Abstract
Background
Implementation of the World Health Organization (WHO) recommended Advanced HIV Disease screening package, remains poor in most settings with limited resources. More than 50% of newly diagnosed-HIV clients are missed on screening as a result of implementation barriers. It is important to mitigate the existing barriers and leverage enablers’ inorder to maximize uptake of the advanced HIV disease screening. This study aimed to identify strategies for scaling up implementation of advanced HIV disease screening among newly HIV-diagnosed clients in pre-ART phase using a Consolidated Framework for Implementation Research-Expert Recommendation for Implementing Change (CFIR-ERIC) guiding tool.
Methods
A qualitative study was conducted at Rumphi district hospital in Malawi (August – September, 2023). Two sessions of Focus group discussions (FDGs) involving key stakeholders were facilitated to identify specific strategies following the initial study on exploration of barriers and facilitators of advanced HIV disease screening package. Participants comprised healthcare providers, purposively selected from key hospital departments. A deductive approach was used to analyze FDG transcripts where emerging themes were mapped with ERIC list of strategies. CFIR-ERIC Matching tool version 1.0, was used to generate an output of the most to least expert-endorsed Level 1 and Level 2 strategies.
Findings
About 25 key healthcare workers participated in FDGs. Overall, 6 Level 1 strategies (≥ 50% expert endorsement score) and 4 Level 2 strategies (≥ 20%, ≤ 49% expert endorsement score) were identified, targeting barriers associated with availability of resources, intervention complexity, access to knowledge and information, communication; and implementation leads. Most of the reported strategies were cross-cutting and aimed at enhancing clinical knowledge of the intervention (distributing training materials, educational meetings), developing stakeholders’ interrelations (network weaving) as well as improving clinical workflow (environmental restructuring). Use of evaluative and iterative strategies such as monthly data collection for evaluation were also recommended as part of continuous improvement while an AHD coordinator was recommended to be formally appointed inorder to spearhead coordination of AHD screening services.
Conclusion
Through the involvement of key stakeholders and the use of CFIR-ERIC matching tool, this study has identified cross-cutting strategies that if well implemented, can help to mitigate contextual barriers and leverage enablers for an improved delivery of AHD screening package.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Despite the Universal Test and Treat (UTT) approach as well as the significant progress in expanding access to antiretroviral therapy (ART), advanced HIV disease (AHD) prevalence remain high among the newly HIV-diagnosed clients [1, 2]. The World Health Organization (WHO), defines AHD in adult patients as those having CD4 count < 200 CD4 cells/mm3 or WHO Stage III & IV defining illness at presentation [3]. Advanced HIV disease in the pre-ART phase has been singled out as the major cause of early HIV mortality and treatment complications such as Immune reconstitution inflammatory syndrome (IRIS), a state of hyper-inflammatory response in the first few months of ART treatment [4].
In 2017, WHO recommended a screening and treatment package for AHD in an effort to reduce the number of deaths among people living with HIV (PLWH) [5]. For the newly diagnosed HIV clients, the AHD screening package involve checking CD4 cell count and running some rapid tests to detect Cryptococcal antigen in serum as well as mycobacterial lipoarabinomannan (LAM) antigen in Urine [6]. In 2020, the overall prevalence of AHD for the five referral hospitals in Malawi, supported by Lighthouse organization, was at 35%. At Rumphi District Hospital, where the prevalence of AHD was 41%, 61% of newly diagnosed-HIV clients had no documentation of CD4 Cell count as a baseline test for determining AHD [7]. Such a low screening coverage is evidence enough of existing barriers affecting implementation. Moreover, statistics from the Malawi National AIDS Commission (NAC) indicate that AIDS-related deaths have plateaued over the past three years (10,800 in 2020, 13,000 in 2021 and 11,931 in 2022) [2, 8, 9]. Therefore, the importance of AHD screening in pre-ART phase cannot be overemphasized [1, 10, 11].
In our initial study [7], we identified barriers such as poor work coordination among implementers due to absence of communication platforms. Additionally, there was limited resources to support the expansion of AHD screening services, as well as knowledge gap among providers who were yet to undergo formal trainings in AHD. However, external support from Ministry of Health (MoH) implementing partners in form of policy guidelines, mentorship and supervisions as well as the availability of committed focal leaders coordinating ART and HIV testing services (HTS) programs, emerged as enablers of AHD screening package within the facility. Much as the barriers and facilitators of AHD screening are documented, little is known about the specific implementation strategies suitable for overcoming cited barriers often reported in secondary referral facilities. Without efforts to address the barriers and leverage the enablers of AHD screening, AIDS mortality among new ART clients who often present with asymptomatic AHD, will continue to prevail. Hence, strengthening implementation of the AHD screening package is critical. In this study, we aimed to identify strategies to address implementation barriers to AHD screening package at a secondary referral hospital, using the Expert Recommendation for Implementing Change (ERIC) tool.
Methods
Study design
A qualitative study design was conducted to identify strategies for overcoming barriers to AHD screening. The study was conducted following an initial study which explored barriers and facilitators to implementation of AHD screening package at a secondary referral hospital in Malawi [7].
Research frame-work tool
Data collection methods for identifying strategies were framed using a consolidated framework for implementation science (CFIR) and an Expert Recommendation for Implementing Change (ERIC) [12]. The CFIR, is a theoretical framework designed to identify potential contextual determinants of barriers or facilitators of implementation, and it includes 39 constructs within five main domains (intervention characteristics, outer setting, inner setting, characteristics of individuals, and implementation process) [13]. On the other hand, the ERIC is a tool for identifying suitable strategies for overcoming barriers identified through CFIR framework [14]. It was developed through input from 169 implementation science experts, who selected and ranked up to seven of the 73 ERIC strategies they thought would best address each CFIR barrier [12]. The CFIR-ERIC Matching tool was developed as a way to link these two key resources to help users understand which ERIC implementation strategies will best address CFIR related barriers [14].
Study setting
The study was conducted at Rumphi district hospital, located in an urban area in the northern part of Malawi. At the time of data collection, the hospital ART Clinic had 10 691 clients on ART, with HIV adult prevalence of 5.3% as compared to 8.9% national wide [15]. By December 2023, the hospital had registered 879 HIV related deaths with AHD prevalence estimated at 41%. The facility was chosen because It was among the district hospitals that consistently reported high numbers of newly-diagnosed clients missed on AHD screening [8].
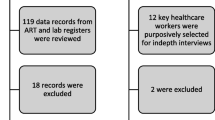
Study population and sampling methods
The study purposively recruited health care workers (HCWs) involved in the implementation of AHD screening package. Ten individuals who participated in the in-depth interviews (IDI) during the initial study [7], were purposively included among the stakeholders, followed by departmental incharges and.hospital managers who were formally invited through letters. A total of 25 stakeholders participated in two focus group discussions, taking into account their level of expertise. Lay cadres and trainees were not included as they were considered not formally trained in the management of AHD, hence lacking adequate information about the screening process.
Data collection procedure and analysis of Focus Group Discussions (FDGs)
Initial stakeholders meeting
The 25 Key AHD players were engaged in the identification of tailored and blended strategies for overcoming the existing barriers. During the meeting, lead investigator (BM) presented the barriers to AHD screening as findings from the initial study [7]. Following the presentation, the moderator (co-author), facilitated further discussion on strategies for mitigating the barriers which were displayed on a projector. To obtain group consent, stakeholders were informed prior to recordings for subsequent data analysis. Every member willing to make a contribution was given a maximum of 2 min. During the discussion, notes were also captured by research team members. At the end of the meeting, the moderator made a summary of major issues that came up. Members were also informed to avail themselves for the second stakeholders meeting after data analysis to review the strategies and select actors. The meeting took a maximum of 3h: 15min.
Data analysis (deductive)
A team of four authors (BM, GG, MM, and SM) were tasked to translate sections of recordings into word transcripts. After a week, the team met and combined the transcripts. The transcripts were then reviewed to ensure nothing is omitted. Each research team member was then tasked to independently read the transcripts and identify themes rising under every CFIR barrier presented during stakeholders meeting. The identified themes were then independently matched to a suitable strategy on the ERIC list of strategies. The findings from all the four members were compared and any disagreements were resolved through consensus. A list of mapped strategies were reviewed and refined by an independent team of experts.
The lead author (B.M) then used the CFIR-ERIC Matching tool version 1.0, an excel sheet to produce an output of the most to least expert-endorsed Level 1 and Level 2 strategies. Level 1 strategies being those with majority endorsement (50% +) by implementation experts (n = 169) through a survey; while Level 2 strategies being those outputs falling within 20% to 49.9% of experts endorsed strategies for addressing barriers [16].
Final stakeholders meeting
The second stakeholders meeting was convened inorder to present the generated ERIC list strategies with endorsement scores. All the 25 stakeholders who attended the first meeting were formally invited through emails and hand written letters. Participants were allowed to suggest any changes or additions to the strategies and propose actors for each category of strategies. During the meeting, an intervention table was constructed, describing ERIC implementation strategies including activities and actors to be involved in the implementation process. All the tables containing strategies were member-checked with selected key experts and further refined as needed.
Results
A total of 25 key healthcare workers (HCWs) participated in two set of stakeholders meetings with 60% (n = 15) of the participants being males. The median and average years of working were 15.6 and 15.7 respectively. All key departments including laboratory, ART Clinic and hospital wards were equally represented by key implementers of AHD (Table 1).
CFIR ERIC- tailored strategies, practices and actors
Using CFIR-ERIC matching tool, we identified several strategies matched to the most prominent barriers associated with availability of resources, intervention complexity, and work infrastructure, access to knowledge and information, communication, as well as implementation leads [7]. Stakeholders also went in as far as identifying actors such as formally appointed coordinator, site champions, management and others. Table 2 provides an outline of ERIC strategies descriptions, target practices and proposed actors to spearhead implementation of different tasks while Table 3 provides an implementation research logic model (IRLM) aligning the identified components In the implementation process and the expected outcomes.
Below is an overview of CFIR categorized barriers and the CFIR-ERIC recommended strategies with expert endorsement percentage (%) scores in two categories: level 1 strategies (≥ 50% expert endorsement score) highlighted in green; level 2 strategies (≥ 20%, ≤ 49% expert endorsement score) Overall, there were 7 Level 1and 4 level 2 strategies identified through the CFIR-ERIC Matching tool targeting contextual barriers (Table 4). Most of the strategies identified aimed at enhancing clinician and member knowledge as well as revising the clinic work flow to improve implementation process.
Implementation leads
Stakeholders noticed that most of the challenges encountered in the implementation of AHD screening package can be quickly resolved by having a formally appointed coordinator for AHD who would work hand in hand with other HIV programme coordinators. A TB clinician was then identified during the meeting and recommended to the hospital management for a formal appointment.
“But we really need coordinator in AHD who could be moving around in different departments checking if there are problems that need to be resolved, otherwise without coordinator challenges will continue as their lack ownership” [RDH/FG 1/ L3]
Therefore, stakeholders unanimously agreed to adopt one ERIC strategy (identify and appoint champions 60%) which was considered to address a range of implementation challenges.
Intervention complexity
With regards to implementation of interventions, stakeholders recommended that healthcare workers needed to be oriented in the use of recently introduced forms and registers for AHD which simplifies work in terms of making requests as well as documentation of results.
“Even the current lab form for TB sputum it has got everything, it has a section where it says if the clients is HIV positive, WHO stage 3 or critically ill can do TB-LAM and others AHD screening tests. So with this form it is very easy to grasp what need to be done as all ADH tests are indicated, so we can just orient the people – yes even during morning handovers, we can simply share everyone the forms and orient them” [RDH/FG2/R1-L2]
“We need also to ask MoH to send additional registers for AHD as current it’s only at ART and it is very easy to miss some of the patients in the wards or out-patient department who donot pass through ART” [RDH/FG2/R2]
Three level 2 ERIC strategies were therefore adopted to address barriers associated with complexity of AHD screening package including: promoting adaptability (40%,) conduct on-going training or orientation for AHD providers in key departments (37%), and identify & prepare champions (30%) to build capacity and motivate staff members to adopt new strategies.
Communication and networks
Stakeholders highlighted a number of strategies to improve communication among implementers working in different departments. They highlighted creation of social media platforms such as WhatsApp group for AHD, and facilitation of inter-departmental meetings to implementation challenges and share other useful updates regarding AHD services.
“I think through the WhatsApp forum we have suggested, we can be sharing weekly rosters between laboratory and ART for us to know who is now covering on AHD in our departments and including their phone numbers so that we can call whenever we want to inquire about services” [RDH/FG1/R8]
The ERIC strategies recommended for mitigating communication barriers focused on establishing stakeholder’s interrelationship and they included one level 1 strategy: network weaving (70%) and two level 2 strategies: build coalition (39%) as well as creation of a learning collaborative environment (35%) to promote information sharing among implementing teams.
Access to knowledge and information
On strategies for addressing knowledge gap among implementers, most stakeholders were of the view that informal trainings should be promoted alongside distribution of learning materials such as jobAids in all the sites conducting AHD screening.
“In terms of knowledge and information accessibility, we just have to paste jobAids in priotized areas like in the lab, HTS, Wards and there at ART clinic” [RDH/GF1/R15]
“We have the resources but people are not using them rightfully” [RDH/GFI/L2]
Recommended ERIC strategies selected were those centered on enhancing providers and practice member knowledge about the intervention and they included two level 1 strategies (conducting education meetings 79%; developing education materials 59% and distributing education materials 56%) and two level 2 strategies (create a learning collaborative 45%; conduct on-going trainings 38%).
Availability of resources
During the second stakeholders meeting, members from ART were optimistic that the new ART facility under construction will have the needed infrastructure and equipment for AHD screening which will limit movement of clients from ART to Laboratory.
“The good thing is that the current ART clinic under construction has a Min-Laboratory so maybe laboratory will provide training or personnel to run the min-lab… we will provided a list of what is required for a functional min-lab” [RD/FD2/Lab1]
Recommended ERIC strategies for addressing gaps relating to unavailable resources and structural barriers include access to new funding (78%, level 1 strategy) and development of resource sharing agreements (26%) through strong partnerships with MoH implementing organizations.
Discussion
This study aimed at identifying strategies for optimizing AHD screening, a process that initially involved identification of barriers and facilitators [7]. We therefore adopted a systematic approach of gathering input from key stakeholders on specific strategies for addressing implementation barriers within the facility. Using the CFIR-ERIC Matching tool, we identified 12 cross-cutting Implementation strategies (with 7 level 1 and 5 level 2 ERIC strategies categories) targeting barriers associated with availability of resources including physical and work structure, intervention complexity; knowledge and information gap; as well as communication.
Most of the implementation barriers were interlinked, hence, required both tailored and multifaceted approaches to be addressed at all levels of a healthcare facility [17]. Just like other projects that utilized the CFIR-ERIC Matching tool, we found the tool easy to use and appropriate as it provided a standard way of developing discreet and multifaceted strategies for addressing barriers AHD screening pathways [18].
With the knowledge of the existing barriers and facilitators described in our initial exploratory study [7], stakeholders were able to identify actors and targets for improvement using evaluative and iterative strategies such as ongoing monitoring and collection of statistical data on screening coverage and linkage to care. Such evaluative strategies have been applied before in evaluation of HIV programmes [19]. With the use of effective frameworks such as CFIR, evaluative and iterative strategies can be used to provide basis for understanding the context in which the intervention is implemented as well as assessing the progress of implementation process [20].
Availability of resources such as funding, space, materials and equipment are key for a successful implementation and delivery of the intervention [21]. In our study, stakeholders proposed changes in physical and work infrastructure as a way to improve clinical work flow in ADH screening. The construction of the new ART clinic comprising a min-laboratory was therefore seen as a fundamental step towards improving accessibility of AHD screening services among PLWH. Currently, the ART clinic department make use of lay cadres in sample collection and escorting patients to the laboratory to ensure that screening is done with sense of urgency. Therefore, improved clinical work flow may lead to reduction of clients waiting times.
Poor communication networks were significantly highlighted during the initial exploratory study [7]. This may have been attributed to fragmented teams and frequent changes in personnel working in strategic screening sites [22]. Recognizing it as an important aspect of effective delivery of AHD screening, stakeholders made a resolution to promote facility-based communication networks that are proven to be cost-effective. Following the proposal made during the initial stakeholders meeting, a WhatsApp group forum was created to facilitate consultations between healthcare providers in the management of patients where formal communication systems are inefficient [22, 23]. This complements the CFIR-ERIC Matching tool recommendations on promotion of network weaving and implementation team meetings to aid information sharing and collaborative problem-solving regarding the intervention [14].
To address the knowledge gap and improve self-efficacy among AHD providers, a package of multifaceted strategies aiming at enhancing clinical member knowledge of intervention, were recommended. These include conducting on-going trainings and educational meetings, developing and distributing educational materials such as jobAids and guidelines for staff with inadequate knowledge to use [22, 24]. These strategies are well cited in other implementation research and interventional studies [24, 25]. Improved clinical knowledge of the intervention leads to improved provider’s self-confidence, uniformity and consistent quality of work [25].
To ensure maximum utilization of ERIC strategies identified, there is need to leverage the existing enablers of AHD screening such as mentorship and supervision programs to fill the gap of knowledge. It is also important to promote Integration of AHD services in ART and HIV testing services to reduce duplication of services for a more efficient delivery [26, 27].
Currently, there is overwhelming evidence that AHD screening improves early diagnosis and management of opportunistic conditions, thereby contributing to general improvement of quality of life for PLWH who would otherwise succumb to death [9, 28]. Hence the urgent need to coordinate implementation of the highlighted cost -effective approaches in addressing barriers affecting AHD service delivery.
The importance of having implementation team leads cannot be over-emphasized [28]. During the second stakeholders meeting, members made recommendation to the hospital management to formalize the appointment of a coordinator for AHD services within the facility. This is in line with ERIC strategy on identifying and appointing site champions to oversee the implementation of the proposed strategies. Both healthcare workers under MoH and Right to Care organization, expressed willingness to work with the coordinator in improving the delivery of AHD services within the district. Working collaborations increases use of best practices and uptake of the interventions at an organizational level [29].
Study limitations
Strategies identified in this study are site specific which makes it difficult to generalize the findings. While the findings might play a critical role in improving the delivery of AHD screening during piloting, there could be challenges in sustaining the implementation where little support is given to the facility to integrate the practices. One of the study strength is that key stakeholders including AHD providers, heads of departments, and hospital managers were involved in the identification of the strategies. This ensures that the strategies are acceptable and appropriate for implementers to adopt and sustain.
Conclusion and recommendation
Through the involvement of key stakeholders, this study has identified strategies considered appropriate in addressing implementation barriers to AHD screening at a facility level. Most of them aimed at enhancing clinical knowledge of the intervention, developing stakeholders’ interrelations as well as improving clinical workflow. If well implemented, can mitigate most barriers, leverage enablers and strengthen the delivery of AHD screening package. However, there is need to incorporate behavior change strategies to ensure continued adherence to the strategies. Future studies conducted on large scale must include peripheral sites and involve HIV clients to better understand their perspectives regarding AHD screening experiences.
Availability of data and materials
Raw data for dataset D1 are not publicly available to preserve individuals’ privacy under the European General Data Protection Regulation. However, data requests can be made to Rumphi District Hospital through the corresponding author (Brany Mithi, branytitus@gmail.com) upon reasonable request.
Data availability
The data used in this study are available from the corresponding author (Brany Mithi, branytitus@gmail.com) upon reasonable request.
Abbreviations
- ART:
-
Antiretroviral Therapy
- AHD:
-
Advanced HIV Disease
- CFIR:
-
Consolidated Framework for Implementation Research
- COMREC:
-
College of Medicine Research Ethics
- CrAg:
-
Cryptococcol Antigen
- EGPAF:
-
Elizabeth Glaser Pediatric Aids Foundation
- ERIC:
-
Expert Recommendation for Implementing Change
- HCWs:
-
Health Care Workers
- HIV:
-
Human Immunodeficiency Virus
- IDIs:
-
In-depth Interviews
- IRIS:
-
Immune Reconstitution Inflammatory Syndrome
- MoH:
-
Ministry of Health
- MPHIA:
-
Malawi Population based HIV Impact Assessment
- OIs:
-
Opportunistic Infections
- PEPFAR:
-
President's Emergency Plan For AIDS Relief
- PLHIV:
-
People Living With HIV
- SSA:
-
Sub-Saharan Africa
- TAT:
-
Turn Around Time
- TB:
-
Tuberculosis
- UNAIDS:
-
United Nations Programme on HIV/AIDS
- WHO:
-
World Health Organization
References
Nicol E, et al. Enhancing linkage to HIV care in the ‘Universal Test and Treat’ era: Barriers and enablers to HIV care among adults in a high HIV burdened district in KwaZulu-Natal, South Africa. BMC Public Health. 2023;23(1):1756. https://doi.org/10.1186/s12889-023-16576-w.
Malawi Ministry of Health. Malawi Population-based HIV Impact Assessment (MPHIA) 2020–2021: Final Report. Report. 2022;2:13–126. Available: https://phia.icap.columbia.edu/malawi-final-report-2020-2021/.
Waldrop G, Doherty M, Vitoria M, Ford N. Stable patients and patients with advanced disease: consensus definitions to support sustained scale up of antiretroviral therapy. Trop Med Int Health. Sep.2016;21(9):1124–30. https://doi.org/10.1111/tmi.12746.
Bosamiya SS. The immune reconstitution inflammatory syndrome. Indian J Dermatol. 2011;56(5):476–9. https://doi.org/10.4103/0019-5154.87114.
Guidelines for managing advanced HIV disease and rapid initiation of antiretroviral therapy July 2017. no. July, 2017.
Chihana ML, et al. Distribution of advanced HIV disease from three high HIV prevalence settings in Sub-Saharan Africa: a secondary analysis data from three population-based cross-sectional surveys in Eshowe (South Africa), Ndhiwa (Kenya) and Chiradzulu (Malawi). Glob Health Action. 2019;12(1):1679472. https://doi.org/10.1080/16549716.2019.1679472.
Mithi B, Bula A, Kapanda L, Ngwalangwa F, Sambala EZ. Barriers and facilitators to implementing advanced HIV disease screening at a secondary referral hospital -Malawi: a convergent parallel study. BMC Health Serv Res. 2023;23(1):1015. https://doi.org/10.1186/s12913-023-10009-5.
Nyasulu P, editor. Advanced HIV Disease Update : Malawi HIV in Malawi-HIV prevalence ( 2020 HIV Spectrum ). 2020. Available: https://cquin.icap.columbia.edu/wp-content/uploads/2020/07/AHD-Meeting_Malawi-Presentation.pdf.
Koenig SP, et al. Same-day HIV testing with initiation of antiretroviral therapy versus standard care for persons living with HIV: A randomized unblinded trial. PLoS Med. 2017;14(7):1–15. https://doi.org/10.1371/journal.pmed.1002357.
Halperin J, et al. A care continuum of immediate ART for newly diagnosed patients andpatients presenting later to care at a federally qualified health center in New Orleans. Open Forum Infect Dis. 2019;6(4):ofz161. https://doi.org/10.1093/ofid/ofz161.
Sanga ES, Mukumbang FC, Mushi AK, Lerebo W, Zarowsky C. Understanding factors influencing linkage to HIV care in a rural setting, Mbeya, Tanzania: qualitative findings of a mixed methods study. BMC Public Health. 2019;19(1):1–15. https://doi.org/10.1186/s12889-019-6691-7.
Powell BJ, et al. A refined compilation of implementation strategies: Results from the Expert Recommendations for Implementing Change (ERIC) project. Implement Sci. 2015;10(1):1–14. https://doi.org/10.1186/s13012-015-0209-1.
Damschroder LJ, Reardon CM, Widerquist MAO, Lowery J. The updated Consolidated Framework for Implementation Research based on user feedback. Implement Sci. 2022;17(1):1–16. https://doi.org/10.1186/s13012-022-01245-0.
Shin MH, Montano A-RL, Adjognon OL, Harvey KLL, Solimeo SL, Sullivan JL. Identification of Implementation Strategies Using the CFIR-ERIC Matching Tool to Mitigate Barriers in a Primary Care Model for Older Veterans. Gerontologist. Apr.2023;63(3):439–50. https://doi.org/10.1093/geront/gnac157.
MPHIA. Malawi population-based HIV impact assessment MPHIA 2020 -2021. 2021. Available: https://phia.icap.columbia.edu/wp-content/uploads/2022/03/110322_MPHIA_Summary-sheet-English.pdf.
Waltz TJ, et al. Use of concept mapping to characterize relationships among implementation strategies and assess their feasibility and importance: Results from the Expert Recommendations for Implementing Change (ERIC) study. Implement Sci. 2015;10(1):1–8. https://doi.org/10.1186/s13012-015-0295-0.
Powell BJ, et al. Enhancing the Impact of Implementation Strategies in Healthcare: A Research Agenda. Front public Heal. 2019;7:3. https://doi.org/10.3389/fpubh.2019.00003.
Dekker M, Jongerden IP, de Bruijne MC, Jelsma JGM, Vandenbroucke-Grauls CMJE, van Mansfeld R. Strategies to improve the implementation of infection control link nurse programs in acute care hospitals. J Hosp Infect. 2022. https://doi.org/10.1016/j.jhin.2022.07.005.
Goorts K, Dizon J, Milanese S. The effectiveness of implementation strategies for promoting evidence informed interventions in allied healthcare : a systematic review. BMC Health Serv Res. 2021;21(1):241.
Toropova A, et al. Effectiveness of a multifaceted implementation strategy for improving adherence to the guideline for prevention of mental ill-health among school personnel in Sweden : a cluster randomized trial. Implement Sci. 2022. https://doi.org/10.1186/s13012-022-01196-6.
Ashok M, Hung D, Rojas-Smith L, Rojas-Smith MT, Harrison M. Framework for research on implementation of process redesigns. Qual Manag Healthc. 2018;27(1):17–23. Available: https://journals.lww.com/qmhcjournal/fulltext/2018/01000/framework_for_research_on_implementation_of.3.aspx.
Rogers HL, et al. Barriers and facilitators in the implementation of an evidence-based health promotion intervention in a primary care setting: a qualitative study. J Health Organ Manag. 2021;35(9):349–67. https://doi.org/10.1108/JHOM-12-2020-0512.
R. Olum, F. Bongomin. Social media platforms for health communication and research in the face of COVID-19 pandemic: a cross sectional survey in Uganda. medRxiv. p. 2020.04.30.20086553, 2020.
Woods J, Moorhouse M, Knight L. A descriptive analysis of the role of a WhatsApp clinical discussion group as a forum for continuing medical education in the management of complicated HIV and TB clinical cases in a group of doctors in the Eastern Cape, South Africa. South Afr J HIV Med. 2019;20(1):982. https://doi.org/10.4102/sajhivmed.v20i1.982.
Steenland M, et al. Effects of appointment scheduling on waiting time and utilisation of antenatal care in Mozambique. BMJ Glob Health. 2019;4(6):e001788.
Government of Lesotho. Approach to the management of advanced HIV disease ( AHD ) Government of Lesotho. 2020. https://differentiatedservicedelivery.org/Portals/0/adam/Content/gDujY9rV90i3ggXjQ3Upow/File/LesothoAdvancedHIVDiseaseManual_June252020_vF.pdf.
Garrib A, et al. Integrated care for human immunodeficiency virus, diabetes and hypertension in Africa. Transactions of the Royal Society of Tropical Medicine and Hygiene. 2019;113(12):808–11. https://doi.org/10.1093/trstmh/try098.
Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. Aug.2009;4:50. https://doi.org/10.1186/1748-5908-4-50.
Santos WJ, Graham ID, Lalonde M, Demery Varin M, Squires JE. The effectiveness of champions in implementing innovations in health care: a systematic review. Implement Sci Commun. 2022;3(1):80. https://doi.org/10.1186/s43058-022-00315-0.
Acknowledgements
Would like to acknowledge the following individuals for their contributions towards this article. Directors and coordinator from Malawi HIV Implementation Research Scientist Training (M-HIRST) program for approving the research protocol for funding; Staff members from Rumphi District Hospital for their participation in different stages of the research including stakeholders meeting. Further acknowledgments goes to MoH for partly funding the study.
Funding
The research was supported by the Fogarty International Center of the National Institutes of Health (NIH) under the Award Number D43TW010060 and Malawi Ministry of Health, through research Department. The content does not represent the official views of the NIH or MoH. The funders had no role in the study design, data collection and analysis. Decision to publish or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
BM, EK, ZJ developed protocol, collected, analyzed data and wrote the manuscript. AB played a role in qualitative data validation, codebook development and thematic analysis. GG, MMC and SM participated in the review of the identified implementation strategies. EZS supervised research protocol development and reviewed the entire manuscript document. ASM supervised manuscript development. All authors read and approved the final manuscript. BM = Brany Mithi, EK = Emily Kumilonde, ZJ = Ziliro Jere, AG = Agatha Bula, GG = Grant Gondwe, MMC = Marion M Chikuse, SM = Simon Manda, EZS = Evanson Z Sambala, ASM = Adamson S Muula.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the National Health Science Research Committee (NHSRC certificate number P.22/09/3050). Informed consent was obtained from all subjects and/or their legal guardian(s). All experiments were performed in accordance with relevant guidelines and regulations (such as the Declaration of Helsinki).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Mithi, B., Sambala, E.Z., Bula, A. et al. Strategies for scaling up pre-ART advanced HIV disease screening at a secondary referral hospital—Malawi: a qualitative study. BMC Health Serv Res 24, 915 (2024). https://doi.org/10.1186/s12913-024-11412-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-024-11412-2