Abstract
Background
Patient-centredness has become a central quality indicator for oncology care. Elements include shared decision-making, patient navigation and integration of psychosocial care, which impact patient-reported and clinical outcomes. Despite efforts to promote patient-centred care in Germany in recent decades, implementation remains fragmented. Further, research on patient experiences with cancer care and its determinants is limited. Therefore, this study examines which patient- and facility-specific factors are associated with patient-centred quality care delivery.
Methods
A cross-sectional study was conducted among 1,121 cancer patients in acute treatment, rehabilitation, and aftercare for different cancer entities across Germany. A participatory developed questionnaire was used. Outcome measures were the quality of physician-patient interaction and provision of psychosocial care during acute care. Predictors comprised patient-specific characteristics and treatment facility-specific factors. Multiple linear regression and multivariate binary logistic regression analyses were performed. In addition, a content analysis of open-ended comments on the patients’ overall cancer care needs was applied.
Results
Multiple linear regression analysis showed recent diagnosis (β=−0.12, p = < 0.001), being male (β=−0.11, p = 0.003), and having a preference for passive decision-making (β=−0.10, p = 0.001) to be significantly associated with higher interaction quality, but not age, education and health insurance type. An overall low impact of patient characteristics on interaction quality was revealed (adj. R2 = 0.03). Binary logistic regression analysis demonstrated the availability of central contact persons (OR = 3.10, p < 0.001) followed by recent diagnosis (p < 0.001), having breast cancer (p < 0.001) and being female (OR = 1.68, p < 0.05) to significantly predict offering psycho-oncological counselling to patients in acute care facilities. The availability of peer support visiting services (OR = 7.17, p < 0.001) and central contact persons (OR = 1.87, p < 0.001) in the care facility, breast cancer diagnosis (p < 0.001) and a higher level of education (p < 0.05) significantly increased the odds of patients receiving information about peer support in the treatment facility. Despite relatively satisfactory quality of physician-patient interactions in cancer care (M = 3.5 (± 1.1)), many patients expressed that better patient-centred communication and coordinated, comprehensive cancer care are needed.
Conclusion
The findings reflect effective developments and improvements in cancer care and suggest that patients’ social characteristics are less decisive for delivering patient-centred quality care than systemic factors surrounding the care facilities. They can serve to inform oncology care in Germany.
Similar content being viewed by others
Background
Patient-centred care and the measurement of its quality through patient-reported outcome measures (PROMs) and patient-reported experience measures (PREMs) have gained relevance in the field of oncology over the past decades [1, 2]. Since research has shown that patient-oriented approaches to health care can potentially improve chronic patients’ care experiences and clinical outcomes [3,4,5], it has become a key component of quality care [1, 4, 6]. Subsequently, patient-centred cancer care has been promoted through various initiatives [7].
In Germany, the Federal Ministry of Health initiated a National Cancer Control Plan (NCCP) in 2008 to provide high-quality, comprehensive care and to strengthen patient-centredness in cancer care comprising acute care, rehabilitation and aftercare [8]. It was driven by the German Cancer Society, which also developed other initiatives to foster excellent patient-centred care, such as the certification system for cancer centres, as one part of the NCCP [9, 10]. Further efforts are reflected in disease management programmes for cancer patients [11] anchored in German health regulations and in the concept of self-help-friendliness [12]. Those enable patient-centred and integrated care that considers supportive psychosocial cancer care (e.g. peer support). In particular, the importance of successful patient communication and shared decision-making (SDM) is increasingly recognised as an integral feature of patient-centred care [13,14,15]. Research has emphasised the significance of high-quality physician-patient relationships, with SDM being an important element for treatment and adherence [16, 17]. These relationships have also been found to correlate with patient satisfaction and improved decision-making in cancer care [18]. Therefore, several supportive tools and training programmes for healthcare professionals have been introduced in Germany [19, 20]. Other examples of changes in German cancer care are patient involvement in multidisciplinary tumour boards [21] and progress in patient navigation [22]. The latter has led to the provision of oncology nurse navigators or similar contact persons in some cancer facilities across Germany [23, 24]. This, in turn, has been shown to positively influence patients’ satisfaction with care and relates to their quality of life [22, 25].
Although these developments are encouraging and promising, they have not been systematically implemented in all cancer care facilities [26]. Initiatives remain scattered, as there is no standard for establishing them in Germany to target patient-centred care, mainly due to systemic reasons surrounding healthcare [15, 27]. In addition, other framework conditions affect patient-centred quality care. For instance, oncological care units are exposed to economic constraints and staff shortages while patient numbers increase [28]. This trend results in less time available for patients and thus can lower physician-patient interaction quality [29] and hinder cooperation with psychosocial cancer care [30]. The introduction of diagnosis-related groups (DRGs) has exacerbated these developments and may decrease the quality of care experienced by patients [31]. Moreover, the COVID-19 pandemic negatively impacted and limited cancer care, particularly concerning psycho-oncological care [32].
Recent data on patient satisfaction with care revealed positive experiences of many cancer patients in Europe [33,34,35] but also demonstrated persisting unmet needs concerning communication and coordinated supportive psychosocial care [34,35,36]. Despite the shift towards patient-centred care and numerous changes within the oncology care system, studies suggest that the quality of cancer care in some European countries is still determined by patient characteristics such as age, educational background and time to treatment [34, 37,38,39]. For Germany, current data assessing patient satisfaction and determinants of quality cancer care is limited. Thus, this study aims to gather the care experiences and needs of cancer patients in Germany and to assess satisfaction with care to identify strengths and weaknesses of oncological care and its developments. In particular, the goal of this study was to examine which patient-related and facility-specific factors correlate with different indicators of patient-centred care within the German oncology care system to inform it further. Subsequently, the objectives of this research are: (1) to examine which patient- and cancer care facility-specific factors are associated with better physician-patient interaction and (2) are associated with the offering of psychosocial support in acute care, and (3) to identify the overall cancer care needs of patients.
Methods
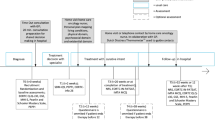
Study design, population and recruitment
This study applied a cross-sectional design. Data were collected between October 2020 and September 2021 with a self-administered questionnaire to investigate care experiences and needs of cancer patients in Germany. The survey is part of a project examining health literacy and peer support activities of cancer patients. It follows a participatory research approach and has been conducted in cooperation with the House of Cancer Self-Help– Federal Association (HKSH), an association of ten nationwide cancer peer support organisations (PSOs). Ethical approval was granted by the Local Psychological Ethics Committee at the Center for Psychosocial Medicine of the University Medical Center Hamburg (No. LPEK-0109).
German-speaking participants and non-participants of peer support groups (PSGs) aged 18 years and older with a cancer diagnosis of any type and at any stage, were eligible to participate. A multi-channel approach was adopted for broad patient recruitment. More than 60,000 brochures and posters with information about the study were sent to 1,382 cancer care providers for acute care, rehabilitation, aftercare and supportive psychosocial care throughout Germany from October 2020 onwards. These care and counselling facilities, such as cancer societies, cancer counselling centres, oncological rehabilitation clinics, certified cancer centres, hospitals with oncological departments, and oncological specialised practices and PSOs, were notified of the study in advance by mail. Snowball sampling of patients also took place through the HKSH, peer support groups outside PSOs, and the German Cancer Society to disseminate the call for study participation (via email, post and PSO journals). In addition, the study information was circulated in a newsletter of the National Contact and Information Centre for the Initiation and Support of Self-Help Groups (NAKOS) and at an online patient congress. Reminder emails were sent in February and May 2021 to increase the response rate. Patients could choose between online and paper-pencil participation. Participation was anonymous, and all participants gave their informed consent by confirming (online or by sending in the paper questionnaire) that they had read the study information and data protection policy, and that they are willing to participate.
Measures and variables
The questionnaire used in this research is part of a larger survey and covers various aspects such as diagnosis and treatment, care experience, socio-demographics, and other dimensions (see supplementary file 1). It was newly developed in collaboration with representatives of oncology, medical sociology, PSOs and PSGs and is based on a previous data collection that included qualitative interviews and a quantitative survey with PSG leaders, as well as a literature screening of instruments.
Outcome variables
A modified version of the 14-item Questionnaire on the Quality of Physician-Patient Interaction (QQPPI) [40] was used to measure patients’ perception of the quality of physician-patient interaction in consultations during acute cancer care. The QQPPI was validated in a sample of patients in outpatient care and showed very good internal consistency (Cronbach’s α = 0.95) [40]. We used 7 items of the original QQPPI scale (items 2, 4, 6, 7, 8, 11, 14). The other items were deleted to make the questionnaire generalisable to any type of cancer care settings, in line with the authors’ recommendation to use a shortened version [40]. Two new items (numbers 8 and 9) were added as they were identified by cancer PSO members as important to patients. The 9-item scale showed identical reliability (Cronbach’s α = 0.95). The scale items refer to statements about the interaction and are to be rated on a 5-point Likert scale ranging from 1 ‘does not apply’ to 5 ‘fully applies’ (see supplementary file 2). For analyses, a sum score ranging from 1 (low quality) to 5 (high quality) was calculated from the 9 items. Accordingly, successful interaction of high-rated quality is characterised by detailed information from the physician regarding treatment and illness, sufficient time, taking the patient seriously, and involving the patient and their relatives in treatment decisions.
Two binary outcome variables as indicators of quality care assessed the provision of psychosocial services in the acute treatment facility. One item asked whether the patients were offered psycho-oncological counselling (see supplementary file 1, item B.5a), and another whether they received information about the possibility of participating in a PSG (item C.2) during acute care (each with the response option 0 = no or 1 = yes).
In addition, in the sense of patient involvement and to obtain more detail on patients’ experiences and opinions, a content analysis was conducted on open-ended responses to the question of whether the patients had any specific wishes and needs regarding their overall cancer care (see supplementary file 1, item B.10). As the responses were provided as bullet points or short sentences, they were grouped and categorised inductively into broad themes by two researchers using Excel spreadsheets, applying a simple qualitative content analysis [41] to provide (frequency) counts through content coding.
Independent variables
Patient-related predictors comprised social (sex, age, education), clinical (time since diagnosis, cancer type) and healthcare-specific characteristics (insurance type, decision-making style). Sex was dichotomised in 0 = male and 1 = female. Age (at diagnosis) was coded as a continuous variable in years by subtracting years since diagnosis from age at time of participation. Schooling was coded into low (= 1), medium (= 2) and high (= 3), i.e. ≤ 9 years of education; 10 years of education and ≥ 11 years of schooling and takes into account the three different schooling types in Germany. Time since diagnosis was grouped into the following three categories: 1 ‘<1 year (newly diagnosed)’, 2 ‘diagnosis 1 to < 5 years’ and 3 ‘5 + years (cancer survivors)’. Type of self-reported primary cancer diagnosis was grouped based on distribution into breast cancer (= 1), prostate cancer (= 2) and other cancer types (= 3). Besides, the type of health insurance was assessed and dichotomised into 1 = statutory and 2 = private health insurance. To measure patients’ preference regarding medical decision-making, a modified version of item 13 of the Patient Participation Questionnaire [42] was used to assess participants’ general attitudes towards different models of decision-making. The wording in the question was changed from “Who should make the medical decisions about your problems” to “Who in your opinion should make the medical decisions for the diseases you have?” and gendered the response options (see item E.10 in the supplementary file 1). Patients were asked to indicate who should make the medical decisions for their disease, with values ranging from 1 = passive (equivalent to paternalistic model preference; ‘The doctor should decide’) to 5 = active (corresponding to informed decision-making model preference; ‘I should decide’). For binomial logistic regression, patients’ preference for medical decision-making was grouped into three categories in analogy to the models of physician-patient relationships (1 = paternalistic model; 2 = SDM, 3 = informed decision making).
Predictors relating to care facility characteristics were examined through two single items. One item assessed if there was a central contact person available in the hospital to guide the patients through treatment and further care, and a second item assessed whether visiting services of PSGs were available in the hospital (response options 0 = no, 1 = yes).
Statistical analyses
Data analysis was performed using IBM SPSS Statistics 27. Descriptive statistics were used to examine the participants’ clinical and socio-demographic characteristics and the distribution of the values of the outcome variables. Missing value imputation by using mean value imputation and series mean imputation were performed for missing single item data. If crucial data on sociodemographic information or outcome variables was missing, cases were excluded from analyses. For scales, a maximum of three missing responses were tolerated. If more than three items were missing, the total score was treated as a missing value. Multiple linear regression was used to assess the quality of the interaction considering patient-specific variables described above. The method of regression was forced entry and cases were excluded listwise. Multivariate binary logistic regression analyses were conducted to assess the associations between multiple patient- and facility-specific variables, and the provision of psychosocial care in acute cancer care. The method of logistic regression was forced entry, with all variables being entered into the models and the values of the relevant parameters were estimated using maximum-likelihood estimation. Reference categories were set as the first. Statistical significance was set at an α level of 0.05 for all analyses.
Results
Patient characteristics
A total of 1,356 patients responded to the study. Respondents with missing information on socio-demographic characteristics were excluded. After data cleaning, the dataset consisted of 1,121 participants who completed the questionnaire, mainly online (84%). The patients’ characteristics are shown in Table 1. Patients from all 16 federal states participated, the majority of them from North Rhine-Westphalia, the most populous state in Germany. Both newly diagnosed patients and cancer survivors participated, with an average time of 4.6 ± 6.0 years after cancer diagnosis. About 30% of patients were still undergoing treatment at the time of the survey. The participants’ mean age was 61.3 ± 12.4 years at participation. Most participants were female (54.7%), had a high level of education (58.3%) and lived in a partnership (83.2%). The respondents were predominantly breast cancer patients (30.6%), followed by prostate cancer patients (19.3%). Cancer stages varied, ranging from UICC (Union Internationale Contre le Cancer) stage 0 to IV, with most patients not knowing their disease stage (43.5%). Less than half of the participants were members of PSGs (45.2%). Most patients preferred SDM (76%) and had statutory health insurance (83.1%).
Quality of physician-patient interaction
On a scale from 1 (low) to 5 (high), the average quality score for physician-patient interaction during consultations in acute cancer care was 3.5 (± 1.1) among respondents. To determine the association between the quality of physician-patient interaction in care facilities and patient characteristics, a multiple linear regression was performed. Before regression analysis, normality, linearity, multicollinearity, and independence of residuals were checked and no concerns were found. Six explanatory variables were entered into the regression model with the quality of physician-patient interaction as the outcome variable (Table 2). Indicating a normal distribution, the analysis revealed the model to be a poor model fit to the data (F(6,1010) = 5.43, p < 0.001), being statistically significant and explaining 3% of the variability in the dependent variable (adjusted R2 = 0.03). The results revealed more recent diagnoses (β=−0.12, p = < 0.001), being male (β=−0.11, p = 0.003) and patients’ preference for a more passive role in decision-making (β=−0.10, p = 0.001) to be significantly associated with interactions of better quality.
Other quality care indicators
Provision of psycho-oncological counselling
In total, 55.5% (n = 587) of respondents were offered psycho-oncological counselling in the hospital for acute treatment. The majority of them (63.4%) made use of this offer. To test which patient- and facility-specific factors shape whether cancer patients were offered psycho-oncological counselling or not, a binomial logistic regression was conducted. All model coefficients and odds can be found in Table 3. The model was statistically significant (χ²(12) = 203.67, p < 0.001). Goodness-of-fit was assessed using the Hosmer-Lemeshow-Test, indicating a good model fit, χ²(8) = 4.78, p > 0.05. Of the eight variables entered into the regression model, four contributed significantly to predicting the provision of psycho-oncological counselling: sex (p < 0.05), cancer type (p < 0.001), time since diagnosis (p < 0.001) and availability of a central contact person in the hospital (p < 0.001), while the other variables showed no significant associations. Being female increased the likelihood of provision of psycho-oncological support, OR = 1.68 (95%-CI[1.13, 2.50]), and the availability of a central contact person for patients, OR = 3.10 (95%-CI[2.19, 4.39]), as patients had 3.1 times higher odds of being offered psycho-oncological counselling if a central contact person was available in the hospital. Having a cancer diagnosis other than breast cancer (e.g. prostate cancer OR = 0.32 (95%-CI[0.18, 0.57]), and a diagnosis longer ago ( 5+ years) compared to patients with a recent diagnosis (< 1 year), OR = 0.42 (95%-CI[0.29, 0.62]) decreased the likelihood of psycho-oncological support provision.
Information about peer support participation
Of all respondents, 33.3% (n = 327 patients) were informed in the hospital about cancer PSGs. A second multivariate binomial logistic regression examined what factors determine the provision of this information about PSGs and the possibility of participating in them. Nine variables were entered into the final regression model. The model was statistically significant (χ²(13) = 155.19, p < 0.001) and showed a good model fit, χ²(8) = 9.18, p > 0.05. As presented in Table 4, four of the nine variables entered into the regression model contributed significantly to predicting the provision of PSG information. In particular, if visiting services of PSGs were available in the hospital compared to non-availability, patients were 7.2 times more likely to have been informed about the possibility of participating in a PSG (OR = 7.17 (95%-CI[4.75, 10.82]), p < 0.001). Similarly, the availability of a central contact person for patients, OR = 1.87 (95%-CI[1.33, 2.65]) significantly increased the likelihood of provision of information about PSGs (p < 0.001). Besides, breast cancer patients compared to prostate cancer (OR = 0.51 (95%-CI[0.27, 0.97]), p < 0.05) or other entities (OR = 0.41 (95%-CI[0.27, 0.64]), p < 0.001), and patients with medium educational levels compared to low education, OR = 1.78 (95%-CI[1.00, 3.17]), were more likely to have been provided PSG information than not, while other patient-related variables were non-significant.
Patient needs for care
In free text comments, 411 patients stated special wishes and needs regarding their previous oncological care. Those expressed by more than 10 respondents each are listed in Table 5. The most frequently mentioned theme identified relates to more education and information about medical findings, risks, side effects and consequences of treatments (n = 137). Another theme was the choice of therapy. In this regard, 125 patients emphasised that they would have preferred other treatment options and that further care options such as “pain treatment”, “incontinence care” or “rehabilitation for follow-up treatment” were missing. Another aspect of patient needs identified concerned better communication between patient and physician, pointed out by 39 respondents. Participants desired conversations at “eye level” with more “empathy”, “respect” and “to be taken seriously”. Other key wishes for patients’ cancer care were categorised into increased social support and greater inclusion of supportive psychosocial care such as psycho-oncological and peer-support services. Here, participants stated that psychosocial services are often not mentioned or recommended, although they are needed both after and during treatment as a kind of “co-care”, which in their view should be offered “at every step of the treatment”.
The above-mentioned categories are framed by patients’ expressed needs relating to certain structures of cancer care. For instance, participants noted the lack of time of the staff in care facilities (n = 23). Subsequently, some respondents called for improved framework conditions in hospitals (n = 13). Other mentions referred to improved aftercare (n = 28) that is needed as “there are significant gaps in care and counselling” and cooperation between physicians, clinics and rehabilitation facilities was lacking. One patient affirmed in this context: “Those affected want structured aftercare with a specialised aftercare and treatment concept”. A stronger involvement of relatives was another need (n = 13). Some patients (n = 29) also asked for a central, accessible contact person, such as oncology navigators or at least “always the same doctor” responsible for the patients and who can be contacted “in case questions arise or there is a need for information, and who is also familiar with the case”.
Discussion
The findings propose that contrary to previous data [34, 37,38,39], the quality of physician-patient interaction is not so much determined by the social characteristics of the patients. This is indicated by the non-significant results for the variables age and education alongside insurance type. Therefore, the findings do not support previous results suggesting that older patients [34, 38, 39, 43] and patients with higher educational levels [37, 43] experience better interactions in cancer care. As a more recent time of diagnosis was the most decisive factor for a better quality of the physician-patient interaction and the R2 of the linear regression model was relatively small, the results suggest that its quality is rather determined by other system- and facility-related factors of cancer care not assessed in the study. These might be aspects addressed in the free text comments, such as staff and time available in the care facility. Overall, these results are encouraging and may reflect successful changes in oncology care towards improved patient-centred care. Interestingly, male and more passive patients regarding decision-making showed significantly better interaction quality, albeit with a small effect. Possibly, these patients are less critical in reviewing their experience and more trusting in the assessment of their physicians and their overall care, raise fewer questions about their disease and treatment and are less likely to talk about comprehensive needs [44]. Similarly, Heerdegen et al. [38] demonstrated that male patients were more likely to experience ‘excellent’ cancer care.
Consistent with previous literature [18, 33,34,35], the assessed quality of physician-patient interaction correlates highly with overall patient satisfaction with care, highlighting its importance and showing that patients are relatively satisfied with the quality in total, as participants scored an average of 3.5 points out of 5 on the interaction quality. Considering that more than a third of the patients were diagnosed and treated during the COVID-19 pandemic, the results possibly indicate the provision of continued quality cancer care despite pandemic-related difficulties [32]. This is confirmed by an additional data analysis, which showed that less than 10% of these participants experienced any treatment changes or cancellations due to the pandemic (data not shown). However, the scores on interaction quality varied widely on a few items, indicating some potential for improvement. This is supported by the identified patients’ needs from the free text comments concerning better patient-centred communication and interaction. Previous studies have also shown that communication is often an unmet need [34, 35], and that poor physician-patient communication can be a barrier to SDM [45], which should be implemented more often [15, 26, 27].
Regarding other quality care indicators, the results further support the finding that instead of patient characteristics, systemic improvements in cancer care are more relevant in determining delivery of patient-centred care, such as providing supportive psychosocial offers. In particular, the availability of central contact persons in the hospital e.g. oncology nurse navigators, significantly increased the likelihood of offering psycho-oncologic counselling and was found to be more likely for patients with a more recent diagnosis. Moreover, as breast cancer patients, compared to other cancer diagnoses, showed a higher likelihood of having been provided psycho-oncologic support, this could also indicate the successful implementation of integrated care for breast cancer, driven by disease management programmes and establishing breast care nurses [11]. As breast cancer patients in Germany are often treated in certified cancer centres, this may also reflect the effect of certification systems by the German Cancer Society [9, 10] to promote integrated cancer care. Additionally, independent from cancer type, female patients were found to be more likely to receive psycho-oncologic counselling, yet with a lower impact. This might stem from the assumption that female patients often have higher levels of distress and hence higher needs but are also more willing to participate in psychosocial care and more likely to recognise their need for such than men [44]. Although not significant but by trend, younger age at diagnosis was associated with higher likelihood of psycho-oncological counselling provision. To explain this, physicians may expect higher distress in younger patients, as cancer incidences are overall lower, and diagnoses can potentially be more drastic among younger age groups [44]. These findings are in line with previous studies showing that physicians judge patients’ needs for psychosocial services based on their sex and age [35, 44].
Central contact persons were also crucial for the provision of information about PSGs in cancer treatment facilities, in addition to PSG visiting services, while patient-related characteristics other than higher education and type of cancer did not prove to be relevant determinants. While this may not seem surprising, it demonstrates that the one measure of patient-centeredness is a precondition for patient-oriented, integrated care, or propels its next level. The result underlines the importance of central contact persons acting as patient navigators and promoters of psychosocial services in cancer care. As breast cancer patients were more likely to receive information about PSGs, the structured, comprehensive care approach to breast cancer care appears to enhance both the provision of professional counselling and peer support as forms of psycho-oncological support. Further, it can be assumed that integrated care benefits from established patient organisations, such as Germany’s largest cancer PSO, Frauenselbsthilfe Krebs, which is particularly committed to supporting women with breast cancer and gynaecological cancers. Other authors have already revealed that delivery of integrated care also positively affects timely access to care and patient-reported satisfaction with care [23, 33, 46]. At the same time, respondents’ free text comments highlight that supportive services are not always sufficiently integrated into cancer care and patients’ wishes for such, as previously mentioned in international literature [30, 34,35,36]. Yet, the logistic regression models explained only a relatively small amount of variation in the provision of psychosocial care proposing that other factors not depicted here are more influential. These could be disease-related clinical, or facility-related factors, such as the general amount of time available for patients, or physicians’ individual attitudes towards psychosocial care. For instance, not all physicians have a positive attitude towards PSGs and therefore may not suggest them to patients, regardless of their characteristics [30].
Moreover, patients criticise the framework conditions of the hospitals, noting shortcomings in the care system as a whole and aspects of consultations that stem from insufficient time or staff, in line with Osborn’s [28] findings. As a possible solution to some of the issues and needs identified, many patients wished for a central, accessible contact person, such as an oncology nurse navigator. As the provision of such has shown to be positively associated with the quality indicators of patient-centred care, they should be implemented more consistently across cancer care facilities in Germany. Integrated care can further be supported by making stronger use of concepts such as self-help friendliness in hospitals [12] and enabling PSG visiting services through increased cooperation. Besides, the results represent the need to focus on improving patient-centred comprehensive communication at eye level, which should be considered by physicians and can include SDM. In general, more resources are required to further improve the patient-oriented quality of cancer care.
While the findings are encouraging and map recent developments in cancer care towards more patient-centred care that are noticed by patients, there are several limitations of the study to be considered. Firstly, the current sample is not representative, although a multi-channel recruitment approach was followed to include cancer patients with heterogeneous socio-demographic characteristics. Patients with high educational levels are overrepresented and non-German speaking patient groups with migration backgrounds, who may be particularly vulnerable to experiencing poorer quality of care, are underrepresented. Additionally, more than 40% of the participants were PSG members who potentially review care quality more critical than non-members. Moreover, the participants’ overall satisfaction with their cancer care was high in this study, which could have been different in a more balanced sample. This may have led to a bias in the data towards positive reporting. Besides, the regression analyses mainly focused on patient experiences with acute hospital care and did not cover experiences in rehabilitation and aftercare equally. Due to recruitment during the first peak of the COVID-19 pandemic, fewer patients in inpatient acute care were reached. With the large share of long-term cancer survivors participating, recall bias is likely. Additionally, the study relied on patients’ reported assessments of psychosocial care service provision, which may have further biased the results. Levels of distress, social support and quality of life may have also influenced the provision of psychosocial care, yet those variables were not included in the regression models as they were only reported at the time of study participation and do not necessarily reflect circumstances during treatment immediately after diagnosis. A more balanced sample and the inclusion of further relevant covariates may have increased the explained variance. This should be considered for future research. Lastly, causality cannot be depicted due to the cross-sectional study design.
Conclusions
Overall, the results show a tendency for cancer patients with a recent diagnosis to experience better patient-centred care and for organisational factors rather than patients’ social characteristics to determine indicators of quality care. Progressive changes and effective strategies to increase patient-centred care, such as disease management programmes and patient navigators, are reflected in the findings. Nevertheless, the results also highlight the need for further implementation and fostering of these approaches across cancer care facilities and cancer entities in Germany. Physicians are encouraged to offer psychosocial support to all patients, regardless of their social characteristics, and to take into account the identified experiences and needs of patients. In particular, physicians are advised to support integrated care through further collaboration with psychosocial care and to improve patient-centred communication at eye level to increase the quality in cancer care delivery.
Declarations.
Data availability
The datasets used and/or analysed in this study are available from the corresponding author on request.
Abbreviations
- PROMs:
-
Patient-reported outcome measures
- PREMs:
-
Patient-reported experience measures
- NCCP:
-
National Cancer Control Plan
- SDM:
-
Shared decision-making
- DRGs:
-
Diagnosis-related groups
- HKSH:
-
House of Cancer Self-Help– Federal Association
- PSO:
-
Peer support organisation
- NAKOS:
-
National Contact and Information Centre for the Initiation and Support of Self-Help Groups
- PSG:
-
Peer support group
- QQPPI:
-
Quality of Physician-Patient Interaction
- UICC:
-
Union Internationale Contre le Cancer
References
Institute of Medicine (US) Committee on Quality of Health Care in America. Crossing the Quality Chasm: a New Health System for the 21st Century. Washington (DC): National Academies Press (US); 2001.
Rudolph C, Petersen GS, Pritzkuleit R, Storm H, Katalinic A. The acceptance and applicability of a patient-reported experience measurement tool in oncological care: a descriptive feasibility study in northern Germany. BMC Health Serv Res. 2019;19(1):786.
Coulter A, Ellins J. Effectiveness of strategies for informing, educating, and involving patients. BMJ. 2007;335(7609):24–7.
Vaitiekunas L, Coomer K, Turner C, Brown A, Sabesan S. Medical Oncology Care Plan: a tool for improving the provision of clinical information to patients. Intern Med J. 2021;51(8):1332–5.
Gorod A, Hallo L, Merchant S. Governance of patient-centred care: a systemic approach to cancer treatment. Syst Res Behav Sci. 2021;38(2):257–71.
Groene O, Skau JK, Frølich A. An international review of projects on hospital performance assessment. Int J Qual Health Care. 2008;20(3):162–71.
Blümel M, Spranger A, Achstetter K, Maresso A, Busse R, Germany. Health Syst Rev Health Syst Transit. 2020;22(6):1–272.
Bundesministerium für Gesundheit. Ziele des Nationalen Krebsplans. 2012. Available online: https://www.bundesgesundheitsministerium.de/themen/praevention/nationaler-krebsplan/handlungsfelder/ziele-des-nationalen-krebsplans.html (accessed 6 May 2023).
Kowalski C, Graeven U, von Kalle C, et al. Shifting cancer care towards Multidisciplinarity: the cancer center certification program of the German cancer society. BMC Cancer. 2017;17(1):850.
Wesselmann S. Entwicklung Der Zertifizierungsverfahren für Organkrebszentren Und Onkologische Zentren Der Deutschen Krebsgesellschaft. Onkologe. 2012;18:511–6.
Becker G, Hettenbach A, Neuschwander EA, Bamberg M, Wallwiener D. Disease Management Program breast Cancer–first experience. Breast Care. 2006;1(3):152–6.
Kofahl C, Trojan A, Knesebeck O, Nickel S. Self-help friendliness: a German approach for strengthening the cooperation between self-help groups and health care professionals. Soc Sci Med. 2014;123:217–25.
Kane HL, Halpern MT, Squiers LB, Treiman KA, McCormack LA. Implementing and evaluating shared decision making in oncology practice. CA Cancer J Clin. 2014;64(6):377–88.
Barry MJ, Edgman-Levitan S. Shared decision making–pinnacle of patient-centered care. N Engl J Med. 2012;366(9):780–1.
Dahl Steffensen K, Mølri Knudsen B, Finderup J, Willemann Würgler M, Olling K. Implementation of patient-centred care in Denmark: the way forward with shared decision-making. Z Evid Fortbild Qual Gesundhwes. 2022;171:36–41.
Orom H, Underwood W, Cheng Z, Homish DL, Scott I. Relationships as Medicine: quality of the physician-patient relationship determines physician influence on treatment recommendation adherence. Health Serv Res. 2018;53(1):580–96.
Gaster C, Hofheinz RD, Burkhardt H. Shared decision-making in Oncology: preferences in older versus younger patients of an Oncology Clinic - A Conjoint Analysis. Oncol Res Treat. 2021;44(1–2):4–11.
Nakayama K, Osaka W, Matsubara N, Takeuchi T, Toyoda M, Ohtake N, Uemura H. Shared decision making, physicians’ explanations, and treatment satisfaction: a cross-sectional survey of prostate cancer patients. BMC Med Inf Decis Mak. 2020;20(1):334.
Härter M, Dirmaier J, Scholl I, Donner-Banzhoff N, Dierks ML, Eich W, Müller H, Klemperer D, Koch K, Bieber C. The long way of implementing patient-centered care and shared decision making in Germany. Z Evid Fortbild Qual Gesundhwes. 2017;123–124:46–51.
Stolz-Klingenberg C, Bünzen C, Coors M, Flüh C, Margraf NG, Wehkamp K, Clayman ML, Scheibler F, Wehking F, Rüffer JU, Schüttig W, Sundmacher L, Synowitz M, Berg D, Geiger F. Sustainability of large-scale implementation of shared decision making with the SHARE TO CARE program. Front Neurol. 2022;13:1–9.
Diekmann A, Heuser C, Schellenberger B, Bohmeier B, Holmberg C, Ansmann L, Ernstmann N. Patient participation in multidisciplinary tumor conferences: providers’ perceptions of patients’ need satisfaction and emotional experiences. Psychooncology. 2020;29(8):1263–71.
Budde H, Williams GA, Winkelmann J, Pfirter L, Maier CB. The role of patient navigators in ambulatory care: overview of systematic reviews. BMC Health Serv Res. 2021;21(1):1166.
Gödde K, Fügemann H, Desch A, Stumm J, Schindel D, Rieckmann N, Meisel A, Müller-Nordhorn J, Goerling U, Holmberg C. Development of a patient-oriented navigation model for patients with lung cancer and stroke in Germany. BMC Health Serv Res. 2022;22(1):785.
Porzig R, Neugebauer S, Heckmann T, et al. Evaluation of a cancer patient navigation program (onkolotse) in terms of hospitalization rates, resource use and healthcare costs: rationale and design of a randomized, controlled study. BMC Health Serv Res. 2018;18:413.
Feiten S, Scholl I, Dünnebacke J, et al. Shared decision-making in routine breast cancer care inGermany-A cross-sectional study. Psychooncology. 2022;31(7):1120–6.
Maes-Carballo M, Martín-Díaz M, Mignini L, Khan KS, Trigueros R, Bueno-Cavanillas A. Evaluation of the Use of Shared Decision Making in Breast Cancer: International Survey. Int J Environ Res Public Health. 2021;18(4):2128. d.
Bohmeier B, Schellenberger B, Diekmann A, Ernstmann N, Ansmann L, Heuser C. Opportunities and limitations of shared decision making in multidisciplinary tumor conferences with patient participation - A qualitative interview study with providers. Patient Educ Couns. 2021;104(4):792–9.
Osborn M, Johnson R, Thompson K, et al. Models of care for adolescent and young adult cancer programs. Pediatr Blood Cancer. 2019;66(12):27991.
Dougherty E, Pierce B, Ma C, Panzarella T, Rodin G, Zimmermann C. Factors associated with work stress and professional satisfaction in oncology staff. Am J Hosp Palliat Care. 2009;26(2):105–11.
Ziegler E, Nickel S, Trojan A, Klein J, Kofahl C. Self-help friendliness in cancer care: a cross-sectional study among self-help group leaders in Germany. Health Expect. 2022;25(6):3005–16.
European Observatory on Health Systems and Policies. Diagnosis related groups in Europe. 2011. Available online: https://eurohealthobservatory.who.int/docs/librariesprovider3/studies---external/diagnosis_related_groups.pdf?sfvrsn=55ad0545_1&download=true (accessed 5 May 2023).
Arndt V, Doege D, Fröhling S, et al. Cancer care in German centers of excellence during the first 2 years of the COVID-19 pandemic. J Cancer Res Clin Oncol. 2023;149(2):913–9.
Baxter S, Johnson M, Chambers D, Sutton A, Goyder E, Booth A. The effects of integrated care: a systematic review of UK and international evidence. BMC Health Serv Res. 2018;18(1):350.
Ellegaard MB, Grau C, Zachariae R, Bonde Jensen A. Fear of cancer recurrence and unmet needs among breast cancer survivors in the first five years. A cross-sectional study. Acta Oncol. 2017;56(2):314–20.
Arditi C, Eicher M, Colomer-Lahiguera S, Bienvenu C, Anchisi S, Betticher D, Dietrich PY, Duchosal M, Peters S, Peytremann-Bridevaux I. Patients’ experiences with cancer care in Switzerland: results of a multicentre cross-sectional survey. Eur J Cancer Care. 2022;31(6):e13705.
Steeb T, Wessely A, Merkl H, et al. Experiences of In-Patients with skin Cancer in a German University Hospital setting: a cross-sectional survey. Patient Prefer Adherence. 2021;15:41–8.
Aelbrecht K, Hanssens L, Detollenaere J, Willems S, Deveugele M, Pype P. Determinants of physician-patient communication: the role of language, education and ethnicity. Patient Educ Couns. 2019;102(4):776–81.
Heerdegen ACS, Petersen GS, Jervelund SS. Determinants of patient satisfaction with cancer care delivered by the Danish healthcare system. Cancer. 2017;123(15):2918–26.
Nguyen TV, Bosset JF, Monnier A, et al. Determinants of patient satisfaction in ambulatory oncology: a cross sectional study based on the OUT-PATSAT35 questionnaire. BMC Cancer. 2011;11:526.
Bieber C, Nicolai J, Müller KG, Eich W. Der Fragebogen Zur Arzt-Patient-Interaktion (FAPI)– validierung und psychometrische Optimierung anhand einer stichprobe chronischer Schmerzpatienten. Klin Diagnostik Evaluation. 2011;4(1):78–93.
Mayring PH, Fenzl T. Qualitative inhaltsanalyse. In: Baur N, Blasius J, editors. Handbuch Methoden Der Empirischen Sozialforschung. Springer; 2022. pp. 691–706.
Härter M, Dirmaier J, Scholl I. Abschlussbericht Zum Projekt Validierung Und Normierung Des Fragebogens Zur Partizipativen Entscheidungsfindung (PEFFB) bei chronischen Erkrankungen. Hamburg: Universitätsklinikum Hamburg Eppendorf. 2010. https://doi.org/10.2314/GBV:683341022. Available online.
Tremblay D, Roberge D, Berbiche D. Determinants of patient-reported experience of cancer services responsiveness. BMC Health Serv Res. 2015;15:425.
Faller H, Weis J, Koch U, Brähler E, Härter M, Keller M, Schulz H, Wegscheider K, Boehncke A, Hund B, Reuter K, Richard M, Sehner S, Wittchen HU, Mehnert A. Utilization of professional psychological care in a large German sample of cancer patients. Psychooncology. 2017;26(4):537–43.
Covvey JR, Kamal KM, Gorse EE, et al. Barriers and facilitators to shared decision-making in oncology: a systematic review of the literature. Support Care Cancer. 2019;27(5):1613–37.
Tremblay D, Roberge D, Touati N, Maunsell E, Berbiche D. Effects of interdisciplinary teamwork on patient-reported experience of cancer care. BMC Health Serv Res. 2017;17(1):218.
Acknowledgements
The authors would like to thank the peer support organisations, cancer care facilities involved and all participants.
Funding
This work was supported by the German Cancer Aid (grant number 70113227).
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
CK, JK and EZ planned and conducted the study. CK and EZ collected the data. EZ developed the manuscript outline, analysed the data, interpreted the results and wrote the manuscript. CK and JK provided critical remarks to the manuscript draft. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The questionnaire, methodology and data protection regulations for this study were approved by the Local Psychological Ethics Committee at the Centre for Psychosocial Medicine, University Medical Centre Hamburg (Ethics approval number: LPEK-0109). Informed consent was obtained from all individual participants on the basis of study information and data privacy statement.
Consent for publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ziegler, E., Klein, J. & Kofahl, C. Patient experiences and needs in cancer care– results from a nationwide cross-sectional study in Germany. BMC Health Serv Res 24, 572 (2024). https://doi.org/10.1186/s12913-024-10951-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-024-10951-y