Abstract
Background
Healthcare regulators in many countries undertake inspections of healthcare providers and publish inspection outcomes with the intention of improving quality of care. Comprehensive inspections of general practices in England by the Care Quality Commission began for the first time in 2014. It is assumed that inspection and rating will raise standards and improve care, but the presence and extent of any improvements is unknown. We aim to determine if practice inspection ratings are associated with past performance on prescribing indicators and if prescribing behaviour changes following inspection.
Methods
Longitudinal study using a dataset of 6771 general practices in England. Practice inspection date and score was linked with monthly practice-level data on prescribing indicators relating to antibiotics, hypnotics and non-steroidal anti-inflammatory drugs. The sample covers practices receiving their first inspection between September 2014 and December 2018. Regression analysis and the differential timing of inspections is used to identify the impact on prescribing.
Results
Better-rated practices had better prescribing in the period before inspections began. In the six months following inspections, no overall change in prescribing was observed. However, the differences between the best and worse rated practices were reduced but not fully. The same is also true when taking a longer-term view. There is little evidence that practices responded in anticipation of inspection or reacted differently once the ratings were made public.
Conclusion
While some of the observed historic variation in prescribing behaviour has been lessened by the process of inspection and ratings, we find this change is small and appears to come from both improvements among lower-rated practices and deteriorations among higher-rated practices. While inspection and rating no doubt had other impacts, these prescribing indicators were largely unchanged.
Similar content being viewed by others
Background
Healthcare regulators in many countries undertake inspections of healthcare providers and publish the outcomes of those inspections in some form, with the intention of promoting compliance with inspection standards or other guidance and so improving the quality of care [1]. Despite the widespread use of such inspections, their mechanism of action and their impact is poorly understood and often contentious [2,3,4].Furthermore, most research has focused on secondary care and recent systematic review highlights the lack of knowledge on the impact of inspection in primary care, both internationally and in the UK in particular [5].
In England, high-profile failures in the provision of care in some hospitals led to a public inquiry and several critical reports by government and parliament [6,7,8,9,10].This attention resulted in questions being raised about the ability of the healthcare regulator, the Care Quality Commission (CQC), to adequately fulfil its role to monitor and oversee the quality of health and social care. A new CQC regulation model was developed in response to these concerns and the CQC began to implement this model in 2014 [11].
The new model included a programme of extensive inspection and rating of all general practices in England, approximately 7000 practices. The first practices were inspected in September 2014 and had their inspection ratings published in November 2014. When inspecting practices, the CQC focused on five key domains of care: Safe, Effective, Responsive, Caring and Well-led plus an additional Overall rating, which aggregates the ratings from each domain. On each of these six, a rating of ‘Outstanding’, ‘Good’, ‘Requires Improvement’ or ‘Inadequate’ was awarded. The inspection ratings received must be displayed by the practice in an area visible to patients.
In addition to inspecting and rating practices, the CQC also monitored practice performance using a range of performance measures under its Intelligent Monitoring system [12,13,14]. For general practices, this monitoring included four indicators relating to the prescribing behaviour of practices. These four indicators targeted the prescribing of antibiotics, hypnotics and non-steroidal anti-inflammatory drugs due to concerns about patient safety from over-prescribing of these drugs. The importance of appropriate antibiotic prescribing has been highlighted by the Chief Medical Officer [15] and by the United Nations [16]. Overuse of hypnotics is linked to higher mortality [17], while overuse of selected non-steroidal anti-inflammatory drugs is linked to greater cardiovascular risk [18].
The relationship between CQC inspection and performance has been investigated in secondary care but not in primary care [19, 20]. Our aim was to determine if practice rating scores were associated with past performance on these four prescribing indicators and also if prescribing behaviour changed following the inspection.
Methods
Data
To analyse the response of practice prescribing to healthcare regulation we used two sources of data: (1) CQC inspection and ratings data [21] and (2) general practice prescribing data [22]. We also controlled for practice population size [23].
CQC inspection and ratings data were provided by the CQC. These data included the inspection date, rating publication date and the inspection rating score for general practices which received their first inspection between September 2014 and December 2018. The Overall rating is used throughout this study as it represents how the practice performance was assessed over a range of areas, giving the most complete indication of quality.
General practices prescribing data contained monthly prescribing data for all practices in England for the period April 2013 to June 2019, detailing the total number of items for each medicine prescribed by the practice in each month [22].
The following indicators were generated from the prescribing data:
-
1.
Total number of antibacterial drug items per 100 Specific-Therapeutic-Group-Age-sex weightings-Related Prescribing-Units (STAR-PUs). STAR-PUs were used to adjust for those practices expected to use more of a certain drug type due to differences in demographics, usually due to an older population [24, 25]. Overuse of antibiotics can result in antibacterial resistance. They should only be used when appropriate to maintain their effectiveness. Practices which prescribe a large number of antibacterial drugs may be using them inappropriately. A higher value on this indicator may suggest poor prescribing behaviour.
-
2.
Broad-spectrum antibiotics as a percentage of all antibiotics. Narrow-spectrum antibiotics are often cheaper and effective against specific bacterial infections. They should be used instead of broad-spectrum antibiotics, unless they are known to be ineffective against the target bacteria. A higher value on this indicator suggests poor prescribing behaviour.
-
3.
Total number of hypnotic drug items per 1000 STAR-PUs. When used for long periods of times these drugs have a high risk of side effects. Their use should be restricted to only appropriate cases. A higher value on this indicator may suggest poor prescribing behaviour.
-
4.
Percentage of Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) that are Ibuprofen and Naproxen. The long-term use of this drug group has been linked to cardiovascular and gastro-intestinal events. Risks are lower for Ibuprofen and Naproxen and therefore their use should be greater. A lower value on this indicator suggests poor prescribing behaviour.
These prescribing indicators were uniquely suitable for our analysis as they were used in the CQC Intelligent Monitoring framework as well as being monitored under the NHS Key Therapeutic Topics [12, 26]. Furthermore, while CQC Intelligent Monitoring included 33 indicators in total, only these four prescribing indicators are generated from data that is freely available at a monthly frequency that would allow the impact of inspection to be investigated.
The data from these sources were linked to form a single dataset on inspections, ratings, prescribing indicators and practice population size for 6990 practices. Data were cleaned to remove 180 practices which closed between April 2013 and June 2019. Additionally, 39 very small practices with fewer than 1000 patients were excluded as practices observed to have fewer than 1000 patients are typically either serving specific populations (such as people experiencing homelessness) or are in the process of closing, opening, or merging. The final analysis sample consisted of 6771 practices.
Analytical approach
First, we assessed the degree to which such prescribing behaviours differed according to subsequent ratings before the inspection cycle began. This would indicate if practice ratings captured either prescribing behaviour directly or other aspects of practice quality that influenced prescribing behaviour. Using data from April 2013 to August 2014, before the earliest inspections, we estimated the association between performance on each prescribing indicator and the inspection rating the practice would go on to receive. We controlled for practice size and prescribing trends, the latter using a set of 17 categorical variables for the sequence of months. A panel data random effects model was used to allow for repeated observations. Where the indicator represented a percentage, the regressions are weighted by the denominator.
Second, we assess if prescribing behaviours changed after inspection. As there was a lag between the inspection visit and the rating being published, changes in prescribing behaviour may have been prompted by the inspection visit, the published inspection rating or both. We hypothesised the strongest effect was likely to follow the inspection visit, as this was the intervention most noticeable to practices. We further hypothesised that changes would differ between practices that received different inspection ratings.
We estimated three specifications, all using a linear fixed effects model, and all using data from April 2013 to June 2019. As practices were inspected at different times throughout 2014–2017, each specification takes advantage of this staggered inspection schedule. Practices act as a control group either before they are ever inspected or outside of the specific inspection period modelled in each specification. Regressions included indicators for month-year and for practice, and practice population size.
Our first specification modelled performance on each prescribing indicator in the six months post-inspection and did not differentiate any changes by inspection rating scores. This provided the overall impact of practice inspection on the selected prescribing indicators.
Our second specification modelled performance on each prescribing indicator by inspection rating score. The inspection rating score is interacted with the post-inspection period covering the inspection month and the six months immediately following. This provided the post-inspection change for each inspection rating score.
Our third specification included the inspection rating score interacted with the month prior to inspection and with the months more than six months post-inspection. This provided any impact in anticipation of inspection and any longer-term impacts on each prescribing indicator.
All model equations and variables are described fully in the online appendix. In additional models we replaced the inspection date with the date the rating was published, typically three months after the inspection. All data analysis were conducted with Stata Version 16.
Results
The majority of practices were rated as Good (79.56%), followed by Requires Improvement (12.94%), Outstanding (4.3%) and Inadequate (3.2%).
Summary statistics for prescribing indicators and practice size in the pre-inspection period are shown in Table 1. On average, practices issued 11.59 antibacterial prescriptions per month per 100 STARPUs and 5.5% of antibiotics prescribed were broad spectrum. Practices issued on average 5.55 hypnotic prescriptions per month per 1000 STARPUs. Of all non-steroidal anti-inflammatory drugs, 67.60% were Ibuprofen/Naproxen. Finally, the average size of the practice population during this period was 7533 patients.
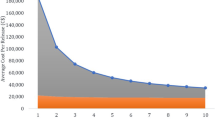
Across all indicators there was evidence of variation in prescribing behaviour according to practice inspection rating score (Fig. 1; Table 2). These differences were in the expected direction, with poorer prescribing behaviour found in practices with worse inspection rating scores. For example, prior to inspection, practices with an Outstanding inspection rating score were prescribing fewer broad spectrum antibiotics and a greater proportion of Ibuprofen/Naproxen.
From Table 2, practices that, when later inspected, received ratings of Requires Improvement or Inadequate generally had worse prescribing behaviour. Of the eight coefficients relating to these ratings, seven suggested worse prescribing behaviour, four of which were statistically significant at p < 0.05 or better. The largest effect was found on the percentage of Ibuprofen/Naproxen, where the coefficient for Inadequate practices suggests these prescribe 3.374% points fewer of the (more desirable) non-steroidal anti-inflammatory drugs [95% CI: -4.837,-1.911]. This difference represented 25% of the standard deviation for this indicator. In contrast, practices with an Outstanding inspection rating tended to perform better than those rated Good. The signs of all four coefficients suggested better prescribing, although only the coefficient on percentage of Ibuprofen/Naproxen was statistically significant.
Table 3 presents results from four regressions, estimating the change in four indicators of prescribing performance in the six months following an inspection. These estimates combine practices receiving all four inspection rating scores and overall these is no statistically significant change.
From Table 4 we observe that practices with poorer inspection ratings (Inadequate or Requires Improvement) improved their prescribing after inspection, while practices with better inspection ratings (Good and Outstanding) worsened. These changes are statistically significant for antibacterial prescriptions in Outstanding practices; for broad spectrum antibiotics in Requires Improvement and Good practices; and for NSAIDs in Requires Improvement practices. For example, in this post-inspection period, practices with a Requires Improvement rating increased their prescribing of Ibuprofen/Naproxen by 0.772% points [95% CI: 0.401,1.143]. This is an improvement in prescribing representing 6% of the standard deviation for this indicator.
Changes in prescribing behaviour in anticipation of an inspection were statistically significant only for practices rated Requires Improvement and only relating to NSAIDs (Table 5). Changes in prescribing behaviour also appear to exist beyond the six-month period previously measured. The sign on all coefficients for Inadequate and Requires Improvement practices suggest improved prescribing in the longer term and six of these eight coefficients are statistically significant at p < 0.05 or better. The sign on all coefficients for Good and Outstanding practices suggest worsening prescribing in the longer term and five of these eight coefficients are statistically significant at p < 0.05 or better.
In supplementary analysis using the date of publication of the rating as the intervention point of interest, we found no substantive differences in how prescribing behaviour changes when compared with the analysis using inspection date presented above.
Discussion
Summary
Prior to inspection, we found statistically significant differences in prescribing indicators according to subsequent rating category. These differences followed the expected pattern, with better prescribing behaviour being associated with better ratings scores.
There was no overall impact of inspection in the six months after practices were inspected when grouping together all inspection rating scores. Prescribing behaviour generally improved for practices rated Inadequate or Requires Improvement, but worsened for those rated Good or Outstanding. In the longer term these different responses to inspection grew and reduce pre-existing variation in prescribing performance by rating.
Strengths and limitations
This was the first study to measure the impact of the comprehensive CQC inspection system in primary care. The prescribing data used was collected for all practices and published at monthly intervals, providing a rich source of information about prescribing behaviour. We controlled for practice size and used panel data methods to control for unobservable differences between practices that could affect their prescribing.
However, our analysis was also limited in its focus on only four prescribing indicators. This was arguably a narrow lens through which to determine practice response to inspection, although these indicators were monitored by the CQC. That most practices were rated as Good is also a limitation for our study, suggesting that many practices may not have been motivated to change or improve.
Comparison with existing literature
External inspections of this type, certainly have the potential to change behaviour and do so via influencing various mediators of organisational change [5]. Similar analysis has also looked at the association between CQC inspections and relevant indicators in hospital maternity and emergency departments [19, 20]. These studies found no association between inspection scores and performance indicators, both when looking at pre- or post-inspection performance. Our findings in primary care depart from this literature slightly in two ways. Firstly, we found modest associations between inspection ratings scores and prior performance. Secondly, we found some small changes post-inspection for practices with different ratings. However, as the post-inspection changes differed by the rating received, they effectively cancelled each other out. This resulted in finding no overall association between inspection and these indicators.
There was also no positive, clinically significant impact on adverse events following hospital inspection [27]. Other interventions to targeting prescribing, such as regulatory risk communications [28], have been more successful in changing behaviour.
Conclusion
Prescribing behaviour, particularly that of antibacterial drugs, is a global issue and healthcare regulation may be one method by which to promote appropriate behaviour. There is some evidence that data on prescribing behaviour was modestly predictive of subsequent inspection ratings for general practices, but it does not seem likely that this relationship would be sufficiently strong to be used in making judgements on whether, when and where to inspect in general practice. This raises some cautions about the capacity to be more responsive and intelligence-led in the inspection programme. While some of the observed historic variation in prescribing behaviour has been reduced by the process of CQC inspection and ratings. This change was small and came from better practices worsening as well as worse practices improving, such that overall prescribing was unchanged by inspection. Though the lack of improvement following inspection might be concerning, especially given the resources dedicated to inspection, research on a wider range of performance measures would be needed before the value of inspection could be determined.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Øyri SF, Bates DW, Wiig S. Comparison of external evaluation policies and regulations for quality improvement and safety of health services in Norway and the United States. International Journal of Health Governance; ahead-of-print. Epub ahead of print 2023. https://doi.org/10.1108/IJHG-06-2023-0065/FULL/PDF.
Flodgren G, Gonçalves-Bradley DC, Pomey M. External inspection of compliance with standards for improved healthcare outcomes. Cochrane Database Syst Reviews; 2016.
Brubakk K, Vist GE, Bukholm G, et al. A systematic review of hospital accreditation: the challenges of measuring complex intervention effects. BMC Health Serv Res. 2015;15:280.
Hovlid E, Husabø G, Teig IL, et al. Contextual factors of external inspections and mechanisms for improvement in healthcare organizations: a realist evaluation. Soc Sci Med. 2022;298:114872.
Hovlid E, Braut GS, Hannisdal E, et al. Mediators of change in healthcare organisations subject to external assessment: a systematic review with narrative synthesis. BMJ Open. 2020;10:e038850.
Francis R. Report of The Mid Staffordshire NHS Foundation Trust Public Inquiry. London, 2013.
National Audit Office. The Care Quality Commission: Regulating the quality and safety of health and adult social care. London, 2011.
House of Commons Health Select Committee. 2012 accountability hearing with the Care Quality Commission. London, 2012.
Department of Health. Performance and capability review of the Care Quality Commission, https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/215158/dh_132791.pdf (2012, accessed 15 September 2023).
Department of Health. Patients First and Foremost. The Initial Government Response to the Report of The Mid Staffordshire NHS Foundation Trust Public Inquiry, https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/170701/Patients_First_and_Foremost.pdf (2013, accessed 1 September 2023).
Care Quality Commission. A new start. Consultation on changes to the way CQC regulates, inspects and monitors care, http://www.cqc.org.uk/sites/default/files/documents/cqc_consultation_2013_tagged_0.pdf (2013, accessed 1 September 2023).
Care Quality Commission. Intelligent Monitoring. NHS GP practices. Indicators and methodology. London, 2015.
Griffiths A, Beaussier A-L, Demeritt D et al. Intelligent Monitoring? Assessing the ability of the Care Quality Commission’s statistical surveillance tool to predict quality and prioritise NHS hospital inspections. Qual Health Care 2016; bmjqs-2015-004687-.
Allen T, Walshe K, Proudlove N, et al. Using quality indicators to predict inspection ratings: cross-sectional study of general practices in England. Br J Gen Pract. 2020;70. https://doi.org/10.3399/bjgp19X707141. Epub ahead of print.
Davies SC. Annual Report of the Chief Medical Officer. Volume, Two. 2011. Infections and the rise of antimicrobial resistance, https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/138331/CMO_Annual_Report_Volume_2_2011.pdf (2013, accessed 21 September 2023).
World Health Organization. Antimicrobial resistance: global report on surveillance 2014, http://apps.who.int/iris/bitstream/10665/112642/1/9789241564748_eng.pdf?ua=1 (2014, accessed 21 September 2023).
Weich S, Pearce HL, Croft P, et al. Effect of anxiolytic and hypnotic drug prescriptions on mortality hazards: retrospective cohort study. BMJ. 2014;348:g1996–1996.
Trelle S, Reichenbach S, Wandel S, et al. Cardiovascular safety of non-steroidal anti-inflammatory drugs: network meta-analysis. BMJ. 2011;342:c7086–7086.
Allen T, Walshe K, Proudlove N, et al. Measurement and improvement of emergency department performance through inspection and rating: an observational study of emergency departments in acute hospitals in England. Emerg Med J. 2019;36:326–32.
Allen T, Walshe K, Proudlove N, et al. The measurement and improvement of maternity service performance through inspection and rating: an observational study of maternity services in acute hospitals in England. Health Policy (New York). 2020;124:1233–8.
Care Quality Commission. How to get and re-use CQC information and data, https://www.cqc.org.uk/about-us/transparency/using-cqc-data (2019, accessed 21 June 2023).
NHS BSA. English prescribing data, https://www.nhsbsa.nhs.uk/prescription-data/prescribing-data/english-prescribing-data-epd (2019, accessed 14 June 2023).
NHS Digital. Numbers of Patients Registered at a GP Practice, https://data.gov.uk/dataset/numbers_of_patients_registered_at_a_gp_practice (2019, accessed 22 September 2023).
Lloyd DC, Harris CM, Roberts DJ. Specific therapeutic group age-sex related prescribing units (STAR-PUs): weightings for analysing general practices’ prescribing in England. BMJ. 1995;311:991–4.
NHS Digital. Prescribing measures, indicators and comparators, https://webarchive.nationalarchives.gov.uk/ukgwa/20180307182940/http://content.digital.nhs.uk/prescribing/measures (2017, accessed 10 September 2023).
Health & Social Care Information Centre. Medicines OptimisationKey Therapeutic Topics Comparators 2015/16, https://webarchive.nationalarchives.gov.uk/ukgwa/20180307195533mp_/http://content.digital.nhs.uk/media/18422/Descriptions-and-Specifications-201516/pdf/Descriptions_and_Specifications_2015_16.pdf (2015, accessed 22 September 2023).
Castro-Avila A, Bloor K, Thompson C. The effect of external inspections on safety in acute hospitals in the National Health Service in England: A controlled interrupted time-series analysis. J Health Serv Res Policy. 2019. https://doi.org/10.1177/1355819619837288.
Weatherburn CJ, Guthrie B, Dreischulte T, et al. Impact of medicines regulatory risk communications in the UK on prescribing and clinical outcomes: systematic review, time series analysis and meta-analysis. Br J Clin Pharmacol. 2020;86:698–710.
Acknowledgements
The authors would like to acknowledge the support of the Care Quality Commission in providing data for this study.
Funding
The report is an output from independent research commissioned and funded by the NIHR Policy Research Programme (PR-R11-0914-12001 Provider ratings: the effects of the Care Quality Commission’s new inspection and rating system on provider performance). The views expressed in the publication are those of the author(s) and not necessarily those of the NHS, the NIHR, the Department of Health, ‘arms’ length bodies or other government departments.
Author information
Authors and Affiliations
Contributions
All authors devised the analysis. TA prepared the data, conducted the analysis and prepared first draft. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
No human participation. Ethical approval was not required for this study.
Consent for publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Allen, T., Walshe, K., Proudlove, N. et al. Association between regulator inspection and ratings on primary care prescribing: an observational study in England 2014 to 2019. BMC Health Serv Res 24, 679 (2024). https://doi.org/10.1186/s12913-024-10906-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-024-10906-3