Abstract
Background
In low and middle-income countries (LMICs), non-communicable diseases (NCDs) are on the rise and have become a significant cause of mortality. Unfortunately, accessing affordable healthcare services can prove to be challenging for individuals who are unable to bear the expenses out of their pockets. For NCDs, the treatment costs are already high, and being multimorbid further amplifies the economic burden on patients and their families. The present study seeks to bridge the gap in knowledge regarding the financial risks that come with NCD multimorbidity. It accomplishes this by examining the catastrophic out-of-pocket (OOP) expenditure levels and the factors that contribute to it at Tikur Anbesa Specialized Hospital, Addis Ababa, Ethiopia.
Methods
A facility-based cross-sectional study was conducted at Tikur Anbesa Specialized Hospital between May 18 and July 22, 2020 and 392 multimorbid patients participated. The study participants were selected from the hospital’s four NCD clinics using systematic random sampling. Patients’ direct medical and non-medical out-of-pocket (OOP) expenditures were recorded, and the catastrophic OOP health expenditure for NCD care was estimated using various thresholds as cutoff points (5%, 10%, 15%, 20%, 25%, and 40% of both total household consumption expenditure and non-food expenditure). The collected data was entered into Epi Data version 3.1 and analyzed using STATA V 14. Descriptive statistics were utilized to present the study’s findings, while logistic regression was used to examine the associations between variables.
Results
A study was conducted on a sample of 392 patients who exhibited a range of socio-demographic and economic backgrounds. The annual out-of-pocket spending for the treatment of non-communicable disease multimorbidity was found to be $499.7 (95% CI: $440.9, $558.6) per patient. The majority of these expenses were allocated towards medical costs such as medication, diagnosis, and hospital beds. It was found that as the threshold for spending increased from 5 to 40% of total household consumption expenditure, the percentage of households facing catastrophic health expenditures (CHE) decreased from 77.55 to 10.46%. Similarly, the proportion of CHE as a percentage of non-food household expenditure decreased from 91.84 to 28.32% as the threshold increased from 5 to 40%. The study also revealed that patients who traveled to Addis Ababa for healthcare services (AOR = 7.45, 95% CI: 3.41–16.27), who were not enrolled in an insurance scheme (AOR = 4.97, 95% CI: 2.37, 10.4), who had more non-communicable diseases (AOR = 2.05, 95% CI: 1.40, 3.01), or who had more outpatient visits (AOR = 1.46, 95%CI: 1.31, 1.63) had a higher likelihood of incurring catastrophic out-of-pocket health expenditures at the 40% threshold.
Conclusion and recommendation
This study has revealed that patients with multiple non-communicable diseases (NCDs) frequently face substantial out-of-pocket health expenditures (CHE) due to both medical and non-medical costs. Various factors, including absence from an insurance scheme, medical follow-ups necessitating travel to Addis Ababa, multiple NCDs and outpatient visits, and utilization of both public and private facilities, increase the likelihood of incurring CHE. To mitigate the incidence of CHE for individuals with NCD multimorbidity, an integrated NCD care service delivery approach, access to affordable medications and diagnostic services in public facilities, expanded insurance coverage, and fee waiver or service exemption systems should be explored.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Introduction
Non-communicable diseases (NCDs) represent a significant global challenge, with a substantial burden impacting numerous individuals worldwide. At present, NCDs are accountable for 74% of all deaths (41 million) and 80% of disability, with 15 million premature deaths occurring between the ages of 30 and 70. Low and Middle-Income Countries (LMICs) bear the impact of this burden, with 78% of all NCD deaths and 85% of premature deaths occurring in these nations. Four categories of diseases, namely cardiovascular disease (CVD), cancer, chronic Respiratory Disease (CRD), and diabetes mellitus (DM), are responsible for over 80% of all premature NCD deaths [1,2,3]. NCD multimorbidity is a co-existence of two or more NCDs in an individual.
NCDs have a significant impact on healthcare expenditure, contributing to reduced productivity and limited economic growth. The World Health Organization (WHO) has set a target of achieving Universal Health Coverage for over 1 billion people by 2023. Nevertheless, every year, approximately 808 million individuals spend more than 10% of their household budget on healthcare, and nearly 100 million people fall into extreme poverty due to high Out-Of-Pocket (OOP) health expenses. NCDs play a substantial role in these OOP payments, which in turn exacerbates health inequalities globally. OOP health expenditures place a considerable economic burden on households, obstructing efforts to alleviate poverty [4, 5].
According to recent global burden of disease data, NCDs such as CVD, cancer, CRD, and DM account for 39% of total annual mortality in Ethiopia [1, 3, 6]. By the year 2040, it is anticipated that Ethiopia will be the first densely populated African nation to encounter a substantial upsurge in premature mortality and disability resulting from NCDs [7]. Even though the national response to NCDs showed a significant increase between 2013/14 and 2019/20, these disease conditions are underestimated. According to the recent Ethiopian National Health Account (NHA) report NCDs shared 24.7% of the total health expenditure where the government and households contributed larger parts. In addition 80% of this share was spent on curative care which makes share of preventive care insignificant compared to the rapidly increasing disease burden [8].
Even though OOP payments below 15–20% of total health expenditure are a good indicator to reduce the risk of catastrophic health spending, in 2020, globally 16.36% of total health expenditure came from OOP payments. In many countries, OOP payments are still too high [9, 10]. Due to this, people may decide not to seek the healthcare they need, which may lead to a depreciated health status and decreased productivity, which will worsen the economic status of the population [11].
NCD multimorbidity has a strong and lifelong impact on the lives of those affected and is unlikely to be cured. It is associated with more complex healthcare needs, increased OOP expenditures, and higher health service utilization than people with a single condition [12, 13]. Evidence shows that more than 25% of the world population on average suffers from multimorbidity, and this figure is expected to increase in the coming years.
Multimorbidity is also becoming a source of inequality across the world, including in many LMICs with fragile healthcare systems and comparatively low levels of government spending on health and imperfect health insurance. Numerous findings across the world indicate that NCD multimorbidity is a serious concern, and some indicate that it is far more prevalent than a single health condition alone [14,15,16,17,18,19,20,21,22] .
Findings show that there is variation in NCD multimorbidity burden of across different settings. For instance, in a cross-country study conducted in middle income countries, the prevalence of multimorbidity ranged from 3.9% in Ghana to 33.6% in Russia [12]. While in LMICs the prevalence of multimorbidity showed a wide variation ranging from 3.2–90.5% [23]. Moreover in a study conducted in Bahirdar city, Ethiopia, the prevalence of NCD multimorbidity was 54.8% (CI = 52.2%, 57.4%) where 39.6% had two NCDs and 15.2% had more than three NCDs [24]. Similarly, a study from Hawassa, Ethiopia indicated that (17.8%) of participants had NCD multi-morbidity [22].
The burden of multimorbidity presents substantial financial burden on patients and healthcare systems worldwide. As compared to a singles NCD, the financial risk due to NCD multimorbidity is resulting severe economic consequences for patients and their household where it is associated with a substantially higher likelihood of experiencing CHE (AOR = 1.29) [25]. Similar evidences showed that the risk of financial hardship increase as the number of disease conditions increase, for each additional chronic disease increases the likelihood of a household facing a financial burden due to OOP payment increases by 46% [26]. Furthermore, multimorbidity also has a policy level implication where majority countries total health expenditure is being spent for patients with multimorbidity [13, 18].
In Ethiopia, As stated in the National Health Account, 2019/20, from the total health expenditure, OOP by households accounts for 30.5% [8]. These burden of OOP payments can lead to significant financial distress, affecting both the utilization of healthcare services and the overall health status of patients [27].
As a result of high OOP payment, considerable proportion of households face CHE. This financial burden can discourage patients from seeking necessary medical care, resulting in delayed diagnoses and treatments, which are particularly critical for managing NCDs. A study conducted in Ethiopia that assessed the cause of medical costs observed substantial burden due to OOP for direct medical costs for a large number of NCDs (e.g., ischemic heart disease, asthma, stroke) which led the population to substantial poverty [28]. Inadequate financial protection can lead to poor health outcomes for NCD patients as they may forego treatment or rely on less effective, informal care options due to cost constraints [27].
The limited coverage of health insurance forced patients to pay substantial amounts of OOP expenditure for consultations, medications, and other related healthcare services [29]. In LMICs, the coping strategies adopted by households who faced CHE such as borrowing money, selling assets, or reducing expenditure on essential needs like food and education has a long term effects on household wellbeing. This will create a inequalities with regard to healthcare access making patients more vulnerable [30].Even though there are studies that are conducted on the financial burden of different single NCD conditions [27, 29, 31, 32], to the best of our knowledge, there is no study or comprehensive studies done regarding the financial risk of NCD multimorbidity and the extent of CHE. Therefore, the study aimed to examine the level of catastrophic out-of-pocket health expenditure associated with NCD multimorbidity and its determinant factors. Finding from this study provides current evidence related to magnitude of CHE due to OOP payment for the treatment of NCD multimorbidity and it adds an input to fill the information gap on the issue.
Methods
Study setting and design
Facility based cross sectional study was conducted at Tikur Anbesa Specialized Hospital (TASH) which is largest specialized and teaching hospital in Addis Ababa Ethiopia. The hospital offers diagnosis and treatment for approximately 370,000 to 400,000 patients annually by receiving patients who are referred from different health facilities in Addis Ababa or across the [31, 33]country [33]. The study was conducted from 18th May to 22th July 2020 among NCD patients attending follow-up appointments at TASH.
Eligibility criteria
All NCD multimorbid patients who came to NCD departments of TASH for a regular follow up during the time of data collection were included in the study. Whereas patients who get health service cost reimbursement by their employer and multi morbid patients who have a communicable disease as one of their disease conditions were not be included in this study.
Sampling and sampling procedures
The sample size was calculated using the single population proportion formula. Since no prior study exists on the level of CHE among NCD multimorbid patients, authors agreed to use a proportion of 0.5 in order to maximize the sample size. A 10% non-response rate was also considered. After applying the formula and adjusting for non-response, the final calculated sample size was 423.
The total sample size was proportionally allocated for the four NCD units found at the hospital based on their patient load in the previous year. Based on the allocation, 124 samples were given for the oncology clinic, 126 samples for the cardiac clinic, 101 samples for the renal clinic and 69 samples for the diabetic clinic (Fig. 1). A sampling frame was prepared for each NCD clinic by reviewing patient appointment log book found at each OPD and patients who have been appointed or expected to visits that particular OPD during the data collection period were identified. Then the populated list of patients was then screened if they have a single NCD or more than one NCD by refereeing the patent registration book using their medical recording number. Following to that, using the final list of multimorbid patients, the allocated sample was selected using a systematic random sampling.
Data collection procedures
Data was collected using pretested, trained interviewer-administered structured questionnaire. The questionnaire was adapted from a tool from WHO “Study on Global Ageing and Adult Health (SAGE) individual questionnaire” [34] and from a study on “Out-of-pocket expenditures for prevention and treatment of cardiovascular disease in general and specialized hospitals in Addis Ababa, Ethiopia” [29].
The questionnaire included: general socio-demographic and socioeconomic characteristics of participants, health care utilization status, insurance status, number of NCDs that the patients are having, monthly OOP health expenditure for treatment of their chronic non-communicable conditions, monthly household consumption expenditure questions. Initially, the questionnaire was prepared in English, then translated into Amharic for better communication with respondents, then translated back to English by a different person to ensure consistency. Data were collected by four data collectors who are health professionals with BSc degree, in a face-to-face interview with our respondents.
To ensure the quality, five days intensive training was provided for the data collectors; the principal investigator strictly supervised the overall data collection process. The questionnaire was pretested on 5% of the sample. The data was also reviewed and checked for completeness and clarity by the supervisor and principal investigator prior to data entry.
Variables
In this study the dependent variable were CHE and independent variables were age, sex, marital status, employment status, educational status of the respondent and wealth quintile group of the household, insurance status, umber of NCD, number of OPD visit, hospitalization status, type of health facility visited.
Variable measurements
Out-of-pocket health expenditure
In the study, direct medical and non-medical out of pocket expenditures were measures by asking patients how much they have paid at point of care for medical care purpose such as for consultation/registration, diagnosis, medication, physiotherapy, inpatient services, and other medical expenses were recorded. the direct non-medical cost were cost for transportation and accommodation and other non-medical expenditures.
Yearly OOP expenditure for outpatient service was calculated by multiplying respondents’ OOP expenditure for one OPD visit with the number of total OPD visits the respondents have done in the past 12 months. Hospitalization OOP payment was calculated the same way by adding OOP payment for a recent IPD admission within the past 12 months and multiplying by the number of IPD admissions. All expenses were reported in ETB and exchanged to USD using average exchange rate on May to July 2020 where 1 ETB was equivalent to 0.0289 USD.
Catastrophic health expenditure
We defined a household as facing CHE when a percentage of the household’s OOP health payments above a specified threshold. The threshold levels considered for calculation of catastrophic payments may differ according to country context [32, 35].In this study, we used total household consumption expenditure and non-food expenditure as a denominator to measure catastrophic health expenditure by using different thresholds as a cutoff point (5%, 10%, 15%, 20%, 25%, and 40% of both total household consumption expenditure and non-food expenditure ).
-
Therefore:
We calculated CHE by using Wagstaf and Van Doorslaer approach where CHE headcount is the percentage of households incurring CHE and it measures the magnitude of catastrophic health expenditure[36]
CHE overshoot was measured to understand the average degree to which the OOP expenditure exceed the given threshold by using the following formula
Mean positive overshoot (MPO) was calculated to which capture the intensity of CHE by dividing overshoot by headcount. MPO indicates the average percentage of OOP medical expenditure in excess of the threshold among households incurring CHE [36].
Operational definitions
Household food expenditure
Patient reported monthly household expenditrue for food items were changed to annual food expenditrue Multimorbidity in this study multimorbidity was defined as the presence of more than one of the listed disease condition such as, hypertension, diabetes mellitus, arthritis, asthma, cataract, mental illness, malignancy, stroke, chronic kidney disease, and heart disease, in one individual. The reported co morbidity were counted to label as multimorbidity.
Wealth quintile
Five wealth quintiles were constructed using principal component analysis by household assets such as livestock, type of house, and durable, productive assets.
Household non-food expenditure
Patient reported monthly household expenditrue for non food items were changed to annual food expenditrue.
Out - of - pocket payments
Are payments made by households at the point of using any health goods or services offered by provider, without reimbursement from a third party.
Data analysis procedures
Data was exported to STATA version 14 for analysis and descriptive statistics including proportion, percentage, frequency distribution, mean and standard deviation were used to summarize the data. Tables, bar and pie charts were used to present study findings. Binary logistic regression model were implemented to identify factors associated with incurring CHE at different denominators and cutoff threshold. Odds ratio with 95% Confidence interval was used to measure the strength of association between dependent and independent variables by using P-value < 0.05 to determine the level of statistical significance. Two regression models were applied to see association between the dependent variables and determinant factors. Assumptions of logistic regression was assessed by checking if our response variable takes only two outcomes, and all the data points are from independent observation. Multicollinearity test was done to check if there is correlation between independent variables where we assured there is no multicollinearity with a VIF value of 2.16 for model 1 and 1.45 for model 2.
Model 1
Model 2
Ethical consideration
Ethical clearance was obtained from the Institutional Review Board of Addis Ababa University College of Health Sciences, School of Public Health. After approval of the IRB, verbal informed consent from each study participants was attained. The interview was undertaken with privacy. Respondent’s name and identification were not mentioned to ensure the confidentiality of the study. Our participants were assured that they can withdraw from the interview at any time they want, and this study will not cause harm to participants except for taking a few minutes of their time.
Results
Characteristics of participant
In this study, 392 patients who came to the NCD clinics of TASH from May to July 2020 were identified and included with a response rate of 92.6%. From the total 48.7% (191) were male and the mean age was 51 years with minimum of 24 and maximum of 82 years. Also 284 (72.4%) of them were married and 105(26.8%) completed college or university. The majority 295(75.3%)lives in Addis Ababa and 240 (61.2%) of them were unemployed (Table 1).
Clinical information
Regarding participants self-reported health condition, 159(40.56%) of them reported having relatively medium health conditions while 18(4.59%)mentioned they have very poor health conditions. Hypertension and diabetic mellitus were reported by 271 (69.13%) and 230 (58.69%) of participants respectively. Whereas fewer respondents had asthma 25 (6.38%)and mental illness 17 (4.34%) respectively (Table 2). As depicted on Fig. 2, majority participants 241 (61.7%) had 2 NCDs, 103 (26.2%)3) of them had 3 NCDs and four participants (1.02%) had 7 NCDs.
Health care utilization
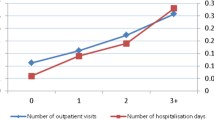
Every participant has a medical follow up at TASH, 24% of respondents had a regular follow up every month and 21% has every six months. The average, outpatient visits done by these multimorbid participants were 6.8 times (95% CI: 6.5, 7.2). Regarding hospitalization status, 133 (33.93%) were admitted to the hospital, among those admitted, the average number of admission were 1.5 times (95%CI: 1.41, 1.75). For one hospital admission, the average length of stay was 14.1 days (95%CI: 12.6, 15.6). Over the study year, 246 (62.76%) participants visited only public facilities while the rest 146 (37.24%) went to both public and private health facilities.
Out of pocket health expenditure
The total annual OOP spending for the treatment of NCD multimorbidity was $499.7 (95%CI: $440.9, $558.6) per patient. Mean OOP expenditure for one outpatient visit was $460.7(95%CI: $406.4, $515) per patient. Relatively increased amount of money was spent for medications $25.3 (95% CI: $22.8, $27.8) and diagnosis $17.2 (95% CI: $ 14.9, $ 19.4) where relatively lower money was paid for registration (Fig. 3). The 33% respondents that had been admitted to the hospital on average one patient paid $ 538.5 (95%CI: $488.7, $588.4) for one admission and increased amount of money was paid for hospital beds $21.6 (95%CI: $10.1, $33.2) followed by medications $11.3 (95%CI: $8.0, $14.7) (Fig. 4).
Incidence and intensity of CHE
The magnitude of CHE differs as we changed the denominator and the cutoff point. From the total respondents, the proportion of households facing CHE as a share of total household consumption expenditure decreased from 77.55 to 10.46% as the threshold increased from 5 to 40%. For CHE as a share of household non-food expenditure, the proportion decreased from 91.84 to 28.32%, as the threshold increased from 5 to 40% (Table 3).
Finding from the conducted regression analysis indicated that, at 40% cut off point of total household nonfood expenditure, living outside of Addis Ababa (AOR = 7.45,95%CI:3.41–16.27), not being a member of an insurance scheme(AOR = 4.97,95%CI: 2.37,10.4), having an increased number of NCDs (AOR = 2.05, 95% CI:1.40, 3.01), having increased number of outpatient visits (AOR = 1.46 ,95%CI; (1.31, 1.63) had an increased odds of incurring CHE (Table 4).
For CHE at the 10% threshold level of OOP health payment as a share of total household consumption expenditure, the likelihood of facing CHE was more for those who live outside of Addis Ababa (AOR = 7.35, 95%CI: 2.99,18.06), households who were not an insurance scheme member (AOR = 7.3 95%CI: 3.56,14.9), a household with a member having an increased number of NCDs (AOR = 2.82,95%CI; (1.72 ,4.62), having increased number of outpatient visits (AOR = 2.04,95%CI;1.71,2.42). Further getting a heath care service both at public and private facilities had 2.47 times more increased likelihood of facing CHE as compared to those who went to only public health facilities (AOR = 2.47, 95%CI: 1.18,5.14) (Table 5).
Discussion
This study aimed to evaluate the CHE due to NCD multimorbidity. Based on our findings, the proportion of CHE as a share of total household consumption expenditure with 5% and 10% cutoff threshold was 77.5% and 56.12% respectively. Similarly, the proportion of CHE as a share of household non-food expenditure was 46.68% and 28.32% with 25% and 40% threshold. We have also idenitfed some imrotantr variables that contriute for the CHE occurance, such as place of residency, the number of NCDs, the type of health facility utilized, the number of outpatient treatment visits, and the insurance status of the household.
In defining the term multimorbidity, many literatures agree that, it is the co-occurrence of more than one chronic condition in one individual. But there is no uniform agreement on the list of these chronic disease conditions that has to be used in defining and classifying patients as multimorbid [13].There is also no consensus on denominator and cutoff points to define CHE [32]. Different literature uses different approaches. For these reasons, comparison between studies was challenging.
Studies have shown that having multiple chronic NCDS diseases can lead to increased health care cost. A cross-sectional study conducted in India found that respondents with more than two NCDs incurred a significantly higher amount of OOP expenses. Similarly, in Switzerland, an observational study found that health costs were 5.5 times higher in multimorbid patients. In addition, 32.6% more cost was added for each additional NCD condition. [15, 20].
There is evidence to suggest as the number of additional NCDs increase there is a higher healthcare costs and increased out-of-pocket expenses for households. Studies conducted in Australia and Spain have supported this finding, showing a correlation between the number of chronic conditions and an increase in out-of-pocket expenses for medical and health-related purchases. [18, 26, 38]. this implies that individuals with multimorbidity incur higher healthcare costs compared to those with a single chronic disease. This could be attributed to the consumption of multiple medications, the need for frequent and extensive medical investigations, increased visits to healthcare facilities, and a higher likelihood of complications, which further contribute to higher costs.
Despite differences in the calculation of CHE and cut-off thresholds, the findings of this study is in line with global trends where the economic burden of NCDs is becoming a serious publc health concern. We discovered that multimorbid patients face CHE at varying levels of OOP payment for health services and cut-off points. Studies found that NCDs contribute to substantial OOPE which mostly led to CHE and impoverishment. according to a Pakistani study on hypertension and diabetes patients, average OOPE expenditure, as a percentage of total household consumption expenditure, was 60% higher for households with a member having multiple conditions compared to households with only one NCD. [39]. Similarly, findings from China and India also supported our finding where multimorbid patients have substantially higher likelihood of experiencing CHE( with AOR = 1.29(95% CI: 1.26, 1.32) in China and (β = 0.53, ρ < 0.00) in India [25, 40]. This finding adds to the broader evidence on financial challenges related to NCDs and raising important questions about the effectiveness of current healthcare financing strategies and its implication on the population’s economic burden related to NCDs.
The study has revealed that i family member residing outside of Addis Ababa who requires treatment for NCD conditions, are more likely to face CHE (with a p-value < 0.001). This finding is consistent with studies conducted in four other LMICs - Argentina, China, India and Tanzania - which have also reported a significant positive correlation between the place of residency and facing CHE(AOR = 2.69, 95% CI:1.31–5.53 [41]. Similarly in Kenya, households that were located outside the city and came to get health care service are more likely to experience CHE (OR = 1.38, 95% CI 1.14–1.67) [42].
Findings from this study was also supported by a study in Addis Ababa on CHE for CVD treatment, that showed traveling to Addis Ababa for health care significantly increased the chance of facing CHE (AOR = 3.25,95%CI:1.79–5.90) [29]. It is known that multiple NCDs can lead to complications demanding advanced and specialized care. In the context of LMICs, this level of care is often unavailable in proximity as a result patients may need to travel to the city, thus causing a delayed care that will further worsen the patient’s condition and increase the need for more advanced care and increased chances of incurring CHE.
It has been observed through studies that uninsured households are more likely to face catastrophic payments. This has also been shown in a study conducted in Iran where it was found that health insurance reduces the chance of households facing CHE. Another study conducted in China showed that catastrophic payments occurred more frequently in patients without health insurance when compared to those with health insurance. Similarly, in Northeast Ethiopia, insured households were 81% less likely to encounter catastrophic health expenses compared to non-insured households. However, in Turkey, uninsured households had a relatively lower risk of catastrophic payment [43,44,45,46]. This variation may be due to the difference in the implementation mechanism, the extent and nature of health services covered by insurance, coverage, and protective capacity of the insurance schemes applied among countries.
According to this study, the presence of an additional NCD increases the likelihood of incurring CHE by 2.05 and 2.82 times, resulting in 40% of household consumption expenditure and 10% of household non-food expenditure respectively. These findings are consistent with a similar study conducted in Bangladesh, which showed that for every additional chronic illness, there is a 1.47 times higher risk of incurring catastrophic payments [47]. Studies conducted in China and Australia have shown that health care costs are directly proportional to the number of chronic NCD conditions a person has [26, 48]. This means that households with an increased number of such conditions are more likely to face CHE as the cost of healthcare becomes significantly higher.Since each additional NCD typically requires ongoing medical care, such as medications, consultations, and possible hospitalizations, the cost of care escalate when multiple chronic conditions are present within a household. Moreover, decreased productivity and income loss for affected individuals and their caregivers, further exacerbates the financial strain on households, making it harder to meet their healthcare expenses without forgoing other essential needs.
The study found a strong link between households that visited both private and public hospitals and experiencing CHE that exceed 10% of their total household consumption expenditure. This is consistent with a similar study conducted in Bangladesh, which showed that households that utilized both public and private facilities were at a higher risk of facing CHE [47]. Additionally, a study conducted in Addis Ababa supports the findings of this research. It revealed that seeking medical care at private hospitals increased the likelihood of CHE by 20 times (OR = 20.7, 95%CI; 10.2–42.04, p value < 0.001) [29]. This suggests that some private health facilities may have higher prices for their services compared to public health facilities, leading to higher payments and possibly overpriced services.
As per our finding, for every additional health facility visit, the odds of facing CHE increased by 1.46 to 2.04 times, which is consistent with a study conducted in Iran. The study showed that each additional health care service obtained increases the chance of CHE by 1.5 times [49]. Therefore, if people have more visits to health facilities, they may end up paying more out-of-pocket money and face CHE, which, in turn, will increase the indirect cost. In our study setting, multimorbid patients visit the health facility separatly for each of their specific disease conditions. Therefore, in similar setting where integrated NCD care delivery method is not available, the risk of facing CHE could be substantial.
This study is significant for the scientific community as it sheds light on an area that has previously received little attention. The research brings to light the problems that NCD patients face, which have not been explored before. However, there are some limitations to the study, such as the fact that it was conducted in a healthcare facility, and some respondents found it difficult to answer questions related to household consumption expenditure. A household survey may have been more appropriate. Additionally, since the data was collected retrospectively, responses, such as household consumption expenditure and health care utilization may be subject to recall bias. Similarly, since we have a estimated the cost data using cost from a single visit the annual cost data might not be the exact amount. Furthermore, the study did not adequately represent patients who came from outside of Addis Ababa to seek medical follow-up. This gap could be filled by conducting further national level research.
Concussion and recommendations
Multimorbid patients come to health facilities more frequently and they are exposed to increase financial problems. CHE mostly affected those family members who come from out of Addis Ababa to get health care services, those who have increased number of NCD conditions, household who were not a member of an insurance system, those who use both public and private health facilities, and patients who visit health facility more frequently were affected by CHE.
The financial strain associated with having multiple disease conditions that require lifelong care in resource limited setting is a serious challenge and barrier in achieving the UHC. Therefore, there is a need for comprehensive healthcare restructurings to ease the financial burden of NCD multimorbidity on households particularly in low-resource settings like Ethiopia. finical risk protection policies should be evaluated and revised if they are truly protecting the community form finical hardships.
To reduce OOP expenses related to non-medical costs, an integrated approach to NCD care service delivery can be applied. This can help improve patient outcome, reduce the need for frequent health faculity visits and the associated costs.
Our findings show that medications and diagnostic services are the primary cost drivers for OOP expenses. To reduce costs, affordable medications and diagnostic services should be made available in public facilities. Additionally, efforts should be made to ensure that NCD care services are available across the country, so that patients do not have to travel to the capital city for healthcare services.
Further research is needed on a larger scale, including private facilities and regional states, to identify the NCD combinations that cause the greatest financial burden on households. This will help generate more evidence to identify prominent NCDs among the population and take measures to reduce the financial impact.
Data availability
The datasets generated during the current study is available from the corresponding author on reasonable request.
Abbreviations
- AA:
-
Addis Ababa
- CHE:
-
Catastrophic Health Expenditure
- CNCD:
-
Chronic Non Communicable Disease
- COPD:
-
Chronic Obstetric Pulmonary Disease
- CVD:
-
Cardiovascular Disease
- DM:
-
Diabetic Mellitus
- ETB:
-
Ethiopian Birr
- HH:
-
Household
- HICs:
-
High-Income Countries
- IPD:
-
Inpatient Department
- LMICs:
-
Low and Middle-Income Countries
- NCD:
-
Non Communicable Disease
- OPD:
-
Out Patient Department
- OOP:
-
Out - Of–Pocket
- SDG:
-
Sustainable Development Goal
- TASH:
-
Tikur Anbesa Specialized Hospital
- WHO:
-
World Health Organization
References
Metrics, IfH. Evaluation. Findings from the global burden of disease study 2017. Lancet [Internet]. 2018.
Bank W. Estimated deaths by cause and region, 2000 and 201. World Bank; 2016.
Global Burden of Disease Study. 2019. GBD 2019.
Jan S, Laba T-L, Essue BM, Gheorghe A, Muhunthan J, Engelgau M, et al. Action to address the household economic burden of non-communicable diseases. Lancet. 2018;391(10134):2047–58.
Organization WH. Tracking universal health coverage: 2017 global monitoring report. 2017.
Organization WH. Noncommunicable diseases country profiles 2018. 2018.
Bollyky TJ, Templin T, Cohen M, Dieleman JL. Lower-income countries that face the most rapid shift in noncommunicable disease burden are also the least prepared. Health Aff. 2017;36(11):1866–75.
Health FDRoEMo. ETHIOPIA HEALTH ACCOUNTS REPORT 2019/20. Ethiopia Federal Democratic Republic of Ethiopia Ministry of Health, Partnership and Cooperation Directorate; 2022.
Organization WH. Tracking universal health coverage: first global monitoring report. World Health Organization; 2015.
Bank W. Out-of-pocket expenditure (% of current health expenditure) World Bank Data Set 2023 [Available from: worldbank.org.
Azzani M, Roslani AC, Su TT. Determinants of Household Catastrophic Health expenditure: a systematic review. Malays J Med Sci. 2019;26(1):15–43.
Lee JT, Hamid F, Pati S, Atun R, Millett C. Impact of Noncommunicable Disease Multimorbidity on Healthcare Utilisation and Out-Of-Pocket expenditures in Middle-Income countries: Cross Sectional Analysis. PLoS ONE. 2015;10(7):e0127199.
Wang L. The health and economic burden of multimorbidity in Australia. University of Tasmania; 2017.
MacMahon S, Calverley P, Chaturvedi N, Chen Z, Corner L, Davies M, et al. Multimorbidity: a priority for global health research. London, UK: The Academy of Medical Sciences; 2018.
Pati S, Agrawal S, Swain S, Lee JT, Vellakkal S, Hussain MA, et al. Non communicable disease multimorbidity and associated health care utilization and expenditures in India: cross-sectional study. BMC Health Serv Res. 2014;14(1):451.
Nguyen TN, Ngangue P, Bouhali T, Ryan BL, Stewart M, Fortin M. Social Vulnerability in patients with multimorbidity: a cross-sectional analysis. Int J Environ Res Public Health. 2019;16(7).
Navickas R, Petric VK, Feigl AB, Seychell M. Multimorbidity: what do we know? What should we do? J Comorb. 2016;6(1):4–11.
Orueta JF, Garcia-Alvarez A, Garcia-Goni M, Paolucci F, Nuno-Solinis R. Prevalence and costs of multimorbidity by deprivation levels in the basque country: a population based study using health administrative databases. PLoS ONE. 2014;9(2):e89787.
Mini GK, Thankappan KR. Pattern, correlates and implications of non-communicable disease multimorbidity among older adults in selected Indian states: a cross-sectional study. BMJ Open. 2017;7(3):e013529.
Bahler C, Huber CA, Brungger B, Reich O. Multimorbidity, health care utilization and costs in an elderly community-dwelling population: a claims data based observational study. BMC Health Serv Res. 2015;15:23.
Déruaz-Luyet A, N’Goran AA, Senn N, Bodenmann P, Pasquier J, Widmer D et al. Multimorbidity and patterns of chronic conditions in a primary care population in Switzerland: a cross-sectional study. BMJ open. 2017;7(6).
Woldesemayat EM, Kassa A, Gari T, Dangisso MH. Chronic diseases multi-morbidity among adult patients at Hawassa University Comprehensive Specialized Hospital. BMC Public Health. 2018;18(1):352.
Abebe F, Schneider M, Asrat B, Ambaw F. Multimorbidity of chronic non-communicable diseases in low-and middle-income countries: a scoping review. J Comorbidity. 2020;10:2235042X20961919.
Eyowas FA, Schneider M, Balcha SA, Pati S, Getahun FA. Multimorbidity and health-related quality of life among patients attending chronic outpatient medical care in Bahir Dar, Northwest Ethiopia: the application of partial proportional odds model. PLoS Global Public Health. 2022;2(11):e0001176.
Zhao Y, Atun R, Oldenburg B, McPake B, Tang S, Mercer S et al. Multimorbidity, Health Service Use and Catastrophic Health Expenditure by Socio-Economic Groups in China: A Panel Data Analysis. Health Service Use and Catastrophic Health Expenditure by Socio-Economic Groups in China: A Panel Data Analysis (08/19/2019 06: 25: 50). 2019.
McRae I, Yen L, Jeon YH, Herath PM, Essue B. Multimorbidity is associated with higher out-of-pocket spending: a study of older australians with multiple chronic conditions. Aust J Prim Health. 2013;19(2):144–9.
Kasahun GG, Gebretekle GB, Gecho YH, Woldemariam AA, Fenta TG. Catastrophic Healthcare Expenditure and Coping Strategies among Patients Attending Cancer Treatment Services in Addis Ababa, Ethiopia. 2020.
Verguet S, Memirie ST, Norheim OF. Assessing the burden of medical impoverishment by cause: a systematic breakdown by disease in Ethiopia. BMC Med. 2016;14(1).
Tolla MT, Norheim OF, Verguet S, Bekele A, Amenu K, Abdisa SG et al. Out-of-pocket expenditures for prevention and treatment of cardiovascular disease in general and specialised cardiac hospitals in Addis Ababa, Ethiopia: a cross-sectional cohort study. BMJ global health. 2017;2(2).
Rahman T, Gasbarro D, Alam K. Financial risk protection from out-of-pocket health spending in low-and middle-income countries: a scoping review of the literature. Health Res Policy Syst. 2022;20(1):83.
Aster E, THE FINANCIAL BURDEN OF OUT. OF POCKET EXPENDITURE FOR TREATMENT OF DIABETIC MELLITUS IN ADDIS ABABA. 2018.
Hailemichael Y, Hailemariam D, Tirfessa K, Docrat S, Alem A, Medhin G, et al. Catastrophic out-of-pocket payments for households of people with severe mental disorder: a comparative study in rural Ethiopia. Int J Ment Health Syst. 2019;13:39.
Addis Ababa Uinversity College of Health Sciences Background of Tikur Anbessa Hospital. 2020 [ http://www.aau.edu.et/chs/tikur-anbessa-specialized-hospital/background-of-tikur-anbessa-hospital/
Organization WH. STUDY ON GLOBAL AGEING AND ADULT HEALTH Individual Questionnaire Wave 1 Set A.
Xu K, Evans DB, Kawabata K, Zeramdini R, Klavus J, Murray CJL. Household catastrophic health expenditure: a multicountry analysis. Lancet. 2003;362(9378):111–7.
Wagstaff A, Doorslaer E. Catastrophe and impoverishment in paying for health care: with applications to Vietnam 1993–1998. Health Econ. 2003;12(11):921–33.
Sancho-Mestre C, Vivas-Consuelo D, Alvis-Estrada L, Romero M, Uso-Talamantes R, Caballer-Tarazona V. Pharmaceutical cost and multimorbidity with type 2 diabetes mellitus using electronic health record data. BMC Health Serv Res. 2016;16(1):394.
Glynn LG, Valderas JM, Healy P, Burke E, Newell J, Gillespie P, et al. The prevalence of multimorbidity in primary care and its effect on health care utilization and cost. Fam Pract. 2011;28(5):516–23.
Datta BK, Husain MJ, Asma S. Assessing the relationship between out-of-pocket spending on blood pressure and diabetes medication and household catastrophic health expenditure: evidence from Pakistan. Int J Equity Health. 2019;18(1):9.
Pradhan J, Dwivedi R, Banjare P. Relying on whom? Correlates of out of pocket health expenditure among the rural elderly in Odisha, India. Ageing Int. 2017;42(3):306–23.
Huffman MD, Rao KD, Pichon-Riviere A, Zhao D, Harikrishnan S, Ramaiya K, et al. A cross-sectional study of the microeconomic impact of cardiovascular disease hospitalization in four low- and middle-income countries. PLoS ONE. 2011;6(6):e20821.
Barasa EW, Maina T, Ravishankar N. Assessing the impoverishing effects, and factors associated with the incidence of catastrophic health care payments in Kenya. Int J Equity Health. 2017;16(1):31.
Rezapour A, Arabloo J, Tofighi S, Alipour V, Sepandy M, Mokhtari P et al. Determining equity in household’s health care payments in Hamedan province, Iran. 2016.
Heeley E, Anderson CS, Huang Y, Jan S, Li Y, Liu M, et al. Role of health insurance in averting economic hardship in families after acute stroke in China. Stroke. 2009;40(6):2149–56.
Mekonen AM, Gebregziabher MG, Teferra AS. The effect of community based health insurance on catastrophic health expenditure in Northeast Ethiopia: a cross sectional study. PLoS ONE. 2018;13(10):e0205972.
Ozgen Narci H, Sahin I, Yildirim HH. Financial catastrophe and poverty impacts of out-of-pocket health payments in Turkey. Eur J Health Econ. 2015;16(3):255–70.
Rahman MM, Gilmour S, Saito E, Sultana P, Shibuya K. Health-related financial catastrophe, inequality and chronic illness in Bangladesh. PLoS ONE. 2013;8(2):e56873.
Wang Z, Li X, Chen M. Catastrophic health expenditures and its inequality in elderly households with chronic disease patients in China. Int J Equity Health. 2015;14(1):8.
Kavosi Z, Rashidian A, Pourreza A, Majdzadeh R, Pourmalek F, Hosseinpour AR, et al. Inequality in household catastrophic health care expenditure in a low-income society of Iran. Health Policy Plan. 2012;27(7):613–23.
Acknowledgements
This article was prepared based on the thesis work done by MH and the authors would like to acknowledge the Addis Ababa University’s College of Health Sciences and School of Public Health for making this work possible. We would also want to appreciate the Tikur Anbesa Specialized Hospital administration office and hospital professionals for their assistance. Finally, we like to thank our data collectors for his hard work.
Funding
This study was funded by Addis Ababa University and the funder had no role in the study design, in data collection and analysis, in the interpretation or write-up process.
Author information
Authors and Affiliations
Contributions
This study was conceived by MH and MM, MH developed the original formulation of study and objectives. Regulatory approvals were secured by MH, MM and BT. Data were obtained and supervised by MH with the aid of a team of data collectors. The study was monitored and supervised by MM and BT. MH done data analysis and wrote the original draft of the article and it was revised by MM. All authors read, commented and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
Ethical clearance was obtained from the Institutional Review Board of Addis Ababa University College of Health Sciences, School of Public Health. A formal letter was written to Tikur Anbesa Hospital from the AAU School of Public Health. Additionally, after receiving ethical approval from the IRB of AAU, we have explained the objective and purpose of the study and verbal informed consent from each study subject was obtained. The interview was undertaken with privacy. Respondent’s name and identification were not mentioned to ensure the confidentiality of the study. Our participants were assured that they can withdraw from the interview at any time they want, and this study will not cause harm to participants except for taking a few minutes of their time. All methods were performed in accordance with the relevant guidelines and regulations such as Declaration of Helsinki.
Consent for publication
NA.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Habtemichael, M., Molla, M. & Tassew, B. Catastrophic out-of-pocket payments related to non-communicable disease multimorbidity and associated factors, evidence from a public referral hospital in Addis Ababa Ethiopia. BMC Health Serv Res 24, 896 (2024). https://doi.org/10.1186/s12913-024-11392-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-024-11392-3