Abstract
Background
There are limited data available on macrolide-lincosamide-streptogramin (MLS) resistance of Staphylococcus aureus (S. aureus) and coagulase-negative staphylococci (CoNS) from bovine milk in China. To address this knowledge gap, MLS resistance was determined in 121 S. aureus and 97 CoNS isolates. Minimum inhibitory concentrations (MICs) of MLS antibiotics were determined by an agar dilution method, while differentiation of MLS phenotypes was performed by a double-disc diffusion test. MLS resistance genotypes were determined by PCR for corresponding resistance genes.
Results
Forty (33.1 %) S. aureus and 65 (67.0 %) CoNS were resistant to erythromycin, whereas all 218 isolates were susceptible to quinupristin/dalfopristin. Among 40 erythromycin-resistant (ER-R) S. aureus and 65 ER-R CoNS isolates, 38 S. aureus and 40 CoNS isolates exhibited the inducible MLS (iMLS) resistance phenotype and 2 S. aureus and 20 CoNS isolates expressed the constitutive MLS resistance (cMLS) phenotype. At the same time, 5 CoNS isolates exhibited resistance to erythromycin but susceptibility to clindamycin (the MS phenotype). An inactivating enzyme gene lnu(A), methylase genes erm(C) and erm(B), efflux genes msr(A)/msr(B), a phosphotransferase gene mph(C), an esterase gene ere(A) and the streptogramin resistance determinant vga(A) were detected individually or in combinations. Among them, genes lnu(A), erm(C) and mph(C) predominated. The ereA gene was detected for the first time in staphylococci of bovine milk origin. Resistance genes also existed in erythromycin-susceptible isolates.
Conclusions
Our study demonstrated a high level of resistance to MLS antibiotics in staphylococci from bovine mastitic milk, especially with a high rate of the iMLS phenotype in S. aureus isolates. These data suggest that MLS antibiotics should be used judiciously to treat or prevent bovine mastitis caused by staphylococci.
Similar content being viewed by others
Background
Bovine mastitis is the most costly disease for the dairy industry worldwide. Although a wide variety of pathogens have been isolated as causative agents of this disease, Staphylococcus aureus (S. aureus) is considered as one of the most important pathogens due to its resistance to certain antibiotics and its propensity to recur chronically. Recently, coagulase-negative staphylococci (CoNS) have been considered as opportunistic pathogens that cause bovine mastitis in many countries and could be therefore described as emerging mastitis pathogens [1, 2]. Increasing attention has been paid to CoNS in both subclinical and clinical mastitis cases throughout the world [3, 4]. Macrolide-lincosamide-streptogramin (MLS) antibiotics, including erythromycin, clindamycin and spiramycin, are frequently used for treatment of bovine mastitis [5, 6]. Thus, results from an in vitro susceptibility testing are an important tool to guide a veterinarian in selecting the most efficacious antimicrobial agent(s) for therapeutic and prophylactic intervention.
Three mechanisms are mainly responsible for acquiring resistance to MLS antibiotics in staphylococci: (1) target site modifications by methylation or mutation; (2) active efflux of antibiotics; or (3) inactivation of antibiotics. The first mechanism includes target site modifications by a methylase encoded by one or more of the erm genes, methylating 23S rRNA and thereby altering binding sites for MLS antibiotics [7]. Phenotypically, this resistance appears either inducible (resistant to 14- and 15-membered macrolides and susceptible to 16-membered macrolides, lincosamides and streptogramin B) or constitutive (resistant to all forms of these antibiotics) [8]. The second mechanism involves a macrolide efflux pump encoded by msr(A) and/or msr(B) genes. This pump protein belongs to the ABC transporter family and exports 14-membered macrolides and streptogramin B antibiotics from bacterial cells, while lincosamide and streptogramin A antibiotics remain unaffected (the MS phenotype) [9]. The third mechanism encompasses several enzymes. A lincosamide nucleotidyltransferase encoded by the lnu(A) gene confers resistance only to lincosamides and has been detected in CoNS isolates from bovine mastitis [10]. Esterases encoded by ere(A)/(B) genes hydrolyze the lactone ring of the macrocyclic nucleus [11]. Furthermore, vga(A)/(B) genes have been characterized as a determinant of streptogramin A resistance [11]. Finally, the macrolide phosphotransferase C encoded by the mph(C) gene inactivates some macrolide antibiotics and has been detected in CoNS isolated from bovine subclinical mastitis [12].
The reported resistance of S. aureus and CoNS isolated from bovine mastitis to MLS antibiotics in different countries was generally low [12, 13]. Meanwhile, there was a paucity of data regarding MLS-resistance phenotypes and genotypes of S. aureus and CoNS isolated from bovine mastitis in China, except one study [5]. The objective of this study was to determine the MLS resistance phenotypes and genotypes of 121 S. aureus and 97 CoNS isolates from mastitic milk from dairy farms of the Shaanxi province in Northwestern China.
Methods
Bacterial isolates
Milk samples were obtained from dairy cows with clinical mastitis under the ethical approval granted by the College of Animal Science and Technology, the Northwest Agriculture and Forestry (A&F) University (Permit Number: NWAFU1008), as described previously [14]. A total of 121 coagulase-positive S. aureus (CoPSA) and 97 coagulase-negative staphylococci (CoNS) were used in this study. CoNS species were identified by sequencing analyses based on sodA and/or gap genes [14]. Ninety-seven CoNS isolates encompassed 9 CoNS species: Staphylococcus haemolyticus (S. haemolyticus, n = 31), Staphylococcus aureus (S. aureus, n = 28), Staphylococcus chromogenes (S. chromogenes, n = 11), Staphylococcus sciuri (S. sciuri, n = 9), Staphylococcus epidermidis (S. epidermidis, n = 7), Staphylococcus simulans (S. simulans, n = 5), Staphylococcus hyicus (S. hyicus, n = 3), Staphylococcus warneri (S. warneri, n = 2) and Staphylococcus saprophyticus (S. saprophyticus, n = 1).
Antibiotic susceptibility testing
Minimum inhibitory concentrations (MICs) of antimicrobial agents, including 14-membered (erythromycin), 15-membered (azithromycin), 13- and 15-membered mixture (tulathromycin) and 16-membered (tylosin and spiramycin) macrolides, lincosamides (clindamycin) and streptogramins (quinupristin/dalfopristin) were determined using an agar dilution method. Clindamycin, azithromycin, tulathromycin and spiramycin were purchased from Dalian Meilun Biology Technology Co., Ltd. (Dalian, China). Tylosin was purchased from Shanghai Kai Yang Biotechnology Co., Ltd. (Shanghai, China). Erythromycin was bought from Sigma-Aldrich (Beijing, China) and quinupristin/dalfopristin was obtained from Santa Cruz biotechnology, Inc. (Shanghai, China). The approved veterinary specific CLSI MIC breakpoints of erythromycin and clindamycin are ≥ 8 μg/mL and 4 μg/mL, respectively [15]. MIC breakpoint for spiramycin (≥32 μg/mL) was adopted from the Swedish Antibiotic Utilisation and Resistance in Human Medicine (SWEDRES) and Swedish Veterinary Antimicrobial Resistance Monitoring (SVARM) system (SWEDRES-SVARM) [16]. The MIC breakpoint for tylosin (≥20 μg/mL) was based on the Veterinary Antimicrobial Decision Support (VADS) according to a previous study [5]. There were no veterinary specific CLSI, VADS or SWEDRES-SVARM-approved breakpoints for azithromycin and quinupristin-dalfopristin. Therefore, we used a human specific CLSI document M100-S21 [17] as a reference to determine breakpoints for azithromycin (≥8 μg/mL) and quinupristin-dalfopristin (≥4 μg/mL). In addition, there was no CLSI, VADS or SVARM-approved breakpoint for tulathromycin. The standard reference strain S. aureus ATCC 29213 served as a quality control in every test run.
Detection of MLS resistance phenotypes
In order to differentiate different types of resistance phenotype for erythromycin-resistant (ER-R) isolates, a double-disk diffusion test (D test) was performed with erythromycin (15 μg/disc) and clindamycin (2 μg/disc), following the procedure recommended by CLSI [17]. Staphylococcal isolates showing resistance to erythromycin (zone size ≤13 mm) but being sensitive to clindamycin (zone size ≥21 mm) and producing a D-shaped zone of inhibition around clindamycin with flattening towards erythromycin disc was defined as having an inducible type of MLS resistance (D+, iMLS). In addition, resistance to erythromycin (zone size ≤13 mm) as well as to clindamycin (zone size ≤14 mm) indicated a constitutive type of MLS resistance (cMLS). Staphylococcal isolates showing resistance to erythromycin (zone size ≤13 mm) while being sensitive to clindamycin (zone size ≥21 mm) with no blunting zone were classified as the MS phenotype.
Detection of MLS resistance genotypes
Staphylococcal isolates were incubated in the Brain Heart Infusion broth (Oxoid) at 37 °C for 16-18 h. Then, bacteria were harvested by centrifugation. Plasmid and chromosome DNA of bacterial isolates were extracted using a commercial DNAout kit (Tiandz Inc., Beijing, China) as described previously [14]. The screening of MLS resistance determinants including methylase genes erm(A), erm(B) and erm(C); phosphotransferase genes mph(A) and mph(C); lincosamide nucleotidyltransferase genes lnu(A) and lnu(B); erythromycin esterase genes ere(A) and ere(B); streptogramin resistance genes vga(A), vga(B), vgb(A) and vgb(B), and the macrolide efflux determinants msr(A)/msr(B) was performed by PCR using the specific primers as described in previous studies [11, 12, 18–20]. PCR products were randomly selected and sequenced to ensure specificity and accuracy. Sequence comparisons were performed using the Basic Local Alignment Search Tool (BLAST) program (http://www.ncbi.nlm.nih.gov/BLAST/).
Results and discussion
Characterization of MLS resistance phenotypes in erythromycin-resistant isolates and MIC distribution
Of the 121 coagulase-positive S. aureus (CoPSA) isolates, 40 were resistant to at least one MLS antibiotic. Thirty-eight out of 40 ER-R CoPSA (95 %) isolates exhibited iMLS phenotypes, whereas only 2 isolates expressed cMLS phenotypes, with no MS phenotype. The MICs of the macrolides and lincosamides antibiotics for the 40 ER-R CoPSA isolates are summarized in Table 1. Among ER-R CoPSA, 100 %, 100 %, 80 %, 17.5 % and 5 % of isolates were resistant to erythromycin, azithromycin, spiramycin, tylosin and clindamycin, respectively. The MIC50 and MIC90 values of 14-membered, 15-membered macrolides and 16-membered macrolide spiramycin were ≥128 μg/mL, while the MIC50 values of 16-membered macrolides tylosin and lincosamides were in the susceptible range. No isolate expressed resistance to quinupristin/dalfopristin (MICs ≤ 1 μg/mL).
Among 97 CoNS isolates, 65 isolates exhibited MLS resistance phenotypes. Among them, 40 showed the iMLS phenotype and 20 expressed the cMLS phenotype, while 5 exhibited the MS phenotype. The MICs of the antimicrobial agents tested are summarized in Table 2. Eighteen isolates with cMLS phenotypes exhibited a high-level of resistance to erythromycin, clindamycin, azithromycin, spiramycin and tylosin with MIC values of ≥256 μg/mL. Furthermore, 1 S. haemolyticus with the iMLS phenotype exhibited MICs ≥256 μg/mL for erythromycin and azithromycin while MICs for spiramycin and tylosin were 64 μg/mL and 128 μg/mL, respectively. In addition, 39 CoNS isolates with the iMLS phenotype showed a complete cross-resistance to erythromycin and azithromycin with MICs of ≥256 μg/mL. However, MIC values of 16-membered macrolides tylosin (2-8 μg/mL) and spiramycin (2-16 μg/mL) were in the susceptible ranges.
The iMLS phenotype rate of ER-R S. aureus (38/40) and ER-R CoNS (40/65) isolates was much higher in this study than previous studies, underlining the importance of routine screening of bovine S. aureus and CoNS isolates for inducible resistance phenotypes. Wang et al. [5] reported that the inducible MLS resistance phenotype was detected in 38 out of 72 S. aureus isolates from cows with clinical mastitis in Inner Mongolia of China. In another study, only 3 isolates with the iMLS phenotype were found out of 22 ER-R CoNS in Germany [12]. The reason for the higher rate of the iMLS phenotype in our study is not clear.
Characterization of MLS resistance genotypes in erythromycin-resistant isolates
Among 40 ER-R CoPSA isolates, the most dominant resistance gene was erm(C) (38/40), followed by the mph(C) (27/40), erm(B) (14/40), ere(A) (14/40) and vga(A) (10/40) (Table 3). The msr(A)/msr(B) genes were found in 6 isolates, which were all positive for erm(C) or erm(B) genes and displayed iMLS phenotypes (Table 4). Considering the 65 ER-R CoNS isolates, msr(A)/msr(B) genes were present in 51 isolates, erm(C) in 46, erm(B) in 23, mph(C) in 25, vga(A) in 23 and ere(A) in 9 isolates. At least one of the MLS resistance genes was detected in each ER-R isolate. The simultaneous presence of two or more MLS antibiotic resistance genes was also detected (Table 4). The simultaneous presence of two or more macrolide resistance genes in the same S. aureus or CoNS isolate is well-known and has been reported previously for S. aureus or CoNS isolates from bovine mastitis [5, 12, 21].
Correlation between the MIC values of MLS resistance phenotypes and phenotypes
The possible relationship between MLS resistance phenotypes and genotypes was also explored. Among the 40 ER-R CoPSA isolates, 8 isolates with iMLS phenotypes were sensitive to 16-membered macrolides spiramycin and 32 isolates with iMLS phenotypes were sensitive to tylosin. Those isolates were all erm(B) and/or erm(C) positive. As for the 65 ER-R CoNS isolates, 4 erm(B) and/or erm(C) positive isolates with the MS phenotype and 28 erm(B) and/or erm(C) positive isolates with the iMLS phenotype were sensitive to 16-membered macrolides spiramycin and tylosin, respectively. Furthermore, 1 S. warneri with the MS phenotype and 9 CoNS isolates with the iMLS phenotype were also sensitive to 16-membered macrolides spiramycin and tylosin. Those 10 isolates were negative for erm genes but positive for other MLS resistance genes, such as msr(A)/(B), mph(C), ere(A), lnu(A) or vga(A). In general, erm-carrying ER-R S. aureus and CoNS isolates with iMLS or MS phenotypes possessed a high degree of resistance to erythromycin, azithromycin and clindamycin (inducible), while having a low rate of resistance to 16-membered macrolides tylosin and/or spiramycin.
It has been reported that the lactone rings of 16- and 14-membered macrolides adopt distinctly diverse conformations, thereby enabling the former compounds to avoid steric hindrance with the nucleotide A2058 mutation in E. coli [22]. Such a mechanism may be also responsible for differential sensitivity to 16- and 14-membered macrolides in staphylococci. In addition, differential effects of 14 and 15-membered macrolides versus 16-membered macrolides on expression of erm genes could contribute to our results. Expression of erm genes can be either inducible or constitutive. Inducible erm genes expression is controlled at a post-transcriptional level, which involves a structure upstream from the erm gene composing of a leader peptide and a series of inverted repeats. Formation of different mRNA secondary structures in this regulatory region in the presence or absence of an inducer allows or prevents the translation of the erm gene transcripts [8]. Only 14- and 15-membered macrolide can induce erm expression, while 16-membered macrolides, lincosamides, or streptogramins are not able to induce erm gene expression [8]. However, why 10 CoNS without the erm gene were also sensitive to 16-membered macrolides spiramycin and tylosin in this study is unclear and will be further studied. In addition, previous studies have shown that erm gene expression can quickly and irreversibly switch from inducible expression to constitutive expression under selective pressure due to the structural alterations (sequence deletions of varying length, duplications and mutations), which then renders the respective staphylococcal isolate resistant to all 14-, 15-, and 16-membered macrolides, lincosamides and streptogramin B antibiotics [23–25]. Therefore, different conformational rearrangements in the mRNA structure or structural alterations (deletions, duplications or mutations) in the upstream regulatory region of erm genes could be one of the plausible reasons of our isolates and such resistance mechanism will be further studied.
Other resistance genes may also play a role in the sensitivity to 16-membered macrolides. For example, msr(A)/msr(B) genes in CoPSA isolates. These genes encode an inducible efflux pump which is an ABC transporter. 14- and 15-membered macrolides are inducers and substrates for the pump, while clindamycin is neither an inducer nor a substrate [8]. In our research, all 6 msr(A)/msr(B)-carrying CoPSA isolates were also erm(B) and/or erm(C) genes positive. These isolates had the iMLS phenotype and exhibited MICs of ≥256 μg/mL for erythromycin while susceptible to 16-membered macrolides spiramycin and/or tylosin. However, the situation is much complicated for 51 msr(A)/msr(B)-carrying CoNS isolates. Among them, 31 (17 S. haemolyticus, 7 S. aureus, 4 S. epidermidis and 3 S. chromogenes) had the iMLS phenotype, 15 (9 S. haemolyticus, 2 S. simulans, 2 S. hyicus, 1 S. epidermidis and 1 S. chromogenes) had the cMLS phenotype and 5 (2 S. warneri, 1 S. sciuri, 1 S. aureus and 1 S. saprophyticus) had the MS phenotype.
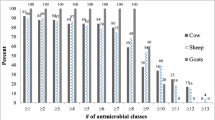
Characterization of MLS resistance genotypes in erythromycin-susceptible isolates
Among 81 erythromycin-susceptible (ER-S) CoPSA isolates, 79 isolates were positive for lnu(A), 69 for erm(C), 47 for mph(C), 66 for erm(B), 64 for msr(A)/(B), 20 for ere(A) and 10 for vga(A) genes (Table 5), but all were susceptible to the corresponding antibiotics (erythromycin, azithromycin, spiramycin, tylosin or clindamycin) in the antibiotic susceptibility testing, due to unknown reasons. As for 32 ER-S CoNS isolates, 7, 9, 20, 11, 7 and 9 CoNS isolates harbored erm(B), erm(C), msr(A)/(B), mph(C), ere(A), vga(A) genes, respectively (Table 5). Furthermore, the lincosamide nucleotidyltransferase gene, lnu(A), was detected in all ER-R S. aureus, ER-R CoNS isolates, ER-S CoNS and 79 ER-S CoPSA isolates (Table 3; Table 5). The presence of lnu(A) among staphylococcal isolates from bovine mastitis has been reported [5, 10, 12]. The lnu(A) gene is mainly carried by small rolling-circle plasmids and it mediates only a low-level of resistance to the lincosamide pirlimycin [10]. The ere(A) gene was detected for the first time in staphylococci of bovine milk origin. Our results are in agreement with previous studies which detected erm(C), lnu(A), mph(C) or erm(A) genes in susceptible S. aureus or CoNS isolates [12, 26, 27]. When Martineau et al. [26] subcultured 4 erythromycin susceptible strains harboring the erm(C) gene with increasing concentration of the antibiotic, they found that those susceptible strains all become resistant. Thus, we need to be vigilant when we use MLS antibiotics on dairy farms.
Conclusions
In summary, a very high rate of iMLS (95 %, 38/40) phenotype of ER-R S. aureus and MLS resistance phenotype (67 %, 65/97) of CoNS isolates from milk of mastitic cows was found in this study in comparison with previous studies, presumably due to extensive use of MLS antibiotics in dairy cows in our region. Our results suggest that MLS antibiotics should be used judiciously for therapeutic and prophylactic intervention of staphylococci infection.
Abbreviations
- cMLS:
-
constitutive MLS resistance phenotype
- CoNS:
-
Coagulase-negative staphylococci
- CoPSA:
-
coagulase-positive Staphylococcus aureus
- ER-R:
-
erythromycin-resistant
- ER-S:
-
erythromycin-susceptible.
- iMLS:
-
inducible MLS resistance phenotype
- MIC:
-
Minimal inhibitory concentration
- MLS:
-
macrolide-lincosamide-streptogramin
References
Pyorala S, Taponen S. Coagulase-negative staphylococci-emerging mastitis pathogens. Vet Microbiol. 2009;134(1-2):3–8.
Taponen S, Pyorala S. Coagulase-negative staphylococci as cause of bovine mastitis-Not so different from Staphylococcus aureus? Vet Microbiol. 2009;134(1-2):29–36.
Frey Y, Rodriguez JP, Thomann A, Schwendener S, Perreten V. Genetic characterization of antimicrobial resistance in coagulase-negative staphylococci from bovine mastitis milk. J Dairy Sci. 2013;96(4):2247–57.
Sawant AA, Gillespie BE, Oliver SP. Antimicrobial susceptibility of coagulase-negative staphylococcus species isolated from bovine milk. Vet Microbiol. 2009;134(1-2):73–81.
Wang Y, Wu CM, Lu LM, Ren GWN, Cao XY, Shen JZ. Macrolide-lincosamide-resistant phenotypes and genotypes of Staphylococcus aureus isolated from bovine clinical mastitis. Vet Microbiol. 2008;130(1-2):118–25.
McDougall S, Agnew KE, Cursons R, Hou XX, Compton CRW. Parenteral treatment of clinical mastitis with tylosin base or penethamate hydriodide in dairy cattle. J Dairy Sci. 2007;90(2):779–89.
Poehlsgaard J, Douthwaite S. The bacterial ribosome as a target for antibiotics. Nat Rev Microbiol. 2005;3(11):870–81.
Depardieu F, Podglajen I, Leclercq R, Collatz E, Courvalin P. Modes and modulations of antibiotic resistance gene expression. Clin Microbiol Rev. 2007;20(1):79–114.
Leclercq R. Mechanisms of resistance to macrolides and lincosamides: Nature of the resistance elements and their clinical implications. Clin Infect Dis. 2002;34(4):482–92.
Lüthje P, von Köckritz-Blickwede M, Schwarz S. Identification and characterization of nine novel types of small staphylococcal plasmids carrying the lincosamide nucleotidyltransferase gene lnu(A). J Antimicrob Chemother. 2007;59(4):600–6.
Roberts MC. Resistance to tetracycline, macrolide-lincosamide-streptogramin, trimethoprim, and sulfonamide drug classes. Mol Biotechnol. 2002;20(3):261–83.
Lüthje P, Schwarz S. Antimicrobial resistance of coagulase-negative staphylococci from bovine subclinical mastitis with particular reference to macrolide-lincosamide resistance phenotypes and genotypes. J Antimicrob Chemother. 2006;57(5):966–9.
Ochoa-Zarzosa A, Loeza-Lara PD, Torres-Rodriguez F, Loeza-Angeles H, Mascot-Chiquito N, Sanchez-Baca S, et al. Antimicrobial susceptibility and invasive ability of Staphylococcus aureus isolates from mastitis from dairy backyard systems. Anton Leeuw Int J G. 2008;94(2):199–206.
Li LP, Zhou LX, Wang LH, Xue HP, Zhao X. Characterization of methicillin-resistant and -susceptible staphylococcal isolates from bovine milk in Northwestern China. PLoS One. 2015;10(3):e0116699.
Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Disk and Dilution Susceptibility Tests for Bacteria Isolated from Animals: Informational supplement. CLSI document 2004, M31-S1. Wayne, PA
Swedish Antibiotic Utilisation and Resistance in Human Medicine (SWEDRES) and Swedish Veterinary Antimicrobial Resistance Monitoring (SVARM). Use of antimicrobials and occurrence of antimicrobial resistance in Sweden. Solna/Uppsala: SWEDRES-SVARM Document; 2012.
Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Susceptibility Testing; Twenty-First Informational Supplement. CLSI document. 2011;31(1):M100–S21.
Lina G, Quaglia A, Reverdy ME, Leclercq R, Vandenesch F, Etienne J. Distribution of genes encoding resistance to macrolides, lincosamides, and streptogramins among staphylococci. Antimicrob Agents Chemother. 1999;43(5):1062–6.
Sutcliffe J, Grebe T, TaitKamradt A, Wondrack L. Detection of erythromycin-resistant determinants by PCR. Antimicrob Agents Chemother. 1996;40(11):2562–6.
Werner G, Cuny C, Schmitz FJ, Witte W. Methicillin-resistant, quinupristin-dalfopristin-resistant Staphylococcus aureus with reduced sensitivity to glycopeptides. J Clin Microbiol. 2001;39(10):3586–90.
Entorf M, Feßler AT, Kadlec K, Kaspar H, Mankertz J, Peters T, et al. Tylosin susceptibility of staphylococci from bovine mastitis. Vet Microbiol. 2014;171(3-4):368–73.
Pfister P, Jenni S, Poehlsgaard J, Thomas A, Douthwaite S, Ban N, et al. The structural basis of macrolide-ribosome binding assessed using mutagenesis of 23 S rRNA positions 2058 and 2059. J Mol Biol. 2004;342(5):1569–81.
Lüthje P, Schwarz S. Molecular analysis of constitutively expressed erm(C) genes selected in vitro in the presence of the non-inducers pirlimycin, spiramycin and tylosin. J Antimicrob Chemother. 2007;59(1):97–101.
Daurel C, Huet C, Dhalluin A, Bes M, Etienne J, Leclercq R. Differences in potential for selection of clindamycin-resistant mutants between inducible erm(A) and erm(C) Staphylococcus aureus genes. J Clin Microbiol. 2008;46(2):546–50.
de Vries LE, Christensen H, Agerso Y. The diversity of inducible and constitutively expressed erm(C) genes and association to different replicon types in staphylococci plasmids. Mobile Genetic Elements. 2012;2(2):72–80.
Martineau F, Picard FJ, Lansac N, Menard C, Roy PH, Ouellette M, et al. Correlation between the resistance genotype determined by multiplex PCR assays and the antibiotic susceptibility patterns of Staphylococcus aureus and Staphylococcus epidermidis. Antimicrob Agents Chemother. 2000;44(2):231–8.
Spiliopoulou I, Petinaki E, Papandreou P, Dimitracopoulos G. erm(C) is the predominant genetic determinant for the expression of resistance to macrolides among methicillin-resistant Staphylococcus aureus clinical isolates in Greece. J Antimicrob Chemother. 2004;53(5):814–7.
Acknowledgments
This study was financially supported by a grant from the National Science Foundation of China (31372282), the China Thousand Talents Program and a University Scientific Research Fund project (Fund No. Z111021305). This work was also partially supported from a discovery grant by Natural Science and Engineering Research Council of Canada.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
LPL and XZ conceived and designed the experiments; LPL, WWF, ZPZ and HPX conducted the laboratory experiments; LPL and XZ performed the data analysis; LPL and XZ wrote the manuscript. All authors read and approved the final manuscript.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Li, L., Feng, W., Zhang, Z. et al. Macrolide-lincosamide-streptogramin resistance phenotypes and genotypes of coagulase-positive Staphylococcus aureus and coagulase-negative staphylococcal isolates from bovine mastitis. BMC Vet Res 11, 168 (2015). https://doi.org/10.1186/s12917-015-0492-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12917-015-0492-8