Abstract
Background
Heart failure (HF) is a complex clinical syndrome with persistently high mortality. High-throughput proteomic technologies offer new opportunities to improve HF risk stratification, but their contribution remains to be clearly defined. We aimed to systematically review prognostic studies using high-throughput proteomics to identify protein signatures associated with HF mortality.
Methods
We searched four databases and two clinical trial registries for articles published from 2012 to 2023. HF proteomics studies measuring high numbers of proteins using aptamer or antibody-based affinity platforms on human plasma or serum with outcomes of all-cause or cardiovascular death were included. Two reviewers independently screened articles, extracted data, and assessed the risk of bias. A third reviewer resolved conflicts. We assessed the risk of bias using the Risk Of Bias In Non-randomized Studies—of Exposure tool.
Results
Out of 5131 unique articles identified, nine articles were included in the review. The nine studies were observational; three used the aptamer platform, and six used the antibody platform. We found considerable heterogeneity across studies in measurement panels, HF definitions, ejection fraction categorization, follow-up duration, and outcome definitions, and a lack of risk estimates for most protein associations. Hence, we proceeded with a systematic review rather than a meta-analysis. In two comparable aptamer studies in patients with HF with reduced ejection fraction, 21 proteins were identified in common for the association with all-cause death. Among these, one protein, WAP four-disulfide core domain protein 2 was also reported in an antibody study on HFrEF and for the association with CV death. We proposed standardized reporting criteria to facilitate the interpretation of future studies.
Conclusions
In this systematic review of nine studies evaluating the association of proteomics with mortality in HF, we identified a limited number of proteins common across several studies. Heterogeneity across studies compromised drawing broad inferences, underscoring the importance of standardized approaches to reporting.
Similar content being viewed by others
Introduction
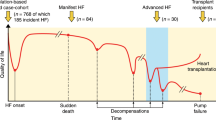
Heart failure (HF) is a clinical syndrome characterized by persistently high morbidity and mortality, despite advances in medical management [1,2,3]. While some individuals with HF will require advanced therapies, including heart replacement, others will respond well to guideline-directed medical therapies. As stratifying the risk of HF clinically is challenging, more precise approaches to risk stratification are critically needed to guide clinical decision-making. This need is emphasized in the 2022 American Heart Association/ American College of Cardiology/Heart Failure Society of America guidelines, which underscore the promise of omics technologies for this purpose [4].
In the last decade, high-throughput proteomics technologies using affinity reagents have emerged that have the potential to respond to the stated need [5]. These affinity-based technologies rely on different methods to measure a large number of proteins: one method which currently targets approximately 7000 human proteins uses slow off-rate modified aptamers (SOMAmer) which are modified short, single-stranded oligonucleotides as protein-binding reagents which are quantifiable by nucleic acid microarrays [6, 7]. The second method uses an antibody-based proximity extension assay that has the capability of identifying up to nearly 3000 human proteins, by relying on the dual binding of antibodies to a target protein to minimize nonspecific binding, and cross-reactivity [8, 9]. Several studies applying these technologies have suggested their value for HF risk stratification [10,11,12,13,14,15,16,17,18,19]. The purpose of this study was to systematically identify, describe, and compare studies that used large-scale antibody or aptamer assays to identify protein biomarkers associated with all-cause or cardiovascular (CV) death in HF. In doing so, we highlight important methodological elements to offer recommendations for future reporting.
Methods
This systematic review was written following the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) checklist [20]. The PRISMA Protocol extension [21] was used for writing the protocol a priori, which was registered in the PROSPERO (identifier: CRD42023449663).
Eligibility criteria (Table 1)
We included observational studies and all phases of clinical trials of (1) adults (aged ≥ 18 years) diagnosed with prevalent or incident HF with reduced ejection fraction (HFrEF) or preserved ejection fraction (HFpEF), (2) with plasma or serum proteome measures from aptamer-based (SomaScan) or antibody-based (Olink) high-affinity proteomic assays, (3) focused on protein association with outcomes, (4) reporting outcomes including all-cause death, CV death, or a composite outcome that includes death, and (5) published after 2012.
Information sources and search strategy
A biomedical librarian (AAL) searched four databases: Embase (Elsevier), PubMed (US National Library of Medicine), Scopus (Elsevier), and Web of Science: Core Collection (Clarivate Analytics) in March 2023, for proteomic studies in patients with HF published since 2012. Additionally, two clinical trial registries, Cochrane Library’s CENTRAL database (Wiley & Sons) and ClinicalTrials.gov (US National Library of Medicine) were searched in May 2023 for HF proteomic studies. EndNote 20 (Clarivate Analytics) was used to collect all records and identify duplicates.
The search strategies used are shown in Additional file 1. No publication language restrictions were used.
Selection process
First, a pilot of the two-step screening process using a random sample of 30 articles was completed by two reviewers (KOK and RO) using Covidence systematic review software (Veritas Health Innovation, Melbourne, Australia).
The two-step screening process was conducted using Covidence. For screening, the titles and abstracts of all unique records from the database searches were independently screened in duplicate by two reviewers (KOK and RO) using the established eligibility criteria (Table 1). Any conflicts or disagreements were resolved by discussion between the reviewers.
Next, the full-text screening of the records included after the first step was performed by two reviewers (KOK and RO) independently and in duplicate using the eligibility criteria. For this step, any conflicts were resolved by a third reviewer (MH).
Data collection and data items
For data collection, we created a standardized table of data items and definitions in Microsoft Excel. Two reviewers (KOK and RO) independently collected the data from each included article. The extracted items were verified by a third reviewer (MH) who resolved any discrepancies in the collected data. For each included study, we collected first author name, publication year, study design, name of cohort/registry, number of participants, years of enrollment, demographics (age, sex, and race/ethnicity or ancestry), ejection fraction (EF) category and definition, assay information (panel version and number of targets), outcome(s), and key findings on the number of significant proteins associated with outcomes (all-cause, CV death, and composite outcomes including death).
Risk of bias assessment
Given the observational nature of the studies included, we assessed the risk of bias for individual studies using the Risk of Bias for Non-randomized Studies—of Exposures (ROBINS-E) tool [22]. Two reviewers (KOK, RO) independently completed the assessment of the included articles, and a third reviewer (MH) checked the results and helped achieve consensus when there was disagreement on the assessed level of risk. Seven domains were covered in the ROBINS-E tool to evaluate bias due to (1) confounding, (2) exposure classification, (3) selection of study participants, (4) departures from intended exposures or post-exposure intervention, (5) missing data, (6) outcome measurement, and (7) the selection of reported results. Each domain was characterized as having low, moderate (some concerns), and high risk of bias. After completing all seven bias domains, an overall assessment was derived from the domain-level judgments using the ROBINS-E tool.
Our evaluation of protein biomarkers, outcome data, and study comparisons was limited to articles assessed with a low or moderate risk of bias.
Data synthesis
We reviewed proteomic associations with all-cause, cardiovascular death, or any composite endpoint that included death as one of the elements of the composite event. We did not consider hospitalizations, which are challenging to interpret due to their inherently multifactorial nature including but not limited to worsening HF, other comorbidities, but also access to care and its multiple determinants [23]. Protein lists from the aptamer and antibody platforms were confirmed using the information on the manufacturers’ websites, (www.somalogic.com and www.olinkexplore.com), in addition to published lists [24]. Due to variations in nomenclatures to designate specific proteins, we used UniProt.IDs [25] to compare findings across studies (www.uniprot.org) and to identify the common proteins. We sought the availability of risk estimates for individual proteins in manuscript tables, figures, texts, and supplemental material. For the studies reporting both minimally and fully adjusted models, only the results from fully adjusted models were considered. To characterize the functional classes of the proteins considered, we relied on the PANTHER Protein Class ontology (http://www.pantherdb.org/) [26].
Results
Selection of studies
As summarized in the PRISMA diagram (Fig. 1), the database and registry searches retrieved 8773 articles of which 3642 were duplicates and 5131 were screened at title and abstract. Of the 5131, we excluded 5104 articles, leaving 27 for full-text screening. After completing the full-text screening, we excluded 17 articles leaving 10 eligible articles, which we then assessed for risk of bias [10, 11, 13, 15, 16, 27,28,29,30,31]. One of the 10 articles was excluded after the risk of bias assessment (Additional file 2: Fig. S1). Therefore, nine articles published between 2017 and 2022 [10, 11, 13, 15, 16, 27,28,29,30] were included in this systematic review (Table 2).
Characteristics of included studies
All studies were observational including seven prospective cohorts [13, 15, 16, 27,28,29,30], one using two clinical trial populations [10], and the last study [11] included three groups with different designs: two nested case–control designs [32, 33], and a population-based cohort [34]. The studies were conducted in the USA [13], France [15], the Netherlands [28], Sweden [16], and three multi-national studies including participants mostly from Europe, the Americas, and Asia [10, 11, 27]. Notably, three studies included patients from the same cohorts [27, 29, 30]. While there were large variations in sample size, we enumerated a total of 7773 participants across the studies; their ages ranged between 53 and 71 years and 41% of participants were women. Two studies that reported race included 96% and 50% patients of European ancestry, respectively [10, 13]. Six of the studies included both derivation and validation or replication cohorts [10, 11, 13, 27, 29, 30].
Clinical characteristics, proteomics measurements, and outcomes
The use of HF diagnostic criteria was reported in three studies [13, 16, 28], two cited the Framingham criteria [13, 28] and one study cited the European Society Guidelines [16] criteria. Five of the studies focused on patients with HFrEF, two studies focused on patients with HFpEF, and two studies included the entire spectrum of HF regardless of EF categorization [29, 30]. The follow-up ranged from 9 to 60 months. Three studies used aptamer assays (n = 1310–4111) and six used antibody assays (n = 92–459). Hence, the heterogeneity across studies was quite substantial pertaining to the assays used, definitions of HF, categorization of EF, follow-up duration, outcomes selection, and definitions. This precluded the conduct of a meta-analysis leading us to proceed with the following systematic review.
Studies by platform
Aptamer-based studies
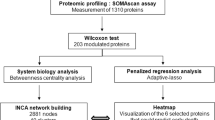
The three aptamer studies were restricted to HFrEF defined by different cut points (EF ≤ 35%, EF < 50%, and EF ≤ 45%) [10, 13, 15]. Two studies [13, 15] used plasma and one serum [10]. Two of the studies used the SomaScan 5k platform (versions 3 and 4) [10, 13] while an earlier version (SomaScan Assay 1.3K. version 1.2) was used in the third study (Table 2) [15].
All three studies developed models using the Least Absolute Shrinkage and Selection Operator (LASSO) penalized regression. The genetic association of specific protein targets was evaluated in two of the studies using protein quantitative trait loci (pQTL) sources [35] to assess aptamer specificity [10, 13].
Antibody-based studies
Among the six antibody-assay studies, two studied HFrEF [27, 28], two HFpEF [11, 16], and two included both HFrEF and HFpEF. The EF group cut points also varied across the studies (Table 2). One of the HFpEF studies included three different groups with different HFpEF cutoffs (EF ≥ 45%, EF ≥ 55%, and EF > 50%) [11]. All six studies applied a limited number of panels available in Olink® targeted panels ranging from 92 to 459 proteins (Table 2).
Associations with outcomes
Among the nine studies, five studies were not considered further (three studies reported only composite outcomes with varied components [15, 28, 36], one focused on the association with the outcome for proteins differentially expressed by sex and did not report overall results [30], and one was restricted to the exploration of immune-related mechanisms) [29]. Thus, we were left with four studies that reported associations with all-cause death [10, 11, 13, 27] among which two also reported on CV death [10, 27] (Fig. 2).
All-cause death
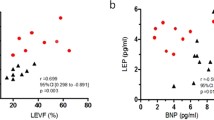
Two aptamer assay studies had reasonably comparable design features: restriction to HFrEF, and report of all-cause death, despite differences in panel version, HFrEF cut-offs, and model adjustment [10, 13]. Comparing the two studies [10, 13], one reported 84 and the other reported 107 unique proteins associated with all-cause death, and 21 proteins were identified in common between the studies [10, 13] (Table 3). Risk estimates with confidence intervals were not provided precluding a meta-analysis of the common proteins between these two studies. The functional class of the common proteins based on their encoded gene by PANTHER Protein Class ontology are listed in Table 3.
One antibody assay study on HFrEF also had a relatively comparable design to the two aptamer HFrEF studies and reported five unique proteins to be associated with all-cause death [27]. A single protein, WAP four-disulfide core domain protein 2 (also known as human epididymis protein 4 (HE4)) was identified in all three HFrEF studies for the association with all-cause death [10, 13, 27]. In addition, five proteins (R-spondin3 (RSPO3), triggering receptor expressed on myeloid cells (TREM1), C-X-C motif chemokine receptor (CXCL13), osteoprotegerin (OPG), and stem cell factor (SCF)) partially overlapped between the studies.
Cardiovascular deaths
Only two studies reported associations of proteins with CV death in HFrEF, one on each platform [10, 27]. In the aptamer study, 77 unique proteins were identified [10] while the antibody study reported three unique proteins [27] for the association with CV death (Fig. 2). The two studies shared three proteins: RSPO3, TREM1, and WAP four-disulfide core domain protein 2.
Overlap across EF groups
Few proteins were reported in common for all-cause death across studies in the different EF groups: HFrEF [10, 13, 27] and HFpEF [11]. Two antibody studies, one in HFpEF (Regan et al.) [11] and the other in HFrEF (Ferreira et al.) [27] each found 11 proteins associated with all-cause death and reported one protein (prolargin — an extracellular matrix protein) in common [11, 27]. Also, one study in HEpEF (Regan et al.) [11] reported one protein (vascular endothelial growth factor D — involved in angiogenesis and remodeling) in common with the other study in HFrEF (Zhang, et al.) [10] for the association with all-cause death.
Studies with risk scores
Five studies developed multi-protein scores to predict all-cause death or composite outcomes and examined the incremental value of these scores over clinical data, most frequently represented by the MAGGIC score and NTproBNP [10, 11, 13, 15, 28]. While the incremental value of the multiprotein scores varied across studies, their comparison is compromised by the degree of heterogeneity across studies which is compounded by differences in the adjusted models applied in generating the scores.
Discussion
To our knowledge, this is the first systematic review of proteomic studies using affinity reagents evaluating death in HF. We selected nine studies based on our inclusion criteria and risk of bias assessment [22]. The studies were highly heterogeneous, with respect to definitions of HF, choices of EF cut-points, assay methods, coverage of the proteome, follow-up duration, and outcomes reported. This heterogeneity precluded the conduct of a meta-analysis, leading us to conduct a systematic review.
Three of the studies (two aptamer- and one antibody-based) reported on all-cause death in HFrEF [10, 13, 27]. Twenty-one proteins were identified in common by the aptamer studies. One of these, WAP four-disulfide core domain protein 2 was associated with all-cause death in all three HFrEF studies [10, 13, 27]. Furthermore, WAP was reported for the association with CV death in two of the three studies [10, 27]. Due to methodological differences including variations in proteomic measurement assay and in the outcomes reported, the studies focused on HFpEF could not be compared with one another.
The proteomic platforms
Three studies [10, 13, 15] utilized the SomaScan aptamer platform which is reported as having a wider human proteome coverage [37, 38]. Six studies [11, 16, 27, 28, 30, 31] used Olink antibody-based assay which is reported to have stronger protein target specificity based on the percentage of proteins on the platform with reported genetic association [37]. However, all six antibody-based studies used panels containing only a subset (3–15%) of the 3072 Olink Explore panel while aptamer studies reported the full array of proteins available on their respective SomaScan versions. Consequently, only 13 of the 21 common proteins between the qualitatively comparable aptamer studies would have been detectable by the antibody studies in this review. Therefore, it is conceivable that a greater number of overlapping proteins might have been identified across the platforms if complete panels were used in the antibody studies. Overall, due to the evolving landscape of both aptamer and antibody proteomic assays with respect to coverage, sensitivity, and validation [37, 39], platform selection considerations in different studies warrant further studies.
Common findings across studies
Two aptamer-based HFrEF studies that reported on all-cause death identified 21 common proteins. One of these proteins, WAP four-disulfide core domain protein 2 was also associated with all-cause death in an antibody study and in the two studies that examined CV death [10, 13, 27]. Hence, WAP four-disulfide core domain protein 2 emerged as a protein of interest for risk stratification in HF, at least when the EF is reduced.
WAP four-disulfide core domain protein 2 is a protease inhibitor with roles in innate immunity and tumorigenesis. Clinically, it has been well studied as a novel therapeutic marker of epithelial ovarian and endometrial cancer [40,41,42]. More recently WAP was shown to be associated with growth differentiation factor 15 (GDF15) levels, which is expressed in inflammation and myocardial ischemia [43] and linked with poor outcomes in HF [44,45,46]. In a clinical trial sub-study of over 500 patients, WAP four-disulfide core domain protein 2 was associated with HF severity and the composite outcome of all-cause death or HF hospitalization and improved risk stratification over common clinical markers [47]. The present systematic review amplifies the findings from these prior reports and calls for additional studies evaluating WAP as a biomarker across the entire spectrum of HF syndrome.
Other proteins were found in common across the HFrEF studies on the different platforms including RSPO3 and OPG, which are both involved in fibrosis, and OPG has been previously reported as associated with HF prognosis [48, 49]. TREM1 and CXCL13 also in common between two of the HFrEF studies across platforms are both inflammatory proteins that have been linked to cardiac remodeling. CXCL13 is believed to be regulated in HF and atherosclerotic lesions alongside its receptor (C-X-C motif chemokine receptor 5-CXCR5) [50,51,52]. Lastly, SCF is a hematopoietic cytokine that may have a role in ischemia [53].
Heterogeneity across studies
In addition to differences in the coverage of the proteome related to differences in platforms, we observed considerable heterogeneity in methodology across the studies. With respect to HF diagnosis, only 3 studies specified their choice of criteria and used two different definitions [13, 16, 28]. The prevalence and case mix of HF varies depending on diagnostic criteria underscoring the need for caution in comparing results across studies [2, 54, 55]. Cut-offs selected for categorization into HFrEF or HFpEF were equally heterogenous: five HFrEF studies had four different cutoffs, and one of the two HFpEF studies included three cohorts with different EF cutoffs. Though EF provides a basis for clinical HF classification, its relevance to the study of proteomics is not clear. One cross-sectional study suggested differences in the circulating proteome across EF groups [56], but the effect of these differences on death is uncertain, particularly given the variability across EF categories in the literature. Few proteins overlapped across studies restricted to HFrEF or HFpEF [10, 11, 13, 15, 16, 27, 28], suggesting some commonality of prognostic value [56]. The duration of follow-up varied across different studies.
Also, the study outcomes were heterogeneous. Six of the nine studies focused on all-cause and/or CV death [10, 11, 13, 27, 29, 30], while the remaining reported composite outcomes that included death however defined differently across the studies [15, 16, 28]. Composite outcomes are commonly used in clinical trials to increase the number of events and improve study power, but improvements in power are contingent upon similar direction and magnitude of risk associated with the individual components of the composite outcome [57, 58].
Common pitfalls across studies
Clinical research studies can serve two distinct purposes: prediction and etiology. Prediction studies primarily aim for risk stratification, offering valuable insights into the likelihood of specific outcomes. However, prediction equations do not inherently provide insights into biological mechanisms or novel therapeutic approaches. In prediction-focused studies, the impact of confounding variables is generally less relevant [59, 60].
On the other hand, clinical research studies can uncover risk factors, unravel underlying biological processes, and potentially unveil new targets for therapeutic interventions. In these etiologic studies, accounting for confounding variables becomes crucial [59]. Often, the findings from such proteomic studies are further examined using Mendelian randomization analyses, which can provide evidence of a potential causal relationship.
It is essential to distinguish between these two categories in proteomics studies — prediction and etiology — when presenting research results. Keeping these purposes separate helps maintain the integrity of study designs and analytical methodologies. In this review, we observed that majority of the studies combined these two purposes.
Additionally, the use of inception cohorts of newly diagnosed HF cases is the preferred design for both prediction and etiologic studies [61]. Cohort studies of prevalent cases are vulnerable to survival bias [62].
Recommendations for future reports
The widespread interpretation challenges discussed above led us to formulate reporting recommendations to facilitate the interpretation of future studies. Several of them are focused on the adoption of state-of-the-art methods for the design and analysis of observational studies. These standards are not new, but their importance cannot be overemphasized as it is critical to abide by them so that the findings of proteomics studies can be compared, and the data pooled for group or individual-level meta-analyses.
-
Standard reporting guidelines such as the STROBE statement [63] (for observational studies), and TRIPOD statement [64] (for risk prediction studies) should be used to ensure complete reporting and will facilitate the assessment of studies’ strengths and weaknesses [65].
-
Study goals should be explicitly defined as either a prediction study or an etiology study and the analysis should be designed in accordance with stated goals.
-
Design should be that of inception-cohort whereby all subjects are enrolled at the same disease stage to the extent possible [61]. Attention to the possibility of index-event bias is also important [66].
-
Recruitment strategies should be explicitly designed to ensure the enrollment of diverse populations in sufficient numbers to enable analyses stratified by race/ethnicity and sex.
-
The ascertainment of HF should rely on standardized criteria, such as the Framingham criteria [67] or the European Society Guidelines [68].
-
Ejection fraction categories: Studies should include all forms of the HF syndrome including the entire EF spectrum. EF categories should be defined using cut-points recommended by the HF guidelines while however acknowledging the lack of consensus across guidelines [4, 68, 69]. The data should be analyzed while including all patients followed by stratified analyses by EF categories and sensitivity analyses to account for variability in EF cut points.
-
Study endpoints should include all-cause death and CV death. When composite outcomes are used individual analyses of the components of said composite outcomes should be reported.
-
Approaches to validation: the findings obtained in derivation cohorts should be validated. This could be accomplished using internal validation or external validation [70]. In the absence of an external validation cohort, temporal validation can be used as an alternative method as indicated in the TRIPOD guidelines. Orthogonal validation of identified proteins is also possible through several means including data from mass spectrometry [71, 72] and genome-wide association studies [37, 73]. The integration of population genomics with high-throughput proteomics can strengthen orthogonal validation and comparisons of identified proteins [39, 74], thereby enhancing the understanding of the correlations and differences among proteins measured on various platforms.
-
Protein nomenclature: reliance on UniProt.IDs [25] in addition to protein target names to facilitate comparison across studies.
-
Populations at high risk of adverse outcomes benefit from near-term risk prediction and risk models should be designed to provide this information as well as longer-term time horizons [75].
Strengths and limitations
This review has important strengths. First, we designed a comprehensive and rigorous search strategy to capture prognostic HF studies using high-throughput proteomics. Second, we assessed the risk of bias to guide our selection of the studies considered and omitted from our analyses the study assessed at a high risk of bias.
This systematic review was limited by the heterogeneity of the studies in addition to the non-availability of hazard ratios and confidence intervals in some studies which precluded the performing a meta-analysis.
Conclusions
We performed a systematic review evaluating the literature on high-throughput proteomics using affinity reagents to characterize proteins associated with death outcomes in patients with HF. Though we report overlapping proteins for all-cause death in HFrEF studies and singled out markers for future studies, the methodological differences noted call for caution in the aggregate interpretation of the findings. Our review points to the substantial heterogeneity across HF prognostic studies using high-throughput proteomic assays, which constitutes a strong rationale to adopt standardized recommendations to strengthen future studies on this topic.
Availability of data and materials
Materials used in this review are available in the reports and the databases used for this review.
Abbreviations
- HF:
-
Heart failure
- HFrEF:
-
Heart failure with reduced ejection fraction
- HFpEF:
-
Heart failure with preserved ejection fraction
- CV:
-
Cardiovascular
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-analyses
- EF:
-
Ejection fraction
- SOMAmer:
-
Slow off-rate modified aptamers.
- MAGGIC:
-
Meta-Analysis Global Group in Chronic Heart Failure
- PROSPERO:
-
International Prospective Register of Systematic Reviews
- ROBINS-E:
-
Risk of Bias for Non-randomized Studies—of Exposures
- HFH:
-
Heart failure hospitalization
- LASSO:
-
Least Absolute Shrinkage and Selection Operator
- pQTLs:
-
Protein quantitative trait loci
References
Levy D, Kenchaiah S, Larson MG, Benjamin EJ, Kupka MJ, Ho KK, et al. Long-term trends in the incidence of and survival with heart failure. N Engl J Med. 2002;347(18):1397–402.
Roger VL. Epidemiology of heart failure. Circ Res. 2021;128(10):1421–34.
Owan TE, Hodge DO, Herges RM, Jacobsen SJ, Roger VL, Redfield MM. Trends in prevalence and outcome of heart failure with preserved ejection fraction. N Engl J Med. 2006;355(3):251–9.
Heidenreich PA, Bozkurt B, Aguilar D, Allen LA, Byun JJ, Colvin MM, et al. 2022 AHA/ACC/HFSA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 0(0):https://doi.org/10.1161/CIR.0000000000001063.
Michelhaugh SA, Januzzi JL Jr. Finding a needle in a haystack: proteomics in heart failure. JACC Basic Transl Sci. 2020;5(10):1043–53.
Gold L, Ayers D, Bertino J, Bock C, Bock A, Brody EN, et al. Aptamer-based multiplexed proteomic technology for biomarker discovery. Plos One. 2010;5(12): e15004.
Kraemer S, Vaught JD, Bock C, Gold L, Katilius E, Keeney TR, et al. From SOMAmer-based biomarker discovery to diagnostic and clinical applications: a SOMAmer-based, streamlined multiplex proteomic assay. PLoS ONE. 2011;6(10): e26332.
Assarsson E, Lundberg M, Holmquist G, Björkesten J, Thorsen SB, Ekman D, et al. Homogenous 96-plex PEA immunoassay exhibiting high sensitivity, specificity, and excellent scalability. Plos One. 2014;9(4): e95192.
Lundberg M, Eriksson A, Tran B, Assarsson E, Fredriksson S. Homogeneous antibody-based proximity extension assays provide sensitive and specific detection of low-abundant proteins in human blood. Nucleic Acids Res. 2011;39(15): e102.
Zhang L, Cunningham JW, Claggett BL, Jacob J, Mendelson MM, Serrano-Fernandez P, et al. Aptamer proteomics for biomarker discovery in heart failure with reduced ejection fraction. Circulation. 2022;146(18):1411–4.
Regan JA, Truby LK, Tahir UA, Katz DH, Nguyen M, Kwee LC, et al. Protein biomarkers of cardiac remodeling and inflammation associated with HFpEF and incident events. Sci Rep. 2022;12(1):20072.
Wallentin L, Eriksson N, Olszowka M, Grammer TB, Hagström E, Held C, et al. Plasma proteins associated with cardiovascular death in patients with chronic coronary heart disease: a retrospective study. Plos Med. 2021;18(1): e1003513.
Gui H, She R, Luzum J, Li J, Bryson TD, Pinto Y, et al. Plasma proteomic profile predicts survival in heart failure with reduced ejection fraction. Circ Genom Precis Med. 2021;14(3): e003140.
Stienen S, Ferreira JP, Kobayashi M, Preud’homme G, Dobre D, Machu JL, et al. Enhanced clinical phenotyping by mechanistic bioprofiling in heart failure with preserved ejection fraction: insights from the MEDIA-DHF study (The Metabolic Road to Diastolic Heart Failure). Biomarkers. 2020;25(2):201–11.
Cuvelliez M, Vandewalle V, Brunin M, Beseme O, Hulot A, de Groote P, et al. Circulating proteomic signature of early death in heart failure patients with reduced ejection fraction. Sci Rep. 2019;9(1):19202.
Hage C, Michaëlsson E, Linde C, Donal E, Daubert JC, Gan LM, et al. Inflammatory biomarkers predict heart failure severity and prognosis in patients with heart failure with preserved ejection fraction: a holistic proteomic approach. Circ Cardiovasc Genet. 2017;10(1):e001633.
Lemesle G, Maury F, Beseme O, Ovart L, Amouyel P, Lamblin N, et al. Multimarker proteomic profiling for the prediction of cardiovascular mortality in patients with chronic heart failure. Plos One. 2015;10(4):e0119265.
Chirinos JA, Orlenko A, Zhao L, Basso MD, Cvijic ME, Li Z, et al. Multiple plasma biomarkers for risk stratification in patients with heart failure and preserved ejection fraction. J Am Coll Cardiol. 2020;75(11):1281–95.
Tromp J, Westenbrink BD, Ouwerkerk W, van Veldhuisen DJ, Samani NJ, Ponikowski P, et al. Identifying pathophysiological mechanisms in heart failure with reduced versus preserved ejection fraction. J Am Coll Cardiol. 2018;72(10):1081–90.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372: n71.
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1.
ROBINS-E Development Group (Higgins J, Morgan R, Rooney A, Taylor K, Thayer K, Silva R, Lemeris C, Akl A, Arroyave W, Bateson T, Berkman N, Demers P, Forastiere F, Glenn B, Hróbjartsson A, Kirrane E, LaKind J, Luben T, Lunn R, McAleenan A, McGuinness L, Meerpohl J, Mehta S, Nachman R, Obbagy J, O'Connor A, Radke E, Savović J, Schubauer-Berigan M, Schwingl P, Schunemann H, Shea B, Steenland K, Stewart T, Straif K, Tilling K, Verbeek V, Vermeulen R, Viswanathan M, Zahm S, Sterne J). Risk Of Bias In Non-randomized Studies - of Exposure (ROBINS-E). 2023. Available from: https://www.riskofbias.info/welcome/robinse-tool.
Zannad F, Garcia AA, Anker SD, Armstrong PW, Calvo G, Cleland JG, et al. Clinical outcome endpoints in heart failure trials: a European Society of Cardiology Heart Failure Association consensus document. Eur J Heart Fail. 2013;15(10):1082–94.
Candia J, Daya GN, Tanaka T, Ferrucci L, Walker KA. Assessment of variability in the plasma 7k SomaScan proteomics assay. Sci Rep. 2022;12(1):17147.
UniProt Consortium. UniProt: the universal protein knowledgebase. Nucleic Acids Res. 2017;45(D1):D158-d69.
Mi H, Muruganujan A, Huang X, Ebert D, Mills C, Guo X, et al. Protocol update for large-scale genome and gene function analysis with the PANTHER classification system (v.14.0). Nat Protoc. 2019;14(3):703–21.
Ferreira JP, Ouwerkerk W, Santema BT, van Veldhuisen DJ, Lang CC, Ng LL, et al. Differences in biomarkers and molecular pathways according to age for patients with HFrEF. Cardiovasc Res. 2021;117(10):2228–36.
Klimczak-Tomaniak D, de Bakker M, Bouwens E, Akkerhuis KM, Baart S, Rizopoulos D, et al. Dynamic personalized risk prediction in chronic heart failure patients: a longitudinal, clinical investigation of 92 biomarkers (Bio-SHiFT study). Sci Rep. 2022;12(1):2795.
Markousis-Mavrogenis G, Tromp J, Ouwerkerk W, Ferreira JP, Anker SD, Cleland JG, et al. Multimarker profiling identifies protective and harmful immune processes in heart failure: findings from BIOSTAT-CHF. Cardiovasc Res. 2022;118(8):1964–77.
Ravera A, Santema BT, de Boer RA, Anker SD, Samani NJ, Lang CC, et al. Distinct pathophysiological pathways in women and men with heart failure. Eur J Heart Fail. 2022;24(9):1532–44.
Eidizadeh A, Schnelle M, Leha A, Edelmann F, Nolte K, Werhahn SM, et al. Biomarker profiles in heart failure with preserved vs. reduced ejection fraction: results from the DIAST-CHF study. ESC Heart Failure. 2023;10(1):200–10.
Kraus WE, Granger CB, Sketch MH, Donahue MP, Ginsburg GS, Hauser ER, et al. A guide for a cardiovascular genomics biorepository: the CATHGEN experience. J Cardiovasc Transl Res. 2015;8(8):449–57.
Green JB, Bethel MA, Armstrong PW, Buse JB, Engel SS, Garg J, et al. Effect of Sitagliptin on cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2015;373(3):232–42.
Jr Taylor HA. The Jackson Heart Study: an overview. Ethn Dis. 2005;15(4 Suppl 6):S6-1 3.
Ferkingstad E, Sulem P, Atlason BA, Sveinbjornsson G, Magnusson MI, Styrmisdottir EL, et al. Large-scale integration of the plasma proteome with genetics and disease. Nat Genet. 2021;53(12):1712–21.
Hage C, Michaëlsson E, Linde C, Donal E, Daubert JC, Gan LM, et al. Inflammatory biomarkers predict heart failure severity and prognosis in patients with heart failure with preserved ejection fraction. Circul Cardiovasc Genet. 2017;10(1):e001633.
Katz DH, Robbins JM, Deng S, Tahir UA, Bick AG, Pampana A, et al. Proteomic profiling platforms head to head: Leveraging genetics and clinical traits to compare aptamer- and antibody-based methods. Sci Adv. 2022;8(33):eabm5164.
Pietzner M, Wheeler E, Carrasco-Zanini J, Kerrison ND, Oerton E, Koprulu M, et al. Synergistic insights into human health from aptamer- and antibody-based proteomic profiling. Nat Commun. 2021;12(1):6822.
Eldjarn GH, Ferkingstad E, Lund SH, Helgason H, Magnusson OT, Gunnarsdottir K, et al. Large-scale plasma proteomics comparisons through genetics and disease associations. Nature. 2023;622(7982):348–58.
Hellström I, Raycraft J, Hayden-Ledbetter M, Ledbetter JA, Schummer M, McIntosh M, et al. The HE4 (WFDC2) protein is a biomarker for ovarian carcinoma. Cancer Res. 2003;63(13):3695–700.
Moore RG, Brown AK, Miller MC, Badgwell D, Lu Z, Allard WJ, et al. Utility of a novel serum tumor biomarker HE4 in patients with endometrioid adenocarcinoma of the uterus. Gynecol Oncol. 2008;110(2):196–201.
Piovano E, Attamante L, Macchi C, Cavallero C, Romagnolo C, Maggino T, et al. The role of HE4 in ovarian cancer follow-up: a review. Int J Gynecol Cancer. 2014;24(8):1359–65.
Kempf T, von Haehling S, Peter T, Allhoff T, Cicoira M, Doehner W, et al. Prognostic utility of growth differentiation factor-15 in patients with chronic heart failure. J Am Coll Cardiol. 2007;50(11):1054–60.
Yamamoto M, Hanatani S, Araki S, Izumiya Y, Yamada T, Nakanishi N, et al. HE4 predicts progressive fibrosis and cardiovascular events in patients with dilated cardiomyopathy. J Am Heart Assoc. 2021;10(15): e021069.
Tang Y, Wang Y, Xu X, Tu LY, Huang P, Yang X, et al. Human epididymis protein 4: a novel predictor of ischemic cardiomyopathy. BMC Cardiovasc Disord. 2021;21(1):511.
Piek A, Meijers WC, Schroten NF, Gansevoort RT, de Boer RA, Silljé HH. HE4 serum levels are associated with heart failure severity in patients with chronic heart failure. J Card Fail. 2017;23(1):12–9.
de Boer RA, Cao Q, Postmus D, Damman K, Voors AA, Jaarsma T, et al. The WAP four-disulfide core domain protein HE4: a novel biomarker for heart failure. JACC Heart Fail. 2013;1(2):164–9.
Kamimura D, Suzuki T, Furniss AL, Griswold ME, Kullo IJ, Lindsey ML, et al. Elevated serum osteoprotegerin is associated with increased left ventricular mass index and myocardial stiffness. J Cardiovasc Med (Hagerstown). 2017;18(12):954–61.
Zhang M, Haughey M, Wang N-Y, Blease K, Kapoun AM, Couto S, et al. Targeting the Wnt signaling pathway through R-spondin 3 identifies an anti-fibrosis treatment strategy for multiple organs. Plos One. 2020;15(3): e0229445.
Smedbakken LM, Halvorsen B, Daissormont I, Ranheim T, Michelsen AE, Skjelland M, et al. Increased levels of the homeostatic chemokine CXCL13 in human atherosclerosis – Potential role in plaque stabilization. Atherosclerosis. 2012;224(1):266–73.
Boufenzer A, Lemarié J, Simon T, Derive M, Bouazza Y, Tran N, et al. TREM-1 mediates inflammatory injury and cardiac remodeling following myocardial infarction. Circ Res. 2015;116(11):1772–82.
Waehre A, Halvorsen B, Yndestad A, Husberg C, Sjaastad I, Nygård S, et al. Lack of chemokine signaling through CXCR5 causes increased mortality, ventricular dilatation, and deranged matrix during cardiac pressure overload. Plos One. 2011;6(4): e18668.
Takematsu E, Massidda M, Auster J, Chen P-C, Im B, Srinath S, et al. Transmembrane stem cell factor protein therapeutics enhance revascularization in ischemia without mast cell activation. Nat Commun. 2022;13(1):2497.
Di Bari M, Pozzi C, Cavallini MC, Innocenti F, Baldereschi G, De Alfieri W, et al. The diagnosis of heart failure in the community: Comparative validation of four sets of criteria in unselected older adults: the ICARe Dicomano Study. J Am Coll Cardiol. 2004;44(8):1601–8.
Bjork JB, Alton KK, Georgiopoulou VV, Butler J, Kalogeropoulos AP. Defining advanced heart failure: a systematic review of criteria used in clinical trials. J Cardiac Fail. 2016;22(7):569–77.
Adamo L, Yu J, Rocha-Resende C, Javaheri A, Head RD, Mann DL. Proteomic signatures of heart failure in relation to left ventricular ejection fraction. J Am Coll Cardiol. 2020;76(17):1982–94.
Armstrong PW, Westerhout CM. Composite end points in clinical research. Circulation. 2017;135(23):2299–307.
Bosco E, Hsueh L, McConeghy KW, Gravenstein S, Saade E. Major adverse cardiovascular event definitions used in observational analysis of administrative databases: a systematic review. BMC Med Res Methodol. 2021;21(1):241.
van Diepen M, Ramspek CL, Jager KJ, Zoccali C, Dekker FW. Prediction versus aetiology: common pitfalls and how to avoid them. Nephrol Dial Transplant. 2017;32(suppl_2):ii1–5.
Ramspek CL, Steyerberg EW, Riley RD, Rosendaal FR, Dekkers OM, Dekker FW, et al. Prediction or causality? A scoping review of their conflation within current observational research. Eur J Epidemiol. 2021;36(9):889–98.
Kent P, Cancelliere C, Boyle E, Cassidy JD, Kongsted A. A conceptual framework for prognostic research. BMC Med Res Methodol. 2020;20(1):172.
Hernán MA, Hernández-Díaz S, Robins JM. A structural approach to selection bias. Epidemiology. 2004;15(5):615–25.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61(4):344–9.
Collins GS, Reitsma JB, Altman DG, Moons KGM. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): the TRIPOD Statement. BMC Med. 2015;13(1):1.
Heus P, Damen J, Pajouheshnia R, Scholten R, Reitsma JB, Collins GS, et al. Uniformity in measuring adherence to reporting guidelines: the example of TRIPOD for assessing completeness of reporting of prediction model studies. BMJ Open. 2019;9(4): e025611.
Dahabreh IJ, Kent DM. Index Event Bias as an Explanation for the Paradoxes of Recurrence Risk Research. JAMA. 2011;305(8):822–3.
McKee PA, Castelli WP, McNamara PM, Kannel WB. The natural history of congestive heart failure: the Framingham study. N Engl J Med. 1971;285(26):1441–6.
McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M, et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: Developed by the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) With the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2021;42(36):3599–726.
Hudson S, Pettit S. What is “normal” left ventricular ejection fraction? Heart. 2020;106(18):1445–6.
Moons KG, Altman DG, Reitsma JB, Ioannidis JP, Macaskill P, Steyerberg EW, et al. Transparent Reporting of a multivariable prediction model for Individual Prognosis or Diagnosis (TRIPOD): explanation and elaboration. Ann Intern Med. 2015;162(1):W1-73.
Benson MD, Ngo D, Ganz P, Gerszten RE. Emerging affinity reagents for high throughput proteomics. Circulation. 2019;140(20):1610–2.
Noor Z, Ahn SB, Baker MS, Ranganathan S, Mohamedali A. Mass spectrometry–based protein identification in proteomics—a review. Brief Bioinform. 2020;22(2):1620–38.
Emilsson V, Ilkov M, Lamb JR, Finkel N, Gudmundsson EF, Pitts R, et al. Co-regulatory networks of human serum proteins link genetics to disease. Science. 2018;361(6404):769–73.
Ritchie SC, Lambert SA, Arnold M, Teo SM, Lim S, Scepanovic P, et al. Integrative analysis of the plasma proteome and polygenic risk of cardiometabolic diseases. Nat Metab. 2021;3(11):1476–83.
Eagle KA, Ginsburg GS, Musunuru K, Aird WC, Balaban RS, Bennett SK, et al. Identifying patients at high risk of a cardiovascular event in the near future. Circulation. 2010;121(12):1447–54.
Acknowledgements
The authors acknowledge the contributions of the NIH Library, Office of Research Services in the planning and execution of this review.
Funding
The work was led by investigators supported by the Intramural Research Program of the National Heart, Lung, and Blood Institute of the National Institutes of Health (NIH). AAL contributed to this work as part of the NIH Library, Office of Research Services support for the NIH Intramural Research Program.
Author information
Authors and Affiliations
Contributions
KOK, RO, MH, and VLR conceptualized the study and all authors contributed to the design. AAL carried out the database searches; KOK and RO carried out our screening, data extraction, and analysis, KOK, RO, and MH performed quality assessment. KOK, RO, MH, AAL, and VLR drafted the manuscript. JJS, JJ, BMP, DL, and PG contributed to the interpretation and presentation of the review findings. All authors contributed to the revision of the manuscript for critically important intellectual content and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
BMP serves on the Steering Committee for the Yale Open Data Access Project funded by Johnson & Johnson. PG serves as an advisor to SomaLogic, Inc. for which he has received no financial remuneration of any kind.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Search Strategy.
Additional file 2.
Risk of bias assessment using the ROBINS-E tool.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kuku, K.O., Oyetoro, R., Hashemian, M. et al. Proteomics for heart failure risk stratification: a systematic review. BMC Med 22, 34 (2024). https://doi.org/10.1186/s12916-024-03249-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12916-024-03249-7