Abstract
Background
Globally, emergency departments (EDs) are overcrowded and unable to meet an ever-increasing demand for care. The aim of this study is to comprehensively review and synthesise literature on potential solutions and challenges throughout the entire health system, focusing on ED patient flow.
Methods
An umbrella review was conducted to comprehensively summarise and synthesise the available evidence from multiple research syntheses. A comprehensive search strategy was employed in four databases alongside government or organisational websites in March 2023. Gray literature and reports were also searched. Quality was assessed using the JBI critical appraisal checklist for systematic reviews and research syntheses. We summarised and classified findings using qualitative synthesis, the Population-Capacity-Process (PCP) model, and the input/throughput/output (I/T/O) model of ED patient flow and synthesised intervention outcomes based on the Quadruple Aim framework.
Results
The search strategy yielded 1263 articles, of which 39 were included in the umbrella review. Patient flow interventions were categorised into human factors, management-organisation interventions, and infrastructure and mapped to the relevant component of the patient journey from pre-ED to post-ED interventions. Most interventions had mixed or quadruple nonsignificant outcomes. The majority of interventions for enhancing ED patient flow were primarily related to the 'within-ED' phase of the patient journey. Fewer interventions were identified for the 'post-ED' phase (acute inpatient transfer, subacute inpatient transfer, hospital at home, discharge home, or residential care) and the 'pre-ED' phase. The intervention outcomes were aligned with the aim (QAIM), which aims to improve patient care experience, enhance population health, optimise efficiency, and enhance staff satisfaction.
Conclusions
This study found that there was a wide range of interventions used to address patient flow, but the effectiveness of these interventions varied, and most interventions were focused on the ED. Interventions for the remainder of the patient journey were largely neglected. The metrics reported were mainly focused on efficiency measures rather than addressing all quadrants of the quadruple aim. Further research is needed to investigate and enhance the effectiveness of interventions outside the ED in improving ED patient flow. It is essential to develop interventions that relate to all three phases of patient flow: pre-ED, within-ED, and post-ED.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
Changes in demographics, the prevalence of multimorbidity, the ongoing challenges posed by the COVID-19 pandemic, and persistent shortages in healthcare staffing have significantly increased the demand for healthcare services. [1,2,3]. Most hospitals face a mismatch between supply and demand, resulting in delays, staffing gaps, and inefficient hospital ward utilisation. This imbalance leads to issues such as overcrowded emergency units, nursing staff shortages, and staff dissatisfaction. [3]. Globally, emergency departments are overcrowded and unable to meet an ever-increasing demand for healthcare [1]. The increasing demand for emergency care services is a significant challenge for healthcare systems worldwide [4,5,6,7,8,9].
Patient flow through the healthcare system refers to the movement of patients through care settings and encompasses the entire patient journey from arrival until the patient departs from the hospital [7, 10, 11]. Effective patient flow is essential for timely, high-quality care, and mismanagement can cause disruptions within the hospital system [3, 9, 12]. Poor patient flow can lead to ED overcrowding when patients experience delays or blockages in the care processes [9].
Access block, defined as the delay of admitted patients from leaving the ED for more than eight hours due to a shortage of hospital beds, is a significant cause of poorer patient outcomes [13]. It specifically impacts admitted patients and is different from ED overcrowding, which affects both admitted and nonadmitted ED patients [13,14,15]. ED overcrowding and access block have numerous negative consequences, such as decreased quality of care, poor patient outcomes, increased risk of death, medical errors, treatment side effects, patient dissatisfaction, reduced hospital capacity, ambulance diversions, increased workload, staff frustration, longer waiting times, increased cost of care, and patients leaving without being seen by a physician. The negative consequences of access block and overcrowding highlight the urgent necessity for interventions to tackle these issues and improve patient outcomes while maximising healthcare system capacity [1, 9, 16,17,18,19].
Studies have shown that addressing patient flow issues can have several benefits, including reduced length of stay (LOS) and faster discharge process [1, 2, 20, 21]. Improving patient flow is essential for enhancing medical quality, safety, and patient satisfaction while also reducing input and facilitating throughput and output from hospitals and EDs [3, 8, 22].
It has become evident that ED overcrowding is not solely an ED problem but rather reflects dysfunction throughout the entire patient journey. However, reform efforts and political pressure traditionally focus on ED processes [23, 24]. Healthcare aims have evolved over time, with measures of ED performance traditionally centred around process measures such as ED length of stay, to now reach for the more balanced Quadruple Aim of Healthcare: increased efficiency, improved population health, better consumer experience and excellent provider experience [25]. Balanced measures of healthcare performance, including experience and care outcomes, are important. Focusing solely on LOS without measuring experience or outcomes can lead to clinician burnout and low-value or dangerous care [26].
Despite extensive literature addressing patient flow interventions and challenges, stakeholders may find it challenging to navigate and determine evidence-based interventions and challenges strongly supported by the evidence. [7, 27,28,29], Syntheses of research on how to improve patient flow rarely provide an overall examination of interventions across the care pathway [13, 30,31,32,33,34,35,36]. Decision-making in a holistic manner to improve patient flow can be a difficult, complex, and potentially risky task for stakeholders [27, 28].
Existing reviews on this topic typically focus solely on interventions based in the ED to improve patient flow within the ED [1, 7, 27, 28, 37,38,39,40]. However, there is currently a noticeable gap in recent reviews that comprehensively address challenges and interventions across the health system for managing ED patient flow. Recognising the importance of a broader health-wide perspective, extending from pre-ED to discharge and beyond, is crucial. This emerging concept requires a holistic approach that views the healthcare system as a continuum of care [41]. Therefore, this review aims to synthesise the literature comprehensively, focusing on evidence-based interventions throughout the entire hospital or health system to enhance ED patient flow. Additionally, it explores outcomes related to ED patient flow improvement and identify challenges within the entire hospital or health system interconnected with the patient flow in the ED, recognising the healthcare system as a continuum of care.
In our study, we utilised the population–capacity–process (PCP) model of health service design. According to this model, effective services establish a connection between a defined population, the necessary capacity, and a streamlined process [42, 43]. The term 'Population' refers to individuals with shared needs, 'capacity' pertains to the human and physical resources needed to meet those requirements, and 'process' encompasses the steps that bridge the gap between the two. This model emerged from a study highlighting that the failure of patient-flow initiatives often results from neglecting one or more of these three domains. Subsequently, the PCP model has found application in other literature [8, 42,43,44,45].
In addition, we applied the Input/Throughput/Output (I/T/O) model of ED patient flow, developed by Asplin et al., which divides ED crowding into three interconnected components: input, throughput, and output [10]. This conceptual framework aids administrators, researchers, and policymakers in comprehending the causes of ED crowding and developing potential solutions.
Methods
An umbrella review was conducted to comprehensively summarise and synthesise the available evidence from multiple research syntheses on various challenges and interventions within the entire health system, specifically focusing on patient flow in the ED. This umbrella review followed the Joanna Briggs Institute methodology for umbrella reviews [46, 47] and the PRIOR checklist for healthcare overviews to ensure thoroughness and transparency [48]. This umbrella review followed an a priori published protocol and was registered with the International Prospective Register of Systematic Reviews (PROSPERO) on 24 April 2023 (CRD42023414182) [49].
Inclusion and exclusion criteria
As this study reviewed both quantitative and qualitative systematic reviews, we considered both interventions and phenomena of interest when defining eligibility criteria for this umbrella review. We used PICO (population, intervention, comparator, outcome) or PICo (population, phenomena of interest and context) elements to clearly define the eligibility criteria.
Types of participants
Participants included consumers of health care services, physicians, nurses, health care professionals, health care workers in clinics, hospitals, ambulance service, primary care, and residential aged care facilities (RACF), carers, health managers and policymakers. Participants who were not responsible for patient flow-related activities, such as healthcare workers without a direct role in patient care or management, were excluded.
Interventions/Phenomena of interest
The interventions reviewed in this study included interventions or potential solutions throughout the entire health system aimed at improving patient flow in the ED. The phenomena of interest were the challenges and root causes, encompassing both internal and external organisational factors, that hinder efficient patient flow in the ED. Interventions or phenomena of interest that were not related directly or indirectly to patient flow in the ED were excluded.
Comparator(s)/Context
This umbrella review aimed to synthesise evidence on challenges and potential solutions throughout the entire health system with a focus on ED patient flow without making direct comparisons between interventions. However, the review considered studies that compared patient flow interventions or strategies against each other or against usual care or no intervention. Studies comparing interventions or exposures unrelated to patient flow in the ED were excluded.
Interventions were not limited to the ED, and any intervention that measured an impact on ED flow was considered.
Outcomes
To provide a balanced overview of the evidence base related to the topic, this review attempted to report both beneficial and adverse outcomes of interventions across the entire health system aimed at improving patient flow in the ED and map them to the Quadruple Aim. Studies that reported outcomes unrelated to interventions or challenges of patient flow in the ED were excluded.
Types of studies
The systematic reviews included in our study were needed to use internationally accepted methodologies such as meta-analyses, qualitative systematic reviews, integrative reviews, scoping reviews, meta-syntheses, and meta-aggregative reviews. In addition, umbrella reviews that reviewed quantitative, qualitative, or both quantitative and qualitative systematic reviews were included. We excluded primary studies, as well as narrative reviews, systematic reviews based on theoretical studies or opinions, editorials, commentaries, predictive studies, and feasibility studies.
Search strategy
Two authors (MS and CS) developed the search strategy, which was then peer-reviewed by an experienced librarian (LE) in accordance with the Peer Review of Electronic Search Strategies (PRESS) 2015 Guideline Statement for systematic reviews [50].
To develop a comprehensive search strategy, several steps were taken [51]. The first step involved conducting a preliminary search in PubMed to identify additional keywords and synonyms relevant to the initial keywords. The initial keywords used were “patient flow”, "emergency department," "emergency care," and "systematic review." Subsequently, a search strategy was developed that included appropriate search terms and Boolean operators (such as "AND" and "OR"), along with MeSH and Emtree terms. After piloting the search strategy in PubMed and making necessary adjustments, the final version of the search strategy was developed. Table 1 presents our final search strategy. The search strategy for each database was subsequently developed according to the specific syntax and indexing of that database (Additional file 1).
In March 2023, we conducted an extensive search in electronic databases, which included CINAHL, PubMed, Web of Science, and Embase. Additionally, we simply conducted a basic search of major systematic review repositories, such as the JBI Database of Systematic Reviews and Implementation Reports, the Cochrane Database of Systematic Reviews, and the PROSPERO register.
Reports on government or organisational websites are eligible for inclusion in an umbrella review and can help decision-makers base their decisions on evidence [52]. As such, we searched for grey reports on relevant government or organisational websites, Google, and Google Scholar. Finally, the reference lists of all included systematic reviews were searched for additional relevant publications.
Study screening and selection
The retrieved references were imported into EndNote v.20.4.1 (Clarivate Analytics, PA, USA), and duplicates were removed. The remaining citations were subsequently uploaded to Covidence Systematic Review Software (Veritas Health Innovation, Melbourne, Australia) for screening, methodological quality appraisal and data extraction.
To enhance consensus among reviewers, a pilot selection process was conducted on a randomly selected 3% of articles. Subsequent minor revisions were made to the eligibility criteria. Two independent reviewers screened the titles and abstracts of all potentially eligible studies, followed by a review of the full text of those that met the initial screening criteria. In cases where disagreements arose, a third reviewer was brought in to resolve disputes that could not be resolved through consensus. We used the PRISMA flowchart to describe the process of study selection in the Results section. The comprehensive details regarding systematic reviews that were excluded after this assessment are presented in Additional file 2.
Assessment of methodological quality
In the present study, two independent reviewers assessed the reviews included within the analysis. The JBI critical appraisal checklist for systematic reviews and research synthesis was utilised to assess the trustworthiness, quality, and research findings of the articles, which was prepared in Covidence. This checklist comprises eleven distinct aspects, and the appraisal of these aspects was conducted using four criteria: "yes", "no", "unclear", and "not applicable" (Additional file 3). Using the JBI critical appraisal toolkit, each of the included studies was categorised into one of three quality levels: low, moderate, or high [52]. The classification criteria categorised a paper as "low quality" if its results were below 50%, "moderate quality" if they ranged between 50 and 69%, and "high quality" if the results were above 69%. Any disagreements between the reviewers were resolved through discussion and consensus within the research team. Our decision was to include all reviews in our study without any prior exclusion based on quality assessment and to provide the results of all quality appraisals. This differs from the JBI methodology, which suggests setting a quality score cut-off [47]. However, as our umbrella review aimed to examine the quality of systematic reviews, we believe it is crucial to present data on all the reviews we have included and enable readers to assess the value of information provided by each systematic review.
Data collection
In this study, two reviewers independently extracted data from the included reviews using the modified JBI data extraction form for systematic reviews and research syntheses [47]. The data extraction form was customised for the purpose of this research and developed in Covidence (Additional file 4). To enhance the clarity, relevance, accuracy, and consistency of data extraction, three reviewers independently piloted the form on a randomly selected 10% of the included studies, which consisted of two narrative syntheses and two meta-analyses. Any potential revisions to the data extraction tool were assessed by all reviewers and discussed in detail before extracting data independently.
Data extracted included citation details, objectives, type of study, description of participants, setting and context, search details, appraisal data, key findings related to integration interventions and challenges, and any comments or notes from the umbrella review authors regarding any included study.
Data synthesis
Four authors (CS, MS, ST, YM) analysed the data extracted to develop a narrative overview of the challenges and interventions in patient flow. Given the heterogeneity in populations, outcomes, and analyses, we summarised the findings of the included reviews using a narrative synthesis approach. Qualitative research synthesis was used, following the guidelines for conducting an umbrella review [46].
A meta-aggregative approach was employed to synthesise qualitative evidence of challenges regarding challenges in patient flow across the healthcare system. The goal was to generate evidence that can guide practitioners and policymakers [47, 53]. The findings on challenges were categorised based on the PCP model.
We also utilised an inductive approach to synthesise evidence on patient flow improvement solutions and gain a comprehensive understanding of applied interventions. Additionally, to provide a clear and structured framework, we adopted the input/throughput/output (I/T/O) model of ED patient flow. [54]. We also used the 'pre-ED', 'within-ED', and 'post-ED' model, as employed by the Sax Institute to describe solutions for reducing access blocks across the health system [13]. 'Input' refers to interventions or challenges before patients arrive in the ED, 'throughput' refers to internal ED issues and interventions while the patient is in the ED, and 'output' refers to interventions and challenges of the patient's journey in leaving and after leaving the ED. Post-ED was classified into three potential pathways: home departure, ward departure, or transfer to a residential care facility. The outcomes of the interventions were indicated using specific symbols: ( +) for positive outcomes, (-) for negative outcomes, ( ±) for mixed outcomes or conflicting evidence, ( =) for nonsignificant outcomes or no difference, and (NR) for not reported or limited evidence.
Additionally, the extracted outcomes of interventions for each component were synthesised and classified based on the Quadruple Aim framework. These outcomes were aligned with the Quadruple Aim framework, which includes QAIM1: improving the patient experience of care, QAIM2: improving population health, QAIM3: reducing costs, and QAIM4: enhancing the work-life balance and satisfaction of healthcare providers.
Results
Study selection
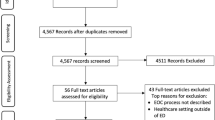
Figure 1 provides an overview of the flow diagram representing the study selection process. Through the literature search, a total of 1263 titles were retrieved. The search in gray literature, PROSPERO databases, and the reference lists of eligible articles yielded 6 additional records. After removing duplicates (n = 460) and screening titles and abstracts, 64 records were considered eligible for full-text review. A total of 39 articles were selected against the selection criteria and included in the literature review.
Description of the included reviews
The general characteristics of the included reviews are presented in Table 2. These reviews cover various topics related to ED interventions, access blocks, patient flow, and healthcare outcomes. The total number of included reviews was 39, and they were conducted between 2017 and 2023, with a significant proportion (n = 12) published in 2020. The studies included in these reviews span a wide range of years, from 1980 to 2022, indicating a comprehensive examination of the literature over an extended period. The included studies comprised 8 scoping reviews, 24 systematic reviews, 3 systematic reviews with meta-analyses, 3 umbrella reviews, and 1 systematic mapping review, representing a diverse range of study designs. This varied selection of methodologies provided a comprehensive and well-rounded examination of the research topic. Among the included reviews, 7 conducted quantitative analysis or meta-analysis, 4 performed narrative synthesis and meta-analysis, and 28 reviews presented the results of the primary studies narratively or descriptively. Full details of the characteristics of the included reviews are available in Additional file 5. The various appraisal instruments and ratings used in the included reviews. The appraisal instruments mentioned include the ROBIS tool, SQUIRE 2.0 checklist, EPHPP, GRADE, Newcastle‒Ottawa Scale Modified tool, AMSTAR 2, modified 7-level rating system, JBI checklists, Cochrane EPOC, NHLBI, NICE quality appraisal tool, EBL critical appraisal tool, RevMan ROBIS tool, QATSDD, SIGN, and CAS Pand MINORS.
Search characteristics: databases, countries, aims of the studies
The search dates varied across the reviews, indicating a range of timeframes for the included studies. The number of studies included in each review varied significantly, ranging from four [61] to 268 [69] studies. The majority of studies included in the analysis originated from Canada, Australia, the USA, and the UK. Among these countries, Canada had the highest number of studies, with a total of 10 [31, 36, 39, 64, 65, 68,69,70,71, 78]. The most frequently searched databases were PubMed and Medline, indicating their popularity among researchers. Additionally, grey literature sources were searched in 18 of the reviews.
The aims of the included studies can be classified into three main categories. The first category focuses on solutions for various challenges encountered in the emergency department, such as access block, consultation time, ED length of stay, ED overcrowding, nonurgent attendance in the ED, and ED boarding [13, 15, 27, 29, 31, 34, 39, 56, 58, 61, 62, 69, 72, 74, 77]. The second category involves interventions aimed at improving ED performance and utilisation. This category includes studies on throughput time, patient outcomes, provider satisfaction, older adults' experience in the ED, and ED patient care processes [7, 30, 32, 33, 35, 36, 55, 57, 59, 63,64,65,66,67,68,69,70,71,72,73,74, 76, 78, 79]. The third category encompasses studies related to challenges specifically related to patient flow [15, 29, 39].
The results of the critical appraisal
A total of 39 reviews were assessed using the JBI Critical Appraisal Checklist for Systematic Reviews and Research Synthesis [47, 52]. The findings of the JBI Critical Appraisal Checklist for Systematic Reviews and Research Synthesis for each of the 31 reviews are summarised in Table 3. The number of criteria met varied across the reviews, with the minimum being 5 out of 11 [60] and the maximum being 11 out of 11 [57, 64, 66, 68]. Among the assessed reviews, one scoping review was determined to be of low quality [60], nine were categorised as moderate quality [13, 27, 34,35,36, 58, 73, 74, 77], and the remaining 27 were deemed high quality [7, 15, 29,30,31,32,33, 39, 43, 55,56,57, 59, 61,62,63,64,65,66,67,68,69, 71, 72, 75, 76, 78,79,80]. Notably, all reviews met criteria 8 and 11, which pertain to the appropriate methods used to combine studies and the recommendations for policy and/or practice supported by the reported data.
Patient flow interventions
Interventions are categorised and presented in Table 4. Interventions were grouped into three main categories: (a) Human Factors; (b) Management-Organisation-Policy; and (c) Infrastructure.
Human factor interventions
In detailing human factor interventions for ED patient flow improvement, all relevant interventions are listed in Table 5. The majority of intervention examples mentioned in the studies were related to the “staffing adjustments” category. “Physician-led ED triage models” were extensively discussed in nine studies [7, 15, 27, 30, 35, 55, 64, 75, 78], highlighting their significance in optimising patient flow. “Nurse-initiated requests for paramedical service or triage nurse ordering (TNO) requests” were examined in six studies [7, 15, 27, 33, 64, 69], indicating their potential impact on improving patient flow. The “modification of staffing patterns” [7, 13, 31, 72, 75] and the “exploration of motivation and payment models” [4, 36, 64, 65, 69, 75] were addressed in five studies. In addition, training for healthcare workers received attention in four studies [29, 35, 72, 78]. It was observed that most interventions focused on the "within-ED" phase solutions, involving actions taken while patients were in the ED. While fewer interventions were identified for the “Post-ED” phase, which involves the patient's journey after discharge to home or a residential care facility, a few studies also mentioned interventions focusing on the “Pre-ED” phase, occurring before patients arrive at the ED. Education for staff in long-term care facilities, the integration of advanced nursing care within these facilities, the implementation of financial disincentives for nonemergency presentations referred by primary health care clinics, patient education through printed materials or personal contact, public education campaigns on the proper use of emergency departments, and family education are examples of interventions outside the hospital context. Overall, it was observed that most interventions within this category had mixed outcomes or conflicting evidence.
Management-organisation-policy interventions
Several key interventions within the main category of management-organisation-policy interventions for patient flow improvement were prominently mentioned in the included studies (Table 6). The majority of intervention examples mentioned in the studies were related to the "structural reorganisation/operational changes" subcategory of the "process improvement" category. The most frequent intervention example was "care transitions and discharge management" for timely patient handover and discharge processes, which was extensively discussed in seven studies [29, 30, 32, 34, 67, 75, 76]. "Fast-track services" for streaming or split-flow processes of nonemergency cases [7, 15, 34, 64, 69, 73] and "team composition interventions" [30, 32, 60, 65, 69, 74] were examined in six studies. It was observed that most interventions focused on the "within-ED" phase and the "ward departure" phase of the "posted" phase, involving actions taken while patients were in the ED or ward. Fewer interventions were identified for the "post-ED" phase, which involves the patient's journey after discharge to home. Overall, most interventions within this category had mixed or nonsignificant outcomes. Some interventions related to residential care facilities and home departure, including "on-site primary and acute treatment for specific conditions in long-term care facilities" [65, 71], "Implementation of the Interventions to Reduce Acute Care Transfers (INTERACT) of long-term care patients" [71], "implementation of extended care paramedics in long-term care centres" [71], "providing long-term care facilities" [34], and "home-based healthcare optimisation" [34, 74], had positive outcomes.
Infrastructure interventions
The most frequently mentioned interventions within the infrastructure category included the “implementation of simulation and predictive models or the utilisation of predictive tools” [29, 30, 35, 72, 73, 75], as well as “electronic board tracking or electronic patient tracking systems” [7, 15, 34, 35, 64, 75] (Table 7). These interventions received more attention in six studies, primarily addressing the "within-ED" phases, as well as the "ward departure" phase during “post-ED” processes. However, fewer interventions were identified for the "output" phase, which involves the patient's journey after discharge to either home or residential care facilities. Overall, the outcomes of most interventions within the technology/innovation category were mixed or nonsignificant. Some specific examples, such as “the use of instant messaging for real-time communication between ED physicians and consultants” [78], “the implementation of strategies to reduce acute care transfers for long-term care patients” [71], and “the utilisation of capacity alert escalation calls” [75], yielded positive results.
Outcomes of patient flow improvement solutions
The outcomes of patient flow improvement solutions are classified in Table 8.
Several outcomes or aims of patient flow improvement solutions were frequently mentioned in the included studies, with "reduction of ED-LOS/hospital LOS" discussed in 24 studies [7, 15, 27, 31, 34, 35, 39, 55, 60,61,62,63,64, 66, 68, 69, 71,72,73,74, 76,77,78,79], "improving the patient experience" in 17 studies [15, 32, 35, 39, 55, 57, 59, 63, 67,68,69, 72, 73, 76, 77, 79, 81], “lowering costs” in 13 studies [60, 61, 64, 65, 68,69,70,71,72,73,74, 78, 79], “reducing patients left without being seen or those who did not wait (LWBS/DNW)” in 11 studies [15, 27, 34, 35, 60, 64, 66, 68, 69, 72, 73], and “decreasing readmission or revisit rates” [34, 39, 61, 65,66,67, 71, 74, 79, 80] and “reducing ED visits” [15, 36, 68,69,70,71, 74, 76, 80] in 10 and 9 studies, respectively, reflecting the multifaceted nature of these solutions and highlighting key areas of focus in optimising healthcare delivery.
The aims to improve the patient experience of care, reduce LWBS/DNW/LAMA, decrease in consultation to decision time, and reduce overcrowding are addressed under QAIM1, while QAIM2 focuses on improving population health, enhancing referrals to community services and parental hospital visit satisfaction, decreasing potentially avoidable diagnostic tests and treatments, and reducing the number of nonurgent, semiurgent, and frequent users. QAIM3 is mapped to reducing costs, ED-LOS and hospital LOS, optimising resource allocation with better clinical outcomes, and decreasing admission rates, ED visits, waiting time, door-to-physician time, and ED boarding hours. In addition, QAIM4 encompasses improving the clinical experiences and satisfaction of staff and reducing ED staff stress levels.
Patient flow challenges across the healthcare system
The findings on root causes of ED patient flow challenges presented in Table 9 were categorised based on the population-capacity-process (PCP) model.
Among the factors related to the population, root causes frequently identified were “the acuity mix of patients in the ED” [15, 36, 55, 61, 68, 72, 73], “rising demand for ED visits and hospitalisation due to an ageing population” [15, 33, 71, 77, 78], and “patient characteristics” [38, 58, 59, 67]. The most common capacity challenges included “limited human resources” [7, 15, 28, 38, 57,58,59, 67, 68, 71], “limited bed availability” [13, 27, 34, 72, 73, 75, 76, 79], and “inappropriate ED utilisation or visits” [39, 69, 70, 75, 76]. Process-related challenges encompassed issues with communication, test results, primary care access, transitions of care, and low-acuity patients. Notable challenges reported were “exit block and delayed transitions of care” [15, 29, 34, 39, 72, 75], “consultation delays” [15, 31, 39, 72, 75], “delays in demanding and receiving diagnostic tests and imaging studies” [15, 39, 55, 75], “limited primary care access” [15, 38, 71], and “difficulties in diverting low acuity patients from ambulances to alternative care sites” [55, 72, 73].
The challenges presented a wide range of outcomes, encompassing adverse patient outcomes, extended length of stay, ED crowding, financial risks for healthcare systems, and patient dissatisfaction. The study identified ED crowding (N = 41 root causes), patient dissatisfaction (N = 25 root causes), prolonged ED-LOS (N = 21 root causes), and extended waiting time (N = 1 root cause) as the most frequent outcomes resulting from the identified root causes of patient flow challenges.
Discussion
Patient flow interventions or solutions
Categorising interventions into human factors, management-organisation-policy, and infrastructure provides a comprehensive understanding of evidence-based strategies to improve patient flow. Additionally, Rasouli et al. broadly categorised approaches or solutions to reduce or prevent ED overcrowding into organisation- or management-level interventions and operation-level interventions [75]. Furthermore, Freitas et al. categorised interventions aimed at improving patient flow and reducing overcrowding into several groups, including diagnostic services, assessment/short stay units, nurse-directed interventions, physician-directed interventions, administrative/organisational interventions, and miscellaneous interventions [7]. Moreover, an overview by Conneely highlighted various interventions, such as gerontologically informed nursing assessment, comprehensive geriatric assessment, ED community transitional strategies, ED-based interventions, and single/multistrategy interventions initiated in the ED [28].
Human factor interventions
In the category of human factor interventions, various interventions have been identified. Similarly, various training and professional development interventions were identified in the studies [30, 65]. These interventions encompassed training sessions on a new rapid assessment and disposition process, brief orientation to the new process, education to increase awareness of national targets, an education day with a focus on specific areas of improvement, training for nurses in coordinating communications, pain management, and triage [24, 82,83,84,85]. Furthermore, Anantharaman et al. found that public education on the proper use of the emergency department can be effective in the short term but may not have a lasting impact. To ensure sustained desired outcomes beyond the education period, additional strategies or interventions may be needed [15, 86]. Physicians working alone or alongside nurses in triage allowed for prompt diagnostic procedures and treatments, leading to reduced length of stay and waiting time per patient [27]. However, some argue that team triage lacks clear advantages and sufficient evidence regarding its benefits [28, 87, 88]. These interventions primarily focus on "within-ED" solutions to enhance the flow and efficiency of the ED.. However, there is a deficiency in interventions addressing the "post-ED" phase to enhance ED patient flow. This phase involves the patient's journey after discharge, including home departure or residential care departure. Additionally, there is a gap in interventions for the "pre-ED" phase, which includes supporting patients at home and redirecting them to more appropriate types of care, such as primary care and other urgent ambulatory care services. Similarly, the findings of Gettel et al. revealed that ED-to-community care transitions often lack effective care coordination and communication, especially for older adults with cognitive impairment [89].
Management-organisation-policy interventions
Notably, structural reorganisation and operational changes have also been frequently mentioned within the management-organisation-policy category, with a focus on care transitions, discharge management, and fast-track services. Aligned with the findings of Ortíz-Barrios et al., various process improvement methodologies have been employed to address crucial issues in emergency departments, including overcrowding, prolonged waiting time, extended length of stay, excessive patient flow time, and high rates of LWBS [73]. It is crucial for future efforts to involve ED administrators, researchers, and stakeholders in designing comprehensive strategies utilising operations research (OR) methods to enhance ED performance and address these specific challenges. Additionally, these interventions predominantly concentrate on solutions in the "within-ED" and "ward departure" phases, and interventions addressing the "post-ED" phase, especially the home departure phase (from either ED or the inpatient wards), to improve ED patient flow are relatively sparse. Alharbi et al. similarly discovered that efforts to reduce inpatient long stays were impacted by various constraints, which included the challenge of meeting the postdischarge needs of specific patient populations. For instance, ventilated patients faced difficulties due to the absence of specialised long-term care units capable of accommodating them and the unavailability of home services resulting from a shortage of trained and dedicated healthcare workers in their area [90].
Infrastructure interventions
The included studies particularly highlighted telehealth and information technology (IT) interventions for improving ED patient flow. The implementation of simulation and predictive models or the utilisation of predictive tools, as well as electronic board tracking or electronic patient tracking systems, were among the most frequently mentioned interventions. The main focus of these interventions to enhance ED patient flow was on solutions “within the ED” and ward departure. However, fewer interventions were identified for the post-ED phase, which involves the patient's journey after leaving the ED. Overall, the outcomes of most interventions within the Technology/Innovation category were mixed or nonsignificant. Based on available evidence, various technologies, such as nurse call lines, on-demand telehealth visits, tele-triage, and paramedic-driven mobile response programs, were identified as valuable tools for screening patients before their arrival at the emergency department, aiming to mitigate ED overcrowding [91, 92]. Additionally, telemedicine tools such as remote patient monitoring and virtual visits have been employed in home hospital settings, while virtual observation units facilitate early discharge from hospitals or emergency departments, enabling patients to transition to home care [79, 93, 94].
The outcomes of patient flow improvement solutions
The overall results of the study indicate a mixed picture in terms of the outcomes of interventions aimed at improving patient flow. While some interventions showed positive outcomes, such as specific interventions targeting residential care facilities and home departure, as well as certain technology-based interventions, the majority of interventions yielded mixed, conflicting, or nonsignificant outcomes. The study's results align with prior overview studies, which suggests that evidence concerning the effectiveness of interventions in ED settings and patient flow is both limited and ineffective. This is due to the heterogeneity of methods, populations, and measured outcomes, which makes it difficult to compare the results of different studies and draw firm conclusions about the effectiveness of interventions [7, 27, 28]. These findings highlight the importance of establishing and utilising a comprehensive range of meaningful outcome measures to accurately evaluate the effectiveness of interventions on patient flow.
The outcomes of ED patient flow solutions encompass a wide range of categories, in accordance with the quadruple aim framework. Other studies have similarly found that process improvement and rapid assessment implementation had a more significant impact on improving ED productivity and performance compared to renovation and facility expansion [95, 96]. By enhancing ED operational efficiency, the healthcare facility was able to handle increased patient volume while simultaneously improving the quality of care and patient satisfaction [97,98,99]. Remarkably, these improvements were achieved with minimal additional resources, space, or staffing [99].
Patient flow challenges
Within the population factors, the most commonly identified root causes were the acuity mix of patients in the ED, the rising demand for ED visits and hospitalisation due to an ageing population, and patient characteristics. Capacity challenges often revolve around limited human resources, limited bed availability, and inappropriate ED utilisation or visits. Process-related challenges encompassed issues with communication, test results, primary care access, transitions of care, and low-acuity patients. In this regard, Manning's study identified five areas of challenges: teamwork, collaboration and communication; public hospitals as complex systems; timely discharge; policy, process, and decision-making; and resources, capacity, and demand [29]. Additionally, according to Morely's report, the predominant causes identified were associated with the volume and demographics of individuals seeking care at the ED, as well as the timely discharge of patients from the ED [15]. Our study also showed that these challenges resulted in various outcomes, including adverse patient outcomes, extended length of stay, ED overcrowding, financial risks for healthcare systems, and patient dissatisfaction. The most frequent outcomes from the identified root causes were ED overcrowding, patient dissatisfaction, prolonged ED-LOS, and extended waiting time. Other studies have found that ED crowding is a complex issue with multiple contributing factors. These factors can be found in the input, throughput, and output areas of the ED [13, 92, 100]. These findings highlight the complex nature of ED patient flow challenges and underscore the need for targeted interventions and system-level changes to address them effectively.
Conclusion
The findings of this study reveal a mixed impact of interventions on patient flow. The evidence available is often of lower quality, consisting mostly of cross-sectional and noncontrolled pre- and postdesign studies. The variation in geographic areas and healthcare systems among the included studies further complicates the interpretation of results. Insufficient evidence exists to definitively support the effectiveness and safety of diversion strategies and other interventions. Many of the initiatives examined in the literature were pilot projects or quality improvement projects, lacking rigorous evaluation against comparator groups. Inconsistencies in assessment and interventions for patient flow improvement are evident, highlighting the need for standardised measures and evidence-based solutions.
Despite efforts and accumulated knowledge, the problem of ED overcrowding remains a global challenge, indicating the limited success in implementing evidence-based solutions for improving patient flow. The focus on ED interventions in the included reviews limits their usefulness for understanding interventions across the care pathway. It is crucial to utilise a comprehensive range of meaningful outcome measures to accurately assess the effectiveness of system-wide interventions and inform system changes and decision-making. The focus on speed, rather than quality or experience of care, is concerning.
Future research should focus on evaluating the effectiveness of specific interventions using consistent conceptual models and standardised measures. The potential displacement of care resulting from interventions to reduce inappropriate admissions should be explored, along with the impact of healthcare professionals delivering the interventions. Further investigation is needed on interventions combining ED care with home follow-up and different models of discharge management. Community screening to identify high-risk patients and diverting frail older individuals from ED presentations may be more effective.
The findings from this literature review suggest the following recommendations:
1. Developing patient flow interventions from the pre-ED phase to the post-ED phase to enhance patient flow in the ED: Given the identified gap that the majority of interventions primarily target the 'within-ED' phase, there is a crucial need to expand interventions for the 'post-ED' and 'pre-ED' phases. This includes strategies for smooth care transitions, effective discharge management, improved access to primary care, diversion of frail older individuals from ED presentations, and efficient transitions for patients after leaving the hospital. By comprehensively addressing these areas across the healthcare system, healthcare systems can mitigate readmission rates, enhance patient satisfaction, and optimise overall patient flow. 2. Embrace community-based care interventions to address the identified challenge of insufficient availability of beds in community-based care settings, which leads to increased length of stay (LOS) for older adults, hospital overcapacity, and ED crowding. Our review highlights the potential positive outcomes associated with community health-related interventions, such as home-based healthcare optimisation, providing free access to primary care for the uninsured, and establishing long-term care facilities. 3. Strengthen Technology and Innovation Interventions: Additional research is needed to investigate and enhance technology or innovation interventions that focus on all three phases of patient flow. While interventions within the telehealth and information technology subcategories have shown promise in improving ED patient flow specifically “within the ED” and during the “departure to the ward” phase, there is a need to expand their effectiveness to the “Post-ED” phase. This research should aim to optimise the implementation of predictive models, electronic tracking systems, and other technological solutions to enhance ED patient flow.
4. Establish Standardised Measures: We need to measure outcomes other than time. To accurately evaluate the effectiveness of interventions on patient flow, it is crucial to establish and utilise a comprehensive range of meaningful outcome measures. These measures should encompass proportion-related outcomes, cost-related outcomes, process-related outcomes, and patient- or provider-related outcomes. By adopting standardised measures, healthcare systems can effectively achieve the goals of the quadruple aim framework.
5. Address Root Causes of Patient Flow Challenges and Conduct Rigorous Research and Evaluation: To address the root causes identified from previous studies, it is essential to design interventions that specifically target these causes and evaluate their effectiveness using standardised measures. Healthcare systems should focus on implementing interventions that address factors such as population dynamics, capacity challenges, and process-related issues. Rigorous evaluation should be conducted to assess how these interventions effectively address the identified root causes and their impact on patient flow. This includes employing controlled studies with comparator groups and exploring potential displacement of care resulting from interventions. By linking interventions to root causes, utilising standardised measures, and conducting comprehensive evaluation, healthcare systems can build a robust evidence base and support evidence-based decision-making for optimising patient flow.
Overall, these recommendations emphasise the importance of implementing comprehensive, evidence-based interventions that address solutions across the entire patient flow process, including the phases before and after the ED visit. By focusing on human factors, management-organisation-policy, and infrastructure interventions.
Limitations
The study had several limitations. First, unsuccessful interventions are unlikely to have been published, so this paper is subject to publication bias. Another limitation of the study was the limited number of primary studies included in the selected reviews that utilised a single intervention strategy. This scarcity made it challenging to draw definitive conclusions regarding the exact effective action component of the intervention strategy. Additionally, there was variability in study populations, intervention components of the solutions, and outcome measures across the primary studies of the included reviews, which limited the ability to make comprehensive and consistent conclusions. Furthermore, an inherent limitation of our approach lies in classifying the extracted outcomes based on the Quadruple Aim framework. For outcomes that were not explicitly mentioned in relation to a specific QAIM, we performed mapping based on our own judgment and interpretation to assign them to the relevant QAIM. It is essential to consider the specific context and how these outcomes contribute to overall improvements in healthcare and patient experiences. The classification may vary depending on the goals and priorities of the healthcare system.
Availability of data and materials
All data generated or analysed during this study are accessible in this published article and its supplemental information files.
Abbreviations
- ACCESS:
-
Acute care emergency surgery service provision
- CCA:
-
Corrected covered area
- CCCs:
-
Capacity command centers
- DNW:
-
Did Not Wait
- ED:
-
Emergency Department
- EDs:
-
Emergency Departments
- EDWIN:
-
Emergency Department Work Index
- GP:
-
General practitioner
- GROOVE:
-
Graphical representation of overlap for overviews
- INTERACT:
-
Implementation of Interventions to Reduce Acute Care Transfers
- JBI:
-
Joanna Briggs Institute
- LAWA:
-
Reduction of patients leaving against medical advice
- LOS:
-
Length of stay
- LWBS:
-
Left Without Being Seen
- NEAT:
-
The National Emergency Access Target
- NP:
-
Nurse practitioner
- OR:
-
Operations Research
- OTS:
-
On-Time Starts
- PCP:
-
Primary Care Provider
- PCP:
-
Population-capacity-process
- PDCA:
-
Plan-Do-Check-Act
- PDSA:
-
Plan, Do, Study, Act
- PHCPs:
-
Primary healthcare professionals
- PICo:
-
Population, Phenomena of interest and Context
- PRESS:
-
Peer Review of Electronic Search Strategies
- PROSPERO:
-
Prospective Register of Systematic Reviews
- QAIM:
-
Quadruple Aim
- QoC:
-
Quality of Care
- TAT:
-
Turnaround Time
- TNO:
-
Triage nurse ordering
- TOT:
-
Decrease in turnover time
References
Åhlin P, Almström P, Wänström C. Solutions for improved hospital-wide patient flows–a qualitative interview study of leading healthcare providers. BMC Health Serv Res. 2023;23(1):1–17.
Vainieri M, Panero C, Coletta L. Waiting times in emergency departments: a resource allocation or an efficiency issue? BMC Health Serv Res. 2020;20(1):1–10.
Winasti W, Elkhuizen S, Berrevoets L, van Merode G, Berden H. Inpatient flow management: a systematic review. Int J Health Care Qual Assur. 2018;31(7):718–34.
Atzema CL, Maclagan LC. The transition of care between emergency department and primary care: a scoping study. Acad Emerg Med. 2017;24(2):201–15.
Dods S, Boyle J, Khanna S, O’Dwyer J, Sier D, Sparks R, et al. Evidence driven strategies for meeting hospital performance targets: The value of patient flow modeling. CSIRO Health Services. 2013;2013(1):2013.
Hu Z, Siddiqui FJ, Fan Q, Lian SW, Liu N, Ong ME. Trends of chronic illness in emergency department admissions among elderly adults in a tertiary hospital over ten years. BMC Health Serv Res. 2021;21(1):1–8.
De Freitas L, Goodacre S, O’Hara R, Thokala P, Hariharan S. Interventions to improve patient flow in emergency departments: an umbrella review. Emerg Med J. 2018;35(10):626–37.
Kreindler S, Aboud Z, Hastings S, Winters S, Johnson K, Mallinson S, et al. How do health systems address patient flow when services are misaligned with population needs? A qualitative study. Int J Health Policy Manag. 2022;11(8):1362–72.
Mohiuddin S, Busby J, Savović J, Richards A, Northstone K, Hollingworth W, et al. Patient flow within UK emergency departments: a systematic review of the use of computer simulation modelling methods. BMJ Open. 2017;7(5):e015007.
Asplin BR. Measuring crowding: time for a paradigm shift. Acad Emerg Med. 2006;13(4):459–61.
Innovation NIf, Improvement. Quality and service improvement tools. NHS Improving Quality UK; 2006.
Leviner S. Patient flow within hospitals: A conceptual model. Nurs Sci Q. 2020;33(1):29–34.
AM MF, Marjanovic S. Access block: A review of potential solutions. Sax Institute 2022.
Affleck A, Parks P, Drummond A, Rowe BH, Ovens HJ. Emergency department overcrowding and access block. Canadian Journal of Emergency Medicine. 2013;15(6):359–70.
Morley C, Unwin M, Peterson GM, Stankovich J, Kinsman L. Emergency department crowding: a systematic review of causes, consequences and solutions. PLoS ONE. 2018;13(8):e0203316.
Davis Z, Zobel CW, Khansa L, Glick RE. Emergency department resilience to disaster-level overcrowding: a component resilience framework for analysis and predictive modeling. J Oper Manag. 2020;66(1–2):54–66.
Di Somma S, Paladino L, Vaughan L, Lalle I, Magrini L, Magnanti M. Overcrowding in emergency department: an international issue. Intern Emerg Med. 2015;10:171–5.
Salway R, Valenzuela R, Shoenberger J, Mallon W, Viccellio A. Emergency department (ED) overcrowding: evidence-based answers to frequently asked questions. Revista Médica Clínica Las Condes. 2017;28(2):213–9.
Siciliani L, Moran V, Borowitz M. Measuring and comparing health care waiting times in OECD countries. Health Policy. 2014;118(3):292–303.
Improta G, Romano M, Di Cicco MV, Ferraro A, Borrelli A, Verdoliva C, et al. Lean thinking to improve emergency department throughput at AORN Cardarelli hospital. BMC Health Serv Res. 2018;18:1–9.
Johnson M, Burgess N, Sethi S. Temporal pacing of outcomes for improving patient flow: design science research in a national health service Hospital. J Oper Manag. 2020;66(1–2):35–53.
Crawford K, Morphet J, Jones T, Innes K, Griffiths D, Williams A. Initiatives to reduce overcrowding and access block in Australian emergency departments: a literature review. Collegian. 2014;21(4):359–66.
Hassanzadeh H, Khanna S, Boyle J, Jensen F, Murdoch A. New bed configurations and discharge timing policies A hospital-wide simulation. Emerg Med Australas. 2022;3:434–41.
Sullivan CM, Staib A, Flores J, Aggarwal L, Scanlon A, Martin JH, et al. Aiming to be NEAT: safely improving and sustaining access to emergency care in a tertiary referral hospital. Aust Health Rev. 2014;38(5):564–74.
Sikka R, Morath JM, Leape L. The quadruple aim: care, health, cost and meaning in work. BMJ Qual Saf. 2015;24(10):608–10.
Bean DM, Taylor P, Dobson RJB. A patient flow simulator for healthcare management education. BMJ Simul Technol Enhanc Learn. 2019;5(1):46–8.
Bittencourt RJ, Stevanato ADM, Bragança CTN, Gottems LBD, O’Dwyer G. Interventions in overcrowding of emergency departments an overview of systematic reviews. Rev Saúde Pública. 2020;54:66.
Conneely M, Leahy S, Dore L, Trépel D, Robinson K, Jordan F, et al. The effectiveness of interventions to reduce adverse outcomes among older adults following Emergency Department discharge: umbrella review. BMC Geriatr. 2022;22(1):1–23.
Manning L, Islam MS. A systematic review to identify the challenges to achieving effective patient flow in public hospitals. Int J Health Plann Manage. 2023;38(3):805–28.
Austin EE, Blakely B, Tufanaru C, Selwood A, Braithwaite J, Clay-Williams R. Strategies to measure and improve emergency department performance: a scoping review. Scand J Trauma Resusc Emerg Med. 2020;28(1):1–14.
Beckerleg W, Wooller K, Hasimjia D. Interventions to reduce emergency department consultation time: A systematic review of the literature. Can J Emerg Med. 2020;22(1):56–64.
Berning MJ, eSilva LOJ, Suarez NE, Walker LE, Erwin P, Carpenter CR, et al. Interventions to improve older adults Emergency Department patient experience A systematic review. Am J Emerg Med. 2020;38(6):1257–69.
Burgess L, Kynoch K, Theobald K, Keogh S. The effectiveness of nurse-initiated interventions in the Emergency Department: A systematic review. Australas Emerg Care. 2021;24(4):248–54.
Clark J, Islam MS. Hospital Access Block: A Scoping Review. J Emerg Nurs. 2022;48(4):430–54.
Di Laura D, D’Angiolella L, Mantovani L, Squassabia G, Clemente F, Santalucia I, et al. Efficiency measures of emergency departments: an Italian systematic literature review. BMJ open quality. 2021;10(3):e001058.
Hong M, Thind A, Zaric GS, Sarma S. The impact of improved access to after-hours primary care on emergency department and primary care utilization: A systematic review. Health Policy. 2020;124(8):812–8.
Boiko O, Edwards M, Zschaler S, Miles S, Rafferty AM. Interprofessional barriers in patient flow management: an interview study of the views of emergency department staff involved in patient admissions. J Interprof Care. 2021;35(3):334–42.
Gualandi R, Masella C, Tartaglini D. Improving hospital patient flow: a systematic review. Bus Process Manag J. 2020;26(6):1541–75.
Pearce S, Marchand T, Shannon T, Ganshorn H, Lang E. Emergency department crowding an overview of reviews describing measures causes and harms. Internal and Emergency Medicine. 2023;1:1–22.
Wilson S, Rixon A, Hartanto S, White P, Judkins S. Systematic literature review of leadership in emergency departments. Emerg Med Australas. 2020;32(6):935–52.
McHugh M, VanDyke K, McClelland M, Moss D. Improving patient flow and reducing emergency department crowding: a guide for hospitals. Prepared by the Health Research & Educational Trust, an affiliate of the American Hospital Association, under contract 290-200-600022, Task Order No. 6). AHRQ Publication No. 2011: 11(12)-0094. Rockville, MD: Agency for Healthcare Research and Quality.
Kreindler SA. Six ways not to improve patient flow: a qualitative study. BMJ Qual Saf. 2017;26(5):388–94.
Kreindler SA, Struthers A, Star N, Bowen S, Hastings S, Winters S, et al. Can facility-based transitional care improve patient flow? Lessons from four Canadian regions. Healthc Manage Forum; 2021;34(3):181–85.
Anwar MR. A realist analysis of streaming interventions in emergency departments. BMJ Leader. 2021;5:167–73.
Roemeling O, Ahaus K, van Zanten F, Land M, Wennekes P. How improving access times had unforeseen consequences: a case study in a Dutch hospital. BMJ Open. 2019;9(9):e031244.
Aromataris E, Fernandez R, Godfrey CM, Holly C, Khalil H, Tungpunkom P. Summarizing systematic reviews: methodological development, conduct and reporting of an umbrella review approach. JBI Evid Implementation. 2015;13(3):132–40.
Aromataris E, Fernandez R, Godfrey C, Holly C, Khalil H, Tungpunkom P. Methodology for JBI umbrella reviews. Joanna Briggs Institute Reviewers' Manual. 2014: edition / Supplement. Australia: The Joanna Briggs Institute. 2014. p. 1–34.
Gates M, Gates A, Pieper D, Fernandes RM, Tricco AC, Moher D, et al. Reporting guideline for overviews of reviews of healthcare interventions development of the PRIOR statement. BMJ. 2022;378:e070849.
Clair Sullivan AS, Emma Bosley, Daniel Bodnar, James Lind, Justin Boyle, Sankalp Khanna, Hamed Hassanzadeh, Tim Saul, Jodie Austin, Jason Pole, Anton Van Der Vegt, Barbora de Courten, Yasaman Meshkat, Sarah Tanner, Mahnaz Samadbeik. Patient Flow in public hospitals: An umbrella review [Protocol]2023; (24 April ). https://www.crd.york.ac.uk/PROSPERO/display_record.php?RecordID=414182.
McGowan J, Sampson M, Salzwedel DM, Cogo E, Foerster V, Lefebvre C. PRESS peer review of electronic search strategies: 2015 guideline statement. J Clin Epidemiol. 2016;75:40–6.
Bonczar M, Ostrowski P, D’Antoni AV, Tubbs RS, Iwanaga J, Ghosh SK, et al. How to write an Umbrella Review? A step-by-step tutorial with tips and tricks. Folia Morphol. 2022;82(1):1–6.
Peters MD, Godfrey C, McInerney P, Munn Z, Tricco AC, Khalil H, Aromataris E, Munn Z. JBI manual for evidence synthesis. JBI Manual Evid Synth. 2020:406–51.
Lockwood C, Munn Z, Porritt K. Qualitative research synthesis: methodological guidance for systematic reviewers utilizing meta-aggregation. JBI Evid Implementation. 2015;13(3):179–87.
Asplin B, Magid D, Rhodes K, Solberg L, Lurie N, Camargo C. A conceptual model of emergency department crowding. Ann Emerg Med. 2003;42:173–80.
Benabbas R, Shah R, Zonnoor B, Mehta N, Sinert R. Impact of triage liaison provider on emergency department throughput: A systematic review and meta-analysis. Am J Emerg Med. 2020;38(8):1662–70.
Blodgett JM, Robertson DJ, Pennington E, Ratcliffe D, Rockwood K. Alternatives to direct emergency department conveyance of ambulance patients: a scoping review of the evidence. Scand J Trauma Resusc Emerg Med. 2021;29(1):1–21.
Boylen S, Cherian S, Gill FJ, Leslie GD, Wilson S. Impact of professional interpreters on outcomes for hospitalized children from migrant and refugee families with limited English proficiency: a systematic review. JBI Evidence Synthesis. 2020;18(7):1360–88.
Brambilla A, Mangili S, Das M, Lal S, Capolongo S. Analysis of functional layout in Emergency Departments (ED) Shedding light on the Free Standing Emergency Department (FSED) model. Applied Sci. 2022;12(10):5099.
Cassarino M, Robinson K, Quinn R, Naddy B, O’Regan A, Ryan D, et al. Impact of early assessment and intervention by teams involving health and social care professionals in the emergency department: A systematic review. PLoS ONE. 2019;14(7):e0220709.
Franklin BJ, Mueller SK, Bates DW, Gandhi TK, Morris CA, Goralnick E. Use of Hospital Capacity Command Centers to Improve Patient Flow and Safety: A Scoping Review. J Patient Saf. 2022;18(6):e912–21.
Gonçalves‐Bradley D, Khangura JK, Flodgren G, Perera R, Rowe BH, Shepperd S. Primary care professionals providing non‐urgent care in hospital emergency departments. Cochrane Database of Systematic Reviews. 2018(2).
Gottlieb M, Farcy DA, Moreno LA, Vilke GM, Guittard JA. Triage nurse-ordered testing in the emergency department setting A review of the literature for the clinician. J Emerg Med. 2021;60(4):570–5.
Gottlieb M, Palter J, Westrick J, Peksa GD. Effect of medical scribes on throughput, revenue, and patient and provider satisfaction: a systematic review and meta-analysis. Ann Emerg Med. 2021;77(2):180–9.
Grant KL, Bayley CJ, Premji Z, Lang E, Innes G. Throughput interventions to reduce emergency department crowding: A systematic review. Can J Emerg Med. 2020;22(6):864–74.
Grant KL, Lee DD, Cheng I, Baker GR. Reducing preventable patient transfers from long-term care facilities to emergency departments: a scoping review. Can J Emerg Med. 2020;22(6):844–56.
Hesselink G, Schoon Y. Effectiveness of interventions to alleviate emergency department crowding by older adults: a systematic review. BMC Emerg Med. 2019;19(1):1–9.
Hughes JM, Freiermuth CE, Shepherd-Banigan M, Ragsdale L, Eucker SA, Goldstein K, et al. Emergency department interventions for older adults: a systematic review. J Am Geriatr Soc. 2019;67(7):1516–25.
Jeyaraman MM, Alder RN, Copstein L, Al-Yousif N, Suss R, Zarychanski R, et al. Impact of employing primary healthcare professionals in emergency department triage on patient flow outcomes: a systematic review and meta-analysis. BMJ Open. 2022;12(4):e052850.
Jeyaraman MM, Copstein L, Al-Yousif N, Alder RN, Kirkland SW, Al-Yousif Y, et al. Interventions and strategies involving primary healthcare professionals to manage emergency department overcrowding: a scoping review. BMJ Open. 2021;11(5):e048613.
Kirkland SW, Soleimani A, Rowe BH, Newton AS. A systematic review examining the impact of redirecting low-acuity patients seeking emergency department care: is the juice worth the squeeze? Emerg Med J. 2019;36(2):97–106.
Leduc S, Cantor Z, Kelly P, Thiruganasambandamoorthy V, Wells G, Vaillancourt C. The safety and effectiveness of on-site paramedic and allied health treatment interventions targeting the reduction of emergency department visits by long-term care patients: systematic review. Prehosp Emerg Care. 2021;25(4):556–65.
Maninchedda M, Proia AS, Bianco L, Aromatario M, Orsi GB, Napoli C. Main Features and Control Strategies to Reduce Overcrowding in Emergency Departments A Systematic Review of the Literature. Risk Manag Healthc Policy. 2023;16:255–66.
Ortíz-Barrios MA, Alfaro-Saíz J-J. Methodological approaches to support process improvement in emergency departments: a systematic review. Int J Environ Res Public Health. 2020;17(8):2664.
Preston L, Chambers D, Campbell F, Cantrell A, Turner J, Goyder E. What evidence is there for the identification and management of frail older people in the emergency department? A systematic mapping review. Southampton (UK): NIHR Journals Library; 2018.
Rasouli HR, Aliakbar Esfahani A, Abbasi FM. Challenges, consequences, and lessons for way–outs to emergencies at hospitals: a systematic review study. BMC Emerg Med. 2019;19(1):1–10.
Sharma S, Rafferty AM, Boiko O. The role and contribution of nurses to patient flow management in acute hospitals: A systematic review of mixed methods studies. Int J Nurs Stud. 2020;110:103709.
Shepherd J, Lourida I, Meertens RM. Radiographer-led discharge for emergency care patients, requiring projection radiography of minor musculoskeletal injuries: a scoping review. BMC Emerg Med. 2022;22(1):1–12.
Voaklander B, Gaudet LA, Kirkland SW, Keto-Lambert D, Villa-Roel C, Rowe BH. Interventions to improve consultations in the emergency department A systematic review. Acad Emerg Med. 2022;29(12):1475–95.
Zepeda-Lugo C, Tlapa D, Baez-Lopez Y, Limon-Romero J, Ontiveros S, Perez-Sanchez A, et al. Assessing the impact of lean healthcare on inpatient care: A systematic review. Int J Environ Res Public Health. 2020;17(15):5609.
Malik M, Moore Z, Patton D, O’Connor T, Nugent L. The impact of geriatric focused nurse assessment and intervention in the emergency department: a systematic review. Int Emerg Nurs. 2018;37:52–60.
Palmer R, Fulop NJ, Utley M. A systematic literature review of operational research methods for modelling patient flow and outcomes within community healthcare and other settings. Health Systems. 2018;7(1):29–50.
Chhabra S, Eagles D, Kwok ESH, Perry JJ. Interventions to reduce emergency department door-to- electrocardiogram times: A systematic review. CJEM. 2019;21(5):607–17.
Holden RJ. Lean thinking in emergency departments: a critical review. Ann Emerg Med. 2011;57(3):265–78.
Sampson F, Goodacre S, O’cathain A. Interventions to improve the management of pain in emergency departments: systematic review and narrative synthesis. Emerg Med J. 2014;31(e1):e9–18.
Williams S, Keogh S, Douglas C. Improving paediatric pain management in the emergency department: an integrative literature review. Int J Nurs Stud. 2019;94:9–20.
Anantharaman V. Impact of health care system interventions on emergency department utilization and overcrowding in Singapore. Int J Emerg Med. 2008;1(1):11–20.
Abdulwahid MA, Booth A, Kuczawski M, Mason SM. The impact of senior doctor assessment at triage on emergency department performance measures: systematic review and meta-analysis of comparative studies. Emerg Med J. 2016;33(7):504–13.
Ming T, Lai A, Lau PM. Can team triage improve patient flow in the emergency department A systematic review and meta-analysis. Adv Emerg Nurs J. 2016;38(3):233–50.
Gettel CJ, Falvey JR, Gifford A, Hoang L, Christensen LA, Hwang U, et al. Emergency department care transitions for patients with cognitive impairment a scoping review. J Am Med Dir Assoc. 2022;23(8):1313.
Alharbi S, Alasmari A, Hanafy E, Ellawindy A. Reduction of hospital bed cost for inpatient overstay through optimisation of patient flow. BMJ Open Quality. 2023;12(2):e002142.
Ashenburg N, Ribeira R, Lindquist B, Matheson LW, Shen S, Yiadom MY. Converting an ED fast track to an ED virtual visit track. NEJM Catal Innov Care Deliv. 2022;3(11):22.
Baugh CW, Freund Y, Steg PG, Body R, Maron DJ, Yiadom MYA. Strategies to mitigate emergency department crowding and its impact on cardiovascular patients. Eur Heart J Acute Cardiovasc Care. 2023;12(9):633–43.
Abiri A, Keadey M, Hughes G, Pitts SR, Moran TP, Ross MA. The impact of virtual care in an emergency department observation unit. Ann Emerg Med. 2023;81(2):222–33.
Sun S, Lu SF, Rui H. Does telemedicine reduce emergency room congestion? Evidence from New York state. Inf Syst Res. 2020;31(3):972–86.
Freibott D. Optimizing emergency department throughput using best practices to improve patient flow. J Nurs Interprof Leadersh Qual Saf. 2017;1(2):7.
Sayah A, Lai-Becker M, Kingsley-Rocker L, Scott-Long T, O’Connor K, Lobon LF. Emergency Department Expansion Versus Patient Flow Improvement: Impact on Patient Experience of Care. J Emerg Med. 2016;50(2):339–48.
Adel H, Wahed MA, Saleh N, editors. A novel approach for improving patient flow in emergency department. 2018 9th Cairo International Biomedical Engineering Conference (CIBEC). IEEE. 2018.
Alowad A, Samaranayake P, Ahsan K, Alidrisi H, Karim A. Enhancing patient flow in emergency department (ED) using lean strategies–an integrated voice of customer and voice of process perspective. Bus Process Manag J. 2021;27(1):75–105.
Sayah A, Rogers L, Devarajan K, Kingsley-Rocker L, Lobon LF. Minimizing ED waiting times and improving patient flow and experience of care. Emerg Med Int. 2014;2014:981472.
Moskop JC, Geiderman JM, Marshall KD, McGreevy J, Derse AR, Bookman K, et al. Another Look at the Persistent Moral Problem of Emergency Department Crowding. Ann Emerg Med. 2019;74(3):357–64.
Acknowledgements
We acknowledge the support of this work from the Emergency Medicine Foundation.
Funding
This study is a part of the research project, which was performed with the support of Australia's Emergency Medicine Foundation.
Author information
Authors and Affiliations
Contributions
MS: Conceptualised and designed the review, developed the search strategy, determined study eligibility, conducted the screening and selection process, resolved disagreements between reviewers, designed the data extraction table, extracted, and analysed the data, wrote the first draft of the manuscript, and extensively revised the manuscript. AS, JB, SK, and JA: Contributed to the design of the review, determined study eligibility, designed the data extraction table, interpreted the data, and provided substantial revisions to the manuscript. EB, DB, JL, and BDC: Provided critical guidance and advice throughout the study, contributed to the design of the data extraction table, and offered valuable commentary on the manuscript. ST and YM: Were responsible for screening and selecting studies, assessing reviews, performing data extraction, and made significant revisions to the manuscript. CS: Conceptualized and designed the review, determined study eligibility, developed the search strategy, designed the data extraction table, interpreted the data, provided revisions to the manuscript, and supervised the entire study.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Samadbeik, M., Staib, A., Boyle, J. et al. Patient flow in emergency departments: a comprehensive umbrella review of solutions and challenges across the health system. BMC Health Serv Res 24, 274 (2024). https://doi.org/10.1186/s12913-024-10725-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-024-10725-6