Abstract
Background
Many factors can decrease job productivity and cause physical and psychological complications for health care professionals providing maternal care. Information on challenges and coping strategies among healthcare professionals providing maternal healthcare services in rural communities is crucial. However, there needs to be more studies, especially qualitative research, to explore challenges and coping strategies for providing maternal health care services in Ethiopia among health care professionals, particularly in the Wolaita zone.
Objective
To explore the challenges and coping strategies of professionals providing maternal health care in rural health facilities in Wolaita Zone, Southern Ethiopia, in 2023.
Method
A phenomenological qualitative study design was applied from May 20 to June 20, 2023. The study was conducted in rural areas of the Wolaita Zone, southern Ethiopia. Healthcare professionals from rural areas were selected using purposive sampling, and in-depth interviews were conducted. A qualitative thematic analysis was employed to analyze the data. Field notes were read, recordings were listened to, and each participant’s interview was written word for word and analyzed using ATLAS.ti 7 software.
Result
Five main themes emerged from the data analysis. These themes included inadequate funding from the government, societal barriers to health and access to health care, professionals’ personal life struggles, infrastructure related challenges and health system responsiveness, and coping strategies. Reporting to responsible bodies, teaching mothers about maternal health care services, and helping poor mothers from their pockets were listed among their coping strategies.
Conclusion
Healthcare professionals have a crucial role in supporting women in delivering babies safely. This study revealed that they are working under challenging conditions. So, if women’s lives matter, then this situation requires a call to action.
Similar content being viewed by others
Introduction
Maternal health deals with the health and well-being of a woman before pregnancy (pre-conception), during pregnancy (ante-natal), and during and after childbirth (peri- and post-natal) [1]. Maternal health is crucial to maintaining the mother’s and child’s health and well-being. Besides its health benefits, maintaining maternal health can also have economic and social benefits [2].
Maternal health care service has gone through many historical transitions and has faced different challenges starting from the Paleolithic era (40,000 B.C.), in which giving birth occurred in challenging and usually life-threatening environments. During the dark and middle Ages, traditional birth attendants’ roles focused on assessing and managing pain during labor and on maintaining hygienic and comfort status for mothers and their newborns, and they were socially marginalized and excluded. A lot of female healers and traditional birth attendants were sanctioned and tortured by burning or hanging as heretics or witches [3, 4].
Coping strategies refer to an individual’s conscious efforts and actions to cope with stress, adversity, or difficult situations [5]. Nowadays, globally, healthcare providers who provide maternity care in rural areas face numerous obstacles, including inadequate basic infrastructure and equipment [4], a lack of opportunities for ongoing professional development and training, excessive workloads and fatigue, and a lack of resources within the health system [6]. Inadequate infrastructure (lack of beds and physical space), staffing shortages, logistical difficulties, low motivation, and few opportunities for in-service training are among the problems faced by African nations, such as Ghana [7]. The absence of formal arrangements, exceptionally written standards, and policies that clearly define their position as healthcare professionals presents several obstacles for them in Somaliland and has an impact on the quality of care they can give. They also mentioned feeling uneasy about practicing within their professional scope because of challenging cultural norms, customs, and Somaliland’s legal system [8]. In Ethiopia, they mentioned that difficulties with limited resources such as water, medicine, and equipment affect the quality of care they give to women giving birth [9].
Research on the difficulties healthcare workers face is well-documented in high-income countries, but it is far less common in low- and middle-income settings [10]. This study aims to investigate and illustrate healthcare workers’ difficulties when delivering maternal healthcare services. This could make it possible to make decisions based on the HCWs’ observations of the circumstances.
Improving maternal health outcomes in rural areas requires an understanding of these obstacles. This study selected rural areas because studies revealed that HCWs providing maternal care in rural areas face more challenges than HCWs in urban areas [11,12,13]. So, this study is done to fill this gap. More thorough studies must be conducted on the coping strategies medical professionals use to overcome these difficulties, which represents another research gap. Coping strategies are essential for removing obstacles to efficient service provision. Policymakers and healthcare professionals can create focused interventions to support HCWs working in rural areas by recognizing and comprehending these strategies. The data produced from this study is used to show comparison and provide insight into the issue of challenges. Because it makes health center restructuring more effective, it is also beneficial for managers of health centers in the study area.
Methods and materials
Study area and study period
The study was conducted in 4 primary hospitals (Halale, Badessa, Bitana, and Bombe primary hospitals) in rural areas of the Wolaita zone, southern Ethiopia. Wolaita is located in the south part of Ethiopia, at a distance of approximately 339 km (210.65 miles) from Addis Ababa, Ethiopia, in the southwest direction.
According to the most recent information available, Wolaita Zone includes 12 woredas and 4 town administrations, totaling 373 kebeles, of which 294 are rural and 79 are urban (source: Wolaita Zone Administration). There are 419 health facilities according to the zonal health department, which are divided into 8 hospitals (4 in town administrations and 4 in rural woredas), 69 health centers, and 342 health posts. According to the Wolaita Zone Health Department, 1,490 healthcare professionals support the zone.
Each health center operates as a primary health care unit (PHCU) and is accompanied by five satellite health posts. Health centers are designed to cater to approximately 25,000 people, while satellite health posts aim to serve up to 5,000 people each. A referral system links each health post to its associated health center, facilitating access to higher levels of care as needed (source: Wolaita Zone Health Department).
The study period was from May 20 to June 20, 2023.
Study design
A qualitative approach and descriptive phenomenological study design were carried out to explore healthcare professionals’ challenges and coping strategies for providing maternal healthcare services in rural areas of the Wolaita zone. A phenomenological study design approach is chosen because phenomenology concerns studying experience from the individual’s perspective [14, 15].
Study participants
According to Creswell (2009), “phenomenology is a research strategy of inquiry in which the researcher identifies the essence of human experiences about a phenomenon as described by participants. The only legitimate informants in the phenomenological study are participants who have had experience related to the targeted thematic issue of the study [16]. The participants of this study were 12 healthcare professionals working in different rural areas of the Wolaita zone.
Participants recruitment
The recruitment of participants was employed by using criterion (purposive) sampling to obtain deep information on the challenges and coping strategies of health care professionals. From all primary hospitals in rural areas of the Wolaita zone, 12 healthcare professionals were included in the study through in-depth interviews. They were selected from different positions (medical director or MCH coordinator), and experiences (from less than one year up to six years) in the study area to collect rich and diverse data.
The purpose was to get detailed information from those health care professionals who meet the criteria since they have work experience and a great deal of experience in positions, and they can experience the various factors that can affect the health care professionals in providing the health care services that were expected of them in their daily practice.
Twelve healthcare professionals were included in the study through an in-depth interview. The information saturation determined the number of participants, and the in-depth interview was stopped when no new information was present.
Data collection procedure
Before data collection, training on qualitative data collection was given to 4 data collectors (MSc degree students). The data were collected face-to-face using an in-depth interview technique with a semi-structured interview guide. The interview guide was developed by reviewing literature considering the context of the study [17,18,19,20]. To maintain consistency, the tools were translated from English to Amharic. The interview guides include the socio-demographic characteristics of the participants and the challenges and coping strategies of health care professionals providing maternal health care services in rural health facilities of the Wolaita zone. The investigator conducted In-depth Interviews, notes were written, and audio records of the interview were recorded during the interview. Probing was used to ensure the depth and clarification of the information provided during the interview.
Informed oral consent was obtained from all participants, and the in-depth interviews were conducted in the participants’ working areas during their regular working hours. During the interview, the place was convenient which means, in a private location with no outsiders and where study participants felt that their confidentiality was protected. As much as possible to the participants to assure both privacy and confidentiality, data collection was stopped when information saturation was achieved, i.e., data were collected until no new information emerged.
Data analysis
For data analysis, first, the record materials were transcribed verbatim into Amharic and then translated into English by the principal investigator. Field notes were incorporated into the transcription simultaneously. Secondly, the transcribed data were translated from Amharic to English independently by replaying the voice recorder tape and rereading notes; this transcription was stored in Microsoft Word documents. The data transcription started at the same time as the data collection period. Each interview was transcribed verbatim before the next one took place and provided direction for the next one. Thirdly, coding was done through ATLAS.ti 7 software by reading and re-reading the compiled transcripts. Before the actual coding began, investigators independently read the transcripts. As the study was exploratory and descriptive, an inductive coding procedure was applied (themes were derived empirically from data related to our research questions) [21]. Codes were organized to create categories and themes. The fourth step involved the development of themes, which were classified according to the study objectives. An inductive thematic approach was applied [21, 22], in which the text relating to each thematic code was used. Finally, the result was presented using themes and categories, supported by quotes to describe the overall essence of the experience.
Trustworthiness
The trustworthiness of the study was maintained by considering the following criteria: Credibility, Dependability, Transferability, and Conformability [23,24,25],
Credibility
Research activities and processes, data collection and analysis, emerging themes, categories, or quotations were audited by advisors, and colleagues and examined by other person with experience in conducting qualitative research.
Dependability
To assure dependability, instead of relying solely on written notes or memories, audio recordings and field notes were used to provide a more accurate and reliable record of participant responses.
Transferability
The methodology, selection, and recruitment of participants, data collection methods, and the analysis process were clearly described. Data was collected till saturation was reached.
Conformability
To prevent the investigator’s bias, the investigator set aside personal experiences and presumptions to illustrate an accurate picture of the participant’s information.
Result
Socio-demographic characteristics
As shown in Table 1 below, among 12 study participants from different rural health facilities in the Wolaita zone, 7 were midwives, and 5 were other professionals (including two medical directors and three maternal and child health care coordinators). Most of the participants were between the ages of 27 and 30 years, with their working experience ranging from less than one year to 6 years. The majority of participants were male and single.
Themes and categories
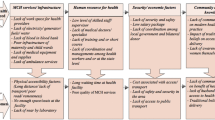
This study explored 5 main themes and 21 categories.
Theme 1: Inadequate government funding
During the interviews, participants consistently voiced their primary concern: inadequate funding from the government. This overarching theme encompassed various sub-themes, including delayed salary and duty payments, shortages of human and material resources, and issues with infrastructure.
Sub-theme 1: Delayed salary and duty payments
A pressing issue highlighted by all participants was the chronic delay in salary and duty payments, particularly affecting those employed in the public sector. This financial instability caused significant hardships among healthcare providers, affecting their motivation and productivity.
One participant, a midwife with six years of experience, expressed frustration:
“Our salary is too small, and without duty payment, it is not enough even to fulfill our basic needs… Due to this, sometimes we feel unmotivated and lose energy to work. We haven’t received our duty payment for two years, and sometimes they delay our monthly salary too… An employee should be paid for his or her job; this is not fair… Married professionals are living with their children; how can they raise their babies? And how can we work in this situation?”
The impact of delayed payments was also noted by a medical director:
“Some professionals stopped working for a while. They returned when Woreda’s administrator promised them to pay their duty… But still, they didn’t receive their duty payment… Now they are not working in the night session, so as the medical director of this primary hospital, if something bad happens, I will be asked, so I work in the night session in addition to my job….”
Sub-theme 2: Shortage of human resources
A critical consequence of inadequate funding is the shortage of human resources in healthcare facilities. This shortfall includes essential professionals such as nurses, doctors, and support staff. Participants emphasized how these shortages strain the healthcare system, leading to longer patient wait times, compromised care quality, and increased workloads for already-stretched staff members.
A medical director highlighted the staffing challenges: “The number of midwives in our hospital is inadequate; however, our budget doesn’t allow us to hire additional staff members.”
Sub-theme 3: Material resource scarcity
Inadequate government funding also manifests in material resource scarcity, further complicating healthcare delivery. Participants cited deficiencies in essential supplies, which directly impact patient outcomes. For instance, the shortage of family planning options was noted as a barrier to maternal health services.
A midwife expressed concerns about resource shortages: “We face challenges such as shortages of essential resources. Family planning services, crucial for maternal health care, are hindered by a lack of intrauterine devices and other contraceptive options.”
Similarly, a manager highlighted infrastructure limitations: “Our hospital has only two ambulances, which is insufficient. The inadequate budget prevents us from acquiring more ambulances to meet our needs.”
Sub-theme 4: Poor construction
Inadequate government funding often results in poorly constructed healthcare facilities, which directly impact maternal health services. Substandard infrastructure can hinder efficient treatment delivery and compromise patient care quality.
Participants highlighted structural issues affecting service delivery: “During the rainy season, water seeps into our hospital rooms through the roof’s pores. Despite the hospital’s attractive exterior, internal conditions pose significant challenges”, remarked a medical director with three years of experience.
Another participant emphasized the facility’s construction challenges: “Our hospital, established just a year ago, faces numerous issues due to poor construction. Room partitions made of metal contribute to uncomfortable conditions, particularly on sunny days when the rooms become excessively warm”, noted an MCH coordinator with less than one year of experience.
Theme 2: Societal barriers to health and access to healthcare
Under this theme, several sub-themes were identified that contribute to challenges in accessing healthcare: lack of awareness, poverty, distance from healthcare facilities, rumors from neighbors, and blaming professionals.
Sub-theme 1: Lack of awareness
A significant barrier identified by participants is the lack of awareness about healthcare services and preventive measures. This ignorance often leads to delays in seeking medical attention and exacerbates health conditions.
An MCH coordinator with 4 years of experience shared: “Mothers often feel uncomfortable with procedures like vaginal examinations and may refuse them, making it challenging to provide adequate care.”
Similarly, a midwife with six years of experience noted: “Due to limited awareness of childbirth procedures, some mothers opt for home births, leading to complications like postpartum hemorrhage.”
Sub-theme 2: Poverty
Poverty emerges as a major barrier to healthcare access, affecting the ability to afford medications and necessary medical supplies. Financial constraints force individuals to delay or forego essential medical treatments, exacerbating health disparities.
A midwife with five years of experience highlighted the issue: “Mothers sometimes lack funds to purchase basic medical supplies like syringes and gloves, which are essential for safe delivery practices.”
Another midwife, with less than one year of experience, added: “Despite the presence of pharmacies, many mothers cannot afford to buy prescribed medications, affecting their treatment outcomes.”
Sub-theme 3: Distance from healthcare facilities
Geographic distance presents a significant challenge for mothers residing in rural or isolated areas, limiting their access to healthcare services. Participants highlighted the difficulties faced when seeking routine care or urgent medical attention due to inadequate transportation options and long travel times.
A midwife with four years of experience expressed concerns: “It’s challenging to ensure quality care for women because many mothers live far from our hospital. Some end up giving birth en route to the healthcare center, missing out on essential antenatal care.”
Another participant noted the distance to referral hospitals: “Our institution is located far from the nearest referral hospital (Otona Referral Hospital), complicating timely access to specialized care for mothers.”
Sub-theme 4: Rumors from neighbors
Community rumors and social pressures contribute to misinformation and mistrust towards healthcare facilities and procedures. False perceptions propagated through word-of-mouth can deter individuals from seeking necessary medical care, leading to preventable health complications.
According to a MCH coordinator with four years of experience: “Some mothers choose home births due to negative rumors spread by neighbors about healthcare professionals and hospital deliveries. This delay in seeking care results in complications like retained placentas.”
Sub-theme 5: Blaming professionals
Misunderstandings and misconceptions about medical practices can lead to blame directed at healthcare professionals, hindering effective patient-provider interactions and adherence to medical advice.
A midwife with five years of experience shared her perspective: “Sometimes, clients misunderstand our recommendations, such as referring mothers with previous C-section scars to referral hospitals for safer deliveries. They blame us for their dissatisfaction or health complications, which undermines our morale, especially amidst delays in duty payments.”
Theme 3: Personal life struggles of healthcare professionals
Healthcare professionals working in rural areas face numerous challenges that indirectly impact maternal healthcare services. Sub-themes identified under this theme include lack of in-service training, working area security and safety, poor mobile network and electric supply, unresponsiveness of responsible bodies, lack of motivation, and fewer educational opportunities.
Sub-theme 1: Lack of In-service training to get updated information
The absence of regular in-service training opportunities hinders professionals’ ability to stay updated with current guidelines and best practices. Limited access to updated information due to poor mobile network coverage exacerbates this challenge.
A midwife with three years of experience expressed her concerns: “Sometimes, I feel anxious when colleagues inform me that the guidelines I’m using are outdated. This issue seems exacerbated by our poor mobile network.”
Another participant, an MCH coordinator with four years of experience, added: “Training opportunities on updated guidelines have been scarce for a considerable time, further complicating our efforts to provide quality care.”
Sub-theme 2: Working area security and safety
Concerns about workplace security contribute to stress and anxiety among healthcare professionals. Reports of stolen equipment underscore the inadequacies in maintaining a secure environment within healthcare facilities.
A midwife with five years of experience shared: “We lack trust in our hospital’s security measures, which has led to instances of equipment theft, compromising patient care.”
Sub-theme 3: Lack of motivation
Delayed duty payments and the rural setting contribute to low motivation among healthcare workers, impacting their commitment and engagement in their roles.
A midwife with two years of experience lamented: “The delayed payment of our salaries demotivates us. How can we stay motivated in a rural area where financial stability is uncertain?”
Sub-theme 4: Fewer educational opportunities
Limited access to further education and skill development opportunities restricts professional advancement and personal growth for healthcare workers in rural settings.
Another midwife reflected on educational limitations: “Many of my peers who graduated with me have pursued higher education, whereas I’m still using my BSc degree from five years ago. This disparity sometimes leaves me feeling demoralized.”
Theme 4: Infrastructure related challenges and Health system responsiveness
The functionality and availability of infrastructure directly impact the quality of healthcare services provided. Issues such as irregular power supplies and unreliable communication networks can significantly hinder medical operations and patient care.
Sub-theme 1: Poor mobile network and electric supply
Reliable electricity and mobile network coverage are crucial for both personal and professional activities. Participants highlighted the challenges they face due to prolonged periods without electricity and inadequate mobile network coverage.
A midwife with six years of experience shared her frustration: “Electricity supply often fails for weeks at a time, affecting everything we do. Additionally, the unreliable mobile network further complicates communication and connectivity.”
Sub-theme 2: Responsible bodies’ lack of responsiveness
The lack of timely response from accountable organizations to reported issues creates frustration and a sense of powerlessness among healthcare professionals. This neglect can undermine trust in the system and impede efforts to address critical infrastructure and operational challenges.
A midwife with four years of experience expressed her disappointment: “Despite repeated reports, administrators often delay or provide incomplete responses to our concerns. This undermines our confidence in their ability to support us effectively.”
Another participant echoed similar sentiments: “Our managers have diligently reported issues to responsible bodies, yet the lack of timely responses continues to hinder our efforts to improve healthcare delivery.”
Theme 5: Coping strategies for the challenges
Healthcare professionals shared various coping strategies they employ to navigate the challenges encountered in delivering maternal healthcare. Sub-themes under this theme include coping with delayed duty payments, inadequate staffing, material scarcity, poverty, lack of awareness, and lack of motivation.
Sub-theme 1: Coping strategies for delayed duty payments
Initiating discussions with relevant authorities emerges as an effective approach to addressing delays in duty payments. This involves open communication and negotiation to resolve payment delays and mitigate their impact on healthcare services.
A Medical Director with three years of experience described their efforts: “We engaged in discussions with woreda administrators regarding delayed payments, and they assured us of prompt resolution. Communicating this to our professionals helped in reinstating those who had ceased work. However, we are still awaiting improvements.”
Sub-theme 2: Coping strategies for inadequate staffing
Due to insufficient staffing, healthcare professionals often resort to working overtime to manage workload demands effectively. This strategy ensures essential tasks are completed despite staffing shortages.
A midwife with five years of experience shared her perspective: “All ten midwives at our hospital are working overtime to compensate for staffing gaps. We rotate shifts equally to maintain maternal health service delivery.”
Another participant highlighted the collaborative effort: “Given the shortage of midwives, nurses also assist in providing maternal health services, demonstrating our team’s commitment despite challenges.”
Sub-theme 3: Coping strategies for material scarcity
Material scarcity poses significant challenges, leading healthcare professionals to adopt proactive coping strategies. Regular inventory checks are one such strategy employed to manage shortages effectively.
A MCH coordinator with four years of experience described their approach: “To mitigate the impact of medication shortages, we conduct regular stock checks to ensure timely replenishment. This proactive measure helps us maintain continuity in healthcare services.”
Additionally, healthcare providers sometimes advise families to purchase inexpensive equipment from nearby pharmacies to address shortages:
“For resource shortages, we occasionally advise families to purchase affordable items like syringes and gloves from local pharmacies”, shared a midwife with six years of experience.
Sub-theme 4: Coping strategies for poverty
Healthcare professionals also navigate challenges posed by poverty, particularly in ensuring access to essential healthcare services. Some professionals extend personal assistance to alleviate financial burdens:
“Despite the availability of free services at government healthcare facilities, some treatments require payment that many mothers cannot afford. Occasionally, we contribute personally to help cover these costs”, shared a midwife with five years of experience.
Sub-theme 5: Coping strategies for lack of awareness
Addressing the lack of awareness among mothers about maternal healthcare services is crucial. Healthcare professionals actively engage in education and advocacy to empower mothers with necessary knowledge:
“We prioritize maternal health education during antenatal care visits, emphasizing the importance of regular check-ups and timely interventions”, explained a MCH coordinator with four years of experience.
Sub-theme 6: Coping strategies for lack of motivation
Maintaining motivation among healthcare professionals is essential for sustaining quality care delivery. Recognizing outstanding performance through rewards serves as a motivational strategy:
“To boost motivation, we implement reward systems to acknowledge and encourage exceptional work among our staff”, highlighted a medical director with five years of experience.
Discussion
Through one-on-one in-depth interviews, this study explored the difficulties and coping strategies faced by HCWs providing maternity health care in the rural Wolaita zone. We discovered that healthcare workers encountered various problems and strategies for overcoming the challenges. The majority of the study’s findings are consistent with earlier research.
According to this study, one of the difficult conditions facing HCWs who work in the rural Wolaita zone is insufficient government funding. Due to this, salaries and duty payments were delayed (all professionals complained about not receiving their duty payments), and it also caused a lack of staff, a shortage of material resources, and poor construction. Delayed salary and duty payments could have a severe negative financial impact on them and their families. It may make providing for necessities like food, housing, and medical care more challenging. This problem may also lead to heightened levels of stress and anxiety in workers, which could negatively impact their general health and output [26]. It also caused a shortage of staff, which can increase the workloads of HCWs. This may lead to reduced productivity, exhaustion, and a compromise in the services [27]. A lack of material resources can make it more difficult for people and organizations to do their duties efficiently. This shortfall could involve equipment or basic supplies required for different operations. Similar research conducted in Ghana, South Africa, Yemen, Pakistan, and the Congo revealed that healthcare workers (HCWs) are fighting to survive in rural areas as providers of maternal health care due to a shortage of materials and human resources that prevents them from providing adequate care in their catchment areas [7, 28,29,30,31] According to studies, most HCWs in African nations experience difficulties due to insufficient material resources [30, 31]. Poorly designed buildings might need more lighting or ventilation, which makes medical procedures dangerous and raises the possibility of mistakes or mishaps during childbirth.
We found societal barriers to health and access to health care include lack of awareness, poverty, distance from health care centers, rumors from neighbors, and blaming professionals. Due to a lack of awareness, some mothers quit antenatal care follow-up, while others prefer traditional birth attendants. Similarly, a study in Indonesia revealed a need for more understanding of a challenging condition for HCWs [12]. Referral hospitals that are far away from primary hospitals are also another challenge reported by study participants. Similarly, studies in Brazil showed that the distance traveled to access care during pregnancy is a significant risk factor for maternal death [32]. Distance is a big problem in Ghana, too [33]. Studies showed that poverty is the main issue in accessing healthcare services in developing countries [34]. It is okay to blame someone for their fault, but blaming without understanding the situation is not good, and rumors from neighbors may affect health care provision, too.
In this study, HCWs also reported that they experienced challenges of personal life struggles such as difficulty in getting updated guidelines, inadequate work-related security and safety(sometimes equipment is stolen, and they don’t trust security teams), poor mobile network and electric supply which is similar with study in New Zealand (infrequent loss of cell phone coverage), Congo (insufficient work-related security) and limited in-service training opportunities in Ghana [7, 31, 35].
We found that healthcare professionals used different coping strategies like reporting to responsible bodies that their institution has an inadequate budget and working overtime to cover the spaces caused by a shortage of midwives for few numbers of ambulances. Clients’ families are asked to use other transportation options like buses and other cars, help poor clients from their pockets, teach mothers to increase their awareness and give recognition and reward programs for hard workers to increase their motivation. However, similar studies in Ghana showed that improvising (like tearing a pillowcase to receive the baby) in the face of insufficient supplies, being one step ahead to avoid adverse outcomes, was found to enable the HCWs to cope with the barriers that they face in their workplaces [36].
Another study in the Democratic Republic of Congo revealed that some HCWs grew food on the land around the health facility, traditional birth attendants worked in the health facilities, they used the income generated from user fees to buy essential equipment and supplies, HCWs asked pregnant women in the antenatal care clinic to bring basic supplies for delivery. To deal with transport challenges, midwives and ex-midwives explained that they organized motorcycle taxis to take women with complications to the referral hospital. HCWs advised women who had signs that they may develop complications to go early to the referral hospital [37].
Strengths and limitations of the study
Due to the insufficient budget, collecting professionals from different primary hospitals in rural areas of the Wolaita zone is challenging. So, we couldn’t collect data using focus group discussions. To get more attention, some study participants gave exaggerated information. The study’s inclusion of health professionals with little experience—more especially, those with less than a year of experience providing care for mothers—was one of its limitations. In comparison to their more seasoned counterparts, less experienced professionals may have had limited exposure to a wider range of challenges and coping strategies, which may have limited the depth of insights offered.
Conclusion
This study revealed that HCWs are facing different kinds of challenges while providing maternal health care in rural health facilities of the Wolaita zone. HCWs play a crucial role in reducing maternal mortality, so reducing the challenges they face indirectly reduces maternal mortality. In this study, HCWs tried different coping strategies but more was needed. Responsible bodies should work hard to mitigate these problems. Challenges faced by healthcare professionals affect their performance. Therefore, finding solutions to the issues they face is more beneficial.
Data availability
The data supporting the findings of this study are not publicly available due to confidentiality and privacy concerns. The data were collected with the understanding that they would remain confidential. Therefore, they are not available for public access.For inquiries related to the data, including requests for data access for research purposes, please contact the corresponding author at netsanetd05@gmail.comData access will be considered on a case-by-case basis, in compliance with ethical guidelines and confidentiality agreements.
Abbreviations
- HCW:
-
Health care worker
- MCH:
-
Maternal and child health
- PHCU:
-
Primary health care unit
References
Facts Q. Factsheet Maternal Health and Rehabilitation What Is Maternal Health ? Common Impairments and Activity Limitations. 2016;2013–4.
Leung H. Journal of fertilization: in Vitro-IVF- Worldwide, Reproductive Medicine. Genet Stem Cell Biol Importance Maternal Health : Ensuring Safe Healthy Pregnancies all. 2023;11(1000298):10–1.
Macnalty A, Flack IH. Section of the-history of Medicine the Pre-history of Midwifery. [Abridged]. Proc R Soc Med. 1947;L:713–22.
à SF, Dickinson E. Stress, coping, and hope. 2010;908:901–8.
Nkowane AM. Nursing and midwifery challenges, obstacles and possibilities to achieve universal health coverage Outline of the presentation 1. SDNM : HSS and education. 2013.
World Health Organization. Midwives ’ Voices Midwives ’ Realities. 2016;1–76.
Adatara P, Amooba PA, Afaya A, Salia SM, Avane MA, Kuug A, et al. Challenges experienced by midwives working in rural communities in the Upper East Region of Ghana: a qualitative study. BMC Pregnancy Childbirth. 2021;21(1):1–8.
Maregn RT, Bourret K, Egal JA, Esse A, Mattison C, Klingberg-. M. Qualitative study of the roles of midwives in the provision of sexual and reproductive healthcare services in the Somaliland health system. 2023;1–8.
Onambele L, Ortega-Leon W, Guillen-Aguinaga S, Forjaz MJ, Yoseph A, Guillen-Aguinaga L et al. Maternal mortality in Africa: Regional trends (2000–2017). Int J Environ Res Public Health. 2022;19(20).
Hill Z, Dumbaugh M, Benton L, Källander K, Strachan D, ten Asbroek A et al. Supervising community health workers in low-income countries - a review of impact and implementation issues. Glob Health Action 2014;7(1).
Navaneetham&Dharmalingam. & A. Dharmalingam Department of Sociology & Social Policy University of Waikato, Hamilton, New Zealand. 2000;(October):1–40.
Afful-Mensah G, Nketiah-Amponsah E, Boakye-Yiadom L. Rural-Urban Differences in the Utilization of Maternal Healthcare in Ghana: The Case of Antenatal and Delivery Services Rural-Urban Differences in the Utilization of Maternal Healthcare in Ghana: The Case of Antenatal and Delivery Services. African Soc Sci Rev [Internet]. 2014;6(1). https://digitalscholarship.bjmlspa.tsu.edu/assr%5Cn
Yaya S, Bishwajit G, Shah V. Wealth, education and urban-rural inequality and maternal healthcare service usage in Malawi. BMJ Glob Heal. 2016;1(2):1–12.
Greening N. Phenomenological Research Methodology. Sci Res J. 2019;VII(V).
Mann JW. Book Review: an introduction to Phenomenological psychology. South Afr J Psychol. 1980;10(3–4):115–115.
Tiada Nama. (1900). Chapter 3: Research Method. In Sample of a Qualitative Methodology Section (pp. 101–73). Retrieved from http://precisionconsultingcompany.com/samples/Sample%20of%20a%20Qualitative%20Methodology%20Section.pdf
Chirwa MD, Nyasulu J, Modiba L, Ganga-Limando M. (2022). Challenges faced by midwives in the implementation of facility-based maternal death reviews in Malawi (pp. 1–23). https://doi.org/10.21203/rs.3.rs-1227560/v1
Bremnes HS, Wiig ÅK, Abeid M, Darj E. Challenges in day-to-day midwifery practice: a qualitative study from a regional referral hospital in Dar Es Salaam, Tanzania. Global Health Action. 2018. https://doi.org/10.1080/16549716.2018.1453333. Advance online publication.
Astutii H, Indrayani, Harianis S. Challenges for midwives in remote areas: an ethnography study. Pakistan J Med Health Sci. 2021;14(4):1691–7.
Mugo NS, Dibley MJ, Damundu EY, Alam A. (2018). Barriers faced by the health workers to deliver maternal care services and their perceptions of the factors preventing their clients from receiving the services: A qualitative study in South Sudan. Maternal and Child Health Journal. Advance online publication. https://doi.org/10.1007/s10995-018-2555-5
Armat MR, Assarroudi A, Rad M, Sharifi H, Heydari A. (2018). The qualitative report inductive and deductive: Ambiguous labels in qualitative content analysis. The Qualitative Report, 23(1), 219–221. Retrieved from https://nsuworks.nova.edu/tqr/vol23/iss1/16
Liu L. Using generic inductive approach in qualitative educational research: a case study analysis. J Educ Learn. 2016;5(2):129.
Dawadi S. Thematic analysis approach: a step by step guide for ELT research practitioners. J NELTA. 2020;25(1–2):62–71.
Abadie F, Codagnone C, Helter T, Lupiáñez-Villanueva F. (2014). Integrated care methodological set-up report. Strategic Intelligence Monitor on Personal Health Systems Phase 3 (SIMPHS 3) (Vol. 3).
Anderson G, Herr K, Nihlen A. (2014). Studying your own school: an educator’s guide to practitioner action research. Stud Your Own School: Educator’s Guide Practitioner Action Res, 26–8.
Kazungu JS, Barasa EW, Obadha M, Chuma J. What characteristics of provider payment mechanisms influence health care providers’ behaviour? A literature review. Int J Health Plann Manage. 2018;33(4):e892–905. https://doi.org/10.1002/hpm.2547.
Combes JB, Elliott RF, Skåtun D. Hospital staff shortage: the role of the competitiveness of pay of different groups of nursing staff on staff shortage. Appl Econ. 2018;50(60):6547–52.
Paxton A, Wardlaw T. Are we making progress in maternal mortality? N Engl J Med. 2011;364(21):1990–3.
Hyzam D, Zou M, Boah M, Saeed A, Li C, Pan S, et al. Health information and health-seeking behaviour in Yemen: perspectives of health leaders, midwives and mothers in two rural areas of Yemen. BMC Pregnancy Childbirth. 2020;20(1):1–12.
Bogren M, Grahn M, Kaboru BB, Berg M. Midwives’ challenges and factors that motivate them to remain in their workplace in the Democratic Republic of Congo - an interview study. Hum Resour Health. 2020;18(1):1–10.
Thopola M, Lekhuleni M. Challenges experienced by midwifery practitioners in the midwifery practice environment of Limpopo Province, South Africa. Afr J Phys Health Educ Recreation Dance Dec. 2015;2015:874–89.
Simões PP, Almeida RMVR. Geographic accessibility to obstetric care and maternal mortality in a large metropolitan area of Brazil. Int J Gynecol Obstet. 2011;112(1):25–9.
Dotse-Gborgbortsi W, Nilsen K, Ofosu A, Matthews Z, Tejedor-Garavito N, Wright J, et al. Distance is a big problem: a geographic analysis of reported and modelled proximity to maternal health services in Ghana. BMC Pregnancy Childbirth. 2022;22(1):1–12. https://doi.org/10.1186/s12884-022-04998-0.
Peters DH, Garg A, Bloom G, Walker DG, Brieger WR, Rahman H, M. Poverty and access to health care in developing countries. Ann N Y Acad Sci. 2008;1136:161–71.
International Labour Office. (2008). ISCO-08. International Standard Classification of Occupations. Department of Statistics, International Labour Office. Retrieved from http://www.ilo.org/public/english/bureau/stat/isco/index.htm
Ismaila Y, Bayes S, Geraghty S. Midwives’ strategies for coping with barriers to providing quality maternal and neonatal care: a glaserian grounded theory study. BMC Health Serv Res. 2021;21(1):1–11.
Health R, Baba A, Theobald S, Martineau T, Lecturer S, Sabuni P et al. (2020). Midwives’ experiences of working in the rural and fragile settings of Ituri province, Democratic Republic of Congo. Rural Remote Health, 20(2).
Acknowledgements
We would like to acknowledge Jimma University for providing the materials used for the work.
Funding
Jimma University.
Author information
Authors and Affiliations
Contributions
N.D.M participated in the design and analysis of the study. M.S.T and D.W.A participated in formal analysis, writing - review & Editing. T.M.M and K.A.G. searched the databases and wrote the first and second drafts of the article. All five authors took part in reviewing the whole process of the manuscript and approved the final version.
Corresponding author
Ethics declarations
Ethical consent and Consent to participate
Ethical clearance was obtained from the Jimma University, College of Health Sciences and Medicine Ethical Review Committee (CHSM/ERC/01/14). A permission letter was received from the Wolaita Zone Health Department and submitted to each rural health center before data collection. Each participant gave their informed oral consent, which stated that they might leave the study at any moment and that participation was completely optional. The information provided by each respondent was kept totally confidential, and the oral informed consent covered the study’s objective and methods, potential risks and benefits, voluntary participation, and right of withdrawal. The 1964 Helsinki Declaration and its later revisions’ ethical guidelines were strictly followed during the conduct of this investigation. Throughout the study, all participant information was kept totally private, and the data was anonymized using unique identifiers.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Milku, N.D., Abose, D.W., Gelaw, K.A. et al. Challenges and coping strategies for providing maternal health care services among health care professionals in rural health facilities in Wolaita Zone, Southern Ethiopia: a qualitative study. BMC Health Serv Res 24, 903 (2024). https://doi.org/10.1186/s12913-024-11389-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-024-11389-y