Abstract
Background
A multitude of studies have highlighted that copy number variants (CNVs) are associated with neurodevelopmental disorders (NDDs) characterized by a wide range of clinical characteristics. Benefiting from CNV calling from WES data, WES has emerged as a more powerful and cost-effective molecular diagnostic tool, which has been widely used for the diagnosis of genetic diseases, especially NDDs. To our knowledge, isolated deletions on chromosome 1p13.2 are rare. To date, only a few patients were reported with 1p13.2 deletions and most of them were sporadic. Besides, the correlation between 1p13.2 deletions and NDDs remained unclear.
Case presentation
Here, we first reported five members in a three-generation Chinese family who presented with NDDs and carried a novel 1.41 Mb heterozygous 1p13.2 deletion with precise breakpoints. The diagnostic deletion contained 12 protein-coding genes and was observed to segregate with NDDs among the members of our reported family. Whether those genes contribute to the patient’s phenotypes is still inconclusive.
Conclusions
We hypothesized that the NDD phenotype of our patients was caused by the diagnostic 1p13.2 deletion. However, further in-depth functional experiments are still needed to establish a 1p13.2 deletion-NDDs relationship. Our study might supplement the spectrum of 1p13.2 deletion-NDDs.
Similar content being viewed by others
Background
Neurodevelopmental disorders (NDDs), encompassing a wide range of clinical phenotypes, include but are not limited to intellectual disability (ID), autism spectrum disorder (ASD), schizophrenia (SCZ), attention deficit hyperactivity disorder (ADHD), developmental delay (DD), epilepsy, and specific learning disorders (SLD) [1,2,3]. A multitude of studies have highlighted that copy number variants (CNVs) are associated with NDDs [1, 4,5,6]. Nevertheless, in most of the observed clinical cases, the pathogenicity of CNVs, especially rare CNVs, remains unclear.
Nowadays, in addition to the conventional detection of single nucleotide variants (SNVs) and small insertions/deletions (Indels), exome-based CNV analysis is another important application of whole-exome sequencing (WES) [7,8,9,10]. Here, by trio WES, a novel 1.41 Mb heterozygous 1p13.2 deletion was detected in a patient with NDDs, and the potentially pathogenic SNVs/Indels related to the patients’ phenotypes were excluded.
To the best of our understanding, isolated deletions on chromosome 1p13.2 are uncommon; thus far, only five published pieces of literature have reported that patients with 1p13.2 deletions displayed NDDs [11,12,13,14,15]. But few patients have a family history, and the definite evidence of the association between 1p13.2 deletion and NDDs still needs further functional studies.
Case presentation
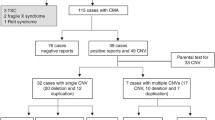
The Guangdong Women and Children Hospital Medical Ethics Committee approved the study, and informed consent was obtained. A 34-year-old gravida 3, para 3 (G3P3) Chinese woman, with neurodevelopmental disability, underwent genetic counseling in Huizhou No.2 Maternal and Children’s Healthcare Hospital and was referred to Medical Genetic Centre in Guangdong Women and Children Hospital for further genetic testing. The proband had a mild facial appearance with full eyebrows, hypertelorism, ptosis, low-set ears, upturned nose, overbite, slightly open mouth and webbed neck, pictures of whom was not authorized by her family. She could sit, walk and run without support, but her gross motor milestones were unclear. No other physical abnormalities were observed during genetic counseling. She was noted to present ID, studied in a special education school in childhood, and could not perform instrumental activities of daily living (including cooking, cleaning, washing clothes, making telephone calls, financial management, and so on). Her receptive language and speech were significantly delayed, and she communicated with others just by a few words. Activities of daily living, such as dressing, eating, bathing and toileting, could be performed by herself. The patient had not any epilepsy history and denied behavioral problems, including ADHD, motor stereotypies, self-injury behavior, aggressive behavior and social anxiety. Four members of the proband’s family, including her mother, her younger brother and two sons, had similar symptoms. In contrast, her elder brother, sister and daughter (who died in a traffic accident) had normal phenotypes (Fig. 1A). After genetic counseling, the proband and her family finally decided to receive trio WES, and also they accepted the screening for fragile X syndrome for her elder son. Further mental and behavioral assessments and brain Magnetic Resonance Imaging (MRI) examinations could not be conducted in the family.
(A) Pedigree for this three-generation family. Arrows indicate the proband. Solid circles/squares indicate individuals with a heterozygous 1p13.2 deletion. (B) Electrophoresis of gap-PCR products. The presence of an 836 bp band indicated that the corresponding individuals in the proband’s family carried the 1p13.2 deletion. (C) The accurate deletion breakpoints for the patients (I-2, II-3, II-5, III-2 and III-3), were validated by Sanger sequencing. A 1,408,072 bp deletion at 1p13.2 was identified (chr1:113,536,526–114,944,597). (D) The 1.31 Mb deletion at 1p13.2 (chr1: 113,538,670–114,937,750) of our proband was detected by chromosomal microarray analysis. (E) Schematic representation of the deletion region in our patients and those included for further analysis, with overlapping deletion regions at 1p13.2. Ideogram of chromosome 1, physical map and deleted regions are referred to their placement on the UCSC Genome Browser on Human (GRCh37/hg19).
Methods
Trio whole-exome sequencing
Peripheral blood samples (2 mL) were drawn from the proband and her family. Genomic DNA samples were isolated using RelaxGene Blood DNA System (Tiangen, Beijing, China), following the manufacturer’s instruction.
Trio WES was performed on the proband and her parents. The target genomic regions were captured by hybridizing the genomic DNA sample library with the xGen® Exome Research Panel v1.0 (IDT, USA). High-throughput sequencing was then performed on the Illumina NovaSeq6000 platform (Illumina, San Diego, CA, USA) with 150 bp paired-end reads. Briefly, raw sequencing reads were aligned to the human reference genome hg19/GRCh37 via BWA [16]. Variants and indels were called by the HaplotypeCaller tool of GATK [17]. VEP was employed to identify the effect of all variants followed by variant annotation with AnnoVar [18]. The annotated variants were filtrated in an in-house stepwise protocol as shown in the Supplemental method. Notably, each variant was compared against public databases, including gnomAD, 1000 genomes project, NHLBI Exome Sequencing Project 6500 (ESP6500), and Exome Aggregation Consortium (ExAC), to achieve allele frequency in the general population. In terms of possible influence on the protein function, candidate variants were evaluated by VarCards [19]. The classification of candidate variants was interpreted based on the American College of Medical Genetics (ACMG) guidelines 2015 [20].
Copy number variants (CNVs) were called by CNVkit [21]. To create a stable and reliable CNV reference, in-house 80 samples without any CNV events larger than 1Mbp over the same sequencing protocol were selected for reference training in an iterative manner. AnnotSV and its annotation databases were locally installed to annotate detected CNV events for each tested sample for following clinical interpretation [22]. The Database of Genomic Variants (DGV) (http://dgv.tcag.ca/dgv/app/home), the DatabasE of genomiC varIation and Phenotype in Humans using Ensembl Resources (DECIPHER) (https://www.deciphergenomics.org/browser) and the Clinical Genome Resource (ClinGen) (http://www.ncbi.nlm.nih.gov/projects/dbvar/clingen/) were used to determine the pathogenicity of candidate CNVs. The clinical significance of the candidate CNVs was evaluated according to the criteria of the ACMG and the ClinGen [23].
Chromosomal microarray analysis
To validate the CNV found by trio WES, chromosomal microarray analysis (CMA) was performed for the proband using an Affymetrix Cytoscan 750K GeneChip. The procedure was performed according to the manufacturer’s instruction. Data analysis was performed using the Chromosome Analysis Suite (ChAS) 4.1 software. CNVs larger than 100 kb or those that affected more than 50 contiguous probes were considered. The pathogenicity evaluation of candidate CNVs referred to the method described in the trio WES section above.
Testing for fragile X syndrome, validation and pedigree analysis
The CGG repeats in the 5′-untranslated region of the FMR1 gene were detected by fluorescence polymerase chain reaction products [24]. Gap-PCR was used to verify the diagnostic deletion, following the manufacturer’s protocol using LA Taq DNA polymerase (TaKaRa, Chiba, Japan). Forward and reverse primers were designed flanking the deletion breakpoints (forward: 5’ GCTTGAGGACAGTAATCACATC 3’; reverse: 5’ GCCTGTAGTCTGATTGCCA 3’). The gap-PCR products were electrophoresed, then sequenced in Tianyi Huiyuan Biotechnology Co., Ltd. (Wuhan, China), and the deletion breakpoints were validated by direct Sanger sequencing.
Results
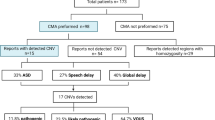
The triplet repeat number of CGG in the FMR1 gene of the proband’s elder son was 25, which is in the normal range (6 to 44 CGG; Supplemental Figure S1) [24]. It partially demonstrated that the NDD phenotype in this family is not related to fragile X syndrome. Subsequently, we evaluated the filtered genetic variants detected by trio WES. Several rare nonsynonymous variants in NDDs-associated genes were identified; these are detailed in Supplemental Table S1. Three rare, maternally-inherited missense variants were identified in genes associated with autosomal dominant conditions that were classified as either benign or likely benign. Other heterozygous variants were in genes associated with autosomal recessive diseases. Based on the pathogenic classification of variants and the inheritance model, none of the nonsynonymous variants were considered to contribute to the phenotype. Besides, the trio WES analysis revealed a maternally inherited 1.31 Mb deletion at 1p13.2 (GRCh37/hg19 chr1: 113,633,912–114,944,107) in the proband. No nonsynonymous hemizygous variants were identified in the deletion region and the putative deletion was confirmed by CMA (Fig. 1D).
As depicted in the electrophoresis diagram (Fig. 1B), the presence of an 836 bp band indicated that the corresponding NDD patients of the family carried this deletion. All five symptomatic patients, including the proband (II-3), her mother (I-2), her younger brother (II-5) and her two sons (III-2 and III-3), carried the same heterozygous deletion, while the deletion was absent in the other three healthy individuals (I-1, II-1 and II-4). As shown in Fig. 1C, the accurate breakpoints of the deletion were identified by Sanger sequencing, by which the size of the deletion was 1,408,072 bp (chr1:113,536,526–114,944,597).
No CNVs fully encompassing the diagnostic 1p13.2 deletion in our cases were recorded in the DGV up to November 11, 2022. However, within the 1,408,072 bp deletion of 1p13.2 identified, one potentially benign CNV larger than 1 Mb in size was found in two individuals in the DGV (accession number: esv23869). According to the data in the DECIPHER database, the deleted 1p13.2 region covered 12 protein-coding genes, which were all listed in Online Mendelian Inheritance in Man (OMIM) database (Supplemental Table S2). Among them, three genes were human genetic disease-associated: AP4B1, associated with autosomal recessive spastic paraplegia 47 (MIM # 614,066), LRIG2, associated with autosomal recessive urofacial syndrome 2 (MIM # 615,112), and PTPN22, associated with susceptibility to diabetes type 1 (MIM # 222,100), rheumatoid arthritis (MIM # 180,300), and systemic lupus erythematosus (MIM # 152,700). Besides, the diagnostic deletion region encompassed HIPK1 and involved parts of TRIM33. The DECIPHER database indicates that these two genes are potentially haploinsufficient, yet there are no definitive human diseases associated with them in the OMIM database (retrieved February 2, 2023).
Discussion and conclusions
NDDs are characterized by a broad range of conditions that impact brain development and produce impairments of functioning. Although several contributing factors, such as prenatal exposure to the drug, virus infection and toxic agents, can lead to congenital NDDs, genetic factors are widely considered to be the most common causes. Unfortunately, due to the complex genetic heterogeneity of NDDs, it is still sometimes difficult to identify the underlying genetic cause. WES outperformed traditional methods in the detection of the prevalent types of pathogenic variants (SNVs and Indels) for NDDs, and has been widely used for genetic testing for patients with NDDs [25, 26]. Nowadays, the combination of variant screening and CNV calling simultaneously was increasingly used in WES, which largely improved the detection efficiency for the diagnosis of NDDs. Here, we reported a proband with NDD, who carried a novel 1.41 Mb heterozygous deletion located at 1p13.2 identified by trio WES. Besides, no pathogenic or likely pathogenic SNVs/Indels associated with her observed phenotypes were detected by trio WES.
We sought to evaluate associations between the 1p13.2 deletion and NDDs. To the best of our knowledge, only five articles have reported 1p13.2 deletions in five patients [11,12,13,14,15]. Additionally, 14 individuals with chromosomal 1p13.2 deletions (0.17-18.88 Mb) partially overlapping the deletion region of our case have been documented in the DECIPHER database (retrieved November 11, 2022), and one of them (DECIPHER patient ID: 274,660) was reported by Linhares et al. in the previous literature [14]. The detailed phenotypes of the reported 18 individuals were summarized in Table 1. To perform a genotype-phenotype correlation study of 1p13.2 deletions, eight previously described patients were excluded for further analysis, including four patients (P5, P6, P7 and P9) carrying double genetic CNVs or pathogenic SNVs, and four patients (P12, P14, P15 and P18) without any NDDs-associated phenotypes recorded in the DECIPHER database. We compared the clinical characteristics of our patients to the remaining 10 patients (Table 2). As shown, a total of 9 out of 10 (90%) patients were described with intellectual disability, 8 (80%) with language impairments, and 8 (80%) with gross motor developmental delay. Besides, 50-60% of cases were observed with short stature, facial appearance and neck abnormality. Such features have occurred in Noonan Syndrome, which is also characterized by developmental delay, intellectual impairment, short stature, and distinctive facial features, such as low-set ears, hypertelorism and ptosis [14]. The deletion region of all the 10 preceding cases encompassed the NRAS gene. The previous studies suggested that such features similar to Noonan Syndrome may be potentially attributed to the haploinsufficiency of the NRAS gene [11, 14]. The definitive association between alteration of the NRAS gene and Noonan syndrome has been demonstrated by the ClinGen Intellectual Disability and Autism Gene Curation Expert Panel. However, the diagnostic 1.41 Mb deletion (chr1:113,536,526–114,944,597) at 1p13.2 in our cases contains 12 protein-coding genes, excluding NRAS. As the proband’s phenotype described above, she also had an intellectual disability, language impairments, a mild facial appearance and a webbed neck, but did not present short stature. It suggested that the phenotypes of our cases could not be explained by the haploinsufficiency of the NRAS gene. We focused on the overlapping deletion regions at 1p13.2 between the 10 patients included in the further analysis and our patient. As illustrated in Fig. 1E, except that the deletion region of P3 was relatively unclear, the overlapping region extends from 113,709,879 to 114,944,597 at 1p13.2, covering 11 genes (Supplemental Table S2). As far as we can see, based on inheritance patterns and clinical correlations, the haploinsufficiency of the genes AP4B1, LRIG2, PTPN22 and HIPK1 may not be thought to lead to the phenotype of this family. To the highest degree of our knowledge, only two studies have suggested that TRIM33 might be a candidate gene associated with autism and that the decreased TRIM33 gene expression might be correlated with autism symptoms [27, 28]. Despite evidence suggesting a potential correlation between the haploinsufficiency of TRIM33 and the development of autism, a kind of NDDs, the correlation is yet to be established. Nevertheless, the phenotypes of our patients could not be fully explained by autism. It stays inconclusive whether the overlapping region contributes to the patients’ phenotypic characteristics.
Many studies have demonstrated that recurrent CNVs are common causes of NDDs and are associated with a constellation of neurodevelopmental traits [5, 29]. Nevertheless, non-recurrent CNVs are also significant pathogenic factors of NDDs. Nearly 5.1% of patients with ID, DD, ASD and multiple congenital abnormalities were found to have a single non-recurrent rare CNV, as well as 7.1% of patients had a known recurrent CNV [30]. Among the previously reported 10 individuals, de novo deletions have been observed in 8 patients (80%), and the inheritances of the remaining two are yet unknown. The 1p13.2 deletion found in our patient was inherited from her mother who had similar phenotypes. Furthermore, no recurrent deletions were reported in the region of 1p13.2, indicating that this region is not prone to hotspot deletion.
In the present study, we first identified a novel 1.41 Mb heterozygous 1p13.2 deletion with precise breakpoints in five patients in a three-generation Chinese family. The 1p13.2 deletion segregates in the NDDs family. Therefore, that may provide strong evidence to support the pathogenicity of the 1p13.2 deletion. It suggested that the NDD phenotype of our patients could be explained by the 1.41 Mb 1p13.2 deletion. Our study might supplement the spectrum of 1p13.2 deletion-NDDs. However, further in-depth functional experiments are still needed to establish a genotype and phenotype relationship.
Data Availability
The raw sequence data reported in this paper have been deposited in the Genome Sequence Archive (Genomics, Proteomics & Bioinformatics 2021) in National Genomics Data Center (Nucleic Acids Res 2022), China National Center for Bioinformation / Beijing Institute of Genomics, Chinese Academy of Sciences (GSA-Human: HRA003956) that are publicly accessible at https://ngdc.cncb.ac.cn/gsa-human.
References
Girirajan S, Brkanac Z, Coe BP, Baker C, Vives L, Vu TH, et al. Relative burden of large CNVs on a range of neurodevelopmental phenotypes. PLoS Genet. 2011;7:e1002334.
Morris-Rosendahl DJ, Crocq M-A. Neurodevelopmental disorders-the history and future of a diagnostic concept. Dialogues Clin Neurosci. 2020;22:65–72.
Wilfert AB, Sulovari A, Turner TN, Coe BP, Eichler EE. Recurrent de novo mutations in neurodevelopmental disorders: properties and clinical implications. Genome Med. 2017;9:101.
Coe BP, Witherspoon K, Rosenfeld JA, van Bon BWM, Vulto-van Silfhout AT, Bosco P, et al. Refining analyses of copy number variation identifies specific genes associated with developmental delay. Nat Genet. 2014;46:1063–71.
Cooper GM, Coe BP, Girirajan S, Rosenfeld JA, Vu TH, Baker C, et al. A copy number variation morbidity map of developmental delay. Nat Genet. 2011;43:838–46.
Kendall KM, Bracher-Smith M, Fitzpatrick H, Lynham A, Rees E, Escott-Price V, et al. Cognitive performance and functional outcomes of carriers of pathogenic copy number variants: analysis of the UK Biobank. Br J Psychiatry. 2019;214:297–304.
Guo W, Lai Y, Yan Z, Wang Y, Nie Y, Guan S, et al. Trio-whole-exome sequencing and preimplantation genetic diagnosis for unexplained recurrent fetal malformations. Hum Mutat. 2020;41:432–48.
Xiang J, Ding Y, Yang F, Gao A, Zhang W, Tang H, et al. Genetic analysis of Children with Unexplained Developmental Delay and/or intellectual disability by whole-exome sequencing. Front Genet. 2021;12:738561.
Zhai Y, Zhang Z, Shi P, Martin DM, Kong X. Incorporation of exome-based CNV analysis makes trio-WES a more powerful tool for clinical diagnosis in neurodevelopmental disorders: a retrospective study. Hum Mutat. 2021;42:990–1004.
Zhao J, Li J, Lai Q, Yu Y. Combined use of gap-PCR and next-generation sequencing improves thalassaemia carrier screening among premarital adults in China. J Clin Pathol. 2020;73:488–92.
Alagia M, Bernardo P, Genesio R, Gennaro E, Brunetti-Pierri N, Coppola A, et al. Dual diagnosis in a child with familial SCN8A-related encephalopathy complicated by a 1p13.2 deletion involving NRAS gene. Neurol Sci. 2021;42:2115–7.
Bisgaard A-M, Rasmussen LN, Møller HU, Kirchhoff M, Bryndorf T. Interstitial deletion of the short arm of chromosome 1 (1p13.1p21.1) in a girl with mental retardation, short stature and colobomata. Clin Dysmorphol. 2007;16:109–12.
Fitzgibbon GJ, Kingston H, Needham M, Gaunt L. Haploinsufficiency of the nerve growth factor beta gene in a 1p13 deleted female child with an insensitivity to pain. Dev Med Child Neurol. 2009;51:833–7.
Linhares ND, Freire MCM, Cardenas RGC do, Pena CL, Lachlan HB, Dallapiccola K. 1p13.2 deletion displays clinical features overlapping Noonan syndrome, likely related to NRAS gene haploinsufficiency. Genet Mol Biol. 2016;39:349–57.
Mattia FR, Wardinsky TD, Tuttle DJ, Grix A, Smith KA, Walling P. Interstitial deletion of the short arm of chromosome 1 (46XY, del(1)(p13p22.3)). Am J Med Genet. 1992;44:551–4.
Li H, Durbin R. Fast and accurate short read alignment with Burrows-Wheeler transform. Bioinformatics. 2009;25:1754–60.
McKenna A, Hanna M, Banks E, Sivachenko A, Cibulskis K, Kernytsky A, et al. The genome analysis Toolkit: a MapReduce framework for analyzing next-generation DNA sequencing data. Genome Res. 2010;20:1297–303.
McLaren W, Gil L, Hunt SE, Riat HS, Ritchie GRS, Thormann A, et al. The Ensembl variant effect predictor. Genome Biol. 2016;17:122.
Li J, Shi L, Zhang K, Zhang Y, Hu S, Zhao T, et al. VarCards: an integrated genetic and clinical database for coding variants in the human genome. Nucleic Acids Res. 2018;46:D1039–48.
Richards S, Aziz N, Bale S, Bick D, Das S, Gastier-Foster J, et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med. 2015;17:405–24.
Talevich E, Shain AH, Botton T, Bastian BC. CNVkit: genome-wide Copy Number Detection and visualization from targeted DNA sequencing. PLoS Comput Biol. 2016;12:e1004873.
Geoffroy V, Herenger Y, Kress A, Stoetzel C, Piton A, Dollfus H, et al. AnnotSV: an integrated tool for structural variations annotation. Bioinformatics. 2018;34:3572–4.
Riggs ER, Andersen EF, Cherry AM, Kantarci S, Kearney H, Patel A, et al. Technical standards for the interpretation and reporting of constitutional copy-number variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics (ACMG) and the Clinical Genome Resource (ClinGen). Genet Med. 2020;22:245–57.
Saluto A, Brussino A, Tassone F, Arduino C, Cagnoli C, Pappi P, et al. An enhanced polymerase chain reaction assay to detect pre- and full mutation alleles of the fragile X mental retardation 1 gene. J Mol Diagn. 2005;7:605–12.
Miller DT, Adam MP, Aradhya S, Biesecker LG, Brothman AR, Carter NP, et al. Consensus statement: chromosomal microarray is a first-tier clinical diagnostic test for individuals with developmental disabilities or congenital anomalies. Am J Hum Genet. 2010;86:749–64.
Srivastava S, Love-Nichols JA, Dies KA, Ledbetter DH, Martin CL, Chung WK, et al. Meta-analysis and multidisciplinary consensus statement: exome sequencing is a first-tier clinical diagnostic test for individuals with neurodevelopmental disorders. Genet Med. 2019;21:2413–21.
Xia K, Guo H, Hu Z, Xun G, Zuo L, Peng Y, et al. Common genetic variants on 1p13.2 associate with risk of autism. Mol Psychiatry. 2014;19:1212–9.
Norouzi Ofogh S, Rasoolijazi H, Shahsavand Ananloo E, Shahrivar Z, Joghataei MT, Sadeghi B, et al. Alteration of TRIM33 expression at transcriptional and translational levels is correlated with autism symptoms. J Mol Neurosci. 2021;71:1368–77.
Smajlagić D, Lavrichenko K, Berland S, Helgeland Ø, Knudsen GP, Vaudel M, et al. Population prevalence and inheritance pattern of recurrent CNVs associated with neurodevelopmental disorders in 12,252 newborns and their parents. Eur J Hum Genet. 2021;29:205–15.
Wayhelova M, Smetana J, Vallova V, Hladilkova E, Filkova H, Hanakova M, et al. The clinical benefit of array-based comparative genomic hybridization for detection of copy number variants in czech children with intellectual disability and developmental delay. BMC Med Genomics. 2019;12:111.
Acknowledgements
We thank the proband and her family for sharing information.
Funding
This work was supported by Guangzhou Municipal Science and Technology Project (202102080358).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Data collection was performed by Lihua Yu, Hongke Ding and Min Liu. Experiments were performed by Ling Liu, Jian Lu, Fangfang Guo. Bioinformatic analysis was performed by Qi Zhang. The entire investigation was supervised by Yan Zhang. The first draft of the manuscript was written by Lihua Yu and Yan Zhang, and all authors revised the manuscript. All authors read and approved the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare that there are no conflicts of interest.
Ethics approval and consent to participate
The study was approved by the Guangdong Women and Children Hospital Medical Ethics Committee (protocol code 202201178 and approved on July 13, 2022). All methods were carried out in accordance with the relevant guidelines and regulations. Informed consent to participate was obtained from all subjects and their legal guardian.
Consent for publication
Informed consent for publication of identifying information/images in an online open-access publication was obtained from all subjects and their legal guardian.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yu, L., Ding, H., Liu, M. et al. A novel 1p13.2 deletion associates with neurodevelopmental disorders in a three-generation pedigree. BMC Med Genomics 16, 114 (2023). https://doi.org/10.1186/s12920-023-01534-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12920-023-01534-7