Abstract
Background
Losing a close other to cancer is an incisive experience that occurs after a long course of illness and intense family caregiving. Despite an evident need for family engagement and support and guidance on this, patients and family members may not receive the attention and support they need when a family unit is experiencing a disruption by death. A clear understanding of the quality of care that is currently provided and its ability to address family needs is necessary to improve end-of-life and bereavement support to families affected by cancer. The purpose of this study is to investigate the quality of support of end-of-life and bereavement care to families, their (un)met needs, grief experiences, and self-perceived health outcomes.
Methods
A multi-center, cross-sectional observational survey study with family members (n = 35) whose close other died of cancer in a health institution or their own home in German-speaking Switzerland.
Results
Bereaved family members were mostly satisfied with end-of-life care. Information on the grief process and services, and acknowledgment of their grief was experienced as helpful. Most coped with their grief drawing on family resources and exhibited resilience, but they reported unmet needs in relation to family togetherness and caregiving.
Conclusion
This study with a small number of family members indicates that support provided to families across settings and illness trajectories is perceived as helpful, with specific needs related to family support. The findings suggest that improvements should focus on ensuring care that addresses the family as a unit and enables togetherness, mutual reflection, meaningful relationships, preparedness for death, resilience, and benefit-finding.
Protocol registration
Similar content being viewed by others
Background
Losing a close other to cancer is an incisive experience that occurs after a long illness course and intense family caregiving [1, 2]. Families’ experience of caregiving, communication about end-of-life, and support received as a family impact on their grief experience and psychosocial health [3,4,5,6], whereas families’ functioning and preparedness for death is associated with complicated grief responses [7, 8]. To promote family resilience and well-being over time and to prevent adverse family outcomes, there is a need to focus cancer care on the family as a unit to address their needs, soften their suffering, increase their preparedness for the loss, and facilitate living with the loss [9,10,11,12]. Evidence-based recommendations include assessing and addressing families’ needs early on, offering practical and emotional support to enable preferred caregiving roles, providing information and communication about end-of-life, promoting families’ preparedness for loss and ability to cope with death and dying as a family, offering health-promoting follow-up care to strengthen family resilience and well-being, and identifying and referring those at risk for complicated courses of bereavement to specialist services [12,13,14,15,16,17].
Despite the availability of evidence-based guidance [13, 14, 16, 17], patients and families may not receive the attention and support they need as a relational family unit that is about to experience a profound disruption by death [18,19,20,21]. Family members’ and cancer care professionals’ focus is often on the person with advanced cancer and care to family members usually ends with the patient’s death [16, 17, 22]. This means that families may not voice their own concerns and needs [23, 24]. At the same time health professionals may not recognize and proactively address families’ role and needs due to a lack of awareness, time, or priority-setting [25, 26]. Improvement in end-of-life and bereavement support to families affected by cancer has therefore been called for [27]. A clear understanding of the quality of care and its ability to address family needs is required. As part of the BEST CARE research project (Guideline-based end-of-life and BEreavement SupporT in Cancer CARE, https://osf.io/j4kfh), we assessed the type and quality of support that families received during end-of-life and in bereavement following the loss of a close other to cancer and explored their (un)met needs and bereavement outcomes.
Methods
A cross-sectional survey was conducted with family members bereaved by cancer. The aims of this study were, first, to explore the quality of support that bereaved family members received at the end-of-life and in bereavement, the fulfillment of their needs during bereavement, and bereavement and health outcomes; second, to examine differences in these outcomes between different places of death (i.e., health institution vs. home care); and third, to examine the relationship between quality of support and bereavement outcomes.
Setting and participants
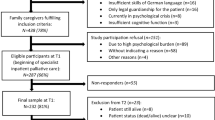
The study was carried out in four hospitals and three home palliative care services in an urban area in German-speaking Switzerland. Family members were eligible to take part if they had been bereaved due to cancer for two to six months, had been a primary support person or carer, and were at least 18 years old. Family members who did not provide informed consent, did not possess sufficient German language skills to complete the questionnaire, were not cognitively able to understand or participate in the study, or had a self-reported mental health illness before their experience of loss, were excluded.
Recruitment and data collection
Eligible participants were prospectively invited to participate by a clinician or service manager within the available recruitment period lasting from December 2021 to September 2022. First, they were informed about the study and received a study flyer. If they agreed, their contact details were communicated to the research team, who sent out a study information pack by email with a personalized link to the online questionnaire (REDcap; https://www.project-redcap.org), or by mail with a paper-pencil questionnaire. Participants were able to complete the questionnaire at a time of their convenience in their own home. Online questionnaires could be interrupted and then continued at a later time. If necessary, family members were reminded by phone or by email at three-week intervals.
The questionnaire had three sections focusing on [1] quality of support received during end-of-life and bereavement (56 items), [2] needs during bereavement (20 items), and [3] bereavement and health outcomes (17 items). Participants rated the questionnaire to be mostly understandable and easy to complete (mdn = 4, score range: 1 = totally disagree to 5 = totally agree, n = 34). They indicated that the length of the questionnaire was rather appropriate in terms of completion time (mdn = 4, score range: 1 = totally disagree to 5 = totally agree, n = 33). Psychometrically validated rating scales were used. In addition, three self-developed rating scales on self-perceived health were used after review for validity by researchers from nursing, bereavement care, family health, and psychology. Some of the measures were translated from English into German with permission using a forward-backward translation procedure [28] (see Table 1). Participating family members provided their demographics and proxy data on the demographics of the deceased and the circumstances of their death. A research assistant entered paper-pencil questionnaires into REDcap via direct entry forms.
Study endpoints
Quality of support received as a family
The support families received from health professionals was assessed by the 14-item German version of the “ICEland Family Perceived Support Questionnaire” (ICE-FPSQ). It includes two subscales: “cognitive support” (5 items) and “emotional support” (9 items), which were rated on a 5-point Likert-type scale from 1 = almost never to 5 = almost always, resulting in a sum score of 14–70 overall, 5–25 for the cognitive, and 5–45 for the emotional support scale. This questionnaire showed high internal consistency (Cronbach’s above > 0.86) [29, 30].
In addition, we assessed which groups of health professionals (i.e., nurses, physicians, medicinal assistants, chaplains, therapists, social workers, and others) provided the support.
Quality of end-of-life care
To assess satisfaction with the end-of-life care, we used the 24-item “Canadian Health Care Evaluation Project - Bereavement Questionnaire” (CANHELP). Items were scored on a 5-point Likert-type scale ranging from 1 = totally disagree to 5 = totally agree. The CANHELP has high internal consistency, with a Cronbach’s alpha of 0.93 [31].
Quality of bereavement support
To obtain information on the type and quality of bereavement support, we adopted a selection of close-ended questions from the “Evaluation of Grief Support Services” (EGGS) by the National Hospice and Palliative Care Organization with permission [32], and one from a previous study by Tracey and Miller [33]. Questions pertained to grief information (i.e. “Were the following communicated to you after the death?”, “How useful was the information provided to you about…?”), follow-up support (e.g., “Was the number of telephone calls you received too few, about right, too many?”, “When you called for information or support, how did we do in getting you help as soon as you needed it?”), and questions about the overall quality of the service (i.e., “After the death, how well would you say our grief support services met your needs?”) and the skills of the person delivering the support (e.g., “How would you describe the skills of the person who provided grief support to you? S/he listened to me, understood me, was honest, was helpful” etc.).
Fulfillment of needs
To assess the (un)met needs among bereaved family members, we used the 20-item “Needs Assessment of Family Caregivers– Bereaved to Cancer” (NAFC-BvC). Each needsitem was rated twice on a 5-point Likert-type scale ranging from 0 = not at all to 4 = extremely, first for their importance and then for their satisfaction. Scores were calculated by multiplying the importance rating by the (reversed) satisfaction rating (scorerange: 0–16). The NAFC-BvC showed satisfactory internal consistency, with a Cronbach’s alpha of > 0.76 [34].
Coping
To measure coping with loss as proposed in the “Model of Meaning Reconstruction” [35, 36], three 5-point Likert-type scale questions were asked: “How much sense would you say have you made of the loss?” (i.e., 1 = no sense, 5 = a good deal of sense), “Despite the loss, have you been able to find any benefit from your experience of the loss?” (i.e., 1 = no benefit, 5 = great benefit), and “Do you feel that you are different, or that your sense of identity has changed, as a result of the loss?” (i.e., 1 = no different, 5 = very different).
Resilience
The 6-item German version of the “Brief Resilience Scale” (BRS-6) was used to examine the individual ability to recover from stress following the loss. Items were rated on a 5-point Likert-type scale ranging from 1 = strongly disagree to 5 = strongly agree. The BRS-6 has sufficient internal consistency, with a Cronbach’s alpha of 0.85 [37, 38].
Grief intensity
The 5-item “Brief Grief Questionnaire” (BGQ-5) was used to assess grief intensity. Items were scored on a 3-point Likert-type scale ranging from 0 = not all to 2 = a lot. This questionnaire exhibits sufficient internal consistency with a Cronbach’s alpha of 0.75 [39].
Self-perceived health
Three self-developed visual rating scales were used to assess self-perceived health, sense of well-being, and self-perceived stress: “How is your current health?” (i.e., 0 = low state of health to 100 = high state of health), “How is your current well-being?” (i.e., 0 = low well-being to 100 = high well-being), “How is your current level of stress?” (i.e., 0 = low stress-level to 100 = high stress-level).
Data analysis
All rating variables were tested for normality using the Kolmogorov-Smirnov test and the Shapiro-Wilk test. Non-parametric statistical methods were used due to non-normal distribution and modest sample sizes to assess differences between the two places of death (two-tailed Mann-Whitney-U-test). To assess relationships between quality of support and bereavement outcomes, Spearman’s correlation was used and effect sizes were interpreted according to Cohen [40] with r = 0.10 indicating a small effect, r = 0.30 indicating a medium effect, and r = 0.50 indicating a large effect. If this relationship was significant, a regression analysis was performed to control for the potential influence of family member age, gender, relationship to deceased (partner / spouse vs. other), and time since death, as described in supplementary file 1. A p-value of < 0.05 was considered statistically significant. The statistical analyses were conducted using IBM SPSS version 28 and Stata/SE version 18 (regression analyses and approximations within scatterplots).
Ethical considerations
The responsible Ethics Committee waived the need for approval (Req-2021-01054). Participants provided their informed consent at the beginning of the questionnaire.
Results
Participant characteristics
Of the 85 family members who received a questionnaire, 35 returned it (11 in electronic and 24 in written form, response rate of 41%). Nearly half of the participants were female (45.7%) (Table 2). Most of the participants were spouses (77.1%) or adult children (17.1%) of the deceased. The participants had lost their close other on average 3.5 months prior to a variety of cancer types. The deceased had been first diagnosed on average five years prior. Two thirds died at home. For most participants, the loss was expected (92.9%), and it predominantly occurred at the place preferred by the deceased (77.1%).
Quality of support
The quality of support that families received was rated with a median score of 50.0 (ICE-FPSQ, score range: 14–70). More specifically, family members rated the received cognitive support with a median score of 20.0 (ICE-FPSQ Cognitive support, score range: 5–25) and the emotional support with a median score of 34.0 (ICE-FPSQ Emotional support, score range: 9–45). Families whose close other had died at home on average had higher results in all three scores than those whose close other had died in an institution. However, these tendencies were not statistically significant (see Table 3).
Bereaved family members rated the quality of end-of-life care with a median score of 4.2 (CANHELP, score range: 1–5), with no statistically significant difference between places of death.
Families reported to have received the following types of bereavement care: acknowledgement of their individual grief experience (78.8%, n = 33), validation of grief as a normal reaction (65.6%, n = 32), information on grief and loss (61.8%, n = 34), and follow-up calls (51.6%, n = 34). Availability of information on coping with grief (57.6%, n = 33) and memorial services (48.3%, n = 29) were considered helpful by about half of the families, information on follow-up visits (33.3%, n = 30) and support groups (34.4%, n = 32) were less often seen as helpful. More than half of the families rated grief support and educational information as sensitive to their cultural and/or spiritual background (73.1%, n = 26). Grief services were perceived to match personal needs (74.1%, n = 27), and were experienced as compassionate (89.7%, n = 29).
On average, families received support from four different professional groups, most often from nurses (97.1, n = 34), followed by medical assistants (80.0%, n = 28), physicians (52.9%, n = 18), and chaplains (44.1%, n = 15). A majority (at least n = 24–25, 89.3%) perceived providers to be highly skilled in listening, showing understanding, and in being trustful, accepting, honest, and helpful.
Needs
Most of the assessed needs were reported as fulfilled (NAFC-BvC; score range: 0–16) in the sense of low relevance or complete satisfaction (Table 3). The least fulfilled needs were “taking part in your usual social / recreational activities” (item 1), “being satisfied with your relationship with family members / friends” (item 10), “taking care of your own health” (item 11), “dealing with your emotional distress” (item 13), and “getting together with family / friends” (item 16). There were no statistically significant differences in scores between places of death.
Bereavement and health outcomes
In terms of coping, bereaved family members reported low levels of meaning-making of the loss (mdn = 1.5, score range:1–5) and of identity change (mdn = 2.0, score range: 1–5). In contrast, families rated their benefit-finding as high (mdn = 4.0, score range: 1–5). No statistically significant differences between places of death were found.
On average, bereaved families showed a median score of 3.5 in their resilience response (BRS, score range: 1–5). There was no significant difference across places of death.
Grief intensity was rated with medium values (mdn = 4.0, score range: 0–10). No statistical significance difference between places of death was found.
Family members indicated their self-perceived health with a median score of 81.0 (score range: 0-100), their sense of well-being with a median score of 66.0 (score range: 0-100), and their self-perceived stress with median score of 40.0 (score range: 0-100) (see Table 3).
Relationships between quality of support and bereavement outcomes
Statistically significant, positive correlations were found between quality of end-of-life care (CANHELP) and resilience (BRS-6) (r = 0.49, p = 0.015, n = 25), and between quality of end-of-life care and benefit-finding (r = 0.47, p = 0.019, n = 25) (see Table 4; Fig. 1 / Supplementary file 2 for scatterplots). These relationships proved to be robust when potential influencers were controlled for using multiple regression analyses (see Table 5). The quality of end-of-life care mean score (CANHELP; range 2.2-5 in the regression sample, n = 25) had a positive relationship with the benefit-finding (range 1–5) that was nearly 1:1 (incremental effect = 0.933, p = 0.025), i.e. an increase in quality of end-of-life care mean score by 1 corresponds to an increase in the benefit-finding by 0.933 on average. The quality of end-of-life care mean score (CANHELP) also had a positive relationship with the resilience mean score (BRS-6; range 2.3-5 in the regression sample, n = 25), whereby an increase in the quality of end-of-life score by 1 implies on average an increase in the resilience score by 0.426 (p = 0.012). Family member age was negatively associated with resilience (incremental effect per year = -0.032, p = 0.004).
Scatterplots of coping (benefit-finding) vs. quality of end-of-life care and resilience (BRS-6) vs. quality of end-of-life care
Note. Added to each scatterplot are a third-degree fractional polynomial approximation (generalized linear model, GLM) and a linear approximation with a 95% confidence interval. Scatterplots of all pairings of quality of support vs. bereavement outcomes are provided in Supplementary file2.
CANHELP = “CANadian Health Care EvaLuation Project– Bereavement version”, score range: 1–5, high score = high satisfaction in EoL care.
BRS-6 = “Brief Resilience Scale”, score range: 1–5; high score = high resilience.
EOL = End-of-Life Care.
Discussion
This cross-sectional study with a small sample of family members recently bereaved due to cancer found that families are mostly satisfied with end-of-life care. About two thirds indicated to receive bereavement support reflective of evidence-based recommendations, such as acknowledgement, validation, and information on dying, grief and available support [41]. Support was received from many different health professionals who had– according to family members high interpersonal skills [42, 43], with nurses and medical office assistants being a core support source for them.
Needs related to family togetherness and relationships, social activities, self-care, and dealing with emotional stress remained most often unmet, reinforcing the need to better support families across settings [9, 18, 44]. Our study shows that families felt less well supported, particularly in relation to their cognitive dimensions (i.e., information, education, reflection opportunities within the family), which has also been previously shown in cancer care setting [18, 45].
We observed some statistically non-significant differences between places of death. Those whose close other had died at home seemed to feel better supported as a family unit than those whose close other had died in hospital or another institutional setting. At the same time, families indicated to have higher unmet needs related to their caregiving role, such as reorganization of roles, getting help from others, dealing with lifestyle changes, or emotional distress, compared to those whose close other died in an institution [11, 46]. In contrast, getting together as a family, navigating the healthcare system, and getting legal paperwork done were more prominent unmet needs among those whose close other died in a hospital. Given the small sample size and low statistical power, these findings need to be interpreted with caution, but suggest that support needs may differ according to place of death. Larger studies with representative samples are needed to verify findings within a cancer care context, potentially extending to other life-limiting illnesses. Overall, a focus on the family as a relational system with support needs related to family management of caregiving, loss, and bereavement, in addition to individual foci on patient or family members, is called for [23, 45, 47,48,49,50].
As previously reported, we also identified an association between high satisfaction with end-of-life support with resilience and benefit-finding, which stresses the importance of quality end-of-life care [3, 7, 8, 51,52,53]. Higher age was associated with lower resilience. Participants indicated moderate grief intensity, high resilience, and benefit-finding. Many family members reported lower levels of meaning-making of the loss, which may be due to the fact that they participated in the study within the first months after their loss [54, 55]. Those caring for their dying family member at home indicated higher stress-levels than those whose close other died in institution, which may be related to the burden of care [4, 8].
Study limitations
Our study is limited by a small, non-representative sample. Partners and those with home care were overrepresented compared to the general population. It is possible that participants represent a more satisfied and resilient group among bereaved family members who are well able to live with their loss in close interactions with their social network [56]. The recruitment of participants in a small geographical area and the limited diversity of the study participants might have introduced a selection bias that may affect the generalizability of the results. Due to low statistical power, lack of statistical significance does not amount to sufficient evidence of the absence of an effect / difference. While we mostly used psychometrically validated instruments, we also relied on three self-developed questions and non-validated German versions. Hence, our findings need to be interpreted with caution. Nevertheless, this cross-sectional observational study offers important insights about the actual quality of support in end-of-life and bereavement care, state of health, and (un)met needs perceived from bereaved family members.
Conclusion
This study reveals high satisfaction with end-of-life support and needs fulfillment based on a small sample of family members recently bereaved to cancer, which is associated with resilience and benefit-finding. The perception of the quality of bereavement care received as a family unit by health professionals in general and during bereavement is more modest, particularly for those whose close other died in an institutional setting such as hospital, suggesting a need for better support structures and care provided by interprofessional teams. While our study focuses on families bereaved due to cancer, our findings may have relevance for other populations, such as families bereaved following a persistent illness. Study findings suggest that improvements should focus on ensuring care that supports the family as a unit and enables togetherness, mutual reflection, meaningful relationships, strong support networks, preparedness for death, family resilience, and benefit-finding. Based on this survey, the quality of and specific needs for bereavement support are less conclusive, partly due to measurement issues, and require further investigation with representative samples to better understand quality of bereavement care [57].
Data availability
Data are available on reasonable request from the authors.
Abbreviations
- BEST CARE:
-
BEreavement SupporT in Cancer CARE
- REDcap:
-
Electronic Data Capture System
- ICE-FPSQ:
-
ICEland Family Perceived Support Questionnaire
- CANHELP:
-
Canadian Health Care Evaluation Project - Bereavement Questionnaire
- EGGS:
-
Evaluation of Grief Support Services
- NAFC-BvC:
-
Needs Assessment of Family Caregivers– Bereaved to Cancer
- BRS-6:
-
Brief Resilience Scale
- BGQ-5:
-
Brief Grief Questionnaire
- IBM SPSS:
-
Statistical Package for the Social Sciences
- Mmdn:
-
median
- r:
-
Correlation coefficient
- p:
-
Type-one error probability
- n:
-
Number of observations
References
Morris SE, Nayak MM, Block SD. Insights from Bereaved Family members about End-of-Life Care and Bereavement. J Palliat Med. 2020;23(8):1030–7.
Morris SE, Moment A, Thomas J. Caring for Bereaved Family members during the COVID-19 pandemic: before and after the death of a patient. J Pain Symptom Manag. 2020;60(2):e70–e4.
Breen LJ, Aoun SM, O’Connor M, Johnson AR, Howting D. Effect of caregiving at end of life on grief, quality of life and general health: a prospective, longitudinal, comparative study. Palliat Med. 2020;34(1):145–54.
Grande G, Rowland C, van den Berg B, Hanratty B. Psychological morbidity and general health among family caregivers during end-of-life cancer care: a retrospective census survey. Palliat Med. 2018;32(10):1605–14.
Zaider TI, Kissane DW, Schofield E, Li Y, Masterson M. Cancer-related communication during sessions of family therapy at the end of life. Psycho-oncology. 2020;29(2):373–80.
Duberstein PR, Maciejewski PK, Epstein RM, Fenton JJ, Chapman B, Norton SA, et al. Effects of the values and options in Cancer Care Communication intervention on personal caregiver experiences of Cancer Care and Bereavement outcomes. J Palliat Med. 2019;22(11):1394–400.
Hamano J, Morita T, Igarashi N, Shima Y, Miyashita M. The association of family functioning and psychological distress in the bereaved families of patients with advanced cancer: a nationwide survey of bereaved family members. Psychooncology. 2020.
Kim Y, Carver CS, Spiegel D, Mitchell HR, Cannady RS. Role of family caregivers’ self-perceived preparedness for the death of the cancer patient in long-term adjustment to bereavement. Psycho-oncology. 2017;26(4):484–92.
Roen I, Stifoss-Hanssen H, Grande G, Brenne AT, Kaasa S, Sand K, et al. Resilience for family carers of advanced cancer patients-how can health care providers contribute? A qualitative interview study with carers. Palliat Med. 2018;32(8):1410–8.
Opsomer S, Lauwerier E, De Lepeleire J, Pype P. Resilience in advanced cancer caregiving. A systematic review and meta-synthesis. Palliat Med. 2022;36(1):44–58.
Laryionava K, Pfeil TA, Dietrich M, Reiter-Theil S, Hiddemann W, Winkler EC. The second patient? Family members of cancer patients and their role in end-of-life decision making. BMC Palliat Care. 2018;17(1):29.
Caruso R, Nanni MG, Riba MB, Sabato S, Grassi L. The burden of psychosocial morbidity related to cancer: patient and family issues. Int Rev Psychiatry. 2017;29(5):389–402.
Hudson P, Hall C, Boughey A, Roulston A. Bereavement support standards and bereavement care pathway for quality palliative care. Palliat Support Care. 2018;16(4):375–87.
Alam S, Hannon B, Zimmermann C. Palliative Care for Family caregivers. J Clin Oncol. 2020;38(9):926–36.
Müller H, Münch U, Bongard S, Hauch H, Sibelius U, Berthold D. [Bereavement care in Germany: Framework for a stepped care model]. Z Evid Fortbild Qual Gesundhwes. 2021;162:40–4.
Keegan O, Murphy I, Benkel I, Limonero JT, Relf M, Guldin MB. Using the Delphi technique to achieve consensus on bereavement care in palliative care in Europe: an EAPC White Paper. Palliat Med. 2021;35(10):1908–22.
National Institute for Clinical Excellence. Guidance on cancer services: improving supportive and palliative care for adults with cancer. The manual. London: NICE: National Institute for Clinical Excellence; 2004.
Hashemi M, Irajpour A, Taleghani F. Caregivers needing care: the unmet needs of the family caregivers of end-of-life cancer patients. Support Care Cancer. 2018;26(3):759–66.
Coyne E, Heynsbergh N, Dieperink KB. Acknowledging cancer as a family disease: a systematic review of family care in the cancer setting. Eur J Oncol Nurs. 2020;49:101841.
Gilliss CL, Pan W, Davis LL. Family involvement in adult chronic Disease Care: reviewing the systematic reviews. J Fam Nurs. 2019;25(1):3–27.
Konradsen H, Brødsgaard A, Østergaard B, Svavarsdóttir E, Dieperink KB, Imhof L, et al. Health practices in Europe towards families of older patients with cancer: a scoping review. Scand J Caring Sci. 2021;35(2):375–89.
Naef R, Peng-Keller S, Rettke H, Rufer M, Petry H. Hospital-based bereavement care provision: a cross-sectional survey with health professionals. Palliat Med. 2020;34(4):547–52.
Vermorgen M, Vandenbogaerde I, Van Audenhove C, Hudson P, Deliens L, Cohen J, et al. Are family carers part of the care team providing end-of-life care? A qualitative interview study on the collaboration between family and professional carers. Palliat Med. 2020;35(1):109–19.
Jack P, James CHC, Leslie F, Ka Man C. Role of patients’ family members in end-of-life communication: an integrative review. BMJ Open. 2023;13(2):e067304.
Chan HY, Lee LH, Chan CW. The perceptions and experiences of nurses and bereaved families towards bereavement care in an oncology unit. Support Care Cancer. 2013;21(6):1551–6.
Hack TF, Carlson L, Butler L, Degner LF, Jakulj F, Pickles T, et al. Facilitating the implementation of empirically valid interventions in psychosocial oncology and supportive care. Support Care Cancer. 2011;19(8):1097–105.
Breen LJ, Moullin JC. The value of implementation science in bridging the evidence gap in bereavement care. Death Stud. 2022;46(3):639–47.
Sousa VD, Rojjanasrirat W. Translation, adaptation and validation of instruments or scales for use in cross-cultural health care research: a clear and user-friendly guideline. J Eval Clin Pract. 2011;17(2):268–74.
Freudiger K, Verweij L, Naef R. Translation and psychometric validation of the German version of the Iceland-Family Perceived Support Questionnaire (ICE-FPSQ): a cross-sectional study, Journal of Family Nursing. accepted for publication.
Konradsen H, Dieperink KB, Lauridsen J, Sorknaes AD, Ostergaard B. Validity and reliability of the Danish version of the ice expressive family functioning and ice family perceived support questionnaires. Scand J Caring Sci. 2018;32(4):1447–57.
Heyland DK, Cook DJ, Rocker GM, Dodek PM, Kutsogiannis DJ, Skrobik Y, et al. Defining priorities for improving end-of-life care in Canada. CMAJ. 2010;182(16):E747–52.
EGSS. [Available from: https://www.nhpco.org/quality-performance-measures/evaluation-grief-support-services-egss.
Gallagher M, Tracey A, Millar R. Ex-clients’ evaluation of bereavement counselling in a voluntary sector agency. Psychol Psychotherapy: Theory Res Pract. 2005;78(1):59–76.
Kim Y, Carver CS, Cannady RS. Bereaved Family Cancer caregivers’ unmet needs: measure development and validation. Ann Behav Med. 2020;54(3):164–75.
Gillies J, Neimeyer RA. Loss, grief, and the search for significance: toward a model of meaning reconstruction in bereavement. J Constructivist Psychol. 2006;19:31–65.
Neimeyer RA, Baldwin SA, Gillies J. Continuing bonds and reconstructing meaning: mitigating complications in bereavement. Death Stud. 2006;30(8):715–38.
Smith BW, Dalen J, Wiggins K, Tooley E, Christopher P, Bernard J. The brief resilience scale: assessing the ability to bounce back. Int J Behav Med. 2008;15(3):194–200.
Chmitorz A, Wenzel M, Stieglitz R-D, Kunzler A, Bagusat C, Helmreich I, et al. Population-based validation of a German version of the brief resilience scale. PLoS ONE. 2018;13(2):e0192761.
Ito M, Nakajima S, Fujisawa D, Miyashita M, Kim Y, Shear MK, et al. Brief measure for screening complicated grief: reliability and discriminant validity. PLoS ONE. 2012;7(2):e31209.
Cohen J. Statistical power analysis. Curr Dir Psychol Sci. 1992;1(3):98–101.
Boven C, Dillen L, Van den Block L, Piers R, Van Den Noortgate N, Van Humbeeck L. In-Hospital bereavement services as an act of Care and a challenge: an integrative review. J Pain Symptom Manage. 2022;63(3):e295–e316.
An AW, Ladwig S, Epstein RM, Prigerson HG, Duberstein PR. The impact of the caregiver-oncologist relationship on caregiver experiences of end-of-life care and bereavement outcomes. Support Care Cancer. 2020;28(9):4219–25.
Bennardi M, Diviani N, Gamondi C, Stüssi G, Saletti P, Cinesi I, et al. Palliative care utilization in oncology and hemato-oncology: a systematic review of cognitive barriers and facilitators from the perspective of healthcare professionals, adult patients, and their families. BMC Palliat Care. 2020;19(1):47.
Alfaro-Díaz C, Svavarsdottir EK, Esandi N, Klinke ME, Canga-Armayor A. Effectiveness of nursing interventions for patients with Cancer and their family members: a systematic review. J Fam Nurs. 2022;28(2):95–114.
Dieperink KB, Coyne E, Creedy DK, Østergaard B. Family functioning and perceived support from nurses during cancer treatment among Danish and Australian patients and their families. J Clin Nurs. 2018;27(1–2):e154–e61.
Woodman C, Baillie J, Sivell S. The preferences and perspectives of family caregivers towards place of care for their relatives at the end-of-life. A systematic review and thematic synthesis of the qualitative evidence. BMJ Supportive & Palliative care. 2016;6(4):418–29.
Guerriere D, Husain A, Zagorski B, Marshall D, Seow H, Brazil K, et al. Predictors of caregiver burden across the home-based palliative care trajectory in Ontario, Canada. Health Soc Care Community. 2016;24(4):428–38.
Ullrich A, Ascherfeld L, Marx G, Bokemeyer C, Bergelt C, Oechsle K. Quality of life, psychological burden, needs, and satisfaction during specialized inpatient palliative care in family caregivers of advanced cancer patients. BMC Palliat Care. 2017;16(1):31.
Hopkinson JB, Brown JC, Okamoto I, Addington-Hall JM. The effectiveness of patient-family carer (couple) intervention for the management of symptoms and other health-related problems in people affected by cancer: a systematic literature search and narrative review. J Pain Symptom Manag. 2012;43(1):111–42.
Duke S, Campling N, May CR, Lund S, Lunt N, Bartlett G, et al. Co-construction of the family-focused support conversation: a participatory learning and action research study to implement support for family members whose relatives are being discharged for end-of-life care at home or in a nursing home. BMC Palliat Care. 2020;19(1):146.
Bachner YG, Guldin MB, Nielsen MK. Mortality communication and post-bereavement depression among Danish family caregivers of terminal cancer patients. Support Care Cancer. 2020.
Aoun SM, Ewing G, Grande G, Toye C, Bear N. The impact of supporting Family caregivers before Bereavement on outcomes after Bereavement: adequacy of end-of-life support and achievement of Preferred Place of Death. J Pain Symptom Manage. 2018;55(2):368–78.
Caserta M, Utz R, Lund D, Supiano K, Donaldson G. Cancer caregivers’ preparedness for loss and bereavement outcomes: do Preloss Caregiver attributes Matter? Omega (Westport). 2019;80(2):224–44.
Wu EX, Collins A, Briggs S, Stajduhar KI, Kalsi A, Hilliard N. Prolonged grief and bereavement supports within a Caregiver Population who Transition through a Palliative Care Program in British Columbia, Canada. Am J Hosp Palliat Care. 2022;39(3):361–9.
Ott CH, Lueger RJ, Kelber ST, Prigerson HG. Spousal bereavement in older adults: common, resilient, and chronic grief with defining characteristics. J Nerv Ment Dis. 2007;195(4):332–41.
Aoun SM, Breen LJ, Howting DA, Rumbold B, McNamara B, Hegney D. Who needs bereavement support? A population based survey of bereavement risk and support need. PLoS ONE. 2015;10(3):e0121101. https://doi.org/10.1371/journal.pone.
Payne S, Hudson P, Grande G. Family carers research: what progress has been made? Palliat Med. 2022:2692163211037855.
Acknowledgements
We would like to thank the clinical staff who assisted with recruitment. We further acknowledge the support of Saskia Oesch and Eva Thuerlimann with data collection.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Author information
Authors and Affiliations
Contributions
MR, QT, and RN derived the methodology, investigated the data, and wrote the original draft of the manuscript. QT implemented the online questionnaire, cleaned, and curated the data. QT and MR conducted the formal analysis and visualization of results. QT conducted the project administration and RN supervised the project. All authors (DB, SPK, AL, QT, MR, RN) contributed to the conceptualisation of the study, validation of the results, review and editing of the manuscript, and have read and approved the final manuscript and take public responsibility for appropriate portions of the content.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This research was submitted to the Ethics Committee of the Canton of Zurich (Req-2021-01054), which waived the need for approval based on Swiss national law. The study was carried out in accordance with relevant guidelines and regulations. The study followed ethical principles and requested participants to declare their informed consent before submitting (online survey) or on the paper-pencil version. Ticking the consent box and the return of the questionnaire was taken as written informed consent.
Consent for publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Thaqi, Q., Riguzzi, M., Blum, D. et al. End-of-life and bereavement support to families in cancer care: a cross-sectional survey with bereaved family members. BMC Health Serv Res 24, 155 (2024). https://doi.org/10.1186/s12913-024-10575-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-024-10575-2