Abstract
Background
Previous studies that assessed the risk of cardiovascular outcomes in survivors of coronavirus disease 2019 (COVID-19) were likely limited by lack of generalizability and selection of controls nonrepresentative of a counterfactual situation regarding COVID-19-related hospitalization. This study determined whether COVID-19 hospitalization was associated with incident cardiovascular outcomes compared to non-COVID-19 pneumonia hospitalization.
Methods
Nationwide population-based study conducted using the Korean National Health Insurance Service database. A cohort of 132,784 inpatients with COVID-19 (October 8, 2020–September 30, 2021) and a cohort of 31,173 inpatients with non-COVID-19 pneumonia (January 1–December 31, 2019) were included. The primary outcome was the major adverse cardiovascular event (MACE; a composite of myocardial infarction and stroke). Hazard ratios (HRs) with 95% confidence intervals (CIs) of all outcomes of interest were estimated between inverse probability of treatment-weighted patients with COVID-19 and non-COVID-19 pneumonia.
Results
After weighting, the COVID-19 and non-COVID-19 pneumonia groups included 125,810 (mean [SD] age, 47.2 [17.6] years; men, 49.3%) and 28,492 patients (mean [SD] age, 48.6 [18.4] years; men, 47.2%), respectively. COVID-19 hospitalization was not associated with an increased risk of the MACE (HR, 0.84; 95% CI 0.69–1.03). However, the MACE (HR, 7.30; 95% CI 3.29–16.21), dysrhythmia (HR, 1.88; 95% CI 1.04–3.42), acute myocarditis (HR, 11.33; 95% CI 2.97–43.20), myocardial infarction (HR, 6.78; 95% CI 3.03–15.15), congestive heart failure (HR, 1.95; 95% CI 1.37–2.77), and thrombotic disease (HR, 8.26; 95% CI 4.06–16.83) risks were significantly higher in patients with COVID-19 aged 18–39 years. The findings were consistent after adjustment for preexisting cardiovascular disease. COVID-19 hospitalization conferred a higher risk of acute myocarditis (HR, 6.47; 95% CI 2.53–16.52) or deep vein thrombosis (HR, 1.97; 95% CI 1.38–2.80), regardless of vaccination status.
Conclusions
Hospitalized patients with COVID-19 were not at an increased risk of cardiovascular outcomes compared to patients with non-COVID-19 pneumonia. Further studies are needed to evaluate whether the increased risk of cardiovascular outcomes is confined to younger patients.
Similar content being viewed by others
Background
By September 6, 2023, the coronavirus disease 2019 (COVID-19) had affected more than 770 million people and caused over 6 million deaths worldwide [1]. Increasing levels of immunity and the development of novel therapies and vaccines have substantially reduced mortality rates. However, 6.2% of patients who recover from acute infection experience persistent symptoms, including fatigue, cognitive problems, or respiratory problems, known as post-COVID conditions [2].
The acute cardiovascular manifestations of COVID-19, which include thrombosis, dysrhythmia, heart failure, and shock, are associated with increased mortality [3]. Previous investigations of the risk of cardiovascular outcomes in the post-acute stage of COVID-19 in hospitalized patients were limited by inadequate risk adjustment for preexisting cardiovascular disease [4, 5]. In a cohort of 153,760 patients from the US Department of Veterans Affairs database, patients who survived acute COVID-19 were at increased risk of cardiovascular outcomes 1 year after infection, regardless of a history of cardiovascular disease or care setting (non-hospitalized, hospitalized, and intensive care unit admission), but the demographic composition (mostly White, older male) may limit the generalizability of the results and the COVID-19-specific sequelae were not assessed [6]. Hospitalization for pneumonia due to pathogens other than the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) may confer a risk of long-term cardiovascular morbidity [7].
Using a Korean nationwide population-based cohort of patients without preexisting cardiovascular disease, we investigated the risk of cardiovascular outcomes among those who survived acute COVID-19 hospitalization. A cohort of hospitalized patients with non-COVID-19 pneumonia was used as a historical comparison group.
Methods
Data source
This retrospective cohort analysis collected data from the Korean National Health Insurance Service (NHIS) database, which includes claim codes from all citizens who reside in Korea, excluding medical aid beneficiaries and healthcare beneficiaries for veterans (~ 97% of the population in 2022) [8]. The database consists of detailed information regarding demographics; primary and secondary diagnoses; prescription and procedure charges; discharge status; and date of death. Diagnostic codes are based on the International Classification of Diseases, 10th Revision (ICD-10). The reimbursement scheme in Korea is based on fee-for-service and does not incentivize upcoding. All prescribed drugs were identified by Anatomical Therapeutic Chemical codes and the Korean Health Insurance Review and Assessment Service charge codes. The NHIS database was linked to the Korean nationwide COVID-19 registry constructed by the Korea Disease Control and Prevention Agency for confirming cases that involved COVID-19 diagnosis (positive real-time reverse transcription polymerase chain reaction from a nasopharyngeal swab) [9] and vaccination. All data were retrieved by an independent technician from the NHIS center.
The requirement for ethical approval was waived by the Institutional Review Board of Chung-Ang University due to analysis of de-identified patient records (1041078–202203-HR-086). The present study complied with the Strengthening the Reporting of Observational Studies in Epidemiology guidelines.
Study population
The COVID-19 group comprised adults (age ≥ 18 years) with confirmed COVID-19 and who were hospitalized between October 8, 2020, and September 30, 2021. The index date was defined as the date of hospitalization. To ensure that the COVID-19 group had a similar follow-up duration as the control group, all patients were followed from the index date to the date of death or 3 months after the end of inclusion period, which was December 31, 2021.
The non-COVID-19 pneumonia group was constructed as a historical control group to (1) compare the risk of cardiovascular outcomes with those of COVID-19 hospitalization and (2) evaluate the sequelae specific to COVID-19. The group included adults (age ≥ 18 years) who were hospitalized for pneumonia caused by pathogens other than SARS-CoV-2 between January 1 and December 31, 2019. Additional file 1: Appendix 1 includes a detailed description of the types of pathogens and the ICD-10 codes. The last follow-up was on March 31, 2020.
For patients with multiple admissions, only the first admission was included. The exclusion criteria were (1) age < 18 years; (2) hospitalization prior to the index date; (3) preexisting cardiovascular disease identified using the ICD-10 codes within 1 year before the index date; and (4) death within the first 30 days following the index date. Preexisting cardiovascular diseases included stroke (ischemic or hemorrhagic); transient ischemic attack (TIA); atrial fibrillation; atrial flutter; ventricular arrhythmias; acute pericarditis; acute myocarditis; myocardial infarction; congestive heart failure; cardiac arrest; pulmonary embolism; and deep vein thrombosis (Additional file 2: Table S1).
Data collection and definitions
Baseline covariates included age; sex; Charlson comorbidities [10] defined using claim codes within 1 year preceding the index date (Additional file 2: Table S2); income level; and hospital size. Body mass index (BMI) and smoking status were additionally retrieved in patients who had undergone a national health examination within 1 year before the index date. Cardiovascular drug therapies prescribed within 1 year before the index date were also extracted (Additional file 2: Table S3). Cardiovascular drug users were defined as patients who used any of the drugs above within 1–30 days before the index hospitalization, given that it was unlikely that these medications were discontinued within 1 month before the said hospitalization. The type of organ dysfunction was identified using the ICD-10 codes (Additional file 2: Table S4). Vasopressor use was defined as the infusion of norepinephrine, epinephrine, vasopressin, dopamine, or dobutamine during the index hospitalization. Procedure codes were retrieved to identify clinical care variables, including supplemental oxygen, high-flow nasal cannula, mechanical ventilation, renal replacement therapy, and extracorporeal membrane oxygenation (ECMO). Mild to moderate illness was defined as no oxygen therapy or receiving supplemental oxygen. Severe to critical illness was defined as receiving high-flow nasal cannula, mechanical ventilation, and/or ECMO.
Outcomes
The primary outcome was the major adverse cardiovascular event (MACE; a composite of myocardial infarction and stroke) [11]. The secondary outcomes were all-cause mortality and each cardiovascular disease. For outcome variables, stroke, TIA, and myocardial infarction were identified using the combination of relevant ICD-10 codes and imaging [12] or procedure codes (Additional file 1: Appendix 2). The first incidence of any of the outcomes between 30 days after the index date and the end of follow-up was assessed. The first 30 days were excluded due to the complexity of differentiating outcomes as COVID-19 complications from the acute disease process.
Statistical analysis
Data are reported as the mean (standard deviation, SD) or median (interquartile range, IQR) for continuous variables and as the frequency (percentage) for categorical variables. The occurrence of primary and secondary outcomes was presented as the cumulative incidence and incidence rates.
Propensity score (PS) analysis using inverse probability of treatment weighting (IPTW) was performed to adjust for potential confounding by baseline characteristics when comparing the COVID-19 and non-COVID-19 pneumonia groups. The PS for each patient was estimated using logistic regression model with COVID-19 as an independent variable and age, sex, comorbidities, income level, hospital size, cardiovascular drug therapies, organ dysfunction, vasopressor use, oxygen therapies, renal replacement therapy, and ECMO as covariates. Then, the PS was used to calculate the inverse probability weight as the probability of being in the COVID-19 group divided by 1 – the probability of being in the COVID-19 group. The IPTW creates a pseudo-population in which baseline covariates are balanced, meaning that both groups have similar proportions of covariates. The method has advantage of increasing power without changing the underlying estimates. To improve the precision of IPTW and reduce bias related to unmeasured confounders, 2.5% from each tail of the PS distribution was trimmed [13]. Covariate balance before and after weighting was assessed by standardized mean differences (SMDs). Hazard ratios (HRs) with 95% confidence intervals (CIs) of the incident primary and secondary outcomes between the groups were estimated from the Fine-Gray subdistribution hazard models where death was considered as a competing risk [14]. In addition, COVID-19 vaccination was employed as a time-varying covariate to eliminate any contribution of vaccine exposure to the potential risk of thrombosis, pericarditis, or myocarditis [15].
Subgroup analyses for the primary and secondary outcomes were conducted according to age (stratified by 18–39, 40–64, and ≥ 65 years); sex; diabetes; hypertension; dyslipidemia; Charlson Comorbidity Index; number of organ dysfunctions; and illness severity. Individual secondary outcomes were combined in a related category of composite outcome (e.g., stroke and TIA were combined to cerebrovascular disease). Multiple sensitivity analyses were performed to test the robustness of the main results. First, the analyses were re-run including patients with preexisting cardiovascular disease, who may be more vulnerable to COVID-19 complications. Second, the initial PS model did not include BMI and smoking status because these data were lacking in a considerable proportion of patients. Thus, a separate analysis investigated possible confounding by BMI and smoking status that included only patients who had these data. Third, some patients may have been diagnosed as stroke or TIA without brain imaging. Thus, the survival models with cerebrovascular outcomes identified using only the ICD-10 codes were utilized. Fourth, the associations between COVID-19 vaccination and MACE, myocardial infarction, stroke, and all-cause mortality were evaluated to assess if vaccines prevent cardiovascular outcomes.
No imputation strategy was conducted due to the small percentage of missing data (0.07%). All tests were two-tailed, and differences were considered statistically significant at a P value of < 0.05. All analyses were performed using SAS version 9.4 (SAS Institute, Cary, NC, USA).
Results
Study population
During the study period, 161,165 individuals were hospitalized with COVID-19 (Fig. 1). After excluding those who met the exclusion criteria, 132,784 participants were included in the main analysis. In the control group, of the 184,937 patients with non-COVID-19 pneumonia who were hospitalized during the pre-COVID-19 period, 31,173 were included.
Patients hospitalized with COVID-19 were more likely to be younger, male, having less comorbidities, having higher income, and admitted in a higher volume hospital (Table 1). Patients with COVID-19 were less likely to have been prescribed with cardiovascular drug therapies. Moreover, the COVID-19 group less frequently developed organ dysfunction and received a lower intensity of organ support. The baseline characteristics and cardiovascular outcomes of study patients who died within the first 30 days following the index date are shown in Additional file 2: Tables S5 and S6. COVID-19 non-survivors were more likely to have cardiovascular risk factors, have been prescribed with cardiovascular drug therapies, develop organ dysfunction, and receive a higher intensity of organ support. However, the incidence of cardiovascular outcomes were generally comparable between the groups, except for the higher rates of atrial fibrillation (2.6% vs 1.4%) and deep vein thrombosis (3.5% vs 0.3%) in COVID-19 non-survivors.
Incident primary and secondary outcomes in COVID-19 vs non-COVID-19 pneumonia
After weighting, the COVID-19 and non-COVID-19 pneumonia groups included 125,810 (mean [SD] age, 47.2 [17.6] years; men, 49.3%) and 28,492 patients (mean [SD] age, 48.6 [18.4] years; men, 47.2%), respectively (Table 1). SMDs in baseline characteristics between the groups were all less than 0.10, indicating that covariates were well-balanced. The median (IQR) follow-up in the COVID-19 and non-COVID-19 pneumonia groups was 169 (128–287) and 277 (142–376) days, respectively. The COVID-19 and non-COVID-19 pneumonia groups had 26,106,978 and 7,589,952 person-days of follow-up, respectively.
Overall, the incidence rate of MACE (per 1,000,000 person-days) was 14.8 and 21.2 among patients who survived the first 30 days of COVID-19 and non-COVID-19 pneumonia hospitalization, respectively (Fig. 2 and Additional file 2: Table S7). The risk was not significantly higher in the COVID-19 group (HR, 0.84; 95% CI 0.69–1.03). The cumulative incidence of MACE, myocardial infarction, stroke, and all-cause mortality in both groups are shown in Fig. 3. The all-cause mortality, congestive heart failure, and cardiac arrest risks were significantly lower in the COVID-19 group (Fig. 2 and Additional file 2: Table S7). Conversely, patients who survived acute COVID-19 hospitalization presented with a significantly higher risk of acute myocarditis (HR, 6.47; 95% CI 2.53–16.52) or deep vein thrombosis (HR, 1.97; 95% CI 1.38–2.80).
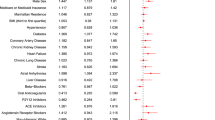
Risk of cardiovascular outcomes in participants hospitalized for COVID-19 or non-COVID-19 pneumonia. The hazard ratios and 95% CIs have been estimated in the inverse probability of treatment-weighted COVID-19 (n = 125,810) and non-COVID-19 pneumonia (n = 28,492) groups. The length of the bar represents the incidence rates per 1,000,000 person-days. CI confidence interval, COVID-19 coronavirus disease 2019, MACE major adverse cardiovascular event, TIA transient ischemic attack. * A composite of myocardial infarction and stroke
Cumulative incidence of A MACE, B myocardial infarction, C stroke, and D all-cause mortality in the COVID-19 and non-COVID-19 pneumonia groups. The median (interquartile range) time to MACE was 91 (53–156) and 76 (46–162) days in the COVID-19 and non-COVID-19 pneumonia groups, respectively. COVID-19 coronavirus disease 2019, MACE major adverse cardiovascular event. * A composite of myocardial infarction and stroke
Subgroup analyses
The results of subgroup analyses were generally consistent with those in the primary analysis, although some did not reach statistical significance (Fig. 4 and Additional file 2: Table S8). Notably, the MACE (HR, 7.30; 95% CI 3.29–16.21), dysrhythmia (HR, 1.88; 95% CI 1.04–3.42), acute myocarditis (HR, 11.33; 95% CI 2.97–43.20), myocardial infarction (HR, 6.78; 95% CI 3.03–15.15), congestive heart failure (HR, 1.95; 95% CI 1.37–2.77), and thrombotic disease (HR, 8.26; 95% CI 4.06–16.83) risks were significantly higher in patients with COVID-19 aged 18–39 years. The risk of acute myocarditis was also significantly higher in COVID-19 patients who had no cardiovascular risk factors, less comorbidities, less organ dysfunction, and mild to moderate illness. Higher HR of acute myocarditis was observed in male compared to female patients. For thrombotic disease, the risk was significantly higher in female patients with COVID-19 who had no cardiovascular risk factors, less comorbidities, less organ dysfunction, and mild to moderate illness.
Subgroup analyses comparing the risk of cardiovascular outcomes in participants hospitalized for COVID-19 or non-COVID-19 pneumonia. The hazard ratios and 95% CIs have been estimated in the inverse probability of treatment-weighted COVID-19 (n = 125,810) and non-COVID-19 pneumonia (n = 28,492) groups. CI confidence interval, COVID-19 coronavirus disease 2019, MACE major adverse cardiovascular event. * A composite of myocardial infarction and stroke
Sensitivity analyses
First, for the analyses including patients with preexisting cardiovascular disease, baseline comorbidities, cardiovascular drug therapies, organ dysfunction, and organ support were more prevalent than those in the primary cohort (Additional file 2: Table S9). The risks of the most cardiovascular outcomes were significantly lower in the COVID-19 group (Additional file 2: Table S10 and Additional file 3: Fig. S1), although the risk of acute myocarditis (HR, 1.99; 95% CI 1.09–3.64) and deep vein thrombosis (HR, 0.61; 95% CI 0.51–0.73) in the COVID-19 group were attenuated after adjustment for preexisting cardiovascular disease. Similar to the primary cohort, the risks of MACE, acute myocarditis, myocardial infarction, and thrombotic disease were significantly higher in patients with COVID-19 aged 18–39 years, although HRs decreased compared to those in the primary cohort (Additional file 2: Table S11 and Additional file 3: Fig. S2). Second, the PS model with available BMI and smoking status data constructed a cohort with similar baseline characteristics compared to the primary cohort (Additional file 2: Table S12). Subgroup analyses with stratification according to BMI and smoking status showed no significant interaction with any variable (Additional file 2: Table S13 and Additional file 3: Fig. S3). Third, the results of the analyses were consistent when only the ICD-10 code-based cerebrovascular outcomes were included (Additional file 2: Table S14). Fourth, the risks of MACE, myocardial infarction, stroke, and all-cause mortality increased in COVID-19 patients who were not vaccinated (Additional file 3: Fig. S4).
Discussion
This large-scale, population-based study of 154,302 Korean patients did not reveal a higher incidence of post-acute cardiovascular outcomes in patients with COVID-19 hospitalization compared to those hospitalized with non-COVID-19 pneumonia. The findings were consistent after adjustment for preexisting cardiovascular disease. However, the risks were higher in patients with COVID-19 aged 18–39 years. COVID-19 patients had a higher risk of acute myocarditis or deep vein thrombosis, regardless of vaccination status. The risks were more pronounced among younger patients with less comorbidities and illness severity. Finally, the current results suggest that COVID-19 vaccination may prevent cardiovascular outcomes.
Several studies from the large US, UK, or global database have provided substantial evidence that the risk of cardiovascular outcomes was significantly higher in COVID-19 survivors compared to non-COVID-19 controls [6, 16, 17]. COVID-19 is associated with endothelial dysfunction and a prothrombic state [18], which can result in micro- and macrovascular thrombosis with subsequent injury to various organs [19]. Furthermore, putative mechanisms include fibrosis and scarring of cardiac tissue due to increased proinflammatory cytokine secretion and activation of transforming growth factor-β signaling and metabolic changes that favor viral survival, resulting in persistent inflammation and tissue injury [20, 21].
Despite these mechanisms, COVID-19 hospitalization was not associated with the increased risk of cardiovascular outcomes in the present study. There are several explanations for these observations. First, a weighted control group was selected from hospitalized patients with non-COVID-19 pneumonia. This study design was based on the mechanisms that the risk of cardiovascular disease may be increased by proinflammatory changes of the atherosclerotic lesions [22], persistent inflammation [23], and persistent procoagulant state [24], which can be observed in non-COVID-19 pneumonia. Comparable rates of organ dysfunction and intensity of organ support were found between the COVID-19 and non-COVID-19 pneumonia groups. Alternatively, previous studies compared outcomes after COVID-19 and general hospital admission [6, 16, 17], which lacks adequate consideration of differential risk by pneumonia severity, and thereby does not necessarily represent an appropriate counterfactual situation to COVID-19 hospitalization. Second, there may be geographic variations in the prevalence of COVID-19 and cardiovascular disease; most previous studies evaluated cardiovascular outcomes in the Western countries. The current study in an Asian population may be clinically relevant, given that angiotensin-converting enzyme 2 expression in tissues differs in the East Asian populations compared to other non-Asian populations under similar conditions [25].
The present study excluded patients who died or had any cardiovascular outcomes within the first 30 days of hospital admission, because cardiac injury is often associated with multiorgan dysfunction during critical illness rather than the disease itself [26]. This method may lead to an underestimation of the true risk of cardiovascular outcomes among patients with COVID-19. For instance, recent studies have shown that cardiovascular complications often preceded death in non-survivors, compared to patients who survived, and most events occurred within 30 days of infection [16, 27]. However, the incidence of outcomes were generally comparable between non-survivors with COVID-19 and non-COVID-19 pneumonia, although the COVID-19 group were more likely to have cardiovascular risk factors and greater illness severity. Moreover, the median time to MACE was longer than 30 days in both groups.
The finding that the increased risk of cardiovascular outcomes is confined to younger patients (aged 18–39 years), who are less likely to have comorbidities and classic cardiovascular risk factors, implies that COVID-19 may be an independent risk factor in this subgroup. Furthermore, the risks were attenuated after adjustment for preexisting cardiovascular disease. However, these should be interpreted with caution due to relatively small number of events producing wide CIs. Acute myocarditis associated with COVID-19 can present as a direct cardiac injury mediated by SARS-CoV-2, which could trigger a nonspecific inflammation using molecular mimicry between viral proteins and cardiomyocytes [28, 29]. The current finding that the risk of acute myocarditis was significantly higher in the COVID-19 group suggest that myocarditis may be triggered by SARS-CoV-2 independently of the occurrence of pneumonia. Furthermore, the increased risk of acute myocarditis, regardless of vaccination status, among younger COVID-19 patients with no cardiovascular comorbidities and less illness severity supports the notion that SARS-CoV-2 may act as an independent risk factor. Notably, the risk of acute myocarditis was more pronounced among COVID-19 patients without preexisting cardiovascular disease. A higher risk of acute myocarditis was observed in male COVID-19 patients, which contrasts with the Western studies showing that female COVID-19 survivors had a higher risk of myocarditis [17]. The risk of deep vein thrombosis was significantly higher in the COVID-19 group without preexisting cardiovascular disease, and this observation is consistent with the results of previous studies [5, 6, 16, 30]. Finally, the finding that vaccination against COVID-19 was associated with a decreased risk of cardiovascular outcomes is consistent with previous studies supporting vaccination, especially for patients with preexisting cardiovascular disease [12].
To the best of our knowledge, this is the first study to assess whether COVID-19 hospitalization was associated with cardiovascular outcomes compared to hospitalization for pneumonia due to other respiratory pathogens in a nationwide cohort of Asian patients. The study derived its cohorts from an entire population in Korea to increase generalizability and had sufficient power to quantify multiple and rare outcomes overall and across various subgroups. In addition, all available baseline covariates were included in the PS used for weighting, and the primary results were generally consistent with multiple sensitivity analyses. Previous studies may have misclassified individuals due to the inherent limitations of using claims data to define variables. For instance, some COVID-19 patients might have been enrolled in the control group if they did not have enough symptoms to be tested. To overcome this limitation, controls were recruited from patients hospitalized before the pandemic (January 1–December 31, 2019) in the present study. Cerebrovascular outcomes and myocardial infarction were rigorously defined using the ICD-10 codes and related imaging or procedures rather than just the codes to obtain more reliable results.
The current study has several limitations. First, the retrospective observational design precludes any causal inference regarding the associations between COVID-19, non-COVID-19 pneumonia, and cardiovascular outcomes. Moreover, there were differences in baseline characteristics between the groups. A robust model was used to reduce the effect of such differences, but the possibility of unmeasured confounders exists. Second, the accuracy of the ICD-10 codes may be limited. It is possible that all ICD-10 codes for each outcome might not have been captured, although the most common ones were included. In addition, patients who had asymptomatic infections or resided in nursing homes for palliative care who were not hospitalized may also develop post-acute complications but were not included. Meanwhile, this approach might have described a more specific population of severe pneumonia. Third, the database did not include information regarding vital signs and laboratory data, but diagnoses, prescriptions, and procedures were used as surrogates of pneumonia severity. Fourth, the diagnosis of acute myocarditis was not supported by histological evidence or cardiac magnetic resonance imaging [31, 32]. Furthermore, a very small number of events (< 100) may be a limiting factor in analysis. Fifth, the increased risk of acute myocarditis in COVID-19 patients might be a result of increased medical care after SARS-CoV-2 infection. However, this ascertainment bias is unlikely to fully explain the present results because the risk of other cardiovascular outcomes was not higher in the COVID-19 group. Sixth, the cardiovascular manifestations of COVID-19 may change over time with the emergence of new variants that induce varying degrees of severity [33]. However, a subgroup analysis assessing the risk of cardiovascular outcomes according to different SARS-CoV-2 variants was not feasible due to lack of data. Seventh, unequal follow-up in the study groups, probably due to differing distribution of the index dates, may bias the analysis. In addition, the follow-up time was relatively short, although the median time to MACE was less than 100 days for both the COVID-19 and non-COVID-19 pneumonia groups.
Conclusions
Korean patients who survived acute COVID-19 hospitalization were not at increased risk of cardiovascular outcomes than those who were hospitalized with non-COVID-19 pneumonia. The present results indicate that the size and direction of the estimates may depend on the choice of control admissions. The findings that the risk of acute myocarditis or deep vein thrombosis was higher in the COVID-19 group are consistent with previous studies suggesting clinically at-risk population. The increased risk of cardiovascular outcomes in younger patients with COVID-19 warrants further study.
Availability of data and materials
All data generated or analyzed during this study are included in this published article and its supplementary information files.
Abbreviations
- BMI:
-
Body mass index
- CI:
-
Confidence interval
- COVID-19:
-
Coronavirus disease 2019
- ECMO:
-
Extracorporeal membrane oxygenation
- HR:
-
Hazard ratio
- ICD:
-
International Classification of Diseases
- IPTW:
-
Inverse probability of treatment weighting
- IQR:
-
Interquartile range
- MACE:
-
Major adverse cardiovascular event
- NHIS:
-
National Health Insurance Service
- PS:
-
Propensity score
- SARS-CoV-2:
-
Severe acute respiratory syndrome coronavirus 2
- SD:
-
Standard deviation
- SMD:
-
Standardized mean difference
- TIA:
-
Transient ischemic attack
References
World Health Organization: Coronavirus disease (COVID-19) pandemic. https://www.who.int/emergencies/diseases/novel-coronavirus-2019 (2023). Accessed 7 Sept 2023.
Global Burden of Disease Long COVID Collaborators, Wulf Hanson S, Abbafati C, Aerts JG, Al-Aly Z, Ashbaugh C, et al. Estimated global proportions of individuals with persistent fatigue, cognitive, and respiratory symptom clusters following symptomatic COVID-19 in 2020 and 2021. JAMA. 2022;328:1604–15.
Guzik TJ, Mohiddin SA, Dimarco A, Patel V, Savvatis K, Marelli-Berg FM, et al. COVID-19 and the cardiovascular system: implications for risk assessment, diagnosis, and treatment options. Cardiovasc Res. 2020;116:1666–87.
Ayoubkhani D, Khunti K, Nafilyan V, Maddox T, Humberstone B, Diamond I, et al. Post-covid syndrome in individuals admitted to hospital with covid-19: retrospective cohort study. BMJ. 2021;372: n693.
Daugherty SE, Guo Y, Heath K, Dasmariñas MC, Jubilo KG, Samranvedhya J, et al. Risk of clinical sequelae after the acute phase of SARS-CoV-2 infection: retrospective cohort study. BMJ. 2021;373: n1098.
Xie Y, Xu E, Bowe B, Al-Aly Z. Long-term cardiovascular outcomes of COVID-19. Nat Med. 2022;28:583–90.
Corrales-Medina VF, Alvarez KN, Weissfeld LA, Angus DC, Chirinos JA, Chang CC, et al. Association between hospitalization for pneumonia and subsequent risk of cardiovascular disease. JAMA. 2015;313:264–74.
National Health Insurance Service: Population coverage. https://www.nhis.or.kr/english/wbheaa02400m01.do (2022). Accessed 27 May 2023.
Corman VM, Landt O, Kaiser M, Molenkamp R, Meijer A, Chu DK, et al. Detection of 2019 novel coronavirus (2019-nCoV) by real-time RT-PCR. Euro Surveill. 2020;25:2000045.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83.
Bosco E, Hsueh L, McConeghy KW, Gravenstein S, Saade E. Major adverse cardiovascular event definitions used in observational analysis of administrative databases: a systematic review. BMC Med Res Methodol. 2021;21:241.
Kim YE, Huh K, Park YJ, Peck KR, Jung J. Association between vaccination and acute myocardial infarction and ischemic stroke after COVID-19 infection. JAMA. 2022;328:887–9.
Desai RJ, Franklin JM. Alternative approaches for confounding adjustment in observational studies using weighting based on the propensity score: a primer for practitioners. BMJ. 2019;367: l5657.
Austin PC, Lee DS, Fine JP. Introduction to the analysis of survival data in the presence of competing risks. Circulation. 2016;133:601–9.
Modin D, Jørgensen ME, Gislason G, Jensen JS, Køber L, Claggett B, et al. Influenza vaccine in heart failure. Circulation. 2019;139:575–86.
Raisi-Estabragh Z, Cooper J, Salih A, Raman B, Lee AM, Neubauer S, et al. Cardiovascular disease and mortality sequelae of COVID-19 in the UK Biobank. Heart. 2022;109:119–26.
Wang W, Wang CY, Wang SI, Wei JC. Long-term cardiovascular outcomes in COVID-19 survivors among non-vaccinated population: a retrospective cohort study from the TriNetX US collaborative networks. EClinicalMedicine. 2022;53: 101619.
Jin Y, Ji W, Yang H, Chen S, Zhang W, Duan G. Endothelial activation and dysfunction in COVID-19: from basic mechanisms to potential therapeutic approaches. Signal Transduct Target Ther. 2020;5:293.
Varga Z, Flammer AJ, Steiger P, Haberecker M, Andermatt R, Zinkernagel AS, et al. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020;395:1417–8.
Farshidfar F, Koleini N, Ardehali H. Cardiovascular complications of COVID-19. JCI Insight. 2021;6: e148980.
Andrade Silva M, da Silva ARPA, do Amaral MA, Fragas MG, Câmara NOS. Metabolic alterations in SARS-CoV-2 infection and its implication in kidney dysfunction. Front Physiol. 2021;12:624698.
Naghavi M, Wyde P, Litovsky S, Madjid M, Akhtar A, Naguib S, et al. Influenza infection exerts prominent inflammatory and thrombotic effects on the atherosclerotic plaques of apolipoprotein E-deficient mice. Circulation. 2003;107:762–8.
Yende S, D’Angelo G, Kellum JA, Weissfeld L, Fine J, Welch RD, et al. Inflammatory markers at hospital discharge predict subsequent mortality after pneumonia and sepsis. Am J Respir Crit Care Med. 2008;177:1242–7.
Yende S, D’Angelo G, Mayr F, Kellum JA, Weissfeld L, Kaynar AM, et al. Elevated hemostasis markers after pneumonia increases one-year risk of all-cause and cardiovascular deaths. PLoS ONE. 2011;6: e22847.
Cao Y, Li L, Feng Z, Wan S, Huang P, Sun X, et al. Comparative genetic analysis of the novel coronavirus (2019-nCoV/SARS-CoV-2) receptor ACE2 in different populations. Cell Discov. 2020;6:11.
Metkus TS, Sokoll LJ, Barth AS, Czarny MJ, Hays AG, Lowenstein CJ, et al. Myocardial injury in severe COVID-19 compared with non-COVID-19 acute respiratory distress syndrome. Circulation. 2021;143:553–65.
Pellicori P, Doolub G, Wong CM, Lee KS, Mangion K, Ahmad M, et al. COVID-19 and its cardiovascular effects: a systematic review of prevalence studies. Cochrane Database Syst Rev. 2021;3:CD013879.
Chen L, Li X, Chen M, Feng Y, Xiong C. The ACE2 expression in human heart indicates new potential mechanism of heart injury among patients infected with SARS-CoV-2. Cardiovasc Res. 2020;116:1097–100.
Ammirati E, Frigerio M, Adler ED, Basso C, Birnie DH, Brambatti M, et al. Management of acute myocarditis and chronic inflammatory cardiomyopathy: an expert consensus document. Circ Heart Fail. 2020;13: e007405.
Katsoularis I, Fonseca-Rodríguez O, Farrington P, Jerndal H, Lundevaller EH, Sund M, et al. Risks of deep vein thrombosis, pulmonary embolism, and bleeding after covid-19: nationwide self-controlled cases series and matched cohort study. BMJ. 2022;377: e069590.
Caforio AL, Pankuweit S, Arbustini E, Basso C, Gimeno-Blanes J, Felix SB, et al. Current state of knowledge on aetiology, diagnosis, management, and therapy of myocarditis: a position statement of the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur Heart J. 2013;34:2636–48.
Ferreira VM, Schulz-Menger J, Holmvang G, Kramer CM, Carbone I, Sechtem U, et al. Cardiovascular magnetic resonance in nonischemic myocardial inflammation: expert recommendations. J Am Coll Cardiol. 2018;72:3158–76.
Lippi G, Mattiuzzi C, Henry BM. Updated picture of SARS-CoV-2 variants and mutations. Diagnosis (Berl). 2021;9:11.
Acknowledgements
This study used the database of the Korea Disease Control and Prevention Agency and the National Health Insurance Service for policy and academic research (KDCA-NHIS-2022-1-437).
Funding
This research was supported by the Chung-Ang University Research Grants in 2022 and the National Research Foundation of Korea grant funded by the Korea government (Ministry of Science, ICT & Future Planning) (2022R1F1A1067609). The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
WYK and SYJ participated in the conception and design of study. SYJ and MTL participated in the data acquisition and data analysis. WYK, SYJ, MSB, and TWK participated in the data interpretation. WYK and MTL participated in the draft of the manuscript. SYJ, MSB, and TWK helped to revise the manuscript for important intellectual content. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The requirement for ethical approval was waived by the Institutional Review Board of Chung-Ang University due to analysis of de-identified patient records (1041078–202203-HR-086).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Appendix 1. International Classification of Diseases, 10th Revision codes used for the identification of pneumonia due to pathogens other than the severe acute respiratory syndrome coronavirus 2. Appendix 2. Outcome definitions.
Additional file 2:
Table S1. Coding for cardiovascular diseases. Table S2. Comorbidities based on the Charlson Comorbidity Index. Table S3. Types and codes for cardiovascular drug therapies.Table S4. ICD-10-based classification of organ dysfunction. Table S5. Baseline characteristics of participants in the COVID-19 and non-COVID-19 pneumonia groups who died within the first 30 days following the index date. Table S6. Cardiovascular outcomes of participants in the COVID-19 and non-COVID-19 pneumonia groups who died within the first 30 days following the index date. Table S7. Comparison of the risk of cardiovascular outcomes in participants hospitalized for COVID-19 or non-COVID-19 pneumonia. Table S8. Subgroup analyses of the risk of cardiovascular outcomes in participants hospitalized for COVID-19 or non-COVID-19 pneumonia. Table S9. Baseline characteristics of participants in the COVID-19 and non-COVID-19 pneumonia groups, including patients with preexisting cardiovascular disease. Table S10. Comparison of the risk of cardiovascular outcomes in participants hospitalized for COVID-19 or non-COVID-19 pneumonia, in cohorts including patients with preexisting cardiovascular disease. Table S11. Subgroup analyses of the risk of cardiovascular outcomes in participants hospitalized for COVID-19 or non-COVID-19 pneumonia, in cohorts including patients with preexisting cardiovascular disease. Table S12. Baseline characteristics of participants in the COVID-19 and non-COVID-19 pneumonia groups, including only patients with body mass index and smoking status data. Table S13. Subgroup analyses of the risk of cardiovascular outcomes in participants hospitalized for COVID-19 or non-COVID-19 pneumonia, in cohorts that included only patients with body mass index and smoking status data. Table S14. Comparison of the risk of cerebrovascular outcomes, identified using only the International Classification of Diseases, 10th Revision codes, in participants hospitalized for COVID-19 or non-COVID-19 pneumonia.
Additional file 3:
Fig. S1. Risk of cardiovascular outcomes in participants hospitalized for COVID-19 or non-COVID-19 pneumonia, in cohorts that included patients with preexisting cardiovascular disease. Fig. S2. Subgroup analyses comparing the risk of cardiovascular outcomes in participants hospitalized for COVID-19 or non-COVID-19 pneumonia, in cohorts that included patients with preexisting cardiovascular disease. Fig. S3. Subgroup analyses comparing the risk of cardiovascular outcomes in participants hospitalized for COVID-19 or non-COVID-19 pneumonia, in cohorts that included only patients with body mass index and smoking status data. Fig. S4. Cumulative incidence of (A) MACE, (B) myocardial infarction, (C) stroke, and (D) all-cause mortality in the COVID-19 group stratified according to vaccination status.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Lee, MT., Baek, M.S., Kim, T.W. et al. Cardiovascular outcomes between COVID-19 and non-COVID-19 pneumonia: a nationwide cohort study. BMC Med 21, 394 (2023). https://doi.org/10.1186/s12916-023-03106-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12916-023-03106-z