Abstract
Background
Sickle cell disease (SCD) is a hemoglobin disorders that concern 300,000 newborns each year around the world. There are hemoglobin haplotypes that affect SCD clinic expression.
Methods
Our goal was to identify the hemoglobin’s haplotypes among individuals with mild malaria independently of SCD status in Côte d’Ivoire. To determine these haplotypes, specific restriction enzyme (RE) is used after PCR amplification with each primer. According to the digestion of PCR product by RE, five hemoglobin’s haplotypes are found in the world.
Results
In Côte d’Ivoire, no study has yet deeply described the distribution of haplotypes. Four different “classical” haplotypes of hemoglobin were detected: Benin (56.5%), Bantou (28.5%), Senegal (4%), Cameroun (1%); and 10% of atypical profiles. Heterozygous haplotype (69%) were more frequent than homozygous haplotype (31%).
Conclusions
In this preliminary study, we note a high prevalence of atypical and heterozygous haplotype. Benin haplotype that is associated with severity of SCD was most predominant in our studied population.
Similar content being viewed by others
Background
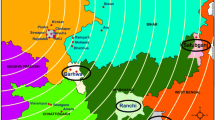
Sickle cell disease (SCD) is a hemoglobin disorders that concerns 300,000 newborns each year around the world [1]. Sub-Saharan’s countries harbored the highest prevalence with S hemoglobin in Central Africa and C in Sahelian areas [2,3,4]. There are hemoglobin haplotypes that affect SCD clinic expression. These haplotypes have different origins [5, 6] and some studies indicated the relation between SCD clinics manifestations and hemoglobin haplotypes. In fact, the presence of some haplotypes reduce the SCD symptoms; and other haplotypes amplify the clinics manifestations [7,8,9,10,11,12,13,14]. To determine these haplotypes, specific restriction enzymes (RE) are used after PCR amplification. Relative to the digestion of PCR product by RE; there are five hemoglobin’s haplotypes around the world: Bantou (CAR), Arabic, Senegal, Cameroun and Benin [15, 16]. In Côte d’Ivoire, no study has yet deeply described the distribution SCD haplotypes. Here we conducted a retrospective preliminary study in Côte d’Ivoire to identify the hemoglobin’s haplotypes among individuals with mild malaria independently to SCD status.
Materials and methods
Sample collections
Abidjan is the economic capital of Côte d’Ivoire with five million inhabitants from a large number of neighboring countries. Participants were recruited from CSUCOM Anonkoua-Kouté (Abidjan, Abobo) in 2013 and 2016 among patients attending the center with mild malaria (parasitemia more than 2000 parasites/µL blood).
The hemoglobin status of the patients was determined based on a standard acetate electrophoresis of hemoglobin using Sebia® Hemoglobin electrophoresis, following the protocol of the manufacturer.For molecular typing, 50 µL of total blood was dried on 5 M Whatman® paper and stored in zip locked bag contained silicate gel until use in 2020.
Haplotype molecular typing
The hemoglobin electrophoresis was performed following the manufacturer’s recommendations with total blood. For molecular typing, DNA purification was performed on blood spots using the Qiagen®Blood Minikit as recommended by the manufacturer. For amplification, different programs were used according to the couple of primers used. Nine pairs of primers have been used following Sutton and co [15] and Doupa and co [17] (Table 1). After amplification, each type of PCR products was digested with a related restriction enzyme (RE). The haplotype profiles were identified according to Sutton and co [15] and Doupa and co [17]. (Table 2).
Results
Demographic results
Of the total 100 patients included in the study, 55% were women. The average age of the patients recruited was 14.5 years.
Haplotype typing
Four different “classical” haplotypes of hemoglobin were detected, Benin (56.5%), Bantou (28.5%), Senegal (4%) and Cameroun (1%). The Arabic haplotype was not observed. In addition, 10% of atypical profiles were detected (i.e. 20 haplotypes). Atypic haplotypes were presents in the groups of Benin (15/20) and Bantou (01/20) (Table 2, Fig. 1).
Gamma PCR products digestion by HindIII (Restriction Enzyme). PCR product size for Gamma is 782 pb xhich gives two fragments of 436 pb and 346 pb. After digestion by HindIII. Homozygote sample will present only 782 pb lane or 436 pb and 346 pb. Heterozygote sample will present three (03) lanes: 782 pb, 436 pb and 346 pb. On this gel, for example, homozygotes samples without restriction site of HindIII are N°7, N°9, N°12, N°18 and N°24. Homozygotes with restriction site are N°2, N°11, N°15 and N°23. All other are heterozygotes
Heterozygous (69%) were more frequent than homozygous (31%). For homozygote, women were more affected than men (40/69 and 29/69 respectively).
Hemoglobin typing and malaria diagnostic
The AA genotype represented 87% of the samples. The other genotypes were AC, AS, SC and CC (8%, 2%, 2% and 1% respectively, Table 3).
Mean parasitemia was 46,376 parasites/µL blood, without any significant difference between haplotypes (t-test, p = 0.95).
All participants with AC or CC genotypes were from the Benin group (homozygote Benin/Benin or Benin/Bantu) whereas AS was found in the Bantu group (Table 3). Atypic, Cameroun and Senegal haplotypes were observed only in normal hemoglobin group (Table 3).
Discussion
Several authors have highlighted the interest of studying hemoglobin haplotypes for individuals with hemoglobin disorders as a modulation of the clinical profile of the disease [7,8,9,10,11,12,13,14]. In Côte d'Ivoire, there is not available data on hemoglobin haplotypes. This study updates data on hemoglobin haplotypes in Côte d'Ivoire amongst individuals living in Abidjan and experimenting mild malaria. During this work, women represented the highest proportion of people attending dispensaries. This is frequently observed as men use to practice self-treatment so they rarely visit dispensaries. Our study indicated a prevalence of 13% of sickle cell trait (3% of SCD) in the population analyzed. Previous studies conducted by Tossea et al. [18] in the same area reported a similar prevalence. This concordance could be due to the design of the two (02) studies. Indeed, these studies were carried out in individuals with middle malaria in Abidjan.
The Benin haplotype was the most prevalent followed by the Bantu one, which can be attributable respectively to ethnic origin of the population in Abidjan, and the high level of migration from central Africa to Ivory Coast. Arab-Indian haplotype was not observed despite migration of populations across the Sahel (Peul and Toucouleur ethnics). A small prevalence of Senegal and Cameroon haplotypes was observed. These different prevalence are in accordance with the geographical distribution of the different populations [5, 6].
Similar to the studies of several authors who reported 5–10% of atypical haplotypes [9, 19,20,21], we found 10% of atypical haplotypes in the population of Abidjan, mostly associated with the Benin haplotype. Due to the fact that the Benin haplotype is associated with a more severe form of expression of SCD and considering the high prevalence of atypical haplotypes, the relationship between these haplotypes and the clinical pattern of sickle cell disease should be investigate further.
Overall a high proportion of heterozygous genotype (61%) was found in Abidjan. That differs from the studies conducted by Doupa et al. (32%) [17]. This difference could be due to their selection of patients harboring SCD and to the limitation of that study to only a single restriction site.
The emergence of these atypics haplotypes and the high proportion of heterozygous haplotypes could support a high level of mixed populations. Indeed, Abidjan is one of the major city in West Africa, with a cosmopolite population. In addition, the important mixing of populations would be a factor in the development of genetic phenomena such as chromosomal recombination’s between haplotype.
Different atypical haplotypes observed show strong similarities with the Benin and Bantu haplotypes. Several others authors [19, 22, 23] obtained similar results relative to atypical haplotypes. The high proportion of atypical haplotype and its similarity with the Benin haplotype could be explained by selection pressure. Indeed, the association of the atypical haplotypes with the more severe Benin haplotype may lead to a more moderate expressive expression of sickle cell disease. More insight studies need to be conducted to explore such associations and their clinic expressions.
Conclusion
In this preliminary study, we note a high prevalence of atypical and heterozygous haplotype. Benin haplotype that is associated with severity of SCD was most predominant in our studied population. Further studies involving a large number of SCD participants could help to estimate an accurate prevalence of hemoglobin haplotypes in Côte d’Ivoire.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- SCD:
-
Sickle cell disease
- RE:
-
Restriction enzyme
- PCR:
-
Polymerase chain reaction
References
WHO. Sickle Cell Disease | Regional Office for Africa [Internet]. [cited 2020 Nov 29]. Available from: https://www.afro.who.int/fr/node/596.
Délicat-Loembet L, et al. Prevalence of the sickle cell trait in Gabon: a nationwide study. Infect Genet Evol. 2014;25:52–6.
SIHIO-TS. Société Ivoirienne d ’ Hématologie-Immunologie Oncologie-Transfusion sanguine. 2018.
Assemblée mondiale de la Santé 59. Drépanocytose : rapport du secrétariat [Internet]. Available from: http://www.who.int/iris/handle/10665/21941#sthash.Rea4mfwr.dpuf 2006.
Shriner D, Rotimi CN. Whole-genome-sequence-based haplotypes reveal single origin of the sickle allele during the holocene wet phase. Am J Human Genet. 2018;102(4):547–56. https://doi.org/10.1016/j.ajhg.2018.02.003.
Pagnier J, Mears JG, Dunda-Belkhodja O, Schaefer-Rego KE, Beldjord C, Nagel RL, et al. Evidence for the multicentric origin of the sickle cell hemoglobin gene in Africa. Proc Natl Acad Sci. 1984;81(6):1771–3. https://doi.org/10.1073/pnas.81.6.1771.
Abou-Elew HH, Youssry I, Hefny S, Hashem RH, Fouad N, Zayed RA. βS globin gene haplotype and the stroke risk among Egyptian children with sickle cell disease. Hematology. 2018;23(6):362–7.
da Silva MAL, Friedrisch JR, Bittar CM, Urnau M, Merzoni J, Valim VS, et al. <i>ß</i>-globin gene cluster haplotypes and clinical severity in sickle cell anemia patients in southern Brazil. Open J Blood Dis. 2014;04(02):16–23. https://doi.org/10.4236/ojbd.2014.42003.
Rolim A, Martins L, Siebra M. B-globin gene cluster haplotypes in a cohort of 221 children with sickle cell anemia or sb0-thalassemia and their association with clinical and hematological features. Acta Haematol. 2010;124:162–70.
Steinberg MH. Predicting clinical severity in sickle cell anaemia. Br J Haematol. 2005;129(4):465–81.
Zago MA, Figueiredo MS, Ogo SH. Bantu βs cluster haplotype predominates among Brazilian Blacks. Am J Phys Anthropol. 1992;88(3):295–8. https://doi.org/10.1002/ajpa.1330880304.
Labie D, Elion J. Modulation polygénique des maladies monogéniques : L’exemple de la drépanocytose. Medecine/Sciences. 1996;12(3):341–9.
Laurentino MR, Maia Filho PA, Barbosa MC, Bandeira IC, Rocha LB, Gonçalves RP. Influence of βS-globin haplotypes hydroxyurea on tumor necrosis factor-alpha levels in sickle cell anemia. Rev Bras de Hematol e Hemoter. 2014;36(2):121–5. https://doi.org/10.5581/1516-8484.20140028.
Simonnet C, Elanga N, Joly P, Vaz T, Nacher M. Genetic modulators of sickle cell disease in French Guiana: markers of the slave trade. Am J Human Biol. 2016;28(6):811–6. https://doi.org/10.1002/ajhb.22871.
Sutton M, Bouhassira EE, Nagel RL. Polymerase chain reaction amplification applied to the determination of β-like globin gene cluster haplotypes. Am J Hematol. 1989;32(1):66–9. https://doi.org/10.1002/ajh.2830320113.
Joly P, Lacan P, Garcia C, Delasaux A, Francina A. Rapid and reliable β-globin gene cluster haplotyping of sickle cell disease patients by FRET Light Cycler and HRM assays. Clin Chim Acta. 2011;412(13–14):1257–61. https://doi.org/10.1016/j.cca.2011.03.025.
Doupa D, Djité M, Kandji PM, Makalou D, Thiam S, Boye O, et al. Polymorphism of the beta gene in homozygous sickle cell patients in senegal and its influence on the main complications of the disease. Adv Biochem. 2018;6(3):19–25.
Tossea SK, Adji EG, Coulibaly B, Ako BA, Coulibaly DN, Joly P, et al. Cross sectional study on prevalence of sickle cell alleles S and C among patients with mild malaria in Ivory Coast. BMC Res Notes. 2018. https://doi.org/10.1186/s13104-018-3296-7.
Zago MA, Silva WA, Dalle B, Gualandro S, Hutz MH, Lapoumeroulie C, et al. Atypical β(S) haplotypes are generated by diverse genetic mechanisms. Am J Hematol. 2000;63(2):79–84.
Cabral CHK, Serafim ÉSSS, de Medeiros WRDB, de Fernandes TAAM, Kimura EM, Costati FF. Determination of βS haplotypes in patients with sickle-cell anemia in the state of Rio Grande do Norte, Brazil. Genet Mol Biol. 2011;34(3):421–4. https://doi.org/10.1590/S1415-47572011005000027.
dos Silva WS, de Klautau-Guimarães MN, Grisolia CK. β-globin haplotypes in normal and hemoglobinopathic individuals from Reconcavo Baiano, State of Bahia, Brazil. Genet Mol Biol. 2010;33(3):411–7. https://doi.org/10.1590/S1415-47572010005000042.
Srinivas R, Dunda O, Krishnamoorthy R, Fabry ME, Georges A, Labie D, et al. Atypical haplotypes linked to the βs gene in Africa are likely to be the product of recombination. Am J Hematol. 1988;29(1):60–2. https://doi.org/10.1002/ajh.2830290117.
Gonçalves I, Périchon B. A novel mosaic Bantu/Benin/Bantu βs haplotype found in several African populations. Human Genet. 1994;94(1):101–3. https://doi.org/10.1007/BF02272853.
Acknowledgements
We would like to thank all the people and institutions that have enabled us to carry out this work.
Funding
This study and Tosséa A. Stéphane Koui were supported by the Rotary International Foundation.
Author information
Authors and Affiliations
Contributions
TASK conducted the laboratory study and wrote the manuscript; AAG, AABA and BC participated in the collection of the blood sampling; AEG participated to the PCR design; AKA ADA realized the laboratory study; BSEG. and OAT participated to the study design and reviewed the manuscript; RJ supervised the study, obtained the ethic clearance and the founds, wrote the protocol and co-wrote the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study is a part of a protocol of survey of sickle cell anemia in Abidjan which received ethical clearance and approval from the National Ethic Committee of Ivory Coast. All the participants gave their informed consent to participate. All methods were performed in accordance with the relevant guidelines and regulations.
Consent for publication
Not Applicable
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Koui, T.A.S., Gnondjui, A.A., Gbessi, A.E. et al. High level of heterozygous haplotype of hemoglobin in Abidjan population with mild malaria. BMC Med Genomics 15, 120 (2022). https://doi.org/10.1186/s12920-022-01263-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12920-022-01263-3