Abstract
Background
The Shimen strain of classical swine fever (CSF) virus (CSFV) causes CSF, which is mainly characterised by disseminated intravascular haemorrhage. Macrophages are an essential component of innate immunity against pathogenic microorganisms; however, the role of macrophages in CSF pathogenesis remains unclear. To illuminate the infective mechanism of CSFV, we used gene co-expression networks derived from macrophages infected with CSFV Shimen and CSFV C as well as uninfected macrophages to screen key regulatory genes, and their contributions to the pathogenesis of CSF were discussed.
Results
Vascular endothelial growth factor A (VEGFA) and plasminogen activator, urokinase (PLAU, which encodes urokinase-type plasminogen activator [uPA]) were identified as coordinated genes expressed in macrophages by gene co-expression networks. Quantitative polymerase chain reaction and western blot analysis confirmed that VEGFA and PLAU were significantly up-regulated at both the transcription and translation levels after infection. Further, confocal microscopy analysis proposed that the VEGFA and uPA proteins were temporally co-localised with the CSFV protein E2.
Conclusions
Our findings suggest that co-expression of VEGFA and PLAU in macrophages contributes to CSFV Shimen infection and serves as a significant avenue for the strain to form an inflammatory microenvironment, providing new insight into the mechanisms of CSF caused by a virulent strain.
Similar content being viewed by others
Background
The Shimen strain of classical swine fever virus (CSFV) causes an especially infectious disease in domestic pigs known as classical swine fever (CSF), which has been listed as a highly contagious disease by the World Organisation for Animal Health [1]. Acute CSF is typically accompanied by haemorrhagic lymphadenitis and diffuse haemorrhage in the skin, kidney, and other organs, often resulting in high mortality within a short period of time. The mechanism by which diffuse haemorrhage occurs in CSF is not yet fully understood.
Vascular endothelial growth factor A (VEGFA), the prototypical member of the VEGF family, plays important roles in mammalian vascular development and in diseases relating to abnormal growth of blood vessels. Tumours and inflammatory disorders often trigger pathological angiogenesis to generate a new vascular supply; detailed pathological studies have revealed the VEGFs as active participants in these processes [2]. Currently, it is accepted that VEGFs produced in tumour cells auto-stimulate neo-angiogenesis of neoplastic tissue and tumour growth [3]. Meanwhile, the role of VEGFA in different inflammatory diseases has been explored, and the blockade of its signalling is considered a protective strategy in the treatment of such diseases [4]. In recent years, increased levels of VEGFA have been observed in pro-inflammatory environments created by viral infections in humans [5, 6], further motivating study of VEGFA.
PLAU encodes urokinase-type plasminogen activator (uPA). Unlike VEGF, uPA promotes vascular permeability and angiogenesis through proteolytic degradation of the extracellular matrix, which assists tumour invasion and metastasis [7]. In the 1970s, uPA was reportedly up-regulated in Rous sarcoma virus-transformed chicken cells [8]. Later, PLAU was associated with the complex phenotype of human cancer, and high serum levels of uPA have been associated with worse overall survival rates among patients with cancer [9]. However, relatively little information is available about the role of uPA in virus–host interactions.
Macrophages are an essential component of innate immunity, with multiple functions in both inhibition and promotion of cell proliferation as well as tissue repair [10]. Despite causing acute organic damage, the CSFV Shimen strain causes no apparent cytopathic effect, but rather propagates efficiently in macrophages [11]. Whether the macrophage-mediated inflammatory response promotes the haemorrhagic mechanism of CSF is unclear. Based on analysis of a digital gene expression (DGE) profile obtained previously [11], the present study identified VEGFA and uPA as potential pathogenic factors co-expressed in CSFV Shimen-infected macrophages. The different effects of CSFV Shimen and CSFV C infection on VEGFA and uPA expression were detected. CSFV C can complete its infection cycle without any pathological symptoms [12], and it was as the control to help understand the contribution of CSFV Shimen to pathogenesis of CSF.
Methods
Experimental design
DGE analysis [13] performed on CSFV Shimen-, CSFV C-, and mock-infected macrophages has been well-described in our previous report [11]. In the present study, series cluster analysis was applied to identify significantly up- and down-regulated genes in CSFV Shimen vs CSFV C and control groups by Fisher’s exact and multiple comparison tests [14]. Further, the co-expression (Pearson correlation coefficient) of VEGFA and PLAU was calculated by Java code [15], and gene co-expression network analyses were carried out to track the interactions among the up- and down-regulated genes. Pearson correlation coefficients were compared for each pair of genes, and the significantly correlated pairs were used to construct a network [16] in which “key regulatory genes” (P-Value < 0.05) were identified to elucidate the role of macrophage status in intrinsic susceptibility to CSFV Shimen infection. Protein-protein interactions involving VEGFA were analysed using STRING (version 10.5; https://string-db.org/cgi/input.pl?sessionId=Ym91vu6hSHFN&input_page_show_search=on). Several proteins interacting with VEGFA were selected from the STRING database for Sus scrofa, one of the ELIXIR Core Data Resources. GO analysis of the proteins was carried out using the GO Term Enrichment tool in AmiGO (http://amigo1.geneontology.org/cgi-bin/amigo/term_enrichment?session_id=), the bar chart for which was constructed by OriginPro 2016 (OriginLab Corp., Northampton, MA, USA). Further tests were conducted to confirm whether the “key regulatory genes” responded to CSFV Shimen infection by inoculating the virus at an MOI (multiplicity of infection) of 5 in macrophages for 0, 12, 24, and 48 h, according to previously described methods [11].
Quantification of mRNA expression using quantitative polymerase chain reaction (qPCR)
Relative mRNA expression was determined by quantitative PCR. Specific oligonucleotide primers for each gene were as follows: VEGFA (5′-CCTTGCTGCTCTACCTCCAC-3′ and 5′- CACTCCAGACCTTCGTCGTT-3′) and PLAU (5′-CGCAAGCTGTGAAATCGTC-3′ and 5′- TTCGCTGCCGTAGTAATGG-3′). qPCR analysis of each gene was performed in triplicate, and the 2-ΔΔCt method was applied to calculate the relative expression levels.
Western blot analysis
The macrophages were lysed with RAPI buffer (Beyotime Institute of Biotechnology, Shanghai, China) and used for western blotting as previously described [11]. Primary antibodies against VEGFA (Ominimabs, Alhambra, CA, USA), uPA (Santa Cruz Biotechnology, Dallas, TX, USA), E2 (MssBio, Guangzhou, China), and β-actin (Biodragon Immunotechnologies, Beijing, China) were used in this study. β-Actin was used as a common internal control to normalise the relative transcription and translation expression of each gene.
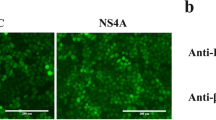
Confocal microscopy
CSFV- or mock-infected macrophages were washed in phosphate buffered saline (PBS) and fixed with methanol/acetone (1:1) for 20 min at 25 °C ± 2 °C followed by a 10-min permeabilisation with 1% Triton X-100 in PBS. After three washes in PBS, the samples were incubated with mouse anti-E2 antibody and rabbit anti-VEGFA antibody or uPA antibody for 1 h at 25 °C ± 2 °C, followed by staining with donkey anti-rabbit IgG conjugated to Alexa Fluor® 594 and donkey anti-mouse IgG conjugated to Alexa Fluor® 488 (Thermo Fisher Scientific, Waltham, MA, USA) at a 1:200 dilution for 1 h at 25 °C ± 2 °C. The nuclei in macrophages were stained with 4′,6-diamidino-2-phenylindole (DAPI). Confocal images were obtained with a laser-scanning confocal microscope (LSM 510 META; Carl Zeiss, Oberköchen, Germany).
Statistical analysis
Statistical analyses were conducted by one-way ANOVA using SPSS 16.0 (SPSS, Chicago, IL, USA), and differences with a p-value < 0.05 were considered statistically significant.
Results
VEGFA and PLAU expression are positively correlated with CSFV Shimen infection
To understand the molecular changes caused by CSFV Shimen, we used significantly up- and down-regulated genes from the DGE database to construct a co-expression network of the CSFV Shimen vs CSFV C and control groups, and a network diagram shows this in detail (see Additional file 1). The datasets used to generate the co-expression network are included in Additional file 2. In Fig. 1a, it is clear that VEGFA and PLAU appear coordinated and up-regulated in macrophages infected with CSFV Shimen. Protein–protein interaction analysis (Fig. 1b) revealed that VEGFA interacts with several proteins, including plasminogen activator inhibitor-1 (SERPINE1), thrombospondin 1 (THBS1), and hepatocyte growth factor (HGF). GO analysis showed that anomalous expression of VEGFA is related to aberrant gene function regulation groups, such as angiogenesis and positive regulation of focal adhesion assembly (Fig. 1c).
The role of VEGFA and PLAU in the co-expression network of cells infected by CSFV Shimen. (a) The co-expression network shows that VEGFA and PLAU are up-regulated in CSFV Shimen-infected cells compared to their levels in CSFV C-infected and mock-infected cells. (b) protein–protein interaction analysis of VEGFA. Each network node represents all proteins produced by a single protein-coding gene locus, and the edges represent protein-protein associations, which means proteins together contribute to shared functions. The meaning of the network edge is confidence, and the thickness of the line indicates the strength of data supports, which edge confidence is divided into 3 levels: medium (0.400), high (0.700), and highest (0.900). (c) GO analysis shows that aberrant expression of VEGFA is related to anomalous regulation of gene function groups
Up-regulation of VEGFA and PLAU by CSFV Shimen infection in macrophages
As shown in Fig. 2a, DGE analysis showed VEGFA and PLAU to be significantly up-regulated in CSFV Shimen-infected macrophages compared to those in CSFV C-infected and control macrophages. qPCR confirmed infection with either CSFV Shimen or CSFV C in a time-dependent manner [11] (Fig. 2b). VEGFA and PLAU mRNA expression were measured by qPCR throughout the 48 h course of CSFV infection, and significant differences (p-value < 0.05) were observed between the 0 and 48 h groups for CSFV Shimen infection, suggesting a VEGFA and PLAU expression pattern similar to that predicted by DGE analysis (Fig. 2c, d).
VEGFA and PLAU mRNA expression are positively correlated with CSFV Shimen infection. (a) DGE analysis shows that VEGFA and PLAU are up-regulated in CSFV Shimen-infected cells compared with levels in CSFV C-infected and mock-infected cells. (b) qPCR analysis of CSFV Shimen and C strain proliferation in macrophages. (c) qPCR analysis of VEGFA mRNA expression. (d) qPCR analysis of PLAU mRNA expression. Significant up-regulated (p-value < 0.05) on VEGFA and PLAU were observed between the 0 and 48 h groups for CSFV Shimen infection in qPCR analysis. Three independent qPCR experiments always obtained consistent conclusion, and one of the results was shown
CSFV Shimen infection induces VEGFA and uPA expression
Western blot analysis confirmed the increased expression of VEGFA and uPA in macrophages after CSFV Shimen infection. E2, a structural protein in CSFV, indicated the extent of CSFV replication in cell samples. VEGFA and uPA expression in macrophages was induced in a time-dependent manner upon treatment with CSFV Shimen, which was concurrent with the increased expression of E2 48 h after CSFV Shimen infection (Fig. 3).
VEGFA and uPA temporally colocalise with CSFV Shimen E2
Confocal microscopy was used to assess whether VEGFA, uPA, and the viral protein E2 were temporally and/or spatially co-localised in the cultured macrophages. Macrophages were treated with fluorescent labels targeting CSFV Shimen, E2, and VEGFA or uPA. Cellular localisation was tracked 24 h after CSFV Shimen infection. Temporal co-localisation of E2 and VEGFA was observed in the CSFV Shimen-infected cells, and the abundance of VEGFA in macrophages was significantly enhanced during the course of CSFV Shimen infection compared to that in uninfected controls (Fig. 4). Similar results were observed for E2 and uPA (Fig. 4). These findings suggest that VEGFA and uPA act as inflammatory cytokines in the invasion of CSFV Shimen into macrophages.
Temporal colocalisation of CSFV E2 with VEGFA and uPA in CSFV Shimen-infected macrophages. (a) Co-localization of CSFV E2 protein with VEGFA in macrophages infected with CSFV Shimen. (b) Co-localization of CSFV E2 protein with uPA in macrophages infected with CSFV Shimen. CSFV E2 antibody fluorescent signals are shown in green, VEGFA and uPA antibody signals in red, and nuclear signals in blue
Discussion
As a virulent strain, CSFV Shimen typically causes diffuse haemorrhagic symptoms in CSF; this is different from the CSFV C strain, which can infect pigs and produce no pathological symptoms [17]. Comparative analysis of molecular changes caused by the two strains in host cells could contribute significantly to the understanding of the related pathological mechanisms. Based on our results, we propose that coordinated expression of VEGFA and PLAU plays an important role in the inflammatory response of macrophages to CSFV Shimen infection.
This study indicated that CSFV Shimen infection triggered VEGFA responses in macrophages at both the transcription and translation levels. VEGFA recruitment by macrophages plays a crucial role in inducing inflammatory neovascularisation for pathological haemangiogenesis and lymphangiogenesis [18]. Assuming a link between angiogenesis and inflammation, the role of VEGFA in viral infectious diseases, especially in haemorrhagic lesions, has been explored. A previous report by Jones et al. revealed that varicella zoster viral infection leads to significantly increased VEGFA levels in cerebrovascular cells [5]. Herpes simplex virus 1 directly induced vascularisation of the cornea by up-regulation of VEGFA expression [19], and the VEGF trap, as an angiogenesis inhibitor, represented a functional approach to mitigating corneal neovascularisation and controlling ocular lesions [20]. A common feature of viral haemorrhagic fevers is viral entry into macrophages and dendritic cells and consequent cytopathic effects. Clinical symptoms of Crimean-Congo haemorrhagic fever (CCHF) include acute viral fever, ecchymosis, and thrombocytopenia, and a recent study showed significantly increased VEGFA levels in patients with CCHF [21]. The acute form of CSF is characterised by high fever and skin haemorrhages approximately two weeks after onset of fever, which indicate haemorrhagic pathological alterations developed in vivo [22]. Interestingly, we previously observed VEGFC up-regulation in swine umbilical vein endothelial cells infected with CSFV Shimen [23]. The VEGF family is known to play a central role in the breakdown of clots, angiogenesis, and increased vascular permeability [24]. Our data support the involvement of the VEGF family in the pathological mechanisms of acute CSF and its contribution to haemorrhagic lesions caused by virulent strains of CSFV.
The present study indicated that PLAU expression was significantly up-regulated in macrophages infected by CSFV Shimen. uPA plays a vital role in maintaining capillary integrity and regulating vascular permeability and participates in many important processes, including inflammation [7]. A previous study reported uPA up-regulation in HIV-infected macrophages; thus, the protein could aid viral fusion or be an endogenous component critical to HIV infection of macrophages [25]. Additionally, uPA expression in macrophages is believed to contribute to cerebral injury in patients with HIV [26]. Generally, when tissues are challenged by pathogens, macrophages are activated and produce large numbers of pro-inflammatory mediators that kill invading organisms and activate adaptive immunity [27]. However, consistently with previous studies, we believe that infection of macrophages by virulent strains of CSFV directly produces a pro-inflammatory environment leading to prolonged capillary inflammation and vasculitis.
VEGF, which is up-regulated by CSFV Shimen infection, is reportedly the prime factor in the initiation of angiogenesis to increase vascular permeability. Additionally, VEGF reportedly induces uPA activation on the surfaces of endothelial cells to provide further angiogenesis-modulating stimuli [28]. The uPA receptor (uPAR) may be a vehicle by which crucial VEGFA-induced proteolytic factors increase vascular permeability [29]. Consistently with this, VEGF led to the redistribution of uPAR/integrin α5β1 complexes to focal adhesions on the surfaces of endothelial cells, thereby enabling matrix degradation and cell invasion [30]. Furthermore, active uPA increases vascular permeability by increasing VE-cadherin degradation [31]. CSFV may produce its characteristic tissue lesions by targeting uPAR and integrin interaction sites independently of VEGF. Consistently, integrin β3 has is also up-regulated by CSFV infection in host cell lines [32].
Conclusions
In conclusion, we showed that VEGFA and PLAU were significantly up-regulated after CSFV Shimen infection. Our results suggest a mechanism of macrophage-mediated inflammatory response to virulent CSFV infections that may explain the as yet indeterminate cause of diffuse haemorrhage in CSF, a highly contagious disease of commercial livestock with a high mortality rate.
Abbreviations
- CSF:
-
Classical swine fever
- CSFV:
-
Classical swine fever virus
- DGE:
-
Digital gene expression
- MOI:
-
Multiplicity of infection
- PLAU:
-
Plasminogen activator, urokinase
- uPA:
-
urokinase-type plasminogen activator
- uPAR:
-
uPA receptor
- VEGFA:
-
Vascular endothelial growth factor A
References
Postel A, Meyer D, Petrov A, Becher P. Recent emergence of a novel porcine pestivirus: interference with classical swine fever diagnosis? Emerg Microbes Infec. 2017;6(4):e19.
JA N, Dvorak AM, Dvorak HF. VEGF-A and the induction of pathological angiogenesis. Annu Rev Pathol-Mech. 2007;2(2):251.
Claesson-Welsh L, Welsh M. VEGFA and tumour angiogenesis. J Intern Med. 2013;273(2):114–27.
Argaw AT, Asp L, Zhang J, Navrazhina K, Pham T, Mariani JN, Mahase S, Dutta DJ, Seto J, Kramer EG, Ferrara N, Sofroniew MV, John GR. Astrocyte-derived VEGF-A drives blood-brain barrier disruption in CNS inflammatory disease. J Clin Invest. 2012;122(7):2454–68.
Jones D, Neff CP, Palmer BE, Stenmark K, Nagel MA. Varicella zoster virus-infected cerebrovascular cells produce a proinflammatory environment. Neurol Neuroim Neuroin. 2017;4(5):e382.
Sessa R, Chen L. Lymphangiogenesis: a new player in herpes simplex virus 1-triggered T-cell response. Immunol Cell Biol. 2017;95(1):5–6.
Nassar T, Yarovoi S, Fanne RA, Waked O, Allen TC, Idell S, Cines DB, Higazi AA. Urokinase plasminogen activator regulates pulmonary arterial contractility and vascular permeability in mice. Am J Resp Cell Mol. 2011;45(5):1015.
Sudol M. From Rous sarcoma virus to plasminogen activator, src oncogene and cancer management. Oncogene. 2011;30(27):3003–10.
RW S, Nielsen HJ, Christensen IJ, Thorlacius-Ussing O, Sørensen S, Danø K, Brünner N. Plasma urokinase receptor levels in patients with colorectal cancer: relationship to prognosis. J Natl Cancer I. 1999;91(10):869.
Wang N, Liang H, Zen K. Molecular mechanisms that influence the macrophage M1–M2 polarization balance. Front Immunol. 2014;5:614.
Ning P, Hu C, Li X, Zhou Y, Hu A, Zhang Y, Gao L, Gong C, Guo K, Zhang X, Zhang Y. Classical swine fever virus Shimen infection increases p53 signaling to promote cell cycle arrest in porcine alveolar macrophages. Oncotarget. 2017;8(34):55938.
Edwards S, Fukusho A, Lefévre PC, Lipowski A, Pejsak Z, Roehe P, Westergaardf J. Classical swine fever: the global situation. Vet Microbiol. 2000;73(2–3):103–19.
Audic S, Claverie JM. The significance of digital gene expression profiles. Genome Res. 1997;7(10):986–95.
Ramoni MF, Sebastiani P, Kohane IS. Cluster analysis of gene expression dynamics. P Natl Acad of Sci USA. 2002;99(14):9121.
PujanaMA HJD, Starita LM, Stevens KN, Tewari M, Ahn JS, Rennert G, Moreno V, Kirchhoff T, Gold B, Assmann V, Elshamy WM, Rual JF, Levine D, Rozek LS, Gelman RS, Gunsalus KC, Greenberg RA, Sobhian B, Bertin N, Venkatesan K, Ayivi-Guedehoussou N, Solé X, Hernández P, Lázaro C, Nathanson KL, Weber BL, Cusick ME, Hill DE, Offit K, Livingston DM, Gruber SB, Parvin JD, Vidal M. Network modeling links breast cancer susceptibility and centrosome dysfunction. Nat Genet. 2007;39(11):1338–49.
WW X, Han MJ, Chen D, Chen L, Guo Y, Willden A, Liu DQ, Zhang HT. Genome-wide search for the genes accountable for the induced resistance to HIV-1 infection in activated CD4+T cells: apparent transcriptional signatures, co-expression networks and possible cellular processes. BMC Med Genet. 2013;6:15.
Postel A, Austermann-Busch S, Petrov A, Moennig V, Becher P. Epidemiology, diagnosis and control of classical swine fever: recent developments and future challenges. Transbound Emerg Dis. 2017;65(1):248–61.
Cursiefen C, Chen L, Borges LP, Jackson D, Cao J, Radziejewski C, Patricia AD, Dana MR, Wiegand SJ, Streilein WJ. VEGF-A stimulates lymphangiogenesis and hemangiogenesis in inflammatory neovascularization via macrophage recruitment. J Clin Invest. 2004;113(7):1040–50.
Wuest TR, Carr DJ. VEGF-A expression by HSV-1–infected cells drives corneal lymphangiogenesis. J Exp Med. 2010;207(1):101–15.
Suryawanshi A, Veigaparga T, Reddy PB, Rajasagi NK, Rouse BT. IL-17A differentially regulates corneal vascular endothelial growth factor (VEGF)-a and soluble VEGF receptor 1 expression and promotes corneal angiogenesis after herpes simplex virus infection. J Immunol. 2012;188(7):3434–46.
Sefikogullari M, Kaya A, Aydin H, Sancakdar E, Celik VK, Bagci G. Increased levels of VEGF-A and HIF-1α in Turkish children with Crimean-Congo hemorrhagic fever. J Arthropod-Borne Di. 2017;11(1):19–26.
Chander V, Nandi S, Ravishankar C, Upmanyu V, Verma R. Classical swine fever in pigs: recent developments and future perspectives. Anim Health Res Rev. 2014;15(1):87–101.
Ning P, Zhang Y, Guo K, Chen R, Liang W, Lin Z, Li H. Discovering up-regulated VEGF-C expression in swine umbilical vein endothelial cells by classical swine fever virus Shimen. Vet Res. 2014;45(1):48.
FM G, Popel AS. Systems biology of vascular endothelial growth factors. Microcirculation. 2018;15(8):715–38.
MA H, Steigbigel RT, Morrison SA. A role for urokinase-type plasminogen activator in human immunodeficiency virus type 1 infection of macrophages. J Virol. 1996;70(7):4451–6.
Nebuloni M, Cinque P, Sidenius N, Ferri A, Lauri E, Omodeo-Zorini E, Zerbi P, Vago L. Expression of the urokinase plasminogen activator receptor (upar) and its ligand (upa) in brain tissues of human immunodeficiency virus patients with opportunistic cerebral diseases. J Neuro-Oncol. 2009;15(1):99–107.
Wynn TA, Chawla A, Pollard JW. Macrophage biology in development, homeostasis and disease. Nature. 2013;496:445–55.
GW P, Breuss JM, Steurer S, Mihaly J, Binder BR. Vascular endothelial growth factor (VEGF) induces rapid prourokinase (pro-uPA) activation on the surface of endothelial cells. Blood. 2004;103(3):955–62.
Breuss JM, Uhrin P. VEGF-initiated angiogenesis and the uPA/uPAR system. Cell Adhes Migr. 2012;6(6):535–40.
Alexander RA, Prager GW, Mihaly-Bison J, Uhrin P, Sunzenauer S, Binder BR, Schütz GJ, Freissmuth M, Breuss JM. VEGF-induced endothelial cell migration requires urokinase receptor (uPAR)-dependent integrin redistribution. Cardiovasc Res. 2012;94(1):125.
Navaratna D, Menicucci G, Maestas J, Srinivasan R, McGuire P, Das A. A peptide inhibitor of the urokinase/urokinase receptor system inhibits alteration of the blood-retinal barrier in diabetes. FASEB J. 2008;22(9):3310.
Li W, Wang G, Liang W, Kang K, Guo K, Zhang Y. Integrin β3 is required in infection and proliferation of classical swine fever virus. PLoS One. 2014;9(10):e110911.
Acknowledgements
The authors thank NovelBio, Ltd., Co. for their excellent technical assistance on gene co-expression network and Wcgene Biotech Shanghai for their excellent technical assistance on primer design.
Funding
This study was supported by the National Natural Science Foundation of China (31470535) in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript, and supported by the Fundamental Research Funds for the Central Universities and the Innovation Fund of Xidian University in the interpretation of data.
Availability of data and materials
All data generated or analysed during this study are included in this published article [and its supplementary information files].
Author information
Authors and Affiliations
Contributions
XG: carried out qPCR and western blot analysis, participated in drafted the manuscript and bioinformatic analysis. AH: carried out qPCR and western blot analysis, participated in drafted the manuscript. XL: carried out confocal microscopy. JH: participated in drafted the manuscript and data analysis. ZW: carried out cell culture and virus inoculation. XZ: participated in drafted the manuscript and data analysis. PN: made substantial contributions to conception and design, acquisition of data, analysis and interpretation of data; performed the statistical investigations and finalized the manuscript. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional files
Additional file 1:
Co-expression network of CSFV Shimen-infected macrophages. (JPG 2474 kb)
Additional file 2:
Datasets used to generate co-expression network. (XLS 32 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Gong, X., Hu, A., Li, X. et al. Coordinated expression of vascular endothelial growth factor A and urokinase-type plasminogen activator contributes to classical swine fever virus Shimen infection in macrophages. BMC Vet Res 15, 82 (2019). https://doi.org/10.1186/s12917-019-1826-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12917-019-1826-8