilitation in chronic obstructive pulmonary disease patients: a randomized controlled trial. Respir Res. 2011;12:112.
Duiverman ML, Wempe JB, Bladder G, Jansen DF, Kerstjens HA, Zijlstra JG, et al. Nocturnal non-invasive ventilation in addition to rehabilitation in hypercapnic patients with COPD. Thorax. 2008;63(12):1052–7.
Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, et al. Standardisation of spirometry. Eur Respir J. 2005;26(2):319–38.
Wanger J, Clausen JL, Coates A, Pedersen OF, Brusasco V, Burgos F, et al. Standardisation of the measurement of lung volumes. Eur Respir J. 2005;26(3):511–22.
Revill SM, Morgan MD, Singh SJ, Williams J, Hardman AE. The endurance shuttle walk: a new field test for the assessment of endurance capacity in chronic obstructive pulmonary disease. Thorax. 1999;54(0040–6376; 3):213–22.
Guyatt GH, Sullivan MJ, Thompson PJ, Fallen EL, Pugsley SO, Taylor DW, et al. The 6-minute walk: a new measure of exercise capacity in patients with chronic heart failure. Can Med Assoc J. 1985;132(8):919–23.
Guyatt GH, Berman LB, Townsend M, Pugsley SO, Chambers LW. A measure of quality of life for clinical trials in chronic lung disease. Thorax. 1987;42(10):773–8.
Wijkstra PJ, TenVergert EM, Van Altena R, Otten V, Postma DS, Kraan J, et al. Reliability and validity of the chronic respiratory questionnaire (CRQ). Thorax. 1994;49(5):465–7.
Revicki D, Hays RD, Cella D, Sloan J. Recommended methods for determining responsiveness and minimally important differences for patient-reported outcomes. J Clin Epidemiol. 2008;61(2):102–9.
Holland AE, Hill CJ, Rasekaba T, Lee A, Naughton MT, McDonald CF. Updating the minimal important difference for six-minute walk distance in patients with chronic obstructive pulmonary disease. Arch Phys Med Rehabil. 2010;91(2):221–5.
Puhan MA, Chandra D, Mosenifar Z, Ries A, Make B, Hansel NN, et al. The minimal important difference of exercise tests in severe COPD. Eur Respir J. 2011;37(4):784–90.
Sutherland ER, Make BJ. Maximum exercise as an outcome in COPD: minimal clinically important difference. COPD. 2005;2(1):137–41.
Jaeschke R, Singer J, Guyatt GH. Measurement of health status. Ascertaining the minimal clinically important difference. Control Clin Trials. 1989;10(4):407–15.
Hartman JE, Ten Hacken NH, Klooster K, Boezen HM, de Greef MH, Slebos DJ. The minimal important difference for residual volume in patients with severe emphysema. Eur Respir J. 2012;40(5):1137–41.
Redelmeier DA, Guyatt GH, Goldstein RS. Assessing the minimal important difference in symptoms: a comparison of two techniques. J Clin Epidemiol. 1996;49(11):1215–9.
Juniper EF, Guyatt GH, Willan A, Griffith LE. Determining a minimal important change in a disease-specific Quality of Life Questionnaire. J Clin Epidemiol. 1994;47(1):81–7.
Puhan MA, Frey M, Buchi S, Schunemann HJ. The minimal important difference of the hospital anxiety and depression scale in patients with chronic obstructive pulmonary disease. Health Qual Life Outcomes. 2008;6:46.
Schunemann HJ, Griffith L, Jaeschke R, Goldstein R, Stubbing D, Guyatt GH. Evaluation of the minimal important difference for the feeling thermometer and the St. George’s Respiratory Questionnaire in patients with chronic airflow obstruction. J Clin Epidemiol. 2003;56(12):1170–6.
Hill K, Dolmage TE, Woon L, Coutts D, Goldstein R, Brooks D. Comparing peak and submaximal cardiorespiratory responses during field walking tests with incremental cycle ergometry in COPD. Respirology. 2012;17(2):278–84.
Effing T, Zielhuis G, Kerstjens H, van der Valk P, van der Palen J. Community based physiotherapeutic exercise in COPD self-management: a randomised controlled trial. Respir Med. 2011;105(3):418–26.
Dyer F, Callaghan J, Cheema K, Bott J. Ambulatory oxygen improves the effectiveness of pulmonary rehabilitation in selected patients with chronic obstructive pulmonary disease. Chron Respir Dis. 2012;9(2):83–91.
Ringbaek T, Martinez G, Durakovic A, Thogersen J, Midjord AK, Jensen JE, et al. Vitamin d status in patients with chronic obstructive pulmonary disease who participate in pulmonary rehabilitation. J Cardiopulm Rehabil Prev. 2011;31(4):261–7.
Leung RW, McKeough ZJ, Peters MJ, Alison JA. Short-form Sun-style t’ai chi as an exercise training modality in people with COPD. Eur Respir J. 2013;41(5):1051–7.
McNamara RJ, McKeough ZJ, McKenzie DK, Alison JA. Water-based exercise in COPD with physical comorbidities: a randomised controlled trial. Eur Respir J. 2013;41(6):1284–91.
Acknowledgements
This study was funded by the Dutch Asthma Foundation.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interest.
Authors’ contributions
The authors have participated in the following activities in the current study: WAA: study design, statistical analysis, interpretation of data and writing the manuscript. MLD: data collection, interpretation of data and writing the manuscript. NtH: interpretation of data and writing the manuscript. HAMK: interpretation of data and writing the manuscript. MHGdG: statistical analysis, interpretation of data and writing the manuscript. PJW: interpretation of data and writing the manuscript. JBW: study design, interpretation of data and writing the manuscript. All authors approved the final version of this manuscript.
Additional files
Additional file 1: Figure S1.
a-i. Scatterplots of change in ESWT versus change in anchor variable.
Additional file 2: Table S1.
Regression equations used to calculate MID values.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Altenburg, W.A., Duiverman, M.L., ten Hacken, N.H. et al. Changes in the endurance shuttle walk test in COPD patients with chronic respiratory failure after pulmonary rehabilitation: the minimal important difference obtained with anchor- and distribution-based method. Respir Res 16, 27 (2015). https://doi.org/10.1186/s12931-015-0182-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12931-015-0182-x