Abstract
Background
Swine acute diarrhea syndrome coronavirus (SADS-CoV) causes acute vomiting and diarrhea in piglets, leading to significant financial losses for the pig industry. Recombinase polymerase amplification (RPA) is a rapid nucleic acid amplification technology used under constant temperature conditions. The study established a real-time reverse transcription (RT)-RPA assay for early diagnosis of SADS-CoV.
Results
The detection limit of the real-time RT-RPA was 74 copies/µL of SADS-CoV genomic standard recombinant plasmid in 95% of cases. The assay was performed in less than 30 min and no cross-reactions were observed with eight other common viruses that affect swine, including classical swine fever virus (CSFV), porcine reproductive and respiratory syndrome virus (PRRSV), pseudo rabies virus (PRV), swine influenza virus (SIV), seneca valley virus (SVA), transmissible gastroenteritis virus (TGEV), porcine epidemic diarrhea virus (PEDV) and porcine deltacoronavirus (PDCoV). The coefficient of variation (C.V.) values of the two standards dilutions and three positive clinical sample ranged from 2.95% to 4.71%. A total of 72 clinical fecal samples from swine with diarrheal symptoms were analyzed with the developed RT-RPA and quantitative RT-PCR. There was 98.61% agreement between the RT-RPA and the quantitative real-time PCR results.
Conclusions
These results indicated that the developed RT-RPA assay had good specificity, sensitivity, stability and repeatability. The study successfully established a broadly reactive RT-RPA assay for SADS-CoV detection.
Similar content being viewed by others
Background
Coronaviruses (CoVs) are a family of enveloped, single-stranded, positive-strand RNA viruses classified within the Nidovirales order [1]. Four genera of coronaviruses, including alpha, beta, gamma and delta, have been confirmed to cause subclinical, respiratory and gastrointestinal disease in humans, other mammals and birds [2, 3]. In February 2017, a new intestinal virus of piglets termed swine acute diarrhea syndrome coronavirus (SADS-CoV), was discovered in southern China, which caused acute vomiting and diarrhea in newborn piglets, resulting in mass mortality. These major economic losses caused by the disease are a huge threat to the local pig industry [4,5,6].
The clinical symptoms caused by SADS-CoV are similar to those caused by the three existing swine enteric coronaviruses (SeCoVs) [7, 8], transmissible gastroenteritis virus (TGEV) [9], porcine epidemic diarrhea virus (PEDV) [10,11,12,13] and porcine deltacoronavirus (PDCoV) [14,15,16,17,18,19,20,21]. The SADS-CoV virus also called swine enteric alphacoronavirus (SeACoV)[4] or porcine enteric alphacoronavirus (PEAV) [6] does not relate to the above three viruses, so it is very important to establish a point-of-care testing (POCT) method that can quickly and accurately identify SADS-CoV.
The SADS-CoV virus belongs to the alphacoronavirus genus of the coronavirus family, with a genome size of about 2.7 kb and a gene structure very similar to that of the bat coronavirus HKU-2 strain. It includes nine ORFs including non-structural polymers ORF1a and ORF1b, structural proteins Spike (S), envelope (E), membrane (M) and nucleocapsid (N), as well as auxiliary proteins NS3a, NS7a and NS7 [4, 5, 22].
At present, the main methods for diagnosing SADS-CoV are reverse transcription PCR (RT-PCR) [23], quantitative real-time PCR [24,25,26], reverse transcriptional loop-mediated isothermal amplification (RT-LAMP) [27, 28], virus isolation culture, immunofluorescence (IF) and immunohistochemistry (IHC), with the gold standard and most common method for the diagnosis of SADS-CoV being nucleic acid testing technology. But some nucleic acid testing methods are time-consuming and complex and require expensive instruments and professional technicians, so it is very important to establish an economical, simple and efficient detection method.
Recombinase polymerase amplification (RPA) is a method that can efficiently amplify DNA at a constant temperature of 37 to 42 °C [29]. In addition, RPA reaction time is shorter at 20 to 30 min compared to RT-LAMP and is a new technique that can be used for clinical and field detection.
The current study is a preliminary examination of reverse transcriptase recombinase polymerase amplification (RT-RPA) fluorescence analysis for the detection of SADS-CoV. The RT-RPA system was found to be accurate, sensitive, specific, and reproducible for point-of-care diagnosis, which would be advantageous for the early diagnosis of diarrhea on pig farms, especially in remote areas and assist the early adoption of effective measures to control the spread of disease.
Results
Screening of the primer–probe set
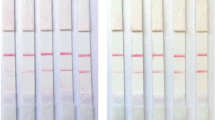
Five pairs of RPA primers were designed for SADS-CoV-M and are listed in Table 1. The extracted viral RNA was used as a template, five primer combinations were amplified using the basic RT-RPA assay and the amplification products were evaluated on 2.0% agarose gels, in Fig. 1.
Evaluation of RT-RPA system detection performance
Specificity and sensitivity
Nine relevant swine viral nucleic acids, from classical swine fever virus (CSFV), porcine reproductive and respiratory syndrome virus (PRRSV), pseudo rabies virus (PRV), swine influenza virus (SIV), seneca valley virus (SVA), transmissible gastroenteritis virus (TGEV), porcine epidemic diarrhea virus (PEDV), porcine deltacoronavirus (PDCoV) and SADS-CoV were used in this study. As shown in Fig. 2, significant amplification was only observed for SADS-CoV but not the eight other viral nucleic acids and the control water.
Serial dilution of the standard recombinant plasmid from 106 to 101 copies/μL was initially conducted to investigate the detection limits of the established RT-RPA assay for SADS-CoV. Figure 3 showed that the RT-RPA assay enabled the detection of SADS-CoV within 30 min and the detection limit was maintained at 101 copies/μL. A probit regression analysis using the results of eight runs was performed to determine the exact detection limit and the results showed that RT-RPA could detect 74 copies/μL standard at 95% probability, as seen in Fig. 4-A. The semi-logarithmic regression analysis was performed using the data from the sensitivity test results of standard samples. There was a significant linear relationship between the logarithm of the standard concentration and the Tt value for SADS-CoV where R2 = 0.9821, as in Fig. 4-B.
Stability and reproducibility
To validate the stability of the established RT-RPA detection system, detectable concentrations of standard were diluted to 105 and 103 copies/μL and the two standard dilutions were repeated five times. The C.V. values of the detectable concentration standard samples was less than 5%, as shown in Table 2. The three clinical SADS-CoV-infected fecal samples were each tested five times and the C.V. values were 4.62%, 4.71% and 4.62%, as listed in Table 2, which indicated that the RPA assay was repeatable and precise.
Performance of the RT-RPA system in clinical samples
A total of 72 samples made up of 24 intestinal and 48 fecal, were collected by the Guangdong Laboratory Animals Monitoring Institute to evaluate SADS-CoV using the RPA and quantitative real-time PCR assays. The results from testing 10 SADS-CoV positive and 62 negative samples with the RT-RPA system compared with quantitative real-time PCR assays, showed that no negative samples from the quantitative real-time PCR assay were found to be positive by the new RT-RPA system. One sample detected as negative by RT-RPA was detected as positive by quantitative real-time PCR and the Ct value of the sample was 21.174.
The coincidence rate defined as the proportion of the number of samples with the same test results in the total number of test samples between the quantitative real-time PCR and the RT-RPA system was 98.61% for SADS-CoV as shown in Table 3. The sensitivity of RT-RPA for the virus was 90.91% and the specificity was 100%, demonstrating that the RT-RPA system was effective and dependable.
Based on the above data, ROCs were plotted to determine the diagnostic accuracy of the RT-RPA system and the quantitative real-time PCR assay. The Youden index of the drawn ROCs curve was 0.91 and the corresponding AUCROC was 0.955. Further analysis showed that there was no significant difference (p < 0.0001) between the two methods of the established RT-RPA system for detecting SADS-CoV and quantitative real-time PCR assay, as seen in Fig. 5.
Discussion
The SADS-CoV virus which is infectious disease, was first identified on Chinese pig farms and therefore may become a significant threat to human and animals’ health. Rapid, convenient diagnosis of SADS-CoV would play a key role in intervention and the implementation of preventive measures. In the present study, a real-time RT-RPA assay was established for rapid and specific detection of SADS-CoV. In a previous report [28], the M protein of SADS-CoV was found to be a highly conserved transmembrane protein and this study designed a primer–probe set based on those M gene sequences.
The RPA technology is ideal for on-site sample testing. The requirements for detection equipment are low, samples can be detected even at human body temperature and the method has high sensitivity, even within 10 copies/μL in some studies [30]. In recent years, the recombinase polymerase amplification lateral flow dipstick (RPA-LFD) detection method has become well known. This method can detect antigens in clinical samples within 10 min, but its sensitivity is lower than that of RT-PCR and quantitative real-time, so it is not suitable for use when the requirements are higher.
The RPA detection can directly use original samples, such as blood, nasal swab, pleural fluid or culture medium, without nucleic acid purification, which saves time in clinical testing and is suitable for high throughput detection [30,31,32]. Due to its convenience and portability, the RPA technique has been used for the rapid detection of various pathogens, such as feline coronavirus (FCoV) [33], avian reovirus [34], human norovirus [35], murine norovirus [36] and pathogenic bacteria [37], but currently there is no current report about the use of the RPA assay for SADS-CoV monitoring.
An RT-RPA fluorescence assay was developed to amplify the M gene of SADS-CoV. It detected SADS-CoV within 15 min at 42 °C, with a detection limit of 74 copies/μL and did not cross-react with CSFV, PRRSV, PRV, SIV, SVA, TGEV, PEDV and PDCoV. There was 98.61% agreement between the RT-RPA and the quantitative real-time PCR results and further analysis showed that there was no significant difference (p < 0.0001) between the two methods. It therefore provided the possibility of rapid clinical detection of SADS-CoV infection and had the potential to detect SADS-CoV in directly boiled animal tissue or stool samples in the future. This procedure would be valuable to reduce sample processing time and increase portability.
Conclusions
This study established a real-time fluorescence-based RT-RPA assay, which can detect SADS-CoV within 15 min and has a detection limit of 74 copies/μL. The SADS-CoV RPA does not cross-react with CSFV, PRRSV, PRV, SIV, SVA, TGEV, PEDV, or PDCoV. Compared with quantitative real-time PCR, this assay is convenient and less labor intensive and it provides the possibility for rapid clinical detection of SADS-CoV infection in a variety of samples.
Although RT-RPA fluorescence analysis technology is simple, rapid and highly specific, it is prone to be contaminated during operation, so it is necessary to standardize operations, keep reagents properly and separate the sample addition area from the amplification area.
Methods
Clinical samples, virus collection, and nucleic acid extraction
Clinical samples including feces and intestinal contents, were collected from breeding farms in southern China in accordance with the recommendations of National Standards for Laboratory Animals of the People’s Republic of China (GB149258-2010). Samples were preserved at − 80 °C in Guangdong Laboratory Animals Monitoring Institute from the time of receipt until use. Nine kinds of porcine viruses, including classical swine fever virus (CSFV), porcine reproductive and respiratory syndrome virus (PRRSV), pseudo rabies virus (PRV), swine influenza virus (SIV), seneca valley virus (SVA), transmissible gastroenteritis virus (TGEV), porcine epidemic diarrhea virus (PEDV), porcine deltacoronavirus (PDCoV) and swine acute diarrhea syndrome coronavirus (SADS-CoV) are prepared by this laboratory.
Before RNA extraction, the sample is added to the sample diluent (PBS) and mixed, with the supernatant for nucleic acid extraction. The DNA/RNA of virus and clinical samples including feces and intestinal contents were extracted using a Baybio Biotech automatic nucleic acid extraction and purification instrument (Guangzhou Co., China), according to the Baypure universal magnetic bead virus DNA/RNA extraction kit instructions and were stored in a − 70 °C freezer.
Primer and probe design
The reference genomic sequences of SADS-CoV-M were downloaded from Genbank with the accession number MK651076. There was currently no software available for RPA primer and probe design [36], so based on the highly conserved M gene nucleic acid alignment, a set of primers and a probe were designed using Primer Premier 5 software (Premier, Canada) and NCBI website (USA) according to the TwistDx Assay Design Manual (TwistDx, UK) and synthesized by Sangon Biotech (Shanghai) Co., Ltd. (Shanghai, China), shown in Table 1.
Cloning of standard recombinant plasmid
A pair of primers M-F and M-R for the SADS-CoV-M gene nucleic acid fragments were designed and the target region was amplified using a one-step quantitative real-time PCR kit (Takara, China). The reaction conditions were reverse transcription (RT) at 37 °C for 30 min, denaturation at 85 °C for five min, 35 cycles at 95 °C for 30 s, 50 °C for 30 s and 72 °C for 45 s and a final extension step at 72 °C for 10 min. The amplicon was recovered using a DNA gel extraction kit (Beyotime Biotechnology, China). The purified amplicon was cloned into the pMD-18 T vector (TAKARA, USA) and designated as pMD-18 T-SADS-CoV-M. The positive plasmid was sequenced by Sangon Biotech (Shanghai, China), quantified by Nano2000 (GE, USA) and converted to copy number.
Development of RT-RPA assays
The basic RT-RPA reaction was conducted in a 50 μL volume using the Basic RT-RPA kit (Hangzhou ZC Bio-Sci&Tech, China), which consisted of 41.5 μL of A buffer, 2 μL of template, 2 μL of each 10 μM primer and 2.5 μL of B buffer. The microtubes were immediately placed in the heating block and incubated at 42 °C for 30 min. The RPA product was cleaned using a PCR products Clean Up Kit (Beyotime Biotechnology) to remove inhibitors that might affect the agarose electrophoresis and then separated on a 2% agarose gel. The amplicons were sequenced using an ABI 3730XL Sanger-based Genetic Analyzer (Applied Biosystems, Waltham, MA, USDA).
Real-time RT-RPA assay was performed using the Fluorescent RT-RPA kit (Hangzhou ZC Bio-Sci&Tech, China). The reaction conditions for real-time RT-RPA were the same as for the basic RT-RPA, except that 0.6μL of water was replaced by 0.6 μL of probe and was performed at 39 °C in a Deaou-308C Tubes Canner (DEAOU Biotechnology, China). According to the manufacturer, a sample was confirmed positive if the amplification curve was above three-and-a-half standard deviations (3.5 SD) from the background in the course of a valid time range after 17 to 18 min of amplification. A threshold time range of zero to four min 30 s was used [33].
System evaluation and validation
Specificity
To investigate the specificity, nine viruses, including CSFV, PRRSV, PRV, SIV, SVA, TGEV, PEDV, PDCoV, and SADS-CoV were evaluated. RNase Free ddH2O was used as a no template control.
Sensitivity
The standard was tenfold serially diluted from 106 to 101 copies/μL with distilled water and used to evaluate the detection limit of the SADS-CoV real-time RT-RPA fluorescence assay. Each dilution was evaluated in eight replicates. A semi-log regression was performed by plotting the threshold time against the log10standard copy numbers using Prism 5.0 software (GraphPad, USA). To determine the analytical sensitivity of the RT-RPA technique, a probit regression was performed using Prism 5.0 software (GraphPad, USA).
Stability and repeatability analysis
To confirm the stability and repeatability of the developed RT-RPA systems, standard dilutions with high 105 copies/μL and low 103 copies/μL concentrations were used to evaluate the coefficients of variation (C.V.) of the RT-RPA systems. The assay for Time threshold (Tt) was defined as the reaction time required for a particular sample to reach sufficiently positive signals above the baseline during real-time amplification. The two standard dilutions and three positive clinical samples were repeated five times, and Tt of reaching positivity were recorded.
RT-RPA and quantitative real-time PCR for the detection of clinical samples
A total of 72 swine clinical fecal samples consisting of 24 intestinal and 48 fecal, from healthy piglets and piglets with diarrhea symptoms (these piglets are less than 15 days of age), were detected using the RT-RPA system and the results were compared with quantitative real-time PCR to check for any nonspecific amplification. The Ct value represents the number of cycles that the fluorescent signal in each reaction tube takes to reach the set threshold. There is a linear relationship between the Ct value and the logarithm of the initial copy number of the template. The higher the initial template concentration, the smaller the Ct value; the lower the initial template concentration, the larger the Ct value. The results were further evaluated by generating receiver operating characteristic curves (ROCs), using MedCalc statistical software, V19.1.4. The SADS nucleic acid was used as the positive control.
Availability of data and materials
All data generated or analyzed during this study are included in this article and are available from the corresponding author on reasonable request.
Abbreviations
- RPA:
-
Recombinase polymerase amplification
- SADS-CoV:
-
Swine acute diarrhea syndrome coronavirus
- RT-RPA:
-
Reverse transcriptase recombinase polymerase amplification
- CSFV:
-
Classical swine fever virus
- PRRSV:
-
Porcine reproductive and respiratory syndrome virus
- PRV:
-
Pseudo rabies virus
- SIV:
-
Swine influenza virus
- SVA:
-
Seneca valley virus
- TGEV:
-
Transmissible gastroenteritis virus
- PEDV:
-
Porcine epidemic diarrheavirus
- PDCoV:
-
Porcine deltacoronavirus
- C.V.:
-
Coefficients of variation
- CoVs:
-
Coronaviruses
- SeCoVs:
-
Swine enteric Coronaviruses
- SeACoV:
-
Swine enteric alphacoronavirus
- PEAV:
-
Porcine enteric alphacoronavirus
- POCT:
-
Point-of-care testing
- RT-PCR:
-
Reverse-transcription polymerase chain reaction
- RT-LAMP:
-
Reverse transcriptional loop-mediated isothermal amplification
- IF:
-
Immunofluorescence
- IHC:
-
Immunohistochemistry
- SD:
-
Standard deviation
- ROCs:
-
Receiver operating characteristic curves
- AUCs:
-
Area Under Curve
- Tt:
-
Time threshold
References
Weiss SR, Navas-Martin S. Coronavirus pathogenesis and the emerging pathogen severe acute respiratory syndrome coronavirus. Microbiol Mol Biol Rev. 2005;69(4):635–64.
King AMQ, Adams MJ, Carstens EB, et al. Virus Taxonomy: Ninth Report of the International Committee on Taxonomy of Viruses[J]. Arch Virol. 2012.
Woo PC, Lau SK, Lam CS, Lau CC, Tsang AK, Lau JH, Bai R, Teng JL, Tsang CC, Wang M, et al. Discovery of seven novel Mammalian and avian coronaviruses in the genus deltacoronavirus supports bat coronaviruses as the gene source of alphacoronavirus and betacoronavirus and avian coronaviruses as the gene source of gammacoronavirus and deltacoronavirus. J Virol. 2012;86(7):3995–4008.
Pan Y, Tian X, Qin P, Wang B, Zhao P, Yang Y-L, Wang L, Wang D, Song Y, Zhang X, et al. Discovery of a novel swine enteric alphacoronavirus (SeACoV) in southern China. Vet Microbiol. 2017;211:15–21.
Gong L, Li J, Zhou Q, Xu Z, Chen L, Zhang Y, Xue C, Wen Z, Cao Y. A New Bat-HKU2-like Coronavirus in Swine, China, 2017. Emerg Infect Dis. 2017;23(9):1607–9.
Zhou P, Fan H, Lan T, Yang X-L, Shi W-F, Zhang W, Zhu Y, Zhang Y-W, Xie Q-M, Mani S, et al. Fatal swine acute diarrhoea syndrome caused by an HKU2-related coronavirus of bat origin. Nature. 2018;556(7700):255–8.
Jung K, Hu H, Saif LJ. Porcine deltacoronavirus infection: Etiology, cell culture for virus isolation and propagation, molecular epidemiology and pathogenesis. Virus Res. 2016;226:50–9.
Pensaert MB, de Bouck P. A new coronavirus-like particle associated with diarrhea in swine. Arch Virol. 1978;58(3):243–7.
Doyle LP, Hutchings LM. A transmissible gastroenteritis in pigs. J Am Vet Med Assoc. 1946;108:257–9.
Wood EN. An apparently new syndrome of porcine epidemic diarrhoea. Vet Rec. 1977;100(12):243–4.
Stevenson GW, Hoang H, Schwartz KJ, Burrough ER, Sun D, Madson D, Cooper VL, Pillatzki A, Gauger P, Schmitt BJ, et al. Emergence of Porcine epidemic diarrhea virus in the United States: clinical signs, lesions, and viral genomic sequences. J Vet Diagn Invest. 2013;25(5):649–54.
Cima G. Fighting a deadly pig disease. Industry, veterinarians trying to contain PED virus, new to the US. J Am Vet Med Assoc. 2013;243(4):469–70.
Jung K, Saif LJ. Porcine epidemic diarrhea virus infection: Etiology, epidemiology, pathogenesis and immunoprophylaxis. Vet J. 2015;204(2):134–43.
Li G, Chen Q, Harmon KM, Yoon KJ, Schwartz KJ, Hoogland MJ, Gauger PC, Main RG, Zhang J. Full-Length Genome Sequence of Porcine Deltacoronavirus Strain USA/IA/2014/8734. Genome Announc. 2014;2(2):e00278-14.
Marthaler D, Jiang Y, Collins J, Rossow K. Complete Genome Sequence of Strain SDCV/USA/Illinois121/2014, a Porcine Deltacoronavirus from the United States. Genome Announc. 2014;2(2):e00218-14.
Wang L, Byrum B, Zhang Y. Detection and genetic characterization of deltacoronavirus in pigs, Ohio, USA, 2014. Emerg Infect Dis. 2014;20(7):1227–30.
Lee S, Lee C. Complete Genome Characterization of Korean Porcine Deltacoronavirus Strain KOR/KNU14–04/2014. Genome Announc. 2014;2(6):e01191-14.
Chen F, Zhu Y, Wu M, Ku X, Yao L, He Q. Full-Length Genome Characterization of Chinese Porcine Deltacoronavirus Strain CH/SXD1/2015. Genome Announc. 2015;3(5):e01284-15.
Janetanakit T, Lumyai M, Bunpapong N, Boonyapisitsopa S, Chaiyawong S, Nonthabenjawan N, Kesdaengsakonwut S, Amonsin A. Porcine Deltacoronavirus, Thailand, 2015. Emerg Infect Dis. 2016;22(4):757–9.
Song D, Zhou X, Peng Q, Chen Y, Zhang F, Huang T, Zhang T, Li A, Huang D, Wu Q, et al. Newly Emerged Porcine Deltacoronavirus Associated With Diarrhoea in Swine in China: Identification, Prevalence and Full-Length Genome Sequence Analysis. Transbound Emerg Dis. 2015;62(6):575–80.
Wang YW, Yue H, Fang W, Huang YW. Complete Genome Sequence of Porcine Deltacoronavirus Strain CH/Sichuan/S27/2012 from Mainland China. Genome Announc. 2015;3(5):e00945-15.
Fu X, Fang B, Liu Y, Cai M, Jun J, Ma J, Bu D, Wang L, Zhou P, Wang H, et al. Newly emerged porcine enteric alphacoronavirus in southern China: Identification, origin and evolutionary history analysis. Infect Genet Evol. 2018;62:179–87.
Si G, Niu J, Zhou X, Xie Y, Chen Z, Li G, Chen R, He D. Use of dual priming oligonucleotide system-based multiplex RT-PCR assay to detect five diarrhea viruses in pig herds in South China. AMB Express. 2021;11(1):99–99.
Zhou L, Sun Y. Wu J-l, Mai K-j, Chen G-h, Wu Z-x, Bai Y, Li D, Zhou Z-h, Cheng J: Development of a TaqMan-based real-time RT-PCR assay for the detection of SADS-CoV associated with severe diarrhea disease in pigs. J Virol Methods. 2018;255:66–70.
Ma L, Zeng F, Cong F, Huang B, Huang R, Ma J, Guo P. Development of a SYBR green-based real-time RT-PCR assay for rapid detection of the emerging swine acute diarrhea syndrome coronavirus. J Virol Methods. 2019;265:66–70.
Huang X, Chen J, Yao G, Guo Q, Wang J, Liu G. A TaqMan-probe-based multiplex real-time RT-qPCR for simultaneous detection of porcine enteric coronaviruses. Appl Microbiol Biotechnol. 2019;103(12):4943–52.
Wang H, Cong F, Zeng F, Lian Y, Liu X, Luo M, Guo P, Ma J. Development of a real time reverse transcription loop-mediated isothermal amplification method (RT-LAMP) for detection of a novel swine acute diarrhea syndrome coronavirus (SADS-CoV). J Virol Methods. 2018;260:45–8.
Zhou L, Chen Y, Fang X, Liu Y, Du M, Lu X, Li Q, Sun Y, Ma J, Lan T. Microfluidic-RT-LAMP chip for the point-of-care detection of emerging and re-emerging enteric coronaviruses in swine. Anal Chim Acta. 2020;1125:57–65.
Piepenburg O, Williams CH, Stemple DL, Armes NA. DNA detection using recombination proteins. PLoS Biol. 2006;4(7):e204–e204.
Xia X, Yu Y, Weidmann M, Pan Y, Yan S, Wang Y. Rapid detection of shrimp white spot syndrome virus by real time, isothermal recombinase polymerase amplification assay. PLoS One. 2014;9(8):e104667.
Daher RK, Stewart G, Boissinot M, Bergeron MG. Recombinase Polymerase Amplification for Diagnostic Applications. Clin Chem. 2016;62(7):947–58.
Liljander A, Yu M, O’Brien E, Heller M, Nepper JF, Weibel DB, Gluecks I, Younan M, Frey J, Falquet L, et al. Field-Applicable Recombinase Polymerase Amplification Assay for Rapid Detection of Mycoplasma capricolum subsp capripneumoniae. J Clin Microbiol. 2015;53(9):2810–5.
Hu X, Xiao L, Cong X, Zhu Y, Huang B, Cong F. Development of a recombinase polymerase amplification fluorescence assay to detect feline coronavirus. Mol Cell Probes. 2020;54:101669.
Ma L, Shi H, Zhang M, Song Y, Zhang K, Cong F. Establishment of a Real-Time Recombinase Polymerase Amplification Assay for the Detection of Avian Reovirus. Front Vet Sci. 2020;7:551350.
Yehia N, Arafa AS. Abd El Wahed A, El-Sanousi AA, Weidmann M, Shalaby MA: Development of reverse transcription recombinase polymerase amplification assay for avian influenza H5N1 HA gene detection. J Virol Methods. 2015;223:45–9.
Ma L, Zeng F, Cong F, Huang B, Zhu Y, Wu M, Xu F, Yuan W, Huang R, Guo P. Development and evaluation of a broadly reactive reverse transcription recombinase polymerase amplification assay for rapid detection of murine norovirus. BMC Vet Res. 2018;14(1):399.
Chen J, Xu Y, Yan H, Zhu Y, Wang L, Zhang Y, Lu Y, Xing W. Sensitive and rapid detection of pathogenic bacteria from urine samples using multiplex recombinase polymerase amplification. Lab Chip. 2018;18(16):2441–52.
Acknowledgements
Special thanks to Xiaoliang Hu for his comments on the revision of this study.
Funding
The work was supported in part by the National key research and development program (2021YFF0703300), Anhui provincial collaborative innovation program (GXXT-2019–035), Chuzhou Science and Technology plan (2019ZN003) and the key discipline construction program of Anhui Science and Technology University (AKZDXK2015A-04). The funding sources was not involved in the design of the research, the collection, analysis and interpretation of data, and the writing of the manuscript.
Author information
Authors and Affiliations
Contributions
CX: Conceptualization, Methodology, Writing-original draft, Writing-review & editing. ZYJ: Writing-review & editing, Data curation. LXC: Methodology, Validation, Writing-review & editing. LYX: Resources. LYZ: Resources. HBH: Resources. GYF: Resources, Supervision, Funding acquisition. WML: Resources, Supervision, Project administration. SY: Resources, Supervision. The author(s) read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study protocol concerning the animals was processed in strict accordance with the recommendations approved by the Animal Care and Welfare Committee of Anhui Science and Technology University and Guangdong Laboratory Animals Monitoring Institute. And all methods were performed in accordance with the Sanitary Standard for the Non-hazardous Treatment of Might Soil (GB7959-87).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Supplementary Fig. 1. Stability test of SADS-CoV for five times replicate experiments using (A) 105 copies/μL and (B) 103 copies/μL concentration standards, respectively.
Additional file 2:
Supplementary Fig. 2. (A-C) Repeatability test of SADS-CoV for five times replicate experiments using three clinical virus-infected samples, respectively.
Additional file 3:
Supplementary Table 1. The detection results of 11 samples by quantitative real-time PCR assays and the RT-PCR system.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Cong, X., Zhu, Y., Liu, X. et al. Establishment of a recombinase polymerase amplification (RPA) fluorescence assay for the detection of swine acute diarrhea syndrome coronavirus (SADS-CoV). BMC Vet Res 18, 369 (2022). https://doi.org/10.1186/s12917-022-03465-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12917-022-03465-4