Abstract
Background
Priority-setting becomes more difficult for decision-makers when the demand for health services and health care resources rises. Despite the fact that the Ethiopian healthcare system places a strong focus on the efficient utilization and allocation of health care resources, studies of efficiency in healthcare facilities have been very limited. Hence, the study aimed to evaluate efficiency and its determinants in public health centers.
Methods
A cross-sectional study was conducted in the East Wollega zone, Oromia Regional State, Ethiopia. Ethiopian fiscal year of 2021–2022 data was collected from August 01–30, 2022 and 34 health centers (decision-making units) were included in the analysis. Data envelope analysis was used to analyze the technical efficiency. A Tobit regression model was used to identify determinants of efficiency, declaring the statistical significance level at P < 0.05, using 95% confidence interval.
Results
The overall efficiency score was estimated to be 0.47 (95% CI = 0.36–0.57). Out of 34 health centers, only 3 (8.82%) of them were technically efficient, with an efficiency score of 1 and 31 (91.2%) were scale-inefficient, with an average score of 0.54. A majority, 30 (88.2%) of inefficient health centers exhibited increasing return scales. The technical efficiency of urban health centers was (β = -0.35, 95% CI: -0.54, -0.07) and affected health centers’ catchment areas by armed conflicts declined (β = -0.21, 95% CI: -0.39, -0.03) by 35% and 21%, respectively. Providing in-service training for healthcare providers increased the efficiency by 27%; 95% CI, β = 0.27(0.05–0.49).
Conclusions
Only one out of ten health centers was technically efficient, indicating that nine out of ten were scale-inefficient and utilized nearly half of the healthcare resources inefficiently, despite the fact that they could potentially reduce their inputs nearly by half while still maintaining the same level of outputs. The location of health centers and armed conflict incidents significantly declined the efficiency scores, whereas in-service training improved the efficiency. Therefore, the government and health sector should work on the efficient utilization of healthcare resources, resolving armed conflicts, organizing training opportunities, and taking into account the locations of the healthcare facilities during resource allocation.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
The physical relationship between resources used (inputs) and outputs is referred to as technical efficiency (TE). A technically efficient position is reached when a set of inputs yields the maximum improvement in outputs [1]. Therefore, as it serves as a tool to achieve better health, health care can be viewed as an intermediate good, and efficiency is the study of the relationship between final health outcomes (lifes saved, life years gained, or quality-adjusted life years) and resource inputs (costs in the form of labor, capital, or equipment) [2].
Efficiency is a quality of performance that is evaluated by comparing the financial worth of the inputs, the resources utilized to produce a certain output and the output itself, which is a component of the health care system. Either maximizing output for a given set of inputs or minimising inputs required to produce a given output would make a primary health care (PHC) facility efficient. Technical efficiency is the minimum amount of resources required to produce a given output. Wastage or inefficiencies occur when resources are used more than is required to produce a given level of output [3].
According to the WHO, in order to make progress towards universal health coverage (UHC), more funding for healthcare is required as well as greater value for that funding. According to the 2010 Report, 20–40% of all resources used for health care are wasted [4]. In most countries, a sizable share of total spending goes into the health sector. Therefore, decision-makers and health administrators should place a high priority on improving the efficiency of health systems [5].
Efficient utilization of healthcare resources has a significant impact on the delivery of health services. It leads to better access to health services and improves their quality by optimizing the use of resources. Healthcare systems can reduce wait times, increase the number of patients served, and enhance the overall patient experience. When resources are used efficiently, it can result in cost savings for healthcare systems, which allows for the reallocation of funds to other areas in need, potentially expanding services or investing in new technologies [6].
Also, efficient use of healthcare resources can contribute to better health outcomes. For example, proper management of medical supplies can ensure that patients receive the necessary treatments without delay, leading to improved recovery rates, and it is key to the sustainability of health services by ensuring that healthcare systems can continue to provide care without exhausting financial or material resources [6, 7].
Furthermore, proper resource allocation can help to reduce disparities in healthcare delivery by ensuring that resources are distributed based on need so that healthcare systems can work towards providing equitable care to all populations. Efficient resource utilization contributes to the resilience of health systems, enabling them to respond effectively to emergencies, such as pandemics or natural disasters, without compromising the quality of care [8].
One of the quality dimensions emphasized in strategegy of Ethiopian health sector transformation plan (HSTP) is the theme around excellence in quality improvement and assurance, which is a component of Ethiopia's National Health Financing Strategy (2015–2035), has been providing healthcare in a way that optimizes resource utilization and minimizes wastage [9]. The majority of efficiency evaluations of Ethiopia's health system have been conducted on a worldwide scale, evaluating various nations' relative levels of efficiency.
Spending on public health nearly doubled between 1995 and 2011. One of the fastest-growing economies, the gross domestic product (GDP) increased by 9% real on average between 1999 and 2012 [5]. As a result, the whole government budget was able to triple within the same time period (at constant 2010 prices), which resulted in additional funding for health [10].
External resources also rose from 1995 to 2011 from US$6 million to US$836 million (in constant 2012 dollar) [11]. The development of the health sector, particularly primary care, was dependent on this ongoing external financing, with external funding accounting for half of primary care spending in 2011 [12]. Over the past 20 years, Ethiopia's health system has experienced exceptional growth, especially at the primary care level. Prior to 2005, hospitals and urban areas received a disproportionate share of public health spending [13].
It is becoming more and more necessary for decision-makers to manage the demand for healthcare services and the available resources while striking a balance with competing goals from other sectors. As PHC enters a new transformative phase, beginning with the Health Sector Transformation Plan (HSTP), plans call for increased resource utilization efficiency. Over the course of the subsequent five years (2015/2016–2019/2020), Ethiopia planned to achieve UHC by strengthening the implementation of the nutrition programme and expanding PHC coverage to everyone through improved access to basic curative and preventative health care services [9, 14].
Increasing efficiency in the health sector is one way to create financial space for health, and this might potentially free up even more resources to be used for delivering high-quality healthcare [15]. While there was a considerable emphasis on more efficient resource allocation and utilization during the Health Care and Financing Strategy (1998–2015) in Ethiopia, problems with health institutions' efficient utilization of resources persisted during this time [10]. Ethiopia is one of the least efficient countries in health system in the world which was ranked 169th out of 191 countries [16].
Although maximising health care outputs requires evaluating the technical efficiency of health facilities in providing medical care, there is the lack of studies of this kind carried out across this country. Although the primary focus of health care reforms in Ethiopia is the efficient allocation and utilization of resources within the health system, there is a lack of studies on the efficiency of the country's primary health care system that could identify contributing factors, including incidents of armed conflict within the catchment population of the healthcare facilities, that may impact the efficiency level of these health care facilities. As a result, in the current study, the factors that might have an impact on the technical efficiency of the health centers were categorized into three categories: factors related to the environment, factors related to the health care facilities, and factors related to the health care providers (Fig. 1).
In addition, the annual report of the East Wollega zonal health department for the Ethiopian fiscal year (EFY) 2021 and 2022 indicated that the performance of the health care facilities in the zone was low compared to other administrative zones of the region, Oromia Regional State. Therefore, this study aimed to evaluate technical efficiency and its determinants in the public health centers in East Wollega Zones, Oromia Regional State, Ethiopia.
Methods and materials
Study settings and design
The study was carried out in public health care facilities, health centers found in East Wollega Zone, Oromia regional state, Ethiopia. The zone's capital city, Nekemte, is located around 330 kms from Addis Ababa, the capital of the country. The East Wollega Zone is located in the western part of the country, Ethiopia. Data for the EFY of July 2021 to June 2022 was retrospectively collected from August 1–30, 2022.
Data envelope analysis conceptual framework
A two-stage data envelope analysis (DEA) was employed in the current study. The two widely used DEA models, Banker, Charnes, and Cooper (BCC) and Charnes, Cooper, and Rhodes (CCR), were used to determine the technical efficiency (TE), pure technical efficiency (PTE), and scale efficiency (SE) scores for individual health centers which were considered as decision-making units (DMUs) in the first stage of the methodological framework. The overall technical efficiency (OTE) for the DMUs was determined using the CCR model, which assumed constant returns-to-scale (CRS), strong disposability of inputs and outputs, and convexity of the production possibility set. This efficiency value ranges from 0 to 1. Since the aim was to use the least amount of inputs with the same level of production in health centers, it is important to note that the model used input–output oriented approach. In general, this model evaluated the health centers' capabilities to produce a particular quantity of output with the least amount of inputs or, alternatively, the highest level of output that can be produced with the same amount of input. Overall, this model measured the ability of the health centers to produce a given level of output using the minimum amount of input, or alternatively, the maximum amount of output using a given amount of input, using the following formula: yrj: amount of output r from health centre j, xij : amount of input i to health centre j, ur: weight given to output; r, vi: weight given to input. i, n: number of health centers; s: number of outputs; m: number of inputs [17, 18].
\(Max\;ho\;=\;\frac{\sum_{r=1}^suryijo}{\sum_{v=1}^mvixijo}\) |
|---|
\(Subject\ to;\) |
\(\frac{\sum_{r=1}^suryijo}{\sum_{v=1}^mvixijo}\;\leq1,j\;=\;1,\;\cdots\;jo,\;\cdots\;n,\) |
\(ur\;\geq\;0\;r\;=\;1,\;\cdots\;,s\;and\;vi\;\geq0,\;i\;=\;1\;\cdots m\) |
\(Max\;ho\;=\;\sum_{r=1}^s\text{uryrjo}.\) |
\(Subject\ to;\) |
\(Max\;ho=\sum_{r=1}^s\text{uryrjo}=1\) |
\(Max\;ho\;=\;\sum_{r=1}^suryr-\sum_{r=1}^svixij\leq\;0,\;j\;=\;1\cdots,\;n\) |
\(ur,\;vi\;\geq\;0\) |
Constant returns to scale (CRS) were measured using the CCR model. The CCR model measuresd the health centre's ability to produce the expected amount of output from a given amount of input using the formula;
\(Max\;ho\;=\;\sum_{r=1}^s\text{uryrjo}.\) |
|---|
\(Subject\;to;\) |
\(Max\;ho\;=\;\sum_{r=1}^s\text{uryrjo}=1\) |
\(Max\;ho\sum_{r=1}^suryr-\sum_{r=1}^svixij\;\leq\;0,\;j=\;1\dots,\;n\) |
\(ur,\;vi\;\geq\;0\) |
The BCC model was used to measure the variable returns to scale (VRS). When there are variations in output production levels and a proportionate increase in all inputs, this model works well for evaluating the PTE of health centers. The equation in use is:
\(Max\;ho\;=\sum_{r=1}^suryr+zjo\) |
|---|
\(Subject\;to;\) |
\(Max\;ho\;=\;\sum_{r=1}^suryr+zjo=1\) |
\(Max\;ho\;=\;\sum_{1=r}^suryr-\sum_{r=1}^svixij+zjo\leq0,\;j\;=\;1,\cdots n\) |
\(ur,\;vi\;\geq\;0\) |
In the methodological framework of the second stage, the OTE scores estimated from the first stage was regeressed using a Tobit regression model. This was to identify determinants of the technical efficiency scores of the primary health care facilities, which included factors related to health centers, health care providers, and the environment. The coefficients (β) of the independent factors indicated their direction of influence on the dependent variable, which was the OTE score. The model used has been expressed below [19].
\(Yi\ast=\;{\mathrm\beta}_0+\mathrm\beta x_i+{\mathrm\varepsilon}_{\mathrm i},\;\mathrm i=1,\;2,\;\dots\mathrm n\) |
|---|
\(Yi\ast\;=\;0,\;if\;yi\;\leq\;0,\) |
\(Yi\ast\;=\;Yi,\;if\;0\;<\;Yi\ast\;=\;1,\;if\;yi\;\geq\;1,\) |
Where γi* is the limited dependent variable, which represented the technical efficiency score, γi is the observed dependent (censored) variable, xi is the vector of independent variables (factors related to health centers, health care providers, and the environment). β0 represented intercept (constant) whereas β1, β2 and β3 were the parameters of the independent variables (coefficients), εi was a disturbance term assumed to be independently and normally distributed with zero mean and constant variance σ; and i = 1, 2,…n, (n is the number of observations, n = 34 health centers).
Study variables
Input variables
The input variables comprised financial resources (salary and incentives) and human resources (number of administrative staffs, clinical and midwife nurses, laboratory technicians and technologists, pharmacy technicians and pharmacists, public health officers, general physicians, and other health care professionals, as well as other non-clinical staffs).
Output variables
Output variables comprised the number of women who had 4 visits of antenatal care (4ANC), number of deliveries, number of mothers who received postnatal care (PNC), number of women who had family planning visits, number of children who received full immunization, number of children aged 6–59 months who received vitamin A supplements, number of clients counseled and tested for human immunodeficiency virus (HIV), number of HIV patients who had follow-up care, number of patients diagnosed for TB, number of TB patients who had follow-up care and complete their treatment, number of outpatients who visited the health facilities for other general health services.
Depedent variable
Overall technical efficiency scores of the health centers.
Independent variables
The explanatory variables used in the Tobit regression model were the location of the health centers, accessibility of the health centers to transportation services, support from non-governmental organisations (NGOs), armed conflict incidents in the catchment areas, adequate electricity and water supply, in-service health care provider training, availability of diagnostic services (laboratory services), availability of adequate drug supply, room arrangements for proximity between related services, and marking the rooms with the number and type of services they provide.
Study health facilities
Public health centers in the districts of the East Wollega Zone were the study facilities. In the context of the Ethiopian health care system, a health center is a health facility within the primary health care system that provides promotive, preventive, curative, and rehabilitative outpatient care, including basic laboratory and pharmacy services. This health facility typically has a capacity of 10 beds for emergency and delivery services. Health centers serve as referral centers for health posts and provide supportive supervision for health extension workers (HEWs). It is expected that one health center provides services to a population of 15,000–25,000 within its designated catchment area. There were 17 districts and 67 public health centers in the zone. Nine districts (50%) and thirty-four health centers (50%) were included in the analysis.
Data collection instrument and technique
Data collection was conducted using the document review checklist, which was developed after the review of the Ethiopian standard related to the requirements for health care facilities. Data for the EFY of July 2021 to June 2022 was retrospectively collected. The contents of the document review checklist (data collection instrument) included inputs, outputs, and factors related to health centers, the environment, and health care providers.
Data analysis
Initially, STATA 14 was used to compute descriptive statistics for each input and output variable. For each input and output variable, the mean, standard deviation (SD), minimum and maximum values were presented. Next, MaxDEA7 (http://maxdea.com) was used to compute the technical efficiency, pure technical efficiency, scale efficiency scores, and input reduction and/or output increases.
The efficiency of the health centers below the efficiency frontier was measured in terms of their distance from the frontier. If the technical efficiency (TE) score closes to 0, it indicates that the health center is technically inefficient because its production lies below the stochastic frontier. The higher the value of the TE score, the closer the unit’s performance is to the frontier. The TE scores typically fall within the range of 0 to 1. A score of 0 usually indicates that the health care facilities (DMUs) were completely inefficient in health service delivery, whereas a score of 1 suggests that the health care facilities operated at maximum efficiency in health service delivery. In this case, the efficiency scores between these two extremes represent varying levels of the health center's performance in health service delivery. As the TE score moves from 0 to 1, it reflects the health centers’ progress toward optimal resource utilization and efficient performance of the health care facilities in health service delivery [20]. In comparison to their counterparts, health centers that implemented the best practice frontier were considered technically efficient, with an efficiency score of 1; (100% efficient), and the health centers were said to be efficient if they utilized their resources optimally, and there was no scope for increasing the outputs without increasing the amount of inputs used. The higher the score, the more efficient a health center is. Those health centers with a TE score estimated to be 1 were considered efficient, whereas those with a TE score of < 1 were considered inefficient. This means that the health centers did not utilize their resources efficiently, resulting in wastage of resources and suboptimal outputs.
In the second stage, the estimated overall technical efficiency scores obtained from the DEA were considered as the dependent variable and regressed against the set of independent variables (Fig. 1) namely healthcare facility-related, healthcare provider-related and environment-related factors. Finally, the statistical significance level was declared at P < 0.05 using the 95% confidence interval (CI).
Results
Inputs used and outputs produced
A total of 34 DMUs were included in the study, and from these DMUs, input and output data were collected based on the data from July 1, 2021, to June 30, 2022 of one EFY. For the purpose of analysis, the input variables were categorized into financial resources and human resources, while maternal and child health (MCH), delivery, and general outpatient service were considered as output variables (Table 1).
Efficiency of the health centers
Efficient decision units in the DEA efficiency analysis model were defined relative to less efficient units, not absolute. The DMUs in our case were health centers. The estimating technique evaluated an individual health center’s efficiency by comparing its performance with a group of other efficient health centers. A health center’s efficiency reference set was the efficient health center that was used to evaluate the other health centers. The reasons behind the classification of an inefficient health centers as inefficient units were demonstrated by the efficient reference set's performance across the evaluation dimensions (Table 2).
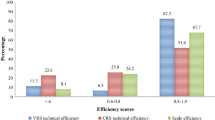
Out of 34 health centers, only 3(8.82%) of them were technically efficient, and almost all 31(91.18%) were inefficient. On average, the OTE of the all 34 health centers was estimated to be 0.47, 95% CI = (0.36, 0.57). The OTE scores of the health centers varied greatly, from the lowest of 0.0003 to the highest of 1, implying that most of the health centers were using more resources to produce output than what other health centers with comparable resource levels were producing.
Scale-inefficient health centers had efficiency scores ranging from 0.0004 to 0.99. Thirty-one (91.2%) scale-inefficient health centers had an average score of 0.54; indicating that these health centers might, on average reduce 46% of their resources while maintaining the same amount of outputs. With a scale efficiency of 100%, three of the healthcare facilities (8.82%) had the highest efficiency score for their particular input–output mix.
Regarding PTE scores, 8(23.53%) of the health centers were efficient, and the average score was 0.77 ± 0.18. The return scales (RTS) of 1(2.94%), 3(8.82%), and 31(88.22%) health centers were decreasing return scales (DRS), constant return scales (CRS), and increasing return scales (IRS), respectively.
Determinants of overall technical efficiency
In this study, the Tobit regression model was used to identify the determinants of the technical efficiency of the health centers. As a dependent variable, the health facility's technical efficiency score was calculated from the DEA; Tobit regression was subsequently carried out (Table 3).
The location of the health centers, armed conflict incidents in the catchment areas of the health centers, and in-service training of the healthcare providers working in healthcare facicilities significantly influenced the technical efficiency scores of the health centers. Accordingly, the OTE of those health centers that were found in urban areas of the districts declined by 35%, 95% CI, β = -0.35(-0.54, -0.07) compared to the health centers found in rural areas of the districts. Similarly, the OTE of the health centers with catchment areas faced armed conflict incidents declined by 21%, 95% CI, β = -0.21 (-0.39, -0.03) compared to those health centers’ catchment areas that did not face the problem.
However, the in-service training of the health care providers who were working in the study healthcare facilities significantly improved the technical efficiency scores of the health centers. As a result, the OTE of the health centers in which their health care providers received adequate in-service training increased by 27%, 95% CI, β = 0.27 (0.05, 0.49).
Discussion
The current study evaluated the technical efficiency of the health centers and identified the determinants of their efficiency. As a result, only one health center out of every 10 health centers operated efficiently, meaning that about 90% of health centers were inefficient. The average PTE score was 77%, which purely reflected the health centers’ managerial performance to organize inputs. This indicated that the health centers exhibited a 33% failure of managerial performance to organize the available health care resources. The ratio of OTE to PTE or CRS to VRS provided the SE scores. Accordingly, the majority of the DMUs, 88.22%, exhibited IRS that could expand their scale of efficiency without additional inputs, whereas only about 2% exhibited DRS that should scale down its scale of operation in order to operate at the most productive scale size (MPSS). Incontrst to this, the study conducted in China showed that more than half of the health care facilities operated at a DRS meaning that again in efficiency could be achieved only through downsizing the scale of operation in nearly 60% of the provinces [21].
In the study, the technical inefficiency of the health centers was significantly higher than the technical inefficiency findings of the study conducted in Sub-Saharan Africa countries (SSA): 65% of public health centers in Ghana [22], 59% in Pujehun district of Sierra Leone [23], 56% of public health centers in Kenya [24], and 50% of public health centers in Jimma Zone of Ethiopia [25] were technically inefficient. Similary, the systematic review study conducted in SSA showed that less than 40% of the studied health facilities were technically efficient in SSA countries [26]. These substantial discrepancies could be due to the armed conflict incidents in the catchment areas of the study health centers. This is supported by evidence that almost half of catchment areas of the studiy health centers experienced such conflicts.
The efficiency scores of the health centers varied significantly, from the lowest of 0.0003 to the highest of 1, indicating that some health centers were using more resources to produce output than other health centers with comparable amounts of resources. While only about one out of ten health centers had a scale efficiency of 100%, indicating that they had the most productive size for the particular input–output mix, in contrast to this, nine out of ten health centers were technically inefficient with 54% scale efficiency, implying they might reduce their healthcare resources almost by half while maintaining the same quantity of outputs (health services). This efficiency score was lower when compared to the efficiency score of health care facilities in Afghanstan, which showed the average efficiency score of health facilities was 0.74, when only 8.1% of the health care facilities had efficiency scores of 1(100% efficient) [27].
In the present study, the inefficiency level of health care facilities was high, which may have had an impact on the delivery of health care services. Different studies showed that the delivery of healthcare services is greatly impacted by the efficient use of healthcare resources [6,7,8]. and despite the scarcity of health care resources in the health sector, in most low- and middle-income countries (LMICs), the inefficiency of the sector persists [28].
Once more, the study identified determinants of the technical efficiency of the health centers. As a result, the efficiency score of those health centers that were located in the urban areas of the study districts declined by one-third. This finding in lines with the study conducted in SSA countries, showed that the location of health care facilities is significantly associated with the technical efficiency of the facilities [26]. Similarly, the study conducted in Europe showed that, despite performing similarly in the efficiency dimensions, a number of rural healthcare care facilities were found to be the best performers compared to urban health facilities [29]. Also, the study conducted in China revealed that the average technical efficiency of urban primary healthcare institutions fluctuated from 63.3% to 67.1%, which was lower than that of rural facilities (75.8–82.2%) from 2009 to 2019 [30].
The availability of different public and private health facilities in urban areas, such as public hospitals and private clinics, might contribute to the fact that rural health centers were significantly more efficient compared to those health centers found in the urban areas of the study districts. Patients might opt for these health facilities rather than public health centers in urban areas. In contrast to this, in rural areas, such options were not available. Again, these health facilities, the public and private health facilities might share the same catchment areas in urban areas, which could impact their health care utilization, resulting in under-utilization and lower outputs (the number of patients and clients who utilized the health services from the health facilities).
Similarly, the armed conflict incidents in the catchment areas of the health centers had a significant impact on the technical efficiency of the health centers. Accordingly, the efficiency of the health centers that of the catchment areas experienced armed conflicts declined by one-fifth compared to the health centers that of the catchment area did not experience such conflicts.
In the same way, the study conducted in Syria showed that the utilization of routine health services, such as ANC and outpatient consultations were negatively correlated with conflict incidents [31]; a study in Cameroon revealed that the population's utilization of healthcare services declined during the armed conflict [32]; a study in Nigeria showed that living in a conflict-affected area significantly decreases the likelihood of using healthcare services [33].
This could be due to the fact that healthcare providers in areas affected by violence may face many obstacles. They first encounter health system limitations: lack of medicines, medical supplies, healthcare workers, and financial resources are all consequences of conflict, which also harms health and the infrastructure that supports it. Additionally, it adds to the load already placed on health services. Second, access to communities in need of health care by both these populations and health personnel is made more challenging by armed conflict [33].
Furthermore, in-service training of the health care providers significantly improved the efficiency of the health centers. In the current study, the efficiency scores of health centers that of the health care providers had adequate in-service training increased by one-fourth compared to those health centers that of the staffs had inadequate in-service training. Similar to this, a scoping review study in LMICs revealed that combined and multidimensional training interventions could aid in enhancing the knowledge, competencies, and abilities of healthcare professionals in data administration and health care delivery [34].
Limitatations of the study
This study thoroughly evaluated the technical efficiency level of public health centers in delivering health services by using an input–output-oriented DEA model. Additionally, it pinpointed the determinants of technical efficiency in these health centers using a Tobit regression analysis. However, this technical efficiency analysis report in this study was based on the inputs and outputs data for the 2021–2022 EFY. Much might have been changed since 2021–2022 EFY. The findings aimed to bring attention to the potential advantages of this particular type of efficiency study rather than to provide blind guidance for decision-making in health care system. Due to a lack of data, the study did not include spending on drugs, non-pharmaceutical supplies, and other non-wage expenditures among the inputs. The DEA model only measures efficiency relative to best practice within the health center samples. Thus, any change in any type and number of health facilities and varibales included in the analysis can result in the different findings.
Policy implication of the study
In the current study, it was found that 90% of health centers were operating below scale efficiency, leading to the wastage of nearly half of the healthcare resources. This inefficiency likely had detrimental effects on healthcare service delivery. The findings suggest that merely allocating resources is insufficient for enhancing facility efficiency. Instead, a dual approach is necessary. This includes addressing enabling factors such as providing in-service training opportunities for healthcare providers and considering the strategic location of healthcare facilities. Simultaneously, it is imperative to mitigate disabling factors, like the incidents of armed conflicts within the catchment areas of these health care facilities. Implementing these measures at all levels could significantly improve the efficiency of health care facilities in healthcare deliveries.
Conclusions
Only one out of ten health centers operated with technical efficiency, indicating that approximately nine out of ten health centers used nearly half of the healthcare resources inefficiently. This is despite the fact that they could potentially reduce their inputs by nearly half while still maintaining the same level of output. The location of health centers and the armed conflict incidents in the catchment areas of the health centers significantly declined the efficiency scores of the health centers, whereas in-service training of the health care providers significantly increased the efficiency of the health centers.
Therefore, we strongly recommend the government and the health sector to focus on improving the health service delivery in the health centers by making efficient utilization of the health care resources, resolving armed conflicts with concerned bodies, organizing training opportunities for health care providers, and taking into account the rural and urban locations of the healthcare facilities when allocating resources for the healthcare facilities.
Availability of data and materials
The datasets used and/or analyzed during this study are available from the corresponding author on reasonable request.
References
Pa S. David JT. Definitions of efficiency. BMJ. 1999;318:1136.
Mooney G, Russell EM, Weir RD. Choices for health care: a practical introduction to the economics of health care provision. London: Macmillian; 1986.
Mann C, Dessie E, Adugna M, Berman P. Measuring efficiency of public health centers in Ethiopia. Harvard T.H. Boston, Massachusetts and Addis Ababa, Ethiopia: Chan School of Public Health and Federal Democratic Republic of Ethiopia Ministry of Health; 2016.
World Health Organization, Yip, Winnie & Hafez, Reem. Improving health system efficiency: reforms for improving the efficiency of health systems: lessons from 10 country cases. World Health Organization; 2015. https://iris.who.int/handle/10665/185989.
Heredia-Ortiz E. Data for efficiency: a tool for assessing health systems’ resource use efficiency. Bethesda, MD: Health Finance & Governance Project, Abt Associates Inc; 2013.
Walters JK, Sharma A, Malica E, et al. Supporting efficiency improvement in public health systems: a rapid evidence synthesis. BMC Health Serv Res. 2022;22:293. https://doi.org/10.1186/s12913-022-07694-z.
Queen Elizabeth E, Jane Osareme O, Evangel Chinyere A, Opeoluwa A, Ifeoma Pamela O, Andrew ID. The impact of electronic health records on healthcare delivery and patient outcomes: a review. World J Adv Res Rev. 2023;21(2):451–60.
Bastani P, Mohammadpour M, Samadbeik M, et al. Factors influencing access and utilization of health services among older people during the COVID − 19 pandemic: a scoping review. Arch Public Health. 2021;79:190. https://doi.org/10.1186/s13690-021-00719-9.
FMOH. Health Sector Transformation Plan (2015/16 - 2019/20). Addis Ababa, Ethiopia: Federal Democratic Republic of Ethiopia Ministry of Health; 2015.
lebachew A, Yusuf Y, Mann C, Berman P, FMOH. Ethiopia’s Progress in Health Financing and the Contribution of the 1998 Health Care and Financing Strategy in Ethiopia. Resource Tracking and Management Project. Boston and Addis Ababa: Harvard T.H. Chan School of Public Health; Breakthrough International Consultancy, PLC; and Ethiopian Federal Ministry of Health; 2015.
Alebachew A, Hatt L, Kukla M. Monitoring and Evaluating Progress towards Universal Health Coverage in Ethiopia. PLoS Med. 2014;11(9):e1001696. https://doi.org/10.1371/journal.pmed.1001696.
Berman P, Mann C, Ricculli ML. Financing Ethiopia’s Primary Care to 2035: A Model Projecting Resource Mobilization and Costs. Boston: Harvard T.H. Chan School of Public Health; 2015.
World Bank. Ethiopia: Public Expenditure Review, Volume 1. Main Report. Public expenditure review (PER);. © Washington, DC; 2000. http://hdl.handle.net/10986/14967. License: CC BY 3.0 IGO.
Federal Democratic Republic of Ethiopia (FDRE). Growth and Transformation Plan II (GTP II) (2015/16–2019/20). Vol. I. Addis Ababa; 2016.
Powell-Jackson T, Hanson K, McIntyre D. Fiscal space for health: a review of the literature. London, United Kingdom and Cape Town, South Africa: Working Paper 1; 2012.
Evans DB, Tandon A, Murray CJL, Lauer JA. The comparative efficiency of National of Health Systems in producing health: An analysis of 191 countries. World Health Organization. 2000;29(29):1–36. Available from: http://www.who.int/healthinfo/paper29.pdf.
Coelli TJ. A Guide to DEAP Version 2.1: a data envelopment analysis (Computer) Program. Centers for Efficiency and Productivity Analysis (CEPA) Working papers, No. 08/96.
Charnes A, Cooper WW, Seiford LM, Tone K. Data envelopment analysis: theory. Data envelopment analysis: a comprehensive text with models applications, references and DEA-solver software. 2nd ed. Dordrecht: Academic Publishers; 1994. p. 1–490.
Carson RT, Sun Y. The Tobit model with a non-zero threshold. Econometr J. 2007;10(1):1–15.
Wang D, Du K, Zhang N. Measuring technical efficiency and total factor productivity change with undesirable outputs in Stata. Stata J: Promot Commun Stat Stata. 2022;22(1):103–24.
Chai P, Zhang Y, Zhou M, et al. Technical and scale efficiency of provincial health systems in China: a bootstrapping data envelopment analysis. BMJ Open. 2019;9:e027539. https://doi.org/10.1136/bmjopen-2018-027539.
Akazili J, Adjuik M. Using data envelopment analysis to measure the extent of technical efficiency of public health centers in Ghana. Health Hum Rights. 2008. http://www.biomedcentral.com/1472–698X/8/11.
Renner A, Kirigia JM, Zere E, Barry SP, Kirigia DG, Kamara C, et al. Technical efficiency of peripheral health units in Pujehun district of Sierra Leone: a DEA application. BMC Health Serv Res. 2005;5:77.
Kirigia JM, Emrouznejad A, Sambo LG, Munguti N, Liambila W. Using data envelopment analysis to measure the technical efficiency of public health centers in Kenya. J Med Syst. 2004;28(2):155–66.
Bobo FT, Woldie M, Muluemebet Wordofa MA, Tsega G, Agago TA, Wolde-Michael K, Ibrahim N, Yesuf EA. Technical efficiency of public health centers in three districts in Ethiopia: two-stage data envelopment analysis. BMC Res Notes. 2018;11:465. https://doi.org/10.1186/s13104-018-3580-6.
Tesleem KB, Indres M. Assessing the Efficiency of Health-care Facilities in Sub-Saharan Africa: A Systematic Review. Health Services Research and Managerial Epidemiology. 2020;7:1–12. https://doi.org/10.1177/2333392820919604.
Farhad F, Khwaja S, Abo F, Said A, Mohammad Z, Sinai I, Wu Z. Efficiency analysis of primary healthcare facilities in Afghanistan. Cost Eff Res Alloc. 2022;20:24. https://doi.org/10.1186/s12962-022-00357-0.
de Siqueira Filha NT, Li J, Phillips-Howard PA, et al. The economics of healthcare access: a scoping review on the economic impact of healthcare access for vulnerable urban populations in low- and middle-income countries. Int J Equity Health. 2022;21:191. https://doi.org/10.1186/s12939-022-01804-3.
Javier GL, Emilio M. Rural vs urban hospital performance in a ‘competitive’ public health service. Soc Sci Med. 2010;71:1131-e1140.
Zhou J, Peng R, Chang Y, Liu Z, Gao S, Zhao C, Li Y, Feng Q, Qin X. Analyzing the efficiency of Chinese primary healthcare institutions using the Malmquist-DEA approach: evidence from urban and rural areas. Front Public Health. 2023;11:1073552. https://doi.org/10.3389/fpubh.2023.1073552.
Abdulkarim E, Yasser AA, Hasan A, Francesco C. The impact of armed conflict on utilisation of health services in north-west Syria: an observational study. BMC Confl Health. 2021;15:91. https://doi.org/10.1186/s13031-021-00429-7.
Eposi CH, Chia EJ, Benjamin MK. Health services utilisation before and during an armed conflict; experiences from the Southwest Region of Cameroon. Open Public Health J. 2020;13:547–54. https://doi.org/10.2174/1874944502013010547.
Alice D. Hard to Reach: Providing Healthcare in Armed Conflict. International Peace Institute. Issue Brief; 2018. Available at: https://www.ipinst.org/2019/01/providing-healthcare-in-armed-conflict-nigeria.
Edward N, Eunice T, George B. Pre- and in-service training of health care workers on immunization data management in LMICs: a scoping review. BMC Hum Res Health. 2019;17:92. https://doi.org/10.1186/s12960-019-0437-6.
Acknowledgements
Our special thanks go to Wollega University and study health facilities.
Funding
We received no financial supports to be disclosed.
Author information
Authors and Affiliations
Contributions
All authors participated in developing the study concept and design of the study. ET. contributed to data analysis, interpretation, report writing, manuscript preparation and acted as the corresponding author. DR, AT, A E, WB, WO, MC, and ML contributed to developing the data collection tools, data collection supervision, data entry to statistical software and report writing.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Wollega University's research ethical guidelines were adhered to carry out this study. The research ethics review committee (RERC) of Wollega University granted the ethical clearance number WURD-202–44/22. A formal letter from the East Wollega Zonal Health Department was taken and given to the district health offices. The objective of the study was clearly communicated to all study health center directors and the required informed consent was obtained from all the study health centers. The study health centers’ confidentially was maintained. The codes from DMU001 to DMU034 were used in place of health facility identification in the data collection checklists. Each document of electronic and paper data was stored in a secure area. The research team was the only one with access to the data that was collected, and data sharing will be done in accordance with the ethical and legal guidelines.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Geta, E.T., Terefa, D.R., Shama, A.T. et al. Technical efficiency and its determinants in health service delivery of public health centers in East Wollega Zone, Oromia Regional State, Ethiopia: Two-stage data envelope analysis. BMC Health Serv Res 24, 980 (2024). https://doi.org/10.1186/s12913-024-11431-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-024-11431-z