Abstract
Background
Treatment options beyond the first-line setting for recurrent or metastatic nasopharyngeal carcinoma (RM-NPC) are limited. The role of the multitarget tyrosine kinase inhibitor anlotinib in RM-NPC is unclear.
Methods
In this prospective, single-arm, phase 2 trial, patients with histologically confirmed RM-NPC and failure of at least two lines of prior systemic treatments were eligible. Anlotinib was given at 12 mg once daily on days 1–14 every 3 weeks until disease progression or intolerable toxicities. The primary end point was disease control rate, defined as the percentage of patients achieving complete response, partial response, or stable disease by RECIST criteria.
Results
From April 2019 to March 2021, 39 patients were enrolled and received a median of 4 cycles (range, 0.5–20) of anlotinib treatment. Partial response and stable disease were observed in 8 and 20 patients, respectively. The disease control rate was 71.8%, and objective response rate was 20.5%. With a median follow-up of 17.2 months, the median progression-free survival was 5.7 months. The 12-month overall survival was 58.3%, and the median overall survival was not reached. The most frequent grade 3/4 treatment-related adverse events were hand-foot syndrome (23.7%), oral mucositis (21.0%), hypertension (7.9%), and triglyceride elevation (7.9%). Hemorrhage, all grade 1 or 2, occurred in 34.2% of the patients.
Conclusions
Anlotinib monotherapy exhibited promising anti-tumor activities and disease control for heavily pretreated RM-NPC patients with a tolerable toxicity profile.
Trial registration
ClinicalTrials.gov: NCT03906058.
Similar content being viewed by others
Background
Nasopharyngeal carcinoma (NPC) ranks 23rd in cancer prevalence globally [1], with new cases arising predominantly in east and southeast Asia. Approximately 10 to 15% of NPC patients have primary metastasis at the time of diagnosis, and 30% will develop local recurrence or distant metastases despite the standard first-line therapeutic regimens [2, 3]. Although cisplatin/gemcitabine (GP)-based regimens have been recommended as the first-line systemic treatment for recurrent or metastatic (RM)-NPC patients [4], patients who are refractory or progress after first-line treatment have few treatment options. Currently, there is no standard therapy in the second or subsequent line setting for RM-NPC. Therefore, a need exists for novel agents or therapeutic modalities for this refractory disease that carries a grave prognosis.
Antiangiogenic therapy hold promise for RM-NPC. NPC is amenable to antiangiogenic therapy as vascular endothelial growth factor (VEGF) is highly expressed in NPC and correlates with survival [5]. However, the addition of anti-VEGF antibody bevacizumab to paclitaxel plus carboplatin as first-line treatment failed to extend the progression-free survival (PFS) and overall survival (OS) of RM-NPC patients [6]. Other antiangiogenic multikinase inhibitors (MKIs) achieved an objective response rate (ORR) between 6.1 and 20% as monotherapy for pretreated RM-NPC [7,8,9]. Safety concerns such as hemorrhage have also hampered the use of antiangiogenic therapies for RM-NPC [10,11,12]. These observations suggest that the exploration of novel antiangiogenic MKIs for RM-NPC is necessary.
Anlotinib is a tyrosine kinase inhibitor that targets vascular endothelial growth factor receptor (VEGFR), fibroblast growth factor receptor (FGFR), platelet-derived growth factor receptors (PDGFR), and c-kit [13, 14]. It has been approved as 3rd line treatment for locally advanced or metastatic non-small cell lung cancer and 2nd line treatment for advanced soft-tissue sarcoma in China [15, 16]. Anlotinib has a low half-maximal inhibitory concentration (IC50) (0.2 nM) and has potent inhibitory activities on FGFR [13, 17]. It has been investigated in a variety of advanced tumors [18,19,20,21] but has not been examined in RM-NPC. This trial investigated the efficacy and safety of anlotinib in pretreated RM-NPC patients. An exploratory analysis was also undertaken to identify prognostic factors for antiangiogenic therapy for RM-NPC.
Methods
Patients
This single arm, phase II trial (ClinicalTrials.gov: NCT03906058) enrolled patients aged 18–70 years with pathologically confirmed locally recurrent or metastatic NPC and disease progression after at least two lines of prior systemic treatments. Patients had to have adequate organ function, an Eastern Cooperative Oncology Group (ECOG) performance status score of 0 or 1, and at least one measurable lesion per RECIST v1.1. Patients were excluded if they had received prior treatment with bevacizumab or VEGFR inhibitors or had received re-irradiation at nasopharyngeal lesions. Detailed eligibility criteria are described in the study protocol.
The trial was conducted according to the provisions of the Declaration of Helsinki and the International Conference on Harmonisation guidelines for Good Clinical Practice and approved by the institutional review board of Sun Yat-Sen University Cancer Center. All patients provided written informed consent before enrollment. The study protocol adhered to the SPIRIT statement and the reporting of the study adhered to the CONSORT statement.
Treatment and assessments
Patients received 12 mg of anlotinib (Chia-tai Tianqing Pharmaceutical Co., Ltd.), orally once daily (2 weeks on and 1 week off), until disease progression or intolerable toxicities. Dose modification was allowed, with two levels of reduction (from 12 mg/day to 10 mg/day and 8 mg/day), for anlotinib-related toxicities according to protocol-specified criteria (generally for grade 3/4 toxicities). If more than 2 levels of dose modifications were required, treatment was terminated.
Responses were assessed by CT and MRI per RECIST v1.1 every two cycles during the anlotinib treatment. Adverse events (AEs) were graded according to the National Cancer Institute Common Terminology Criteria for Adverse Events (CTCAE) v5.0.
Plasma EBV DNA copy number was determined at baseline and every 3 weeks until disease progression by quantitative reverse transcription polymerase chain reaction with probes against EBV genes.
Study end points
The primary end points were disease control rate (DCR), which was the proportion of patients achieving complete response (CR), partial response (PR), and stable disease (SD). The secondary end points included ORR, which was the proportion of patients achieving CR or PR; PFS, calculated from the date of study entry to progressive disease (PD) or death, whichever occurred earlier; OS, calculated from the date of study entry to death of all cause; and duration of response (DOR), which was the duration from initial CR or PR to PD or recurrence.
Statistical analysis
A single-stage phase II design with a type I error of 5% and power of 80% was used to calculate the sample size. We considered the anlotinib treatment to be ineffective if DCR was ≤ 20% based on the result from the phase II study of gefitinib treatment for RM-NPC [22]. It has been reported that pazopanib treatment achieved a DCR of 54.5% (95% CI, 38.0–70.2) in RM-NPC patients (7). However, limited clinical data were available for anlotinib during the study's design phase. Considering the potential challenges of anlotinib tolerability in RM-NPC patients, which could subsequently impact treatment efficacy, we prudently selected a relatively conservative expected DCR of 40%. An estimated sample size of 35 patients was required. If at least 11 cases of CR or PR or SD were observed, the drug would be deemed effective. Assuming a dropout rate of 10%, the maximum estimated sample size was 39 patients.
All patients who received at least one dose of anlotinib were included in the efficacy and safety analysis set (full analysis set). No missing data was imputed. The 95% CIs of ORR and DCR were calculated using the Clopper-Pearson method. PFS and OS were calculated using the Kaplan–Meier method. Safety analysis mainly used descriptive statistics. All statistical analyses were performed using the SPSS 22.0 or GraphPad Prism software.
Results
Patient characteristics and treatment
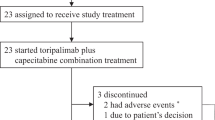
Between March 2019 and March 2021, 42 RM-NPC patients were screened and 39 were eligible (Fig. 1), including 33 males (84.6%) and 6 females (15.4%) (Table 1). Their median age was 48 (range, 20–64) years. Twelve patients (30.8%) had locally recurrent disease at nasopharynx and/or cervical lymph nodes. Twenty-four patients (61.5%) had liver metastasis and 18 (46.2%) had lung metastasis. Thirty-five patients (89.7%) had received primary tumor loco-regional radiotherapy. Ten patients (25.6%) had received at least three prior lines of systemic therapy. Nineteen patients (48.7%) had received anti-PD-1 immunotherapy and 15 (38.5%) had received anti-epidermal growth factor receptor (EGFR) antibody. All 39 patients received at least one dose of anlotinib. By the data cutoff (April 30, 2022), they had received a median of 4 (range, 0.5–20) cycles of anlotinib.
Anti-tumor activities
No patient achieved CR and 8 patients attained PR. The ORR was 20.5% (95% CI, 9.3 to 36.5). Twenty patients had SD and the DCR was 71.8% (95% CI, 55.1 to 85.0) (Table 2). Twenty-one patients (58.3%) had a reduction in target lesion size (Fig. 2). The median time to treatment response was 1.4 months (95% CI, 0.9 to 3.0), and the median DOR was 4.0 months (95% CI, 1.0 to 7.1). Three patients discontinued anlotinib before the 1st efficacy evaluation and were excluded from the per-protocol set (PPS). The ORR and DCR were similar in the PPS population (Table 2).
Tumor responses of 36 patients in the per-protocol set. A The waterfall plot shows the best percentage changes in target lesions from baseline according to Response Evaluation Criteria in Solid Tumours (RECIST), version 1.1. B The spider plot displays longitudinal changes from baseline in tumor size. The dotted lines at − 30% and 20% indicate partial response (PR) and progression per RECIST, respectively. C Treatment exposure and response duration. D Radiographic response by serial CT scans in pulmonary (upper panel) and hepatic (lower panel) metastases in nasopharyngeal carcinoma patients
The median duration of follow up was 17.2 (range, 1.3–32.7) months. Twenty-eight PFS events occurred, and the median PFS was 5.7 months (95% CI, 4.7 to 6.8) (Fig. 3A). The 6-month PFS rate was 36.1%. At the data cutoff, 21 deaths were reported. The 12-month OS was 58.3%, and the median OS was not reached (Fig. 3B).
Safety
Thirty-eight patients were included in the safety set. All patients had treatment-related AEs (TRAEs). The most frequent TRAEs of all grades were hand-foot syndrome (HFS, 63.2%), hypothyroidism (60.5%), hypertension (55.3%), oral mucositis (47.4%), and cholesterol elevation (43.6%) (Table 3). The most frequent grade 3/4 TRAEs were hand-foot syndrome (HFS, 23.7%), oral mucositis (21.0%), hypertension (7.9%), and triglyceride elevation (7.9%). Hemorrhage occurred in 34.2% of the patients, and all were grade 1/2. Nineteen patients (50%) had dose reduction due to TRAEs. Additionally, 4 patients (10.5%) experienced treatment interruptions due to TRAEs. Four patients (10.5%) discontinued anlotinib due to TRAEs, including pharyngeal necrosis (n = 2), HFS (n = 1), and bleeding (n = 1). No treatment-related death was reported.
Subgroup analysis
Patients who had received prior anti-PD-1 immunotherapy (n = 19, 48.7%) had a higher ORR (26.3% vs. 15.0%) and DCR (78.9% vs. 65.0%) than those had not received anti-PD-1 immunotherapy (n = 20, 51.3%). The duration of DCR was also longer in patients who had received prior anti-PD-1 immunotherapy versus those not (median duration of DCR, 24.3 weeks vs. 20.4 weeks) (Additional file 1: Fig S1). Five of the immunotherapy-exposed patients attained PR, and all of these patients finished anti-PD-1 immunotherapy less than 3 months before anlotinib treatment.
Patients with a baseline EBV DNA copy number < 1000 IU/mL (n = 22) had a higher DCR (61.1% vs. 38.8) and ORR (31.8% vs. 7.1%) than patients whose baseline EBV DNA copy number was ≥ 1000 IU/mL (n = 14) (Additional file 1: Fig S2A). The plasma EBV DNA copy number was dynamically monitored in 36 patients. Eighteen patients experienced a decline or no change from baseline, while 18 exhibited an increase in EBV DNA copy number after cycle 1. Patients with a decline or no change in EBV DNA copy number attained a higher DCR than those with an elevated EBV DNA copy number (94.4% vs. 61.1%) (Additional file 1: Fig S2B). Twenty-three patients developed HFS and had a higher DCR than those without HFS (91.3% vs. 53.8%) (Additional file 1: Fig S2A and C).
Discussion
In this trial, RM-NPC patients who received anlotinib monotherapy as third-line or further therapy demonstrated effective disease control and acceptable toxicity profile. Subgroup analysis identified plasma EBV DNA levels and HFS as prognostic factors of treatment response. The findings support further clinical development of anlotinib for RM-NPC patients who have dismal survival outcomes and limited treatment options.
Several antiangiogenic MKIs had been studied in RM-NPC (Additional file 1: Table S1) [7,8,9, 11, 23, 24]. Early trials of sorafenib [23] and sunitinib [11] had shown modest efficacy in RM-NPC but significant risk of fatal hemorrhages. Moderate toxicity was observed during pazopanib [7] and axitinib [8] treatment, but the response rate was still poor, with an ORR of 3.7% to 6.1%. Recent study has reported higher efficacy with apatinib [24] and lucitanib [9] treatment, with an ORR of 20% to 36.4% and a DCR of 54.5% to 90%. However, patients enrolled in the trials mentioned above were resistant to traditional chemotherapy, and most of them had not been exposed to targeted therapy or immunotherapy. In this trial, nearly half (48.7%) of the patients had received anti-PD-1 immunotherapy, and over one third had received anti-EGFR antibody. Anlotinib monotherapy demonstrated an ORR of 20.5%, a DCR of 71.8%, and a median PFS of 5.7 months, which was comparable with the efficacy results of apatinib and lucitanib. These results suggested anlotinib as a promising agent for heavily pretreated NPC patients with both high clinical benefit rate and durable disease control in the era of targeted therapy and immunotherapy. Such an efficacy may be attributed to the high affinity and selectivity of anlotinib for targeted kinases [13, 14].
In this study, patients with prior anti-PD-1 immunotherapy tended to have higher therapeutic efficacy to anlotinib treatment, especially for patients who finished anti-PD-1 immunotherapy less than 3 months before anlotinib treatment. This may be because the anti-tumor immunity remains activated in the short term after the end of immunotherapy, while antiangiogenic drugs could further increase the infiltration of immune effector cells in the tumor microenvironment by normalizing immature blood vessels [25]. The synergistic anti-tumor effect of antiangiogenic therapy and immunotherapy has been indicated by preclinical studies [25] and validated by clinical trials in renal carcinoma [26,27,28], endometrial carcinoma [29], and hepatocellular carcinoma [30]. Recent phase II study [31] has demonstrated the promising therapeutic efficacy and safety of camrelizumab plus apatinib in patients with recurrent or metastatic NPC who failed first-line therapy, with an ORR of 65.5% and a DCR of 86.2%. The phase II TORAL trial (ClinicalTrials.gov: NCT04996758) evaluating the efficacy and safety of anlotinib in combination with the anti-PD-1 antibody toripalimab in RM-NPC is currently ongoing.
Grade 3/4 HFS and oral mucositis observed in this trial were more common than previously reported for anlotinib monotherapy in patients with advanced non-small cell lung cancer, soft-tissue sarcoma, and medullary thyroid carcinoma [18, 20, 21]. The higher incidence of HFS and oral mucositis in RM-NPC may be attributed to previous exposure to chemotherapeutic agents commonly used in NPC, including 5-fluorouracil, capecitabine, docetaxel, and other multikinase inhibitors, which can also cause reactions involving the hands, feet, and mucosa [32]. Previous radiotherapy may have also contributed to the higher incidence of oral mucositis. HFS is reversible in most cases but may impact quality of life. In this trial, HFS was associated with better outcomes in RM-NPC patients with anlotinib treatment. The prognostic value of HFS had also been reported in patients with other advanced malignancies treated with MKIs including anlotinib [33, 34]. One of the main concerns with antiangiogenic agents is the occurrences of bleeding. In this trial, grade 1/2 bleeding occurred in 34.2% of the patients; however, no patient had grade 3/4 bleeding. Considering the occurrence of fatal hemorrhage reported during sunitinib treatment in RM-NPC patients who had received high-dose radiation [11], bleeding should also be monitored closely during the treatment of anlotinib in patients with previous radiotherapy.
In this trial, high baseline EBV DNA copy number (≥ 1000 IU/mL) and increase from baseline in EBV DNA level were all associated with higher rate of disease progression during the anlotinib treatment. In the pilot study of single-agent apatinib treatment in RM-NPC patients, low baseline EBV DNA level was associated with long-term response, while change of EBV-DNA level after apatinib treatment was not correlated with the duration of response [35]. These findings suggested that antiangiogenic therapies may be more effective in preventing disease progression in patients with low disease burden. However, although the correlation between treatment response and EBV DNA changes has also been reported in bevacizumab treatment for RM-NPC patients [6], this observation may speak to the anti-tumor efficacy of these drugs on overall disease burden. Therefore, change of plasma EBV DNA level may not be a specific biomarker for the efficacy of antiangiogenic therapies but should still be monitored during antiangiogenic treatment in NPC patients.
The study has several limitations. First, this is a single-arm study in the absence of a control group. Second, the results of dynamic monitoring of EBV DNA copy numbers were not available in all enrolled patients. Thirdly, the results of our subgroup analysis may be limited by the small cohort size. Finally, only Han Chinese subjects were included in the trial. The efficacy and safety of anlotinib should be evaluated in NPC patients of diverse ethnicities across countries in the future.
Conclusions
Anlotinib as a third- or later-line treatment is well tolerated and has demonstrated promising anti-tumor activity and disease control in heavily pretreated RM-NPC patients. The efficacy and safety of anlotinib in combination with immune checkpoint inhibitors for the treatment of RM-NPC patients should be further explored.
Availability of data and materials
The datasets used and analyzed during the current study are available on reasonable request from the corresponding author.
Abbreviations
- AEs:
-
Adverse events
- CR:
-
Complete response
- CTCAE:
-
Common Terminology Criteria for Adverse Events
- DOR:
-
Duration of response
- ECOG:
-
Eastern Cooperative Oncology Group
- EGFR:
-
Epidermal growth factor receptor
- FGFR:
-
Fibroblast growth factor receptor
- GP:
-
Cisplatin plus gemcitabine
- HFS:
-
Hand-foot syndrome
- IC50:
-
Half-maximal inhibitory concentration
- MKIs:
-
Antiangiogenic multikinase inhibitors
- NPC:
-
Nasopharyngeal carcinoma
- ORR:
-
Objective response rate
- OS:
-
Overall survival
- PD:
-
Progressive disease
- PDGFR:
-
Platelet-derived growth factor receptor
- PFS:
-
Progression-free survival
- PPS:
-
Per-protocol set
- PR:
-
Partial response
- RM-NPC:
-
Recurrent or metastatic nasopharyngeal carcinoma
- SD:
-
Stable disease
- TRAEs:
-
Treatment-related AEs
- VEGF:
-
Vascular endothelial growth factor
- VEGFR:
-
Vascular endothelial growth factor receptor
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–49.
Chua MLK, Wee JTS, Hui EP, Chan ATC. Nasopharyngeal carcinoma. Lancet. 2016;387(10022):1012–24.
Chen YP, Chan ATC, Le QT, Blanchard P, Sun Y, Ma J. Nasopharyngeal carcinoma. Lancet. 2019;394(10192):64–80.
Zhang L, Huang Y, Hong S, Yang Y, Yu G, Jia J, Peng P, Wu X, Lin Q, Xi X, et al. Gemcitabine plus cisplatin versus fluorouracil plus cisplatin in recurrent or metastatic nasopharyngeal carcinoma: a multicentre, randomised, open-label, phase 3 trial. Lancet. 2016;388(10054):1883–92.
Chen L, Lin G, Chen K, Liang R, Wan F, Zhang C, Tian G, Zhu X. VEGF promotes migration and invasion by regulating EMT and MMPs in nasopharyngeal carcinoma. J Cancer. 2020;11(24):7291–301.
Zhou T, Yang Y, Ma S, Lin L, Zhou T, Zhang C, Ding X, Wang R, Feng G, Chen Y, et al. Bevacizumab versus placebo in combination with paclitaxel and carboplatin as first-line treatment for recurrent or metastatic nasopharyngeal carcinoma: a multicentre, randomised, open-label, phase II trial. ESMO Open. 2021;6(6):100313.
Lim WT, Ng QS, Ivy P, Leong SS, Singh O, Chowbay B, Gao F, Thng CH, Goh BC, Tan DS, et al. A phase II study of pazopanib in Asian patients with recurrent/metastatic nasopharyngeal carcinoma. Clin Cancer Res. 2011;17(16):5481–9.
Hui EP, Ma BBY, Loong HHF, Mo F, Li L, King AD, Wang K, Ahuja AT, Chan CML, Hui CWC, et al. Efficacy, safety, and pharmacokinetics of axitinib in nasopharyngeal carcinoma: a preclinical and phase II correlative study. Clin Cancer Res. 2018;24(5):1030–7.
Zhang Y, Luo F, Ma YX, Liu QW, Yang YP, Fang WF, Huang Y, Zhou T, Li J, Pan HM, et al. A phase Ib study of lucitanib (AL3810) in a cohort of patients with recurrent and metastatic nasopharyngeal carcinoma. Oncologist. 2022;27(6):e453–62.
Soria JC, Deutsch E. Hemorrhage caused by antiangiogenic therapy within previously irradiated areas: expected consequence of tumor shrinkage or a warning for antiangiogenic agents combined to radiotherapy? Ann Oncol. 2011;22(6):1247–9.
Hui EP, Ma BBY, King AD, Mo F, Chan SL, Kam MKM, Loong HH, Ahuja AT, Zee BCY, Chan ATC. Hemorrhagic complications in a phase II study of sunitinib in patients of nasopharyngeal carcinoma who has previously received high-dose radiation. Ann Oncol. 2011;22(6):1280–7.
Fountzilas G, Fragkoulidi A, Kalogera-Fountzila A, Nikolaidou M, Bobos M, Calderaro J, Andreiuolo F, Marselos M. A phase II study of sunitinib in patients with recurrent and/or metastatic non-nasopharyngeal head and neck cancer. Cancer Chemother Pharmacol. 2010;65(4):649–60.
Lin B, Song X, Yang D, Bai D, Yao Y, Lu N. Anlotinib inhibits angiogenesis via suppressing the activation of VEGFR2, PDGFRβ and FGFR1. Gene. 2018;654:77–86.
Xie C, Wan X, Quan H, Zheng M, Fu L, Li Y, Lou L. Preclinical characterization of anlotinib, a highly potent and selective vascular endothelial growth factor receptor-2 inhibitor. Cancer Sci. 2018;109(4):1207–19.
Syed YY. Anlotinib: first global approval. Drugs. 2018;78(10):1057–62.
Li S. Anlotinib: a novel targeted drug for bone and soft tissue sarcoma. Front Oncol. 2021;11:664853.
Shen G, Zheng F, Ren D, Du F, Dong Q, Wang Z, Zhao F, Ahmad R, Zhao J. Anlotinib: a novel multi-targeting tyrosine kinase inhibitor in clinical development. J Hematol Oncol. 2018;11(1):120.
Li D, Chi Y, Chen X, Ge M, Zhang Y, Guo Z, Wang J, Chen J, Zhang J, Cheng Y, et al. Anlotinib in locally advanced or metastatic medullary thyroid carcinoma: a randomized, double-blind phase IIB trial. Clin Cancer Res. 2021;27(13):3567–75.
Chi Y, Shu Y, Ba Y, Bai Y, Qin B, Wang X, Xiong J, Xu N, Zhang H, Zhou J, et al. Anlotinib monotherapy for refractory metastatic colorectal cancer: a double-blinded, placebo-controlled, randomized phase III trial (ALTER0703). Oncologist. 2021;26(10):e1693–703.
Han B, Li K, Wang Q, Zhang L, Shi J, Wang Z, Cheng Y, He J, Shi Y, Zhao Y, et al. Effect of anlotinib as a third-line or further treatment on overall survival of patients with advanced non-small cell lung cancer: the ALTER 0303 phase 3 randomized clinical trial. JAMA Oncol. 2018;4(11):1569–75.
Chi Y, Fang Z, Hong X, Yao Y, Sun P, Wang G, Du F, Sun Y, Wu Q, Qu G, et al. Safety and efficacy of anlotinib, a multikinase angiogenesis inhibitor, in patients with refractory metastatic soft-tissue sarcoma. Clin Cancer Res. 2018;24(21):5233–8.
Ma B, Hui EP, King A, To KF, Mo F, Leung SF, Kam M, Lo YM, Zee B, Mok T, et al. A phase II study of patients with metastatic or locoregionally recurrent nasopharyngeal carcinoma and evaluation of plasma Epstein-Barr virus DNA as a biomarker of efficacy. Cancer Chemother Pharmacol. 2008;62(1):59–64.
Elser C, Siu LL, Winquist E, Agulnik M, Pond GR, Chin SF, Francis P, Cheiken R, Elting J, McNabola A, et al. Phase II trial of sorafenib in patients with recurrent or metastatic squamous cell carcinoma of the head and neck or nasopharyngeal carcinoma. J Clin Oncol. 2007;25(24):3766–73.
Ruan X, Liang JH, Pan Y, Cai R, Zhang RJ, He Z, Yang X, Niu Z, Jiang W. Apatinib for the treatment of metastatic or locoregionally recurrent nasopharyngeal carcinoma after failure of chemotherapy: a multicenter, single-arm, prospective phase 2 study. Cancer. 2021;127(17):3163–71.
Fukumura D, Kloepper J, Amoozgar Z, Duda DG, Jain RK. Enhancing cancer immunotherapy using antiangiogenics: opportunities and challenges. Nat Rev Clin Oncol. 2018;15(5):325–40.
Motzer RJ, Penkov K, Haanen J, Rini B, Albiges L, Campbell MT, Venugopal B, Kollmannsberger C, Negrier S, Uemura M, et al. Avelumab plus axitinib versus sunitinib for advanced renal-cell carcinoma. N Engl J Med. 2019;380(12):1103–15.
Rini BI, Plimack ER, Stus V, Gafanov R, Hawkins R, Nosov D, Pouliot F, Alekseev B, Soulières D, Melichar B, et al. Pembrolizumab plus axitinib versus sunitinib for advanced renal-cell carcinoma. N Engl J Med. 2019;380(12):1116–27.
Lee CH, Shah AY, Rasco D, Rao A, Taylor MH, Di Simone C, Hsieh JJ, Pinto A, Shaffer DR, Girones Sarrio R, et al. Lenvatinib plus pembrolizumab in patients with either treatment-naive or previously treated metastatic renal cell carcinoma (Study 111/KEYNOTE-146): a phase 1b/2 study. Lancet Oncol. 2021;22(7):946–58.
Makker V, Colombo N, Casado Herráez A, Santin AD, Colomba E, Miller DS, Fujiwara K, Pignata S, Baron-Hay S, Ray-Coquard I, et al. Lenvatinib plus pembrolizumab for advanced endometrial cancer. N Engl J Med. 2022;386(5):437–48.
Finn RS, Qin S, Ikeda M, Galle PR, Ducreux M, Kim TY, Kudo M, Breder V, Merle P, Kaseb AO, et al. Atezolizumab plus bevacizumab in unresectable hepatocellular carcinoma. N Engl J Med. 2020;382(20):1894–905.
Ding X, Zhang WJ, You R, Zou X, Wang ZQ, Ouyang YF, Peng L, Liu YP, Duan CY, Yang Q, et al. Camrelizumab plus apatinib in patients with recurrent or metastatic nasopharyngeal carcinoma: an open-label, single-arm, phase II study. J Clin Oncol. 2023;41(14):2571–82.
Miller KK, Gorcey L, McLellan BN. Chemotherapy-induced hand-foot syndrome and nail changes: a review of clinical presentation, etiology, pathogenesis, and management. J Am Acad Dermatol. 2014;71(4):787–94.
Ogawa C, Morita M, Omura A, Noda T, Kubo A, Matsunaka T, Tamaki H, Shibatoge M, Tsutsui A, Senoh T, et al. Hand-foot syndrome and post-progression treatment are the good predictors of better survival in advanced hepatocellular carcinoma treated with sorafenib: a multicenter study. Oncology. 2017;93(Suppl 1):113–9.
Nan X, Xie C, Zhu Q, Zhang J, Fu S, Han X, Zhang Q, Han B, Liu J. Hand-foot syndrome and survival in patients with advanced non-small-cell lung cancer receiving anlotinib: a subgroup analysis of data from the ALTER 0303 study. Int J Clin Oncol. 2020;25(8):1492–8.
Huang L, Zhang X, Bai Y, Chua KLM, Xie Y, Shu X, Long B, Fan C, Lim DWT, Tan SH, et al. Efficacy and safety of apatinib in recurrent/metastatic nasopharyngeal carcinoma: a pilot study. Oral Oncol. 2021;115:105222.
Acknowledgements
All the co-authors gratefully thank the patients and their families for participating in this study. Anlotinib was provided by Chia Tai Tianqing Pharmaceutical Group CO. Ltd.
Funding
This study was supported by the National Natural Science Foundation of China (No.81672686 to Prof. Qingqing Cai).
Author information
Authors and Affiliations
Contributions
Concept and design: QC and YF. Provision of study materials or patients: QC, YX, PL. Data analysis and interpretation: YF, NS, QC, QZ. Manuscript writing: all authors. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by the Ethics Committee of Sun Yat-Sen University Cancer Center (B2018-167). Written informed consent was obtained from all patients before enrollment.
Consent for publication
Consents for publication of individual person’s data have been obtained from those patients.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Figure S1.
Treatment exposure and response duration of immunotherapy-exposed and immunotherapy-naïve patients. Figure S2. Subgroup Analysis. (A) Forest plot analysis of DCR by patient subgroups. (B) Best response and EBV DNA change. Changes in plasma EBV DNA copy number post cycle 1 from baseline (left panel) and treatment responses of patients (right panel). (C) Hand-foot syndrome in patients treated with anlotinib (left panel) and treatment responses of patients per occurrence of hand-foot syndrome (right panel). Patient responses are colored coded. EBV, Epstein-Barr virus; PD, progressive disease; PR, partial response; SD, stable disease. Table S1. Studies of antiangiogenic multikinase inhibitors in recurrent and metastatic nasopharyngeal carcinoma.
Additional file 2.
Study protocol.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Fang, Y., Su, N., Zou, Q. et al. Anlotinib as a third-line or further treatment for recurrent or metastatic nasopharyngeal carcinoma: a single-arm, phase 2 clinical trial. BMC Med 21, 423 (2023). https://doi.org/10.1186/s12916-023-03140-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12916-023-03140-x