Abstract
Background
Indigenous adolescents access primary health care services at lower rates, despite their greater health needs and experience of disadvantage. This systematic review identifies the enablers and barriers to primary health care access for Indigenous adolescents to inform service and policy improvements.
Methods
We systematically searched databases for publications reporting enablers or barriers to primary health care access for Indigenous adolescents from the perspective of adolescents, their parents and health care providers, and included studies focused on Indigenous adolescents aged 10–24 years from Australia, Canada, New Zealand, and United States of America. Results were analyzed against the WHO Global standards for quality health-care services for adolescents. An additional ninth standard was added which focused on cultural safety.
Results
A total of 41 studies were included. More barriers were identified than enablers, and against the WHO Global standards most enablers and barriers related to supply factors – providers’ competencies, appropriate package of services, and cultural safety. Providers who built trust, respect, and relationships; appropriate package of service; and culturally safe environments and care were enablers to care reported by adolescents, and health care providers and parents. Embarrassment, shame, or fear; a lack of culturally appropriate services; and privacy and confidentiality were common barriers identified by both adolescent and health care providers and parents. Cultural safety was identified as a key issue among Indigenous adolescents. Enablers and barriers related to cultural safety included culturally appropriate services, culturally safe environment and care, traditional and cultural practices, cultural protocols, Indigenous health care providers, cultural training for health care providers, and colonization, intergenerational trauma, and racism. Nine recommendations were identified which aim to address the enablers and barriers associated with primary health care access for Indigenous adolescents.
Conclusion
This review provides important evidence to inform how services, organizations and governments can create accessible primary health care services that specifically meet the needs of Indigenous adolescents. We identify nine recommendations for improving the accessibility of primary health care services for Indigenous adolescents.
Similar content being viewed by others
Background
Adolescence is an important period of development across the life-course, the period between childhood and adulthood, which is now broadly considered to be between the ages of 10–24 years [1]. This period of life is defined by critical biological, neurocognitive, and social role transitions [1, 2] and a manifestation of this is the shift from childhood diseases and illness to those more prevalent in adolescents, sexual and reproductive health, mental health, injury, drug and alcohol misuse, obesity, and early onset of chronic disease [2, 3]. Adolescence is also a critical time for engagement with health care services, as it is the phase where adolescents shift from accessing care with parents to accessing care independently, and a time to not only to address emergent health needs of adolescents, but also to identify and address risks for future and intergenerational health.
To meet the health and wellbeing needs of adolescents requires access to quality health care for all adolescents, which is now recognised in global health policy [4,5,6]. Accessible and responsive primary health care services are essential to addressing the health care needs of adolescents, as well as optimising opportunities for health promotion and prevention. Yet we know in many settings, adolescents infrequently access health care and/or forego care when it is needed [7]. Barriers to health care experienced by adolescents include a lack of experience and knowledge in relation to health care access, a lack of privacy and confidentiality, a lack of suitable services, location of services, cost, stigma, cultural and community attitudes, legislation and other legal frameworks which impact access for adolescents [8,9,10].
In Australia, adolescents and especially adolescent males are less likely than any other population group to access primary health care services [11]. Data from Australia’s universal health care insurance scheme Medicare indicates that in 2018–19, males aged 10–14 years on average received 5.8 Medicare services per capita, the lowest number of services than any other population group, followed by males aged 15–19 and 20–24 years who received on averaged 6.2 Medicare services per capita [12]. A study by Slade et al. [13], found Australian males aged 16–24 years had the lowest service use for mental health problems compared to any other population group (13% vs 18% for males aged 75–85 year-second lowest group). Similarly, in Canada, New Zealand and United States of America (USA), adolescents are less likely to use primary health care services than any other age groups [14,15,16,17,18,19]. Within these settings, Indigenous adolescents appear to have particularly low access to services, despite their greater health needs compared to their non-Indigenous counterparts [20,21,22,23,24,25]. In Australia, in 2022, 223,877 Aboriginal and Torres Strait Islander Peoples Health Assessment (Medicare Item 715) were conducted, 15% of those Health Assessments were competed by Aboriginal and Torres Strait Islander adolescents aged 15–24 years [26]. This corresponds to 20% of Aboriginal and Torres Strait Islander young population aged 15–24 years having had a Health Assessment in 2022 [26]. Despite the intentions of the Health Assessments, which recognises the unique health and wellbeing needs of Aboriginal and Torres Strait Islander people and encourages engagement in comprehensive primary health care [27], adolescents were less likely to use primary health care services than any other Aboriginal and Torres Strait Islander population group [20, 26]. To date, there has not been a systematic analysis of the enablers and barriers to primary health care access among Indigenous adolescents.
Australia, Canada, New Zealand, and USA all have similar policy frameworks for their Indigenous populations, funding mechanisms, and Indigenous-specific health care services [28,29,30,31,32,33,34]. These services have evolved from an identified need to deliver health care to Indigenous communities that is culturally safe, often as a result of mainstream services failing to provide culturally safe care for Indigenous communities [28]. However, these services have traditionally been designed to target the health needs of mothers, babies and young children (where excess mortality has historically occurred) and adults (burden of chronic illness) [35]. Indigenous adolescents may also experience unique obstacles due to the ongoing effects of colonisation and their impact on the social determinants of health – dispossession of land and country, intergenerational trauma, child removal, racism, and inequity [36,37,38]. Furthermore, Indigenous adolescents comprise a large proportion of the Indigenous population, for example, in Australia, Indigenous adolescents aged 10–24 years make up 30% of Australia’s Indigenous population [39] and experience a large burden of preventable ill health [21].
This review aimed to identify the enablers and barriers experienced by Indigenous adolescents accessing primary health care services as described by Indigenous adolescents, their family members and health care providers, from Australia, Canada, New Zealand, and USA.
Methods
Search strategy and selection criteria
The review study protocol was registered with PROSPERO [CRD42021268266]. This review was reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [40]. Literature from Jan 1, 2002, to December 13, 2023, were compiled from MEDLINE (PubMed), EBSCOhost (CINAHL Complete; and PsycInfo), Embase, Scopus, Web of Science (Core Collection), Ovid (EMCARE), Informit (Health Collection; Humanities & Social Sciences Collection; Indigenous Collection; and Aboriginal and Torres Strait Islander Health Bibliography), PHCRIS, Circumpolar Health, Native Health, and HealthInfoNet databases. Key search terms were used (Indigenous, adolescent, primary health care, Australia, Canada, New Zealand and USA) (Additional file 1) to identify studies from Australia, Canada, New Zealand and USA that identified enablers and barriers experienced by Indigenous adolescents accessing primary health care, including those with a focus on antenatal care, mental health, sexual health, drug and alcohol substance abuse and rehabilitation, from the perspective of either the individual, their parents/guardians/community members or healthcare providers. We focus on studies from Australia, Canada, New Zealand and USA, as Indigenous populations from these high-income countries have similar shared experiences of colonization and similar health policies [41, 42]. Indigenous peoples were defined as individuals and communities who identify as being Indigenous or First Nations [43]; and adolescents were defined as individuals between the ages of 10–24 years, as its algins with ‘contemporary patterns of adolescent growth and popular understandings of this life phase’ ([1], p.1). Studies that contained both Indigenous and non-Indigenous adolescents were included if greater than 50% of participants were Indigenous, and studies where the proportion of adolescents was representative of the adolescent population in the region studied [19], or data were disaggregated by Indigenous status. Studies were included if they were primary qualitative, quantitative, or mixed method studies, including evaluations, and reports and other grey literature (from PHCRIS, Circumpolar Health, Native Health, and HealthInfoNet databases). The review excluded review articles, editorials, and perspectives. Articles were limited to those published in English. Studies were excluded if they did not identify enablers and barriers experienced by Indigenous adolescents accessing primary health care or focused on preventative health intervention programs delivered outside of primary health care, including vaccination, contraception, and physical activity programs, screening programs (mental health, sexual health, cardiovascular health) and harm reduction initiatives (smoking cessation, needle, and syringe exchange), as we focused on the responsive care side of primary health care, e.g. treatment and management of acute and chronic conditions. The reference list of included studies were reviewed for additional studies.
The review team consisted of Aboriginal (SH, TP) and non-Indigenous individuals (PA, ES), with expertise in Aboriginal and Torres Strait Islander health (SH, TP, PA), adolescent health (PA), health services research (SH, PA) and systematic reviews (SH). Title and abstract and full-text review were conducted according to the inclusion and exclusion criteria by two independent reviewers (SH, TP, PA). Conflict between reviewers were resolved by reaching an agreement through discussion and or with another reviewer. Inter-rater reliability between reviewers at title and abstract screening and full text review were moderate (0.67 and 0.73, respectively).
Data extraction and quality appraisal
Data extraction was completed by two independent reviewers (SH and ES). Information extracted from each study included, but was not limited to, author, year, country where study was conducted, geographical setting, population and characteristics of participants, study design, phenomena of interest, and identified enablers and barriers experienced by Indigenous adolescents accessing primary health care. Due to the small number of quantitative studies, quantitative data was converted into ‘qualitized data’. This involved transforming quantitative data into textual descriptions or narrative interpretation of the quantitative results [44]. Following the data extraction process, quality appraisal was performed by two independent reviewers (SH, ES) using tools developed by Joanna Briggs Institute [44]; and the Aboriginal and Torres Strait Islander Quality Appraisal Tool, which assesses the quality of health research from an Indigenous perspective [45]. The Aboriginal and Torres Strait Islander Quality Appraisal Tool was modified to be inclusive of Indigenous populations from Australia, Canada, New Zealand, and USA. The abstract, full-text review, data extraction and quality appraisal were completed using EndNote and Covidence Software [46, 47].
Data analysis
The World Health Organization (WHO) Global standards for quality health-care services for adolescents [6] (Global standards) were adapted and used to explore the enablers and barriers to primary health care for Indigenous adolescents. The Global standards provide guidance for improving the quality of health care services and delivery for adolescents and consider how health systems respond to the health needs of adolescents using a human rights-based approaches to health. In addition to the eight Global standards [6], we included a ninth standard: cultural safety, which encapsulates the unique cultural needs and experience of Indigenous adolescents when accessing primary health care services (Table 1). Cultural safety is defined as:
Cultural safety is not defined by the health professional, but is defined by the health consumer’s experience—the individual’s experience of care they are given, ability to access services and to raise concerns. The essential features of cultural safety are:
- a)
An understanding of one’s culture
- b)
An acknowledgment of difference, and a requirement that caregivers are actively mindful and respectful of difference(s)
- c)
It is informed by the theory of power relations; any attempt to depoliticise cultural safety is to miss the point
- d)
An appreciation of the historical context of colonisation, the practices of racism at individual and institutional levels, and their impact on First Nations people’s living and wellbeing, both in the present and past
- e)
Its presence or absence is determined by the experience of the recipient of care and not defined by the caregiver [48]
Furthermore, these standards were divided into two groups: supply (individual or community level factors that facilitate or prevent access to health care services) and demand (health care system level factors that facilitate or prevent health care service uptake), as health care access is often considered in relation to these two concepts [49]. Findings were thematically analyzed and synthesized using meta-aggregation [44] under each Global standard, and analyzed by service type/focus (primary health care, mental health, and sexual and reproductive health), and urban status, as most Indigenous health research is conducting in rural and remote settings [50]. Urban was defined as the area or region surrounding a (capital) city [51].
Results
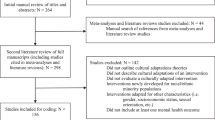
Our search identified 15,702 articles. After abstract review (screening), 144 were deemed potentially relevant. Of these, 103 were excluded after full text review (Additional file 1). In total 41 studies were included in the systematic review (Fig. 1).
Of the 41 studies, most had an overall high-quality assessment against the Joanna Briggs Institute tools except for two studies (Additional file 1) and inter-rater reliability between the two reviewers was high [52, 53]. However, against the Aboriginal and Torres Strait Islander Quality Appraisal Tool, which assesses research quality from an Indigenous perspective, 12 rated high [54,55,56,57,58,59,60,61,62,63,64], 12 medium [61, 65,66,67,68,69,70,71,72,73,74], and 17 poor [24, 52, 53, 75,76,77,78,79,80,81,82,83,84,85,86] (Additional file 1). The overall quality was limited by insufficient description of most criteria, particularly on agreements in relation to intellectual and cultural property, control over the collection and management of research material, capacity strengthening and opportunities to learn, Indigenous research paradigm, and Indigenous governance.
Table 2 summarizes the characteristics of included studies. The majority of studies were from Australia [52, 53, 55, 56, 59, 61,62,63, 69, 74, 76, 78,79,80,81,82, 85, 87, 88], followed by Canada [54, 57, 58, 64, 66, 68, 86, 89], New Zealand [60, 70,71,72,73, 75, 90, 91], and USA [24, 65, 67, 77, 83, 84]. Of the 41 studies, 20 were conducted in or focused on primary health care services [52, 55, 56, 59, 61, 65, 66, 68,69,70, 72, 79,80,81, 83, 85, 87,88,89,90], 15 were conducted on mental health [53, 54, 57,58,59,60, 63, 67, 73, 74, 77, 80, 82, 84, 85], ten on sexual and reproductive health including maternal health [55, 61, 62, 66, 70, 71, 79, 83, 87, 91], and the remaining studies were on health care access [56, 68, 72, 81], health and wellbeing [24, 86], alcohol and other drugs [75, 76], transgender and two-spirit health [65], asthma [64], skin infections [69], physical disability [78], and health knowledge mobilization [89]. Most studies reported results from the perspective of adolescents [24, 52,53,54,55,56, 60,61,62,63,64, 66, 67, 70, 71, 73, 75,76,77,78,79, 81,82,83,84, 87, 90, 91], with the majority of studies involving older adolescents, and conducted in non-urban or a combination of non-urban and urban settings [24, 52,53,54,55,56,57,58,59,60,61,62,63,64,65,66, 68, 69, 72,73,74,75, 77,78,79,80,81, 87,88,89, 91]. Results are presented based on settings and themes – primary health care, mental health, sexual and reproductive health, and urban status.
Primary health care
Table 3 describes the enablers and barriers associated with Indigenous adolescents accessing primary health care services from the perspective of adolescents and health care providers and parents/guardians/community members. Of the 20 studies conducted in or focused on primary health care services [52, 55, 56, 59, 61, 65, 66, 68,69,70, 72, 79,80,81, 83, 85, 87,88,89,90], 11 of those studies were from the perspective of adolescents [52, 55, 56, 61, 66, 70, 79, 81, 83, 87, 90], with most from the perspective of female and older adolescents, and four were conducted in urban settings [70, 83, 85, 89, 90] with another four conducted in both urban and non-urban settings [56, 59, 65, 81]. Both adolescents and health care providers and parents/guardians/community members reported more barriers than enablers, with more enablers and barriers identified under the five standards relating to supply by both groups. No study reported enablers and barriers associated with the data and quality improvement standard (demand).
Factors identified as Providers’ Competencies were common enablers reported by adolescents, including providers who built trust, respect, and relationships with adolescents and families, these were described as facilitating health seeking behavior, health service engagement and access to services [52, 55, 61, 66, 83, 87]; and providers who maintain privacy and confidentiality [52, 83] and were honest, non-judgmental and had good communication skills were seen to have positive provider qualities, which provided for a positive experience [52, 61, 83, 87]. As were factors identified relating to Appropriate Package of Services, particularly the provision of additional services such as outreach, telehealth, social support, and transport facilitated access to services among adolescents [52, 55, 61, 83, 87, 90]. Adolescents also reported factors related to Cultural Safety, specifically the provision of culturally safe environments and care, which acknowledged and reflected adolescents’ culture and beliefs through the inclusion of cultural practices and protocols, these were also considered enablers by adolescents [52, 55, 61, 83, 87]. Embarrassment, shame, or fear (Equity and Non-discrimination) was a common barrier reported by adolescents and often prevent adolescents from seeking and accessing services [55, 61, 66, 81, 87]. Similarly, a low level of health literacy among adolescents including a lack of health seeking behaviors and awareness of services were barriers to adolescents seeking care (Adolescent Health Literacy) [55, 56, 61, 81].
Health care providers and parents/guardians/community members also reported, providers who built trust, respect, and relationships with adolescents and their families (Providers’ Competencies) [59, 65, 69, 88], and positive provider qualities, such as providers who were welcoming, attentive and non-judgmental, had good communication skills, and a positive attitude [59, 69, 79, 88], were commonly reported enablers associated with Indigenous adolescents accessing primary health care services. Health care providers and parents/guardians/community members identified several factors related to Cultural Safety, which were barriers to adolescents and their family’s ability to engage with and access services: colonization and intergenerational trauma limited understanding and knowledge of Indigenous culture and systemic issues such as racism, marginalization, and inequality impact access [65]; not all services were considered culturally safe for Indigenous adolescents [59, 65]; the absence of culture and language were barriers to engaging and communicating with adolescents and their families [69]; no integration or disconnect between western and traditional health and cultural practices [69, 80]; a lack of Indigenous health care providers [69]; and inadequate training on Indigenous cultural [59] and gender and sexuality within the Indigenous context [65]. Similarly, health care providers and parents/guardians/community members recognized several factors as barriers associated with Providers’ Competencies, such as a lack of provider privacy, confidentiality, and trust [59, 79]; previous negative experience with providers [69]; providers reluctant to engage with adolescents and their families [68]; and a lack of specific training and experience in adolescent health, Indigenous culture, LGBTQ [59, 65, 69], impacted adolescents and their families utilization of services and affected providers ability to provider appropriate care.
Mental health
Of the fifteen studies conducted in or focused on mental health services, adolescents and health care providers and parents/guardians/community members reported more enablers than barriers (Table 4). Adolescents reported self-determination and empowerment (Adolescents’ Participation), and their involvement in care and decision making to be important enablers related to adolescents’ participation [60, 67, 73, 82]. This was also recognized by health care providers and parents/guardians/community members as an enabler [67]. Additionally, adolescent, reported several factors associated with Appropriate Package of Services, such as availability of providers and services, and flexible approach to care and pathways [60, 73, 82]; Providers’ Competencies [53, 60, 82]; and Cultural Safety, for example, the provision of traditional healing practices, and the Indigenous workforce and their role in the provision of cultural safe care [53, 60, 67, 82], as significant enablers to their access and utilization of mental health services. Adolescents reported barriers across seven of the nine standards, except for Data and Quality Improvement, and Adolescents’ Participation.
Health care providers and parents/guardians/community members reported several enablers which were identified relating to Appropriate Package of Services: adolescent appropriate care [58]; availability of providers and services [57, 74]; provision of services including multi-disciplinary team, outreach services and transport [58, 59, 67, 74]; flexible approach to care and pathways [59]; continuity of care between providers and services [58]; funding for services and resources [58]; and the use of social media to promote services and increase engagement with adolescents [58], were all considered enablers that facilitated access to care for adolescents. Additionally, health care providers and parents/guardians/community members reported several enablers relating to all other standards expect for Equity and Non-discrimination, and Data and Quality Improvement (Table 4). Similarly, health care providers and parents/guardians/community members reported barriers across most standards except for Data and Quality Improvement.
Sexual and reproductive health
Of the ten studies conducted in or focused on sexual and reproductive health, a similar number of enablers and barriers were identified, with most of them associated with the five standards related to supply and reported by adolescents (Table 5). Most of the enablers reported by adolescents related to Appropriate Package of Services, Providers’ Competencies, and Cultural Safety, whereas the majority of the barriers related to Appropriate Package of Services, Providers’ Competencies, Facility Characteristics, and Adolescent Health Literacy. Barriers identified as Facility Characteristics included, location of services [55] and access to and proximity to public transport [61, 87], opening hours [79], inability to pre-book appointments [55], and a lack of separate entrances and waiting rooms for men and women and privacy of waiting rooms [55]; and barriers associated with Adolescent Health Literacy include, an assumed or lower level of health literacy [55, 61, 91], communication skills and attitudes of adolescents, and adolescents’ ability to make and maintain appointments [61, 87].
Among health care providers and parents/guardians/community members only two enablers were identified: availability of providers (Appropriate Package of Services) [57], and parent/family and community engagement and involvement in care (Community Support) [62]; and seven barriers across seven of the nine standards: workforce challenges (Appropriate Package of Services) [65, 66], a lack of provider privacy, confidentiality and trust (Providers’ Competencies) [62, 66, 79], location of services (Facility Characteristics) [79], embarrassment, shame, or fear (Equity and Non-discrimination) [79], a lower level of health literacy [79] and health seeking behavior [65] (Adolescent health literacy), a lack of community and family acceptance or support (Community Support) [62], and disempowerment (Adolescents’ participation) [66].
Urban status
Overall, there were more studies conducted in non-urban settings and therefore more enablers and barriers identified by both adolescents and health care providers and parents/guardians/community members in non-urban settings compared to urban settings (Table 6). Furthermore, there were similarities and differences in the enablers and barriers identified relating to eight of the nine standards across the two settings. Notable similarities identified as enablers were associated with Provider Competencies—provider trust, respect, and relationships with adolescents and families [52, 55, 66, 69, 83, 88, 91], providers who maintain privacy and confidentiality [52, 83, 88, 91] and positive provider qualities [52, 69, 79, 83]; Equity and Non-discrimination – low or no cost services [69, 83, 90, 91]; Cultural safety – culturally safe environments and care [52, 55, 61, 69, 72, 83, 87], and the Indigenous workforce and their role in the provision of culturally safe care [52, 61, 69, 85, 87]; and barriers: Appropriate Package of Services – services not available when required [55, 68, 70, 85, 87]; Cultural Safety – many providers did not have adequate training about Indigenous culture [65, 70]; and Community Support – fear of child welfare services and police involvement if adolescents and families accessed services [68, 69, 85]. Notable differences in enablers and barriers were identified under eight of the nine standards, particularly relating to Providers’ Competencies, Facility Characteristics, Cultural Safety, Adolescent Health Literacy, Community Support, and Adolescent Participation.
Recommendations
Based on evidence from this review and the Global standards [6] we have developed a set of recommendations for policy and service delivery reform. These recommendations focus on addressing the enablers and barriers associated with each of the nine standards and aim to improve the accessibility of primary health care services for Indigenous adolescents (Table 7).
Discussion
This is the first review to synthesize findings exploring enablers and barriers to primary health care for Indigenous adolescents. The review synthesized literature from 41 studies that identified enablers and barriers to primary health care for Indigenous adolescents. Across the included studies, more barriers were identified than enablers, and against the WHO Global standards most enablers and barriers related to supply factors. The review identified Indigenous adolescents experience similar enablers and barriers to primary health care as non-Indigenous adolescents [8,9,10], however, there are additional enablers and barriers related to cultural safety that Indigenous adolescents also experience.
Previous studies have identified numerous barriers to primary health care among adolescents, such as availability of services, cost, location of services, inconvenient opening hours, adolescents lack awareness of services, lack of confidentiality, lack of provider knowledge and skills, and absence of legal frameworks [8,9,10, 18, 92,93,94,95,96,97,98,99]. While these have also been identified by our review, it’s possible that when these barriers are experienced by Indigenous adolescents they are exacerbated by complex historical factors, intergenerational trauma, racism, and socioeconomic determinants of health [20, 36,37,38], and more complex health needs [21]. Furthermore, enablers and barriers identified under cultural safety were significant to Indigenous adolescents accessing primary health care services. Cultural safety included enablers and barriers related to culturally appropriate services, culturally safe environment and care, traditional and cultural practices, cultural protocols, Indigenous health care providers, cultural training for health care providers, and colonization, intergenerational trauma, and racism. The absence of these factors or the presence of them in the case of colonization, intergenerational trauma and racism, have been previously identified as barriers to heath care access and having a negative effect on the health and wellbeing of Indigenous people [100,101,102]. Importantly, the provision of culturally safe spaces and care, particularly the presence of Indigenous health care workers and their role in facilitating culturally safe care, were significant enablers to Indigenous people accessing primary health care services [103,104,105].
It is well documented Indigenous adolescents experience an excess burden of preventable and treatable diseases. Indigenous adolescents continue to experience communicable diseases typical of childhood [21, 106]. The prevalence of injury, violence, and mental health is highest among Indigenous adolescents compared to non-Indigenous adolescents and are prevailing causes of premature mortality [20, 107]. The early on-set of chronic diseases such as obesity, diabetes and cardiovascular disease are more prevalent in Indigenous adolescents than non-Indigenous adolescents [20, 21, 106, 108]. This excess burden requires a different approach, knowledge, and skills to address, as well as additional care and resources to mitigate any long-term impact.
There are numerous examples available which demonstrates what works in relation to addressing Indigenous health and wellbeing, and adolescent health. Indigenous health services have a proven track record of improving the health of Indigenous people [109]. Their scope of service delivery is far more than comprehensive, it is holistic and robust and tailored to meet the health and wellbeing needs of community and guided by Indigenous leadership and community-control which is critical for ensuring Indigenous representation in decision-making [29, 110]. Furthermore, Indigenous health services are culturally safe, often situated within Indigenous communities, and seen as beacons of Indigenous excellence that facilitate self-determination [29, 110, 111]. Health care providers are instrumental in the delivery of care [104], as this review has identified they can act as an enablers or barriers to care. The WHO has recognized the unique role health care providers play in providing care to adolescents and has developed the Core competencies in adolescent health and development for primary health care providers [112]. Similarly, Indigenous health care providers are an important component to the delivery of culturally safe care, due to their shared Indigenous identity, lived experience and often belonging to the communities in which they practice [103, 113,114,115]. More broadly, evidence has identified models of care that center and involve adolescents in decision making work. For example, headspace a national youth mental healthcare service in Australia was designed in recognition to the unmet need and the high incidence and prevalence of mental health issues among young people [116]. Similar models of care such as school-based health clinics in the USA have demonstrated that the provision of care within a youth setting such as a school can increase access to care, health and educational outcomes [117,118,119].
The review highlighted several gaps in the evidence, including limited evidence on Indigenous adolescents’ access to primary health care services, as well as the perspectives of Indigenous male adolescents; younger adolescents; urban settings; and limited breadth and depth of evidence across primary health care services and health conditions. Furthermore, studies among Indigenous adolescents accessing primary health care services in urban settings is limited and further research is required, including understanding the enablers and barriers to care on both the supply and demand side, and how primary health care services can be improved to better meet the health and wellbeing needs of Indigenous adolescents. Similarly, there was a paucity of studies that focused exclusively on Indigenous male adolescents within primary health care services. The lack of evidence and health research among Indigenous males including Indigenous male adolescents in primary health care services requires action, especially considering Indigenous adolescent males are at greater risk of experiencing mortality and morbidity, their experience of social and cultural determinants of health, and are less likely to engage with primary health care services than female Indigenous adolescents [20, 21, 120].
Our review had several limitations. The search strategy and selection criteria excluded studies on prevention and screening, which are core components of comprehensive primary health care; however, the reviewed focused on the responsive (acute) care component of primary health care services. We defined adolescents as those aged 10–24 years, as such we may have missed studies which did not specify age and referred to younger adolescents as children and older adolescents as adults. Similarly, while the review included 41 studies, there is always a possibility that the review did not identify all potential articles. Most studies were single health service studies, rarely did studies show the depth of adolescent patterns of care across multiple health care services or regions, and most focused predominately on specific diseases or similar health conditions. Furthermore, there were very few quantitative studies that showed the relationship between the barriers & enablers of primary health care, access and health outcomes. Overall, most studies scored highly against the Joanna Briggs Institute tools, however, not against the Aboriginal and Torres Strait Islander Quality Appraisal Tool, where overall quality and reporting for each criterion was relatively poor. Studies were assessed using the information reported, however, this does not mean the processes and activities for which the Aboriginal and Torres Strait Islander Quality Appraisal Tool assess against did not occur. Even though reporting guidelines for Indigenous health research now exist [121], journals do not require studies to demonstrate how they meet the guidelines. The lack of reporting using Indigenous guidelines is of concern given the number of national and international research guidelines [122,123,124,125] that call for Indigenous research to reflect Indigenous ways of knowing, being and doing; including a greater push towards Indigenous research being conducting with and by Indigenous researchers.
If we want primary health care services that are more accessible to adolescents, then these services need to consider Indigenous adolescents, their health needs [21] and the barriers and enablers they experience when accessing services. Based on this review and the WHO Global standards for quality health-care services for adolescents, we have developed nine recommendations for policy and service delivery reform that focus on the enablers that improve the accessibility of primary health care services for Indigenous adolescents (Table 7). However, the full implementation of the recommendations will require a commitment by government at all levels to fully prioritize Indigenous adolescent health programs and policy, with an accompanying commitment to resourcing, staffing and programs focused on Indigenous adolescents.
Conclusion
Indigenous adolescents experience the same barriers and enablers to accessing primary health care services as adolescent more broadly, however, these may be exacerbated by complex historical and socioeconomic factors. Indigenous adolescents also experience additional enablers and barriers to accessing primary health care services. These enablers and barriers were related to aspects of cultural safety – culturally appropriate services, environment, and care, and were found to be significant to Indigenous adolescents’ experience of accessing primary health care services. This review provides important evidence to inform how services, organizations and governments create adolescent accessible primary health care services that specifically meet the needs of Indigenous adolescents.
Availability of data and materials
Data extracted from included studies for this review are available from the corresponding author on reasonable request.
Abbreviations
- USA:
-
United States of America
- WHO:
-
World Health Organization
References
Sawyer SM, Azzopardi PS, Wickremarathne D, Patton GC. The age of adolescence. Lancet Child Adolesc Health. 2018;2(3):223–8.
Sawyer SM, Afifi RA, Bearinger LH, Blakemore SJ, Dick B, Ezeh AC, Patton GC. Adolescence: a foundation for future health. Lancet. 2012;379(9826):1630–40.
World Health O. Adolescent friendly health services : an agenda for change. Geneva: World Health Organization; 2003.
United Nations. Global strategy for women’s, children’s and adolescents’ health (2016–2030). New York: United States of America; 2015.
World Health Organisation. Global Accelerated Action for the Health of Adolescents (AA-HA!): guidance to support country implementation. Geneva: Switzerland; 2017.
World Health Organization. UNAIDS: Global standards for quality health-care services for adolescents: a guide to implement a standards-driven approach to improve the quality of health care services for adolescents. Geneva: World Health Organization; 2015.
Kang M, Robards F, Sanci L, Steinbeck K, Jan S, Hawke C, Luscombe G, Kong M, Usherwood T. Access 3: young people and the health system in the digital age - final research report. Sydney: Department of General Practice Westmead, The University of Sydney, the Australian Centre for Public and Population Health Research, The University of Technology Sydney; 2018.
Patton GC, Sawyer SM, Santelli JS, Ross DA, Afifi R, Allen NB, Arora M, Azzopardi P, Baldwin W, Bonell C, et al. Our future: a Lancet commission on adolescent health and wellbeing. Lancet. 2016;387(10036):2423–78.
Tylee A, Haller DM, Graham T, Churchill R, Sanci LA. Youth-friendly primary-care services: how are we doing and what more needs to be done? Lancet. 2007;369(9572):1565–73.
Booth ML, Bernard D, Quine S, Kang MS, Usherwood T, Alperstein G, Bennett DL. Access to health care among Australian adolescents young people’s perspectives and their sociodemographic distribution. J Adolesc Health. 2004;34(1):97–103.
Health Service Usage and Health Related Actions, Australia, 2014–15. https://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/4364.0.55.0022014-15?OpenDocument. Accessed 29 Apr 2022.
Australian Institute of Health Welfare. The health of Australia’s males. Canberra: AIHW; 2019.
Slade T, Johnston A, Oakley Browne MA, Andrews G, Whiteford H. 2007 national survey of mental health and wellbeing: methods and key findings. Aust N Z J Psychiatry. 2009;43(7):594–605.
Statistics Canada. Primary health care providers, 2019. Ottawa: Statistics Canada; 2020.
Mathias K. Youth-specific primary health care – access, utilisation and health outcomes: a critical appraisal of the literature. New Zealand: Christchurch; 2002.
Lau JS, Adams SH, Boscardin WJ, Irwin CE Jr. Young adults’ health care utilization and expenditures prior to the affordable care act. J Adolesc Health. 2014;54(6):663–71.
Congress US. Office of technology assessment: adolescent health: summary and policy options. Washington DC: US Government Printing Office; 1991.
Hargreaves DS, Greaves F, Levay C, Mitchell I, Koch U, Esch T, Denny S, Frich JC, Struijs J, Sheikh A. Comparison of health care experience and access between young and older adults in 11 high-income countries. J Adolesc Health. 2015;57(4):413–20.
Azzopardi PS, Hearps SJC, Francis KL, Kennedy EC, Mokdad AH, Kassebaum NJ, Lim S, Irvine CMS, Vos T, Brown AD, et al. Progress in adolescent health and wellbeing: tracking 12 headline indicators for 195 countries and territories, 1990–2016. Lancet. 2019;393(10176):1101–18.
Australian Institute of Health and Welfare. Aboriginal and Torres Strait Islander adolescent and youth health and wellbeing 2018. Canberra: AIHW; 2018.
Azzopardi PS, Sawyer SM, Carlin JB, Degenhardt L, Brown N, Brown AD, Patton GC. Health and wellbeing of Indigenous adolescents in Australia: a systematic synthesis of population data. Lancet. 2018;391(10122):766–82.
Price M, Dalgleish J. Help-seeking among Indigenous Australian adolescents: exploring attitudes, behaviours and barriers, vol. 32. Australian Clearinghouse for Youth Studies; 2013.
Teevale T, Denny S, Percival T, Fleming T. Pacific secondary school students’ access to primary health care in New Zealand. NZ Med J. 2013;126(1375):58–68.
Lau M, Lin H, Flores G. Racial/ethnic disparities in health and health care among U.S. adolescents. Health Serv Res. 2012;47(5):2031–59.
Brown ADH, Crengle S, Tewhaiti-Smith J, Westhead S, Bingham B, Brown N, Cassidy-Matthews C, Clark T, Finlay SM, Hansen KL, et al. The health and wellbeing of Indigenous adolescents: a global collective for an equitable and sustainable future. Lancet. 2022;399(10322):341–3.
Services Australia. Medicare item reports. Services Australia: Canberra; 2022.
Indigenous health checks and follow-ups. https://www.aihw.gov.au/reports/indigenous-australians/indigenous-health-checks-follow-ups. Accessed 6 Apr 2023.
Our History & Future. https://amsredfern.org.au/our-history-future/. Accessed 23 May 2022.
Panaretto KS, Wenitong M, Button S, Ring IT. Aboriginal community controlled health services: leading the way in primary care. Med J Aust. 2014;200(11):649–52.
Gallagher J, Mendez JK, Kehoe T. The first nations health authority: a transformation in healthcare for BC first nations. Healthc Manage Forum. 2015;28(6):255–61.
About NITHA | Northern Inter-Tribal Health Authority. https://www.nitha.com/our-history/. Accessed 23 May 2022.
Crampton P, Dowell A, Woodward A. Third sector primary care for vulnerable populations. Soc Sci Med. 2001;53(11):1491–502.
Kruse G, Lopez-Carmen VA, Jensen A, Hardie L, Sequist TD. The Indian health service and American Indian/Alaska native health outcomes. Annu Rev Public Health. 2022;43:559–76.
National Indian Health Board. I/T/U are essential community providers. Washington DC: NIHB; 2011.
Britt H, Miller G, Henderson J, Bayram C, Harrison C, Valenti L, et al. General practice activity in Australia 2015–16. In: General practice series no 40. Sydney: Sydney University Press; 2016.
Lancet T. The past is not the past for Canada’s Indigenous peoples. Lancet. 2021;397(10293):2439.
Burns J, Angelino AC, Lewis K, Gotcsik ME, Bell RA, Bell J, Empey A. Land rights and health outcomes in American Indian/Alaska native children. Pediatrics. 2021;148(5):e2020041350.
Reid P, Cormack D, Paine SJ. Colonial histories, racism and health—the experience of Māori and Indigenous peoples. Public Health. 2019;172:119–24.
Estimates of Aboriginal and Torres Strait Islander Australians. https://www.abs.gov.au/statistics/people/aboriginal-and-torres-strait-islander-peoples/estimates-aboriginal-and-torres-strait-islander-australians/latest-release#:~:text=The%20final%20estimated%20resident%20Aboriginal,of%20the%20total%20Australian%20population. Accessed 15 Mar 2022.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Anderson I, Robson B, Connolly M, Al-Yaman F, Bjertness E, King A, Tynan M, Madden R, Bang A, Coimbra CEA, et al. Indigenous and tribal peoples’ health (The Lancet-Lowitja Institute Global Collaboration): a population study. Lancet. 2016;388(10040):131–57.
Silburn K, Reich H, Anderson I. A global snapshot of indigenous and tribal peoples’ health, The Lancet-Lowitja Institute Collaboration. Melbourne: The Lowitja Institute; 2016.
United Nations. State of the world’s Indigenous peoples: Indigenous peoples’ access to health services, vol. 2. New York: UN; 2015.
The Joanna Briggs Institute. Joanna Briggs Institute Reviewers’ manual. 2014th ed. Adelaide: The Joanna Briggs Institute; 2014.
Harfield S, Pearson O, Morey K, Kite E, Canuto K, Glover K, Gomersall JS, Carter D, Davy C, Aromataris E, et al. Assessing the quality of health research from an Indigenous perspective: the Aboriginal and Torres Strait Islander quality appraisal tool. BMC Med Res Methodol. 2020;20(1):79.
The EndNote Team. EndNote. In: EndNote 20 edn. Philadelphia: Clarivate; 2013.
Veritas Health Innovation. Covidence systematic review software. Melbourne; Available at www.covidence.org.
National Aboriginal and Torres Strait Islander Health Standing Committee of the Australian Health Ministers’ Advisory Council. Cultural respect framework 2016–2026 for Aboriginal and Torres Strait Islander health. Canberra: AHMAC; 2016.
Rodriguez Santana I, Mason A, Gutacker N, Kasteridis P, Santos R, Rice N. Need, demand, supply in health care: working definitions, and their implications for defining access. Health Econ Policy Law. 2021:1–13.
Eades SJ, Taylor B, Bailey S, Williamson AB, Craig JC, Redman S. The health of urban Aboriginal people: insufficient data to close the gap. Med J Aust. 2010;193(9):521–4.
Weeks JR. Defining urban areas. In: Rashed T, Jürgens C, editors. Remote sensing of urban and suburban areas. Dordrecht: Springer, Netherlands; 2010. p. 33–45.
Warwick S, Atkinson D, Kitaura T, LeLievre M, Marley JV. Young Aboriginal people’s perspective on access to health care in remote Australia: hearing their voices. Prog Community Health Partnersh. 2019;13(2):171–81.
Westerman T. Engaging Australian Aboriginal youth in mental health services. Aust Psychol. 2010;45(3):212–22.
Auger MD. We need to not be footnotes anymore’: understanding Métis people’s experiences with mental health and wellness in British Columbia, Canada. Public Health. 2019;176:92–7.
Bell S, Aggleton P, Ward J, Murray W, Silver B, Lockyer A, Ferguson T, Fairley CK, Whiley D, Ryder N, et al. Young Aboriginal people’s engagement with STI testing in the Northern Territory, Australia. BMC Public Health. 2020;20(1):459.
Canuto K, Wittert G, Harfield S, Brown A. “I feel more comfortable speaking to a male”: Aboriginal and Torres Strait Islander men’s discourse on utilizing primary health care services. Int J Equity Health. 2018;17(1):185.
Etter M, Goose A, Nossal M, Chishom-Nelson J, Heck C, Joober R, Boksa P, Lal S, Shah JL, Andersson N, et al. Improving youth mental wellness services in an Indigenous context in Ulukhaktok, Northwest Territories: ACCESS Open Minds Project. Early Interv Psychiatry. 2019;13 Suppl 1(Suppl Suppl 1):35–41.
Hutt-MacLeod D, Rudderham H, Sylliboy A, Sylliboy-Denny M, Liebenberg L, Denny JF, Gould MR, Gould N, Nossal M, Iyer SN, et al. Eskasoni First Nation’s transformation of youth mental healthcare: partnership between a Mi’kmaq community and the ACCESS open minds research project in implementing innovative practice and service evaluation. Early Interv Psychiatry. 2019;13 Suppl 1(Suppl Suppl 1):42–7.
Kalucy D, Nixon J, Parvizian M, Fernando P, Sherriff S, McMellon J, D’Este C, Eades SJ, Williamson A. Exploring pathways to mental healthcare for urban Aboriginal young people: a qualitative interview study. BMJ Open. 2019;9(7):e025670.
McClintock K, Tauroa R, Mellsop G, Frampton C. Pilot of Te Tomo mai, a child and adolescent mental health service evaluation tool for an indigenous rangatahi (youth) population. Int J Adolesc Med Health. 2016;21(1):96–103.
Mooney-Somers J, Olsen A, Erick W, Scott R, Akee A, Maher L. Sexual health through the eyes of Indigenous youth: community-based participatory research with young Indigenous people in Townsville. Sydney: National Centre in HIV Epidemiology and Clinical Research, University of New South Wales; 2009.
Reibel T, Morrison L, Griffin D, Chapman L, Woods H. Young Aboriginal women’s voices on pregnancy care: factors encouraging antenatal engagement. Women Birth. 2015;28(1):47–53.
Schultz R, Quinn S, Wilson B, Abbott T, Cairney S. Structural modelling of wellbeing for Indigenous Australians: importance of mental health. BMC Health Serv Res. 2019;19(1):488.
Stewart M, King M, Blood R, Letourneau N, Masuda JR, Anderson S, Bearskin LB. Health inequities experienced by Aboriginal children with respiratory conditions and their parents. Can J Nurs Res. 2013;45(3):6–27.
Angelino A, Evans-Campbell T, Duran B. Assessing health provider perspectives regarding barriers American Indian/Alaska Native transgender and two-spirit youth face accessing healthcare. J Racial Ethn Health Disparities. 2020;7(4):630–42.
Corosky GJ, Blystad A. Staying healthy “under the sheets”: Inuit youth experiences of access to sexual and reproductive health and rights in Arviat, Nunavut, Canada. Int J Circumpolar Health. 2016;75:31812.
Dickerson DL, Johnson CL. Design of a behavioral health program for urban American Indian/Alaska Native youths: a community informed approach. J Psychoactive Drugs. 2011;43(4):337–42.
Fraser SL, Moulin L, Gaulin D, Thompson J. On the move: exploring Inuit and non-Inuit health service providers’ perspectives about youth, family and community participation in care in Nunavik. BMC Health Serv Res. 2021;21(1):94.
Hendrickx D, Amgarth-Duff I, Bowen AC, Carapetis JR, Chibawe R, Samson M, Walker R. Barriers and enablers of health service utilisation for childhood skin infections in remote Aboriginal communities of Western Australia. Int J Environ Res Public Health. 2020;17(3):808.
Lawton B, Makowharemahihi C, Cram F, Robson B, Ngata T. Pounamu: E Hine: access to contraception for indigenous Mãori teenage mothers. J Prim Health Care. 2016;8(1):52–9.
Makowharemahihi C, Lawton BA, Cram F, Ngata T, Brown S, Robson B. Initiation of maternity care for young Maori women under 20 years of age. N Z Med J. 2014;127(1393):52–61.
Martel R, Reihana-Tait H, Lawrence A, Shepherd M, Wihongi T, Goodyear-Smith F. Reaching out to reduce health inequities for Māori youth. Int Nurs Rev. 2020;67(2):275–81.
McClintock K, Mellsop GW. Te Tomo Mai Appropriate Child and Adolescent Mental Health Service (CAMHS) for an Indigenous Population: Rangatahi (Youth) Perspectives. J Indig Wellbeing. 2013;11(1):125.
Santhanam R, Hunter E, Wilkinson Y, Whiteford H, McEwan A. Care, community capacity: rethinking mental health services in remote indigenous settings. Aust J Prim Health. 2006;12(2):51–6.
Ameratunga S, Jackson N, Peiris-John R, Sheridan J, Moselen E, Clark T. New Zealand adolescents’ concerns about their alcohol use and access to services: associations with ethnicity and other factors. J Ethn Subst Abuse. 2019;18(4):634–53.
Dowsett M, Islam MM, Ganora C, Day C, Lee KSK, Dawson A, Joseph T, White A, Freeburn B, Conigrave KM. Asking young Aboriginal people who use illicit drugs about their healthcare preferences using audio-computer-assisted self-interviewing. Drug Alcohol Rev. 2019;38(5):482–93.
Freedenthal S, Stiffman AR. “They Might Think I Was Crazy”: young American Indians’ reasons for not seeking help when suicidal. J Adolesc Res. 2007;22(1):58–77.
Greenstein C, Lowell A, Thomas D. Communication and context are important to Indigenous children with physical disability and their carers at a community-based physiotherapy service: a qualitative study. J Physiother. 2016;62(1):42–7.
Johnston K, Harvey C, Matich P, Page P, Jukka C, Hollins J, Larkins S. Increasing access to sexual health care for rural and regional young people: similarities and differences in the views of young people and service providers. Aust J Rural Health. 2015;23(5):257–64.
Kurtin M, Barton C, Winefield A, Edwards J. What are the mental health needs of adolescents in Rural South Australia? The perceptions of human service providers. Australas Med J. 2009;1(6):1–33.
Robards F, Kang M, Steinbeck K, Hawke C, Jan S, Sanci L, Liew YY, Kong M, Usherwood T. Health care equity and access for marginalised young people: a longitudinal qualitative study exploring health system navigation in Australia. Int J Equity Health. 2019;18(1):41.
Sabbioni D, Feehan S, Nicholls C, Soong W, Rigoli D, Follett D, Carastathis G, Gomes A, Griffiths J, Curtis K, et al. Providing culturally informed mental health services to Aboriginal youth: The YouthLink model in Western Australia. Early Interv Psychiatry. 2018;12(5):987–94.
Saftner MA, Martyn KK, Momper SL. Urban dwelling American Indian adolescent girls’ beliefs regarding health care access and trust. J Indig Soc Dev. 2014;3(1):1–15.
Salvador J, Goodkind J, Ewing SF. Perceptions and use of community- and school-based behavioral health services among urban American Indian/Alaska Native youth and families. Am Indian Alsk Native Ment Health Res. 2016;23(3):221–47.
Williamson AB, Raphael B, Redman S, Daniels J, Eades SJ, Mayers N. Emerging themes in Aboriginal child and adolescent mental health: findings from a qualitative study in Sydney, New South Wales. Med J Aust. 2010;192(10):603–5.
Yi KJ, Landais E, Kolahdooz F, Sharma S. Factors influencing the health and wellness of urban aboriginal youths in Canada: insights of in-service professionals, care providers, and stakeholders. Am J Public Health. 2015;105(5):881–90.
Mooney-Somers J, Erick W, Scott R, Akee A, Kaldor J, Maher L. Enhancing Aboriginal and Torres Strait Islander young people’s resilience to blood-borne and sexually transmitted infections: findings from a community-based participatory research project. Health Promot J Austr. 2009;20(3):195–201.
Warwick S, LeLievre M, Seear K, Atkinson D, Marley JV. Above and beyond: fashioning an accessible health service for Aboriginal youth in remote Western Australia. Prog Community Health Partnersh. 2021;15(4):463–73.
Hummel B, Bierstone D, Newhook D, Jetty R. Exploring the perspectives of caregivers of urban Inuit children on child health knowledge mobilisation. Int J Circumpolar Health. 2022;81(1):2120174.
Garrett SM, Rose SB, McKinlay EM. Young people talk about primary care and telehealth: a survey of 15- to 25-year olds in the Wellington region of New Zealand. Health Soc Care Community. 2022;30(6):e6345–55.
Rose SB, Garrett SM, McKinlay EM, Morgan SJ. ‘Be nice to us, we’re still learning’: an online survey of young people in Hawkes Bay, New Zealand, about unmet need for sexual health care and improving access to services. Sex Health. 2021;18(5):394–404.
Ford CA, Millstein SG, Halpern-Felsher BL, Irwin CE Jr. Influence of physician confidentiality assurances on adolescents’ willingness to disclose information and seek future health care. A randomized controlled trial. JAMA. 1997;278(12):1029–34.
Kang M, Bernard D, Booth M, Quine S, Alperstein G, Usherwood T, Bennett D. Access to primary health care for Australian young people: service provider perspectives. Br J Gen Pract. 2003;53(497):947–52.
Waddington C, Sambo C. Financing health care for adolescents: a necessary part of universal health coverage. Bull World Health Organ. 2015;93(1):57–9.
Mazur A, Brindis CD, Decker MJ. Assessing youth-friendly sexual and reproductive health services: a systematic review. BMC Health Serv Res. 2018;18(1):216.
Newton-Levinson A, Leichliter JS, Chandra-Mouli V. Sexually transmitted infection services for adolescents and youth in low- and middle-income countries: perceived and experienced barriers to accessing care. J Adolesc Health. 2016;59(1):7–16.
Gleeson CR, Robinson MB, Neal RD. A review of teenagers’ perceived needs and access to primary health care: implications for health services. Prim Health Care Res Dev. 2002;3(3):184–93.
Garney W, Wilson K, Ajayi KV, Panjwani S, Love SM, Flores S, Garcia K, Esquivel C. Social-ecological barriers to access to healthcare for adolescents: a scoping review. Int J Environ Res Public Health. 2021;18(8):4138.
Velasco AA, Cruz ISS, Billings J, Jimenez M, Rowe S. What are the barriers, facilitators and interventions targeting help-seeking behaviours for common mental health problems in adolescents? A systematic review. BMC Psychiatry. 2020;20(1):293.
Priest N, Paradies Y, Trenerry B, Truong M, Karlsen S, Kelly Y. A systematic review of studies examining the relationship between reported racism and health and wellbeing for children and young people. Soc Sci Med. 2013;95:115–27.
Paradies Y, Ben J, Denson N, Elias A, Priest N, Pieterse A, Gupta A, Kelaher M, Gee G. Racism as a determinant of health: a systematic review and meta-analysis. PLoS One. 2015;10(9):e0138511.
Kairuz CA, Casanelia LM, Bennett-Brook K, Coombes J, Yadav UN. Impact of racism and discrimination on physical and mental health among Aboriginal and Torres Strait islander peoples living in Australia: a systematic scoping review. BMC Public Health. 2021;21(1):1302.
Health Workforce Australia. Aboriginal & Torres Strait Islander Health worker project: interim report. Adelaide: Health Workforce Australia; 2011.
Harfield SG, Davy C, McArthur A, Munn Z, Brown A, Brown N. Characteristics of Indigenous primary health care service delivery models: a systematic scoping review. Global Health. 2018;14(1):12.
Mercer C, Byrth J, Jordan Z, Stern C. The experiences of Aboriginal health workers and Non Aboriginal health professionals working collaboratively in the delivery of health care to Aboriginal Australians: a systematic review of qualitative evidence. JBI Libr Syst Rev. 2012;10(56 Suppl):1–12.
Craig E, McDonald G, Adams J, Reddington A, Oben G, Simpson J, Wicken A. Te Ohonga Ake The Health of Māori Children and Young People with Chronic Conditions and Disabilities in New Zealand. Dunedin: New Zealand Child and Youth Epidemiology Service, University of Otago; 2012.
Anderson T. Indigenous youth in Canada. Ottawa: Statistics Canada; 2021.
Deen JF, Adams AK, Fretts A, Jolly S, Navas-Acien A, Devereux RB, Buchwald D, Howard BV. Cardiovascular disease in American Indian and Alaska Native Youth: unique risk factors and areas of scholarly need. J Am Heart Assoc. 2017;6(10):e007576.
Campbell MA, Hunt J, Scrimgeour DJ, Davey M, Jones V. Contribution of Aboriginal community-controlled health services to improving Aboriginal health: an evidence review. Aust Health Rev. 2018;42(2):218–26.
Hayman NE, White NE, Spurling GK. Improving Indigenous patients’ access to mainstream health services: the Inala experience. Med J Aust. 2009;190(10):604–6.
Tilton E, Thomas D. Core functions of primary health care: a framework for the Northern Territory. Darwin: AMSANT; 2011.
World Health Organisation. Core competencies in adolescent health and development for primary care providers. Geneva: WHO; 2015.
Boulton AF, Gifford HH, Potaka-Osborne M. Realising whānau ora through community action: the role of Māori community health workers. Educ Health (Abingdon). 2009;22(2):188.
Minore B, Jacklin K, Boone M, Cromarty H. Realistic expectations: the changing role of paraprofessional health workers in First Nation communities in Canada. Educ Health (Abingdon). 2009;22(2):298.
National Aboriginal and Torres Strait Islander Health Workers Association. The importance of Aboriginal and/or Torres Strait Islander Health Workers and Health Practitioners in Australia’s health system. Canberra: NATSIHWA; 2019.
Rickwood D, Paraskakis M, Quin D, Hobbs N, Ryall V, Trethowan J, McGorry P. Australia’s innovation in youth mental health care: the headspace centre model. Early Interv Psychiatry. 2019;13(1):159–66.
Knopf JA, Finnie RK, Peng Y, Hahn RA, Truman BI, Vernon-Smiley M, Johnson VC, Johnson RL, Fielding JE, Muntaner C, et al. School-based health centers to advance health equity: a community guide systematic review. Am J Prev Med. 2016;51(1):114–26.
Keeton V, Soleimanpour S, Brindis CD. School-based health centers in an era of health care reform: building on history. Curr Probl Pediatr Adolesc Health Care. 2012;42(6):132–56. discussion 157-138.
Ran T, Chattopadhyay SK, Hahn RA. Economic evaluation of school-based health centers: a community guide systematic review. Am J Prev Med. 2016;51(1):129–38.
Fredericks B, Daniels C, Judd J, Bainbridge R, Clapham K, Longbottom M, Adams M, Bessarab D, Collard L, Andersen C, et al. Gendered indigenous health and wellbeing within the australian health system: a review of the literature. Rockhampton: CQUniversity; 2017.
Huria T, Palmer SC, Pitama S, Beckert L, Lacey C, Ewen S, Smith LT. Consolidated criteria for strengthening reporting of health research involving indigenous peoples: the CONSIDER statement. BMC Med Res Methodol. 2019;19(1):173.
National Health and Medical Research Council Australia. Ethical conduct in research with aboriginal and Torres Strait Islander peoples and communities: guidelines for researchers and stakeholders. Canberra: NHMRC; 2018.
Canadian Institutes of Health Research, Natural Sciences and Engineering Research Council of Canada, Social Sciences and Humanities Research Council of Canada. Tri-council policy statement: ethical conduct for research involving humans. Ottowa: CIHR; 2014.
Health Research Council of New Zealand. Guidelines for researchers on health research involving Máori. Auckland: HRCNZ; 2010.
The Sámediggi. Proposal for ethical guidelines for sami health research and research on Sami Human biological material. Norway: The Sámediggi; 2017.
Acknowledgements
The authors wish to acknowledge Tirritpa Richie for his assistance with study selection.
Funding
SH was supported by Australian Government Research Training Program Scholarship, an Aboriginal and Torres Strait Islander Research Training Program, and UQ Poche Centre for Indigenous Health Research Top-Up Scholarships. Funders were not involved in the design, the collection, analysis, and interpretation of review data, writing of the manuscript or in the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
PA and OP were involved in the conceptualization. PA, TP, and SH designed the review. TP and SH conducted the study search, and title and abstract and full-text review with PA. Data extraction and quality appraisal completed by SH and ES. Data analysis conducted by SH and reviewed by PA. SH wrote the original and final draft and were reviewed by all other authors. PA and JW provided supervision.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Harfield, S., Purcell, T., Schioldann, E. et al. Enablers and barriers to primary health care access for Indigenous adolescents: a systematic review and meta-aggregation of studies across Australia, Canada, New Zealand, and USA. BMC Health Serv Res 24, 553 (2024). https://doi.org/10.1186/s12913-024-10796-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-024-10796-5