Abstract
Background
There is evidence that social anxiety disorder (SAD) is a prevalent and disabling disorder. However, most of the available data on the epidemiology of this condition originate from high income countries in the West. The World Mental Health (WMH) Survey Initiative provides an opportunity to investigate the prevalence, course, impairment, socio-demographic correlates, comorbidity, and treatment of this condition across a range of high, middle, and low income countries in different geographic regions of the world, and to address the question of whether differences in SAD merely reflect differences in threshold for diagnosis.
Methods
Data from 28 community surveys in the WMH Survey Initiative, with 142,405 respondents, were analyzed. We assessed the 30-day, 12-month, and lifetime prevalence of SAD, age of onset, and severity of role impairment associated with SAD, across countries. In addition, we investigated socio-demographic correlates of SAD, comorbidity of SAD with other mental disorders, and treatment of SAD in the combined sample. Cross-tabulations were used to calculate prevalence, impairment, comorbidity, and treatment. Survival analysis was used to estimate age of onset, and logistic regression and survival analyses were used to examine socio-demographic correlates.
Results
SAD 30-day, 12-month, and lifetime prevalence estimates are 1.3, 2.4, and 4.0% across all countries. SAD prevalence rates are lowest in low/lower-middle income countries and in the African and Eastern Mediterranean regions, and highest in high income countries and in the Americas and the Western Pacific regions. Age of onset is early across the globe, and persistence is highest in upper-middle income countries, Africa, and the Eastern Mediterranean. There are some differences in domains of severe role impairment by country income level and geographic region, but there are no significant differences across different income level and geographic region in the proportion of respondents with any severe role impairment. Also, across countries SAD is associated with specific socio-demographic features (younger age, female gender, unmarried status, lower education, and lower income) and with similar patterns of comorbidity. Treatment rates for those with any impairment are lowest in low/lower-middle income countries and highest in high income countries.
Conclusions
While differences in SAD prevalence across countries are apparent, we found a number of consistent patterns across the globe, including early age of onset, persistence, impairment in multiple domains, as well as characteristic socio-demographic correlates and associated psychiatric comorbidities. In addition, while there are some differences in the patterns of impairment associated with SAD across the globe, key similarities suggest that the threshold for diagnosis is similar regardless of country income levels or geographic location. Taken together, these cross-national data emphasize the international clinical and public health significance of SAD.
Similar content being viewed by others
Background
There is evidence from both community and clinical studies that social anxiety disorder (SAD), previously termed social phobia, is a prevalent and disabling disorder. In the National Comorbidity Survey (NCS) and National Comorbidity Survey Replication (NCS-R), SAD was one of the most common of all mental disorders (with lifetime prevalence estimates of 16% and 12.1% respectively) [1, 2]. In each of these surveys, SAD age of onset was early, comorbidity with other mental disorders was high, and subsequent impairment was notable [3, 4]. Research in clinical settings has also indicated that SAD is a prevalent and disabling condition in this context [5, 6]. Such data have been key in suggesting the clinical and public health relevance of SAD.
Nevertheless, most of the available data on the epidemiology of SAD originate from high income countries in the West. European epidemiological data have largely been consistent with US data, emphasizing the high prevalence, comorbidity, and morbidity of SAD [7]. A study using the Diagnostic Interview Schedule in four countries (USA, Canada, Korea, and Puerto Rico) found some consistent patterns, including higher rates in females and considerable comorbidity [8]. Still, many questions about the cross-national epidemiology of SAD remain unanswered. It has been suggested, for example, that anxiety disorders such as SAD are a peculiarly Western construct (in the East, for example, there may be more concern with offending others than with embarrassing oneself) [9]; from this perspective it might be hypothesized that SAD is less prevalent elsewhere, or that thresholds for SAD diagnosis differ across the globe.
Few data have systematically addressed the 30-day prevalence of SAD (which is important in establishing the prevalence at a particular point in time), whether age of onset and persistence vary across a range of different countries, whether impairment associated with SAD differs from place to place, and whether SAD treatment differs across the globe. Data on socio-demographic correlates of SAD and on comorbidity with other mental disorders have again mainly been reported in high income Western contexts. The WHO World Mental Health (WMH) Survey Initiative provides an important opportunity to investigate the epidemiology of SAD across a range of countries. In the current study, we assessed 30-day, 12-month, and lifetime SAD prevalence; age of onset; persistence; severity of role impairment associated with SAD; and treatment of SAD, across countries. In addition we investigated socio-demographic correlates of SAD, and comorbidity of SAD with other mental disorders, in the combined sample.
Methods
Samples
Interviews were administered in 13 regions classified by the World Bank [10] as high income (Australia, Belgium, France, Germany, Italy, Japan, New Zealand, Northern Ireland, Poland, Portugal, Spain, The Netherlands, USA), seven as upper-middle income (Brazil, Bulgaria, Colombia-Medellin, Lebanon, Mexico, Romania, South Africa), and six as low/lower-middle income (Colombia, Iraq, Nigeria, Peru, People’s Republic of China [PRC], Ukraine). Classified by region, surveys are from Africa (Nigeria, South Africa), the Americas (Brazil, Colombia, Mexico, Peru, USA), Eastern Europe (Bulgaria, Poland, Romania, Ukraine), Western Europe (Belgium, France, Germany, Italy, Northern Ireland, Portugal, Spain, The Netherlands), Western Pacific (Australia, Japan, New Zealand, PRC), and Eastern Mediterranean (Iraq, Lebanon).
All but ten surveys were based on area probability household samples representative of the entire nation (see Table 1 for survey details). The exceptions were surveys of all urbanized areas in three countries (Colombia, Mexico, Peru), of a specific region in two countries (Colombia-Medellin, Spain-Murcia), of specific metropolitan areas in three countries (São Paulo in Brazil; a series of cities in Japan; Beijing, Shanghai and Shen Zhen in PRC) and of selected states in one country (Nigeria). Respondents had to be at least 18 years of age in most countries (20 in Japan). Five surveys (Colombia, Colombia-Medellin, Mexico, Peru, Poland) had an upper age limit (64 or 65), and one (Australia) had an upper age limit of 85.
Interviews were conducted face to face in respondent homes after obtaining informed consent. Human Subjects Committees monitored the surveys and approved recruitment and consent procedures in each country. Other than in Australia, Iraq, Romania, and South Africa, where all respondents were administered the full interview, internal subsampling was used to reduce respondent burden by dividing the interview into two parts. Part 1 assessed core disorders, including SAD, and was administered to all respondents. Part 2 included additional disorders and correlates and was administered to all Part 1 respondents who met criteria for any lifetime Part 1 disorder plus a probability subsample of other respondents. Part 1 data were weighted to adjust for differential probabilities of selection and to match population distributions on census socio-demographic and geographic distributions. Part 2 data were additionally weighted for the under-sampling of Part 1 respondents without core disorders. Response rates range from a low of 45.9% (France) to 97.2% (Colombia-Medellin) (69.4% weighted average) (Table 1). Technical details about WMH sample design are presented elsewhere [11].
Measures
The WMH interviews assess prevalence and a wide range of predictors and consequences of numerous anxiety, mood, impulse control, and substance use disorders [12]. The full text of the interview schedule is available at www.hcp.med.harvard.edu/wmh. The WMH interview schedule was developed in English and translated into other languages using a standardized WHO translation, back-translation, and harmonization protocol described elsewhere [13]. Consistent interviewer training and quality control monitoring procedures were used in all surveys to facilitate cross-national comparison [14]. The following sections emphasize the measures considered in the current report.
Mental disorders
SAD and other Diagnostic and Statistical Manual of Mental Disorders (DSM)-IV anxiety (i.e., panic disorder with or without agoraphobia, agoraphobia without panic disorder, generalized anxiety disorder, specific phobia, post traumatic stress disorder, and separation anxiety disorder), mood (i.e., major depressive episode, bipolar disorder), impulse control (i.e., intermittent explosive disorder, bulimia nervosa, binge eating disorder, oppositional defiant disorder, conduct disorder, attention deficit disorder), and substance use disorders (i.e., alcohol abuse and drug abuse with or without dependence) were assessed using Version 3.0 of the WHO Composite International Diagnostic Interview (CIDI 3.0) [15], a fully structured lay-administered interview. Respondents were administered the full SAD section if they endorsed a diagnostic stem question for one or more performance or interactional fears described as excessive and causing substantial distress or avoidance. The SAD section screened for lifetime experiences of shyness, fear, and discomfort associated with each of 14 social situations. Respondents endorsing one or more such questions were asked about all DSM-IV criteria. Age of onset (AOO) of each disorder was assessed using special probing techniques shown experimentally to improve recall accuracy [16]. CIDI diagnoses were compared to blinded clinical diagnoses using the Structured Clinical Interview for DSM-IV (SCID) [17] in probability subsamples of WMH respondents from France, Italy, Spain, and the USA. As detailed elsewhere, good CIDI-SCID diagnostic concordance was found for SAD — area under the curve (AUC) = 0.67 — and most other DSM-IV/CIDI disorders [18].
Impairment
The Sheehan Disability Scale (SDS) [19] was used to assess recent impairment in role functioning in each of four domains (home, work, relationship, and social) in respondents with a 12-month SAD diagnosis. The response scale is from 0 to 10, with severe impairment in a specific role domain defined as a score ≥7. In addition, respondents were asked how many days in the past year they were unable to work or carry out their normal activities due to their disorder (days out of role).
Treatment
The 12-month treatment was assessed by asking respondents if they had seen any of a list of professionals for problems with emotions, nerves, mental health, or alcohol or drug use, including both inpatient and outpatient care. Sectors included were as follows: specialty mental health (e.g., psychiatrist and non-psychiatrist mental health specialist), general medical (e.g., general practitioner), human services sector (e.g., religious advisor), and complementary and alternative medicine (e.g., herbalist or homeopath).
Demographic factors
We examined age (18–29, 30–44, 45–59, 60+), time since onset, gender, employment status (student, homemaker, retired, other, employed), marital status (never married, divorced/separated/widowed, currently married), education level (no education, some primary, finished primary, some secondary, finished secondary, some college, finished college), and household income (low, low average, high average, and high, which were based on country-specific quartiles of gross household earnings in the past 12 months) [20].
Statistical analysis
Cross-tabulations were used to calculate prevalence, impairment, comorbidity, and treatment. Significance was calculated using Wald and McNemar’s chi-square tests. Survival analysis was used to estimate AOO and projected lifetime risk, as the young age of many respondents biases the AOO distribution downwards. The actuarial method implemented in SAS 9.4 (PROC LIFETEST) was used to generate the AOO curves. Logistic regression and survival analyses were used to examine socio-demographic correlates. Because the data were weighted and clustered, the Taylor series linearization method [21] implemented in the SUDAAN software package 11.0 [22] was used to estimate design-based standard errors. Statistical significance was consistently evaluated using two-sided tests, with P < 0.05 considered significant.
Results
Prevalence
On average, the estimated lifetime, 12-month, and 30-day prevalence is highest in high income countries (5.5%, 3.1%, 1.7%), intermediate in upper-middle income countries (2.9%, 2.1%, 1.3%), and lowest in low/lower-middle income countries (1.6%, 1.0%, 0.5%) (Table 2). Prevalence rates are highest in the Americas and the Western Pacific region, and lowest in Africa and the Eastern Mediterranean. Across all countries, SAD is a prevalent disorder (4.0%, 2.4%, 1.3%). Comparison of lifetime, 12-month, and 30-day prevalence across all countries, across different income groups, and across different regional groups all reached significance (P < 0.001) (Table 2).
The ratio of the 12-month prevalence to lifetime prevalence is an indirect indicator of disorder persistence. This ratio is lowest in high income countries (57.3%) and the Western Pacific (54.5%), and highest in upper-middle income countries (72.4%), Africa (71.1%), and the Eastern Mediterranean (74.2%). Across all countries, SAD is a persistent disorder (60.2%). The ratio of the 30-day prevalence to 12-month prevalence is an indirect indicator of episode persistence among those with recent disorder. This ratio is again lowest in the Western Pacific (49.4%), and highest in upper-middle income countries (61.4%), Africa (66.7%), and the Eastern Mediterranean (66.0%). Comparison of disorder and episode persistence across all countries, across different income groups, and across different regional groups all reached significance (P < 0.001) (Table 2).
Age of onset
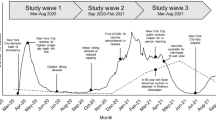
Table 3 and Fig. 1 indicate that the median estimated AOO is similar for high income, upper-middle income, and low/lower-middle income countries. Across all countries, the risk period for onset of SAD ranges from the mid-late adolescence to the early 40s. In high income countries, the earliest median AOO estimates occurr in Poland (50% by age 11), whereas the latest are in The Netherlands (50% by age 17). In upper-middle countries, the earliest median AOO estimates are in Colombia (50% by age 13), and the latest in South Africa (50% by age 26). In low/lower-middle income countries, the earliest median AOO estimates are in Nigeria (50% by age 11), and the latest in Peru (50% by age 16). Projected lifetime risk for SAD across the globe is 4.4%.
Impairment
SAD is associated with substantial impairment in multiple domains of role functioning in the WMH data (Table 4) and with a mean number of days out of work of 24.7 (1.8) in the past year (Appendix 1: Table 8). However, in most countries, the proportion of respondents with 12-month SAD and severe role impairment (SDS score of 7–10) is higher in the domains of relationships and social situations than in the domains of home and work. Furthermore, in most countries, between one-third and one-half of respondents with 12-month SAD have severe role impairment in at least one domain. Notably, there are no significant differences between low, middle, and high income groups, or between different WHO regions, in the proportion of respondents with severe role impairment in at least one domain.
However, there are significant differences across countries in proportion of 12-month SAD respondents with severe role impairment in any of the domains (ranging from 9.4% in PRC Shen Zhen to 71.6% in Spain-Murcia) (Table 4), and there are also some differences in specific domains across country, income region, and WHO region. The proportion of respondents with severe home impairment varies significantly by country and by WHO region; it is lowest in PRC Shen Zhen (2.1%) and the Western Pacific (8.1%), and highest in The Netherlands (41.9%) and the Eastern Mediterranean (15.8%). The proportion of respondents with severe work impairment varies significantly by country and by WHO region; it is lowest in the PRC Shen Zhen (1.4%) and the Eastern Mediterranean (8.4%), and highest in the Netherlands (56.8%) and Western Europe (20.2%). The proportion of respondents with severe relationship impairment varies significantly by country and by income region (lowest in low/lower-middle income countries, i.e., 18%, and highest in upper-middle income countries, i.e., 28.5%). The proportion of respondents with severe social impairment varies by country, by WHO region (lowest in Eastern Europe, i.e., 17.6%, highest in Western Europe, i.e., 31.4%), and by income region (lowest in low/lower-middle income, i.e., 21.2%, highest in high income, i.e., 29.8%).
Socio-demographic correlates
Table 5 shows the bivariate associations of the socio-demographic characteristics with SAD in the combined sample. Both 30-day and lifetime risk of SAD are associated with younger AOO, female gender, not being employed, being unmarried (never married or divorced/widowed/separated), lower educational status, and low household income. SAD recurrence (as indicated by 12-month SAD in lifetime cases) is associated with female gender, earlier AOO, and being unmarried — while persistence (as indicated by 30-day SAD in 12-month cases) is associated with female gender but not with earlier AOO or marital status. SAD recurrence is particularly highly associated with lower education (with no education having an odds ratio [OR] of 5.6, confidence interval [CI] 2.2–14.4), SAD persistence is particularly associated with being a student (OR of 2.1, CI 1.4–3.0), and both recurrence and persistence are associated with being a homemaker. Socio-demographic correlates are similar across countries for the most part, but also demonstrate some differences (Appendix 2: Table 9, Appendix 3: Table 10, and Appendix 4: Table 11).
Comorbidity
Table 6 shows that respondents with either lifetime or 12-month SAD are most likely to meet lifetime criteria for other anxiety disorders (59.8% and 64.9%), less likely to meet lifetime criteria for mood and substance use disorders, and least likely to meet lifetime criteria for impulse control disorders (19.3% and 21.9%); in both cases around 80% of such respondents meet lifetime criteria for any other mental disorder. Similarly, respondents with 12-month SAD are most likely to meet 12-month criteria for other anxiety disorders (52.7%), less likely to meet 12-month criteria for mood and impulse control disorders, and least likely to meet 12-month criteria for substance use disorders (10.2%); with 66.9% of such respondents meeting 12-month criteria for any other disorder. For both lifetime and 12-month SAD, SAD begins earlier in only 31.4–35.4% of cases of anxiety disorder, but SAD begins earlier in 48.8–80.9% of cases of mood disorder, substance use disorder, or impulse control disorder.
Treatment
Among those with 12-month SAD, the percentage reporting treatment of any kind (i.e., specialty mental health, general medical care, health care, human services, complementary and alternative medicine, non-health care) in the past 12 months differs significantly by impairment, with 38% receiving any treatment (Table 7). Across all countries, any treatment is lowest in those with moderate impairment (27.4%), and highest in those with severe impairment (46.9%). This pattern holds true for specialty mental health, general medical care, and health care, but human services, complementary and alternative medicine, and non-health care are most commonly used by those with mild impairment. Treatment rates for those with any impairment are lowest in low/lower-income countries (18.0%), and highest in high income countries (44.2%). This pattern holds true for cases with any impairment across all treatment sectors, and for almost all treatment sectors across different levels of impairment.
Discussion
A number of limitations of the current study deserve mention. A first important issue is that of sampling. Response rates differ widely across the WMH surveys [12]; while response rates do not appear to be related to SAD prevalence, it is possible that in some settings, particularly those where treatment is less available, those with the most severe SAD were unable to participate in surveys. Surveys also differed in their focus; some included only metropolitan areas, while others employed nationally representative samples; such differences may also have affected prevalence estimates. The surveys also excluded a range of respondents, including institutionalized patients, and people who were too intoxicated to be interviewed. Finally, samples in the WMH surveys also reflected survivor bias; given the 10- to 15-year gap in life expectancy between those in lower and higher income countries, this may also affect prevalence estimates [23]. Taken together, the prevalence rates provided here are therefore conservative. It is also relevant to note that only two African countries were studied, limiting conclusions about distinctions across geographic regions.
Second, the measure of SAD used in the WMH surveys has important limitations. The CIDI relies on a screening section that employs relatively few stem questions, and this may lead to under-estimation of SAD in some settings (as noted, there is no stem question that addresses the symptom of offending others, which is thought to characterize social anxiety in some cultures, and which is now captured in the DSM-5 diagnostic criteria for SAD) [24,25,26,27]. Furthermore, no attempt was made to develop distinct cut-off points for SAD in different countries or to go beyond the DSM-IV criteria to develop distinct criteria for different countries that might have increased detection of SAD. It is relevant to emphasize that in countries where blinded clinical reappraisal interviews were undertaken, there was no evidence for systematic bias in the diagnostic threshold for SAD [18]. However, clinical reappraisal interviews were carried out in only a subset of WMH countries, and it is possible that such studies would have found systematic differences in CIDI sensitivity and specificity across contexts.
Bearing in mind these limitations, the WMH surveys provide unique cross-national data on SAD, and are able to address a number of questions about this disorder. Some cross-national differences in SAD epidemiology are apparent: SAD 30-day, 12-month, and lifetime prevalence are lowest in low/lower-middle income countries and in the African and Eastern Mediterranean regions, highest in upper-middle income countries and the Americas and the Western Pacific regions, and there are some differences in domains of role impairment and in treatment rates across country, income region, and WHO region. Crucially, however, there are a number of consistent patterns across the globe: SAD has an early age of onset, is a persistent disorder, and is associated with specific socio-demographic features (younger age, female sex, unmarried status, lower education, and lower income) and with similar patterns of comorbidity and health care utilization.
A previous cross-national study indicated that SAD prevalence differs across different countries, with lifetime prevalence estimates ranging from 0.5 in Korea to 2.6 in the USA [8]. However, that survey was done in only four countries, and assessed only three social fears as part of the simple phobia section of the Diagnostic Interview Schedule. The current data extend such work with surveys across a broad range of countries, and with a comprehensive assessment of SAD. Differences in prevalence across countries continue to be observed, as is the case for other common mental disorders in the WMH surveys. Such differences may reflect artifactual variation across surveys (for example, mental disorder stigma may be higher in lower income settings, resulting in decreased willingness to self-disclose, and an under-estimation of prevalence) or cross-national differences in underlying mechanisms relevant to pathogenesis (for example, greater access to greater social capital and more community engagement in lower income countries).
However, the finding here of similar proportions of SAD respondents with any severe role impairment across country income and geographic groupings suggests that differences in prevalence are not simply due to regional differences in diagnostic thresholding. In higher income countries and in particular regions of the globe such as the Americas, Western Pacific, and Western Europe, there is a higher prevalence of SAD, and SAD is associated with more impairment in the social domain than in other domains, suggesting high demands for social performance in such contexts. The persistence of SAD as well as proportion with any role impairment are highest in upper-middle income countries, Africa, and the Eastern Mediterranean, perhaps pointing to growing performance demands in these regions, but with fewer treatment resources than in higher income countries. The disjunction between lower prevalence but higher persistence of SAD in particular regions may be valuable in suggesting hypotheses, such as this one, about relevant causal mechanisms in SAD.
Our findings that SAD epidemiology demonstrates similar patterns across the globe, being associated with early age of onset, impairment in multiple domains, characteristic socio-demographic correlates (younger age, female gender, unmarried status, lower education, lower household income), and particular patterns of mental disorder comorbidity, again confirms and extends previous work. Thus, for example, we were able to demonstrate that across the globe SAD disorder persistence is particularly highly associated with lower education, episode persistence is particularly associated with being a student, while both disorder and episode persistence are associated with being a homemaker. While it has previously been demonstrated that SAD more likely follows other anxiety disorders, and precedes depression [1], here we provide novel data on the comorbidity of SAD with impulse control disorders; this is valuable given that a link between social anxiety and aggression has been posited in the animal and clinical literature [28, 29]. It is notable that in both lifetime and 12-month SAD, SAD begins earlier in only 31.4–35.4% of cases of comorbid anxiety disorder, due to the common comorbidity with specific phobia which has the earliest onset of the anxiety disorders, but SAD begins earlier in 48.8–80.9% of cases of comorbid mood disorder, substance use disorder, or impulse control disorder. We also provide novel data on treatment rates; these are highest where impairment is most severe and in countries with higher income.
Conclusions
In conclusion, data from the WMH survey provide the most comprehensive picture of the global epidemiology of SAD to date and help address the key question of whether this condition is a peculiarly Western construct. There are apparent differences in SAD prevalence and domains of role impairment across the globe, with further work needed to delineate more rigorously the reasons for such differences and to investigate possible mechanisms relevant to understanding them. Nevertheless, the data indicate that across the world, SAD is a prevalent condition that is characterized by early age of onset, as well as disorder and episode persistence. Furthermore in low, middle, and high income countries, as well as in a range of geographic regions, SAD is associated with specific socio-demographic correlates (younger age, female gender, unmarried status, lower education, lower household income), particular comorbidity patterns (typically beginning later than specific phobia, but earlier than other anxiety disorders, mood, substance use, or impulse control disorders), and common patterns of health care utilization. Taken together, these cross-national data emphasize the international clinical and public health significance of SAD.
References
Magee WJ, Eaton WW, Wittchen HU, McGonagle KA, Kessler RC. Agoraphobia, simple phobia, and social phobia in the National Comorbidity Survey. Arch Gen Psychiatry. 1996;53:159–68.
Ruscio AM, Brown TA, Chiu WT, Sareen J, Stein MB, Kessler RC. Social fears and social phobia in the USA: results from the National Comorbidity Survey Replication. Psychol Med. 2008;38:15–28.
Kessler RC. The impairments caused by social phobia in the general population: implications for intervention. Acta Psychiatr Scand Suppl. 2003;108:19–27.
Kessler RC, Ruscio AM, Shear K, Wittchen HU. Epidemiology of anxiety disorders. Curr Top Behav Neurosci. 2010;2:21–35.
Dalrymple KL, Zimmerman M. Screening for social fears and social anxiety disorder in psychiatric outpatients. Compr Psychiatry. 2008;49:399–406.
Connor KM, Kobak KA, Churchill LE, Katzelnick D, Davidson JR. Mini-SPIN: a brief screening assessment for generalized social anxiety disorder. Depress Anxiety. 2001;14:137–40.
Fehm L, Pelissolo A, Furmark T, Wittchen HU. Size and burden of social phobia in Europe. Eur Neuropsychopharmacol. 2005;15:453–62.
Weissman MM, Bland RC, Canino GJ, Greenwald S, Lee CK, Newman SC, Rubio-Stipec M, Wickramaratne PJ. The cross-national epidemiology of social phobia: a preliminary report. Int Clin Psychopharmacol. 1996;11 Suppl 3:9–14.
Dowbiggin IR. High anxieties: the social construction of anxiety disorders. Can J Psychiatry. 2009;54:429–36.
Data: Countries and Economies. http://datahelpdesk.worldbank.org/knowledgebase/articles/906519%5D.
Heeringa S, Wells E, Hubbard F, Mneimneh Z, Chiu W, Sampson N, Berglund P. Sample designs and sampling procedures. In: Kessler R, Ustun T, editors. The WHO World Mental Health Surveys: global perspectives on the epidemiology of mental disorders. New York: Cambridge University Press; 2008. p. 14–32.
Kessler R, Ustun T. The WHO World Mental Health Surveys: global perspectives on the epidemiology of mental disorders. New York: Cambridge University Press; 2008.
Harkness J, Pennell B-E, Villar A, Gebler N, Aguilar-Gaxiola S, Bilgen I. Translation procedures and translation assessment in the World Mental Health Survey Initiative. In: Kessler R, Ustun T, editors. The WHO World Mental Health Surveys: global perspectives on the epidemiology of mental disorders. New York: Cambridge University Press; 2008. p. 91–113.
Pennell B-E, Mneimneh Z, Bowers A, Chardoul S, Welles J, Viana M, Dinkelmann K, Gebler N, Florescu S, He Y, Huang Y, Tomov T, Vilagut G. Implementation of the World Mental Health Surveys Initiative. In: Kessler R, Ustun T, editors. The WHO World Mental Health Surveys: global perspectives on the epidemiology of mental disorders. New York: Cambridge University Press; 2008. p. 33–57.
Kessler RC, Ustun TB. The World Mental Health (WMH) Survey Initiative Version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI). Int J Methods Psychiatr Res. 2004;13:93–121.
Knäuper B, Cannell C, Schwarz N, Bruce M, Kessler R. Improving accuracy of major depression age-of-onset reports in the US National Comorbidity Survey. Int J Methods Psychiatr Res. 1999;8:39–48.
First MB, Spitzer RL, Gibbon M, Williams BJ. Structured Clinical Interview for Axis I DSM-IV Disorders. New York: Biometrics Research, New York State Psychiatric Institute; 1994.
Haro JM, Arbabzadeh-Bouchez S, Brugha TS, de Girolamo G, Guyer ME, Jin R, Lepine JP, Mazzi F, Reneses B, Vilagut G, Sampson NA, Kessler RC. Concordance of the Composite International Diagnostic Interview Version 3.0 (CIDI 3.0) with standardized clinical assessments in the WHO World Mental Health surveys. Int J Methods Psychiatr Res. 2006;15:167–80.
Sheehan DV, Harnett-Sheehan K, Raj BA. The measurement of disability. Int Clin Psychopharmacol. 1996;11 Suppl 3:89–95.
Levinson D, Lakoma MD, Petukhova M, Schoenbaum M, Zaslavsky AM, Angermeyer M, Borges G, Bruffaerts R, de Girolamo G, de Graaf R, Gureje O, Haro JM, Hu C, Karam AN, Kawakami N, Lee S, Lepine JP, Browne MO, Okoliyski M, Posada-Villa J, Sagar R, Viana MC, Williams DR, Kessler RC. Associations of serious mental illness with earnings: results from the WHO World Mental Health surveys. Br J Psychiatry. 2010;197:114–21.
Wolter K. Introduction to variance estimation. New York: Springer-Verlag; 1985.
Institute RT. SUDAAN: Professional Software for Survey Data Analysis. Research Triangle Park: Research Triangle Institute; 2002.
Riley J. Estimates of regional and global life expectancy, 1800-2001. Popul Dev Rev. 2005;31:537–43.
Stein DJ. Social anxiety disorder in the West and in the East. Ann Clin Psychiatry. 2009;21:109–17.
Stein DJ, Matsunaga H. Cross-cultural aspects of social anxiety disorder. Psychiatr Clin North Am. 2001;24:773–82.
Lewis-Fernandez R, Hinton DE, Laria AJ, Patterson EH, Hofmann SG, Craske MG, Stein DJ, Asnaani A, Liao B. Culture and the anxiety disorders: recommendations for DSM-V. Depress Anxiety. 2010;27:212–29.
Hofmann SG, Anu Asnaani MA, Hinton DE. Cultural aspects in social anxiety and social anxiety disorder. Depress Anxiety. 2010;27:1117–27.
Dixon LJ, Tull MT, Lee AA, Kimbrel NA, Gratz KL. The role of emotion-driven impulse control difficulties in the relation between social anxiety and aggression. J Clin Psychol. 2017;73:722–32.
Neumann ID, Veenema AH, Beiderbeck DI. Aggression and anxiety: social context and neurobiological links. Front Behav Neurosci. 2010;4:12.
Acknowledgements
The WHO World Mental Health Survey Collaborators are Sergio Aguilar-Gaxiola, M.D., Ph.D., Ali Al-Hamzawi, M.D., Mohammed Salih Al-Kaisy, M.D., Jordi Alonso, M.D., Ph.D., Laura Helena Andrade, M.D., Ph.D., Corina Benjet, Ph.D., Guilherme Borges, Sc.D., Evelyn J. Bromet, Ph.D., Ronny Bruffaerts, Ph.D., Brendan Bunting, Ph.D., Jose Miguel Caldas de Almeida, M.D., Ph.D., Graca Cardoso, M.D., Ph.D., Alfredo H. Cia, M.D., Somnath Chatterji, M.D., Louisa Degenhardt, Ph.D., Giovanni de Girolamo, M.D., Peter de Jonge, Ph.D., Koen Demyttenaere, M.D., Ph.D., John Fayyad, M.D., Silvia Florescu, M.D., Ph.D., Oye Gureje, Ph.D., D.Sc., FRC.Psych., Josep Maria Haro, M.D., Ph.D., Yanling He, M.D., Hristo Hinkov, M.D., Chi-yi Hu, Ph.D., M.D., Yueqin Huang, M.D., M.PH., Ph.D., Aimee Nasser Karam, Ph.D., Elie G. Karam, M.D., Norito Kawakami, M.D., D.MSc, Ronald C. Kessler, Ph.D., Andrzej Kiejna, M.D., Ph.D., Viviane Kovess-Masfety, M.D., Ph.D., Sing Lee, M.B., B.S., Jean-Pierre Lepine, M.D., Daphna Levinson, Ph.D., John McGrath, Ph.D., Maria Elena Medina-Mora, Ph.D., Jacek Moskalewicz, Dr.PH., Fernando Navarro-Mateu, M.D., Ph.D., Beth-Ellen Pennell, M.A., Marina Piazza, M.PH., Sc.D., Jose Posada-Villa, M.D., Kate M. Scott, Ph.D., Tim Slade, Ph.D., Juan Carlos Stagnaro, M.D., Ph.D., Dan J. Stein, FRC.PC., Ph.D., Nezar Taib, M.S., Margreet ten Have, Ph.D., Yolanda Torres, M.PH., Maria Carmen Viana, M.D., Ph.D., Harvey Whiteford, Ph.D., David R. Williams, M.P.H., Ph.D., Bogdan Wojtyniak, Sc.D.
Funding
This work was carried out in conjunction with the World Health Organization World Mental Health (WMH) Survey Initiative which is supported by the National Institute of Mental Health (NIMH; R01 MH070884), the John D. and Catherine T. MacArthur Foundation, the Pfizer Foundation, the US Public Health Service (R13-MH066849, R01-MH069864, and R01 DA016558), the Fogarty International Center (FIRCA R03-TW006481), the Pan American Health Organization, Eli Lilly and Company, Ortho-McNeil Pharmaceutical, GlaxoSmithKline, and Bristol-Myers Squibb. We thank the staff of the WMH Data Collection and Data Analysis Coordination Centers for assistance with instrumentation, fieldwork, and consultation on data analysis. None of the funders had any role in the design, analysis, interpretation of results, or preparation of this paper. The views and opinions expressed in this report are those of the authors and should not be construed to represent the views or policies of the World Health Organization, or other sponsoring organizations, agencies, or governments. A complete list of all within-country and cross-national WMH publications can be found at http://www.hcp.med.harvard.edu/wmh/.
The 2007 Australian National Survey of Mental Health and Wellbeing is funded by the Australian Government Department of Health and Ageing. The São Paulo Megacity Mental Health Survey is supported by the State of São Paulo Research Foundation (FAPESP) Thematic Project Grant 03/00204-3. The Bulgarian Epidemiological Study of common mental disorders EPIBUL is supported by the Ministry of Health and the National Center for Public Health Protection. The Chinese World Mental Health Survey Initiative is supported by the Pfizer Foundation. The Shenzhen Mental Health Survey is supported by the Shenzhen Bureau of Health and the Shenzhen Bureau of Science, Technology, and Information. The Colombian National Study of Mental Health (NSMH) is supported by the Ministry of Social Protection. The Mental Health Study Medellin-Colombia was carried out and supported jointly by the Center for Excellence on Research in Mental Health (CES University) and the Secretary of Health of Medellin. The ESEMeD project is funded by the European Commission (Contracts QLG5-1999-01042; SANCO 2004123, and EAHC 20081308), (the Piedmont Region, Italy), Fondo de Investigación Sanitaria, Instituto de Salud Carlos III, Spain (FIS 00/0028), Ministerio de Ciencia y Tecnología, Spain (SAF 2000-158-CE), Departament de Salut, Generalitat de Catalunya, Spain, Instituto de Salud Carlos III (CIBER CB06/02/0046, RETICS RD06/0011 REM-TAP), and other local agencies and by an unrestricted educational grant from GlaxoSmithKline. Implementation of the Iraq Mental Health Survey (IMHS) and data entry were carried out by the staff of the Iraqi MOH and MOP with direct support from the Iraqi IMHS team with funding from both the Japanese and European Funds through the United Nations Development Group Iraq Trust Fund (UNDG ITF). The World Mental Health Japan (WMHJ) Survey is supported by the Grant for Research on Psychiatric and Neurological Diseases and Mental Health (H13-SHOGAI-023, H14-TOKUBETSU-026, H16-KOKORO-013) from the Japan Ministry of Health, Labour and Welfare. The Lebanese Evaluation of the Burden of Ailments and Needs Of the Nation (L.E.B.A.N.O.N.) is supported by the Lebanese Ministry of Public Health, the WHO (Lebanon), National Institute of Health/Fogarty International Center (R03 TW006481-01), anonymous private donations to IDRAAC, Lebanon, and unrestricted grants from Algorithm, AstraZeneca, Benta, Bella Pharma, Eli Lilly, GlaxoSmithKline, Lundbeck, Novartis, OmniPharma, Pfizer, Phenicia, Servier, and UPO. The Mexican National Comorbidity Survey (MNCS) is supported by The National Institute of Psychiatry Ramon de la Fuente (INPRFMDIES 4280) and by the National Council on Science and Technology (CONACyT-G30544- H), with supplemental support from the Pan American Health Organization (PAHO). Corina Benjet has received funding from the (Mexican) National Council of Science and Technology (grant CB-2010-01-155221). Te Rau Hinengaro: The New Zealand Mental Health Survey (NZMHS) is supported by the New Zealand Ministry of Health, Alcohol Advisory Council, and the Health Research Council. The Nigerian Survey of Mental Health and Wellbeing (NSMHW) is supported by the WHO (Geneva), the WHO (Nigeria), and the Federal Ministry of Health, Abuja, Nigeria. The Northern Ireland Study of Mental Health was funded by the Health & Social Care Research & Development Division of the Public Health Agency. The Peruvian World Mental Health Study was funded by the National Institute of Health of the Ministry of Health of Peru. The Polish project Epidemiology of Mental Health and Access to Care - EZOP Project (PL 0256) was supported by Iceland, Liechtenstein, and Norway through funding from the EEA Financial Mechanism and the Norwegian Financial Mechanism. The EZOP project was co-financed by the Polish Ministry of Health. The Portuguese Mental Health Study was carried out by the Department of Mental Health, Faculty of Medical Sciences, NOVA University of Lisbon, with collaboration of the Portuguese Catholic University, and was funded by the Champalimaud Foundation, the Gulbenkian Foundation, the Foundation for Science and Technology (FCT), and the Ministry of Health. The Romania WMH study projects “Policies in Mental Health Area” and “National Study regarding Mental Health and Services Use” were carried out by National School of Public Health & Health Services Management (former National Institute for Research & Development in Health), with technical support of Metro Media Transilvania, the National Institute of Statistics-National Centre for Training in Statistics, SC. Cheyenne Services SRL, Statistics Netherlands and were funded by the Ministry of Public Health (former Ministry of Health) with supplemental support from Eli Lilly Romania SRL. The South Africa Stress and Health Study (SASH) is supported by the US National Institute of Mental Health (R01-MH059575) and the National Institute of Drug Abuse with supplemental funding from the South African Department of Health and the University of Michigan. DJS is supported by the South African Medical Research Council (MRC). The Psychiatric Enquiry to General Population in Southeast Spain - Murcia (PEGASUS-Murcia) Project has been financed by the Regional Health Authorities of Murcia (Servicio Murciano de Salud and Consejería de Sanidad y Política Social) and Fundación para la Formación e Investigación Sanitarias (FFIS) of Murcia. The Ukraine Comorbid Mental Disorders during Periods of Social Disruption (CMDPSD) study is funded by the US National Institute of Mental Health (RO1-MH61905). The US National Comorbidity Survey Replication (NCS-R) is supported by the National Institute of Mental Health (NIMH; U01-MH60220) with supplemental support from the National Institute of Drug Abuse (NIDA), the Substance Abuse and Mental Health Services Administration (SAMHSA), the Robert Wood Johnson Foundation (RWJF; Grant 044708), and the John W. Alden Trust.
Availability of data and materials
Only data from those surveys which are publically available (e.g., National Comorbidity Survey Replication) can be accessed by readers.
Authors’ contributions
RCK, KMS, and DJS conceived the study. KMS and RCK directed the statistical analysis. CCWL carried out the statistical analysis. DJS wrote the first draft of the manuscript. The other co-authors participated in literature searches and early discussions of the data and gave input into the manuscript from the perspective of the participating surveys. All authors read and approved the final version of the manuscript.
Competing interests
In the past 3 years, Dr. Stein has received research grants and/or consultancy honoraria from Biocodex, Lundbeck, Servier, and Sun. In the past 3 years, Dr. Kessler received support for his epidemiological studies from Sanofi Aventis; was a consultant for Johnson & Johnson Wellness and Prevention, Shire, Takeda; and served on an advisory board for the Johnson & Johnson Services Inc. Lake Nona Life Project. Dr. Kessler is a co-owner of DataStat, Inc., a market research firm that carries out health care research. The remaining authors declare that they have no competing interests.
Ethics approval and consent to participate
Local Institutional Review Boards approved each survey, and all respondents gave informed consent.
Study approval statement
Not applicable.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Consortia
Corresponding author
Appendices
Appendix 1
Appendix 2
Appendix 3
Appendix 4
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Stein, D.J., Lim, C.C.W., Roest, A.M. et al. The cross-national epidemiology of social anxiety disorder: Data from the World Mental Health Survey Initiative. BMC Med 15, 143 (2017). https://doi.org/10.1186/s12916-017-0889-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12916-017-0889-2