Abstract
Background
Actinobacillus pleuropneumoniae is a serious pathogen in pigs. The abundant application of antibiotics has resulted in the gradual emergence of drugresistant bacteria, which has seriously affected treatment of disease. To aid measures to prevent the emergence and spread of drug-resistant bacteria, herein, the kill rate and mutant selection window (MSW) of danofloxacin (DAN) against A. pleuropneumoniae were evaluated.
Methods
For the kill rate study, the minimum inhibitory concentration (MIC) was tested using the micro dilution broth method and time-killing curves of DAN against A. pleuropneumoniae grown in tryptic soy broth (TSB) at a series drug concentrations (from 0 to 64 MIC) were constructed. The relationships between the kill rate and drug concentrations were analyzed using a Sigmoid Emax model during different time periods. For the MSW study, the MIC99 (the lowest concentration that inhibited the growth of the bacteria by ≥ 99%) and mutant prevention concentration (MPC) of DAN against A. pleuropneumoniae were measured using the agar plate method. Then, a peristaltic pump infection model was established to simulate the dynamic changes of DAN concentrations in pig lungs. The changes in number and sensitivity of A. pleuropneumoniae were measured. The relationships between pharmacokinetic/pharmacodynamic parameters and the antibacterial effect were analyzed using the Sigmoid Emax model.
Results
In kill rate study, the MIC of DAN against A. pleuropneumoniae was 0.016 µg/mL. According to the kill rate, DAN exhibited concentration-dependent antibacterial activity against A. pleuropneumoniae. A bactericidal effect was observed when the DAN concentration reached 4–8 MIC. The kill rate increased constantly with the increase in DAN concentration, with a maximum value of 3.23 Log10 colony forming units (CFU)/mL/h during the 0–1 h period. When the drug concentration was in the middle part of the MSW, drugresistant bacteria might be induced. Therefore, the dosage should be avoided to produce a mean value of AUC24h/MIC99 (between 31.29 and 62.59 h. The values of AUC24h/MIC99 to achieve bacteriostatic, bactericidal, and eradication effects were 9.46, 25.14, and > 62.59 h, respectively.
Conclusion
These kill rate and MSW results will provide valuable guidance for the use of DAN to treat A. pleuropneumoniae infections.
Similar content being viewed by others
Background
Porcine contagious pleuropneumonia is a serious respiratory disease of pigs caused by Actinobacillus pleuropneumoniae, which mainly grows in the porcine nasal cavity, tonsil recess, and alveolar cells [1,2,3]. The clinical symptoms mainly include acute and chronic symptoms. The acute symptoms are fibrinous hemorrhagic pneumonia and necrotic pneumonia, which often cause pig death. Chronic disease causes a decline in the pig’s feed intake, which slows down pig weight gain and seriously affects production in the pig breeding industry [4]. To date, the disease has spread to all regions of the world, seriously affecting pig production and causing huge economic losses to the breeding industry, consequently attracting increased research attention [5,6,7]. However, there are more than 19 serovars of A. pleuropneumoniae; therefore, the protective effect of the currently available vaccine is not satisfactory [8]. Consequently, antimicrobials still play an important role in the prevention and treatment of this disease, including cephalosporins, fluoroquinolones, and macrolides [9,10,11,12].
Fluoroquinolones are concentration-dependent drugs and have been widely applied to treat gram-negative bacterial infections in humans and animals [13, 14]. However, the abundant use of fluoroquinolones has resulted in the emergence of drug resistant bacteria worldwide, which seriously threatens public health. Therefore, dosage regimens should be optimized to prevent the emergence of drug-resistant bacteria. Pharmacokinetic/pharmacodynamic (PK/PD) synchronization modeling is an important method of dosage optimization [15, 16]. Especially, the mutation selection window (MSW)-based PK/PD model significantly supports methods to inhibit the production and transmission of drug resistant bacteria by analyzing the relationship between PK/PD parameters based on the minimum inhibitory concentration (MIC) or mutant prevention concentration (MPC) [17,18,19]. To date, MSW-based PK/PD analysis has been carried out for several kinds of antibacterial agents, among which fluoroquinolones are the most suitable drugs [20,21,22,23]. The resistance mechanism of bacteria against fluoroquinolones usually emerges gradually from gene point mutations, which is mostly consistent with the mutation mechanism in MSW theory [24, 25]. Danofloxacin (DAN) is a third generation fluoroquinolone antibacterial that is only used in animals. It has good antibacterial activity against bacteria and mycoplasmas, and has been applied to treat porcine respiratory diseases caused by A. pleuropneumoniae, Pasteurella multocida, and Mycoplasma hyopneumoniae [26]. In a previous study, we carried out MSW analysis of DAN against A. pleuropneumoniae in tissue cage fluid (TCF) [12]. However, the PK parameters of DAN in TCF are obviously different from those in the lung, and there are many difficulties in establishing a lung infection model for PK/PD studies. Hence, it is important to establish a peristaltic pump infection model to simulate lung infection.
Therefore, to clarify the antibacterial activity of DAN against A. pleuropneumoniae and prevent the emergence of resistant bacteria, we carried out a PK/PD study based on the kill rate and MSW of DAN against A. pleuropneumoniae. Firstly, the in vitro kill rate of DAN against A. pleuropneumoniae was assessed to study its antibacterial characteristics. Then, an in vitro peristaltic pump infection model was established according to the PK characteristics of DAN in pig lungs, which was used to study the MSW of DAN against A. pleuropneumoniae. We believe that the results of the present study can precisely clarify the antibacterial activities of DAN against A. pleuropneumoniae and will provide a valuable guide for dosage regimen designation to prevent the emergence of resistant bacteria.
Materials and methods
Strains, reagents, and the peristaltic pump model
The standard strain of A. pleuropneumoniae, CVCC259, serovar 1, was provided by the Chinese Veterinary Culture Collection Center (Qingdao, China). DAN mesylate powder (99%) was provided by Guangdong Dahuanong Biotechnology Company (Yunfu, China). Tryptic soy broth (TSB), Mueller-Hinton agar (MHA), nicotinamide adenine dinucleotide (NAD), and newborn bovine serum were provided by Guangdong Huankai Microbiology Technology (Shanghai, China). The peristaltic pump (BT100-1 F), pump head (DG-2-B/D, 10 roller), and rubber hose (inner diameter ≤ 3.17 mm, wall thickness 0.8–1 mm) were purchased from Baoding Longer Constant Pump Ltd. (Baoding, China). Fiber dialysis tubes (Float-A-Lyzer, 1000 KDa, 10 mL) were purchased from SpectrumLabs Inc (California, US). The TSB and MHA used to culture A. pleuropneumoniae contained 4% newborn bovine serum and 1% NAD (1 mg/mL).
MIC and kill curves of DAN against A. Pleuropneumoniae in TSB
A micro-broth dilution method was applied to test the MIC of DAN against A. pleuropneumoniae according to the Clinical & Laboratory Standards Institute (CLSI) standards [27]. In detail, 100 µL of DAN-containing TSB and 100 µL of log phased A. pleuropneumoniae were added to one to nine wells of a 96-well plate, such that the final concentration of DAN ranged from 0.004 to 1 µg/mL and the A. pleuropneumoniae concentration was 105 colony forming units (CFU)/mL. Both positive and negative controls were set. The plate was then incubated in a thermostatic incubator (5% CO2, 37 ℃) for 18–20 h. The MIC was determined as the minimum drug concentration that inhibited bacterial growth. The experiment was carried out in triplicate.
For the time-killing curves, eight drug concentration groups were created by twofold dilution (0.5 to 64 MIC) and a control group (0 MIC) wa set. Briefly, 100 µL of DAN solution (a 100 times dilution of the initial concentration), 1 mL log phase A. pleuropneumoniae (107 CFU/mL), and 8.9 mL TSB were added into 15 mL centrifuge tubes and cultured in an incubator (37 ℃, 5% CO2). The population of A. pleuropneumoniae was counted by the agar plate method at 0, 1, 3, 6, 9, 12, and 24 h, respectively. The detection limit of A. pleuropneumoniae was 50 CFU/mL. When the number of A. pleuropneumoniae was lower than 50 CFU/mL, 50 CFU/mL was applied to construct the kill curves. All experiments were carried out in triplicate. On the kill curves, the vertical axis was the mean number (Log10 CFU/mL) of A. pleuropneumoniae and the horizontal axis was the culture time.
Analysis of the kill rate and DAN concentration
The kill rate (Log10 CFU/mL/h) was measured as the slope of the kill curve during each time period. In this study, we only analyzed the kill rate within 0–3 h (0–1 h, 1–3 h, and 0–3 h) because A. pleuropneumoniae could not be detected after 3 h at 32 and 64 MIC.
A Sigmoid Emax model was applied to analyze the relationships between kill rates and DAN concentrations using WinNonlin software (version 5.2.1, Pharsight, Mountain View, CA, USA). The model formula is described as follows:
where E is the kill rate; Emax is the maximum kill rate of DAN during each time period; E0 is the kill rate in blank TSB; Ce is the DAN concentration; N is the Hill coefficient, representing the steepness of the kill curve; and EC50 is the DAN concentration to produce a 50% maximum kill rate.
The R2 value represented the fit degree of the kill rate and drug concentration at each time period. The larger the R2 value, the higher the correlation between the kill rate and the DAN concentration.
Determination of MIC, MIC99, and MPC of DAN against A. Pleuropneumoniae in MHA
The methods to determine the MIC, MIC99, (the lowest concentration that inhibited the growth of the bacteria by ≥ 99%) and MPC were performed according to our previously published methods using the agar plate method [12]. The details of the methods were as follows:
For the MIC, after culture for 8 h, the log phase A. pleuropneumoniae was diluted to 106 CFU/mL. Then, 100 µL of the bacterial suspension was added to MHA plates containing different DAN concentrations (0.016–1 µg/mL). After drying, the plates were cultured for 18–20 h. The MIC was determined as the minimum drug concentration that prevented bacterial growth.
For the MIC99, a series of DAN-containing MHA agar plates were prepared using 10% decreases in the (90%, 80%, 70%, 60%, and 50%). Log phase A. pleuropneumoniae was diluted (10− 1, 10− 2, 10− 3, 10− 4, 10− 5, and 10− 6) and dropped onto each MHA plate and cultured for 24 h. The number of A. pleuropneumoniae colonies were counted. The ratio of recovery growth was calculated as the number of colonies in each drug-containing plate divided the number on the blank plate and the linear relationship to the drug concentrations was determined. The MIC99 was defined as the lowest concentration that inhibited the growth of the bacteria by ≥ 99% (1% recovery).
For MPC, 100 mL of a log phase bacterial suspension was centrifuged at 5000 × g, 4 °C for 20 min. The supernatant was removed and 1 mL blank TSB was added to make the bacterial number about 1.5 × 1011 CFU/mL. Then, 100 µL of the bacterial suspension was added to a series DAN-containing MHA plates (containing DNA at 1, 2, 4, 8, 16, 32, and 64 MIC) and incubated for 72 h. The minimum concentration of DAN that inhibited bacterial growth was defined as the MPCpr. Then, the drug concentration was decreased linearly from 50 to 10% of the MPCpr and the procedures were repeated. MPC was defined as the lowest concentration of DAN that could inhibit the growth of the bacteria. All tests were carried out in triplicate.
Establishment of the in vitro peristaltic pump model
The peristaltic pump model was constructed according to our previous study [28] and the specific model schematic diagram can found in a published paper [29]. It included a blue-cap bottle (500 − 5000 mL, for storage of fresh media), a three-necked flask (350 mL, representing the central chamber, containing 300 mL of TSB, the dialysis tube (containing 10 mL of bacterial suspension), and magnetic rotor, placed in a large beaker containing water (37 °C) on a thermostatic magnetic stirrer), and a waste liquid collection bottle that was connected through the peristaltic pump and a rubber tube. The PK parameters of DAN in pig lungs were taken from a previously published report [30]. The elimination halflife (t1/2β) of DAN in pig lungs was 10.46 ± 0.76 h. For ease of calculation, we set the t1/2β at 12 h. The elimination rate constant (Kel) was calculated as 0.693/t1/2β. The peristaltic pump flow rate (Q) was calculated as Kel×VC (the central chamber broth volume). After the flow rate was set, the device was run for 2 h to stabilize it. Then, log phase A. pleuropneumoniae (108 CFU/mL) was added to the dialysis tube. When the bacterial population was stabilized at about 108 CFU/mL, the in vitro dynamic infection model was successfully established.
Antibacterial effect and MIC changes during MSW of DAN against A. pleuropneumoniae
According to the MIC99 and MPC, seven dosing groups were applied: 0, 0.025, 0.05, 0.1, 0.2, 0.4, and 0.8 µg/mL, respectively. To quickly balance the drug concentration in the dialysis tube, at the beginning of the test, the same drug dose was added to the central chamber and the dialysis chamber, simultaneously, three times (24 h/time). Then, 0.1 mL of the bacterial suspension was collected from the dialysis chamber using a 1 mL sterile syringe at 0, 3, 6, 9, 12, and 24 h after each administration, and at 48 and 72 h after the last administration. The agar plate method was applied to determine the bacterial count. Each dose group was assessed three times. The mean value of the bacterial count was applied to draw the dynamic kill curves.
The MIC of DAN toward A. pleuropneumoniae was tested at 24 h after each administration and at 48 and 72 h after the last administration. The A. pleuropneumoniae with an increased MIC were passaged for five generations to monitor the stability of the MIC.
PK/PD integration and analysis
The drug concentrations were simulated using a first-order elimination rate process and calculated according to the following formula:
where C is the drug concentrations at time t; C0 is the initial concentration of DAN; k is the constant of the elimination rate; and t is the time after drug administration.
The DAN concentrations were calculated and the drug concentration-time curves were plotted. The values of the area under concentration-time curve (AUC24 h) and maximum concentration (Cmax) during 24 h were analyzed using a non-compartment model (WinNonlin software).
The antibacterial effect (I) was defined as the maximum change in the number of bacteria during the interval of each administration.
The PK/PD parameters (AUC24h/MIC99, and Cmax/MIC99) were calculated directly using the values of AUC24h and Cmax divided by the MIC99. The percentage of time when the drug concentration was above MIC99 during the dosing interval (%T > MIC99) was calculated using pharmacodynamic models in the WinNonlin software.
An inhibitory Sigmoid Emax model was applied to analyze the relationship between PK/PD parameters and I. The formula was described as follows:
where I is the bacterial count change at different drug concentrations; Imax is the bacterial count change in the control group; I0 is the maximum change of bacterial count in the treatment group; Ce is the PK/PD parameter; IC50 is the value of PK/PD parameter to reach half of the I0; and N is the Hill coefficient, used to determine the slope of the PK/PD parameter and I curves.
R2 was applied to fit the relation between the PK/PD parameters and I. The bigger the R2 value, the better the fitting between PK/PD parameters and I. The values of the PK/PD parameters to produce a bacteriostatic effect (0 Log10 CFU/mL reduction), a bactericidal effect (3 Log10 CFU/mL reduction), and an eradication effect (4 Log10 CFU/mL reduction) were then calculated.
Results
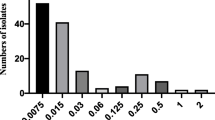
MIC and kill curves of DAN against A. Pleuropneumoniae in TSB
The MIC of DAN against A. pleuropneumoniae was 0.016 µg/mL in TSB. The change in A. pleuropneumoniae numbers in different time periods after being exposed to different DAN concentrations are listed in Table 1. The kill curves are shown in Fig. 1. Table 1 showed that when the DAN concentration was under 4 MIC, a bacteriostatic effect could be produced. When the DAN concentration reached 8 MIC, a bactericidal effect was produced; however, it took a long time (> 6 h). When the concentration of DAN increased to more than 16 MIC, an eradication effect was rapidly produced (< 6 h).
From the kill curves (Fig. 1), we observed that the growth of A. pleuropneumoniae was delayed and did not reach the maximum growth at 0.5 MIC compared with the control group. At 1 − 4 MIC, the number of A. pleuropneumoniae gradually decreased with increasing drug concentration, but ultimately recovered. At 8 MIC, DAN produced a bactericidal effect with no bacterial recovery. At 16 − 32 MIC, the number of bacteria decreased rapidly until they were below the limit of detection, and no bacteria recovered.
PK/PD analysis between the kill rate and DAN concentration
When the drug concentration exceeded 16 MIC, no bacteria could be detected after 6 h. Therefore, in this experiment, we only calculated the kill rate within 3 h and the values during different time periods are listed in Table 2. The results showed that the kill rate increased linearly with increasing DAN concentration during the 0–1 h time period. During 1–3 h, the kill rate also gradually increased under 16 MIC, but did not increase when the concentration exceed 16 MIC. The kill rate in the 0–1 h time period was significantly higher than that in 1–3 h time period, which indicated that DAN produced a rapid antibacterial effect against A. pleuropneumoniae.
The PK/PD parameters between the kill rate and DAN concentrations during each time period are listed in Table 3. The results showed that the correlation between the kill rate and DAN concentration was very high at different time periods (the R2 values range from 0.991 to 0.996). The time period with the best fit correlation with the drug concentration was 0–1 h (Fig. 2), and its maximum kill rate was 3.23 Log10 CFU/mL/h. Figure 2 shows the fitted curve between the kill rate and DAN concentrations for the 0–1 h time period, showing that the kill rate correlated positively with the drug concentration.
MIC, MIC99, and MPC in MHA
The MIC, MIC99 and MPC values of DAN against A. pleuropneumoniae were 0.0625, 0.05, and 0.4 µg/mL in MHA, respectively.
PK and in vitro dynamic kill curves
According to formula 2, the drug concentrations of DAN at each time point were obtained by extrapolation. After WinNonlin analysis, the Cmax and AUC24h were obtained after each administration. The semi-logarithmic concentration-time curves are shown in Fig. 3. The results showed that the drug concentration was located in different parts of the MSW. The 0.025 µg/mL group was located outside the MSW, the 0.05 and 0.1 µg/mL groups were partially located in the lower part of the MSW, and the 0.2 and 0.4 µg/mL groups were located in the middle part of the MSW. The 0.8 µg/mL group was located in the upper part and outside the MSW.
The kill curves under different DAN concentrations are shown in Fig. 4. The results showed that all the bacterial populations decreased, but eventually recovered after each administration (except for 0.8 µg/mL). The antibacterial effects are shown in Table 4. The 0.025 µg/mL group could achieve a bacteriostatic effect, the 0.05 and 0.1 µg/mL groups could achieve a bactericidal effect, and the 0.2–0.8 µg/mL groups could achieve an elimination effect. We can also observed that the antibacterial effect after each administration has little different in the 0.025 µg/mL group. However, when the drug concentration exceed 0.025 µg/mL, the bacterial reduction after the first administration was significantly higher than that after the second and third administrations. The greater the dose, the greater the difference, while the difference between the second and third administrations is not significant.
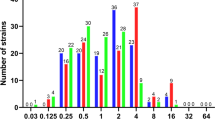
The MIC changes of A. pleuropneumoniae under each dosage are depicted in Fig. 5. The results showed that when the drug concentration was lower than the MIC99 and higher than the MPC, the MIC of A. pleuropneumoniae did not change. When the drug concentrations were in the middle of the MSW, the MIC would increase significantly with increasing administration times (increased by 8-fold in the 0.1 µg/mL group, and by 2-fold in the 0.2 µg/mL group), and would recover to the initial value after the third administration (in the 0.05 and 0.4 µg/mL groups).
PK/PD integration
The values of PK/PD parameters and the corresponding I values are shown in Table 4. After PK/PD integration, the relationships between PK/PD parameters and I were exhibited in Figs. 6 and 7, and 8.
Based on the R2 values, we selected AUC24h/MIC99 as the PK/PD parameter for analysis. The values of the PK/PD parameters and AUC24h/MIC99 required to predict different antibacterial effects are shown in Table 5. The results showed that the AUC24h/MIC99 values required to achieve bacteriostatic, bactericidal, and eradication effects were 9.46, 25.14, and 36.06 h, respectively.
Discussion
A. pleuropneumoniae is a pathogen that can cause serious respiratory diseases in pigs. Antibiotics have played an important role in treating infectious diseases. However, with the extensive use of antibiotics, bacteria have gradually developed drug resistance [31,32,33]. New drugs could effectively treat drug resistant bacteria; however, the speed of drug development cannot keep pace with the increase in drug-resistant bacteria. Therefore, optimizing dosage regimens of currently available drugs is a more realistic method.
The static time kill curve (STKC) is a basic method to study the antibacterial characteristics of drugs, which can be used to intuitively understand the antibacterial activity of drugs against pathogens by determining the kill rate, antibacterial effect, and bacterial regrowth [34]. The kill rate is a pharmacodynamic parameter obtained based on MIC and kill curves, which represents the slope of the kill curve at a certain time period, and is the combined result of the bacterial growth rate and death rate, thereby reflecting the dynamic relationship between the kill rate and drug concentrations. The kill rate method directly reflects the antibacterial activity of the drug itself and can divide drugs into concentration-dependent and time-dependent drugs [28]. The PK/PD integration between the kill rate and drug concentrations in different time periods can describe the bactericidal kinetic characteristics of drugs against bacteria in more detail [35, 36].
In this study, DAN exhibited concentration-dependent antibacterial effects against A. pleuropneumoniae based on the kill rate. With the increase in drug concentration, the bacterial population decreased rapidly. When the drug concentration increased to 64 MIC, only 3 h was needed to achieve an eradication effect. These results are consistent with those of other researchers. Tomc et al. [37] studied the kill rate of fluoroquinolones against different bacteria, showing that fluoroquinolones were more effective than βlactam drugs, and the times required to produce a bactericidal effect were 1.5 h for Enterobacteriaceae, 4–6 h for Staphylococcus aureus, and ≥ 6 h for Streptococcus. The results of the kill rate at 1–3 h showed that the kill rate did not continue to increase with the increase of the drug concentration. One reason could be that when the drug concentration increased to 16 MIC, the number of bacteria decreased rapidly and soon fell below the detection limit, which affected the calculation of the kill rate.
For A. pleuropneumoniae, the target infectious organ is the lung, making it difficult to obtain real-time and continuous dynamic PK and PD data in pigs. To date, a tissue cage model [12] has been applied for PK/PD analysis of DAN against A. pleuropneumoniae. However, such studies cannot truly reflect the antibacterial effect in clinical infection, because the drug PK values are different between tissue fluid and the lung. The peristaltic pump model can simulate the dynamic change in drug concentrations and bacterial populations in the target organs, which can reflect a realtime antibacterial effect, especially when simulating the PK and PD in difficult to obtain organs. Therefore, in this experiment, a peristaltic pump infection model was used to carry out the MSW study of DAN against A. pleuropneumoniae by simulating the PK values for DAN in pig lungs.
From the MSW study, we found that the antibacterial effect was different after each drug administration. The antibacterial effect after the first administration was significantly higher than that after the second and third treatments. There are several possible explanations for this phenomenon. Firstly, the initial bacterial population (108 CFU/mL) is higher than that in other studies (106 CFU/mL), which might have resulted in the population of sensitive bacteria being relatively high. After the first drug administration, a high proportion of the A. pleuropneumoniae population could be inhibited or killed, which could produce a greater antibacterial effect (a large change in the bacterial population). When the drug concentration decreased, it still could inhibit bacterial growth, resulting in the A. pleuropneumoniae population being unable to recover to the maximum value. After the second administration, the remaining initial bacterial population was small, resulting in a smaller antibacterial effect. Secondly, after a large number of sensitive bacteria were killed, the insensitive bacteria were screened out. However, the growth rate of the insensitive bacteria might be slower than that of the sensitive bacteria. Therefore, the total amount of bacteria could not recover to the initial level when the drug concentration declined, which could affect the calculation of the antibacterial effect.
In this experiment, we found that the MIC of A. pleuropneumoniae increased when the DAN concentrations were located between the MIC99 and the MPC. These results were consistent with previous reports [38,39,40]. There are two reasons for this phenomenon. Firstly, in the original flora, sensitive bacteria are the dominant bacteria, whereas there are fewer insensitive drug-resistant bacterial subpopulations. When the drug concentration was between MIC99 and MPC, the sensitive bacteria were gradually killed after multiple administrations and the insensitive bacteria gradually increased and became the dominant flora. Another reason could be that sensitive bacteria and insensitive bacteria had gene mutations under continuous drug selection pressure. A. pleuropneumoniae might have multiple drug-resistant gene mutations, which could make it more resistant to DAN. In this study, we found the MIC was increased by 8fold in 0.1 µg/mL group, and by 2-fold in the 0.2 µg/mL group (the corresponding mean values of AUC24h/MIC99 were 31.29 and 62.59 h, respectively), which might produce multiple genetic mutations in A. pleuropneumoniae.
When selecting drugs to treat bacterial infections, PK/PD parameters are an important reference index [41]. For fluoroquinolones, AUC24h/MIC is the most commonly applied PK/PD parameter [42]. To date, several studies have reported the PK/PD integration of DAN against ruminant pathogenic bacteria in ex vivo. One study [43] established a sheep tissue cage model to study the PK/PD of DAN against Mantella hemolytica in serum and tissue cage fluid, in which the values of AUC24h/MIC required to achieve bacteriostatic, bactericidal, and elimination effects were 17.8, 20.2, and 28.7 h in serum and 20.6, 25.5, and 41.6 h, in tissue cage fluid, respectively. Shojaee et al. [44] established a cattle tissue cage model to study the PK/PD of DAN against M. haemolyticus in serum and tissue cage fluid, and the values of AUC24h/MIC to produce bacteriostatic, 50% population reduction, bactericidal, and elimination effects were 15.9, 16.7, 18.15, and 33.5 h in serum, and 15.0, 16.34, 17.8, and 30.7 h in tissue cage fluid, respectively. There have been reports of ex vivo PK/PD analysis of DAN against porcine pathogenic bacteria. Li et al. [45] studied the PK/PD integration of DAN against Pasteurella multocide and Haemophilus parasuis in piglet serum, and the results showed that the mean AUC24h/MIC values for bacteriostatic and bactericidal effects were 32 and 49.8 h for P. multocide, and 14.6 and 37.8 h for H. parasuis, respectively. Yang et al. [46] used an ultrafiltration probe model to study the PK/PD integration of DAN against Escherichia coli in piglet ileal samples, and the mean values of AUC24h/MIC for bacteriostatic, bactericidal, and eradication effects were 99.85, 155.57, and 218.02 h, respectively. In the present study, the results showed that the correlation of AUC24h/MIC99 and Cmax/MIC99 (the R2 values were 0.8062 and 0.8063, respectively) were better than that of %T > MIC99 (R2 = 0.6950) to I. Considering that AUC24h also had the property of timeliness, we used AUC24h/MIC99 for PK/PD integration. The values of AUC24h/MIC99 to achieve bacteriostatic, bactericidal, and elimination effects were 9.46, 25.14, and 36.06 h, respectively. However, a multiple gene mutant resistant A. pleuropneumoniae might emerge when the AUC24h/MIC99 is located between 31.29 and 62.59 h; therefore, the value of AUC24h/MIC99 required to produce elimination effects should be greater than 62.59 h.
Conclusions
In conclusion, DAN exhibited a concentration-dependent antibacterial activity against A. pleuropneumoniae according to the kill rate. The maximum value of kill rate was 3.23 Log10 CFU/mL/h during the 0–1 h period. When the drug concentration was located in the middle part of the MSW, drug-resistant bacteria might be induced. Therefore, this dosage should be avoided to produce a mean value of AUC24h/MIC99 between 31.29 and 62.59 h. The values of AUC24h/MIC99 to achieve bacteriostatic, bactericidal, and eradication effects were 9.46, 25.14, and > 62.59 h, respectively. We believe these kill rates and MSW results will provide a valuable guidance for the use of DAN to treat A. pleuropneumoniae infections.
Data availability
The data used in the study analyses can be made available by the corresponding author on reasonable request.
Abbreviations
- MSW:
-
mutant selection window
- MIC:
-
minimum inhibitory concentration
- TSB:
-
tryptic soy broth
- MPC:
-
mutant prevention concentration
- PK/PD:
-
pharmacokinetic/pharmacodynamic
- TCF:
-
tissue cage fluid
- MHA:
-
Mueller-Hinton agar
- NAD:
-
Nicotinamide adenine dinucleotide
- CFU:
-
Colony forming units
References
Sassu EL, Bossé JT, Tobias TJ, Langford PR, Hennig-Pauka I. Update on Actinobacillus pleuropneumoniae-knowledge, gaps and challenges. Transbound Emerg dis. 2018;65:72–90. https://doi.org/10.1111/tbed.12739.
Stringer OW, Li Y, Bossé JT, Langford PR, JMM, Profile. Actinobacillus pleuropneumoniae: a major cause of lung disease in pigs but difficult to control and eradicate. J med Microbiol. 2022;71(3):001483. https://doi.org/10.1099/jmm.0.001483.
Gale C, Velazquez E. Actinobacillus pleuropneumoniae: a review of an economically important pathogen. Livestock. 2020;25(6):308–14. https://doi.org/10.12968/live.2020.25.6.308.
Bossé JT, Janson H, Sheehan BJ, Beddek AJ, Rycroft AN, Kroll JS, et al. Actinobacillus pleuropneumoniae: pathobiology and pathogenesis of infection. Microbes Infect. 2002;4(2):225–35. https://doi.org/10.1016/s1286-4579(01)01534-9.
Tobias TJ, Bouma A, Daemen AJ, Wagenaar JA, Stegeman A, Klinkenberg D. Association between transmission rate and disease severity for Actinobacillus pleuropneumoniae infection in pigs. Vet res. 2013;44(1):1–10. https://doi.org/10.1186/1297-9716-44-2.
Stringer OW, Li Y, Bossé JT, Forrest MS, Hernandez-Garcia J, Tucker AW, et al. Rapid Detection of Actinobacillus pleuropneumoniae from clinical samples using recombinase polymerase amplification. Front vet sci. 2022;9:805382. https://doi.org/10.3389/fvets.2022.805382.
Zhu R, Jiang H, Wang J, Bao C, Liu H, Li F, et al. Dynamic immune response characteristics of piglets infected with Actinobacillus pleuropneumoniae through omic. AMB Express. 2021;11(1):1–14. https://doi.org/10.1186/s13568-021-01336-z.
Scherrer S, Peterhans S, Neupert C, Rademacher F, Bartolomei G, Sidler X, et al. Development of a novel high resolution melting assay for identification and differentiation of all known 19 serovars of Actinobacillus pleuropneumoniae. MicrobiologyOpen. 2022;11(2):e1272. https://doi.org/10.1002/mbo3.1272.
Blondeau JM, Fitch SD. Mutant prevention and minimum inhibitory concentration drug values for enrofloxacin, ceftiofur, florfenicol, tilmicosin and tulathromycin tested against swine pathogens Actinobacillus pleuropneumoniae, Pasteurella multocida and Streptococcus suis. PLoS ONE. 2019;14(1):e0210154. https://doi.org/10.1371/journal.pone.0210154.
Yao L, Yang L, Ling Y, Wei Y, Shen X, Ding H. Pharmacokinetic/pharmacodynamic relationships of tulathromycin against Actinobacillus pleuropneumoniae in a porcine tissue cage infection model. Front vet sci. 2022;9:822432. https://doi.org/10.3389/fvets.2022.822432.
Zhang L, Wu X, Huang Z, Zhang N, Wu Y, Cai Q, et al. Pharmacokinetic/pharmacodynamic assessment of cefquinome against Actinobacillus pleuropneumoniae in a piglet tissue cage infection model. Vet Microbiol. 2018;219:100–6. https://doi.org/10.1016/j.vetmic.2018.02.027.
Zhang L, Kang Z, Yao L, Gu X, Huang Z, Cai Q, et al. Pharmacokinetic/pharmacodynamic integration to evaluate the changes in susceptibility of Actinobacillus pleuropneumoniae after repeated administration of danofloxacin. Front Microbiol. 2018;9:2445. https://doi.org/10.3389/fmicb.2018.02445.
Sumi CD, Heffernan AJ, Lipman J, Roberts JA, Sime FB. What antibiotic exposures are required to suppress the emergence of resistance for gram-negative bacteria? A systematic review. Clin Pharmacokinet. 2019;58:1407–43. https://doi.org/10.1007/s40262-019-00791-z.
Nguyen TD, Le HB, Dong TO, Pham TD. Determination of fluoroquinolones in pharmaceutical formulations by extractive spectrophotometric methods using ion-pair complex formation with bromothymol blue. J anal Methods chem. 2018;2018:8436948. https://doi.org/10.1155/2018/8436948.
Rayner CR, Smith PF, Andes D, Andrews K, Derendorf H, Friberg LE, et al. Model-informed drug development for anti-infectives: state of the art and future. Clin Pharmaco ther. 2021;109(4):867–91. https://doi.org/10.1002/cpt.2198.
Rodríguez-Gascón A, Solinís MÁ, Isla A. The role of PK/PD analysis in the development and evaluation of antimicrobials. Pharmaceutics. 2021;13(6):833. https://doi.org/10.3390/pharmaceutics13060833.
Drlica K. The mutant selection window and antimicrobial resistance. J Antimicrob Chemoth. 2003;52(1):11–7. https://doi.org/10.1093/jac/dkg269.
Drlica K, Zhao X. Mutant selection window hypothesis updated. Clin Infect dis. 2007;44(5):681–8. https://doi.org/10.1086/511642.
Xilin Z, Drlica K. Restricting the selection of antibiotic-resistant mutant bacteria: measurement and potential use of the mutant selection window. J Infect dis. 2002;185(4):561–5. https://doi.org/10.1086/338571.
Cui J, Liu Y, Wang R, Tong W, Drlica K, Zhao X. The mutant selection window in rabbits infected with Staphylococcus aureus. J Infect dis. 2006;194(11):1601–8. https://doi.org/10.1086/508752.
Lozano-Huntelman NA, Singh N, Valencia A, Mira P, Sakayan M, Boucher I, et al. Evolution of antibiotic cross-resistance and collateral sensitivity in Staphylococcus epidermidis using the mutant prevention concentration and the mutant selection window. Evol appl. 2020;13(4):808–23. https://doi.org/10.1111/eva.12903.
Liang B, Bai N, Cai Y, Wang R, Drlica K, Zhao X. Mutant prevention concentration-based pharmacokinetic/pharmacodynamic indices as dosing targets for suppressing the enrichment of levofloxacin-resistant subpopulations of Staphylococcus aureus. Antimicrob Agents Ch. 2011;55(5):2409–12. https://doi.org/10.1128/aac.00975-10.
Alieva KN, Strukova EN, Golikova MV, Portnoy YA, Zinner SH, Firsov AA. Time inside the mutant selection window as a predictor of staphylococcal resistance to linezolid. J Antibiot. 2018;71(5):514–21. https://doi.org/10.1038/s41429-017-0016-9.
Ma X, Zheng B, Wang J, Li G, Cao S, Wen Y, et al. Quinolone resistance of Actinobacillus pleuropneumoniae revealed through genome and transcriptome analyses. Int J Mol Sci. 2021;22(18):10036. https://doi.org/10.3390/ijms221810036.
Toutain PL, Pelligand L, Lees P, Bousquet-Mélou A, Ferran AA, Turnidge JD. The pharmacokinetic/pharmacodynamic paradigm for antimicrobial drugs in veterinary medicine: recent advances and critical appraisal. J vet Pharmacol ther. 2021;44(2):172–200. https://doi.org/10.1111/jvp.12917.
Stetsko TI, Kotsiumbas II, Liubenko YM, Padovskyi VN, Uhryn HP. Antimicrobial activity of danofloxacin regarding to bacteria, pathogens of respiratory infections in pigs. Scientific messenger of LNU of veterinary medicine and biotechnologies. Series: Veterinary Sci. 2019;21(95):22–6. https://doi.org/10.32718/nvlvet9504.
CLSI. Performance standards for antimicrobial disk and dilution susceptibility tests for bacteria isolated from animals; approved standard, VET 01-A4, 4th edn. 2013.
Zhang N, Gu X, Ye X, Wu X, Zhang B, Zhang L, et al. The PK/PD interactions of doxycycline against Mycoplasma gallisepticum. Front Microbiol. 2016;7:653. https://doi.org/10.3389/fmicb.2016.00653.
Wang W, Yu J, Ji X, Xia X, Ding H. Pharmacokinetic/pharmacodynamic integration of amphenmulin: a novel pleuromutilin derivative against Mycoplasma gallisepticum. Microbiol Spectr. 2024;12(2):e03675–23. https://doi.org/10.1128/spectrum.03675-23.
Xu Z, Huang A, Luo X, Zhang P, Huang L, Wang X, et al. Exploration of clinical breakpoint of Danofloxacin for Glaesserella parasuis in plasma and in PELF. Antibiotics. 2021;10(7):808.
Laxminarayan R, Sridhar D, Blaser M, Wang M, Woolhouse M. Achieving global targets for antimicrobial resistance. Science. 2016;353(6302):874–5. https://doi.org/10.3390/antibiotics10070808.
Vanni M, Merenda M, Barigazzi G, Garbarino C, Luppi A, Tognetti R, et al. Antimicrobial resistance of Actinobacillus pleuropneumoniae isolated from swine. Vet Microbiol. 2012;156(1–2):172–7. https://doi.org/10.1016/j.vetmic.2011.10.022.
Kim B, Hur J, Lee JY, Choi Y, Lee JH. Molecular serotyping and antimicrobial resistance profiles of Actinobacillus pleuropneumoniae isolated from pigs in South Korea. Vet Quart. 2016;36(3):137–44. https://doi.org/10.1080/01652176.2016.1155241.
Thorsted A, Tano E, Kaivonen K, Sjölin J, Friberg LE, Nielsen EI. Extension of pharmacokinetic/pharmacodynamic time-kill studies to include lipopolysaccharide/endotoxin release from Escherichia coli exposed to cefuroxime. Antimicrob Agents Ch. 2020;64(4):02070–19. https://doi.org/10.1128/aac.02070-19.
Ferro BE, van Ingen J, Wattenberg M, van Soolingen D, Mouton JW. Time-kill kinetics of antibiotics active against rapidly growing mycobacteria. J Antimicrob Chemoth. 2015;70(3):811–7. https://doi.org/10.1093/jac/dku431.
Cheah SE, Li J, Nation RL, Bulitta JB. Novel rate-area-shape modeling approach to quantify bacterial killing and regrowth for in vitro static time-kill studies. Antimicrob Agents Ch. 2015;59(1):381–8. https://doi.org/10.1128/aac.04182-14.
Fung-Tomc JC, Gradelski E, Valera L, Kolek B, Bonner DP. Comparative killing rates of fluoroquinolones and cell wall-active agents. Antimicrob Agents Ch. 2000;44(5):1377–80. https://doi.org/10.1128/aac.44.5.1377-1380.2000.
Xiong M, Wu X, Ye X, Zhang L, Zeng S, Huang Z, et al. Relationship between cefquinome PK/PD parameters and emergence of resistance of Staphylococcus aureus in rabbit tissue-cage infection model. Front Microbiol. 2016;7:874. https://doi.org/10.3389/fmicb.2016.00874.
Zhang B, Gu X, Li Y, Li X, Gu M, Zhang N, et al. In vivo evaluation of mutant selection window of cefquinome against Escherichia coli in piglet tissue-cage model. BMC vet res. 2014;10(1):1–8. https://doi.org/10.1186/s12917-014-0297-1.
Zhu YL, Hu LF, Mei Q, Cheng J, Liu YY, Ye Y, et al. Testing the mutant selection window in rabbits infected with methicillin-resistant Staphylococcus aureus exposed to Vancomycin. J Antimicrob Chemoth. 2012;67(11):2700–6. https://doi.org/10.1093/jac/dks280.
Leroy B, Uhart M, Maire P, Bourguignon L. Evaluation of fluoroquinolone reduced dosage regimens in elderly patients by using pharmacokinetic modelling and Monte Carlo simulations. J Antimicrob Chemoth. 2012;67(9):2207–12. https://doi.org/10.1093/jac/dks195.
Preston SL, Drusano GL, Berman AL, Fowler CL, Chow AT, Dornseif B, et al. Pharmacodynamics of levofloxacin: a new paradigm for early clinical trials. JAMA. 1998;279(2):125–9. https://doi.org/10.1001/jama.279.2.125.
Aliabadi FS, Landoni MF, Lees P. Pharmacokinetics (PK), pharmacodynamics (PD), and PK-PD integration of danofloxacin in sheep biological fluids. Antimicrob Agents Ch. 2003;47(2):626–35. https://doi.org/10.1128/aac.47.2.626-635.2003.
Shojaee AF, Lees P. Pharmacokinetic-pharmacodynamic integration of danofloxacin in the calf. Res vet sci. 2003;74(3):247–59. https://doi.org/10.1016/S0034-5288(03)00005-5.
Zhou YF, Sun Z, Wang RL, Li JG, Niu CY, Li XA, et al. Comparison of PK/PD targets and cutoff values for danofloxacin against Pasteurella multocida and Haemophilus parasuis in piglets. Front vet sci. 2022;9:811967. https://doi.org/10.3389/fvets.2022.811967.
Yang Y, Cheng P, Xiao T, Ulziikhutag J, Yu H, Li J, et al. Pharmacokinetics and pharmacodynamics integration of danofloxacin against Eschrichia Coli in piglet ileum ultrafiltration probe model. Sci rep-UK. 2021;11(1):1–10. https://doi.org/10.1038/s41598-020-80272-7.
Funding
This work was supported by National Natural Science Foundation of China (32172862); National Key R&D Program of China (2021YFD1301200); Outstanding Youth Foundation of He’nan Scientific Committee (222300420043); Leading Talents of Scientific and Technological Innovation in the Central Plains (224200510024); the Innovative Research Team (in Science and Technology) in University of Henan Province (24IRTSTHN035); the joint fund of science and technology research and development plan in Henan province(225200810044).
Author information
Authors and Affiliations
Contributions
HW and LZ contributed to the methodology, software use, validation, data analysis, writing, and project administration. CL, KD, and LW contributed to manuscript revision, and funding acquisition. All authors contributed to the article and approved the final version.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wang, H., Liao, C., Ding, K. et al. Evaluation the kill rate and mutant selection window of danofloxacin against Actinobacillus pleuropneumoniae in a peristaltic pump model. BMC Vet Res 20, 241 (2024). https://doi.org/10.1186/s12917-024-04016-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12917-024-04016-9