Abstract
Background
Gastric cancer (GC) is one of the most common malignancies, affected by several genetic loci in the clinical phenotype. This study aimed to determine the association between PTGER4 and PRKAA1 gene polymorphisms and the risk of GC.
Methods
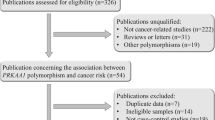
A total of 509 GC patients and 507 age and sex-matched healthy controls were recruited to explore the association between PTGER4 and PRKAA1 genetic polymorphisms and GC susceptibility. Logistic regression analysis was used to study the correlation between these SNPs and GC, with odd ratio (OR) and 95% confidence interval (CI) as indicators. Multifactor dimensionality reduction was utilized to analyze the genetic relationships among SNPs. was conducted to predict gene expression, the impact of SNPs on gene expression, and the signaling pathways involved in PTGER4 and PRKAA1.
Results
Overall, rs10036575 in PTGER4 (OR = 0.82, p = 0.029), rs10074991 (OR = 0.82, p = 0.024) and rs13361707 (OR = 0.82, p = 0.030) in PRKAA1 were associated with susceptibility to GC. Stratification analysis revealed that the effects of these SNPs in PTGER4 and PRKAA1 on GC susceptibility were dependent on smoking and were associated with a reduced risk of adenocarcinoma (p < 0.05). Bioinformatics analysis showed an association between SNPs and corresponding gene expression (p < 0.05), and PRKAA1 may affect GC by mediating RhoA.
Conclusion
This study suggests that PTGER4 and PRKAA1 SNPs might affect the susceptibility of GC, providing a new biological perspective for GC risk assessment, pathogenesis exploration, and personalized treatment.
Similar content being viewed by others
Introduction
Gastric cancer (GC) is a common malignancies worldwide, with over one million new cases each year and ranking as the fourth leading cause of cancer-related death [1, 2]. In the Nordic countries, GC has an estimated heritability of 22%, with multiple genetic pathogenic mutations in high penetrance genes [3]. It is estimated that there will be 10 million new GC cases and 5.6 million GC deaths in China between 2021 and 2035 [4]. GC is a highly aggressive malignancy with heterogeneity, posing a significant global health burden [5]. Its specific pathogenesis remains unclear, with both environmental and genetic factors playing a role in its occurrence and development [6]. Recent studies have identified several risk factors associated with GC, including age, gender, obesity, cigarette smoking, alcohol consumption, diet, and Helicobacter pylori infection [7,8,9]. Furthermore, genetic factors are believed to play a significant role in GC pathogenesis [10]. Single nucleotide polymorphisms (SNPs) are the most common form of gene mutation in the human genome. Genome-wide association studies have identified several GC susceptibility loci [11, 12].
PRKAA1 is a gene e that encodes adenosine monophosphate-activated protein kinase (AMPK), a central metabolic switch involved in various diseases related to energy metabolism, particularly cancer [10, 13]. AMPK has been found to play a role in tumorigenesis and development through regulatory pathways [14]. Interestingly, PRKAA1 promotes tumorigenesis and invasion, and its gene polymorphisms may be involved in the occurrence and development of GC by affecting energy metabolism regulation [14, 15]. Among these polymorphisms, the association between PRKAA1 polymorphisms (rs13361707 and rs10074991) and GC risk has been extensively studied [16,17,18]. However, there is limited validation of the relationship between PRKAA1 polymorphisms and GC risk in the Chinese Han population.
PTGER4 is a G-protein-coupled receptor that mediates the action of prostaglandin E2 (PGE2), playing a crucial role in cancer cell proliferation, invasion, stem cell regeneration, and tumor angiogenesis [19]. PTGER4 also plays a significant role in regulating cell migration and immune response [20, 21]. Studies have shown that PTGER4 is involved in the growth and development of carcinomas, including colorectal cancer [19, 22,23,24]. Studies have shown that PTGER4 is involved in the growth and development of carcinomas, including colorectal cancer [25]. However, there have been few studies on PTGER4 expression in GC, and the detailed biological mechanism of its role in tumor cells remains poorly understood. The role of PTGER4 polymorphism in GC function is also unknown. Therefore, further research on the role of PTGER4 gene polymorphism in GC is essential. A comprehensive study of the relationship between PTGER4 gene polymorphism and GC susceptibility can provide a foundation for the diagnosis and treatment of GC.
This study aims to investigate the relationship between PTGER4 and PRKAA1 SNPs and the risk of GC, examining the roles of PTGER4 and PRKAA1 genes in the occurrence and development of GC. A deeper understanding of GC pathogenesis is crucial for early detection, identification of risk factors, and personalized treatment.
Methods
Study subjects
A total of 1,016 subjects (509 GC cases and 507 healthy controls) were enrolled in this study to investigate the association between the PTGER4 and PRKAA1 genes polymorphisms and the risk of GC. The diagnosis of GC patients was confirmed through histopathological analysis and pathological data. Patients with a prior history of cancer, chemotherapy or radiotherapy, and immune system disorders were excluded from the case group. Blood samples were collected from patients prior to each treatment period. The control group was randomly selected from healthy volunteers who had no history of cancer. All participants provided written informed consent. Demographic data (age, gender, body mass index (BMI), smoking and drinking status) and clinical data (lymph node metastasis, staging, and adenocarcinoma status) were obtained through questionnaire surveys and hospital records. Definition of smoking and drinking status: Non-smokers/non-drinkers: Non-smokers/non-drinkers are participants who have never smoked or drank, or have only occasionally smoked or drank without developing a sustained habit. Smokers/drinkers are participants who continue to engage in smoking or drinking behavior and have developed a sustained habit of smoking or drinking.
SNP selection and genotyping
The physical location of the PTGER4 and PRKAA1 genes was searched using NCBI database (https://www.ncbi.nlm.nih.gov/gene/). SNPs within 500 kb of PTGER4 and PRKAA1 genes with minor allele frequency (MAF) > 0.05, Hardy-Weinberg equilibrium (HWE) > 0.05, min genotype frequency > 75%, and r2 > 0.8 in the Chinese Han Beijing (CHB) population of 1000 Genome Project were screened using the VCF to PED Converter window (http://grch37.ensembl.org/HomoSapiens/Tools/VcftoPed) and Haploview software. Finally, Based on primer design and genotyping results, a total of nine SNPs (rs4613763, rs6880778, rs11742570, rs9292777, rs7725052, rs12186979, and rs10036575 in PTGER4, rs10074991 and rs13361707 in PRKAA1) were chosen for the association analysis. The functional annotation of SNPs was predicted using the Regulomedb database (https://regulomedb.org/). Peripheral blood genomic DNA was extracted using GoldMag DNA Purification Kit (GoldMag Co. Ltd.). The concentration and purity of DNA are detected using NanoDrop 2000 (Thermo Scientific). The Agena MassARRAY platform (Agena Bioscience, San Diego, CA, USA) was used for SNPs genotyping. AgenaTyper 4.0 software was used to organize and analyze genotype data.
Bioinformatics analysis
Bioinformatics analysis was conducted using various databases. The Ualcan database (https://ualcan.path.uab.edu/analysis.html) was used to compare the expression of PTGER4 and PRKAA1 genes in stomach adenocarcinoma (STAD) and normal tissues. The GTEx Portal database (https://gtexportal.org/home/) predicted the association between SNPs and the expression levels of PTGER4 and PRKAA1 in gastric tissue. The GEO database (https://www.ncbi.nlm.nih.gov/gds) was utilized to analyze the relationship between GC and the expression levels of PTGER4 and PRKAA1 genes using the GSE26309 dataset. The STRING database (https://www.string-db.org/) was used to identify the interaction between PTGER4 and PRKAA1-related proteins. KEGG (Kyoto Encyclopedia of Genes and Genomes) [26] pathway enrichment analysis (https://www.kegg.jp/kegg/kegg1.html) and key target regulatory pathways were performed using the oebiotech platform (https://cloud.oebiotech.com/task/).
Statistical analysis
Statistical analysis was conducted using SPSS (version 25), PLINK (version 1.9), and multifactor dimensionality reduction (MDR, version 3.0.2) software. A p-value < 0.05 was considered statistically significant. Logistic regression analysis was used to assess the correlation between genetic variations and the risk of GC, with odds ratios (OR) and 95% confidence intervals (CI) as indicators. Baseline data of controls and GC case groups were matched using student’s t-test and χ2 test. The genotype distributions in controls were assessed for Hardy-Weinberg equilibrium using the χ2 test.
Results
Subjects characteristics
In this study, a total of 1,016 subjects (509 GC cases and 507 controls) of the Han ethnicity from Hainan province were enrolled using a case-control experimental design. Table 1 provides a summary of the demographic characteristics and clinical information of the participants. The GC case group (61.35 ± 8.84) consisted of 382 males (75%) and 127 females (25%), and the control group (61.12 ± 11.33) consisted of 379 males (75%) and 128 females (25%). Among the participants, 279 cases (55%) were over the age of 60 years, and 325 cases (62%) were in the control group. There were no significant differences in terms of age (p = 0.712), gender (p = 0.913), smoking (p = 0.333), and drinking (p = 0.063) distributions between the control and GC case groups. Furthermore, it was observed that 314 (62%) patients had adenocarcinoma, 235 (46%) patients had lymph node metastasis, and 239 (47%) patients were in stage III-IV.
Genetic characteristics of selected SNPs
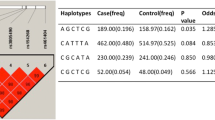
Nine selected SNPs were genotyped, including seven SNPs (rs4613763, rs6880778, rs11742570, rs9292777, rs7725052, rs12186979, and rs10036575) in PTGER4 and two variants (rs10074991 and rs13361707) in PRKAA1 (Table 2). The p-values of HWE for all selected SNPs in PTGER4 and PRKAA1 were > 0.05. The MAFs of rs10074991 and rs13361707 in the PRKAA1 gene, as well as rs10036575 in the PTGER4 gene, were lower in GC patients compared to healthy controls (Table 2). Additionally, the SNP rs10074991 (OR = 0.82, 95% CI = 0.69–0.97, p = 0.024), rs13361707 (OR = 0.82, 95% CI = 0.69–0.98, p = 0.030), and rs10036575 (OR = 0.82, 95% CI = 0.69–0.98, p = 0.029) were identified as protective factors for GC susceptibility.
Overall correlation analysis
Table 3 presents the overall association of the nine selected SNPs with GC susceptibility. The SNP rs10036575 showed a moderate reduction in GC predisposition under the co-dominant (OR = 0.69, 95% CI = 0.49–0.97, p = 0.035) and log-additive (OR = 0.83, 95% CI = 0.70–0.98, p = 0.034) models. The SNP rs10074991 was found to be a protective SNP against GC occurrence under the co-dominant (OR = 0.68, 95% CI = 0.48–0.96, p = 0.028) and log-additive (OR = 0.83, 95% CI = 0.70–0.98, p = 0.028) models. Similarly, rs13361707 exhibited decreased odds of GC under the co-dominant (OR = 0.69, 95% CI = 0.49–0.98, p = 0.036) and log-additive (OR = 0.83, 95% CI = 0.70–0.99, p = 0.034) models.
Stratification analysis by smoking and adenocarcinoma
Stratification analysis by smoking was performed (Table 4). Among non-smokers, the recessive models showed protective effects of rs10036575 [OR (95% CI) = 0.59 (0.35–0.99), p = 0.045], rs10074991 [OR (95% CI) = 0.56 (0.34–0.94), p = 0.029], and rs13361707 [OR (95% CI) = 0.58 (0.35–0.97), p = 0.037] on the occurrence of GC. Table 5 demonstrates that rs10036575 in the co-dominant (OR = 0.67, p = 0.046) and recessive (OR = 0.70, p = 0.045) models, as well as rs10074991 in co-dominant (OR = 0.65, p = 0.034), recessive (OR = 0.70, p = 0.045) and additive (OR = 0.81, p = 0.038) models, were significantly associated with a reduced risk of GC adenocarcinoma.
MDR analysis
The interaction between seven candidate SNPs in PTGER4 is illustrated in Fig. 1. Table 6 displays all the experimental results. The best multi-gene locus model for predicting the risk of GC was found to be the seven-variant model: rs4613763, rs6880778, rs11742570, rs9292777, rs7725052, rs12186979, rs10036575 (CVC = 10/10, p < 0.001), which is the best multi-gene locus model. The six-SNP model is rs4613763, rs11742570, rs9292777, rs7725052, rs12186979, rs10036575 (CVC = 7/10, p < 0.001) and the three-SNP model is rs9292777, rs12186979, rs10036575 (CVC = 6/10, p < 0.001) were also better models. Therefore, the impact of the seven candidate SNPs on GC risk may be interdependent.
Association between SNPs and PTGER4 and PRKAA1 expression
The prediction results through the Ualcan database showed that the expression of PRKAA1 in STAD tissue was significantly higher than that in normal tissues (p < 0.001) (Fig. 2A). However, no difference was found in the expression level of PTGER4 between STAD tissue and normal tissue (Fig. 2A). Furthermore, we used the GTEX database to predict the relationship between SNPs and the expression levels of PTGER4 and PRKAA1 in the stomach. It was found that there were significant differences in gene expression levels among different genotypes of rs10036575, rs10074991, and rs13361707 (p < 0.001, Fig. 2B), indicating that mutations at these loci may affect gene expression.
Association between SNPs and PTGER4 and PRKAA1 expression
A: The expression levels of PTGER4 and PRKAA1 in STAD and normal tissues;
B: The different genotypes of SNPs and genes expression levels in stomach
Alt: Alternative; Het: Heterozygous; Homo: Homozygous; Ref: Reference; STAD: stomach adenocarcinoma
PTGER4 and PRKAA1 may affect GC by mediating RhoA
Referring to mining of the GEO database, the GSE26309 dataset was divided into AGS gastric cancer cells Control group, RhoA activator group (LPA), RhoA GEF exchange factor (NET1) knockdown group (shNET1), NET1 knockdown and RhoA activator group (shNET1-LPA) (Fig. 3A). Among them, Control group (2 samples) and shNET1 group (4 samples) clustered together, while LPA (2 samples) and shNET1-LPA (4 samples) clustered together (Fig. 3B). The results showed that PTGER4 expression (p = 0.003) was observably increased in LPA group compared with shNET1 group (Fig. 3C). The results of protein interaction map (Fig. 4A) and enrichment analysis (Fig. 4B) indicate that 22 proteins related to PTGER4 and PRKAA1 were involved in the regulation of AMPK, Insulin and Adipocytokine signaling pathway. The pathway mechanism revealed that serine/threonine-protein kinase (STK11, LKB1) activates AMpkase (PRKAA1, PRKABs, and PRKAGs) and thus Acetyl-CoA carboxylase 1 (ACACA), AMpkase can also target tuberin (TSC2) in PI3K/AKT signaling pathway to activate Raptor (RPTOR) and mTOR phosphorylation, thus regulating Rho (https://www.kegg.jp/pathway/map04150, Fig. 4C).
Discussion
As we all know, the occurrence and development of GC are the result of the combined action of genes and the environment, and the genetic variations are likely to be related to the etiology of GC [27]. The identification of SNPs that can indicate GC is a significant advancement in the prevention and treatment of GC. In-depth exploration of the correlation between these SNPs and GC is of great importance for early detection and prevention of GC. The findings of this study demonstrated that rs10036575 in PTGER4 and rs10074991 and rs13361707 in PRKAA1 were significantly associated with a reduced risk of GC. Furthermore, these three SNPs were significantly associated with the expression levels of their corresponding genes (PTGER4 and PRKAA1). Additionally, PRKAA1 may affect GC through the mediation of RhoA.
PRKAA1 is the catalytic subunit of the AMPK energy sensor kinase, which regulates cellular energy metabolism through phosphorylation [14]. The AMPK signaling pathways may be involved in the development of GC by participating in cell invasion and metastasis, autophagy and epithelial mesenchymal transformation [28]. Studies have shown that genetic variations of PRKAA 1are risk factors for GC [14, 29]. The relationship between PRKAA1 gene polymorphisms and GC susceptibility has attracted widespread attention from researchers, but the results are not entirely consistent. Numerous reports have indicated that the rs13361707 locus of the PRKAA1 gene can increase GC risk [18, 29,30,31], and the rs10074991 locus can increase the risk of gastric cardia and non-cardia GC [32], which contradicts the findings of this study on the population of Hainan province. This discrepancy may be due to differences in the studied population and the limitations of the sample size, and further verification with a larger sample size is required. Stratified analysis suggests a protective effect of PRKAA1 rs10074991 and rs13361707 on GC in non-smokers, and rs10074991 was also associated with GC adenocarcinoma. Enrichment analysis reveals that PRKAA1, as an AMPKase, can participate in the regulation of AMPK and PI3K/AKT/mTOR pathways. In summary, PRKAA1 gene variation plays a crucial role in GC tumorigenesis.
The protein encoded by PTGER4 (Prostaglandin E Receptor 4) is a member of the G-protein coupled receptor family and is one of the four receptors identified for prostaglandin E2 (PGE2). Studies have found that PTGER4 gene locus are associated with various diseases, such as rs4613763 being associated with ulcerative colitis [33, 34]. Among a large number of cancer patients, the mortality rate is significantly higher in smokers compared to non-smokers, such as in lung cancer [35, 36]. These results are consistent with the stratified analysis of PTGER4 rs10036575 in non-smokers with GC. When BMI ≤ 24 kg/m2, PTGER4 rs10036575 may act as a protective factor for GC, while for BMI > 24 kg/m2, it may be associated with susceptibility to GC, suggesting a certain correlation between GC diagnosis and BMI [37]. In this study, PTGER4 rs10036575 was found to be a protective factor in non-smokers and participants with adenocarcinoma. Moreover, there is a significant correlation between rs10036575 and PTGER4 gene expression. In conclusion, genetic variations and expression levels of PTGER4 may influence GC.
However, there are limitations in the present study that should be addressed Firstly, a large proportion of the study sample lacked information on smoking, alcohol consumption, and BMI, which may have influenced the results. Additionally, the lack of information on Helicobacter pylori infection status limits the ability to draw conclusions on the relationship between PTGER4 and PRKAA1 polymorphisms and GC risk. Future studies should aim to collect more comprehensive information, including these factors, to obtain a more accurate understanding of the potential relationship between PTGER4 and PRKAA1 polymorphisms and GC risk. Finally, this study did not confirm the association between SNPs and gene expression, as well as the specific functional mechanisms. Therefore, further research is required to delve into these matters and gain a more comprehensive understanding.
Conclusion
Our results demonstrate that the PTGER4 gene locus rs10036575 and PRKAA1 gene loci rs10074991 and rs13361707 are associated with GC susceptibility, suggesting that variations in PTGER4 and PRKAA1 may affect GC susceptibility. This study also highlights the protective role of PTGER4 polymorphisms in GC predisposition. These findings provide a new biological perspective for assessing GC risk, exploring its pathogenesis, and developing personalized treatments.
Data Availability
The datasets used and analyzed during this study are available from the corresponding author on reasonable request.
References
Thrift AP, El-Serag HB. Burden of gastric Cancer. Clin Gastroenterol Hepatology: Official Clin Pract J Am Gastroenterological Association. 2020;18(3):534–42.
Machlowska J, Baj J, Sitarz M, Maciejewski R, Sitarz R. Gastric Cancer: epidemiology, risk factors, classification, genomic characteristics and treatment strategies. Int J Mol Sci 2020, 21(11).
Yan C, Zhu M, Ding Y, Yang M, Wang M, Li G, Ren C, Huang T, Yang W, He B, et al. Meta-analysis of genome-wide association studies and functional assays decipher susceptibility genes for gastric cancer in chinese populations. Gut. 2020;69(4):641–51.
Wang Z, Han W, Xue F, Zhao Y, Wu P, Chen Y, Yang C, Gu W, Jiang J. Nationwide gastric cancer prevention in China, 2021–2035: a decision analysis on effect, affordability and cost-effectiveness optimisation. Gut. 2022;71(12):2391–400.
Gao JP, Xu W, Liu WT, Yan M, Zhu ZG. Tumor heterogeneity of gastric cancer: from the perspective of tumor-initiating cell. World J Gastroenterol. 2018;24(24):2567–81.
Shah D, Bentrem D. Environmental and genetic risk factors for gastric cancer. J Surg Oncol. 2022;125(7):1096–103.
Zhang R, Li H, Li N, Shi JF, Li J, Chen HD, Yu YW, Qin C, Ren JS, Chen WQ, et al. Risk factors for gastric cancer: a large-scale, population-based case-control study. Chin Med J. 2021;134(16):1952–8.
Maddineni G, Xie JJ, Brahmbhatt B, Mutha P. Diet and carcinogenesis of gastric cancer. Curr Opin Gastroenterol. 2022;38(6):588–91.
Senchukova MA. Helicobacter Pylori and Gastric Cancer Progression. Curr Microbiol. 2022;79(12):383.
Shi Y, Hu Z, Wu C, Dai J, Li H, Dong J, Wang M, Miao X, Zhou Y, Lu F, et al. A genome-wide association study identifies new susceptibility loci for non-cardia gastric cancer at 3q13.31 and 5p13.1. Nat Genet. 2011;43(12):1215–8.
Tanikawa C, Kamatani Y, Toyoshima O, Sakamoto H, Ito H, Takahashi A, Momozawa Y, Hirata M, Fuse N, Takai-Igarashi T, et al. Genome-wide association study identifies gastric cancer susceptibility loci at 12q24.11-12 and 20q11.21. Cancer Sci. 2018;109(12):4015–24.
Jin G, Lv J, Yang M, Wang M, Zhu M, Wang T, Yan C, Yu C, Ding Y, Li G, et al. Genetic risk, incident gastric cancer, and healthy lifestyle: a meta-analysis of genome-wide association studies and prospective cohort study. Lancet Oncol. 2020;21(10):1378–86.
Shackelford DB, Shaw RJ. The LKB1-AMPK pathway: metabolism and growth control in tumour suppression. Nat Rev Cancer. 2009;9(8):563–75.
Zhang Y, Zhou X, Cheng L, Wang X, Zhang Q, Zhang Y, Sun S. PRKAA1 promotes proliferation and inhibits apoptosis of gastric Cancer cells through activating JNK1 and akt pathways. Oncol Res. 2020;28(3):213–23.
Dargiene G, Streleckiene G, Skieceviciene J, Leja M, Link A, Wex T, Kupcinskas L, Malfertheiner P, Kupcinskas J. TLR1 and PRKAA1 gene polymorphisms in the development of Atrophic Gastritis and Gastric Cancer. J Gastrointest Liver Diseases: JGLD. 2018;27(4):363–9.
Jiang Y, Li W, Lu J, Zhao X, Li L. Association between PRKAA1 rs13361707 T > C polymorphism and gastric cancer risk: evidence based on a meta-analysis. Medicine. 2018;97(14):e0302.
Chen M, Jiang B, He B, Tang M, Wang P, Chen L, Lu J, Lu P. Genetic variations in PRKAA1 predict the risk and progression of gastric Cancer. BMC Cancer. 2018;18(1):923.
Kim YD, Yim DH, Eom SY, Moon SI, Yun HY, Song YJ, Youn SJ, Hyun T, Park JS, Kim BS, et al. Risk of gastric cancer is associated with PRKAA1 gene polymorphisms in Koreans. World J Gastroenterol. 2014;20(26):8592–8.
Baba Y, Nosho K, Shima K, Goessling W, Chan AT, Ng K, Chan JA, Giovannucci EL, Fuchs CS, Ogino S. PTGER2 overexpression in colorectal cancer is associated with microsatellite instability, independent of CpG island methylator phenotype. Cancer Epidemiol Biomarkers Prevention: Publication Am Association Cancer Res Cosponsored Am Soc Prev Oncol. 2010;19(3):822–31.
Tongtawee T, Bartpho T, Kaewpitoon S, Kaewpitoon N, Dechsukhum C, Leeanansaksiri W, Loyd RA, Talabnin K, Matrakool L, Panpimanmas S. Genetic polymorphisms in TLR1, TLR2, TLR4, and TLR10 of Helicobacter pylori-associated gastritis: a prospective cross-sectional study in Thailand. Eur J cancer Prevention: Official J Eur Cancer Prev Organisation (ECP). 2018;27(2):118–23.
Sugimoto Y, Narumiya S. Prostaglandin E receptors. J Biol Chem. 2007;282(16):11613–7.
Hawcroft G, Ko CW, Hull MA. Prostaglandin E2-EP4 receptor signalling promotes tumorigenic behaviour of HT-29 human colorectal cancer cells. Oncogene. 2007;26(21):3006–19.
Han S, Roman J. Suppression of prostaglandin E2 receptor subtype EP2 by PPARgamma ligands inhibits human lung carcinoma cell growth. Biochem Biophys Res Commun. 2004;314(4):1093–9.
Tian L, Suzuki M, Nakajima T, Kubo R, Sekine Y, Shibuya K, Hiroshima K, Nakatani Y, Fujisawa T, Yoshino I. Clinical significance of aberrant methylation of prostaglandin E receptor 2 (PTGER2) in nonsmall cell lung cancer: association with prognosis, PTGER2 expression, and epidermal growth factor receptor mutation. Cancer. 2008;113(6):1396–403.
Kabashima K, Sakata D, Nagamachi M, Miyachi Y, Inaba K, Narumiya S. Prostaglandin E2-EP4 signaling initiates skin immune responses by promoting migration and maturation of Langerhans cells. Nat Med. 2003;9(6):744–9.
Kanehisa M, Goto S. KEGG: kyoto encyclopedia of genes and genomes. Nucleic Acids Res. 2000;28(1):27–30.
Mocellin S, Verdi D, Pooley KA, Nitti D. Genetic variation and gastric cancer risk: a field synopsis and meta-analysis. Gut. 2015;64(8):1209–19.
Benito-Cuesta I, Ordóñez-Gutiérrez L, Wandosell F. AMPK activation does not enhance autophagy in neurons in contrast to MTORC1 inhibition: different impact on β-amyloid clearance. Autophagy. 2021;17(3):656–71.
Qiu LX, He J, Cheng L, Zhou F, Wang MY, Sun MH, Zhou XY, Li J, Guo WJ, Wang YN, et al. Genetic variant of PRKAA1 and gastric cancer risk in an eastern chinese population. Oncotarget. 2015;6(40):42661–6.
Eom SY, Hong SM, Yim DH, Kwon HJ, Kim DH, Yun HY, Song YJ, Youn SJ, Hyun T, Park JS, et al. Additive interactions between PRKAA1 polymorphisms and Helicobacter pylori CagA infection associated with gastric cancer risk in Koreans. Cancer Med. 2016;5(11):3236–335.
Helgason H, Rafnar T, Olafsdottir HS, Jonasson JG, Sigurdsson A, Stacey SN, Jonasdottir A, Tryggvadottir L, Alexiusdottir K, Haraldsson A, et al. Loss-of-function variants in ATM confer risk of gastric cancer. Nat Genet. 2015;47(8):906–10.
Hu N, Wang Z, Song X, Wei L, Kim BS, Freedman ND, Baek J, Burdette L, Chang J, Chung C, et al. Genome-wide association study of gastric adenocarcinoma in Asia: a comparison of associations between cardia and non-cardia tumours. Gut. 2016;65(10):1611–8.
Latiano A, Palmieri O, Latiano T, Corritore G, Bossa F, Martino G, Biscaglia G, Scimeca D, Valvano MR, Pastore M, et al. Investigation of multiple susceptibility loci for inflammatory bowel disease in an italian cohort of patients. PLoS ONE. 2011;6(7):e22688.
McGovern DP, Gardet A, Törkvist L, Goyette P, Essers J, Taylor KD, Neale BM, Ong RT, Lagacé C, Li C, et al. Genome-wide association identifies multiple ulcerative colitis susceptibility loci. Nat Genet. 2010;42(4):332–7.
Jung KJ, Jeon C, Jee SH. The effect of smoking on lung cancer: ethnic differences and the smoking paradox. Epidemiol Health. 2016;38:e2016060.
Bagnardi V, Rota M, Botteri E, Tramacere I, Islami F, Fedirko V, Scotti L, Jenab M, Turati F, Pasquali E, et al. Alcohol consumption and site-specific cancer risk: a comprehensive dose-response meta-analysis. Br J Cancer. 2015;112(3):580–93.
Guggenheim DE, Shah MA. Gastric cancer epidemiology and risk factors. J Surg Oncol. 2013;107(3):230–6.
Acknowledgements
The authors thank all participants and volunteers in this study.
Funding
This work was supported by the 2020 Hainan Provincial Major Science and Technology Project (grant number: ZDKJ202005) and the specific research fund of The Innovation Platform for Academinicians of Hainan Province (grant number: YSPTZX202029).
Author information
Authors and Affiliations
Contributions
SY Y, RS T, and ZW C drafted the manuscript; PL and FX H performed the DNA extraction and genotyping; GH Y, RL Z, and YN L performed the data analysis; SY Y, RS T, and ZW C revised the manuscript, JS conceived and supervised the study. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Approval for this study was taken from the Ethics Committee of Hainan Cancer Hospital and all experiments complied with the Declaration of Helsinki. a. Informed consent was obtained from all participants. All methods were carried out in accordance with relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yu, S., Tu, R., Chen, Z. et al. Association of PTGER4 and PRKAA1 genetic polymorphisms with gastric cancer. BMC Med Genomics 16, 209 (2023). https://doi.org/10.1186/s12920-023-01645-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12920-023-01645-1