Abstract
Background
Sarcoptic mange is a common, pruritic parasitic skin disease of dogs. Due to its highly contagious character, it represents a potential veterinary and public health risk. Because of clinical similarity with other diseases, cross-antigenicity, and low sensitivity of available diagnostic methods, therapeutical trial is frequently used to confirm the disease. Considering the variety of available acaricidal molecules as well as the need to use the most effective treatment, the present paper reviews evidence comparing different types of systemic treatment of canine scabies.
Results
Analysis of the results showed that afoxolaner, fluralaner and sarolaner as well as several macrocyclic lactones such as selamectin, moxidectin and milbemycin oxime can lead to parasitological and clinical cure.
Conclusion
The similarity in the clinical and parasitological efficacy of these substances enhances the need for comparative studies, which could allow the identification of the most efficacious product.
Similar content being viewed by others
Background
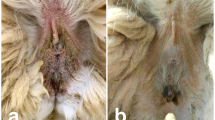
Canine sarcoptic mange is a highly pruritic, non-seasonal, contagious and potentially zoonotic parasitic skin disease caused by the mite Sarcoptes scabiei var. canis. Dogs worldwide can be affected and no breed, age or sex predisposition has been demonstrated so far [1]. Contamination occurs through direct contact with an infested host or with a fomite, due to the capacity of the mite to survive and remain infective in the environment for up to 21 days [2, 3]. Clinical presentation is characterized by intense pruritus, alopecia, papules, erythema, scaling and crusting. The disease is often complicated by secondary pyoderma, which determines the extent of the lesions and contributes to the diversity of clinical presentation, ultimately complicating the diagnosis [2, 4]. Hypothetical diagnoses are based on the clinical presentation [1], while confirmation is obtained by demonstrating the presence of the parasite, its eggs or fecal pellets in skin scrapings [2] or positive serology [3] or a favorable response to a specific therapy [2, 5]. The diagnosis of sarcoptic mange may be complicated by several factors: the mites are difficult to find by skin scraping in early infections and in animals harboring low levels of parasitism, and therefore only 20 – 50% of skin scrapings from infested dogs are positive [1]. Serological diagnosis also has certain limitations : seroconversion occurs 3-5 weeks post infection or 1 to 3 weeks after the onset of the clinical signs, leading to false negative results if the animals are sampled too soon [2]. Furthermore, cross-antigenicity between Sarcoptes scabiei, house dust mites and storage mites has also been documented [2, 6]. Hence, therapeutical trial is one of the most frequently used methods to confirm the diagnosis in cases with suggestive clinical presentation but negative test results. In this context, only the most effective molecules should be used to confirm the diagnosis and/or to treat the disease. While the efficacy of contact topical acaricidal has always been considered to be limited and influenced by several factors, systemically acting acaricides, orally or topically administered, are widely recognized as efficient molecules and consequently preferred for treatment of the disease [3]. Macrocyclic lactones include several licensed molecules that have traditionally been used for the treatment of sarcoptic mange. More recently, other therapeutic options in the isoxazoline class have demonstrated their efficacy against S. scabiei. This paper critically reviews the literature on systemic treatments of canine scabies and uses available evidence to determine the most effective therapy, according to the relevant literature identified. The selected format is a critically appraised topic (CAT).
Clinical scenario
The patient is a four-year-old German wirehaired pointer presented for a chronic, generalized, highly intense pruritus. The dog is used for hunting and is in close contact with two other dogs, who had started to develop similar clinical signs. A dermatological examination revealed the presence of alopecic and erythematous plaques, with scales and crusts distributed mainly on the ear pinnae, hocks and elbows. Microscopical examination of multiple skin scrapes revealed the presence of S. scabiei mites, enabling confirmation of sarcoptic mange. Given the range of licensed therapeutic options, the question is, which systemic molecule provides the most rapid clinical and parasitological cure.
Clinical question
A population, intervention, comparison, outcome (PICO) question was formulated: “In dogs with sarcoptic mange, which systemic treatment is the most efficacious?”
P (population) = dog with sarcoptic mange.
I (intervention) = systemic treatment.
C (comparison) = different systemic molecules.
O (outcome) = clinical and parasitic resolution.
Preferred study type = clinical trials.
Search strategy
A literature review was conducted to identify different types of treatments using the following criteria: ((dogs OR canine) AND (scabies OR Sarcoptes scabiei OR sarcoptic mange) AND (treatment)). Two electronic databases were searched (PubMed and CAB), with no time limit up to 4th October 2022. In this study we followed the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) updated guideline for systematic review stated in 2020 [7].
Quantity and quality of evidence
The search produced 51 results in PubMed and 47 in CAB. The preferred language was English. Among the full-text potentially eligible articles, only 16 met the eligibility criteria, including relevance to our PICO question and multi-animal inclusion, and were included in our review, whereas case reports and case series articles were excluded (Fig. 1).
The data that highlight the quality of the evidence, such as the journals in which the articles were published, the number of enrolled subjects, and the type of study are summarized in Table 1. All the papers included in this study were published in international peer-reviewed journals. The quality of evidence presented in the selected papers was very uneven. The main factors responsible were variable numbers of the enrolled subjects, as well as the study design. However, in all cases, the quality was considered sufficient to contribute to the conclusion of the PICO.
Results and discussion
Out of the 16 studies included in our review, nine tested products that only contained macrocyclic lactones as miticide [8,9,10,11,12,13,14,15,16], isoxazoline alone was tested in five studies [3, 4, 17,18,19], the efficacy of isoxazoline compared with an association of an isoxazoline plus a milbemycin was analyzed in two studies [20, 21], and isoxazolines and a milbemycin were compared in one study [17]. The majority of studies used positive controls [3, 11, 13,14,15,16, 19, 20], but four of the studies had no control group [4, 9, 10, 13], and in five of the studies, treated groups were compared with a placebo [8, 11, 17, 19] or with untreated groups [18].
Positive skin scraping was the sine qua non inclusion criterion in all but five studies described in four articles [8,9,10, 13] and was also the technique used to evaluate the efficacy of the parasitological cure. Animals enrolled and still present at the end of the study were declared parasitologically cured in 12 of the studies [3, 4, 8, 11, 12, 14,15,16,17,18,19,20]. Interestingly, one study demonstrated that adding vitamin E and selenium to a protocol of a weekly subcutaneous administration of ivermectin improved efficacy from 82% to 100% by day 28 [16]. Although the use of ivermectin may be preferred due to its low cost, the high probability of side effects in some breeds, the fact the product is not licensed in some countries, as well as the reported refractory cases should be taken into account [22].
The majority of substances tested led to a marked improvement in skin lesions and pruritus. Dogs were declared clinically cured in five of the studies, three of which tested macrocyclic lactones. In the first of these studies, 2 mg/kg of milbemycin oxime was administrated orally two or three times, either weekly or at two week intervals [9]. However, the timing of the clinical evaluation relative to the time treatment was administered was not mentioned in the study, and what is more, a relapse of sarcoptic mange was reported in two dogs in the same study [9]. In the second of the five studies, a topical 0.5% ivermectin solution was applied on day 1 and day 15 of the study, at a dose of 500 μg/kg. The dogs were evaluated as clinically cured by day 150 [10]. The third study evaluated the efficacy of oral and/or subcutaneous weekly administration of moxidectin until clinical remission (3-6 weeks). Thirty-seven of the enrolled animals were evaluated as clinically cured within this 3-to-6-week time frame. Among the original total of 41 dogs, seven exhibited side effects, and in three animals, treatment was discontinued for this reason [13]. The other two studies that reported a clinical cure tested molecules belonging to the more recently discovered isoxazoline class. The animals in the study using oral or topical fluralaner and oral sarolaner were considered clinically cured by day 84 [3] while animals treated with afoxolaner, and afoxolaner plus milbemycin oxime were declared cured by day 56 [21]. A slightly more rapid disappearance of clinical symptoms was reported with the medication in which milbemycin oxime was added to afoxolaner, despite the fact that the dose of milbemycin oxime added in the tested product was below the therapeutic dose recommended for sarcoptic mange [20]. These results are consistent with those obtained previously in a similar study [20], except that in the study that tested oral administration of milbemycin oxime, the dogs were followed up for longer, i.e. between 42 and 150 days. It has already been reported that resolution of alopecia in dogs with sarcoptic mange increases significantly after day 56, and that a period of four weeks between administration of the treatment and clinical evaluation is most likely too short to allow complete resolution of the lesions [20]. A longer observation period would therefore improve the reliability of clinical cure.
Five studies tested the efficacy of selamectin and/or imidacloprid plus moxidectin, and showed that two monthly applications of either of the two spot-on products can lead to parasitological and clinical cure. However, results differed regarding the time of the appearance of the parasitological cure, which varied between day 22 and day 60 [11, 12, 14, 15]. Moreover, the only study of the efficacy of a macrocyclic lactone against an isoxazoline showed that sarolaner was slightly more effective, reaching 100% efficacy by day 60, compared to 96% efficacy of the product containing imidacloprid plus moxidectin [17].
A single oral dose of fluralaner administered 10 to 20 minutes after food, or topically, was shown to lead to parasitological cure and to a significant improvement in skin lesions and pruritus by day 28 [4, 19]. All the other tests of isoxazolines, sarolaner, afoxolaner, and afoxolaner plus milbemycin oxime, demonstrated high efficacy against canine sarcoptic mange after a monthly dose, and all the products tested led to parasitological cure [16, 17, 19, 20].
It is known that successful treatment of canine sarcoptic mange depends to a great extent on the product’s ability to immediately eliminate all active mites. The effect must last long enough to prevent renewed contamination from eggs laid by hatched larvae, fomites or through contact with other infected animals [3]. Interestingly, none of the studies we reviewed reported treatment of the environment. However, when required (multiple animals involved, with no possibility of housing them individually), in-contact dogs were also treated.
The main results of all the studies are summarized in Table 2.
Conclusion and implication for practitioners
Our analysis of scientific evidence allowed us to conclude that two administrations one-month apart of topical spot-on 10% imidacloprid plus 2.5% moxidectin or 12% selamectin as well as oral sarolaner, afoxolaner, and afoxolaner plus milbemycin oxime, or one administration of topical or oral fluralaner, can lead to parasitological cure plus at least significant improvement of clinical lesions and pruritus. Moreover, no side effects were reported. The oral treatment with fluralaner allowed the most rapid parasitological cure, by day 14 all animals having negative skin scrapings. It is also the substance that was the fastest in resolving clinical signs within 21 days after a single dose. However, this data should be interpreted with caution, taking into account that weekly control during one month after the administration of the treatment were not performed in all studies.
Due to the similar clinical and parasitological efficacy of these substances, comparative studies using a similar design are now needed to identify the most efficient product. Previous studies have been demonstrated that clinical healing and absence of parasites at skin scrapings occur weeks to months before obtaining negative serum Sarcoptes-IgG tests [5]. However, adding to the classical evaluation methods a long-term serological surveillance might add new useful data and provide for clinicians a complete data set for tested molecules.
Thus, when deciding which product to use, other criteria may need to be taken into consideration such the safety of macrocyclic lactones in some breeds, the fact the extent and severity of skin lesions may interfere with the application of the topical products, the availability of licensed products, the frequency of administration, the compliance of the patient and the agreement of the owner regarding the method of administration.
Availability of data and materials
All data analysed during this study are included in this published article.
References
Miller WH Jr, Griffin CE, Campbell KL. Parasitic skin diseases. In: Mosby E, editor. Muller and Kirk’s Small Animal Dermatology. 7th ed. St Louis: Saunders; 2012. p. 284–342.
Arlian LG, Morgan MS. A review of Sarcoptes scabiei: past, present and future. Parasit Vectors. 2017;10(1):297.
Chiummo R, Petersen I, Plehn C, Zschiesche E, Roepke R, Thomas E. Efficacy of orally and topically administered fluralaner (Bravecto((R))) for treatment of client-owned dogs with sarcoptic mange under field conditions. Parasit Vectors. 2020;13(1):524.
Romero C, Heredia R, Pineda J, Serrano JA, Mendoza GD, Trapala P, Cordero AM. Efficacy of fluralaner in 17 dogs with sarcoptic mange. Vet Dermatol. 2016;27(5):353-e388.
Moog F, Brun J, Bourdeau P, Cadiergues MC. Clinical, parasitological, and serological follow-up of dogs with sarcoptic mange treated orally with lotilaner. Case Rep Vet Med. 2021;2021:6639017.
Lower KS, Medleau LM, Hnilica K, Bigler B. Evaluation of an enzyme-linked immunosorbent assay (ELISA) for the serological diagnosis of sarcoptic mange in dogs. Vet Dermatol. 2001;12(6):315–20.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Scheidt VJ, Medleau L, Seward RL, Schwartzman RM. An evaluation of ivermectin in the treatment of sarcoptic mange in dogs. Am J Vet Res. 1984;45(6):1201–2.
Miller WH Jr, de Jaham C, Scott DW, Cayatte SM, Bagladi MS, Buerger RG. Treatment of canine scabies with milbemycin oxime. Can Vet J. 1996;37(4):219–21.
Paradis M, de Jaham C, Page N. Topical (pour-on) ivermectin in the treatment of canine scabies. Can Vet J. 1997;38(6):379–82.
Shanks DJ, McTier TL, Behan S, Pengo G, Genchi C, Bowman DD, Holbert MS, Smith DG, Jernigan AD, Rowan TG. The efficacy of selamectin in the treatment of naturally acquired infestations of Sarcoptes scabiei on dogs. Vet Parasitol. 2000;91(3–4):269–81.
Six RH, Clemence RG, Thomas CA, Behan S, Boy MG, Watson P, Benchaoui HA, Clements PJ, Rowan TG, Jernigan AD. Efficacy and safety of selamectin against Sarcoptes scabiei on dogs and Otodectes cynotis on dogs and cats presented as veterinary patients. Vet Parasitol. 2000;91(3–4):291–309.
Wagner R, Wendlberger U. Field efficacy of moxidectin in dogs and rabbits naturally infested with Sarcoptes spp., Demodex spp and Psoroptes spp. mites. Vet Parasitol. 2000;93(2):149–58.
Krieger K, Heine J, Dumont P, Hellmann K. Efficacy and safety of imidacloprid 10% plus moxidectin 2.5% spot-on in the treatment of sarcoptic mange and otoacariosis in dogs: results af a European field study. Parasitol Res. 2005;97(Suppl 1):S81–8.
Fourie LJ, Heine J, Horak IG. The efficacy of an imidacloprid/moxidectin combination against naturally acquired Sarcoptes scabiei infestations on dogs. Aust Vet J. 2006;84(1–2):17–21.
Behera SK, Dimri U, Singh SK, Mohanta RK. The curative and antioxidative efficiency of ivermectin and ivermectin + vitamin E-selenium treatment on canine Sarcoptes scabiei infestation. Vet Res Commun. 2011;35(4):237–44.
Becskei C, De Bock F, Illambas J, Cherni JA, Fourie JJ, Lane M, Mahabir SP, Six RH. Efficacy and safety of a novel oral isoxazoline, sarolaner (Simparica), for the treatment of sarcoptic mange in dogs. Vet Parasitol. 2016;222:56–61.
Beugnet F, de Vos C, Liebenberg J, Halos L, Larsen D, Fourie J. Efficacy of afoxolaner in a clinical field study in dogs naturally infested with Sarcoptes scabiei. Parasite. 2016;23:26.
Taenzler J, Liebenberg J, Roepke RK, Frenais R, Heckeroth AR. Efficacy of fluralaner administered either orally or topically for the treatment of naturally acquired Sarcoptes scabiei var. canis infestation in dogs. Parasit Vectors. 2016;9(1):392.
Hampel V, Knaus M, Schafer J, Beugnet F, Rehbein S. Treatment of canine sarcoptic mange with afoxolaner (NexGard((R))) and afoxolaner plus milbemycin oxime (NexGard Spectra((R))) chewable tablets: efficacy under field conditions in Portugal and Germany. Parasite. 2018;25:63.
Romero-Nunez C, Bautista-Gomez LG, Sheinberg G, Martin-Cordero A, Flores-Ortega A, Heredia-Cardenas R. Efficacy of afoxolaner plus milbemycin oxime and afoxolaner alone as treatment for sarcoptic mange in naturally infested dogs. Can J Vet Res. 2020;84(3):212–6.
Terada Y, Murayama N, Ikemura H, Morita T, Nagata M. Sarcoptes scabiei var. canis refractory to ivermectin treatment in two dogs. Vet Dermatol. 2010;21(6):608–12.
Acknowledgements
The authors thank Daphne Goodfellow for English editing.
Funding
This research received no external funding.
Author information
Authors and Affiliations
Contributions
Conceptualization, M.O.D. and MC.C; data curation, M.O.D.; writing— preparation of the original draft, M.O.D.; writing—review and editing, MC.C; supervision, MC.C. Both authors have read and agreed to the submitted version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
M.O.D. declares no conflict of interest. Over the past five years, M.-C.C. has received research support and lecturing honorarium from Elanco, Virbac and Zoetis.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Dumitrache, M.O., Cadiergues, MC. The most effective systemic treatment in dogs with sarcoptic mange: a critically appraised topic. BMC Vet Res 19, 189 (2023). https://doi.org/10.1186/s12917-023-03759-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12917-023-03759-1