Abstract
Over 90% of the world’s severe and fatal Plasmodium falciparum malaria is estimated to affect young children in sub-Sahara Africa, where it remains a common cause of hospital admission and inpatient mortality. Few children will ever be managed on high dependency or intensive care units and, therefore, rely on simple supportive treatments and parenteral anti-malarials. There has been some progress on defining best practice for antimalarial treatment with the publication of the AQUAMAT trial in 2010, involving 5,425 children at 11 centres across 9 African countries, showing that in artesunate-treated children, the relative risk of death was 22.5% (95% confidence interval (CI) 8.1 to 36.9) lower than in those receiving quinine. Human trials of supportive therapies carried out on the basis of pathophysiology studies, have so far made little progress on reducing mortality; despite appearing to reduce morbidity endpoints, more often than not they have led to an excess of adverse outcomes. This review highlights the spectrum of complications in African children with severe malaria, the therapeutic challenges of managing these in resource-poor settings and examines in-depth the results from clinical trials with a view to identifying the treatment priorities and a future research agenda.
Similar content being viewed by others
Background
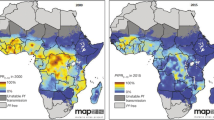
In many parts of the world malaria incidence has declined, in part due to substantial donor investment targeting the scaling up of insecticide-treated nets (ITN) and other vector control measures. Nevertheless, in 2010 it was estimated that there were 500 million episodes of Plasmodium falciparum malaria each year [1,2]. In the same year, the World Health Organization (WHO) estimated that there were approximately 650,000 deaths directly attributed to malaria worldwide [3]. The heaviest burden of P. falciparum malaria falls on sub-Saharan Africa (sSA), where children under five years old are disproportionately affected by this parasite (Figure 1). Today, 57% of Africa’s populations still live in areas with moderate to high malaria transmission. Ten countries account for 87% of people exposed to the highest malaria endemicities globally, where the P. falciparum rates in children two- to ten-years old exceed 50%. Malaria, therefore, remains a very common cause of hospital admission in sSA, and where severe malaria is mainly a disease of children under five years of age. It has been estimated that approximately 90% of the world’s severe and fatal malaria affects young children in sSA [4,5].
Severe malaria is a complex multisystem disorder with a clinical presentation that has many similarities to severe bacterial sepsis, despite distinctive differences in pathogenesis. Children typically present when they are critically ill with life-threatening complications yet, in most African hospitals, few will ever be managed on an intensive care unit or in a high dependency facility. The high, and frequently seasonal, burden of cases of severe malaria presents a unique challenge to health services and clinicians working in resource-limited hospitals. This review intends to provide an overview of the spectrum and complications of severe malaria, highlighting treatment priorities for children managed within low-resource settings in Africa and re-examining what has been learnt from clinical trials to outline a future research agenda. In order to contextualise the current and future relevance of this review and the continued necessity to prioritise research funding for this condition, I will briefly summarise the current status of malaria eradication efforts, aimed at reducing the disease burden and mortality, and accordingly, if successful and sustained, negating the necessity for future investment in this clinical disease.
Malaria control: are we nearly there yet?
The global strategy towards gradual malaria eradication which has been developed and ratified into policy was reviewed in 2010 in a four-part Lancet series [6-9]. It focuses on aggressive control of transmission and investment in vaccine development, insecticides, new treatments and diagnostics. Hospital admissions and deaths due to malaria are, therefore, important barometers for the effectiveness of these measures to control and eliminate malaria. Substantial reductions have been witnessed in several African countries, in some cases directly or plausibly linked to the scaling up of control efforts [10-14]. However, many of the encouraging reports have tended to be from areas with relatively low baseline malaria transmission intensities. In some cases, the greatest decline in malaria hospitalisation preceded the scale-up of ITN use or the introduction of artemisinin combination therapies [13], suggesting that more complex mechanisms are involved. Other sSA countries have documented either no decline in severe or fatal malaria [4], an increase in hospitalisations during the same period [15,16] or a resurgence following sustained control [17]. The downstream effects on the spectrum of severe malaria are uncertain, although there are reports that cerebral malaria is now being witnessed in children over five years old, in areas where it was previously rare (KM verbal communication).
With regard to vaccine development, immunological and clinical data from large Phase III multicentre vaccination trials of the most promising candidate on the market to date (RTS,S), a vaccine which is directed against the pre-erythrocytic stage of P. falciparum malaria, were encouraging. However, longer term follow-up indicated these responses were imperfect and short-lived. In the 18 months following vaccination with RTS,S, vaccine efficacy (VE) against clinical malaria in children was 46% (95% confidence interval (CI) 42% to 50%) but only 27% (95% CI 20% to 32%) in infants vaccinated between 6- and 12-weeks old [18,19]. VE waned with time in both groups and VE was more notable at sites with a lower baseline incidence of malaria [20]. Although further results of the long term follow up are expected, in essence, this is the status of malaria vaccine research and the culmination of over 20 years of development and clinical trials.
Severe malaria
Formerly, severe malaria in African children was considered to comprise two distinct clinical syndromes: cerebral malaria and severe malarial anaemia. This paradigm was supported by clinical, molecular, immunological and genetic studies and, indeed, substantially influenced their experimental design. As a consequence, it was held that most malaria deaths were attributable to cerebral malaria and, thus, were primarily neurological in origin, with a smaller number resulting from severe malarial anaemia, which could be mitigated by an immediate blood transfusion. Over the last three decades substantial research funding has enabled much clearer and detailed clinical phenotyping of severe malaria in African children, its pathophysiology and complications. What has been determined is that severe malaria encompasses a complex syndrome affecting many organs resulting in biochemical and haematological derangements which have many features in common with the pathophysiological derangements complicating children with severe sepsis. Moreover, in-hospital deaths, most occurring within 24 hours of admission, appear to be a consequence of a wide spectrum of pathophysiological determinants. At the clinical level, a key challenge for health services in Africa, owing to the large burden of paediatric admissions with P. falciparum malaria infection, is distinguishing those who are at greatest risk of poor outcome, using largely clinical criteria, in order to target parenteral antimalarials and supportive therapies [21]. This is reviewed in the next section.
Case definitions and defining those at greatest risk
Differentiating ‘true cases’ of severe malaria from other acute infections remains both a clinical and epidemiological challenge, as most symptoms of malaria are indistinguishable from other major causes of morbidity, in malaria-endemic sSA where parasite carriage is the norm rather than the exception. For example, a child with severe respiratory distress and P. falciparum malaria could either have severe malaria or very severe pneumonia, an issue that has been covered in a number of publications [22-26]. Determining the cases at greatest risk of poor outcome has been helped by a number of seminal papers. A prospective study of 1,844 paediatric hospital admissions with P. falciparum malaria in Kenya established that two clinical features, impaired consciousness (defined as coma or prostration) and respiratory distress (a clinical sign of metabolic acidosis), identified 84% of fatal cases. Prostration (the inability to sit upright in children over eight months or breast feed), any respiratory distress, hypoglycemia, jaundice, or any combination of these, predicted 92% of fatal cases. Relevant to the traditional severe malaria paradigm was that severe malarial anaemia (defined as a haemoglobin (Hb) <5 g/dl) in the absence of these two clinical signs had a very low mortality (1.3%) [27]. Similar findings were reported in Gambian children with severe malaria where neurological status (coma with or without extensor posturing), tachycardia, tachypnoea, hypoglycemia and hyperlactatemia (plasma lactate level, >5 mmol/L) were found as independent indicators of a fatal outcome [28]. Using data from six research units in Africa (SMAC network) the Lambaréné Organ Dysfunction Score was developed, which combines three variables: coma, prostration and deep breathing. The scores ranged from 0 to 3. Sixty-one percent of the children had none of the three signs, 26% had one, 10% had two and 3% had all three signs (case fatality rate 36%). However, it was unclear how the score was constructed since, at an individual level, prostration and coma are mutually exclusive, thus impossible to score 3 [29]. Probably one of the most comprehensive descriptions of the clinical and laboratory complications of severe malaria (and a subsequent evaluation of prognostic markers) comes from the large Phase III randomised clinical trial comparing artesunate and quinine (African Quinine Artesunate Malaria Trial: AQUAMAT) [30]. AQUAMAT included 5,425 participants and was conducted in 11 centres across nine countries, spanning East, West and Central sSA, thus covering a range of malaria transmission intensities. Baseline characteristics included severe acidosis (base excess < −−‐8; 43%), coma (37%), convulsions (32%), severe anaemia (Hb <5 g/dl; 30%), hypoglycaemia (blood sugar level <3 mmol/L; 10%) and compensated shock (9%). In a subsequent sub-analysis of the AQUAMAT data which investigated predictors of poor outcome, four parameters (out of 20 indicators of severity) were identified that were independently associated with fatality in a multivariate analysis [31]. These were base deficit (>8 mmol/L), coma, elevated blood urea nitrogen (BUN, >20 mg/dL) and underlying chronic illness. In those with coma and acidosis, case fatality was 23%, in children with a combination of coma, acidosis and raised BUN, mortality was 43% (Figure 2). Finally, since asymptomatic carriage of parasites is common in endemic areas, a further refinement aimed at improving the specificity of the case definition for either epidemiological or research purposes proposed the addition of a parasitaemia threshold [32]. The malarial-attributable case fraction (MAF) for children with clinical evidence of severe disease increased from 85% to 95% with the inclusion of a parasitaemia threshold of over 2,500c parasites/ml and with the exclusion of those presenting with malaria parasites but had a primary diagnosis of gastroenteritis with severe dehydration, pneumonia, culture-proven bacteraemia, or meningitis.
Combinations of presentations and the associated mortality in children in the AQUAMAT trial. Venn diagram illustrating the combinations of presentations and associated mortality from von Seidlein et al. 2012 [31].
The latest WHO guidelines [21], informed by systematic reviews by the expert advisory group, have drawn on these resources to inform clinical and therapeutic management recommendations and provided a comparison of the clinical spectrum of malaria in adults and children largely using the AQUAMAT data set [30] and adult data from the corresponding artesunate-quinine trial (SEAQUAMAT) conducted in southeast Asia [33] (Table 1).
Severe malaria: the clinical syndromes and complications
Cerebral malaria
Neurological involvement is common in African children. Typically, children with cerebral malaria present with a history of a febrile illness lasting one to three days with convulsions, impaired consciousness, with or without brain-stem signs. This is strictly defined as an unrousable coma that persists for more than one hour following a seizure (irrespective of anticonvulsant medication) since many children with malaria regain full consciousness after a brief convulsion. The most widely used paediatric classification of impaired consciousness in sSA is the Blantyre Coma Scale (BCS), a practical tool developed for children who are too young to speak [34,35]. Coma is classified as a BSC of 2 (out of a possible 5) or less. The precision of the clinical diagnosis of cerebral malaria, optimal for intervention studies, has been shown to be considerably improved by ophthalmoscopy (in temporarily-dilated pupils) to assess for malaria retinopathy [36]. The observation of a specific malaria retinopathy is supported by autopsy evidence of intracerebral parasite sequestration in a study of 27 Malawian children with fatal cerebral malaria [37].
Neuroimaging data describing the changes associated with cerebral malaria in African children remains very limited. The only prospective study using magnetic resonance imaging (MRI) involved 120 Malawian children with cerebral malaria (strictly defined as a BCS ≤ 2 plus positive retinopathy on ophthalmoscopy) [38]. It identified the most common pathological finding as an abnormal T2 signal in the basal ganglia (84%). In addition, cerebral volume was moderately-severely increased in nearly 50%, supporting evidence from previous autopsy data, which until this study remained inconclusive owing to the possibility that the findings could not exclude post-morbid changes. Potential mechanisms for increased volume suggested including parasite sequestration [37], venous congestion [39] or ischemic (due to seizures) and cytotoxic oedema. The MRI imaging indicated evidence of uncal or cerebellar herniation in nearly 10% [38], an unexpected finding since previous autopsy studies indicated that evidence of herniation was uncommon [37]. Clinically, papilloedema (a putative clinical sign of raised intracranial pressure) is considered uncommon in children with severe malaria. This is supported by a review of ophthalmoscopic findings from 436 children prospectively recruited into several studies of cerebral malaria in Kenya, Malawi and The Gambia [36]. Bilateral swelling of the optic nerve heads occurred in only 6% in marked contrast to the very prevalent retinal changes. Of note, in over 50% of children with papilloedema there was no other abnormality in the fundus; however, prognosis with this sign was very poor.
Seizures are the most common neurological complication of acute P. falciparum malaria, manifesting as either simple tonic-clonic or partial convulsive episodes [40] to clinically silent electrical status [41], which may or may not be clinically detected as excess salivation and/or an irregular respiratory pattern [42]. Overall, 38% of Kenyan children had a history of seizures or evidence of seizures at admission to hospital. Multiple seizures occurred in over 50% of these cases, with 22% having a prolonged seizure episode (>30 minutes). The peak prevalence of seizures (49%) occurred in children 27- to 33-months old and were generally associated with a shorter duration of illness and higher P. falciparum malaria parasitaemia [43]. Whilst short-lived seizures frequently occur in young children with febrile illnesses, and have limited prognostic significance, whether these are specifically related to acute malarial illness was explored in a paper examining the MAF. Children admitted with two or more seizures in 24 hours prior to admission had very high MAFs, suggesting that acute malaria was the chief cause of convulsions [44].
In addition to seizures, abnormal motor posturing (AMP) is also a common complication of children with cerebral malaria, manifesting as generalised extension of the trunk, increased muscular tone and posturing in the upper and lower limbs and clinically characterised as de-corticate, de-cerebrate or opisthotonic posturing. Whilst the aetiology and pathogenesis remains poorly understood, Idro and colleagues attempted to define the burden and the prognosis of each type of posturing. In 417 Kenyan children with cerebral malaria, 163 (39.1%) had posturing during hospital stay, with 50% developing AMP after admission [45], indicating a higher prevalence than previously described since previous studies mainly reported this complication at the point of admission. De-corticate posturing was the commonest manifestation occurring in 80 (49%), de-cerebrate AMP in 61 (37%) and opisthotonic posturing in 22 patients (14%). Case fatality rate was high in those with AMP (31; 19%), with the terminal mode of death in 19 (61%) suggestive of trans-tentorial herniation. Posturing was associated with age over three years but not with any of the markers of severity, except for opisthotonic posturing which was independently associated with severe metabolic acidosis. Seizures after admission were more common in those with de-cerebrate and opisthotonic manifestations.
Outcome for cerebral malaria remains poor with high in-hospital mortality and neurological sequalae in survivors. In the AQUAMAT trial the subgroup with the greatest mortality were children with coma, with an overall mortality of 359/1,825; 19.6% [30]. Outcome was no better in the artesunate-treated children (18%) than in the quinine-treated children (21%). Estimates of the prevalence of neurological sequelae deficits in survivors of cerebral malaria vary [46-48]. To counter this, a meta-analysis was conducted including studies which had similar case definitions of cerebral malaria, indicating that sequelae occurred in approximately 11% [49]. The most common neurological sequelae reported were ataxia (43%), hemiplegia (39%), speech disorders (39%), blindness (30%), and cognitive [50,51] and behavioural abnormalities [52]. Some of the deficits were transient (for example, ataxia) and fully resolved, whereas others showed improvement over months (for example, hemiparesis) but did not fully resolve [53]. A history of previous seizures, deep coma and focal neurological signs observed during admission were independent risk factors associated with persisting impairments [54].
Severe anaemia
Severe anaemia in children in sSA remains a leading cause of hospital admission [55] and a major factor in the 800,000 malaria deaths/year [56]. It is a common presenting feature of severe P. falciparum malaria in African children, particularly young infants in high transmission settings. It is caused by haemolysis of both infected and uninfected erythrocytes and exacerbated by impaired erythropoiesis [57]. Within international guidelines (WHO) and across different African countries there are some discrepancies with respect to the definition of severe anaemia (and, thus, the threshold haemoglobin or haematocrit level at which transfusion is recommended), some defining severe anaemia as Hb <5 g/dl whereas others use Hb <6 g/dl. For research definitions, severe malarial anaemia is defined as Hb <5 g/dl in recent guidelines (with parasitological evidence of malaria infection) [58].
In terms of prognosis, since the prevalence of pre-morbid chronic mild to moderate anaemia is very common in these populations, presentation in the absence of any other complications has a lower MAF [32] and carries a good prognosis with a case-fatality of <1% [27]. However, if combined with a parasitaemia of ≥2,500 the MAF increases to over 90% [32]. It is also important to note that, in addition to those presenting with severe anaemia, this complication may also develop during hospital admission especially in children with hyperparasitaemia [59], hence the frequent need to monitor Hb. The presence of respiratory distress increases case fatality (approximately 15%) rising to 40% if also complicated by impaired consciousness [27,60]. Although timely transfusion can be life-saving, access to adequate supplies of blood for transfusion remains a key challenge in sSA. In order to preserve this scarce resource, guidelines developed by the WHO encourage the rational use of blood transfusion and recommend that transfusion be reserved for children with profound anaemia (Hb ≤4 g/dL) or for those with a Hb between 4 to 6 g/dL who have additional severity critieria in areas where malaria is hyperendemic but suggest a higher transfusion threshold of 7 g/dl in areas of low malaria transmission [21]. Guideline-adherence remains poor and hampered by the lack of clinical evidence that this policy is safe in both the short and long term. It has been shown that 63% of the early deaths occur in children awaiting transfusion [61-63]. Furthermore, WHO guidelines recommend a standard volume of 20 ml/kg of whole blood (or 10 ml/kg packed cells) for any level below 5 g/dl; however, in practice this results in only a modest Hb rise of mean 2.5 to 3.3 g/dl following initial transfusion with approximately 25% remaining severely anaemic (<5 g/dL) [61]. High case fatalities of children with severe malaria anaemia has resulted in recommendations that the current transfusion guidelines be evidence-based and tested in a clinical trial [64,65].
Metabolic acidosis and respiratory distress
Improved diagnostic capabilities have led to a better understanding of the importance of metabolic acidosis as a common complication of severe malaria, despite its clinical correlates (deep ‘Kussmaul’ breathing) being recognised for decades [10,19]. Historically, respiratory distress in children with severe malaria has been considered synonymous with congestive cardiac failure [66], although recent work suggests that heart failure is rare, whereas deep breathing or metabolic acidosis [67] is central to the pathophysiology. Moreover, clinical examination findings and chest radiographs are usually normal, providing further evidence that pulmonary oedema or ‘acute respiratory distress syndrome’ is rare in children, although common in adult severe malaria [21].
Despite being a common complication of severe malaria, the aetiology of malarial acidosis is not well understood. At a clinical level metabolic acidosis is more frequent in children with severe anaemia [23], hypovolaemia [21], altered rheological properties of non-parasitised red blood cells (npRBCs) [24] and hepatic or renal dysfunction (due to decreased elimination) [16,25,68]. Both increased production and impaired metabolism of lactate [20] and ketoacids [14,21,22] have been implicated as causes; however, other unidentified organic acids also contribute [21,69,70]. Use of sodium bicarbonate to correct acidosis has fallen out of favour, largely since it failed to address the underlying processes and conferred no clinical benefit [27]. Treatment of acidosis with signs of hypovolaemic shock is covered later in the clinical trials section (see Fluid and vasopressin use for correction of acidosis and shock). Current management guidelines recommend prompt correction of hypoglycaemia, severe anaemia with a blood transfusion, intravenous fluids at 3 to 4 ml/kg/hour (maintenance) and careful monitoring [21].
Hypoglycaemia
Hypoglycaemia is an important complication of severe P. falciparum malaria, especially in children and pregnant women. Ten percent of children enrolled in the AQUAMAT trial had hypoglycaemia (glucose <3 mmol/L) at the point of admission [30] whereas other studies in African children report higher frequencies at and during the course of admission [71-74]. Hypoglycaemia is independently associated with poor outcome [27,53,75], specifically an increased mortality [28,71,76,77], predominantly when accompanied by acidaemia (pH <7.3) or hyperlactataemia (lactate >5 mmol/l) [60,73]. If not carefully monitored, hypoglycaemia can go unnoticed leading to neurological impairment and neurological sequelae [47,54,75]. The aetiology is incompletely understood and is likely to be multifactorial. Depletion of glucose stores due to starvation, parasite utilisation of glucose and cytokine-induced impairment of gluconeogenesis have been implicated [78]. Hyperinsulinaemia, secondary to quinine therapy, has been advanced as an iatrogenic cause and is well established in adults [79,80]. Data on its relationship in African children with severe malaria are relatively few, but what does exist indicates that insulin levels are appropriately low during episodes of hypoglycaemia, either at admission or during quinine treatment [74,81].
In clinical practice there are several definitions of hypoglycaemia, each targeting a different blood glucose threshold. In adults and children hypoglycaemia defined as a blood glucose of <2.2 mmol/L has been shown to be associated with a poor outcome [81] and, hence, this definition is incorporated as the research case definition of severe malaria (for epidemiological and research purposes) [21]. Paediatric treatment guidelines indicate a blood glucose of <3 mmol/L [82], which is now incorporated in the latest 2012 WHO severe malaria guidelines as the threshold for intervention [21]. A retrospective study examining the outcome across the range of blood glucose in 418 Malian children with severe malaria found a 61.5% case fatality at a glucose level of <2.2 mmol/L and 46.2% in those with low glycaemia (blood glucose 2.2 to 4.4 mmol/L) compared to 13.4% in those with normoglycaemia (4.5 to 8.2 mmol/L) [83]. The authors concluded that 6.1 mmol/L is an optimum threshold for intervention, which is substantially higher than currently recommended [58]. The poor outcomes of children at higher glucose levels (up 4.0 mmol/L) were also noted in a general admission population of Kenyan children in whom this was found associated with increased odds of mortality compared to all levels of glucose concentration above this threshold [84]. Risk factors associated with hypoglycaemia (glucose ≤3 mmol/l) at baseline and subsequent development of hypoglycaemia was examined in a retrospective review of 1,234 cases of severe P. falciparum malaria [85]. Included in the study were 952 children admitted to hospital before and 282 children admitted after the introduction of the new WHO quinine regimen (when a loading dose of quinine was increased from 10 mg/kg to 20 mg/kg). At baseline (and before use of quinine) hypoglycaemia was present in 16% of the initial cohort and 9% of the second cohort. Following admission (and initiation of intravenous quinine therapy), 15% developed one or more episodes of hypoglycaemia, with over 70% of episodes occurring within 24 hours of admission. There was no evidence of a relationship between quinine dose and any degree of hypoglycaemia after admission. Admission characteristics that predicted later hypoglycaemia were hypoglycaemia, severe anaemia and temperature gradient (a marker of impaired perfusion). Hypoglycaemic episodes were more common during transfusions or periods of disruption of intravenous glucose infusion. Overall, fatal outcome was more common in children developing hypoglycaemia after admission (case fatality 24%) than their euglycaemic counterparts (8%) [85].
As in sepsis, dysregulation of the cortisol, insulin, mitochondrial, or other metabolic pathways have been implicated in the aetiology of hypoglycaemia and deserve further investigation. The evidence supporting the current threshold suggests that intervention at a higher cutoff maybe warranted but this needs to be tested in an adequately powered clinical trial directly investigating the optimum threshold for treating hypoglycaemia and the best mode of treatment (dextrose loading or infusion).
Evidence for renal involvement in African paediatric severe malaria
Renal involvement in severe malaria is common in adult non-immune case series and semi-immune cases in south- and southeast Asia (around 25% to 50% across various series). Patients may progress to acute kidney injury with anuric or oliguic renal failure [86]. However, in paediatric severe malaria acute renal impairment has been assumed to be minimal [87], but the piecemeal accumulation of data now suggests this problem has been under-recognised. Studies examining prognostic risk factors in Gambian children with severe malaria noted that biochemical evidence of hepatic and renal dysfunction were important additional markers of a poor prognosis, but, contrary to the adult experience in severe malaria, none developed acute renal failure [28]. Several large clinical studies have confirmed the independent significance of raised BUN (>20 mg/dl) or creatinine (>80 mmols/L) and acidosis as poor prognostic signs in severe malaria in African children [31,60]. BUN and pH are measures of hypovolaemia or dehydration but also reflect decreased elimination due to impaired renal function. These measures are key laboratory parameters incorporated in the Risk Injury Failure Loss End-Stage (RIFLE) classification of acute kidney injury [88]. A prospective study in Kenyan children [60] showed that an elevated creatinine (>80 mmols/L) complicated 96/469 (20%) cases at admission and was associated with a case fatality of 26%. In the same study, four factors were independently associated with fatal outcome (deep ‘acidotic’ breathing, hypoxia (SaO2 < 90%), hypoglycaemia (<2.5 mmol/L) and creatinine >80 mmol/L (the odds ratio for mortality with elevated creatinine was 5.76 (95% CI 2.3 to 14.3) P = 0.0002). In the AQUAMAT trial 1,009/4,148 (24%) had a BUN >20 mg/dL [30] and this parameter was established as one of the three independent clinical features predicting fatal outcome, together with acidosis and impaired consciousness/convulsions [31]. The mortality in children with all three predictors was 43% (Figure 2). In the FEAST trial BUN >20 mg/dL was present on admission in 444/2,118 (21%), with prevalence varying across the sites, being more frequent in hyperendemic areas of Eastern Uganda 265/1,037 (25.6%) and less frequent in Kilifi, Kenya where malaria is mesoendemic (25/189 (13.2%) [89] (KM, unpublished data).
The aetiology of renal injury in the paediatric kidney is unknown and may reflect multiple insults including hypovolaemia or dehydration (pre-renal failure) and direct tubular or glomerular injury. Pathological studies in adults with severe malaria have shown sequestration of parasitised red cells in glomerular and tubulo-interstitial vessels and acute tubular damage due to accumulation of monocytes in glomerular capillaries. The level of sequestration in the kidney was greater in those who developed renal failure than in fatal cases without renal failure [90]. No equivalent autopsy data are available for African children. WHO malaria treatment guidelines consider acute kidney injury as a serum creatinine level >250 mmol/L in adults [91] but does not indicate any criteria for children. Guidelines for the diagnosis and treatment of renal involvement are needed, as is rational integrated fluid management and other supportive treatment in paediatric malaria [87], which do not currently exist.
Haemoglobinuria
Haemoglobinuria, or blackwater fever (BWF), a syndrome comprising acute intravascular haemolysis, fever and the passage of dark- or red-coloured urine, in patients with current or recent malaria infection, is recognised as a potential complication of malaria. Classically, it was noted to be a consequence of long term use of quinine in non-immune expatriates [92-94]. In African children BWF is considered as a rare complication of malaria [27,28,91,95], which is now supported by data from the AQUAMAT trial [30]. BWF was reported in only 237/5,426 (4.4%) with a case fatality rate similar to the rest of the trial participants (22 deaths: 9.3%) [31]. The development of haemoglobinuria in children after admission, irrespective of treatment arm, was also rare, <1%. A prospective study of severe malaria in children in Papua New Guinea, reported the presence of BWF, attributable to the passage of haemoglobin and/or myoglobin (suggesting muscle breakdown) in the urine, but found no association with glucose-6-phosphate dehydrogenase (G6PD) deficiency [96]. In Vietnam, in a case series of semi-immune adults with BWF, in which only 32% had concurrent P. falciparum malaria infection, aetiological factors included quinine treatment (56%) and G6PD deficiency (54%) [97]. In Africa, recent publications describing case-series of BWF tend to be from regions where children are exposed to intense P. falciparum malaria transmission (Nigeria, Democratic Republic of Congo (DRC), and Uganda) [98-100]. In a case-control study conducted in the DRC, the majority (88.4%) of BWF cases occurred in the rainy season when BWF was apparently more likely to be related to quinine pre-treatment. In this series, seven children (16.2%) developed acute renal failure [98]. In Nigerian children, a study of severe malaria reported that haemoglobinuria (defined by dip-stick testing of urine) occurred in 48/251 (19.1%), was commonly associated with clinical jaundice (28/48, 58.3%) and that 6% developed renal failure [100]. Unlike the G6PD variants in southeast Asia the African variant (A-) is a mild variant, with most males retaining 20% of normal G6PD activity, sufficient to protect carriers from side-effects of oxidizing drugs or food products. G6PD deficiency is, therefore, unlikely to be a major cause of BWF; if it were, then one would expect that BWF would be more widely reported as a common complication of malaria owing to the high population frequencies in sSA, where it is present in 18% to 20% in males and 5% in females [101].
There is, however, renewed interest in this topic since there have been a number of case series reported from Europe of delayed haemolytic anaemia following treatment of severe malaria with injectable artesunate [102,103]. All cases were successfully treated with transfusions. The syndrome, now labeled as Post-Artesunate Non-infectious Delayed Haemolysis and Anaemia (PANDHA) or PADH for short, is reported to occur in up to 25% of artesunate-treated non-immune adults, typically two weeks after the treatment course. An expert group review panel reviewed world literature and found that PADH was not specific to a particular preparation or manufacturer [104]. Further insights into its pathogenesis have now been established as the delayed clearance (through haemolysis) of once-infected red cells. These ‘pitted’ erythrocytes had been previously spared by artesunate (with quinine treatment they would be removed from the circulation), since the artemisinins induce splenic removal of parasites leaving the red cell intact (a process known as pitting) [105]. Why some patients are susceptible to PADH remains unknown. Data from malaria endemic areas on the occurrence of this condition are lacking.
Increased risk of bacterial co-infection
Bacteraemia is an important complication of severe malaria in African children but is often under recognised, largely a result of limited and poorly maintained microbiology services across sSA. Nevertheless, data have slowly emerged, mainly from hospitals linked to research programmes, indicating that there may be a biological link between malaria and susceptibility to invasive bacterial infection (IBI). A study in Teule, Tanzania, reported that up to a third of paediatric severe malaria deaths were attributed to bacteraemia [106]. Another large epidemiological study conducted in Kilifi, Kenya, showed that more than 50% of all cases of bacteraemia occurred in the presence of malaria [107]. A systematic review compiling data from epidemiological studies and clinical studies of paediatric hospital admissions of P. falciparum malaria (describing IBI) across sSA examined the evidence supporting a biological or epidemiological relationship [108]. In the meta- analysis of ten studies which included data from 15 centers in 11 sSA countries involving 7,208 children with severe malaria, reported over the period 1992 to 2010, found a mean prevalence of IBI co-infection of 6.4% (95% CI 5.81 to 6.98%). Bacterial co-infection resulted in higher case fatalities compared to children with severe malaria alone 81/336 (24.1%) versus 585/5,760 (10.2%). The major pathogens associated with IBI were non-typhoidal salmonellae (NTS), Escherichia coli and other enteric gram-negative organisms. There was also some evidence indicating greater risk of NTS IBI in children with malarial anemia [108].
In order to reduce IBI-associated malaria mortality, whilst minimising the risks of excess antibiotic prescribing, further research is needed to establish children at greatest risk of bacteraemia, to inform a policy for targeted antibiotic therapy. For example, Nadjm and colleagues proposed simple clinical criteria [106] which identified 85% of malarial cases with culture-proven bacteraemia. The criteria included an axillary temperature >38°C or <36°C with parasitological evidence of current or recent P. falciparum malaria infection plus one or more of: prostration, respiratory distress (chest indrawing or deep breathing), severe anaemia (Hb <5 g/dL), or HIV infection. A pathogen was isolated from aerobic blood cultures in approximately 20% of children (1-week to 12-years old) meeting these criteria. The ‘Teule criteria' are yet to be tested in prospective intervention trials, which could help with future policy of directed (where microbiological services are not available) or short-course empiric therapy with early termination guided by culture results to prevent development of resistance, which is commonly practiced in high-income countries [109].
Treatment of severe malaria
Quinine has been the mainstay of treatment for African children with severe malaria for decades; it remains effective and little drug resistance has been reported from the continent. The arrival of the artemesinin compounds led to a series of small clinical trials to test their safety and efficacy. The first comparative clinical trials investigated artemether (derivative of dihydroartemisinin, the active antimalarial agent), which because of its poor water solubility can only be injected by the intramuscular route. In clinical trials it proved to be safe but when the data on efficacy were collated in a meta-analysis (including 1,919 randomised patients) it did not lead to an improved overall survival, specifically in African children. This was followed by trials investigating another artemisinin formulation, artesunate, which in contrast to parenteral artemether, is water-soluble and can be given intravenously and is instantly bioavailable [110]. Even intramuscular artesunate is absorbed reliably and rapidly, with peak concentrations occurring within one hour [111]. The SEAQUAMAT trial, conducted in South East Asia (including 202 children) was stopped early after enrolment of 1,461 patients owing to a substantial benefit for patients receiving artesunate [33]. Mortality in artesunate recipients was 15% (107 of 730) compared with 22% (164 of 731) in quinine recipients; a relative reduction of 34.7% (95% CI 18.5 to 47.6%; P = 0.0002).
A further trial in African children was justified since expert review at that time considered that the issue of parasite drug resistance to quinine was not an issue (as it was in South East Asia), that quinine remained the optimal antimalarial and owing to the rapid tempo of severe disease in African children with severe malaria compared with adults in South East Asia there were questions about the generalisabilty of the SEAQUAMAT trial. In severe malaria in children most deaths occur within the first 24 hours whereas survival benefit for many patients in the SEAQUAMAT trial occurred after this time point. These issues highlight the importance of equipoise as a strong scientific justification and a prerequisite to conduct further clinical trials with meaningful clinically relevant endpoints (that is, disability-free survival). The AQUAMAT trial enrolled children at the point of hospital admission. The criteria for enrolment were broad and pragmatic with a view to future generalisability of the trial results, principally if the clinician considered the child required parenteral antimalarial medication they were eligible for inclusion in the trial. Diagnosis was reinforced by quality controlled laboratory evidence of P. falciparum malaria infection. The primary endpoint was in-hospital mortality. By intention to treat, 297 children (10.9%) receiving quinine treatment died compared to 230 (8.5%) children who received artesunate. Overall, this translated to a relative reduction in mortality of 22.5% (95% CI 8.1 to 36.9) in children in the artesunate arm (P = 0.002) [30], with no difference in outcome whether the drugs were administered intravenously or intramuscularly. In the analysis of secondary endpoints there were no differences in outcome across any of the major clinical spectra defining severe malaria. The development of coma and/or convulsions was more common during hospital admission in the quinine arm (P = 0.02); but there were no other differences between the arms in number of other complications, additional treatments prescribed, time to recovery or numbers with neurological sequelae – which included 61 persistent mild, moderate or severe such sequelae among survivors [30]. The trial led to a major guideline change for anti-malarial treatment of paediatric severe malaria, which now recommends a preference for parenteral artesunate over quinine [21].
Adjunctive therapies in severe malaria
The outcome of severe malaria is largely determined by the complications and number of vital organ dysfunction and quality of care available. For most African children this will not include an admission to an intensive care or high-dependency care unit, instead management will be more usually on a busy paediatric ward. It is important to emphasize that the most important factor for management is the implementation of specific antimalarial drug treatment and that this is given as early as possible to reduce the risk of adverse outcome. As is the case in management of severe sepsis, supportive therapies aimed at correcting deranged physiology are also fundamental to improving outcome; however, of the adjunctive agents tested in clinical trials in both adults and children all have failed to show benefit, with the exception of renal replacement therapy in adults [112]. With respect to the high risk group of cerebral malaria, of the 33 clinical trials summarised in Table 2 investigating a range of specific or supportive therapies, 15 have been targeted to the sub-group with cerebral malaria and most have shown harm in those receiving the interventional therapy. These will be reviewed, initially in chronological order, but are largely clustered within a treatment-specific paradigm.
In general, many of these trials were single-centre phase I or II studies with low sample sizes, often constrained by funding and slow or truncated trial recruitment. A number of trials were terminated early due to political instability, meeting pre-defined safety stopping rule or due to evidence of adverse outcome in the interventional arm. Many trials had primary endpoints targeting clinical surrogates for prognosis (for example, correction of acidosis or cytokine or parasite clearance) and so, as is usual in Phase II trials were not powered to inform meaningful endpoints such as mortality, but are important steps in the justification for further testing in larger trials. Methodological issues were noted in some trials, for example, in some the primary endpoint was not pre-specified, methods of randomisation were not reported and some trials appeared to recruit patient populations with substantially lower overall lower mortality than would be expected, thus reducing the external validity of the results. How we interpret these trials is possibly helped by one overarching emerging theme: that most did not result in a positive outcome for any of the patient-centred endpoints in the interventional arms (that is, those that are clinically relevant). Ordinarily, the early stopping of trials, especially when interim analysis suggests large treatment effects, has been criticised as, more often than not, interim results on small numbers tend to overestimate treatment effects [113] which are often not replicated in larger multi-centre studies. Some therapies may have been disregarded for the same reason in severe malaria; however, it would be difficult to warrant further exploration of a therapeutic intervention in which a trial had been stopped by an external committee reviewing safety for excess harm rather than for futility.
Steriods: dexamethasone
In order to reduce or prevent cerebral oedema, two separate trials investigated whether the addition of dexamethasone improved the outcome of cerebral malaria in adults and children [114,115]. The trial in Thai adults showed that dexamethasone-treated patients had a more prolonged period of coma (mean 63.2 hours versus 47.4 hours in the placebo arm). Disturbingly, its use led to an increased risk of pneumonia and/or gastrointestinal bleeding in 26/50 compared to 11/50 in the placebo arm [114]. The second trial, conducted in Indonesian children and adults with cerebral malaria, also showed that dexamethasone led to an increased risk of gastrointestinal bleeding with no apparent benefit [115]. A Cochrane review that pooled the data from these two trials (N = 143 participants) found no difference in mortality (relative risk 0.89; 95% CI 0.48 to 1.68; 143 participants, increased risk of GI bleeding in both trials 7/71 (10%) in the intervention-arm compared to 0/72 (0%) in control, a relative risk of 8.17 (1.05, 63.57). The review found no overall increased risk in invasive bacterial infection [116] but highlighted that a major limitation was that neither had trial follow up beyond discharge from hospital, so that the effects of corticosteroids on residual neurological deficits, therefore, could not be assessed. The review concluded there was no evidence to support the use of dexamethasone in cerebral malaria, although numbers involved were small and the assessment of complications in both trials was incomplete.
Pentoxifyllin
The pathogenesis of severe malaria involves several different processes, including enhanced production of the cytokines including tumour necrosis factor (TNF), sequestration of parasite red cells to the endothelium and decreased erythrocyte deformability. Since pentoxfylline (Pt) has beneficial effects on many of these processes, in particular increasing red cell deformability (and thus improving local tissue perfusion), it was postulated that it might improve outcome in severe malaria. The next phase of trials investigated the addition of Pt to standard antimalarial therapies, primarily aimed at suppression of TNFα production. In total, five trials investigated its use in cerebral malaria, or all-cause severe malaria [117-121]. Two were conducted in African children (Burundi [117] and Kenya [121]). Three trials were stopped early: one due to civil conflict [117] and two due to safety concerns [119,121]. The Burundi trial had enrolled 56 of a projected 100 children with cerebral malaria when it was stopped. There were no deaths in the Pt arm (n = 26) compared to 5 of 30 (17%) in the control arm; 8% of both groups developed neurological sequelae [117]. Owing to the small sample size the results were inconclusive. The second paediatric study, a dose escalation study, conducted in Kenyan children with cerebral malaria was stopped due to safety concerns. A significantly higher mortality occurred in the Pt arm 4/10 (40%) versus 1/5 (20%) in controls [121]. A trial conducted in Thai adults (n = 45) showed no significant differences in any of the arms (which investigated low dose Pt, high dose Pt versus control) for any of the outcome measures [118]. Another trial conducted in Indian adults involving 22 in the Pt arm and 30 controls showed reductions in TNFα (baseline to day 3) in the Pt arm compared to increases in the control arm. Mortality was 25% in the control arm and 10% in the Pt arm [120]. However, there were methodological limitations in this trial since the method for allocation of study arms was not stipulated nor were the study endpoints pre-specified. Owing to lack of overall clinical benefit, and those that were favorable largely related to secondary endpoints, and a suggestion of increased adverse outcome, further exploration of anti-TNF therapies have not been pursued.
Monoclonal antibodies, immunoglobulins and anti-sequestration therapies
A controlled factorial trial of monoclonal antibodies (Mab) against TNF-α in Gambian children (N = 610) which also compared artemether and quinine, showed faster fever clearance but no survival benefit in children treated with Mab (19.9%) compared to controls (20.8%), after adjustment for antimalarial strategy [122]. The trial also demonstrated a significantly increased risk of long-term (six months) neurological sequelae in survivors 15/221 (6.8%) in Mab recipients compared with 5/225 (2.2%) in controls. The authors suggested that whilst there was evidence that antibody acts to retain and prolong TNF within the circulation (leading to fever reduction) this may inadvertently increase its harmful effects on the vascular endothelium and, in turn, aggravate neurologic complications. A trial investigating pooled intravenous immunoglobulin (IVIG) from blood bank adult donors and, thus, presumptively immune to malaria in Malawian children with cerebral malaria was stopped early after enrolling 31 children for futility (in accordance to a pre-planned stopping rule) [123]. For those receiving IVIG 10/16 (62.5%) died or developed neurological sequelae compared to 3/15 (20%) in the placebo arm. A further placebo controlled trial conducted in 28 Thai adults >14 years old (enrolled using WHO severe malaria criteria) investigated polyclonal anti-TNF-α antibodies in addition to artesunate. Included in the study were seven participants with cerebral malaria, 46% had hyperparasitemia (13 of 28) and 39% had circulatory shock (11 of 28) [124]. Compared to controls antibody treatment reduced IFN-g concentrations in a dose-related manner and unbound TNF-α was undetectable after Fab treatment, irrespective of dose. The composite clinical endpoint, including duration of coma in cerebral malaria and the development of other severe manifestations or complications, was hampered since it was only possible to record coma recovery in five patients; hence, the results were largely inconclusive.
A controlled Phase II trial investigating the use of the oral anthelmintic drug levamisole hydrochloride (previously shown to inhibit cytoadherence in vitro and reduce sequestration of late-stage parasites in uncomplicated P. falciparum malaria [125]) included 56 Bangladeshi adults with criteria for all-cause severe malaria [126]. Linked pharmokinetic studies indicated absorption of levamisole was reliable with a mean plasma level of 97% of expected levels in healthy adults. However, there was little marked effect upon parasite sequestration, lactate clearance (a putative marker of tissue oxygenation and microcirculatory perfusion) or mortality. The authors suggested that despite previous observations in uncomplicated malaria treated with quinine, rapid parasite clearance with intravenous artesunate may have obscured any marginal benefit of levamisole on parasite sequestration.
Seizure prophylaxis
Since convulsions are common in severe malaria, in particular the sub-group with cerebral malaria, and associated with adverse outcomes including death and neurological sequelae (in children), routine administration of anti-epileptics to prevent the seizures was suggested. In a double-blind controlled trial in Thailand involving both children and adults with cerebral malaria, randomised to receive either a single dose of phenobarbitone (Pb) or placebo, there was a lower seizure rate in the Pb group at 12.5% (3/24) compared to 54% (13/24) in the placebo arm (P = 0.006) [127]. There was no effect on mortality, eight (33%) versus five (21%), respectively. Based on this small study the authors recommended that guidelines should advocate that all patients with cerebral malaria should receive a single intramuscular loading dose of Pb. A large single centre paediatric placebo-controlled trial (N = 340) conducted in Kenyan children with cerebral malaria, designed to provide the evidence for this new recommendation, examined a single intramuscular dose of Pb (20 mg/kg) versus placebo. As expected Pb recipients had a lower rate of seizures (defined as three or more seizures of any duration) than the placebo recipients (18 (11%) versus 46 (27%) odds ratio 0.32 (95% CI 0.18 to 0.58)) but the case fatality rate was more than double in the Pb arm (30 (18%) compared to placebo 14 (8%) deaths, relative risk 2.39 (95% CI 1.28 to 4.64)) [128]. The chief mode of death in those receiving Pb was respiratory arrest. Following this trial the guidelines changed and no longer recommend Pb prophylaxis in cerebral malaria. A further placebo controlled trial, conducted at the same centre in Kenya, in non-traumatic encephalopathy (including a cerebral malaria subgroup (N = 110)) investigated the use of fosphenytoin (a drug often used for seizure prophylaxis in neuro-trauma that has minimal cardiorespiratory side effects). It was terminated due to slow recruitment/futility. At least one seizure (monitored clinically and by electroencephalogram) occurred in 33/83 (40%) in children receiving fosphenytoin versus 32/88 (36%) receiving placebo (P = 0.733) [129]. In the cerebral malaria subgroup the prevalence of seizures in the fosphenytoin arm was 20, 37% which was identical to the placebo arm 21, 38%. Overall, 18 children treated with fosphenytoin (21%) died compared with 15 in the placebo arm (17%) (P = 0.489). In survivors rates of neurologic sequelae at three months were the same (10%) in both arms [129]. A study from India, reporting results from a clinical trial in adults as a correspondence piece, gave only limited details of the clinical trial methodology. The successful use of prophylactic Pb reported in this trial is questionable since it was not reported in full [130].
Osmotherapy: mannitol for treatment or prevention of cerebral oedema
Leading up to these trials were two observational studies, one case series and one uncontrolled trial, investigating mannitol and other osmotic diuretics as adjuncts for treating brain swelling (cerebral oedema) in African children with cerebral malaria [39,131]. These early studies suggested that mannitol may improve outcomes [39], and case series of children receiving urea with dexamethasone was reported to have a dramatic improvement [131]. A subsequent placebo-controlled trial, conducted in 156 Ugandan children with cerebral malaria, investigated a single dose of 5 ml/kg of 20% (1 g/kg) of intravenous mannitol infused over 20 minutes in addition to intravenous quinine. No important differences were found in the main outcomes, including time to regain consciousness or death [132]. Six children had postmortems of whom five had signs of anoxia and cerebral oedema; the sixth child had signs of acute tubular necrosis at autopsy. A controlled trial examining the use of 1.5 g/kg mannitol followed by 0.5 g/kg every eight hours in Indian adults with death as the primary endpoint found an increased mortality in those receiving mannitol, 9/30 (30%), compared to 4/31 (13%) in the control (no mannitol) arm [133]. Mannitol also prolonged coma resolution. Whilst there is good evidence that brain swelling complicates both adult and paediatric cerebral malaria, trials to date have shown no benefit of osmotherapy or steroids (see earlier).
Iron chelation
The use of iron chelating agents was considered for adjunctive therapy in severe malaria. The positive hypothesis suggested that by chelating free iron these drugs would thus withhold iron which is required by malaria parasites to mature and multiply and, thus, limit or inhibit parasite reproduction rate. A Cochrane review of the data on the uses of iron chelation was conducted in 2007 [134]. Whilst seven trials involving 570 participants met the inclusion criteria, four of these were excluded as they included non-severe or asymptomatic malaria or had methodological issues. In children with severe malaria two controlled trials examined desferrioxamine (DFO) [135,136] with cerebral malaria and one studied deferiprone [137] in Indian adults (13 to 84 years) with severe malaria.
The first study conducted in a Zambian hospital involving 83 children with cerebral malaria indicated a lower mortality in DFO recipients, 7/42 (16.7%), compared to placebo, 9/41 (22%). Moreover, time to coma recovery was faster in the DFO arm [135]. A second, larger paediatric trial conducted at two centres in Zambia was stopped early on the recommendations of the data monitoring committee for safety, as there were more deaths in the DFO arm, 18.3% (32/175) compared to 10.7% (19/177) in the placebo group [136]. Overall, the pooled estimate for both trials (435 participants) indicated a non-significant increased risk of death in the DFO group. The risk of experiencing persistent seizures was lower with DFO compared with placebo (RR 0.80, 95% CI 0.67 to 0.95; 334 participants, one trial), but adverse effects (including phlebitis and recurrent hypoglycaemia) were more common with DFO (risk ratio for hypoglycaemia 1.48 (95% CI 0.97 to 2.26)) [134]. The adult trial comparing deferiprone with placebo found that the deferiprone group had significantly faster coma recovery and parasite clearance [137]. No adverse effects were reported for this trial. No evidence of benefit or harm overall was concluded by Cochrane review [134].
Acidosis correction
N-acetylcysteine (NAC) has been proposed to lead to correction of metabolic acidosis by its antioxidant effect acting through direct scavenging of free radicals and replenishment of glutathione and cysteine. NAC has also been shown to have anti-parasitic effects [138]. Three trials have examined effects of different doses as adjunctive treatments to quinine or artesunate. The first, a small placebo controlled trial of NAC in Thai adults (N = 15 in each arm) had lactate clearance as the primary endpoint. Lactic acidosis resolution was better at 24 hours in the NAC group (10/15) than in the placebo group (3/15) (P = 0.011), as was median coma resolution although with wide variation and, thus, was non-significant. Need for renal replacement therapy (two in each arm) or death (arm in each arm) were similar [139]. A placebo controlled trial of three different NAC dosage regimens given in addition to artesunate had some methodological issues since the key endpoints were not pre-specified; methods of randomisation were not indicated and the study required patients to remain in hospital for 28 days. Few differences were found in fever, parasitaemia clearance and adverse medical events, although the reporting of these was incomplete. There were only two deaths in the trial indicating that the patients probably did not have severe malaria [140]. A multisite double-blind placebo controlled trial on the use of high dose intravenous NAC as adjunctive treatment to artesunate in 108 adults in South East Asia found that NAC had no significant effect on mortality, lactate clearance times (P = 0.74) or coma recovery times (P = 0.46). Parasite clearance time was increased but largely attributable to differences in baseline parasitaemia,nor did NAC have any effect on red cell deformability properties [141]. In summary, despite some methodological concerns and the small size of the trials, the limited data available from these do not provide justification for further investigation of NAC as an adjunctive treatment. Similarly, a lack of efficacy was found in another small study of L-arginine; however, the results were not conclusive since the trial was halted early due to political instability [142].
Fluid resuscitation, inotrope and and vasopressors: shock and acidosis
Both dopamine and adrenaline (epinephrine) are used in the management of infection-induced haemodynamic shock as second line treatments when shock is refractory to fluid boluses or when hypotension prevails [109]. Dopamine has been used to improve mean arterial pressure (MAP) and cardiac output, primarily by increasing stroke volume and heart rate and low dose therapy has been used in the past to treat pre-renal acute kidney injury. Dopamine however carries an increased risk of supraventricular and ventricular arrhythmias. Adrenaline increases the MAP since it is a powerful vasopressor agent, but increases the risk of aerobic lactate production [109]. In Vietnamese adults with severe sepsis (n = 10) and severe malaria (n = 13), a crossover trial examining increasing intravenous adrenaline infusion compared to increasing dopamine doses found adrenaline and dopamine infusions led to significant mean increases in cardiac index (which was greater with adrenaline than dopamine), increased MAP and a reduction in systemic vascular resistance. However, inotropic doses of adrenaline resulted in the development of lactic acidosis and falling pH and thus curtailed the adrenaline dose-profile at some stage in 16 patients (84%). No significant differences were found between sepsis and malaria subgroups with respect to disease effects or responses to treatments [143]. Further investigation of adrenaline was, therefore, not warranted.
Justification for investigating fluid resuscitation as an adjunctive treatment in children with severe malaria originated from the high mortality noted in association with metabolic acidosis [27,67,144]. It was postulated that in children with severe malaria complicated by metabolic acidosis in accordance with other causes of paedaitric severe life threatening illness this is commonly due to some degree of hypovolaemia [145], although this view was controversial in severe malaria [146]. Prospective studies had identified markers of impaired perfusion (delayed capillary refilling time, weak pulse, subnormal systolic blood pressure and increased creatinine) in children with metabolic acidosis as key correlates with poor outcome [60]. Initial dose-finding studies in this subgroup established that boluses of 20 to 40 ml/kg normalised low central venous pressure, reduced tachycardia and tachypnoea without adverse consequences [147] and further studies established appropriate effects of fluid therapy on myocardial performance [148]. In total, five Phase II trials were conducted in Kenyan children with severe malaria comparing different fluid types on physiological endpoints, including correction of metabolic acidosis (base excess) and haemodynamic parameters as well as mortality and neurological sequelae in survivors. The results of these trials are individually summarised in Table 2 [60,149-152] but have been formally collated (four of five) in a meta-analysis examining types of fluid resuscitation therapy published in 2010 [153]. This review compiled data from all published paediatric clinical trials of fluid resuscitation. In the subgroup with malaria these were the only four trials (none of which had a control arm), and all had similar designs, all showing comparable reductions in acidosis (the primary endpoint) as well as features of shock in children receiving either 0.45% human albumin solution, 0.9% saline or Gelofusine (a gelatin based colloid) [153]. When the mortality data from all four trials were combined in the meta-analysis this indicated that albumin significantly reduced mortality (secondary endpoint) compared to either of the other fluids (saline or Gelofusine), risk ratio 0.31 (95% CI 0.14 to 0.68) (P = 0.004). There was a non-significant increase in neurological sequelae in survivors in those treated with albumin 9/97 (9%) compared to other resuscitation fluids, 6/54 (6%) in saline and 1/37 (3%) in gelofusine [153]. A further trial comparing Dextran 70 (D70) (n = 39) and 6% hydroxyethyl starch (HES) (n = 40) found no difference in the primary outcome (shock resolution at eight hours) (D70: 23/37 (62%) versus HES: 25/39 (64%)), although resolution of acidosis was better in the HES arm. Overall, case fatality (four in each arm, 5%) was similar [152].
The Fluid Resuscitation as A Supportive Therapy trial (FEAST) was conducted to provide evidence on the best fluid management for children with shock and severe febrile illness for doctors practicing in hospitals in resource-limited settings [89]. FEAST was a multicenter three-arm controlled trial comparing albumin bolus, and saline bolus to no bolus control. FEAST was conducted at six centres in three East African countries and involved 3,121 children enrolled at the point of hospital admission. Shock was defined pragmatically (incorporating parameters from all the published paediatric shock definitions including modest hypotension) and the controlled part of the trial (FEAST A) only excluded children without severe hypotension. Two major subgroups included in the trial were those with severe sepsis (n = 1,330) and severe P. falciparum malaria (n = 1,793). The data monitoring committee stopped the trial early after enrollment of 3,141 of a projected 3,600 due to safety concerns. The primary endpoint, 48-hour mortality, was significantly worse in the two fluid bolus arms, 111/1,050 (10.6%) in the albumin-bolus and 110/1,047 (10.5%) in the saline-bolus, compared to the control (no bolus) 76/1,044 (7.3%); relative risk (95% CI) any bolus versus control 1.45 (1.13 to 1.86, P = 0.003). Secondary endpoints including 28-day mortality were worse in the bolus arms, 12% versus 8.7% in the control arm. There was no difference between the treatment arms in the number of adverse events (suspected pulmonary oedema, brain swelling or allergic events). In the subgroup with severe malaria, 48-hour mortality was 110/1,202 (9.2%) in the bolus arms compared to 34/591 (5.7%) in the control (no bolus) arm, a relative risk of death of 1.59 (1.10 to 2.31). In all pre-specified sub-groups analysis, there was no evidence of a benefit of fluid boluses [89]. In a subsequent publication, early shock reversal at one hour (responders), the central principle of the surviving sepsis guidelines, was superior in the bolus arms compared to no bolus control (43% versus 32%, P <0.001). Despite this, excess mortality with boluses was still evident in both ‘responders’ (relative risk 1.98 (0.94 to 4.17), P = 0.06), as well as ‘non-responders’ at one hour (relative risk 1.67 (1.23 to 2.28), P = 0.001), with no evidence of heterogeneity (P = 0.68) [154]. Examining the terminal modes of death, the major difference between bolus and control arms was the higher proportion of cardiogenic shock in the bolus arms (n = 123; 4.6% versus 2.6% in controls, P = 0.008), rather than respiratory events or neurological terminal clinical events [154]. A major issue raised following the publication of FEAST was whether the criteria used to define shock in the trial were applicable to other guidelines, including the WHO definition of shock. A further publication provided data to address this issue showing that of the relatively limited number of children fulfilling the WHO shock definition 48-hour mortality was 24/50 (48%) in those receiving boluses compared to 3/15 (20%) in the no-bolus control, an increased absolute risk of 28% and a relative increase of 240% (P = 0.07 by two-sided Fisher’s exact test). Moderate hypotension, consistent with many definitions in paediatric shock, was also associated with increased 48-hour mortality on boluses (an absolute risk of 9.4% (‐2.6 to 21.4%)) [155].
A systematic review conducted after the FEAST trial concluded that the majority of evidence from randomised trials to date came from the FEAST trial and that boluses significantly increased mortality of children in shock, compared to those who did not receive boluses. The evidence was considered to be of high quality and sufficiently precise [156]. Prior to FEAST the evidence supporting fluid resuscitation was reviewed in the 2008 Surviving Sepsis Campaign Guidelines which was informed by a modified Delphi process, graded the current paediatric recommendation (20 ml/kg boluses over five to ten minutes up to 60 ml/kg) as 2C, indicating a weak recommendation with low quality of evidence [109,157]. The systematic review concluded that withholding of bolus fluids should be considered for populations similar to those enrolled in FEAST and that there remained important questions about the extent to which these results are applicable to other populations [156].
Transfusion
A Cochrane review including the only two African randomised controlled trials (RCTs) [158,159] conducted before 2000 (involving 114 and 116 children randomised to blood transfusion or oral haematinics) concluded that there was insufficient information on whether routinely giving blood to clinically stable children with severe anaemia either reduces death or results in a higher haematocrit measured at one month, and indicated the need for a definitive trial [64]. Since then a recent trial has evaluated the safety and efficacy of a higher volume of whole blood (30 ml/kg, n = 78) against the standard volume (20 ml/kg, n = 82) in Ugandan children which was found to be safe and resulted in an accelerated hematological recovery in children with severe anaemia [160]. A clinical trial is underway that is evaluating whether a liberal rather than conservative transfusion strategy in terms of a larger initial volume of transfused blood and incorporating a higher threshold of haemoglobin of <6 g/dl for transfusion will decrease both short and long term mortality (TRACT trial: ISRCTN84086586).
Conclusions
In conclusion, human trials carried out on the basis of pathophysiology studies, have so far made little progress on reducing mortality, despite appearing to reduce morbidity endpoints (such as convulsions, shock reversal or improvements in acid base balance or cytokines); more often than not, the supportive interventions have shown harm. A new line of investigation that aims to disrupt sequestration [161] looks promising and early phase trials are planned. For the key risk factors for poor outcome – coma, abnormal renal function, hypoglycaemia and acidosis – further studies and trials need to be conducted to help us understand how best to treat these complications.
References
Gething PW, Patil AP, Smith DL, Guerra CA, Elyazar IR, Johnston GL, et al. A new world malaria map: Plasmodium falciparum endemicity in 2010. Malaria J. 2011;10:378.
Noor AM, Kinyoki DK, Mundia CW, Kabaria CW, Mutua JW, Alegana VA, et al. The changing risk of Plasmodium falciparum malaria infection in Africa: 2000-10: a spatial and temporal analysis of transmission intensity. Lancet. 2014;383:1739–47.
World Health Organization. World Malaria Report: 2012. Geneva; 2012.
Roca-Feltrer A, Carneiro I, Armstrong Schellenberg JR. Estimates of the burden of malaria morbidity in Africa in children under the age of 5 years. Trop Med Int Health. 2008;13:771–83.
Black RE, Cousens S, Johnson HL, Lawn JE, Rudan I, Bassani DG, et al. Global, regional, and national causes of child mortality in 2008: a systematic analysis. Lancet. 2010;375:1969–87.
Feachem RG, Phillips AA, Hwang J, Cotter C, Wielgosz B, Greenwood BM, et al. Shrinking the malaria map: progress and prospects. Lancet. 2010;376:1566–78.
Moonen B, Cohen JM, Snow RW, Slutsker L, Drakeley C, Smith DL, et al. Operational strategies to achieve and maintain malaria elimination. Lancet. 2010;376:1592–603.
Sabot O, Cohen JM, Hsiang MS, Kahn JG, Basu S, Tang L, et al. Costs and financial feasibility of malaria elimination. Lancet. 2010;376:1604–15.
Tatem AJ, Smith DL, Gething PW, Kabaria CW, Snow RW, Hay SI. Ranking of elimination feasibility between malaria-endemic countries. Lancet. 2010;376:1579–91.
Barnes KI, Durrheim DN, Little F, Jackson A, Mehta U, Allen E, et al. Effect of artemether-lumefantrine policy and improved vector control on malaria burden in KwaZulu-Natal. South Africa PLoS Med. 2005;2:e330.
Chizema-Kawesha E, Miller JM, Steketee RW, Mukonka VM, Mukuka C, Mohamed AD, et al. Scaling up malaria control in Zambia: progress and impact 2005-2008. Am J Trop Med Hyg. 2010;83:480–8.
Nyarango PM, Gebremeskel T, Mebrahtu G, Mufunda J, Abdulmumini U, Ogbamariam A, et al. A steep decline of malaria morbidity and mortality trends in Eritrea between 2000 and 2004: the effect of combination of control methods. Malaria J. 2006;5:33.
O'Meara WP, Bejon P, Mwangi TW, Okiro EA, Peshu N, Snow RW, et al. Effect of a fall in malaria transmission on morbidity and mortality in Kilifi, Kenya. Lancet. 2008;372:1555–62.
Okiro EA, Hay SI, Gikandi PW, Sharif SK, Noor AM, Peshu N, et al. The decline in paediatric malaria admissions on the coast of Kenya. Malaria J. 2007;6:151.
Okiro EA, Alegana VA, Noor AM, Snow RW. Changing malaria intervention coverage, transmission and hospitalization in Kenya. Malaria J. 2010;9:285.
Okiro EA, Bitira D, Mbabazi G, Mpimbaza A, Alegana VA, Talisuna AO, et al. Increasing malaria hospital admissions in Uganda between 1999 and 2009. BMC Med. 2011;9:37.
Hamel MJ, Adazu K, Obor D, Sewe M, Vulule J, Williamson JM, et al. A reversal in reductions of child mortality in western Kenya, 2003-2009. Am J Trop Med Hyg. 2011;85:597–605.
Agnandji ST, Lell B, Soulanoudjingar SS, Fernandes JF, Abossolo BP, Conzelmann C, et al. First results of phase 3 trial of RTS, S/AS01 malaria vaccine in African children. N Engl J Med. 2011;365:1863–75.
Agnandji ST, Lell B, Fernandes JF, Abossolo BP, Methogo BG, Kabwende AL, et al. A phase 3 trial of RTS, S/AS01 malaria vaccine in African infants. N Engl J Med. 2012;367:2284–95.
Targett G. Randomised controlled trial: phase 3 trial with the RTS, S/AS01 malaria vaccine shows protection against clinical and severe malaria in infants and children in Africa. Evid based Med. 2014. doi:10.1136/ebmed-2014-110089.
World Health Organization. Management of Severe Malaria: A Practical Handbook. 3rd ed. Geneva; 2012.
English M, Punt J, Mwangi I, McHugh K, Marsh K. Clinical overlap between malaria and severe pneumonia in Africa children in hospital. Trans R Soc Trop Med Hyg. 1996;90:658–62.
Berkley JA, Bejon P, Mwangi T, Gwer S, Maitland K, Williams TN, et al. HIV infection, malnutrition, and invasive bacterial infection among children with severe malaria. Clin Infect Dis. 2009;49:336–43.
Koram KA, Molyneux ME. When is "malaria" malaria? The different burdens of malaria infection, malaria disease, and malaria-like illnesses. Am J Trop Med Hyg. 2007;77:1–5.
Bassat Q, Guinovart C, Sigauque B, Mandomando I, Aide P, Sacarlal J, et al. Severe malaria and concomitant bacteraemia in children admitted to a rural Mozambican hospital. Trop Med Int Health. 2009;14:1011–9.
Reyburn H, Mbatia R, Drakeley C, Carneiro I, Mwakasungula E, Mwerinde O, et al. Overdiagnosis of malaria in patients with severe febrile illness in Tanzania: a prospective study. BMJ. 2004;329:1212.
Marsh K, Forster D, Waruiru C, Mwangi I, Winstanley M, Marsh V, et al. Indicators of life-threatening malaria in African children. N Engl J Med. 1995;332:1399–404.
Waller D, Krishna S, Crawley J, Miller K, Nosten F, Chapman D, et al. Clinical features and outcome of severe malaria in Gambian children. Clin Infect Dis. 1995;21:577–87.
Helbok R, Kendjo E, Issifou S, Lackner P, Newton CR, Kombila M, et al. The Lambarene Organ Dysfunction Score (LODS) is a simple clinical predictor of fatal malaria in African children. J Infect Dis. 2009;200:1834–41.
Dondorp AM, Fanello CI, Hendriksen IC, Gomes E, Seni A, Chhaganlal KD, et al. Artesunate versus quinine in the treatment of severe falciparum malaria in African children (AQUAMAT): an open-label, randomised trial. Lancet. 2010;376:1647–57.
von Seidlein L, Olaosebikan R, Hendriksen IC, Lee SJ, Adedoyin OT, Agbenyega T, et al. Predicting the clinical outcome of severe falciparum malaria in African children: findings from a large randomized trial. Clinical Infect Dis. 2012;54:1080–90.
Bejon P, Berkley JA, Mwangi T, Ogada E, Mwangi I, Maitland K, et al. Defining childhood severe falciparum malaria for intervention studies. PLoS Med. 2007;4:e251.
Dondorp A, Nosten F, Stepniewska K, Day N, White N, South East Asian Quinine Artesunate Malaria Trial (SEAQUAMAT) Group. Artesunate versus quinine for treatment of severe falciparum malaria: a randomised trial. Lancet. 2005;366:717–25.
Molyneux ME, Taylor TE, Wirima JJ, Borgstein A. Clinical features and prognostic indicators in paediatric cerebral malaria: a study of 131 comatose Malawian children. Q J Med. 1989;71:441–59.
Newton CR, Chokwe T, Schellenberg JA, Winstanley PA, Forster D, Peshu N, et al. Coma scales for children with severe falciparum malaria. Trand Roy Soc Trop Med Hyg. 1997;91:161–5.
Lewallen S, Harding SP, Ajewole J, Schulenburg WE, Molyneux ME, Marsh K, et al. A review of the spectrum of clinical ocular fundus findings in P. falciparum malaria in African children with a proposed classification and grading system. Trans R Soc Trop Med Hyg. 1999;93:619–22.
Taylor TE, Fu WJ, Carr RA, Whitten RO, Mueller JG, Fosiko NG, et al. Differentiating the pathologies of cerebral malaria by postmortem parasite counts. Nat Med. 2004;10:143–5.
Potchen MJ, Birbeck GL, Demarco JK, Kampondeni SD, Beare N, Molyneux ME, et al. Neuroimaging findings in children with retinopathy-confirmed cerebral malaria. Eur J Radiol. 2010;74:262–8.
Newton CR, Crawley J, Sowumni A, Waruiru C, Mwangi I, English M, et al. Intracranial hypertension in Africans with cerebral malaria. Arch Dis Child. 1997;76:219–26.
Molyneux ME. Malaria-clinical features in children. J Roy Soc Med. 1989;82:35–8.
Birbeck GL, Molyneux ME, Kaplan PW, Seydel KB, Chimalizeni YF, Kawaza K, et al. Blantyre Malaria Project Epilepsy Study (BMPES) of neurological outcomes in retinopathy-positive paediatric cerebral malaria survivors: a prospective cohort study. Lancet Neuro. 2010;9:1173–81.
Crawley J, Smith S, Kirkham F, Muthinji P, Waruiru C, Marsh K. Seizures and status epilepticus in childhood cerebral malaria. QJM. 1996;89:591–7.
Idro R, Gwer S, Kahindi M, Gatakaa H, Kazungu T, Ndiritu M, et al. The incidence, aetiology and outcome of acute seizures in children admitted to a rural Kenyan district hospital. BMC Pediatr. 2008;8:5.
Kariuki SM, Ikumi M, Ojal J, Sadarangani M, Idro R, Olotu A, et al. Acute seizures attributable to falciparum malaria in an endemic area on the Kenyan coast. Brain. 2011;134:1519–28.
Idro R, Otieno G, White S, Kahindi A, Fegan G, Ogutu B, et al. Decorticate, decerebrate and opisthotonic posturing and seizures in Kenyan children with cerebral malaria. Malar J. 2005;4:57.
Brewster DR, Kwiatkowski D, White NJ. Neurological sequelae of cerebral malaria in children. Lancet. 1990;336:1039–43.
Bondi FS. The incidence and outcome of neurological abnormalities in childhood cerebral malaria: a long-term follow-up of 62 survivors. Trans R Soc Trop Med Hyg. 1992;86:17–9.
Sowunmi A, Walker O, Salako LA. Cerebral malaria in non-paediatric subjects resident in southwestern Nigeria. Afr J Med Med Sci. 1993;22:49–53.
Newton CR, Krishna S. Severe falciparum malaria in children: current understanding of pathophysiology and supportive treatment. Pharmacol Ther. 1998;79:1–53.
Carter JA, Mung'ala-Odera V, Neville BG, Murira G, Mturi N, Musumba C, et al. Persistent neurocognitive impairments associated with severe falciparum malaria in Kenyan children. J Neurol Neurosurg Psychiatry. 2005;76:476–81.
Boivin MJ, Bangirana P, Byarugaba J, Opoka RO, Idro R, Jurek AM, et al. Cognitive impairment after cerebral malaria in children: a prospective study. Pediatrics. 2007;119:e360–6.
Idro R, Kakooza-Mwesige A, Balyejjussa S, Mirembe G, Mugasha C, Tugumisirize J, et al. Severe neurological sequelae and behaviour problems after cerebral malaria in Ugandan children. BMC Res Notes. 2010;3:104.
Idro R, Jenkins NE, Newton CR. Pathogenesis, clinical features, and neurological outcome of cerebral malaria. Lancet Neurol. 2005;4:827–40.
Idro R, Carter JA, Fegan G, Neville BG, Newton CR. Risk factors for persisting neurological and cognitive impairments following cerebral malaria. Arch Dis Child. 2006;91:142–8.
de Benoist B, McLean E, Egli I, Cogswell M, editors. Worldwide Prevalence of Anaemia 1993–2005: WHO Global Database on Anaemia. Geneva: World Health Organization; 2008.
Rowe AK, Rowe SY, Snow RW, Korenromp EL, Schellenberg JR, Stein C, et al. The burden of malaria mortality among African children in the year 2000. Int J Epidemiol. 2006;35:691–704.
Mackintosh CL, Beeson JG, Marsh K. Clinical features and pathogenesis of severe malaria. Trends Parasitol. 2004;20:597–603.
Severe malaria. Trop Med Int Health. 2014;19:7–131.
McGregor IA, Gilles HM, Walters JH, Davies AH, Pearson FA. Effects of heavy and repeated malarial infections on Gambian infants and children; effects of erythrocytic parasitization. Br Med J. 1956;2:686–92.
Maitland K, Levin M, English M, Mithwani S, Peshu N, Marsh K, et al. Severe P. falciparum malaria in Kenyan children: evidence for hypovolaemia. QJM. 2003;96:427–34.
English M, Ahmed M, Ngando C, Berkley J, Ross A. Blood transfusion for severe anaemia in children in a Kenyan hospital. Lancet. 2002;359:494–5.
Lackritz EM, Campbell CC, Ruebush 2nd TK, Hightower AW, Wakube W, Steketee RW, et al. Effect of blood transfusion on survival among children in a Kenyan hospital. Lancet. 1992;340:524–8.
Cheema B, Molyneux EM, Emmanuel JC, M'Baya B, Esan M, Kamwendo H, et al. Development and evaluation of a new paediatric blood transfusion protocol for Africa. Transfus Med. 2010;20:140–51.
Meremikwu M, Smith HJ. Blood transfusion for treating malarial anaemia. Cochrane Database Syst Rev. 2000;2, CD001475.
Brabin BJ, Premji Z, Verhoeff F. An analysis of anemia and child mortality. J Nutri. 2001; 131:636S-645S. discussion 646S-648S.
Hendrickse RG, Hasan AH, Olumide LO, Akinkunmi A. Malaria in early childhood. An investigation of five hundred seriously ill children in whom a "clinical" diagnosis of malaria was made on admission to the children's emergency room at University College Hospital, Ibadan. Ann Trop Med Parasitol. 1971;65:1–20.
English M, Waruiru C, Amukoye E, Murphy S, Crawley J, Mwangi I, et al. Deep breathing in children with severe malaria: indicator of metabolic acidosis and poor outcome. Am J Trop Med Hyg. 1996;55:521–4.
Day NP, Phu NH, Mai NT, Chau TT, Loc PP, Chuong LV, et al. The pathophysiologic and prognostic significance of acidosis in severe adult malaria. Crit Care Med. 2000;28:1833–40.
Sasi P, Burns SP, Waruiru C, English M, Hobson CL, King CG, et al. Metabolic acidosis and other determinants of hemoglobin-oxygen dissociation in severe childhood Plasmodium falciparum malaria. Am J Trop Med Hyg. 2007;77:256–60.
Dondorp AM, Chau TT, Phu NH, Mai NT, Loc PP, Chuong LV, et al. Unidentified acids of strong prognostic significance in severe malaria. Crit Care Med. 2004;32:1683–8.
Elusiyan JB, Adejuyigbe EA, Adeodu OO. Hypoglycaemia in a Nigerian paediatric emergency ward. J Trop Pediatr. 2006;52:96–102.
English M, Wale S, Binns G, Mwangi I, Sauerwein H, Marsh K. Hypoglycaemia on and after admission in Kenyan children with severe malaria. QJM. 1998;91:191–7.
Krishna S, Waller DW, ter Kuile F, Kwiatkowski D, Crawley J, Craddock CF, et al. Lactic acidosis and hypoglycaemia in children with severe malaria: pathophysiological and prognostic significance. Trans R Soc Trop Med Hyg. 1994;88:67–73.
Taylor TE, Molyneux ME, Wirima JJ, Fletcher KA, Morris K. Blood glucose levels in Malawian children before and during the administration of intravenous quinine for severe falciparum malaria. N Engl J Med. 1988;319:1040–7.
Holding PA, Stevenson J, Peshu N, Marsh K. Cognitive sequelae of severe malaria with impaired consciousness. Trans R Soc Trop Med Hyg. 1999;93:529–34.
Schellenberg D, Menendez C, Kahigwa E, Font F, Galindo C, Acosta C, et al. African children with malaria in an area of intense Plasmodium falciparum transmission: features on admission to the hospital and risk factors for death. Am J Trop Med Hyg. 1999;61:431–8.
Kawo NG, Msengi AE, Swai AB, Chuwa LM, Alberti KG, McLarty DG. Specificity of hypoglycaemia for cerebral malaria in children. Lancet. 1990;336:454–7.
Roe JK, Pasvol G. New developments in the management of malaria in adults. QJM. 2009;102:685–93.
Phillips RE, Looareesuwan S, Molyneux ME, Hatz C, Warrell DA. Hypoglycaemia and counterregulatory hormone responses in severe falciparum malaria: treatment with Sandostatin. Q J Med. 1993;86:233–40.
Das BS, Satpathy SK, Mohanty D, Mohanty S, Mishra SK, Satapathy PC, et al. Hypoglycaemia in severe falciparum malaria. Trans Roy Soc Trop Med Hyg. 1988;82:197–201.
White NJ, Miller KD, Marsh K, Berry CD, Turner RC, Williamson DH, et al. Hypoglycaemia in African children with severe malaria. Lancet. 1987;1:708–11.
Advanced Life Support Group. Advanced Paediatric Life Support: The Practical Approach. 4th ed. Oxford: Blackwell Publishing Group; 2004.
Willcox ML, Forster M, Dicko MI, Graz B, Mayon-White R, Barennes H. Blood glucose and prognosis in children with presumed severe malaria: is there a threshold for 'hypoglycaemia'? Trop Med Int Health. 2010;15:232–40.
Achoki R, Opiyo N, English M. Mini-review: management of hypoglycaemia in children aged 0-59 months. J Trop Pediatr. 2010;56:227–34.
Ogetii GN, Akech S, Jemutai J, Boga M, Kivaya E, Fegan G, et al. Hypoglycaemia in severe malaria, clinical associations and relationship to quinine dosage. BMC Infect Dis. 2010;10:334.
Trang TT, Phu NH, Vinh H, Hien TT, Cuong BM, Chau TT, et al. Acute renal failure in patients with severe falciparum malaria. Clin Infect Dis. 1992;15:874–80.
Ehrich JH, Eke FU. Malaria-induced renal damage: facts and myths. Pediatr Nephrol. 2007;22:626–37.
Slater MB, Anand V, Uleryk EM, Parshuram CS. A systematic review of RIFLE criteria in children, and its application and association with measures of mortality and morbidity. Kidney Int. 2012;81:791–8.
Maitland K, Kiguli S, Opoka RO, Engoru C, Olupot-Olupot P, Akech SO, et al. Mortality after fluid bolus in African children with severe infection. N Engl J Med. 2011;364:2483–95.
Nguansangiam S, Day NP, Hien TT, Mai NT, Chaisri U, Riganti M, et al. A quantitative ultrastructural study of renal pathology in fatal Plasmodium falciparum malaria. Trop Med Int Health. 2007;12:1037–50.
Severe falciparum malaria. World Health Organization, Communicable Diseases Cluster. Trans R Soc Trop Med Hyg. 2000;94:S1-90.
Patel A, Lodha A, Chaudhuri J, Jadia P, Joshi T, Dalal J. Formulation, process development and evaluation of artemether and lumefantrine soft gelatin capsule. J Phar Bioallied Sciences. 2012;4:S98–S100.
Danis M, Nozais JP, Paris L, Robert C, Katlama C, Gentilini M, et al. Blackwater fever after ingestion of mefloquine. Three cases Presse Med. 1993;22:80.
Orlando G, Isabella L, Atzori C, Cargnel A. Blackwater fever after halofantrine. Lancet. 1996;347:1408–9.
Pasvol G. Management of severe malaria: interventions and controversies. Infect Dis Clin North Am. 2005;19:211–40.
O'Donnell A, Weatherall DJ, Taylor AM, Reeder JC, Allen SJ. Muscle cell injury, haemolysis and dark urine in children with falciparum malaria in Papua New Guinea. Trans R Soc Trop Med Hyg. 2006;100:817–25.
Tran TH, Day NP, Ly VC, Nguyen TH, Pham PL, Nguyen HP, et al. Blackwater fever in southern Vietnam: a prospective descriptive study of 50 cases. Clin Infect Dis. 1996;23:1274–81.
Bodi JM, Nsibu CN, Longenge RL, Aloni MN, Akilimali PZ, Tshibassu PM, et al. Blackwater fever in Congolese children: a report of clinical, laboratory features and risk factors. Malar J. 2013;12:205.
Ahmed I, Olowe O. Haemoglobinuria in Nigerian children. Afr J Med Sci. 1971;2:101–8.
Ajetunmobi WA, Orimadegun AE, Brown BJ, Afolabi NK, Olabiyi FA, Anetor JI, et al. Haemoglobinuria among children with severe malaria attending tertiary care in Ibadan. Nigeria Malar J. 2012;11:336.
Howes RE, Dewi M, Piel FB, Monteiro WM, Battle KE, Messina JP, et al. Spatial distribution of G6PD deficiency variants across malaria-endemic regions. Malar J. 2013;12:418.
Zoller T, Junghanss T, Kapaun A, Gjorup I, Richter J, Hugo-Persson M, et al. Intravenous artesunate for severe malaria in travelers, Europe. Emerg Infect Dis. 2011;17:771–7.
Kreeftmeijer-Vegter AR, van Genderen PJ, Visser LG, Bierman WF, Clerinx J, van Veldhuizen CK, et al. Treatment outcome of intravenous artesunate in patients with severe malaria in the Netherlands and Belgium. Malar J. 2012;11:102.
Experts Group Meeting on delayed haemolytic anaemia following treatment with injectable artesunate. Vienna, Austria; 2013. Medicines for Malaria Venture (MMV); Geneva.
Jaureguiberry S, Ndour PA, Roussel C, Ader F, Safeukui I, Nguyen M, et al. Postartesunate delayed hemolysis is a predictable event related to the lifesaving effect of artemisinins. Blood. 2014;124:167–75.
Nadjm B, Amos B, Mtove G, Ostermann J, Chonya S, Wangai H, et al. WHO guidelines for antimicrobial treatment in children admitted to hospital in an area of intense Plasmodium falciparum transmission: prospective study. BMJ. 2010;340:c1350.
Scott JA, Berkley JA, Mwangi I, Ochola L, Uyoga S, Macharia A, et al. Relation between falciparum malaria and bacteraemia in Kenyan children: a population-based, case-control study and a longitudinal study. Lancet. 2011;378:1316–23.
Church J, Maitland K. Invasive bacterial co-infection in African children with Plasmodium falciparum malaria: a systematic review. BMC Med. 2014;12:31.
Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med. 2013;41:580–637.
Hien TT, Davis TM, Chuong LV, Ilett KF, Sinh DX, Phu NH, et al. Comparative pharmacokinetics of intramuscular artesunate and artemether in patients with severe falciparum malaria. Antimicrobial Agents Chemotherapy. 2004;48:4234–9.
Nealon C, Dzeing A, Muller-Romer U, Planche T, Sinou V, Kombila M, et al. Intramuscular bioavailability and clinical efficacy of artesunate in gabonese children with severe malaria. Antimicrob Agents Chemother. 2002;46:3933–9.
Phu NH, Hien TT, Mai NT, Chau TT, Chuong LV, Loc PP, et al. Hemofiltration and peritoneal dialysis in infection-associated acute renal failure in Vietnam. N Engl J Med. 2002;347:895–902.
Pocock SJ, Hughes MD. Practical problems in interim analyses, with particular regard to estimation. Controlled Clin Trials. 1989;10:209S–21S.
Warrell DA, Looareesuwan S, Warrell MJ, Kasemsarn P, Intaraprasert R, Bunnag D, et al. Dexamethasone proves deleterious in cerebral malaria. A double-blind trial in 100 comatose patients. N Engl J Med. 1982;306:313–9.
Hoffman SL, Rustama D, Punjabi NH, Surampaet B, Sanjaya B, Dimpudus AJ, et al. High-dose dexamethasone in quinine-treated patients with cerebral malaria: a double-blind, placebo-controlled trial. J Infect Dis. 1988;158:325–31.
Prasad K, Garner P. Steroids for treating cerebral malaria. Cochrane Database Syst Rev. 2000;2, CD000972.
Di Perri G, Di Perri IG, Monteiro GB, Bonora S, Hennig C, Cassatella M, et al. Pentoxifylline as a supportive agent in the treatment of cerebral malaria in children. J Infect Dis. 1995;171:1317–22.
Looareesuwan S, Wilairatana P, Vannaphan S, Wanaratana V, Wenisch C, Aikawa M, et al. Pentoxifylline as an ancillary treatment for severe falciparum malaria in Thailand. Am J Trop Med Hyg. 1998;58:348–53.
Hemmer CJ, Kern P, Holst FG, Nawroth PP, Dietrich M: Neither heparin nor acetylsalicylic acid influence the clinical course in human Plasmodium falciparum malaria: a prospective randomized study. Am J Trop Med Hyg 1991;45:608-612.
Das BK, Mishra S, Padhi PK, Manish R, Tripathy R, Sahoo PK, et al. Pentoxifylline adjunct improves prognosis of human cerebral malaria in adults. Trop Med Int Health. 2003;8:680–4.
Lell B, Kohler C, Wamola B, Olola CH, Kivaya E, Kokwaro G, et al. Pentoxifylline as an adjunct therapy in children with cerebral malaria. Malar J. 2010;9:368.
van Hensbroek MB, Palmer A, Onyiorah E, Schneider G, Jaffar S, Dolan G, et al. The effect of a monoclonal antibody to tumor necrosis factor on survival from childhood cerebral malaria. J Infect Dis. 1996;174:1091–7.
Taylor TE, Molyneux ME, Wirima JJ, Borgstein A, Goldring JD, Hommel M. Intravenous immunoglobulin in the treatment of paediatric cerebral malaria. Clin Exper Immunol. 1992;90:357–62.
Looareesuwan S, Sjostrom L, Krudsood S, Wilairatana P, Porter RS, Hills F, et al. Polyclonal anti-tumor necrosis factor-alpha Fab used as an ancillary treatment for severe malaria. Am J Trop Med Hyg. 1999;61:26–33.
Dondorp AM, Silamut K, Charunwatthana P, Chuasuwanchai S, Ruangveerayut R, Krintratun S, et al. Levamisole inhibits sequestration of infected red blood cells in patients with falciparum malaria. J Infect Dis. 2007;196:460–6.
Maude RJ, Silamut K, Plewes K, Charunwatthana P, Ho M, Abul Faiz M, et al. Randomized controlled trial of levamisole hydrochloride as adjunctive therapy in severe falciparum malaria with high parasitemia. J Infect Dis. 2013;209:120–9.
White NJ, Looareesuwan S, Phillips RE, Chanthavanich P, Warrell DA. Single dose phenobarbitone prevents convulsions in cerebral malaria. Lancet. 1988;2:64–6.
Crawley J, Waruiru C, Mithwani S, Mwangi I, Watkins W, Ouma D, et al. Effect of phenobarbital on seizure frequency and mortality in childhood cerebral malaria: a randomised, controlled intervention study. Lancet. 2000;355:701–6.
Gwer SA, Idro RI, Fegan G, Chengo EM, Mpoya A, Kivaya E, et al. Fosphenytoin for seizure prevention in childhood coma in Africa: a randomized clinical trial. J Crit Care. 2013;28:1086–92.
Kochar Shubhakaran DL, Kumawat BL, Kochar SK. Seizures in cerebral malaria. QJM. 1997;90:605–7.
Kingston ME. Experience with urea in invert sugar for the treatment of cerebral malaria. J Trop Med Hyg. 1971;74:249–52.
Namutangula B, Ndeezi G, Byarugaba JS, Tumwine JK. Mannitol as adjunct therapy for childhood cerebral malaria in Uganda: a randomized clinical trial. Malar J. 2007;6:138.
Mohanty S, Mishra SK, Patnaik R, Dutt AK, Pradhan S, Das B, et al. Brain swelling and mannitol therapy in adult cerebral malaria: a randomized trial. Clin Infect Dis. 2011;53:349–55.
Smith HJ, Meremikwu M. Iron chelating agents for treating malaria. Cochrane Database Syst Rev. 2000;2, CD001474.
Gordeuk V, Thuma P, Brittenham G, McLaren C, Parry D, Backenstose A, et al. Effect of iron chelation therapy on recovery from deep coma in children with cerebral malaria. N Engl J Med. 1992;327:1473–7.
Thuma PE, Mabeza GF, Biemba G, Bhat GJ, McLaren CE, Moyo VM, et al. Effect of iron chelation therapy on mortality in Zambian children with cerebral malaria. Trans R Soc Trop Med Hyg. 1998;92:214–8.
Mohanty D, Ghosh K, Pathare AV, Karnad D. Deferiprone (L1) as an adjuvant therapy for Plasmodium falciparum malaria. Indian J Med Res. 2002;115:17–21.
Gruarin P, Primo L, Ferrandi C, Bussolino F, Tandon NN, Arese P, et al. Cytoadherence of Plasmodium falciparum-infected erythrocytes is mediated by a redox-dependent conformational fraction of CD36. J Immunol. 2001;167:6510–7.
Watt G, Jongsakul K, Ruangvirayuth R. A pilot study of N-acetylcysteine as adjunctive therapy for severe malaria. QJM. 2002;95:285–90.
Treeprasertsuk S, Krudsood S, Tosukhowong T, Maek AN, Vannaphan S, Saengnetswang T, et al. N-acetylcysteine in severe falciparum malaria in Thailand. Southeast Asian J Trop Med Public Health. 2003;34:37–42.
Charunwatthana P, Abul Faiz M, Ruangveerayut R, Maude RJ, Rahman MR, Roberts 2nd LJ, et al. N-acetylcysteine as adjunctive treatment in severe malaria: a randomized, double-blinded placebo-controlled clinical trial. Crit Care Med. 2009;37:516–22.
Yeo TW, Lampah DA, Rooslamiati I, Gitawati R, Tjitra E, Kenangalem E, et al. A randomized pilot study of L-arginine infusion in severe falciparum malaria: preliminary safety, efficacy and pharmacokinetics. PloS One. 2013;8:e69587.
Day NP, Phu NH, Mai NT, Bethell DB, Chau TT, Loc PP, et al. Effects of dopamine and epinephrine infusions on renal hemodynamics in severe malaria and severe sepsis. Crit Care Med. 2000;28:1353–62.
English M, Sauerwein R, Waruiru C, Mosobo M, Obiero J, Lowe B, et al. Acidosis in severe childhood malaria. QJM. 1997;90:263–70.
Maitland K, Newton CR. Acidosis of severe falciparum malaria: heading for a shock? Trends Parasitol. 2005;21:11–6.
Planche T. Malaria and fluids-‐balancing acts. Trends Parasitol. 2005;21:562–7.
Maitland K, Pamba A, Newton CR, Levin M. Response to volume resuscitation in children with severe malaria. Pediatr Crit Care Med. 2003;4:426–31.
Yacoub S, Lang HJ, Shebbe M, Timbwa M, Ohuma E, Tulloh R, et al. Cardiac function and hemodynamics in Kenyan children with severe malaria. Critical Care Med. 2010;38:940–5.
Maitland K, Pamba A, English M, Peshu N, Marsh K, Newton C, et al. Randomized trial of volume expansion with albumin or saline in children with severe malaria: preliminary evidence of albumin benefit. Clin Infect Dis. 2005;40:538–45.
Maitland K, Pamba A, English M, Peshu N, Levin M, Marsh K, et al. Pre-transfusion management of children with severe malarial anaemia: a randomised controlled trial of intravascular volume expansion. Brit J Haematol. 2005;128:393–400.
Akech S, Gwer S, Idro R, Fegan G, Eziefula AC, Newton CR, et al. Volume expansion with albumin compared to gelofusine in children with severe malaria: results of a controlled trial. PLoS Clin Trials. 2006;1:e21.
Akech SO, Jemutai J, Timbwa M, Kivaya E, Boga M, Fegan G, et al. Phase II trial on the use of Dextran 70 or starch for supportive therapy in Kenyan children with severe malaria. Crit Care Med. 2010;38:1630–6.
Akech S, Ledermann H, Maitland K. Choice of fluids for resuscitation in children with severe infection and shock: systematic review. BMJ. 2010;341:c4416.
Maitland K, George EC, Evans JA, Kiguli S, Olupot-Olupot P, Akech SO, et al. Exploring mechanisms of excess mortality with early fluid resuscitation: insights from the FEAST trial. BMC Med. 2013;11:68.
Kiguli S, Akech SO, Mtove G, Opoka RO, Engoru C, Olupot-Olupot P, et al. WHO guidelines on fluid resuscitation in children: missing the FEAST data. BMJ. 2014;348:f7003.
Ford N, Hargreaves S, Shanks L. Mortality after fluid bolus in children with shock due to sepsis or severe infection: a systematic review and meta-analysis. PloS One. 2012;7:e43953.
Dellinger RP, Levy MM, Carlet JM, Bion J, Parker MM, Jaeschke R, et al. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock: 2008. Intensive Care Med. 2008;34:17–60.
Holzer BR, Egger M, Teuscher T, Koch S, Mboya DM, Smith GD. Childhood anemia in Africa: to transfuse or not transfuse? Acta Trop. 1993;55:47–51.
Bojang KA, Palmer A, Boele van Hensbroek M, Banya WA, Greenwood BM. Management of severe malarial anaemia in Gambian children. Trans Roy Soc Trop Med Hyg. 1997;91:557–61.
Olupot Olupot P, Engoru C, Thompson J, Nteziyaremye J, Chebet M, Ssenyondo T, et al. Phase II trial of standard versus increased transfusion volume in Ugandan children with acute severe anemia. BMC Med. 2014;12:67.
Leitgeb AM, Blomqvist K, Cho Ngwa F, Samje M, Nde P, Titanji V, et al. Low anticoagulant heparin disrupts Plasmodium falciparum rosettes in fresh clinical isolates. Am J Trop Med Hyg. 2011;84:390–6.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The author declares that she has no competing interests.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Maitland, K. Management of severe paediatric malaria in resource-limited settings. BMC Med 13, 42 (2015). https://doi.org/10.1186/s12916-014-0263-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12916-014-0263-6