Abstract
Background
Aromatase inhibitors improve male fertility by modifying the hormonal control of spermatogenesis. The present study aimed to investigate the effects of oral administration of letrozole on testosterone and estradiol concentrations and their ratios in blood serum, seminal plasma, prostatic fluid, sperm quality in fresh semen, and prostate gland dimensions. Seven adult male intact mixed-breed dogs were selected. The animals received letrozole (72 µg/kg, PO) daily for four weeks. Blood samplings and semen collections were carried out on days 0 (control), 14 (treatment), 28 (treatment), and 42 (post-treatment).
Results
Our results showed that letrozole administration resulted in a 4.3 fold significant increase in serum, seminal plasma, and prostatic fluid testosterone levels after 14 days. This remained high until the end of the study. Serum and prostatic fluid estradiol levels did not change significantly over the study period. However, the seminal plasma estradiol level showed a significant increase on day 14. The estradiol: testosterone ratio was significantly reduced on day 14 in serum, seminal plasma, and prostatic fluid samples. Letrozole significantly improved the ejaculated spermatozoa viability and concentration after 28 days of oral administration. However, the sperm plasma membrane functional integrity and kinematic parameters were not significantly affected by the treatment. Transabdominal ultrasound examination revealed a significant increase in the height, width, and volume of the prostate gland after 28 days of treatment.
Conclusions
According to the present research, oral administration of letrozole for 28 days affects local and systemic sex hormone balance leading to an improvement of the ejaculated canine spermatozoa viability and concentration concurrent with an increase in the prostate gland dimensions.
Similar content being viewed by others
Background
Spermatogenesis is closely regulated through paracrine/endocrine mechanisms [1, 2]. Secretion of follicle-stimulating hormone (FSH) and luteinizing hormone (LH) from the pituitary stimulates the production of testosterone, dihydrotestosterone, and finally estradiol from Leydig and Sertoli cells. Both androgens and estradiol play crucial roles in maintaining normal spermatogenesis [3]. A concrete body of evidence shows that both absolute testosterone and estradiol concentrations, as well as the estradiol: testosterone ratio at either systemic or local levels are important determinants of normal spermatogenesis [4]. While estrogens play a role in regulating sperm maturation, motility, differentiation of somatic cells, and proliferation of spermatogonia and Sertoli cells [5], there are dose-dependent inhibitory and stimulatory effects of estradiol on testicular cell function [6]. An excess estrogen concentration may harm testicular function by decreasing the expression of androgen receptors [7]. Estrogen suppresses LH secretion using a negative feedback mechanism on the hypothalamus and pituitary. The suppression of estrogen increases testosterone levels by stimulating LH. Testosterone secretion mainly leads to germ cell differentiation by regulating Sertoli cell function, potentially improving reproductive performance [8].
Estrogen: testosterone ratios are influenced by various factors, especially the aromatase enzymatic complex, which is responsible for converting testosterone to estradiol in ovaries and testicular cells of different species [9]. However, increasing intratesticular estrogen and the resulting elevation of the estrogen: testosterone ratio has the potential to cause infertility in transgenic male mice [10]. Aromatase inhibitors (AIs) prevent the conversion of androgens into estrogens in the absence of high estrogen levels in oligozoospermic/azoospermic men [11]. The efficacy of AIs has been studied for their effects on spermatogenesis and semen quality in rats [12], fish [13], lizards [14], markhoz goats [15, 16], stallions [17], humans [18,19,20], and in dogs [21,22,23]. Letrozole, a reversible AI, is one of the options used to treat human oligospermia and azoospermia [24]. Rezaei et al. (2022) showed that subcutaneous injection of this drug in bucks increased seminiferous tubule diameter, Sertoli cell number, semen volume, and sperm concentration [15]. Consistent with the previous studies, Wang et al. (2018) found that this treatment could promote the proliferation rate of mouse spermatogenesis cell lines [25]. A study on stallion concluded that the early mention medication increases serum testosterone concentrations and decreases serum levels of estradiol and inhibin [17].
Some experimental studies support evidence that testosterone, dihydrotestosterone, and the balance of androgens and estrogen have prominent roles in prostate growth and maturation [26,27,28]. Prostatic hyperplasia and hypertrophy can occur in AI-treated mice. It may be attributed to long-term estrogen deficiency and high concentrations of androgens [29]. Similarly, another study found that letrozole causes an increase in the size of the prostate lobes in rats [30]. It needs to be noted that the etiopathology of prostatic hyperplasia and hypertrophy is different among various species [31].
Some dogs are referred to veterinary clinics due to low semen quality. AIs such as 4-androstene-4-ol-3,17-dione and anastrozole [22, 23] have been used to improve semen quality but the effect of letrozole on canine semen quality, reproductive hormones, and prostatic volume has not been studied. Animal studies have served as the basis for further experimental studies and applications in human subjects [32,33,34]. In this study, our objective was to assess the impact of orally administering of the third generaion type II AI on the semen quality of healthy adult dogs. We assessed the prostatic volume, size, and shape during this treatment by ultrasonography.
Results
Serum testosterone concentration
The testosterone concentration was increased from 11.61 ± 18.54 ng/ml (day 0, control) to a maximum concentration of 61.8 ± 2.11ng/ml on day 42. The serum testosterone concentration increased 4.32 times during the study (Table 1). Testosterone concentrations on days 14, 28, and 42 were significantly increased compared with the pre-treatment (control) testosterone concentration on day 0 (P < 0.01), but no significant differences were found between testosterone concentrations on days 14, 28, and 42. The trend of standard deviation indicated a decrease from the beginning to the end of the study, so some differences in testosterone concentrations were detected between individual dogs at the start of the study (Table 1).
Serum estradiol concentration
The changes in estradiol concentrations were not significantly different between the sampling days (Table 1).
Serum estradiol: testosterone ratios
The serum estradiol: testosterone ratios were significantly decreased during and after treatment compared to before it (P < 0.03; Table 1).
Seminal plasma testosterone concentration
The seminal plasma testosterone concentration was increased from day 0 to day 28 and 42 (P < 0.04), and from day 14 to 42 of sampling (P < 0.001). The concentration of seminal plasma testosterone increased gradually from day 0 (0.14 ± 0.15 ng/ml) to day 42 (26.3 ± 11.42 ng/ml) about 186.85 times (Table 1).
Seminal plasma estradiol concentration
The seminal plasma estradiol concentration significantly increased from day 0 compared to day 14 (P = 0.02). There were no significant differences in estradiol seminal plasma concentrations among other days of sampling (Table 1).
Seminal plasma estradiol: testosterone ratios
The estradiol: testosterone ratios were significantly decreased between day 0 and day 14, 28, and 42 (P < 0.001). This ratio decreased from day 0 to day 42 about 99.39% (Table 1).
Prostatic fluid testosterone concentration
The prostatic fluid testosterone concentration was increased about 151.75 times from day 0 compared with day 42 (P = 0.04; Table 1). There was no significant increase in prostatic fluid testosterone concentration on other days.
Prostatic fluid estradiol concentration
There were no significant differences in prostatic fluid estradiol concentration between different sampling days (Table 1).
Prostatic fluid estradiol: testosterone ratios
The decrease in prostatic fluid estradiol: testosterone ratios was significant between day 0 and days 14 and 28 (P < 0.001). The prostatic fluid estradiol: testosterone ratios decreased significantly decreased by approximately 99.13% between day 0 and day 42 (P < 0.001; see Table 1).
Sperm analysis
Oral letrozole administration for four weeks improved significantly (P < 0.01) the percent of live sperm using eosin-nigrosine staining in the fresh semen. In contrast, the sperm membrane functional integrity (HOST-positive) and abnormal morphology were not affected by the treatment. The sperm concentration increased significantly after 28 days of this treatment in compared to days 0 and 14 (P < 0.02). However, it did not change until the end of treatment period (Table 1). This treatment did not affect the fresh sperm kinematic factors during the current study (P > 0.05; Table 2).
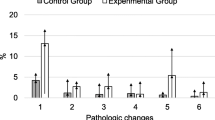
Prostate gland dimensions
The transabdominal ultrasound examination of the prostate gland indicated a significant increase in the prostatic gland height, width, and volume after 28 days of letrozole treatment in compared with days 0 and 14 (P ≤ 0.05, Table 3).
Discussion
Oral letrozole administration (72 µg/kg) for 30 days increased testosterone concentration and decreased estradiol: testosterone ratios in serum, seminal plasma, and prostatic fluid. Furthermore, the viability and concentration of sperm improved following this treatment and the prostate gland volume increased in treated dogs. Testosterone, FSH, and LH concentrations are mainly affected by the circulating estradiol level, as estradiol acts a negative feedback on GnRH. In men, low estradiol levels cause a rapid increase in testosterone, FSH, and LH levels [35,36,37]. The treatment of two azoospermic dogs with high plasma estradiol-17 beta concentration, using AI 4-androstene-4-ol-3,17-dione for 4 weeks, decreased the plasma estradiol concentration. Consequently, plasma testosterone concentration increased, and a small number of sperm were detected in the semen 3–6 weeks after the start of treatment [23].
It has been described that type I estrogen antagonists, such as tamoxifen, inhibit the function of estrogen. These drugs may induce some estrogenic responses [38]. A reduction in prostatic volume, testosterone concentration, and quality of semen was observed when this treatment was used in Beagle dogs [21]. Corrada et al. (2004) also showed the estrogenic impact of this medication on hypothalamic-pituitary levels, resulting in lower plasma FSH and LH levels and, consequently, lower plasma testosterone concentrations [21]. Although several researchers have challenged the effect of this drug, the results of some studies support the idea that AIs can increase spermatogenesis in humans, dogs, and rats [12, 39].
Letrozole has been found to cause parallel estradiol reduction, thereby increasing testosterone and stimulating spermatogenesis [40]. Several studies investigating the effects of this treatment on the quality of semen have demonstrated a positive effect on sperm concentration and motility [20, 40]. Ribeiro et al. (2016) hypothesized that AI therapy has a progressive impact on spermatogenesis and LH concentrations [11]. Other studies have focused on the effects of letrozole and anastrozole on the quality of semen and estradiol: testosterone ratios in infertile men, with the results indicating improved sperm concentration, motility, semen volume, estradiol: testosterone ratios, and serum testosterone [40]. Similarly, Saylam et al. (2011) prescribed this treatment in infertile men, noting significant decreases in estradiol: testosterone ratios and increases in sperm motility and concentration after treatment [41]. Party et al. (2009) reported that, after using letrozole for up to four months in a man with primary infertility, normal spermatogenesis was detected in the testicular biopsy [42]. A study on the effects of this medication in healthy adult male horses further supports the effect of AIs, with researchers concluding that the drug increases serum testosterone concentration and decreases serum levels of estradiol and inhibin in stallions. However, this study showed that the treatment had no effects on sperm production [17].
The reduction in estradiol levels caused by AIs was linked to higher levels of serum FSH and LH, as well as an increase in circulating testosterone levels in elderly men [43]. The main sites where the aromatase substrate, essential for estrogen synthesis, is produced are predominantly Leydig, Sertoli, and germinal cells [43]. Therefore, it is likely that letrozole enhances the process of spermatogenesis and boosts sperm concentration through a potential increase in FSH levels [43]. Rezaei et al., (2020) demonstrated an elevation in the Sertoli cell count within the testes of bucklings injected with letrozole. The stimulation of Sertoli cells by this medication is attributed to various mechanisms including: (i) augmentation of LH-induced testosterone secretion, (ii) direct enhancement of FSH levels, and (iii) suppression of estrogens and/or estrogen receptor blockade [16]. Sertoli cells play a crucial role as the primary recipient cell for FSH and testosterone, creating a conducive setting that supports the development, maturation, and proliferation of germ cells into spermatozoa through physical interaction [44]. While it is widely documented that anastrozole and letrozole effectively inhibit aromatase activity by nearly 100%, the use of these inhibitors in men does not lead to complete suppression of plasma estradiol levels [36, 37, 45].
Gonzalez et al. (2009) investigated the effect of 60-day administration of the AI anastrozole and the antiestrogenic receptor blocker tamoxifen on normal and hyperplastic prostate glands in dogs. Anastrozole decreased prostate volume to a greater exent than tamoxifen in dogs with hyperplastic prostate glands. In normal dogs, libido, testicular consistency and scrotal diameter, semen volume, sperm count, motility, and morphological abnormalities remained unaltered in the anastrozole group throughout the study [22]. AIs are effective in counteracting stromal changes associated with estrogens due to the build-up of androgens, the aromatase substrate. Some developed AIs have been found to influence the epithelial and stromal compartments of canine benign prostatic hyperplasia, decreasing intraprostatic aromatase activity, estradiol levels, and androgenic receptors [45]. The prostate is an androgen-dependent organ, but both animal [46] and human [47] studies suggest that estradiol has an independent effect on the prostate. This is because testosterone is aromatized to estradiol, meaning that some of the trophic effects of testosterone on the prostate might be mediated via its aromatization to estradiol [43]. In a study in older men treated with transdermal testosterone gel, prostate volume significantly increased (despite on-treatment serum testosterone levels being similar in the AI group), suggesting that the trophic effects of testosterone on prostate volume are mediated via its aromatization to estradiol. In contrast, serum prostate specific antigen (PSA) increased significantly (although within the normal range) in both the testosterone and AI groups, suggesting that the increase in PSA is primarily an androgen-driven process [43].
In our study, prostate width, height and volume increased significantly after 28 days treatment of dogs with letrozole. The focal prostatic hyperplasia, as well as the enlargement of the anterior and dorsal prostate lobes, were observed in peripubertal rats following both short-term and long-term treatment with AIs [30]. The equilibrium between androgens and oestrogen plays a crucial role in both the normal function and disorders of the prostate [28]. The manifestation of prostatic hyperplasia resulting from temporary suppression of aromatase in peripubertal animals aligns perfectly with the finding that prolonged lack of estrogen leads to prostatic hyperplasia and enlargement in mature aromatase knockout mice [48].
The present study is the first investigation into the impact of letrozole on canine semen quality and reproductive hormone (testosterone and estradiol) concentrations in serum, semen, and prostate. The results and conclusions of this study are limited by the small number of dogs, the short period devoted to monitoring, the lack of measurement of testicular size and volume, and the lack of FSH and LH assay.
Conclusions
In conclusion, this study has demonstrated the efficacy of letrozole in changing serum, semen, and prostatic fluid testosterone concentrations and estradiol: testosterone ratios. Increasing sperm viability and concentration may have been attributed to the reduction in estradiol: testosterone ratio. Therefore, the potential clinical effects of this treatment in low fertility or infertile dogs should be considered. Further studies are suggested to improve our understanding of the mechanism behind this drug’s efficacy and to evaluate the clinical efficacy of this medication on subfertile and infertile dogs.
Methods
The Iranian animal ethics framework under the supervision of the Iranian Society for the Prevention of Cruelty to Animals and Shiraz University Research Council approved experimental protocols in this study (IACUC no: 4687/63). The European Council Directive (2010/63/EU) recommendations of September 22, 2010, regarding the standards in the protection of animals used for experimental purposes, were also followed.
Animals
Seven adult male intact mixed-breed dogs, aged 3 ± 1 years old and weighting 20 ± 2 kg, were selected and enrolled for this study. General and reproductive examinations were performed using palpation and ultrassonography and healthy animals with fertile reproductive histories were included in the study. The dogs were trained for semen collection and produced normal ejaculates [49]. They were owned and kept by the School of Veterinary Medicine of Shiraz University. All dogs received 300 g/dog/day of commercial dog food (Nutri® dry dog food; Behintash Co. Iran), and they had free access to water. The dogs were adapted to the new condition for two weeks. Anti-parasitic treatment was performed using Panvermic® tablets (praziquantel 50 mg; mebendazole 220 mg; pirantel Pamoate 144 mg; Drag Pharma, Chile). Praziquantel and mebendazole were administered at doses of 5 mg/kg and 22 mg/kg, respectively.
Experimental design
This research was designed as a longitudinal cohort study for 42 days, with the sampling on day 0 considered the control group compared with other days of sampling. Blood and semen samples were collected on days 0 (control), 14, 28 (treatment), and 42 (post-treatment). The dogs received 72 µg/kg of oral letrozole tab (Letrofem 2.5 mg, Iran Hormone, Iran) daily for four weeks from day 1 of the study [50]. The canine dose of this drug was estimated based on the human dose of this drug and the following equation: [Canine allometric coefficient (1.8)×human dose (mg/kg)] [51]. The blood samples were collected from the jugular vein into simple glass tubes at 9 a.m., centrifuged for 10 min at 750 ×g, and the serum samples stored at -20 °C. The semen samples were collected by one operator using manual masturbation into pre-warmed (37 °C) plastic tubes (Falcon, USA). Prostate fluid was collected at the end of the semen collection. The fresh semen centrifuged for 10 min at 600×g and the seminal plasma preserved at -20 °C for further analysis.
Prostate ultrasound
Ultrasound examination of the prostate was performed using an ultrasound machine equipped with a trans-abdominal micro convex probe 3.5–10 MHz (SIUI 900 V, China) before semen collection on days 0, 14, 28, and 42. Prostate volume was calculated by measuring length in the longitudinal section and width and depth in the transverse section of preserved ultrasound images. The volume of the prostate was calculated using the following function: prostate volume (cm3)=[(L×W×D)/2.26] + 1.8 [52]. The expected normal prostate volume of dogs was estimated by their weight and age: Prostate volume=(0.867×BW)+(1.885×age) + 15.88 [53] and compared with the calculated prostate volume using ultrasound exam to confirm that there was no prostatic hyperplasia at the beginning of the study.
Hormone assays
The concentration of estradiol (intra-assay C.V. <9%; sensitivity 8.68 pg/ml; Diametra, Italy) and testosterone (intra-assay C.V. 4.8%; sensitivity 57 pg/ml; Monobind, USA) in serum, seminal plasma, and prostatic fluid were measured using solid-phase sandwich ELISA commercial kits. The ELISA kits were validated for measuring estradiol and testosterone in dog`s serum, seminal plasma, and prostatic fluid samples in the Laboratory of Clinical Pathology, School of Veterinary Medicine, Shiraz University [54].
Fresh semen primary preparation
Upon receipt, all semen samples including three fractions of ejaculation were centrifuged for 10 min at 600 ×g in a pre-warmed (37 °C) laboratory centrifuge equipped with a swing-out rotor [55]. Next, a part of the seminal plasma was removed for hormone measurements so that 2 ml remained above the sperm pellet. The sperm pellet was then gently resuspended in remaining seminal plasma, and the resulting sperm suspension was used for the downstream procedures as follows:
Kinematic parameters
Sperm motion parameters were objectively evaluated using Computer-Assisted Sperm Analysis (CASA) software (Houshmand Fanavar, Tehran, Iran). A 10 µL sample of sperm was loaded onto a pre-warmed (37 °C) sperm chamber (Sperm meter™, India) with a chamber depth of 10 micrometers. Immediately, the sperm motion parameters were analyzed under a bright-field light microscope (Pro-Way, China). A minimum of 400 cells in 4 random microscopic fields (×100 magnification) were included in the analysis. A sperm cell was classified as immotile when the Velocity Average Path (VAP) value was less than 10 mm/second, and the CASA frame rate was set to 50 Hz.
Sperm concentration
The sperm concentration was calculated using the standard hematology hemocytometer method. A sample of sperm suspension was diluted at 1:100 (dilution factor, df) in double distilled water, loaded into a hemocytometer (Neubauer, Germany) chamber, and subjected to sperm counting for the final cell concentration calculations in each mL of the sample. The total number of sperm (n) was counted in five squares, with at least 200 sperm for normal semen samples. Then, the number of sperm in each milliliter was calculated using the following formula: n×df×50,000.
Sperm viability and morphology
The eosin-nigrosine supravital staining procedure was used to determine the viability status of sperm cells. The stain and microscopic slide need to be prewarmed (37 °C). Equal volumes (200 µl) of the sperm suspension and stains were mixed on a microscopic slide, smeared after 30 s, and air-dried immediately. At least 200 cells were observed under a bright-field light microscope (Olympus, Japan) with ×1000 magnification in immersion oil. Sperm cells, excluding the eosin stain in the head region, were considered to be membrane-intact and live spermatozoa and sperm cells with a stained head were considered to be membrane disrupted and dead spermatozoa. Also, the sperm with abnormal morphologies in the head, mid-piece, or tail regions were classified as abnormal [56].
Sperm plasma membrane functional integrity
The functional integrity of the sperm was evaluated using a hypo-osmotic swelling test in a hypotonic sucrose solution. A 10 µL sample of sperm was mixed with 90 µL of pre-warmed (37 °C) hypotonic solution and incubated for 30 min at 37 °C. Next, a wet smear was prepared and evaluated under a bright-field light microscope (Olympus, Germany) with ×400 magnification. At least 200 cells were evaluated, and sperm cells with swelling/coiling of the tail were considered to have intact plasma membranes [56].
Statistical analysis
At first, the normal distribution of data was assessed and confirmed using the Kolmogorov–Smirnov test. The treatment effects were then analyzed by a one-way repeated-measures analysis of variance (ANOVA) test. Tukey’s multiple comparison tests were used to compare differences between the sampling days. The analysis was performed using Graphed Prism Version 6 software. To calculate estradiol: testosterone ratios, the raw data of estradiol concentration for each dog was converted from pg/ml to ng/ml, and then the ratios were calculated for each dog on every sampling day. The percentage of changes was calculated using the following function: ((new value - original value) / original value) × 100. P values less than 0.05 were considered significant. Data were expressed as the mean and standard deviation (SD).
Data availability
The data-sets analyzed during the current study are available from the corresponding author on request.
Abbreviations
- AIs:
-
Aromatase Inhibitors
- CASA:
-
Computer-Assisted Sperm Analysis
- FSH:
-
Follicle-Stimulating Hormone
- GnRH:
-
Gonadotropin-Releasing Hormone
- LH:
-
Luteinizing Hormone
- MAD:
-
Mean Angular Displacement
- PSA:
-
Prostate Specific Antigen
- SD:
-
Standard Deviation
References
Fontbonne A. Infertility in male dogs: recent advances. Rev Bras Reprod Anim. 2011;35(2):266–73.
Peters MA, de Rooij DG, Teerds KJ, van Der Gaag I, van Sluijs FJ. Spermatogenesis and testicular tumours in ageing dogs. J Reprod Infertil. 2000;120(2):443–52.
Foote R, Swierstra E, Hunt W. Spermatogenesis in the dog. Anat Rec. 1972;173(3):341–51.
Kato J, Kobayashi T, Villee CA. Effect of clomiphene on the uptake of estradiol by the anterior hypothalamus and hypophysis. Endocrinology. 1968;82(5):1049–52.
Meccariello R, Chianese R, Chioccarelli T, Ciaramella V, Fasano S, Pierantoni R, et al. Intra-testicular signals regulate germ cell progression and production of qualitatively mature spermatozoa in vertebrates. Front Endocrinol. 2014;5:69.
Schulster M, Bernie AM, Ramasamy R. The role of estradiol in male reproductive function. Asian J Androl. 2016;18(3):435.
Kaushik M, Misro M, Sehgal N, Nandan D. Effect of chronic oestrogen administration on androgen receptor expression in reproductive organs and pituitary of adult male rat. Andrologia. 2010;42(3):193–205.
Spitzer M, Huang G, Basaria S, Travison TG, Bhasin S. Risks and benefits of testosterone therapy in older men. Nat Reviews Endocrinol. 2013;9(7):414–24.
Meyer K, Martino-Andrade A, Santos A, Spercoski K, Morais R. Domestic cat testicular aromatase activity as assessed by the tritiated water-release assay. Anim Reprod. 2018;11(4):549–56.
Li X, Nokkala E, Yan W, Streng T, Saarinen N, Wärri A, et al. Altered structure and function of reproductive organs in transgenic male mice overexpressing human aromatase. Endocrinology. 2001;142(6):2435–42.
Ribeiro MA, Gameiro L, Scarano WR, Briton-Jones C, Kapoor A, Rosa MB, et al. Aromatase inhibitors in the treatment of oligozoospermic or azoospermic men: a systematic review of randomized controlled trials. JBRA Assist Reprod. 2016;20(2):82–8.
Walker UJ, Nogues V. Changes induced by treatment with aromatase inhibitors in testicular leydig cells of rats and dogs. Exp Toxicol Pathol. 1994;46(3):211–3.
Shen Z-G, Fan Q-X, Yang W, Zhang Y-L, Wang H-P. Effects of 17α-methyltestosterone and aromatase inhibitor letrozole on sex reversal, gonadal structure, and growth in yellow catfish Pelteobagrus fulvidraco. Biol Bull. 2015;228(2):108–17.
Cardone A, Comitato R, Bellini L, Angelini F. Effects of the aromatase inhibitor fadrozole on plasma sex steroid secretion, spermatogenesis and epididymis morphology in the lizard, Podarcis sicula. Mol Reprod Dev. 2002;63(1):63–70.
Rezaei A, Vaziry A, Farshad A. Letrozole, an aromatase inhibitor, improves seminal parameters and hormonal profile in aged endangered Markhoz bucks. Anim Bioscience. 2022;35(11):1666–74.
Rezaei A, Vaziry A, Farshad A, Farzinpour A, Rostamzadeh J. Effects of letrozole administration on growth and reproductive performance in Markhoz goat bucklings. Theriogenology. 2020;147:183–91.
Stein TA, Ball B, Conley AJ, Bhatnagar A, Roser J. The effects of an aromatase inhibitor (letrozole) on hormone and sperm production in the stallion. Theriogenology. 2002;58(2–4):381–3.
Hero M, Toiviainen-Salo S, Wickman S, Mäkitie O, Dunkel L. Vertebral morphology in aromatase inhibitor–treated males with idiopathic short stature or constitutional delay of puberty. J Bone Min Res. 2010;25(7):1536–43.
Pavlovich CP, King P, Goldstein M, Schlegel PN. Evidence of a treatable endocrinopathy in infertile men. J Urol. 2001;165(3):837–41.
Raman JD, Schlegel PN. Aromatase inhibitors for male infertility. J Urol. 2002;167(2 Part 1):624–9.
Corrada Y, Arias D, Rodrıguez R, Spaini E, Fava F, Gobello C. Effect of tamoxifen citrate on reproductive parameters of male dogs. Theriogenology. 2004;61(7–8):1327–41.
Gonzalez G, Guendulain C, Maffrand C, Gobello C. Comparison of the effect of the aromatase inhibitor, anastrazole, to the antioestrogen, tamoxifen citrate, on canine prostate and semen. Reprod Domest Anim = Zuchthygiene. 2009;44(Suppl 2):316–9.
Kawakami E, Taguchi N, Hirano T, Hori T, Tsutsui T. Therapeutic effect of aromatase inhibitor in two azoospermic dogs with high plasma estradiol-17beta levels. J Veterinary Med Sci. 2003;65(12):1343–5.
Stephens SM, Polotsky AJ, editors. Big enough for an aromatase inhibitor? How adiposity affects male fertility. Seminars in reproductive medicine. Thieme Medical; 2013.
Wang S, Wang S, Li H, Li X, Xie M, Wen J, et al. Effect of aromatase inhibitor letrozole on the proliferation of spermatogonia by regulating the MAPK pathway. Exp Ther Med. 2018;15(6):5269–74.
Härkönen PL, Mäkelä SI. Role of estrogens in development of prostate cancer. J Steroid Biochem Mol Biol. 2004;92(4):297–305.
Prins GS, Huang L, Birch L, Pu Y. The role of estrogens in normal and abnormal development of the prostate gland. Ann N Y Acad Sci. 2006;1089(1):1–13.
McPherson SJ, Ellem SJ, Risbridger GP. Estrogen-regulated development and differentiation of the prostate. Differentiation. 2008;76(6):660–70.
Murata Y, Robertson KM, Jones ME, Simpson ER. Effect of estrogen deficiency in the male: the ArKO mouse model. Mol Cell Endocrinol. 2002;193(1–2):7–12.
Bajpai A, Simm PJ, McPherson SJ, Russo VC, Azar WJ, Wark JD, et al. Peripubertal aromatase inhibition in male rats has adverse long-term effects on bone strength and growth and induces prostatic hyperplasia. J Endocrinol. 2010;207(1):27.
Mahapokai W, van Sluijs FJ, Schalken JA. Models for studying benign prostatic hyperplasia. Prostate Cancer Prostatic Dis. 2000;3(1):28–33.
Hodjati H, Hosseinzadeh A, Farzaneh BA, Johari HG, Ebrahimi N, Tahmasebi K, et al. Inferior Vena Cava Repair using diaphragm in animal model. Ann Vasc Surg. 2020;67:468–73.
Hodjati H, Moosavi SM, Hosseinzadeh A, Anbardar MH, Sherafatmand S, Kazemnia K, et al. Renal revascularization by a pedicled intestinal segment wrapping the kidney: a new method for kidney revascularization. Int Urol Nephrol. 2022;54(2):257–62.
Kazemi K, Hosseinzadeh A, Shahriarirad R, Nikeghbalian S, Kamran H, Hosseinpour P, et al. Comparison of oral Sirolimus, Prednisolone, and combination of both in Experimentally Induced Peritoneal Adhesion. J Surg Res. 2022;276:168–73.
Pitteloud N, Dwyer AA, DeCruz S, Lee H, Boepple PA, Crowley WF Jr, et al. Inhibition of luteinizing hormone secretion by testosterone in men requires aromatization for its pituitary but not its hypothalamic effects: evidence from the tandem study of normal and gonadotropin-releasing hormone-deficient men. J Clin Endocrinol Metab. 2008;93(3):784–91.
T’Sjoen GG, Giagulli VA, Delva H, Crabbe P, De Bacquer D, Kaufman J-M. Comparative assessment in young and elderly men of the gonadotropin response to aromatase inhibition. J Clin Endocrinol Metab. 2005;90(10):5717–22.
Raven G, de Jong FH, Kaufman J-M, de Ronde W. In men, peripheral estradiol levels directly reflect the action of estrogens at the hypothalamo-pituitary level to inhibit gonadotropin secretion. J Clin Endocrinol Metab. 2006;91(9):3324–8.
Gobello C. Dopamine agonists, anti-progestins, anti-androgens, long-term-release GnRH agonists and anti-estrogens in canine reproduction: a review. Theriogenology. 2006;66(6–7):1560–7.
Trunet P, Mueller P, Bhatnagar A, Dickes I, Monnet G, White G. Open dose-finding study of a new potent and selective nonsteroidal aromatase inhibitor, CGS 20 267, in healthy male subjects. J Clin Endocrinol Metab. 1993;77(2):319–23.
Gregoriou O, Bakas P, Grigoriadis C, Creatsa M, Hassiakos D, Creatsas G. Changes in hormonal profile and seminal parameters with use of aromatase inhibitors in management of infertile men with low testosterone to estradiol ratios. Fertil Steril. 2012;98(1):48–51.
Saylam B, Efesoy O, Çayan S. The effect of aromatase inhibitor letrozole on body mass index, serum hormones, and sperm parameters in infertile men. Fertil Steril. 2011;95(2):809–11.
Patry G, Jarvi K, Grober ED, Lo KC. Use of the aromatase inhibitor letrozole to treat male infertility. Fertil Steril. 2009;92(2):829. e1-. e2.
Dias JP, Melvin D, Shardell M, Ferrucci L, Chia CW, Gharib M, et al. Effects of transdermal testosterone gel or an aromatase inhibitor on prostate volume in older men. J Clin Endocrinol Metab. 2016;101(4):1865–71.
Berger T, Conley AJ, Van Klompenberg M, Roser JF, Hovey RC. Increased testicular sertoli cell population induced by an estrogen receptor antagonist. Mol Cell Endocrinol. 2013;366(1):53–8.
Ito K, Fukabori Y, Shibata Y, Suzuki K, Mieda M, Gotanda K, et al. Effects of a new steroidal aromatase inhibitor, TZA-2237, and/or chlormadinone acetate on hormone-induced and spontaneous canine benign prostatic hyperplasia. Eur J Endocrinol. 2000;143(4):543–54.
Rhodes L, Ding VD, Kemp RK, Khan MS, Nakhla AM, Pikounis B, et al. Estradiol causes a dose-dependent stimulation of prostate growth in castrated beagle dogs. Prostate. 2000;44(1):8–18.
Zhang Z, Duan L, Du X, Ma H, Park I, Lee C, et al. The proliferative effect of estradiol on human prostate stromal cells is mediated through activation of ERK. Prostate. 2008;68(5):508–16.
McPherson SJ, Wang H, Jones ME, Pedersen J, Iismaa TP, Wreford N, et al. Elevated androgens and prolactin in aromatase-deficient mice cause enlargement, but not malignancy, of the prostate gland. Endocrinology. 2001;142(6):2458–67.
Mason SJ. An update on male canine infertility. Veterinary Clin North America: Small Anim Pract. 2023;53(5):1063–81.
da Rocha AA, da Cunha IC, Ederli BB, Albernaz AP, Quirino CR. Effect of daily food supplementation with essential fatty acids on canine semen quality. Reprod Domest Anim. 2009;44(Suppl 2):313–5.
Nair AB, Jacob S. A simple practice guide for dose conversion between animals and human. J Basic Clin Pharm. 2016;7(2):27.
Kamolpatana K, Johnston GR, Johnston SD. Determination of canine prostatic volume using transabdominal ultrasonography. Veterinary radiology & ultrasound: the official journal of the American College of Veterinary Radiology and the International Veterinary. Radiol Association. 2000;41(1):73–7.
Sannamwong N, Saengklub N, Sriphuttathachot P, Ponglowhapan S, editors. Formula-derived prostate volume determination of normal healthy intact dogs in comparison to dogs with clinical BPH. 7th International Symposium on Canine and Feline Reproduction Whistler; 2012.
Mogheiseh A, Nazifi S, Gharibnavaz M, Zamani R, Nikahval B, Khanbazi MH. Effects of short-term administration of melatonin before gonadectomy on oxidative stress, cortisol and sex hormones in male dogs. Andrologia. 2022;54(3):e14354.
Sugai N, Werre S, Cecere J, Balogh O. Defining an optimal range of centrifugation parameters for Canine Semen Processing. Animals: Open Access J MDPI. 2023;13:8.
Kolster KA. Evaluation of canine sperm and management of Semen disorders. Veterinary Clin North Am Small Anim Pract. 2018;48(4):533–45.
Acknowledgements
Not applicable.
Funding
The School of Veterinary Medicine, Shiraz University (Grant No. 99GCB2M154630), financially supported the study. There was no financial support for this work that could have influenced its outcome. The funding body had no role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to all parts of the study from designing a study to writing and preparing of manuscript. A.M., N.D., and M.R.D. contributed to the study design, performing study, sampling, data collection and analysis, and preparing manuscript. S.N. and I.A. aimed in designing and performing study and laboratory analyses.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval was provided by the ethics committee of the Iranian Society for the Prevention of Cruelty to Animals and the Shiraz University Research Council (IACUC no: 4687/63). The recommendations of European Council Directive (2010/63/EU) of September 22, 2010, regarding the standards in the protection of animals used for experimental purposes, were also followed. As the corresponding author, I hereby affirm, on behalf of all researchers engaged in this study, that we have collectively granted our informed consent to participate. Additionally, before the commencement of data collection, a comprehensive overview of the study’s aims, methodologies, potential risks, and benefits was presented to the owner, and informed consent was duly acquired from all owners participating in the research.
Consent to publish
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Mogheiseh, A., Derakhshandeh, N., Divar, MR. et al. Effects of short-term oral letrozole on fresh semen parameters, endocrine balance, and prostate gland dimensions in domestic dogs. BMC Vet Res 20, 416 (2024). https://doi.org/10.1186/s12917-024-04278-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12917-024-04278-3