Abstract
Background
Noninvasive prenatal testing (NIPT) to detect fetal aneuploidy using next-generation sequencing on ion semiconductor platforms has become common. There are several sequencers that can generate sufficient DNA reads for NIPT. However, the approval criteria vary among platforms and countries. This can delay the introduction of such devices and systems to clinics. A comparison of the sensitivity and specificity of two different platforms using the same sequencing chemistry could be useful in NIPT for fetal chromosomal aneuploidies. This would improve healthcare authorities’ confidence in decision-making on sequencing-based tests.
Methods
One hundred and one pregnant women who were predicted at high risk of fetal defects using conventional prenatal screening tests, and who underwent definitive diagnosis by full karyotyping, were enrolled from three hospitals in Korea. Most of the pregnant women (69.79 %) received NIPT during weeks 11–13 of gestation and 30.21 % during weeks 14–18. We used Ion Torrent PGM and Proton semi-conductor-based sequencers with 0.3× sequencing coverage depth. The average total reads of 101 samples were approximately 4.5 and 7.6 M for PGM and Proton, respectively. A Burrows-Wheeler Aligner (BWA) algorithm was used for the alignment, and a z-score was used to decide fetal trisomy 21. Interactive dot diagrams from the sequencing data showed minimal z-score values of 2.07 and 2.10 to discriminate negative versus positive cases of fetal trisomy 21 for the two different sequencing systems.
Results
Our z-score-based discrimination method resulted in 100 % positive and negative prediction values for both ion semiconductor PGM and Proton sequencers, regardless of their sequencing chip and chemistry differences. Both platforms performed well at an early stage (11–13 weeks of gestation) compared with previous studies.
Conclusions
These results suggested that, using two different sequencers, NIPT to detect fetal trisomy 21 in early pregnancy is accurate and platform-independent. The data suggested that the amount of sequencing and the application of common, simple, and robust statistical analyses are more important than sequencing chemistry and platform types. This result has practical implications in countries where PGM is approved for NIPT but the Proton system is not.
Similar content being viewed by others
Background
Recently, early stage prenatal screening to detect fetal aneuploidy has become common for pregnant women [1, 2]. Women over the age of 35 have an increased risk of giving birth to an abnormal baby; hence, accurate prediction-based tests for fetuses are required. Several prenatal screening methods are in use. Common first-trimester screening comprises a combination of ultrasound and maternal serum markers [3]. Women at high risk for fetal chromosome abnormalities have the option to undergo invasive prenatal diagnostic tests such as chorionic villus sampling (CVS) at 10–13 weeks gestational age or amniocentesis at 15–18 weeks gestational age [4, 5]. However, these tests are reported to be associated with iatrogenic pregnancy loss [6].
Decades ago, researchers discovered that cancer DNA could be detected as both circulating tumor cells and cell-free DNA (cfDNA) in human blood. Using this observation, researchers proposed that fetal DNA could be detected using molecular assays and cell-free fetal DNA (cffDNA) was indeed detected in maternal blood [7]. Today, women can choose noninvasive prenatal testing (NIPT) of cffDNA [8]. CffDNA is generally produced from apoptotic trophoblasts in the placenta [7] during pregnancy, and the amount of cffDNA increases with gestational age. During weeks 10–22 of gestation, approximately 10 % of free DNA in the mother’s plasma is estimated to be cffDNA. There is a very high level of variance in the fraction and amount of cffDNA among individuals [9]. Therefore, applying molecular testing requires an extremely accurate detection approach or a massive amount of data to overcome this detection difficulty. Our previous work [10] showed that it is possible to detect fetal chromosome abnormalities for pregnant women in weeks 12–21 of gestation by amplifying and producing a large number of DNA fragments for quantitative analyses. The percentage of cffDNA is proportional to gestational age; therefore, it is important to perform the test at the right time. At the early stage of pregnancy, the fraction of fetal DNA is perhaps the most important factor for NIPT, because the common aneuploidies are very difficult to detect for pregnant women in the early weeks of gestation [11] because of the lack of fetal DNA.
To carry out efficient NIPT, it is necessary to understand the limitations and characteristics of cffDNA. For example, cffDNA is normally only around 150 base pairs (bp) [12]. Also, cffDNA has a short half-life of about 16 min [13, 14].
NIPT technologies have been well accepted because of two critical clinical benefits: there is no risk of pregnancy loss and NIPT can be used as an early pregnancy test compared with amniocentesis; however, discordant NIPT data resulting from placental or maternal cell mosaicism requires full karyotyping, which is the gold standard for aneuploidy tests, to confirm positive outputs [15–17].
Nowadays, next-generation sequencing (NGS) is widely used for NIPT [18–24]. Ion Torrent PGM from Life Technologies, a semiconductor-based sequencing platform assessed here for NIPT and compared with its later and larger-capacity version of Ion Torrent Proton, enables a reduced turnaround time of sequencing data to within 2 to 4 h for a clinical sequencing service. A recent study described the outcomes for noninvasive detection of common fetal trisomy 13, 18, and 21 using the ion semiconductor platform, Ion Proton, which produced greater than 98 % sensitivity and specificity [23]. However, there are many different types and versions of sequencers, making it necessary for granting authorities to evaluate the generality and robustness of such sequencers for NIPT.
As far as we know, there has been no direct comparison between PGM and Proton sequencers for NIPT with large sample sizes. Another reason to compare PGM and Proton sequencers is that PGM is faster. The turnaround time for clinical applications is very important, and ion semiconductor sequencers, such as PGM, have been widely accepted because of their simplicity and speed. Prenatal testing using PGM has become feasible for the noninvasive detection of fetal aneuploidy [25]. PGM machines are small and inexpensive; therefore, comparing the benefits and overall accuracy of both PGM and Proton in terms of data produced could be important clinically for doctors who would like to use NIPT. The experimental cost of the bench-top PGM sequencer is much lower than other common sequencers, although PGM’s general sequencing accuracy is lower. From Ion 314/316/318 chips of PGM, 70 Mbp to 2 Gbp of raw sequencing data can be produced, and 85 % of the reads usually reaches Q20, a common sequencing quality threshold. With the Ion Proton platform, nearly 10 Gbp of raw sequencing data are produced with approximately 75 % of them reaching Q20. This amount is sufficient to determine the quantitative variation caused by chromosomal abnormality. A recent study confirmed that high-throughput ion semiconductor sequencing was feasible in noninvasive prenatal testing of fetal aneuploidies [10, 23]. In that study, only eight maternal plasma DNA samples were used, comprising four normal pregnancies and four with trisomy 21 fetuses, which were sequenced on Ion Torrent 314/316/318/PI chips [26]. Separately, using different samples, Ion Proton sequencer-based results have also demonstrated successfully that ion semiconductor sequencing is suitable for NIPT [10, 23].
Here, we compared the Ion Torrent PGM and Proton platforms for NIPT for fetal trisomy 21 directly using PGM and Proton simultaneously for the same set of samples to provide some general applicability of ion semiconductor-based sequencers. We were also interested in demonstrating whether any sequencers could discriminate fetal aneuploidy from normal chromosomes in blood, even if the fetal DNA fraction is not sufficient for NIPT. In doing so, we tried to detect fetal trisomy 21 for the pregnant women, most of whom (69.79 %) were at weeks 11 to 13 of gestation.
Methods
Study subjects
From December 2014 to April 2015, 101 pregnant women aged between 25 and 42 years (Table 1) were enrolled under an Institutional Review Board protocol in three hospitals (Mirae & Heemang, Namujungwon, and GN in Korea) after high-risk group screening. Sixty-seven of them (69.79 %) were at weeks 11–13 of gestation, and 29 (30.21 %) were at weeks 14–18 of gestation. Participants underwent invasive diagnostic testing (amniocentesis) for fetal karyotyping, the results of which were blinded. Before amniocentesis, they agreed to participate in this study, donated their blood samples, and provided written informed consent.
We used the outcomes of the standard prenatal aneuploidy screening with individual risk scores and interpretations generated by accredited clinical laboratories to identify the group at high risk of fetal defects. First-trimester serum markers included pregnancy-associated plasma protein A (PAPP-A) and free beta subunit or total human chorionic gonadotropin (hCG). A low level of PAPP-A and high hCG might indicate Down syndrome. First-trimester serum markers were used in combination with sonographic measurement of fetal nuchal translucency to classify the women into high- or low-risk groups. The second-trimester serum test, termed quadruple screening, was used alone to evaluate and define aneuploidy risk. Chromosomal abnormality was tested with cultured fetal cells from amniotic fluid, as described by Barch et al. [27]. The result of cytogenetic analysis on all 101 pregnant women indicated that 96 (95.0 %) were chromosomally normal, and five (5.0 %) had trisomy 21.
CfDNA preparation and massively parallel short read sequencing
More than 10 mL of peripheral blood was collected and stored in a BCT™ tube (Streck, Omaha, NE, USA). The blood sample was centrifuged at 1200 × g for 15 min at 4 °C. The plasma portion was transferred to microcentrifuge tubes and centrifuged again at 16,000 × g for 10 min at 4 °C. One mL of plasma was used to extract cfDNA, using a QIAamp Circulating Nucleic Acid Kit (Qiagen, Netherland). The end-repair of the plasma cfDNA was performed using T4 DNA polymerase, Klenow DNA polymerase and T4 polymerase kinase. DNA libraries for the Ion PGM and Proton sequencing systems were prepared according to the protocol provided by the manufacturer (Life Technologies, SD, USA). PGM 318 and Proton PI Chip Kit version 2.0 were used to produce an average of 0.3× sequencing coverage depth per nucleotide. Barcode Indexing was used in both PGM and Proton chips. The index served as a token to differentiate each sample from the multiplexed sample mixtures.
Data analysis
DNA fragments with different lengths derived from the Ion Torrent Suite software were trimmed from the 3' end using a sequencing quality value of >15 and filtered by read length (<50 bp) and GC contents (35–45 %). The Picard program (http://broadinstitute.github.io/picard/) was used to remove duplicate DNA reads. The sequence fragments from each sample were then mapped to the human reference genome sequence (hg19). We evaluated BWA [28], Bowtie [29], and SOAP2 [30] mapping software and chose BWA to acquire the final mapping results. Every chromosome was divided into segments with a bin size of 300 kb to calculate the z-scores to determine trisomy 21. For all 101 samples, we calculated the z-score for each chromosome of each sample to detect the aneuploidy with mapped reads, as well as the average mapped reads and standard deviation (SD) of 96 euploid samples. The z-score of case 1 for chr21, for example, was calculated as follows: z-scorechr21_case1 = (mapped reads of chr21case1 – mean mapped reads of chr21euploid group)/(SD for mean mapped reads of chr21euploid group). The minimal z-scores to determine negative versus positive cases of trisomy were > 2.07 and > 2.10 for fetal trisomy 21 for PGM and Proton systems, respectively. We used Student’s t-test to evaluate the statistical significance of the comparison between the euploid and T21 groups, and a value < 0.05 was considered statistically significant.
Results
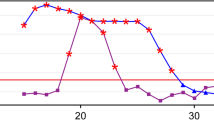
By comparing the sequencing results, we found that the sequencing qualities of both platforms were slightly different, although they are very similar sequencers from the same company. The average total reads of the 101 samples were approximately 4.5 and 7.6 M for PGM and Proton, respectively. For the 318 chip of the PGM sequencer, the average read mapped ratio was higher with a lower SD, the mean read length was longer with a higher SD and the Phred quality score was higher with a higher SD. The Proton PI chip had a better correlation coefficient between the chromosome length and the total reads of the corresponding chromosome. However, we observed that the sequencing quality differences between both platforms did not affect the final z-score results, indicating that the number of DNA reads is more important than individual sequence fragment quality. Interactive dot diagrams for fetal trisomy 21 for the PGM and Proton systems showed the smallest z-score values of 100 % positive predictive value (PPV) and negative predictive value (NPV) (Fig. 1). Figure 2 shows a comparison for an identical sample sequenced by PGM and Proton platforms. The z-scores of the negative samples showed almost the same trends between the platforms, while those of the positive samples showed the same trends. For PGM, the smallest z-score value of 2.07 showed a 100 % PPV and NPV. The minimal z-score of 2.10 was used to classify negative versus positive cases for the Proton system. Table 2 shows the PPVs and NPVs of the NIPT outcomes for fetal trisomy 21 for PGM and Proton, respectively. For both PGM and Proton, the PPV (95 % CI: 47.8–100.0 %) and NPV (95 % CI: 96.2–100.0 %) were 100 %.
Discussion
We compared the PGM with Proton ion semiconductor systems by performing NIPT using cfDNA in a high-risk population. Comparison of the PGM 318 and Proton PI chips was performed with five different parameters to measure their sequencing quality, which revealed sequencer-specific differences (Table 3). However, the two different platforms showed the same accuracy (100 %) using the same set of samples. Our results suggested that prenatal prediction of Down syndrome could be performed equally well by both semiconductor-based sequencing platforms. In addition, we found that early fetal aneuploidy detection (weeks 11–13 of pregnancy) is possible, in addition to detection in the late stage of pregnancy.
Previous studies detected no quality differences between Ion Torrent sequencer and the nucleotide synthesis-based Illumina sequencers by comparing PGM data vs. HiSeq2000- and MiSeq-derived data, although the error rate of PGM data was relatively higher than those of the HiSeq2000 and MiSeq data [31, 32]. Chen et al. [33] evaluated the performances of Proton and MiSeq systems for extremely low-coverage sequencing, and showed that both sequencers detected aneuploidies correctly. Wang et al. concluded that the data quality of Ion Torrent PGM was generally better than that of the Proton system [26]. However, they showed that both PGM- and Proton-based semiconductor high-throughput sequencing was feasible in the noninvasive prenatal testing of fetal aneuploidies [26], although it was carried out with a very small number of samples. In our previous study, we showed that the detection of fetal T18 and T21 could be carried out using the Ion Torrent Proton system [10]. A large-scale clinical study by Liao et al. also showed that NIPT using an Ion Proton sequencer could be successful [23]. In addition, the Ion Proton system can generate about 80 million raw reads in 3–4 h, allowing chromosomal aneuploidy detection in 2 working days. Hence, it could be suitable for operations that require fast and accurate turnaround times [33].
Conventional prenatal screening is not perfect and its detection accuracy for chromosomal aneuploidy is below 100 %. Screens using maternal serum markers and ultrasound have been approved, but have lower accuracy. Henry et al. [34] analyzed Down syndrome births after routine noninvasive screening, based on conventional, non-sequencing tests, which have mostly replaced age-related invasive processes. They found that despite the increase in prenatal screening, newborn children with Down syndrome increased in women over the age of 35 years, because the mothers believed that a single blood test would be sufficient to detect trisomy 21.
A positive NIPT result should include a follow-up test with an invasive prenatal method to confirm the fetal chromosomal aneuploidies. Accurate detection of common chromosomal aneuploidies, particularly T18 and T21, has been consistently reported in previous works of NIPT using cfDNA [18–23]. The current price of a plasma cfDNA test is $800–2000 in the US and $500–1500 in some other countries [8]. Two previous studies evaluated the cost of a cfDNA test in women with positive prevalent screening outcomes and concluded that the use of the cfDNA test was associated with a net price reduction compared with conventional CVS or amniocentesis [35, 36]. One limitation of our current study is that it could not detect additional positive cases for other common chromosomal aneuploidies, such as T18 and T13.
In terms of the time to perform NIPT, a previous study [10] reported that for high sensitivity and specificity, the samples should be collected during weeks 14–21 of gestation. It is advantageous to find a chromosomal abnormality at an early stage of pregnancy; therefore, it is crucial to investigate whether a similar accuracy could be achieved in early pregnancy to expand the clinical utility of NIPT. Our current results indicated that both semiconductor-based platforms are sufficiently sensitive and effective for pregnant women, most of which were at 11 to 13 weeks of gestation.
Although both the PGM and Proton platforms yielded similar results for NIPT, using the minimal z-scores thresholds identified here for classification cannot be a standard measure, because there is usually a grey zone where the classification is not certain and further investigation is required. Therefore, a larger sample size is required to confirm the reliability and validity of our results.
Conclusions
We showed that fetal trisomy 21 could be detected successfully by two different ion semiconductor sequencers (Ion Torrent PGM and Proton) and confirmed that both Ion chips are suitable for cfDNA screening for pregnant women at an early stage. In Korea, PGM is approved as a medical instrument for cfDNA testing, while the Proton awaits approval. Therefore, our investigation provided evidence of PGM’s applicability to public clinical tests. As PGM has been used for NIPT for some years, these results could be used in other countries where NIPT is provided to pregnant women.
Availability of data and materials
The information supporting the conclusions of this article is included within the article.
Abbreviations
- Bp:
-
base pairs
- cfDNA:
-
cell-free DNA
- cffDNA:
-
cell-free fetal DNA
- CVS:
-
chrorionic villus sampling
- hCG:
-
human chorionic gonadotropin
- NGS:
-
next-generation sequencing
- NIPT:
-
non-invasive prenatal testing
- NPV:
-
negative predictive value
- PPV:
-
positive predictive value
- SD:
-
standard deviation
References
Morgan S, Delbarre A, Ward P. Impact of introducing a national policy for prenatal Down syndrome screening on the diagnostic invasive procedure rate in England. Ultrasound Obstet Gynecol. 2013;41(5):526–9.
ACOG Practice Bulletin No. 77. screening for fetal chromosomal abnormalities. Obstet Gynecol. 2007; 109(1):217–227.
Nicolaides KH. Screening for fetal aneuploidies at 11 to 13 weeks. Prenat Diagn. 2011;31(1):7–15.
Fortuny A, Borrell A, Soler A, Casals E, Costa D, Carrio A, Puerto B, Seres A, Cararach J, Delgado R. Chorionic villus sampling by biopsy forceps. Results of 1580 procedures from a single centre. Prenat Diagn. 1995;15(6):541–50.
Crandall BF, Kulch P, Tabsh K. Risk assessment of amniocentesis between 11 and 15 weeks: comparison to later amniocentesis controls. Prenat Diagn. 1994;14(10):913–9.
Tabor A, Alfirevic Z. Update on procedure-related risks for prenatal diagnosis techniques. Fetal Diagn Ther. 2010;27(1):1–7.
Lo YM, Corbetta N, Chamberlain PF, Rai V, Sargent IL, Redman CW, Wainscoat JS. Presence of fetal DNA in maternal plasma and serum. Lancet. 1997;350(9076):485–7.
Benn P, Cuckle H, Pergament E. Non-invasive prenatal testing for aneuploidy: current status and future prospects. Ultrasound Obstet Gynecol. 2013;42(1):15–33.
Norton ME, Brar H, Weiss J, Karimi A, Laurent LC, Caughey AB, Rodriguez MH, Williams J 3rd, Mitchell ME, Adair CD, et al. Non-Invasive Chromosomal Evaluation (NICE) Study: results of a multicenter prospective cohort study for detection of fetal trisomy 21 and trisomy 18. Am J Obstet Gynecol. 2012;207(2):137 e131-138.
Jeon YJ, Zhou Y, Li Y, Guo Q, Chen J, Quan S, Zhang A, Zheng H, Zhu X, Lin J, et al. The feasibility study of non-invasive fetal trisomy 18 and 21 detection with semiconductor sequencing platform. PLoS One. 2014;9(10):e110240.
Wang E, Batey A, Struble C, Musci T, Song K, Oliphant A. Gestational age and maternal weight effects on fetal cell-free DNA in maternal plasma. Prenat Diagn. 2013;33(7):662–6.
Chan KC, Zhang J, Hui AB, Wong N, Lau TK, Leung TN, Lo KW, Huang DW, Lo YM. Size distributions of maternal and fetal DNA in maternal plasma. Clin Chem. 2004;50(1):88–92.
Lo YM, Zhang J, Leung TN, Lau TK, Chang AM, Hjelm NM. Rapid clearance of fetal DNA from maternal plasma. Am J Hum Genet. 1999;64(1):218–24.
Smid M, Galbiati S, Vassallo A, Gambini D, Ferrari A, Viora E, Pagliano M, Restagno G, Ferrari M, Cremonesi L. No evidence of fetal DNA persistence in maternal plasma after pregnancy. Hum Genet. 2003;112(5–6):617–8.
Grati FR, Malvestiti F, Ferreira JC, Bajaj K, Gaetani E, Agrati C, Grimi B, Dulcetti F, Ruggeri AM, De Toffol S, et al. Fetoplacental mosaicism: potential implications for false-positive and false-negative noninvasive prenatal screening results. Genet Med. 2014;16(8):620–4.
McNamara CJ, Limone LA, Westover T, Miller RC. Maternal source of false-positive fetal sex chromosome aneuploidy in noninvasive prenatal testing. Obstet Gynecol. 2015;125(2):390–2.
Wang Y, Chen Y, Tian F, Zhang J, Song Z, Wu Y, Han X, Hu W, Ma D, Cram D, et al. Maternal mosaicism is a significant contributor to discordant sex chromosomal aneuploidies associated with noninvasive prenatal testing. Clin Chem. 2014;60(1):251–9.
Bianchi DW, Parker RL, Wentworth J, Madankumar R, Saffer C, Das AF, Craig JA, Chudova DI, Devers PL, Jones KW, et al. DNA sequencing versus standard prenatal aneuploidy screening. N Engl J Med. 2014;370(9):799–808.
Sparks AB, Struble CA, Wang ET, Song K, Oliphant A. Noninvasive prenatal detection and selective analysis of cell-free DNA obtained from maternal blood: evaluation for trisomy 21 and trisomy 18. Am J Obstet Gynecol. 2012;206(4):319. e311-319.
Lau TK, Cheung SW, Lo PS, Pursley AN, Chan MK, Jiang F, Zhang H, Wang W, Jong LF, Yuen OK, et al. Non-invasive prenatal testing for fetal chromosomal abnormalities by low-coverage whole-genome sequencing of maternal plasma DNA: review of 1982 consecutive cases in a single center. Ultrasound Obstet Gynecol. 2014;43(3):254–64.
Ehrich M, Deciu C, Zwiefelhofer T, Tynan JA, Cagasan L, Tim R, Lu V, McCullough R, McCarthy E, Nygren AO, et al. Noninvasive detection of fetal trisomy 21 by sequencing of DNA in maternal blood: a study in a clinical setting. Am J Obstet Gynecol. 2011;204(3):205. e201-211.
Ashoor G, Syngelaki A, Wagner M, Birdir C, Nicolaides KH. Chromosome-selective sequencing of maternal plasma cell-free DNA for first-trimester detection of trisomy 21 and trisomy 18. Am J Obstet Gynecol. 2012;206(4):322. e321-325.
Liao C, Yin AH, Peng CF, Fu F, Yang JX, Li R, Chen YY, Luo DH, Zhang YL, Ou YM, et al. Noninvasive prenatal diagnosis of common aneuploidies by semiconductor sequencing. Proc Natl Acad Sci U S A. 2014;111(20):7415–20.
Vrachnis N, Vlachadis N, Creatsas G. DNA sequencing versus standard prenatal aneuploidy screening. N Engl J Med. 2014;371(6):578.
Yuan Y, Jiang F, Hua S, Du B, Hao Y, Ye L, Liu J, Feng K, Huang X, Yi X, et al. Feasibility study of semiconductor sequencing for noninvasive prenatal detection of fetal aneuploidy. Clin Chem. 2013;59(5):846–9.
Wang Y, Wen Z, Shen J, Cheng W, Li J, Qin X, Ma D, Shi Y. Comparison of the performance of Ion Torrent chips in noninvasive prenatal trisomy detection. J Hum Genet. 2014;59(7):393–6.
Barch MJKT, Spurbeck JL. The AGT cytogenetics laboratory manual. 3rd ed. New York: Lippincott-Raven; 1997.
Li H, Durbin R. Fast and accurate short read alignment with Burrows-Wheeler transform. Bioinformatics. 2009;25(14):1754–60.
Langmead B, Trapnell C, Pop M, Salzberg SL. Ultrafast and memory-efficient alignment of short DNA sequences to the human genome. Genome Biol. 2009;10(3):R25.
Li R, Yu C, Li Y, Lam TW, Yiu SM, Kristiansen K, Wang J. SOAP2: an improved ultrafast tool for short read alignment. Bioinformatics. 2009;25(15):1966–7.
Quail MA, Smith M, Coupland P, Otto TD, Harris SR, Connor TR, Bertoni A, Swerdlow HP, Gu Y. A tale of three next generation sequencing platforms: comparison of Ion Torrent, Pacific Biosciences and Illumina MiSeq sequencers. BMC Genomics. 2012;13:341.
Boland JF, Chung CC, Roberson D, Mitchell J, Zhang X, Im KM, He J, Chanock SJ, Yeager M, Dean M. The new sequencer on the block: comparison of Life Technology’s Proton sequencer to an Illumina HiSeq for whole-exome sequencing. Hum Genet. 2013;132(10):1153–63.
Chen S, Li S, Xie W, Li X, Zhang C, Jiang H, Zheng J, Pan X, Zheng H, Liu JS, et al. Performance comparison between rapid sequencing platforms for ultra-low coverage sequencing strategy. PLoS One. 2014;9(3):e92192.
Henry GP, Britt DW, Evans MI. Screening advances and diagnostic choice: the problem of residual risk. Fetal Diagn Ther. 2008;23(4):308–15.
Palomaki GE, Kloza EM, Lambert-Messerlian GM, Haddow JE, Neveux LM, Ehrich M, van den Boom D, Bombard AT, Deciu C, Grody WW, et al. DNA sequencing of maternal plasma to detect Down syndrome: an international clinical validation study. Genet Med. 2011;13(11):913–20.
Song K, Musci TJ, Caughey AB. Clinical utility and cost of non-invasive prenatal testing with cfDNA analysis in high-risk women based on a US population. J Matern Fetal Neonatal Med. 2013;26(12):1180–5.
Acknowledgements
We thank MyungJun Jeong and Kyungtae Min for facilitating and participating in the experiments, and assisting the manuscript preparation. We thank Maryana Bhak for editing the manuscript.
Funding
This work was supported by GenomeCare internal research funding. JB was mainly supported by the 2014 Research Fund (1.140113.01) of UNIST (Ulsan National Institute of Science & Technology). JB is partly supported by The Genome Research Foundation, and Geromics internal research funding. Ion Proton platform is supported by Creative Dasan LINC-Dankook University.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Competing interests
We declare the following interests: co-author Sunshin Kim is employed by GenomeCare. Co-authors Hwanjong Kwak, Sunghoon Park, and Hee Jae Joo are employed by TheragenEtex Bio Institute. Co-author Hongliang Chen is employed by Xiamen Vangenes BioTech. Co-author Byung Chul Kim is employed by Clinomics Inc. and Jong Bhak is employed by TGI, UNIST and Geromics Inc.
Authors’ contributions
Conceived and designed the experiments: SK, BK and JB. Performed the experiments: HK and SP. Analyzed the data SK, SL, JK, MK, HC, SP, HLC and HJJ. Contributed reagents/materials/analysis tools: HJ, SH, SL, JK, MK, HC, HLC, KH, HK and HJJ. Contributed to the writing of the manuscript: SK, HJ, SH, KH, BK and JB. All authors read and approved the final manuscript.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Kim, S., Jung, H., Han, S.H. et al. Comparison of two high-throughput semiconductor chip sequencing platforms in noninvasive prenatal testing for Down syndrome in early pregnancy. BMC Med Genomics 9, 22 (2016). https://doi.org/10.1186/s12920-016-0182-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12920-016-0182-9