Abstract
Background
Screening, brief intervention, and referral (SBIR) is an evidence-based, comprehensive health promotion approach commonly implemented to reduce alcohol and substance use. Implementation research on SBIR demonstrate that patients find it acceptable, reduces hospital costs, and it is effective. However, SBIR implementation in hospital settings for multiple risk factors (fruit and vegetable consumption, physical activity, alcohol and tobacco use) is still emergent. More evidence is needed to guide SBIR implementation for multiple risk factors in hospital settings.
Objective
To explore the facilitators and barriers of SBIR implementation in a rural hospital using the Consolidated Framework for Implementation Research (CFIR).
Methods
We conducted a descriptive qualitative investigation consisting of both inductive and deductive analyses. We conducted virtual, semi-structured interviews, guided by the CFIR framework. All interviews were audio-recorded, and transcribed verbatim. NVivo 12 Pro was used to organize and code the raw data.
Results
A total of six key informant semi-structured interviews, ranging from 45 to 60 min, were carried out with members of the implementation support team and clinical implementers. Implementation support members reported that collaborating with health departments facilitated SBIR implementation by helping (a) align health promotion risk factors with existing guidelines; (b) develop training and educational resources for clinicians and patients; and (c) foster leadership buy-in. Conversely, clinical implementers reported several barriers to SBIR implementation including, increased and disrupted workflow due to SBIR-related documentation, a lack of knowledge on patients’ readiness and motivation to change, as well as perceived patient stigma in relation to SBIR risk factors.
Conclusion
The CFIR provided a comprehensive framework to gauge facilitators and barriers relating to SBIR implementation. Our pilot investigation revealed that future SBIR implementation must address organizational, clinical implementer, and patient readiness to implement SBIR at all phases of the implementation process in a hospital.
Similar content being viewed by others
Introdution
Cancer is the leading cause of death in Canada and globally. It is projected that 43% or 2 in 5 Canadians will be diagnosed with cancer in their life time [1]. In Alberta, the leading cause of death for those ages 35–64 years old was cancer, followed closely by circulatory disease [2]. However, an estimated 40% of cancers are preventable, as they are attributed to modifiable risk factors, including tobacco consumption, alcohol use, physical activity, and low fruit and vegetable consumption [3, 4]. The Canadian Population Attributable Risk of Cancer study conducted in 2015 found that Alberta had 2,780 new cancer cases attributed to tobacco smoking, 994 to low physical activity, 280 to alcohol use, and 891 to low fruit and vegetable consumption [5]. Tobacco use [6, 7], alcohol use [8,9,10], low physical activity [11,12,13,14] and low fruit and vegetable consumption [15,16,17] are also causally linked to major chronic diseases: diabetes, cardiovascular disease, and chronic obstructive pulmonary disease (COPD) [18]. These chronic diseases and cancers are preventable by changing behavior concerning these risk factors.
Screening, Brief Intervention and Referral (SBIR) is a comprehensive and integrated health promotion intervention that links screening for risk factors with provision of brief advice and referrals to services that support behavior change for patients at elevated risk. In the 1980s SBIR was developed by a consortium of researchers at the World Health Organization (WHO) to screen for alcohol use disorders, followed by subsequent research in 1997 in the United States, Australia, and European countries [19]. The effectiveness of SBIR at reducing alcohol and substance use disorders and decreasing health system cost led to the inclusion of screening for other modifiable risk factors, such as tobacco use [20,21,22]. Research evidence supports the feasibility of SBIR implementation, its acceptability to patients and providers, and its effectiveness at reducing risk factors related to health behaviors [22,23,24]. Most research has focused on SBIR for alcohol use in primary care settings or emergency departments, but the implementation and evaluation of SBIR in a wide range of hospital settings and for other modifiable risk factors is still emergent [21].
Hospital settings are ideal for SBIR implementation for several reasons. First, these risk factors account for 22% of healthcare expenditures because they are leading factors of chronic diseases and cancers [25]. Secondly, 33% of patients in hospital beds have conditions related to at least one of the four risk factors [26]. Thirdly, Broyles and her colleagues (2012) have demonstrated that 80% of patients are comfortable with and accept SBIR interventions from nurses. Patients also trust and respond to behavioral health advice from health professionals during healthcare encounters [27].
Understanding the barriers and facilitators to SBIR implementation in a hospital setting is critical to providing guidance for SBIR implementation. Currently, there is little evidence or few best practices to guide SBIR implementation and the integration of health promotion services for multiple risk factors in hospital settings [19, 21]. This lack of evidence has resulted in health promotion initiatives in hospital settings failing to continue beyond the pilot stage [28]. The objective of the research is to examine the barriers and facilitators of SBIR implementation experienced by the project CPSI implementation support team (IST) and the clinical team implementers (CTI) at the rural pilot hospital.
Pilot hospital implementation setting
The Cancer Prevention and Screening Innovation (CPSI), a unit in Alberta Health Services’ (AHS) Provincial Population and Public Health, developed the health promoting hospitals initiative based on the WHO’s health promoting hospital framework. The CPSI team collaborated with the pilot hospital to test the feasibility of integrating SBIR for tobacco use, alcohol use, low physical activity, and unhealthy diet into the everyday work of healthcare providers.
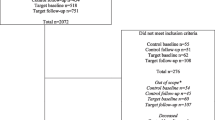
Between May 2019 and September 2020, 24 healthcare providers (nurses, social workers, and allied public health workers) in 6 units of the pilot hospital (acute care, allied health, addictions and mental health, chronic disease management, home care, and public health) implemented SBIR. SBIR was initially planned for May 2019 to September 2021, but the implementation slowed down in March 2020 due to the COVID pandemic. In September 2020, SBIR was paused indefinitely as clinical staff from the rural hospital and CPSI were redeployed to cover the COVID − 19 pandemic. During the implementation period, 543 patients participated in screening for the four factors, 52.8% were screened at the chronic disease management unit and the rest were from the other five units. Those patients screened as medium or high risk for the factors were: 27% for tobacco use, 35% for alcohol use, 59% for low physical activity, and 78% for insufficient fruit and vegetables. Of those screened medium/high risk, 59–71% received brief advice depending on the risk factor. Lastly, of those screened medium/high risk, 2–29% received referral depending on the risk factor. The detail information about the SBIR implementation processes, coverage of the SBIR intervention for each risk factors, the effectiveness of the SBIR pilot, and the patient demographics related to the risk factors are published elsewhere [29].
Methods
Study design
We carried out a qualitative inquiry based on the interpretivist approach, pragmatism, using an abductive approach to thematic analysis to evaluate the barriers and facilitators of SBIR implementation in a hospital setting. This approach combines both inductive and deductive analyses to gauge and analyze the implementation teams’ unique experiences and learnings within the theoretical context of the Consolidated Framework for Implementation Research (CFIR). The study was conducted after the indefinite pause of project implementation due to COVID-19.
Study participants
In October 2021, we invited clinical team implementers (CTI) and project implementation support team members (IST) to participate in the current qualitative study. A study invitation was sent by email to all implementation team members. We recruited participants through a combination of convenience and snowball sampling. COVID-19 was a main barrier for recruitment as clinical staff were redeployed to respond to the COVID − 19 pandemic. We used the snowball method to reach as many clinicians as possible since we could not determine who from the original pilot units were available or still located at the hospital. A total of six semi-structured, in-depth interviews were carried out with two clinical implementers and four support members. The clinicians included two registered female nurses from the pilot hospital. The first nurse was the super-user for SBIR implementation. She was also the facilitator who mentored other clinicians implementing SBIR in the six units at the hospital for the duration of the project. She was the on-ground day-to-day contact for all the clinical implementers and CPSI team. She had the experience of all implementation processes, barriers, and facilitators across all the units. The second nurse’s primary role was administrating vaccines in the public health unit, and she completed SBIR with her patients. The implementation support participants consisted of two managers, a program coordinator, and a program evaluator from CPSI, AHS, who had engaged all units to co-design and monitor the SBIR implementation process across units. During the interviews, we encouraged study participants (except the public health nurse, who was asked to share information related to her unit) to reflect on the SBIR work across the units. Most interviews lasted between 45 and 60 min, with one participant completing the interview in 15 min.
Written informed consent procedures were virtually completed. The current study received approval from our institution’s research ethics board.
Study procedures
From October to November 2021, all participants took part in a virtual, semi-structured in-depth interview. Interviews were conducted by a study investigator with mixed-methods research expertise (SM), who had not previously worked with the interviewed team members. Two investigators prepared interview guides with a standardized set of questions and discussion-stimulating probes informed by the CFIR framework (SM, KA). All interviews were conducted, audio recorded, and transcribed over the Zoom videoconferencing platform. As a quality control measure, all transcripts were reviewed and compared against their original audio file to verify accuracy and completeness. After which, audio files were digitally discarded. Participants’ confidentiality and privacy was maintained by de-identifying all transcripts and redacting any personally identifying information. Each interviewee was also assigned a reference number.
Interview guide
Informed by the CFIR, two interview guides were prepared for clinical implementers and project support team members. The CFIR provides a comprehensive framework for identifying and classifying barriers and facilitators that impact program implementation in healthcare settings [30]. We took a systematic approach to developing two, participant-specific interview guides, recognizing the distinct role clinical and project support teams played throughout the pilot implementation process. As such certain CFIR domains were more applicable to specific team members. For example, only IST participants were asked Process–planning, engaging questions since they were involved in the related tasks. Questions regarding Characteristics of the Individuals–stage of change and self-efficacy were only asked of clinical implementers because they integrated SBIR into their practice. A breakdown of interview question by CFIR domain is provided in Supplementary Table 1. Data analysis.
We adapted Thompson’s (2022) abductive or hybrid approach to thematic analysis, combining an initial bottom-up, inductive thematic analysis of interview transcripts, with a subsequent deductive analysis in which interviews were situated and contextualized within the broader CFIR framework [31]. All coding decisions and analytic direction were discussed among the study team.
Initially, an inductively driven analysis was performed, using Clarke and Braun’s (2006) six-step process: data familiarization, generating initial codes, searching for themes, defining, and naming themes, and producing a report. Inductive thematic analysis allows us to examine the unique perspectives, highlight similarities and differences, and generate unanticipated insights [32]. First, the primary investigator carried out a comprehensive and in-depth scan of all interview transcripts, noting emerging trends and patterns in brief analytic and reflexive memos. Second, an initial matrix of descriptive codes was generated from the transcripts of our first three interview, capturing patterns and commonalities observed in the raw data. This matrix served as a starting point for the coding of subsequent interviews. The codes were iteratively refined to ensure they were distinct and non-repetitive. Third, the team analyzed connections between and across codes and abstracted a set of themes and sub-themes, which were subsequentially tested for referential adequacy within the raw data. Finally, in line with the research question, themes were organized into two overarching components, facilitators and barriers.
Subsequently, a deductive analysis was carried out, whereby the five CFIR domains and 28 constructs were used to organize and interpret emerging themes and prepare a narrative synthesis of our qualitative findings. The themes were deductively mapped back to the excel spreadsheet containing the CFIR domains, constructs, and initial questions. To ensure that barrier and facilitator themes were mapped to the appropriate CFIR domains and constructs, all investigators reviewed and refined the synthesized table of results. Representative quotes were reported for each identified theme. Findings were organized by facilitators and barriers, and specific CFIR domains/constructs. This analysis allowed us to provide a substantiative account (thick description) of various facilitators and barriers as we were able situate our emerging themes within the broader contextual determinants of implementation. All data organization, coding, and analyses were carried out in NVivo 12 Pro.
Results
Our inductive analysis revealed barriers and facilitators to SBIR implementation in six contexts: the SBIR tool, patients, clinical implementors, the pilot hospital, the Alberta health care system, and the broader community. Implementation support team participants primarily perceived facilitators to SBIR implementation while clinical implementors largely perceived barriers to implementation. This may reflect each group’s unique roles and capacity of engagement throughout the implementation process (Supplementary Table 2).
Key facilitators to SBIR implementation
At the health system level, the key facilitator to SBIR implementation was related to planning and engagement, as outlined in Table 1. Prior to SBIR implementation, the support team built formative and collaborative relationships with relevant clinical departments within Alberta Health Services (AHS). These relationships helped to align the intervention with Canadian guidelines and AHS’ health promotion and disease prevention standards on fruit and vegetable consumption, tobacco use, alcohol use, and physical activity. This enabled the development and evaluation of the SBIR intervention.
At the hospital level, the implementation support team customized PowerPoint presentations and promotional materials to brand the SBIR intervention (readiness for implementation, leadership engagement). These resources facilitated managers’ understanding and buy-in. To ensure successful SBIR implementation, feedback reports were co-designed with unit managers to support decision making (Readiness- leadershipaccess to knowledge and information).
The support team developed flexible drop-in style training sessions, customized the SBIR to clinicians’ workflow, and created scripts to support clinicians’ confidence in conducting SBIR with their patients (Readiness– access to knowledge and information). As well, the support team funded a dedicated implementation facilitator (Readiness–available resources) at the pilot hospital and trained SBIR super-users to support clinical implementers’ information needs and confidence during SBIR with patients (knowledge and self-efficacy). The support team perceived that training would increase clinical implementers’ understanding of all SBIR risk factors and their impact on patient health. The support team also perceived that training would increase clinical implementers’ motivation and confidence to apply SBIR within their practice (Readiness–available resources).
The support team enabled the SBIR intervention to be operationalized by developing context-specific resources for all stages of the SBIR intervention: feedback reports, funding a dedicated SBIR implementation facilitator, training, and resources for clinical staff to implement SBIR with patients, and patient risk factor pamphlets (Readiness–access to information).
Key b to SBIR implementation
Clinical implementers faced several challenges with integrating SBIR plans, training, resources, and tools into their clinical practice, as summarized in Table 2. In particular, clinicians noted barriers related to adaptability and design quality and packaging. First, clinicians reported that the screening questions did not fit with the patient’s appointment purpose. Second, clinicians indicated the SBIR paper screening form made it difficult to manage patient information: potential for errors in data transfer; restricted information flow (using fax machine); incomplete screening due to user error; and possible breech of patient confidentiality and privacy (faxing to a unit outside of the hospital). Third, the SBIR intervention impacted clinicians’ workflow and workload by increasing the amount of time they needed to spend with the patient. Clinicians reported that they often referred to paper-based educational materials because they forgot the meaning of the risk assessment score for each factor. Despite the support teams’ efforts to tailor the SBIR intervention to clinicians’ workflow, the data collection increased clinicians’ existing workload and interrupted their workflow.
Clinicians noted barriers related to patients’ needs and resources. First, clinician’s felt that by providing information brochures to all medium and high-risk scoring patients, they did not consider the patients’ readiness to change. Second, clinicians indicated that referral wait times were lengthy for risk factor behavior change resources. They perceived that patients’ readiness to change could be supported after SBIR with immediate access to resources within the community, especially for physical activity and fruit and vegetable intake. Third, clinicians perceived that the difficult referral pathways and AHS health system barriers were reflective of broader challenges with the healthcare system’s focus on disease treatment rather than prevention. Clinician felt that healthcare providers often see patients at later stages of health decline rather than preventing disease. During SBIR implementation, clinicians discovered that they had limited knowledge on supporting patient through behavior changes and there were scarce patients’ resources on physical activity and nutrition.
Clinicians perceived barriers related to patients’ knowledge and beliefs, reporting they often encountered patients expecting immediate health benefits from short term behavior changes. They recognized that patient’s choices were based on convenience and felt that patients lacked health literacy. Clinicians indicated that they often did not know how to address patients’ beliefs on instant behavior change or immediate health benefits, and this resulted in their low motivation to implement SBIR. While clinicians were provided SBIR training, they lacked the experience and clinical training to address patients’ questions regarding the modifiable risk factors. Clinicians indicated that healthcare providers tend to judge “good” and “bad” behaviors rather than recognizing that patients’ process to understanding and changing risk factor behavior requires small steps or gradual behavioral change. Clinical implementers reported that executing the referral process proved difficult due to the lack of trust between providers. Perceived challenges to executing, reflecting, and evaluating can be found in the Table 1.
Diverging perspectives on facilitators and barriers
We noted tensions between how participants defined barriers and facilitators. For example, the support team and clinical implementers held opposing views on implementation climate. For the support team, management buy-in and leadership involvement was a driving factor to sway clinician hesitancy to implement.
The support team perceived management leadership and project champions were key to facilitating implementation. They also perceived that identification of super-users would facilitate implementation by developing workflow pathways. Clinicians, however, felt that all managers and super users did not buy into SBIR. As a result, they could not influence clinicians’ hesitancy or their attitudes towards SBIR.
The different perspectives on management, super-users, and champions could be attributed to the role and position that the support team and clinical implementers played in the SBIR implementation, which affected their ability to observe SBIR in action.
Discussion
The clinical implementers primarily reported barriers and the implementation support team primarily reported facilitators to implementing SBIR. Tackling the barriers to SBIR implementation is of paramount importance to effectively develop better plans to support future SBIR implementation in hospital settings.
The support team and clinical implementers both encountered challenges with the paper format of the SBIR (design), which interrupted clinicians’ workflow and data management. Other studies have indicated that when SBIR is integrated into the electronic health records (EHR), workflow barriers were removed: audio-visual aids and systemized reminders facilitated innovation implementation to support workflow [21, 33]. Paper SBIR forms have been negatively perceived as an unsustainable innovation because it exists outside of the EHR as a separate work process [34]. Comparative studies of the effects of paper-based and EHR processes on healthcare provider work practices have demonstrated the value of EHR to significantly improve the efficiency of clinicians’ use of time [35]. Using EHR can streamline clinicians’ workflow. It also removes the need to manually fax patients’ information from one site to another as all EHR are linked together. EHR align health systems operation, workflow, and enables healthcare providers to intervene at earlier stages of patients’ health [36, 37]. However, EHR also create vast changes to the healthcare system that requires technological interoperability, stakeholder involvement across the healthcare system, and significant government investment [38]. As well, it is important to understand the social context for implementation will vary depending on the care setting [39]. EHR are not a panacea to public health challenges, but they can be an effective tool when designed with end-users in mind.
Clinicians reported barriers to SBIR implementation related to their own, and their patients’ knowledge / beliefs and self-efficacy, which led to a hesitancy to complete SBIR with patients. Other studies have also found healthcare providers often lacked sufficient SBIR related knowledge and SBIR training to reduce the stigma associated with substance use [33, 40, 41]. Evidence indicates that formal training in SBIR for clinicians facilitates knowledge and self-efficacy in SBIR [42]. However, educational programs for SBIR and substance use remain inadequate and limited with a predominate focus on physicians [43]. In the current post-pandemic climate, future SBIR implementation will need to consider co-designing SBIR education for nurses, provide flexible training schedules, and comprehensive education materials that are also time sensitive [41, 44].
Clinicians perceived significant barriers for patients (patients’ needs and resources), particularly patients’ lack of risk factor knowledge, readiness to change, and the stigma associated with disclosing alcohol use. Other studies have also found patients often lack knowledge about risk factors, the skills and motivation to change their behavior [40]. Clinicians and patients’ perceptions of stigma around alcohol [45, 46]; weight- healthy eating [47,48,49]; and tobacco [50] impacts patients’ decision to seek medical care [51] and contributes to adverse health outcomes [52]. Stigma related to these risk factors have been documented in the literature, which have created hesitancy in clinicians and patients [53]. Future SBIR implementation will need to co-design patient-centered communication strategies in SBIR with patients [54,55,56] and train clinicians to provide nonjudgmental screening and brief intervention. Some destigmatizing and nonjudgmental approaches involve understanding the terminologies used by communities, demonstrating understanding and acceptance [57] and disentangling the patients’ behavior from their identity [58].
Studies have also found that patients lack sufficient resources and programs in their communities to support their risk factor related behavior change [41, 59]. Strategies to mitigate the paucity of support services in communities may include electronic health (eHealth) solutions provided through websites (programs, social networks), mobile devices (smart phones, tablets), and digital technologies (apps and tracking devices). eHealth patient resources for physical activity [60], physical activity and healthy eating [61], alcohol use [62], and smoking cessation [63] demonstrate effectiveness as standalone applications or in combination with face-to-face clinical support. However, just as there are health inequities, there are also communication and technology inequities. eHealth solutions must be designed and implemented with underserved populations in mind, which means eHealth solutions may need to create or build patient readiness for digital technology / internet / communication literacy for these types of support services to be usable and effective [64]. If clinicians are expected to utilize eHealth solutions, they will need to be involved in co-designing its utility and incorporation into seamless workflow [60].
Aside from the strategies suggested in the above, many of the barriers found in this study (networks and communications, culture, implementation climate, readiness for implementation, knowledge and beliefs, self-efficacy) can be translated as opportunities to assess readiness [65]. Utilizing a CFIR based readiness assessment provides a systems approach to assessing contextual factors of readiness [65, 66] compared to individual perceptions approach [67]. Miake-Lye et al. (2020) systematic review and content analysis of readiness assessments indicate that nearly all the questions could be mapped back to CFIR. SBIR implementation in Alberta hospital settings would benefit from considering the barriers found in each of the constructs here and assess readiness at different stages of project development and implementation.
Strength and limitations
This study’s strengths include the use of CFIR as the basis for the development of the semi-structured interview questions, data collection, and analysis. It offers a comprehensive approach to understanding the barriers and facilitators of SBIR implementation. Second, the semi-structured interview foregrounds the participants’ lead and perspectives and ensured our interviews were conversational and organically stimulated discussions around areas of inquiry. Third, our abductive approach to thematic analysis allowed us to not only champion participants’ unique perspectives, but enabled thick description, by contextualizing their experiences within the broader determinants of implementation uptake.
Despite the strength of this research, there are also limitations. First, this is a single site study and only a few of the clinical implementers participated in the interviews. Second, due to the COVID– 19 pandemic, this study took place almost one year after SBIR was indefinitely paused in the pilot hospital. All healthcare teams, including those in the pilot site and CPSI, were responding to COVID-19. Third, the smaller number of clinical participants limits the transferability of study findings to other health contexts. Despite our best efforts to recruit more clinical implementers, employing both convenience and snowball sampling, they were either not available or could not be located after COVID– 19 redeployments. More interviews in the future with clinical implementers would provide greater detail on their patients’ needs and resources, their SBIR knowledge and beliefs, the intervention’s adaptability and design, and diverse perspectives of other barriers and facilitators to SBIR implementation. Fourth, the absence of interviews with patients limited the ability to thoroughly investigate patients’ needs and resources from their own perspective. Future studies would benefit from taking a patient-centered approach to investigating SBIR implementation to ensure it is acceptable to them. Lastly, future studies will need to document, compare and contrast the differences and similarities of implementing each risk factor from the perspective of the clinicians and patients. Approaches to plan and evaluate SBIR maybe similar, but patients and clinicians’ experiences of each risk factor maybe more nuanced.
Conclusion
The current study offers unique insights into the facilitators and barriers of implementing a SBIR intervention for multiple risk factors in the hospital setting. The key facilitator of implementation lies with planning and engaging partners and stakeholders to ensure that screening questions, advice, and support services were aligned with other departments at AHS. This provided health system alignment around guidelines, questions, and practices. Collaborating with managers and providing SBIR training to clinicians ensured their readiness to use SBIR. However, clinicians reported several barriers to integrating SBIR into their workflow, including a lack of knowledge and self-efficacy around supporting patients with behavior change and providing adequate support to meet patients’ needs. Enhancing clinician training to include patient-centered communication, ways to approach patient stigma, and more information resources on the risk factors would improve clinicians and patients SBIR experience. Additionally, the pen-and-paper approach was found to impede clinicians’ workflow and operations. Future implementation studies will explore the delivery of SBIR through an electronic medical record and will integrate barriers/facilitators identified here to improve intervention delivery and clinician readiness.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AHS:
-
Alberta Health Services
- CFIR:
-
Consolidated Framework for Implementation Research
- CPSI:
-
Cancer Prevention and Screening Innovations
- CTI:
-
Clinical team implementers
- eHealth:
-
Electronic health
- EHR:
-
electronic health record
- IST:
-
Implementation support team
- SBIR:
-
Screening brief intervention and referral
- WHO:
-
World Health Organization
References
Canadian Cancer Statistics Advisory Committee, collaboration with the Canadian Cancer Society. S, Canada and the Public Health Agency of Canada K. Canadian Cancer Statistics [Internet]. Can. Cancer Socity. 2021 [cited 2022 Mar 8]. Available from: cancer.ca/Canadian-Cancer-Statistics-2021-EN.
Alberta Health Services. The 2017 Report on Cancer Statistics in Alberta (ROCSIA) [Internet]. Cancer Meas. Outcomes Res. Eval. 2017. Available from: https://public.tableau.com/views/The2017ReportonCancerStatisticsinAlberta/Highlights?showVizHome=no.
Grundy A, Poirier AE, Khandwala F, Grevers X, Friedenreich CM, Brenner DR. Cancer incidence attributable to lifestyle and environmental factors in Alberta in 2012: summary of results. C open. 2017;5.
Poirier AE, Ruan Y, Volesky KD, King WD, O’Sullivan DE, Gogna P et al. The current and future burden of cancer attributable to modifiable risk factors in Canada: Summary of results. Prev Med (Baltim). 2019;122.
Brenner DR, Friedenreich CM, Ruan Y, Poirier AE, Walter SD, King WD et al. The burden of cancer attributable to modifiable risk factors in Canada: methods overview. Prev Med (Baltim). 2019;122.
Madero-Cabib I, Bambs C. Association between lifetime tobacco use and alcohol consumption trajectories and cardiovascular and chronic respiratory diseases among older people. Int J Environ Res Public Health. 2021;18.
Manhapra A, Rosenheck R. Tobacco Use Disorder among patients with smoking-related Chronic Medical Disease: Association with Comorbid Substance Use disorders. J Addict Med. 2017;11.
Pan CS, Ju TR, Lee CC, Chen YP, Hsu CY, Hung DZ et al. Alcohol use disorder tied to development of chronic kidney disease: a nationwide database analysis. PLoS ONE. 2018;13.
Schwarzinger M, Thiébaut SP, Baillot S, Mallet V, Rehm J. Alcohol use disorders and associated chronic disease - A national retrospective cohort study from France. BMC Public Health. 2017;18.
Rumgay H, Shield K, Charvat H, Ferrari P, Sornpaisarn B, Obot I et al. Global burden of cancer in 2020 attributable to alcohol consumption: a population-based study. Lancet Oncol. 2021;22.
Briant KJ, Sanchez JI, Ibarra G, Escareno M, Gonzalez NE, Gonzalez VJ et al. Using a culturally tailored intervention to increase colorectal cancer knowledge and screening among hispanics in a rural community. Cancer Epidemiol Biomarkers Prev [Internet]. 2018;27:1283–8. Available from: http://cebp.aacrjournals.org/content/27/11/1283.full-text.pdfhttp://ovidsp.ovid.com/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=emexb&AN=624899327http://ucalgary-primo.hosted.exlibrisgroup.com/openurl/01UCALG/UCALGARY?sid=OVID:embase&id=pmid:29871884&.
Goetzel RZ, Liss-Levinson RC, Goodman N, Kennedy JX. Development of a community-wide cardiovascular risk reduction assessment tool for small rural employers in upstate New York. Prev Chronic Dis. 2009;6.
Garcia LMT, Da Silva KS, Del Duca GF, Da Costa FF, Nahas MV. Sedentary behaviors, leisure-time physical inactivity, and chronic diseases in Brazilian workers: A Cross sectional study. J Phys Act Heal. 2014;11.
Christofoletti M, Del Duca GF, da Silva KS, Meneghini V, de Carvalho Malta D. Physical inactivity, television time and chronic diseases in Brazilian adults and older adults. Health Promot Int. 2020;35.
Serdula MK, Byers T, Mokdad AH, Simoes E, Mendiein JM, Coates RJ. The association between fruit and vegetable intake and chronic disease risk factors. Epidemiology. 1996;7.
Hung HC, Joshipura KJ, Jiang R, Hu FB, Hunter D, Smith-Warner SA et al. Fruit and vegetable intake and risk of major chronic disease. J Natl Cancer Inst. 2004;96.
Boeing H, Bechthold A, Bub A, Ellinger S, Haller D, Kroke A et al. Critical review: vegetables and fruit in the prevention of chronic diseases. Eur J Nutr. 2012.
Ng R, Sutradhar R, Yao Z, Wodchis WP, Rosella LC. Smoking, drinking, diet and physical activity - modifiable lifestyle risk factors and their associations with age to first chronic disease. Int J Epidemiol. 2020;49.
Babor TF, McRee BG, Kassebaum PA, Grimaldi PL, Ahmed K, Bray J, Screening. Brief intervention, and Referral to Treatment (SBIRT): toward a Public Health Approach to the management of substance abuse. Subst Abus. 2007;28:7–30.
Minian N, Lingam M, Moineddin R, Thorpe KE, Veldhuizen S, Dragonetti R et al. Impact of a web-based clinical decision support system to assist practitioners in addressing physical activity and/or healthy eating for smoking cessation treatment: protocol for a hybrid type i randomized controlled trial. JMIR Res Protoc. 2020;9.
Thoele K, Moffat L, Konicek S, Lam-Chi M, Newkirk E, Fulton J et al. Strategies to promote the implementation of Screening, Brief Intervention, and Referral to Treatment (SBIRT) in healthcare settings: a scoping review. Subst Abuse Treat Prev Policy [Internet]. 2021;16:42. Available from: https://substanceabusepolicy.biomedcentral.com/articles/https://doi.org/10.1186/s13011-021-00380-z.
Mullen KA, Manuel DG, Hawken SJ, Pipe AL, Coyle D, Hobler LA et al. Effectiveness of a hospital-initiated smoking cessation programme: 2-year health and healthcare outcomes [Internet]. Tob. Control. England: BMJ Publishing Group; 2017. p. 293–9. Available from: http://krs.summon.serialssolutions.com/2.0.0/link/0/eLvHCXMwlV1Lj9MwELZYkAAJ8SgsFAoyFzilJI6f3JZVCxyQEFq0cIqc2FHL0gQ17YF_z0zilGZBK_USVfFDsf15_Lmeb0xIyqZxdMkmmDKXsbKSW40Ha7AIl6h_dxLwZVmMeuf3p-rzF_Hum5jtacSGB_pJKt8gzAuwFZ0jNwxyIqJYMMX0EbnBNLAFhPn3s79HCaq9gxG.
Bruguera P, Barrio P, Manthey J, Oliveras C, López-Pelayo H, Nuño L et al. Mid and long-term effects of a SBIRT program for at-risk drinkers attending to an emergency department. Follow-up results from a randomized controlled trial. Eur J Emerg Med. 2021;28.
Schröder H, Cárdenas-Fuentes G, Martínez-González MA, Corella D, Vioque J, Romaguera D et al. Effectiveness of the physical activity intervention program in the PREDIMED-Plus study: a randomized controlled trial [Internet]. Int. J. Behav. Nutr. Phys. Act. England: BioMed Central Ltd; 2018. p. 110. Available from: http://krs.summon.serialssolutions.com/2.0.0/link/0/eLvHCXMwnV1Lj9MwELa2e0JCiDeBZWUuICGlTezYSbjttl3gsKhCIHGzEj8gok2rPiTEr2fGcaoGbhwqtfE4rTUznpn0m8-EcDZO4r_2BO2ETq023OTcSkgZeA65gnEy18bZFNuf30_zxWdx_U3Mz4joW2M8hl_XzbhdrsZt88NDLTcrPelhY5PF7RQieAb3nIzIKOdlX7F.
Manuel DG, Perez R, Bennett C, Laporte A, Wilton AS, Gandhi S et al. A $4.9 Billion Decrease in Health Care Expenditure: The Ten-Year Impact of Improving Smoking, Alcohol, Diet and Physical Activity in Ontario [Internet]. Inst. Clin. Eval. Sci. Toronto, Ontario; 2016 [cited 2022 May 26]. p. 180. Available from: https://www.researchgate.net/publication/301282804.
Manuel DG, Perez R, Bennett C, Rosella L, Choi B. 900,000 Days in Hospital: The Annual Impact of Smoking, Alcohol, Diet and Physical Activity on Hospital Use in Ontario [Internet]. ICES. 2014 [cited 2022 May 26]. Available from: https://www.ices.on.ca/Publications/Atlases-and-Reports/2014/900000-Days-in-Hospital.
Broyles LM, Rosenberger E, Hanusa BH, Kraemer KL, Gordon AJ. Hospitalized patients’ acceptability of nurse-delivered screening, brief intervention, and referral to treatment. Alcohol Clin Exp Res. 2012;36.
Whitehead D. The European Health promoting hospitals (HPH) project. How far on? Health Promot Int. 2004;19.
Adhikari K, Kashif Mughal M, Whitworth J, Bischoff M, Teare GF. Implementing screening, Brief Intervention and Referral Intervention for Health Promotion and Disease Prevention in Hospital Settings in Alberta: a pilot study. Int J Public Health. 2023;68.
Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science [Internet]. Implement. Sci. England: BioMed Central Ltd; 2009. p. 50. Available from: http://krs.summon.serialssolutions.com/2.0.0/link/0/eLvHCXMwpV3NbhMxELagXJCqqvx22xL5xmlh12uvvb01VQNHhEBCXCzH9tII2KBu-hI8NTO2t60Tbr1FGTuONTOfZ8YzY0Ia9q4qtzCBO1VzW1cNN8JIU9fecnAF4HMD6Bhef_twIT99FvNv4vIu_LF1oV-r9j1Y0KrEh7pLXqKv_oSByobCrfn3CYI59niPlZBxbOrWuDt.
Thompson J. A guide to Abductive Thematic Analysis. Qual Rep. 2022;27:1410–21.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3.
Correa VC, Lugo-Agudelo LH, Aguirre-Acevedo DC, Contreras JAP, Borrero AMP, Patiño-Lugo DF et al. Individual, health system, and contextual barriers and facilitators for the implementation of clinical practice guidelines: a systematic metareview. Heal Res Policy Syst. 2020.
Keen A, Thoele K, Oruche U, Newhouse R. Perceptions of the barriers, facilitators, outcomes, and helpfulness of strategies to implement screening, brief intervention, and referral to treatment in acute care. Implement Sci. 2021;16.
Vaghefi I, Hughes JB, Law S, Lortie M, Leaver C, Lapointe L. Understanding the impact of electronic medical record use on practice-based population health management: a mixed-method study. JMIR Med Inf. 2016;4.
Kite BJ, Tangasi W, Kelley M, Bower JK, Foraker RE. Electronic Medical Records and Their Use in Health Promotion and Population Research of Cardiovascular Disease. Curr Cardiovasc Risk Rep [Internet]. 2014;9:422. https://doi.org/10.1007/s12170-014-0422-5.
Carmichael JM, Meier J, Robinson A, Taylor J, Higgins DT, Patel S. Leveraging electronic medical record data for population health management in the Veterans Health Administration: successes and lessons learned. Am J Heal Pharm. 2017;74.
Yuan B, Li J, Wu P. The effectiveness of electronic health record promotion for healthcare providers in the United States since the Health Information Technology for Economic and Clinical Health Act: an empirical investigation. Int J Health Plann Manage. 2021;36.
Rajamani S, Hultman G, Bakker C, Melton GB. The role of organizational culture in health information technology implementations: a scoping review. Learn Heal Syst. 2021.
Vendetti J, Gmyrek A, Damon D, Singh M, McRee B, Del Boca F. Screening, brief intervention and referral to treatment (SBIRT): implementation barriers, facilitators and model migration. Addiction. 2017;112.
Johnson M, Jackson R, Guillaume L, Meier P, Goyder E. Barriers and facilitators to implementing screening and brief intervention for alcohol misuse: a systematic review of qualitative evidence. J Public Health (Bangkok). 2011.
Babor TF, Higgins-Biddle JC, Higgins PS, Gassman RA, Gould BE. Training Medical Providers to Conduct Alcohol screening and brief interventions. Subst Abus. 2004;25.
Neushotz LA, Fitzpatrick JJ. Improving substance abuse screening and intervention in a primary care clinic. Arch Psychiatr Nurs. 2008;22.
Galanis P, Vraka I, Fragkou D, Bilali A, Kaitelidou D. Nurses’ burnout and associated risk factors during the COVID-19 pandemic: a systematic review and meta-analysis. J Adv Nurs. 2021.
Keyes KM, Hatzenbuehler ML, McLaughlin KA, Link B, Olfson M, Grant BF et al. Stigma and treatment for alcohol disorders in the United States. Am J Epidemiol. 2010.
Bryan AEB, Kim HJ, Fredriksen-Goldsen KI. Factors associated with high-risk alcohol consumption among lgb older adults: the roles of gender, social support, perceived stress, discrimination, and stigma. Gerontologist. 2017;57.
Himmelstein MS, Puhl RM, Quinn DM. Intersectionality: an understudied Framework for addressing Weight Stigma. Am J Prev Med. 2017;53.
Phelan SM, Burgess DJ, Yeazel MW, Hellerstedt WL, Griffin JM, van Ryn M. Impact of weight bias and stigma on quality of care and outcomes for patients with obesity. Obes Rev. 2015.
Tomiyama AJ, Carr D, Granberg EM, Major B, Robinson E, Sutin AR et al. How and why weight stigma drives the obesity epidemic and harms health. BMC Med. 2018;16.
Carter-Harris L, Ceppa DKP, Hanna N, Rawl SM. Lung cancer screening: what do long-term smokers know and believe? Heal Expect. 2017;20.
Taber JM, Leyva B, Persoskie A. Why do people avoid Medical Care? A qualitative study using National Data. J Gen Intern Med. 2015;30.
Kane JC, Elafros MA, Murray SM, Mitchell EMH, Augustinavicius JL, Causevic S et al. A scoping review of health-related stigma outcomes for high-burden diseases in low- and middle-income countries. BMC Med. 2019.
Hanschmidt F, Manthey J, Kraus L, Scafato E, Gual A, Grimm C et al. Barriers to alcohol screening among hypertensive patients and the role of stigma: lessons for the implementation of screening and brief interventions in European primary care settings. Alcohol Alcohol. 2017;52.
Jay M, Gillespie C, Schlair S, Sherman S, Kalet A. Physicians’ use of the 5As in counseling obese patients: is the quality of counseling associated with patients’ motivation and intention to lose weight? BMC Health Serv Res. 2010;10.
Helitzer DL, LaNoue M, Wilson B, de Hernandez BU, Warner T, Roter D. A randomized controlled trial of communication training with primary care providers to improve patient-centeredness and health risk communication. Patient Educ Couns. 2011;82.
Dang BN, Westbrook RA, Njue SM, Giordano TP. Building trust and rapport early in the new doctor-patient relationship: a longitudinal qualitative study. BMC Med Educ. 2017;17.
Ortega P, Prada J. Words matter: translanguaging in medical communication skills training. Perspect Med Educ. 2020;9.
Moore MD, Ali S, Burnich-Line D, Gonzales W, Stanton MV, Stigma. Opioids, and Public Health Messaging: The Need to Disentangle Behavior From Identity [Internet]. Am. J. public Heal. United States; 2020. p. 807–10. Available from: https://go.exlibris.link/gxKHls4b.
Hargraves D, White C, Frederick R, Cinibulk M, Peters M, Young A et al. Implementing SBIRT (screening, brief intervention and referral to treatment) in primary care: lessons learned from a multipractice evaluation portfolio. Public Health Rev. 2017.
Wattanapisit A, Tuangratananon T, Wattanapisit S. Usability and utility of eHealth for physical activity counselling in primary health care: a scoping review. BMC Fam Pract. 2020;21.
Gill DP, Blunt W, Boa Sorte Silva NC, Stiller-Moldovan C, Zou GY, Petrella RJ. The HealtheSteps™ lifestyle prescription program to improve physical activity and modifiable risk factors for chronic disease: a pragmatic randomized controlled trial. BMC Public Health. 2019;19.
Johansson M, Berman AH, Sinadinovic K, Lindner P, Hermansson U, Andréasson S. Effects of internet-based cognitive behavioral therapy for harmful alcohol use and alcohol dependence as self-help or with therapist guidance: three-armed randomized trial. J Med Internet Res. 2021;23.
Zhao K, Wang X, Cha S, Cohn AM, Papandonatos GD, Amato MS et al. A Multirelational Social Network Analysis of an Online Health Community for Smoking Cessation [Internet]. J. Med. Internet Res. Canada: JMIR Publications; 2016. p. e233–e233. Available from: https://go.exlibris.link/F9gml3qt.
Lee EWJ, McCloud RF, Viswanath K. Designing Effective eHealth interventions for Underserved groups: five lessons from a decade of eHealth intervention Design and Deployment. J Med Internet Res. 2022;24.
Miake-Lye IM, Delevan DM, Ganz DA, Mittman BS, Finley EP. Unpacking organizational readiness for change: an updated systematic review and content analysis of assessments. BMC Health Serv Res. 2020;20.
Kononowech J, Hagedorn H, Hall C, Helfrich CD, Lambert-Kerzner AC, Miller SC et al. Mapping the organizational readiness to change assessment to the Consolidated Framework for Implementation Research. Implement Sci Commun. 2021;2.
Weiner BJ. A theory of Organizational Readiness for Change. Implement Sci. 2009;4.
Acknowledgements
Not applicable.
Funding
This research was funded by Alberta Health through the Cancer Prevention and Screening Innovation (CPSI) in Alberta Health Services. Provision of funding by Alberta Health does not signify that this project represents the policies or views of Alberta Health. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
Author information
Authors and Affiliations
Contributions
K.A and G.T was involved in the conception and design of the study. J.L and S.M were responsible for designing the interview guide. S.M was responsible for conducting the data analysis. S.M prepared a first draft of the manuscript. K.A, G.T, and S.M contributed to interpretation of data and provided intellectual content and revisions to manuscript. J.L reviewed and offered improvements to the draft manuscript. All authors read and approved the final draft.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
This research project received ethics approval from the Health Research Ethics Board of Alberta– Cancer Committee– at the University of Calgary: HREBA.CC-19-0441. All participant filled and signed an informed consent form for this research study prior to any data collection. This study complies with the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
12913_2024_10676_MOESM2_ESM.docx
Supplementary Material 2: Facilitators and barriers of SBIR implementation in hospital settings using the Consolidated Framework for Implementation Research (CFIR)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Mah, S.S., Teare, G.F., Law, J. et al. Facilitators and barriers for implementing screening brief intervention and referral for health promotion in a rural hospital in Alberta: using consolidated framework for implementation research. BMC Health Serv Res 24, 228 (2024). https://doi.org/10.1186/s12913-024-10676-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-024-10676-y