Abstract
Background
The associations between trajectories of different health conditions and cognitive impairment among older adults were unknown. Our cohort study aimed to investigate the impact of various trajectories, including sleep disturbances, depressive symptoms, functional limitations, and multimorbidity, on the subsequent risk of cognitive impairment.
Methods
We conducted a prospective cohort study by using eight waves of national data from the Health and Retirement Study (HRS 2002–2018), involving 4319 adults aged 60 years or older in the USA. Sleep disturbances and depressive symptoms were measured using the Jenkins Sleep Scale and the Centers for Epidemiologic Research Depression (CES-D) scale, respectively. Functional limitations were assessed using activities of daily living (ADLs) and instrumental activities of daily living (IADLs), respectively. Multimorbidity status was assessed by self-reporting physician-diagnosed diseases. We identified 8-year trajectories at four examinations from 2002 to 2010 using latent class trajectory modeling. We screened participants for cognitive impairment using the 27-point HRS cognitive scale from 2010 to 2018 across four subsequent waves. We calculated hazard ratios (HR) using Cox proportional hazard models.
Results
During 25,914 person-years, 1230 participants developed cognitive impairment. In the fully adjusted model 3, the trajectories of sleep disturbances and ADLs limitations were not associated with the risk of cognitive impairment. Compared to the low trajectory, we found that the increasing trajectory of depressive symptoms (HR = 1.39; 95% CI = 1.17–1.65), the increasing trajectory of IADLs limitations (HR = 1.88; 95% CI = 1.43–2.46), and the high trajectory of multimorbidity status (HR = 1.48; 95% CI = 1.16–1.88) all posed an elevated risk of cognitive impairment. The increasing trajectory of IADLs limitations was associated with a higher risk of cognitive impairment among older adults living in urban areas (HR = 2.30; 95% CI = 1.65–3.21) and those who smoked (HR = 2.77; 95% CI = 1.91–4.02) (all P for interaction < 0.05).
Conclusions
The results suggest that tracking trajectories of depressive symptoms, instrumental functioning limitations, and multimorbidity status may be a potential and feasible screening method for identifying older adults at risk of cognitive impairment.
Similar content being viewed by others
Background
Cognitive impairment is a prevalent condition among older individuals, which manifests as difficulties in memory, learning, concentration, and decision-making. With rapid population aging, the prevalence of cognitive impairment will be higher [1]. Chen et al. reported that the prevalence of mild cognitive impairment in older adults was 21.2% [2]. Cognitive impairment is associated with various negative health outcomes, including an increased risk of mortality, the onset of dementia, higher rates of disability and hospitalization, and a decline in quality of life [3, 4]. Therefore, the prevention and management of cognitive impairment in the elderly have long been crucial concerns in promoting the well-being of the aging population.
As the global population increasingly ages, the coexistence of physical and psychological disorders is emerging as a significant worldwide challenge [5]. Additionally, there may be interactions between physical and psychological disorders. Sleep disorders, depressive symptoms, functional limitations, and multimorbidity each belong to different categories of physical or psychological disorders. Previous studies have reported that those disorders are risk factors that can adversely affect cognitive function [6,7,8,9]. However, most of the previous studies only conducted single-point measurements of these variables. Such single assessments of them frequently resulted in inconsistent findings and erroneous associations. Because patients’ sleep disorders and depressive symptoms often fluctuated at different stages of the illness, this could lead to erroneous associations with the risk of cognitive impairment. The remitting and relapsing nature of sleep disorders and depressive symptoms necessitates an investigation into their course in relation to the risk of cognitive impairment. Additionally, sleep disorders, depressive symptoms, and functional limitations were associated with some chronic diseases, such as cardiovascular diseases, which were also related to cognitive impairment [10, 11]. Consequently, extended observation over a longer period could uncover more insightful associations that a single assessment might overlook.
In recent years, there have been limited studies exploring the impact of trajectories of depressive symptoms, functional limitations, and sleep disorders on cognitive function decline. Mirza et al. reported that the increasing depressive symptoms were associated with a higher risk of dementia compared to the low depressive symptom trajectory [12]. Kaup et al. also found similar results, and they also discovered that a moderate and increasing trajectory of depressive symptoms was not significantly associated with the risk of dementia after full adjustment [13]. Yang et al. discovered that among Chinese older individuals, there was a high risk of mild cognitive impairment in the increasing instrumental activities of daily living (IADLs) limitation group, as reported using a group-based trajectory model [14]. Changes in sleep duration over time were also independently associated with cognitive decline among older adults [15, 16]. Due to the interplay of these physical and psychological disorders and their potential relationship with cognitive impairment, it is necessary to use long-term cohort follow-up data to investigate the independent impact of multiple disease trajectories on cognitive impairment, after controlling for other confounding factors.
To address the aforementioned issues, we employed 8 years of repeated measurement data from the Health and Retirement Study (HRS) to examine different trajectories and their subsequent effects on cognitive impairment. Our study aimed to investigate the relationship between long-term health status and cognitive impairment and to provide a reference for disease surveillance and prevention in clinical practice.
Methods
Study design and participants
We utilized cohort data from the HRS, a nationally representative longitudinal survey of adults aged 50 years and older in the USA [17, 18]. The HRS collected information on demographics, socioeconomic status, physical and mental health, and more. Further details on the sample design and procedures can be found in the cohort profile [17]. The standardized and validated measures of sleep disturbances, depressive symptoms, and functional limitations ensured the reliability and validity of the HRS study. The reporting of this study conforms to the Strengthening the Reporting of Observational Studies in Epidemiology guidelines.
Our study included participants who were not explicitly diagnosed with cognitive impairment, dementia, or Alzheimer’s disease, but had data on sleep conditions, depressive status, functional limitations, and multimorbidity status at four examination rounds in 2002, 2004, 2006, and 2010. We used this data to identify 8-year trajectories of sleep disturbances, depressive symptoms, functional limitations, and multimorbidity status. Participants were followed up for cognitive impairment until 2018, with assessments conducted every 2 years. This study utilized data from four assessments of the participants to construct trajectory models for different health conditions. At baseline, a total of 23,212 participants aged 60 years or older were included. After excluding 329 participants with Alzheimer’s disease and those who lacked information on Alzheimer’s disease (n = 14,447), 366 participants with dementia, and 2150 participants with cognitive impairment before 2010, we further excluded 710 participants without sufficient information on sleep disturbances, 294 participants without sufficient information on depressive symptoms, and 506 participants without sufficient information on multimorbidity status, as well as those with missing information on covariates (n = 91). Finally, we included 4319 participants in this cohort study (Fig. 1).
The HRS has received approval from the University of Michigan Institutional Review Board (IRB Protocol: HUM00061128). All participants provided oral informed consent.
Assessment of sleep disturbances, depressive symptoms, functional limitations and multimorbidity status
Sleep disturbances were assessed using a modified version of the Jenkins Sleep Scale, which demonstrated a good reliability (Cronbach’s alpha) of at least 0.7 [19]. Four items, including difficulty falling asleep, difficulty staying asleep, waking up too early during the night, and feeling rested when waking up in the morning, were considered. Participants were asked to rate their responses on a scale of 1 to 3, with “1 = rarely or never,” “2 = sometimes,” and “3 = most of the time.” After reverse coding the last item, the scores were summed, resulting in a total score ranging from 3 to 12 [20]. A higher score indicated a higher level of sleep disturbances [20].
Depressive symptoms were assessed using the 8-item Centers for Epidemiologic Research Depression (CES-D) scale, which measured the frequency of feelings on eight dichotomous items in the past week, including “depressed,” “everything was an effort,” “happy,” “life was enjoyable,” “sad,” and “unable to get going” [21, 22]. We reverse-coded the items on “happy” and “life was enjoyable” and then summed all the items. The total scores ranged from 0 to 8, with higher scores indicating more severe depressive symptoms.
Functional limitations were assessed by using activities of daily living (ADLs) and IADLs, respectively. ADLs limitations were assessed in six activities of daily living, including walking across a room, dressing, bathing, eating, getting in or out of bed, and using the toilet [23]. IADLs limitations were assessed in five instrumental activities of daily living, which included using a telephone, managing money, taking medications, shopping for groceries, and preparing hot meals [23]. If the respondent reported no difficulty with the item, it was coded as 0. If they reported difficulty, it was coded as 1. ADLs ranged from 0 to 6, and IADLs ranged from 0 to 5, with higher scores indicating greater ADLs limitations and IADLs limitations.
Multimorbidity status was assessed by calculating the sum score of 8 self-reported physician-diagnosed conditions: type 2 diabetes, stroke, hypertension, heart disease, chronic lung disease, arthritis, psychological diseases, and cancer [23].
Assessment of cognitive impairment
The cognitive function was assessed at each survey wave using the 27-point HRS cognitive scale. This scale consisted of immediate and delayed 10-noun free recall to assess memory, serial sevens subtraction to assess working memory, and counting backwards to assess the speed of mental processing [19, 24]. The total scores ranged from 0 to 27, with a score of 11 or less indicating cognitive impairment [23, 24].
Covariates
We assessed covariates using information from the 2010 examination. The following measures include age (< 70 years, 70 ~ 79 years, ≥ 80 years), gender (female, male), educational level (less than high school, high school or associate degree, some college or associate degree, college degree or above), marital status (married, unmarried), residence (rural, urban), total wealth income (the lowest quartile, Quartile 2, Quartile 3, the highest quartile), self-reported body mass index (BMI; underweight, normal, obesity, overweight) [25], physical activity (no, yes), drinking (no, yes), and smoking (no, yes) were considered.
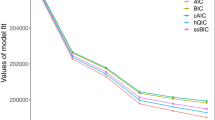
Statistical analysis
We used latent class trajectory models (LCTM) to identify trajectories of sleep disturbances, depressive symptoms, ADLs limitations, IADLs limitations, and multimorbidity status over time [12]. LCTM, as a finite mixture model, can identify latent classes of individuals who exhibit similar progressions of a determinant over time or with age [12]. Our models utilized second-order polynomials and calculated the posterior probabilities for each trajectory, taking into account the age level. Every participant was assigned to the trajectory with the highest probability. The best-fitting number of trajectories was selected based on the minimum Bayesian Information Criterion (BIC), while ensuring the posterior probabilities by class (> 0.70) and class size (≥ 2% of the population). To facilitate interpretability, we assigned labels to the trajectories based on the basis of their modeled graphic patterns.
To assess the risk of cognitive impairment, the examination date of the fourth examination (2010) was considered as time zero for the survival model. Time to event (cognitive impairment) was defined as follows: participants were followed up from the start date of the survival analyses (2010) and censored on the date of cognitive impairment, death, or being lost to follow-up. Participants were censored on the date that they were last seen or contacted when they were lost to follow-up. After assessing adherence to the proportional hazards assumption by plotting smoothed Schoenfeld residuals against time, there were no violations of the assumption. The hazard ratio (HR) for cognitive impairment was computed by using Cox proportional hazard models, based on the assigned trajectory. For all analyses, we fitted three models: model 1 was a univariate model; model 2 adjusted for age, gender, educational level, marital status, residence, total wealth income, self-reported BMI, physical activity, drinking, and smoking; and model 3 was a full model adding all trajectories. Moreover, considering that chronic diseases can impair both functional independence and cognitive performance, we further adjusted for various diseases, including cardiovascular diseases (stroke, hypertension, heart disease) and other diseases (type 2 diabetes, chronic lung disease, arthritis, psychological diseases, and cancer), to test the robustness of the results.
We conducted subgroup analysis based on age, gender, educational level, marital status, residence, total wealth income, self-reported BMI, physical activity, drinking, smoking, and all trajectories. In order to fully explore the combined effects of these variables, we selected significant risk trajectories and calculated their total scores. We then observed the impact of the total scores on the outcome. All analyses were done using R software, version 4.2.1 for Windows. Two-sided P values less than 0.05 were considered statistically significant.
Results
Trajectories of sleep disturbances, depressive symptoms, ADLs limitations, IADLs limitations and multimorbidity status
Of 4319 participants, the mean age was 75.47 years old (SD = 5.55) and 2653 (61.4%) were female. We identified two trajectories of sleep disturbances (Additional file 1: Fig. S1): one characterized by maintaining low sleep disturbances score (low; 3194 [74%]) and the other characterized by maintaining high scores throughout the follow-up period (high; 1125 [26%]). Compared with individuals in the low trajectory, those in the high trajectory were more likely to be older, female, and less educated and to engage in no physical activity, not drink, not smoke, have an increasing trajectory of depressive symptoms and IADLs limitations, and have a high trajectory of multimorbidity status (Additional file 1: Table S1).
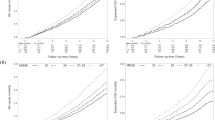
The trajectories of depressive symptoms were characterized by two patterns. The majority of participants maintained low CES-D scores (low; 3906 [90.4%]), and a smaller percentage had low starting scores that steadily increased throughout follow-up (increasing; 413 [9.6%]) (Fig. 2A). Compared with individuals in the low trajectories, those in the increasing trajectory were more likely to be female, less educated, and unmarried and to have lower income and abnormal BMI, engage in no physical activity, not drink, smoke, have a high trajectory of sleep disturbances and multimorbidity status, and have an increasing trajectory of ADLs limitations and IADLs limitations (Additional file 1: Table S2).
Trajectories of depressive symptoms, ADLs limitations, IADLs limitations, and multimorbidity status from 2002–2010. A Depressive symptoms: class 1 (black line, maintaining low CES-D score) and class 2 (red line, low starting CES-D scores that steadily increased throughout follow-up). B ADLs limitations: class 1 (black line, maintaining low ADLs score) and class 2 (red line, low starting ADLs scores that steadily increased throughout follow-up). C IADLs limitations: class 1 (black line, maintaining low IADLs score) and class 2 (red line, low starting IADLs scores that steadily increased throughout follow-up). D Multimorbidity status: class 1 (black line, maintaining low multimorbidity status), class 2 (red line, maintaining high multimorbidity status throughout follow-up), class 3 (green line, low starting multimorbidity status that increased early), and class 4 (blue line, low starting multimorbidity status that increased late). ADLs, activities of daily living; CES-D, Centers for Epidemiologic Research Depression; IADLs, instrumental activities of daily living
Both the trajectories of ADLs limitations and IADLs limitations were characterized by maintaining low scores (ADLs limitations = 4080 [94.5%]; IADLs limitations = 3906 [90.4%]) and initial low scores that steadily increased throughout the follow-up period (ADLs limitations = 239 [5.5%]; IADLs limitations = 3906 [90.4%]) (Fig. 2B, C). Compared with individuals in the low trajectories, those in the increasing trajectory of ADLs limitations and IADLs limitations were both more likely to be older, female, less educated, and unmarried and to have lower income, engage in no physical activity, and have no history of drinking or smoking (Additional file 1: Table S3 and Table S4). Individuals with an increasing trajectory of ADLs limitations were also more likely to exhibit a high trajectory of sleep disturbances and multimorbidity status, as well as an increasing trajectory of depressive symptoms and IADLs limitations. Meanwhile, individuals with an increasing trajectory of IADLs limitations were more likely to exhibit an increasing trajectory of depressive symptoms and ADLs limitations, as well as a high trajectory of multimorbidity status (Additional file 1: Table S3 and Table S4).
The trajectories of multimorbidity status were characterized by maintaining low multimorbidity status (low; 2073 [48.0%]), low starting scores that increased early (increasing early; 961 [22.3%]), low starting scores that increased late (increasing late; 1106 [25.6%]), and maintaining high scores throughout follow-up (high; 179 [4.1%]) (Fig. 2D). Compared with individuals in the other trajectories, those in the high trajectory were more likely to be female, to have lower education levels and lower income, to experience obesity, to engage in no physical activity, to not drink, smoke, to have a high trajectory of sleep disturbances, and to have an increasing trajectory of depressive symptoms, ADLs limitations, and IADLs limitations (Additional file 1: Table S5).
The associations of trajectories of sleep disturbances, depressive symptoms, ADLs limitations, IADLs limitations and multimorbidity status with the risk of cognitive impairment
During 25,914 person-years, 1230 participants developed cognitive impairment. Older adults with cognitive impairment were more likely to be older, female, less educated, and unmarried and to live in rural areas, have less income, report no physical activity and drinking, and smoke (Table 1).
In the univariate model, we found that compared with the low trajectory, the high trajectory of sleep disturbances (HR = 1.19; 95% CI = 1.05–1.35) and multimorbidity status (HR = 1.89; 95% CI = 1.49–2.39) were both associated with a higher risk of cognitive impairment (Table 2). Using the low trajectory as the reference trajectory, we found that individuals in the increasing trajectory of depressive symptoms (HR = 1.80; 95% CI = 1.53–2.12), ADLs limitations (HR = 1.88; 95% CI = 1.54–2.31), and IADLs limitations (HR = 2.98; 95% CI = 2.34–3.78) all had a higher risk of cognitive impairment (Table 2).
In the fully adjusted model 3, the trajectories of sleep disturbances and ADLs limitations were not associated with the risk of cognitive impairment. Compared to the low trajectory, we found that the high trajectory of multimorbidity status (HR = 1.48; 95% CI = 1.16–1.88), the increasing trajectory of depressive symptoms (HR = 1.39; 95% CI = 1.17–1.65), and the increasing trajectory of IADLs limitations (HR = 1.88; 95% CI = 1.43–2.46) still presented a higher risk of cognitive impairment (Table 2). After adjusting for different diseases, such as cardiovascular diseases and others, the results showed that the association between the trajectories of sleep disturbances, depressive symptoms, ADLs limitations, and IADLs limitations, and the risk of cognitive impairment remained stable (Additional file 1: Table S6).
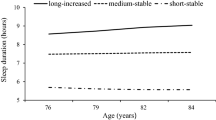
Subgroup analysis showed that there were no statistically significant differences among subgroups in terms of the trajectories of sleep disturbances, depressive symptoms, multimorbidity status, and ADLs limitations (Additional file 1: Table S7- Table S10), except the trajectories of IADLs limitations (Fig. 3). Compared with older populations who lived in rural areas (HR = 1.39; 95% CI = 0.86–2.25), the increasing trajectory of IADLs limitations posed a higher risk of cognitive impairment for those who lived in urban areas (HR = 2.30; 95% CI = 1.65–3.21; P for interaction = 0.049). Compared with older adults who never smoked (HR = 1.27; 95% CI = 0.86–1.89), the increasing trajectory of IADLs limitations posed a higher risk of cognitive impairment for those who smoked (HR = 2.77; 95% CI = 1.91–4.02; P for interaction = 0.033).
Subgroup analysis of associations between the trajectories of IADLs limitations and risk of cognitive impairment. Notes: all models were model 3. Data were represented as HR and 95%CI. BMI, body mass index; HR, hazard ratio; IADLs, instrumental activities of daily living; 95%CI, 95% confidence interval
Based on the above results, we calculated the total scores of trajectories, including depressive symptoms (low = 0; high = 1), multimorbidity status (low, increasing early, increasing late = 0; high = 1), and IADLs limitations (low = 0; increasing = 1). The total scores of risk trajectories ranged from 0 to 3. For every point increase in the risk trajectories, the risk of cognitive impairment increased by 49% (HR = 1.49; 95% CI = 1.32–1.67).
Discussion
In our 16-year cohort study, we identified two trajectories of sleep disturbances (low, high), depressive symptoms (low, increasing), ADLs limitations (low, increasing), and IADLs limitations (low, increasing), as well as four trajectories of multimorbidity status (low, increasing early, increasing late, high). The high trajectory of multimorbidity status, increasing trajectory of depressive symptoms, and increasing trajectory of IADLs limitations all posed a higher risk of cognitive impairment. Furthermore, the increasing trajectory of IADLs limitations had a higher risk of cognitive impairment for older populations who lived in urban areas and smoked. For every point increase in the total scores of risk trajectories, which included multimorbidity status, depressive symptoms, and IADLs limitations, the risk of cognitive impairment increased by 49%.
The varying trajectories of depressive symptoms, multimorbidity status, and IADLs limitations over nearly 8 years predicted the risks of cognitive impairment. We observed that individuals with increasing depressive symptoms had a significantly higher risk of cognitive impairment. Mirza et al. reported that only increasing depressive symptoms was associated with a higher risk of dementia, compared to the low depressive symptom trajectory, which supported our findings [12]. Mirza et al. proposed that depressive symptoms might lie in a continuum between subclinical cognitive impairment and overt dementia [12, 26, 27]. Kong et al. reported that older adults with increasing and persistently high depressive symptoms may experience worse memory [28]. By identifying patterns in the progression of depressive symptoms in our study, we found that the gradual escalation of depressive symptoms started several years before cognitive impairment occurred. But the important thing to note is that there is often a bidirectional relationship between depression and cognitive impairment, meaning that cognitive impairment in its early stages often leads to the onset of depression. The specific mechanisms of the impact of depressive symptoms on cognitive impairment are relatively few and complex. Inflammatory, trophic, and cerebrovascular factors may contribute, in addition to monoamine deficiency and the severity of plaques and tangle pathology [29].
Furthermore, we found that increasing IADL limitations, rather than ADL limitations increased the risk of cognitive impairment. Similarly, Sun et al. reported that the loss of ADL limitations among older adults was not found to be a significant risk factor for cognitive function [30]. Meanwhile, a study utilizing a group-based trajectory model indicated that the high-risk IADL group increased the risk of mild cognitive impairment among Chinese older individuals [14]. However, a bidirectional relationship might exist between cognitive function and functional limitations. Zang et al. reported that persons with dementia experienced steady declines in physical functioning [31]. In our study, we assessed IADL limitations using five instrumental activities of daily living, including using a telephone, managing money, taking medications, shopping for groceries, and preparing hot meals. Our findings reported an association between IADL limitations and cognitive impairment, but not ADL limitations. This might indicate that IADL limitations were the pre-cognitive impairment performances, similar to depressive symptoms [31]. Besides, it may be economical and convenient to adopt the IADL limitations as a supplementary screening tool for high-risk populations who develop cognitive impairment. However, we still need to explore the bidirectional relationship between physical functioning and cognitive impairment using appropriate causal inference methods in the future. We found that high multimorbidity status was a risk factor for cognitive impairment. Cross-sectional studies reported that multimorbidity was correlated with cognitive impairment [32, 33]. Limited studies have explored the association between comorbidity at multiple time points and cognitive impairment among older adults. Jones et al. reported that the severity of multimorbidity including arthritis, heart/circulation problems, and diabetes contributed to poorer delayed recall performance and lower semantic fluency scores in a cohort study [34]. Chronic co-morbidities, such as arthritis and diabetes, are risk factors for subsequent dementia due to their poorer progression of high inflammatory status [35].
After adjusting for covariates, it was found that high sleep disturbance and increasing ADLs limitations were not associated with the risk of cognitive impairment. However, the incidence of cognitive impairment was higher among older populations experiencing high sleep disturbances and increasing ADLs limitations, compared with those who reported low sleep disturbances and ADLs limitations, respectively. Zitser et al. also found that there was no significant association between sleep duration patterns and cognitive function or brain structure [36]. Previous studies have found that sleep disturbances and ADLs limitations were associated with risk of cognitive impairment when measuring them at a single point [7,8,9]. Our findings may indicate that more research is necessary to comprehend the impact of sleep disturbances and ADLs limitations on the risk of cognitive impairment. It is important to explore possible influencing factors within longitudinal data, rather than measuring them at a single point. For example, Guo et al. found that a persistent short nighttime sleep duration trajectory and persistent seldom daytime napping duration were associated with a higher risk of multimorbidity [37]. Multimorbidity may mediate the associations between sleep disturbances and cognitive impairment when the study measures sleep only once.
Compared with individuals in the low trajectories, those in the increasing trajectory of depressive symptoms and IADLs limitations were more likely to be female, less educated, and unmarried and to have lower income and engage in less physical activity. Meanwhile, compared with individuals in the other trajectories, those in the high trajectory of multimorbidity status were also more likely to be female and less educated, to have lower income, and to engage in less physical activity. Previous studies have also reported similar findings [12, 23]. Our results indicate that female, older adults with lower educational level and income should be the key population at risk for experiencing the poor course of depressive symptoms, functional limitations, and multimorbidity status. Besides, the older population may experience a decrease in their ability to engage in physical activity due to exacerbated depressive symptoms, functional limitations, and multimorbidity status. Consequently, older adults at risk trajectories engaged in less physical activity.
Population aging is associated with the co-occurrence of physical and psychological disorders [5]. In general, early screening and detection of cognitive impairment is more cost-effective and convenient than the clinical diagnosis of dementia. Identification of risk factors is essential for timely intervention to delay cognitive decline. Our study suggests that the trajectory of depressive symptoms, IADLs limitations, and multimorbidity may be risk factors for cognitive impairment. This strategy can be useful for more accurately identifying individuals at risk for cognitive impairment than a single time-point observation, as we know that exposure to risk factors can vary over time. In order to reduce the risk of cognitive impairment, observing the daily activities and psychological status of the elderly, as well as recording the multimorbidity, is conducive to providing critical interventions for high-risk populations.
Strengths and limitations
The major strength of this study was its ability to identify different courses of sleep disturbances, depressive symptoms, ADLs limitations, IADLs limitations, and multimorbidity status, and their relationship to the development of cognitive impairment. However, this study still had several limitations. Firstly, we used self-reported data on cognitive impairment and multimorbidity. Although multimorbidity was self-reported clinical diagnosis, the absence of a diagnosis record may introduce recall bias. Secondly, we only considered other covariates, such as physical activity, drinking, and smoking at a single point. However, these factors could change over time as potential risk factors for cognitive impairment. Furthermore, some relevant characteristics, such as social factors, were not measured in our study. Further research on the relationship between the observed trajectories and cognitive impairment would benefit from investigating these characteristics, including the changes in lifestyle habits and social factors. Exploring the impact of these factors on the association between health status and the development of cognitive impairment using cohort studies, randomized controlled trials (RCT), or structural equation analysis is crucial for improving cognitive impairment in the future. Finally, it should be noted that dementia is defined by the presence of cognitive decline sufficient enough to interfere with independence. It is possible that functional decline is not a risk factor but rather a manifestation of the onset of cognitive impairment. We conducted a cohort study to present that the decline in physical function may increase the risk of cognitive impairment after controlling other trajectories. In addition, the ADLs limitations and IADLs limitations primarily assess the activities of daily living, while the cognitive scale primarily assesses memory, which does not fully represent a clinical diagnosis of dementia. On the contrary, the use of this cognitive scale in a large-sample cohort study may reduce this possibility. In order to clarify the bidirectional relationship between physical disorders and mental health in the future, RCT is needed to explore the effect of early intervention for functional impairment on cognitive impairment.
Conclusions
In conclusion, the increased risk of subsequent cognitive impairment among individuals with exasperate courses of depressive symptoms, instrumental functioning limitations, and multimorbidity suggests that we should pay more attention to the impact of long-term changes in health status on mental disorders. The courses of depressive symptoms, instrumental functioning limitations, and multimorbidity may serve as effective screening and warning indicators of cognitive impairment in the daily care of older adults. Future studies are warranted to unravel the biological underpinnings of these associations. In addition, causal inference methods could be used to investigate the potential of using trajectories (as opposed to single assessments) as a screening method to identify older adults at risk of cognitive impairment and intervene early.
Availability of data and materials
The HRS datasets are openly available from https://hrsdata.isr.umich.edu/data-products/public-survey-data (accessed on 10 May 2023).
Abbreviations
- ADLs:
-
Activities of daily living
- BIC:
-
Bayesian Information Criterion
- BMI:
-
Body mass index
- CES-D:
-
Center for Epidemiology Depression Scale
- CI:
-
Confidence interval
- HR:
-
Hazard ratios
- HRS:
-
Health and Retirement Study
- IADLs:
-
Instrumental activities of daily living
- LCTM:
-
Latent class trajectory models
- RCT:
-
Randomized controlled trials
- SD:
-
Standard deviation
References
Yin P, Ma Q, Wang L, Lin P, Zhang M, Qi S, et al. Chronic obstructive pulmonary disease and cognitive impairment in the Chinese elderly population: a large national survey. Int J Chron Obstruct Pulmon Dis. 2016;11:399–406. https://doi.org/10.2147/COPD.S96237.
Chen P, Cai H, Bai W, Su Z, Tang YL, Ungvari GS, et al. Global prevalence of mild cognitive impairment among older adults living in nursing homes: a meta-analysis and systematic review of epidemiological surveys. Transl Psychiatry. 2023;13:88. https://doi.org/10.1038/s41398-023-02361-1.
Chen B, Wang M, He Q, Wang Y, Lai X, Chen H, et al. Impact of frailty, mild cognitive impairment and cognitive frailty on adverse health outcomes among community-dwelling older adults: A systematic review and meta-analysis. Front Med (Lausanne). 2022;9:1009794. https://doi.org/10.3389/fmed.2022.1009794.
Pike KE, Cavuoto MG, Li L, Wright BJ, Kinsella GJ. Subjective cognitive decline: level of risk for future dementia and mild cognitive impairment, a meta-analysis of longitudinal studies. Neuropsychol Rev. 2022;32:703–35. https://doi.org/10.1007/s11065-021-09522-3.
Ni Y, Zhou Y, Kivimäki M, Cai Y, Carrillo-Larco RM, Xu X, et al. Socioeconomic inequalities in physical, psychological, and cognitive multimorbidity in middle-aged and older adults in 33 countries: a cross-sectional study. Lancet Healthy Longev. 2023;4:e618–28. https://doi.org/10.1016/S2666-7568(23)00195-2.
Qin S, Leong RLF, Ong JL, Chee MWL. Associations between objectively measured sleep parameters and cognition in healthy older adults: a meta-analysis. Sleep Med Rev. 2023;67:101734. https://doi.org/10.1016/j.smrv.2022.101734.
Wong R, Lovier MA. Sleep disturbances and dementia risk in older adults: findings from 10 years of National U.S. prospective data. Am J Prev Med. 2023;64:781–7. https://doi.org/10.1016/j.amepre.2023.01.008.
Pearson O, Uglik-Marucha N, Miskowiak KW, Cairney SA, Rosenzweig I, Young AH, et al. The relationship between sleep disturbance and cognitive impairment in mood disorders: a systematic review. J Affect Disord. 2023;327:207–16. https://doi.org/10.1016/j.jad.2023.01.114.
Chodosh J, Miller-Martinez D, Aneshensel CS, Wight RG, Karlamangla AS. Depressive symptoms, chronic diseases, and physical disabilities as predictors of cognitive functioning trajectories in older Americans. J Am Geriatr Soc. 2010;58:2350–7. https://doi.org/10.1111/j.1532-5415.2010.03171.x.
van Nieuwkerk AC, Delewi R, Wolters FJ, Muller M, Daemen M, Biessels GJ. Cognitive impairment in patients with cardiac disease: implications for clinical practice. Stroke. 2023;54:2181–91. https://doi.org/10.1161/STROKEAHA.123.040499.
Katabathula S, Davis PB, Xu R. Comorbidity-driven multi-modal subtype analysis in mild cognitive impairment of Alzheimer’s disease. Alzheimers Dement. 2023;19:1428–39. https://doi.org/10.1002/alz.12792.
Mirza SS, Wolters FJ, Swanson SA, Koudstaal PJ, Hofman A, Tiemeier H, et al. 10-year trajectories of depressive symptoms and risk of dementia: a population-based study. Lancet Psychiatry. 2016;3:628–35. https://doi.org/10.1016/S2215-0366(16)00097-3.
Kaup AR, Byers AL, Falvey C, Simonsick EM, Satterfield S, Ayonayon HN, et al. Trajectories of depressive symptoms in older adults and risk of dementia. JAMA Psychiat. 2016;73:525–31. https://doi.org/10.1001/jamapsychiatry.2016.0004.
Yang J, Zhang Y, Shen S, Yu H, Yang L, Zhao Y, et al. Instrumental activities of daily living trajectories and risk of mild cognitive impairment among Chinese older adults: results of the Chinese longitudinal healthy longevity survey, 2002–2018. Front Public Health. 2023;11:1165753. https://doi.org/10.3389/fpubh.2023.1165753.
Zhu Q, You Y, Fan L, Fan H. Associations between sleep duration patterns and cognitive decline trajectories in older Chinese adults. Aging Clin Exp Res. 2021;33:3057–63. https://doi.org/10.1007/s40520-021-01851-w.
Ma Y, Liang L, Zheng F, Shi L, Zhong B, Xie W. Association between sleep duration and cognitive decline. JAMA Netw Open. 2020;3:e2013573. https://doi.org/10.1001/jamanetworkopen.2020.13573.
Sonnega A, Faul JD, Ofstedal MB, Langa KM, Phillips JW, Weir DR. Cohort Profile: the Health and Retirement Study (HRS). Int J Epidemiol. 2014;43:576–85. https://doi.org/10.1093/ije/dyu067.
HRS Survey Data. 2022. https://hrsdata.isr.umich.edu/data-products/public-survey-data.
Qi X, Pei Y, Malone SK, Wu B. Social isolation, sleep disturbance, and cognitive functioning (HRS): a longitudinal mediation study. J Gerontol A Biol Sci Med Sci. 2023;78:1826–33. https://doi.org/10.1093/gerona/glad004.
Jenkins CD, Stanton BA, Niemcryk SJ, Rose RM. A scale for the estimation of sleep problems in clinical research. J Clin Epidemiol. 1988;41:313–21. https://doi.org/10.1016/0895-4356(88)90138-2.
Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale). Am J Prev Med. 1994;10:77–84.
Lewinsohn PM, Seeley JR, Roberts RE, Allen NB. Center for Epidemiologic Studies Depression Scale (CES-D) as a screening instrument for depression among community-residing older adults. Psychol Aging. 1997;12:277–87. https://doi.org/10.1037//0882-7974.12.2.277.
Quiñones AR, Nagel CL, Botoseneanu A, Newsom JT, Dorr DA, Kaye J, et al. Multidimensional trajectories of multimorbidity, functional status, cognitive performance, and depressive symptoms among diverse groups of older adults. J Multimorb Comorb. 2022;12:26335565221143012. https://doi.org/10.1177/26335565221143012.
Crimmins EM, Kim JK, Langa KM, Weir DR. Assessment of cognition using surveys and neuropsychological assessment: the Health and Retirement Study and the Aging, Demographics, and Memory Study. J Gerontol B Psychol Sci Soc Sci. 2011;66(Suppl 1):i162–71. https://doi.org/10.1093/geronb/gbr048.
World Health Organization: Body mass index (BMI). 2023. https://www.who.int/data/gho/data/themes/topics/topic-details/GHO/body-mass-index. Accessed 13 June 2023.
Mirza SS, de Bruijn RF, Direk N, Hofman A, Koudstaal PJ, Ikram MA, et al. Depressive symptoms predict incident dementia during short- but not long-term follow-up period. Alzheimers Dement. 2014;10(Suppl):S323–9. https://doi.org/10.1016/j.jalz.2013.10.006.
Ismail Z, Smith EE, Geda Y, Sultzer D, Brodaty H, Smith G, et al. Neuropsychiatric symptoms as early manifestations of emergent dementia: provisional diagnostic criteria for mild behavioral impairment. Alzheimers Dement. 2016;12:195–202. https://doi.org/10.1016/j.jalz.2015.05.017.
Kong D, Lu P, Solomon P, Woo J, Shelley M. Depressive symptom trajectories and cognition among older American couples: a dyadic perspective. J Aging Health. 2023;35:282–93. https://doi.org/10.1177/08982643221125838.
Enache D, Winblad B, Aarsland D. Depression in dementia: epidemiology, mechanisms, and treatment. Curr Opin Psychiatry. 2011;24:461–72. https://doi.org/10.1097/YCO.0b013e32834bb9d4.
Sun Q, Jiang N, Lu N, Lou VWQ. Bidirectional relationship between cognitive function and loss hierarchy of activities of daily living among older adults with disabilities in urban China: a cross-lagged analysis. BMJ Open. 2022;12:e057211. https://doi.org/10.1136/bmjopen-2021-057211.
Zang E, Shi Y, Wang X, Wu B, Fried TR. Trajectories of physical functioning among US adults with cognitive impairment. Age Ageing. 2022;51:afac139. https://doi.org/10.1093/ageing/afac139.
Kim S. Cognitive function, and its relationships with comorbidities, physical activity, and muscular strength in Korean older adults. Behav Sci (Basel). 2023;13:212. https://doi.org/10.3390/bs13030212.
Martínez-Horta S, Bejr-Kasem H, Horta-Barba A, Pascual-Sedano B, Santos-García D, de Deus-Fonticoba T, et al. Identifying comorbidities and lifestyle factors contributing to the cognitive profile of early Parkinson’s disease. BMC Neurol. 2021;21:477. https://doi.org/10.1186/s12883-021-02485-1.
Jones JD, Malaty I, Price CC, Okun MS, Bowers D. Health comorbidities and cognition in 1948 patients with idiopathic Parkinson’s disease. Parkinsonism Relat Disord. 2012;18:1073–8. https://doi.org/10.1016/j.parkreldis.2012.06.004.
Cunningham C, Hennessy E. Co-morbidity and systemic inflammation as drivers of cognitive decline: new experimental models adopting a broader paradigm in dementia research. Alzheimers Res Ther. 2015;7:33. https://doi.org/10.1186/s13195-015-0117-2.
Zitser J, Anatürk M, Zsoldos E, Mahmood A, Filippini N, Suri S, et al. Sleep duration over 28 years, cognition, gray matter volume, and white matter microstructure: a prospective cohort study. Sleep. 2020;43:zsz90. https://doi.org/10.1093/sleep/zsz290.
Guo J, Li A, Chen M, Wei D, Wu J, Wang T, et al. Association of longitudinal patterns of nighttime sleep duration and daytime napping duration with risk of multimorbidity. Sleep Health. 2023;9:363–72. https://doi.org/10.1016/j.sleh.2023.02.003.
Acknowledgements
We would like to thank all individuals who participated in the HRS study and all the study team members for their tremendous efforts in collecting and managing the data.
Funding
JL received funding from the National Natural Science Foundation of China (72122001, 72211540398; URL: https://www.nsfc.gov.cn/). The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
JL and LT conceptualized and designed the study. JL did the data acquisition. MD did the data curation, formal analysis, and writing of the original draft. MD, LT, ML, and JL did the writing—reviewing and editing. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The HRS has received approval from the University of Michigan Institutional Review Board (IRB Protocol: HUM00061128). All participants provided oral informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Fig. S1.
Trajectories of sleep disturbances. Table S1. The participants’ characteristics stratified by trajectories of sleep disturbances. Table S2. The participants’ characteristics stratified by trajectories of depressive symptoms. Table S3. The participants’ characteristics stratified by trajectories of ADLs limitations. Table S4. The participants’ characteristics stratified by trajectories of IADLs limitations. Table S5. The participants’ characteristics stratified by trajectories of multimorbidity status. Table S6. Trajectories of sleep disturbances, depressive symptoms, ADLs limitations, and IADLs limitations and risk of cognitive impairment. Table S7. Subgroup analysis of the trajectories of sleep disturbances and risk of cognitive impairment. Table S8. Subgroup analysis of the trajectories of depressive symptoms and risk of cognitive impairment. Table S9. Subgroup analysis of the trajectories of multimorbidity status and risk of cognitive impairment. Table S10. Subgroup analysis of the trajectories of ADLs limitations and risk of cognitive impairment.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Du, M., Tao, L., Liu, M. et al. Trajectories of health conditions and their associations with the risk of cognitive impairment among older adults: insights from a national prospective cohort study. BMC Med 22, 20 (2024). https://doi.org/10.1186/s12916-024-03245-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12916-024-03245-x