Abstract
Introduction
The United Kingdom (UK) government's healthcare policy in the early 1990s paved the way adoption of the skills mix development and implementation of diagnostic radiographers' X-ray reporting service. Current clinical practice within the public UK healthcare system reflects the same pressures of increased demand in patient imaging and limited capacity of the reporting workforce (radiographers and radiologists) as in the 1990s. This study aimed to identify, define and assess the longitudinal macro, meso, and micro barriers and enablers to the implementation of the diagnostic radiographer musculoskeletal X-ray reporting service in the National Healthcare System (NHS) in England.
Methods
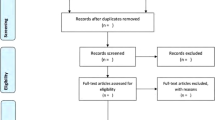
Multiple independent databases were searched, including PubMed, Ovid MEDLINE; Embase; CINAHL, and Google Scholar, as well as journal databases (Scopus, Wiley), healthcare databases (NHS Evidence Database; Cochrane Library) and grey literature databases (OpenGrey, GreyNet International, and the British Library EthOS depository) and recorded in a PRISMA flow chart. A combination of keywords, Boolean logic, truncation, parentheses and wildcards with inclusion/exclusion criteria and a time frame of 1995–2022 was applied. The literature was assessed against Joanna Briggs Institute's critical appraisal checklists. With meta-aggregation to synthesize each paper, and coded using NVivo, with context grouped into macro, meso, and micro-level sources and categorised into subgroups of enablers and barriers.
Results
The wide and diverse range of data (n = 241 papers) identified barriers and enablers of implementation, which were categorised into measures of macro, meso, and micro levels, and thematic categories of context, culture, environment, and leadership.
Conclusion
The literature since 1995 has reframed the debates on implementation of the radiographer reporting role and has been instrumental in shaping clinical practice. There has been clear influence upon both meso (professional body) and macro-level (governmental/health service) policies and guidance, that have shaped change at micro-level NHS Trust organisations. There is evidence of a shift in culturally intrenched legacy perspectives within and between different meso-level professional bodies around skills mix acceptance and role boundaries. This has helped shape capacity building of the reporting workforce. All of which have contributed to conceptual understandings of the skills mix workforce within modern radiology services.
Similar content being viewed by others
Background
The implementation of the diagnostic radiographer musculoskeletal X-ray reporting service within National Healthcare System (NHS) clinical practice in England is now an established advanced clinical practice role. Although, the progression of increasing the radiographer reporting workforce has been slow. As a profession, radiography in England officially originated in 1920 with the formation of the Society of Radiographers (SoR), establishing qualifications and standards of practice, of which reporting of X-ray examinations for diagnosis was commonplace by non-medical radiographers, laypersons [1,2,3] and soldiers in late nineteenth century military campaigns [4] and the first world war [1,2,3, 5,6,7,8,9,10,11,12,13]. Between 1923 and 1925, the General Medical Council (GMC) and the British Medical Association (BMA) pressured a resolution to Articles 27 and 28 of the SoR Articles of Association to legally prevent radiographers from providing reports and diagnoses from X-ray examinations to protect the newly emerging medical profession of radiologists (previously termed medical-radiographers) [1, 5, 12, 13].
Although the discussion on radiographers reporting and diagnosing was raised further in 1929 [1] with the affiliation of the SoR and the British Institute of Radiology (BIR), and in 1975 [14, 15] in response to workforce shortages and reporting workload increases [16]. It wasn't until 1977 that the College of Radiographers (CoR) was formed to oversee education and professional responsibility (forming the joint Society and College of Radiographers (SCoR) professional body). The CoR amended Article 21 of the 'Articles of Association for Radiographers' in 1978 [17] to legally allow diagnostic radiographers to report Ultrasound (US) examinations. This critical and consequential shift in the scope of radiographers' practice was supported further by the Forrest Report [18] recommendations on mammography reporting and the concept of Red Dot [19] practice pressured the CoR 'Code of Professional Conduct' [20] to include "a radiographer may provide a description of images, measurements and numerical data"(1988, p.4).
The NHS drive for patient-focused improvements in England through White Paper policy reform such as 'Health of the Nation' [21], and delays to reporting [22], prompted pilot trials of X-ray reporting by radiographers by Saxton [23], Chapman [24], Loughran [25, 26], and Wilson [27]. The CoR supported in partnership and in combined working groups with the Department of Health (DoH), and the Royal College of Radiologists (RCR), moved to amend of the CoR 'Code of Professional Conduct' [28], to allow radiographers to provide both verbal and written reports on images. The following year, the Audit Commission Report [29] evidenced backlogs in reporting due to the limited radiologist workforce impacting reporting delays and recommended the DoH commission work on training radiographers to interpret and report images. In response, the CoR accredited the first postgraduate reporting programmes in musculoskeletal X-ray for radiographers [30].
Since the development of radiographer musculoskeletal X-ray reporting in 1994, there has been a growing body of research supporting this scope of practice following radiology-based hierarchical efficacy frameworks [31,32,33,34,35,36]. Reviewing the technical efficacy of radiographers' training accuracy in reporting musculoskeletal X-ray images under exam conditions with robust reference standards in controlled conditions (diagnostic accuracy [37]) of observer performance studies [38,39,40]. With progression onto the clinical validity of radiographers' accuracy in reporting musculoskeletal X-ray images in clinical practice environments (diagnostic performance [37]) [26, 39, 41,42,43,44,45,46,47] and when compared against other healthcare professions' performance (diagnostic outcome [37]) [39, 46, 48,49,50,51,52]. Thereafter assessing the clinical utility of radiographer's musculoskeletal X-ray reports on the effect on diagnostic thinking efficacy (discharging of patients [53,54,55,56,57]), the therapeutic efficacy in aiding treatment, management and outcomes [54], and the societal efficacy of cost–benefit [58, 59].
Current NHS clinical practice reflects the same pressures as in the 1990s. Implementation of musculoskeletal X-ray reporting by radiographers by the NHS and stakeholders has been slow to adjust and adapt whilst population growth has accelerated, evidenced in the continued backlog of reporting delays [60]. This study aimed to identify, define and assess the longitudinal macro, meso, and micro barriers and enablers to the implementation of the diagnostic radiographer musculoskeletal X-ray reporting service in the NHS in England.
Methods
The protocol for this systematic review was registered with the International Prospective Register of Systematic Reviews (PROSPERO, registration number: CRD42022384191) and follows a predetermined published protocol in accordance with the reporting guidance provided in the Preferred Reporting Items for Systematic Reviews and Meta-Analysis Protocols (PRISMA-P) statement [61] (Additional files 1, 2).
Study search strategy
The PICOs [62, 63] (Population, Intervention, Comparison, Outcomes study design) framework was used to structure the search strategy. Search terms combined keywords using operators (AND/OR) and Boolean logic to connect words, phrases, and similar concepts (synonyms), with the use of truncation, parentheses, and wildcards (Table 1).
Participants/population characteristics
Literature reporting the implementation of diagnostic radiographers reporting musculoskeletal X-ray examinations in the NHS in England.
Intervention characteristics
The experimental intervention was classed as the musculoskeletal X-ray radiographer X-ray reporting service in the NHS in England. The controlled intervention was the existing consultant radiologist musculoskeletal X-ray reporting service in the NHS in England.
Comparators
There was no comparator assessment of data against the consultant radiologist role or service, other than what was reported in the literature from observer performance studies.
Outcomes
The primary outcome measures were to identify, define and assess against a socio-institutional theoretical model of macro, meso, and micro-levels [64] (Table 2) of enablers and barriers to the implementation of diagnostic radiographers reporting musculoskeletal X-ray examinations in the NHS in England since 1995.
Multiple electronic databases were searched in January 2023, including PubMed, Ovid MEDLINE; Ovid Embase; CINAHL, and Google Scholar, as well as journal databases (ScienceDirect, Wiley), healthcare databases (NHS Knowledge and Library Hub Database; Cochrane Library) and grey literature databases (OpenGrey, GreyNet International, and the British Library EthOS depository).
Inclusion and eligibility criteria
Published peer-review articles that discuss or identify the enablers or barriers to the reporting radiographer service in England including grey literature (such as reports, thesis, research, technical papers, conference papers, government documents, white papers, and evaluations). Defined by the 'Luxembourg Convention' definition [65] as (grey) literature produced on all levels of government, academics, business and industry, in print and electronic formats that discuss or identify the subject topic was reviewed, whilst identifying where bias may be present and the level of empirical evidence found within the grey literature. The exclusion criteria included non-english language papers, studies based on radiographic practice outside of England or private healthcare settings, and diagnostic imaging modalities other than X-ray (Table 3).
Screening
Screening and data extraction was performed with Rayyan [66] software with the assistance of a reference management tool [67]. The inclusion period started from 1995 when the first diagnostic radiographers graduated from an SCoR validated postgraduate clinical reporting programme with a qualification to report musculoskeletal X-rays. Literature from this period will discuss the implementation and facilitation of the role (practically). Although there are many papers pre-1995 that discuss the potential for the role (theoretically) and argue the need for clinical practice development and scope of practice, these papers do not discuss the practical enablers and barriers of the implemented role in practice.
The title, abstract and keywords were evaluated to determine each article for inclusion. If there was uncorrelated information in the title and abstract to determine inclusion, the full paper was retrieved and reviewed to resolve and determine the decision. Studies were excluded based on unrelated titles, abstract and full-text reviews, or duplication with a record documenting the reasoning.
Data extraction and analysis
Data were extracted from the selected studies (Table 4). To address the wide and diverse range of data found, the results were analysed against the Joanna Briggs Institute [68] (JBI) validated critical appraisal checklists (Table 5) for validity, transparency, and rigor. The findings were displayed in a thematic matrix, and a meta-aggregation [69, 70] (different methodologies in the found literature) of the qualitative data into categories (macro, meso, and micro), and synthesize the findings into subthemes. A meta-analysis was not performed as the aim of this paper was not a quantitative summary of observer performance (efficacy) to justify the role, or against a comparator group (improve the power of a study or answer a hypothesis). Additionally, it was expected the various found observer performance quantitative data would contain significant heterogeneity within the different sample sizes, conduct, statistical analysis, and effect sizes.
The meta-aggregation [69, 70] was completed to synthesize each paper, with the findings coded using NVivo [71]. The context was grouped into macro, meso, and micro-level [64] sources and then categorised into subgroups of enablers and barriers. The results were displayed in a PRISMA [72] flow chart, with the findings displayed in a thematic matrix (in historical context ordering) with the subthemes and JBI [68] outcome scores. The search was conducted by the principal author, to minimise selection bias, all selected papers and results were checked by the researchers, two having radiography backgrounds (knowledge of healthcare research and the topic) and two having nursing backgrounds (knowledge of healthcare research and policy). If differences between researchers on the included literature occurred, a consensus final decision approach was agreed.
Results
There were limitations as to any literature search due to some databases (PubMed, Ovid Medline, Ovid Embase) not having the capacity to filter studies based on context/topic such as 'diagnostic radiography' or 'X-ray imaging' or geographic location (England). Database search results focused predominantly on phrases such as 'enablers, drivers, barriers, facilitators, implementation, opposition, and restrictions'. However, database results were dominated by papers that included these keywords but contained irrelevant subjects that did not meet the inclusion criteria. In total, n = 241 papers were included in the results (Fig. 1) and displayed in thematic matric (Table 6). Covering a range of literature from observational studies (n = 16), surveys (n = 25), randomised control trials (n = 5), case studies (n = 8), literature reviews (n = 17), economic analysis (n = 1), clinical audits (n = 4), thesis (n = 3), book chapters (n = 2), governmental reports (n = 10), parliamentary reports (n = 3), NHS reports (n = 35), workforce reports (n = 22), professional body guidance documents (n = 28) reports (n = 7), and statements (n = 8), and expert commentaries (n = 47).
The breakdown of literature was predominantly from the micro level (n = 126; 52.2%), with lesser evidence from meso (n = 63; 26.1%) and macro levels (n = 52; 21.6%). Data analysis and synthesis of the empirical evidence examining the barriers to implementing the reporting radiographer service (Fig. 2) highlighted patterns and trends in publications over four main themes. Workforce shortages [29, 108, 136, 176, 195, 196, 199, 203, 211, 226, 235, 239, 254, 265, 266, 273, 276, 285] (n = 19/28 years) were the leading theme between 1995 and 2022. The barriers included examples of the limited number of consultant radiologists within England [108, 136, 176, 184, 185, 196, 203, 211, 226, 235, 239, 242, 254, 266, 273, 276, 285], due to variables of training numbers, current workforce, and expectations of retirement of staff, which consequentially influenced professional body (meso-level) preferences of outsourcing or regional radiologist networking [108, 173, 181, 184, 195, 196, 199, 203, 211, 213, 226, 235, 239, 242, 254, 265, 266, 276, 285] as opposed to supporting (micro-level) internal skills mix working in departments. Conversely, the limited consultant radiologists workforce affected the availability (micro and meso-level) for mentoring and supporting radiographers in reporting education and training programmes [6, 12, 13, 80, 81, 88, 104, 153, 162, 163, 174, 200, 209, 218, 219, 225, 229, 240, 250, 253, 279, 283, 284]. Reciprocally the limited radiographer workforce also limits the availability of clinical departments (micro-level) to release radiographers to attend educational programmes and support the release of staff for advanced practice roles [200, 209, 218, 219, 250, 253, 283, 284]. Furthermore, there are trends that link workforce limitations with radiologists' opposition (micro and meso-level) to the delegation of tasks [6, 12, 13, 73, 76, 78, 80, 81, 88, 104, 108, 114, 116, 117, 120, 122, 132, 133, 138, 144, 147, 158, 162, 164, 166, 167, 169, 173, 179, 181, 200, 201, 204, 205, 209, 219, 225, 229, 231, 253, 261, 265, 274, 276, 283, 284, 286] (Fig. 2), and to a minor degree, management support (micro-level) for radiographer reporting training [163, 174, 200, 209, 218, 219, 225, 229, 240, 250, 279, 283, 284]. It is noted there was a trend (micro and meso-level) in the literature debating the training standard and curricula [13, 81, 83, 88, 93, 104, 108, 114, 133, 155, 158, 167, 185, 284] between radiologists and reporting radiographers, often centred around medical and non-medical perspectives that were often used to support barriers to adoption of the service delivery.
Exploring the enabler data by theme (Fig. 3) demonstrated twelve themes with promoting advanced practice [6, 13, 26, 38,39,40,41, 45,46,47, 49, 51,52,53,54,55,56,57,58,59, 73,74,75, 77, 79, 80, 83,84,85,86, 88,89,90,91, 94, 96, 99, 101,102,103,104,105,106,107, 110, 111, 113, 115,116,117,118,119,120,121,122,123,124, 127, 128, 130, 134, 138, 139, 141, 142, 144, 146,147,148, 150, 151, 154,155,156,157,158,159, 161,162,163,164,165,166, 170, 171, 174,175,176,177,178, 180,181,182, 185, 187, 188, 190,191,192,193,194,195,196, 198, 200,201,202,203, 206,207,208,209,210, 212, 214, 215, 217,218,219,220,221,222,223,224,225,226,227,228,229,230, 232,233,234,235,236, 238,239,240,241, 243, 245, 247,248,249,250, 253,254,255,256,257,258,259,260,261, 263,264,265, 268, 270, 273,274,275, 277,278,279,280, 282,283,284,285, 287, 288] in radiographer reporting (n = 19/28 years) supported at macro, meso and micro-levels as the leading theme between 1995 and 2022, closely followed by skills mix working (n = 14/28 years) in Fig. 3. There were trends related to specific peaks of literature over the years which link macro-level governmental NHS reform policy in 2000 to remove "traditional and unnecessary demarcations and introduce more flexible working practices" [95,96,97,98, 100, 101], the 2006 push to increase the advanced practice workforce numbers [134, 135], the 2012 policies advocating reporting radiographers to speed up reporting Turnaround Times (TATs) [177, 178], the 2014 five year forward [197], the 2017 Cancer Workforce plan [227, 287, 289], and the 2019 NHS long term plan [237, 244, 246, 247, 252], and the Richards [259] and the Getting it Right First Time [260] reports to improve patient care with increasing the workforce and reporter capacity, supporting other enablers such as promoting advanced practice and skills mix to achieve those targets (Fig. 3). Backed by meso-level professional policy guidance and statements in 1997 [85] of the rationale of the role, 2006 defence of the role [138], with 2007 interprofessional team working agreements [142], 2010 defining terminology and roles [165, 166], 2012 further team working endorsement [182, 183], 2013 formalising roles [188], acceptance of roles [208] and quality standards [272] in reporting and training [277].
Discussion
The main enabler themes (n = 12; Fig. 3) that have influenced and assisted facilitation of the radiographer X-ray reporting role and the barrier themes (n = 4; Fig. 2) that have impacted, restricted and impeded the implementation and its progression can be explored using Kingdon’s [290, 291] Multiple Streams Framework (MSF) to explore the different rational solutions that exist and change overtime to any issue. Kingdon’s [290] uses the theoretical MSF to trace how the different macro, meso, and micro-levels (classed as streams in the MSF [290]) interact and cross-over to influence policy agendas, and how coupling of different streams (macro, meso, and micro-levels) can influence solutions through connecting to build flexibility and a momentum of change (historical, socio, political, organisational, geographical, governance and resource factors).
Context
The historical context of demand of patient imaging referrals [29] against the capacity of the workforce to perform the reporting of X-ray imaging examinations has been at the forefront of the literature [96, 108, 134, 176, 178, 181, 185, 196, 203, 211, 220, 226, 227, 235, 239, 240, 247, 254, 266, 276, 292], and the contemporary [293] perspective shows no signs of abating. This unequilibrium of streams in NHS service delivery has been and still is the primary context to this advanced practice, with patients being at the heart of everything that is done in the NHS [294]. To address these problems, there has been what Kingdon [290] would describe as ‘policy windows’ at the macro-level [245, 247, 248, 278, 292] of short-term funding policy agendas to increase training of reporting radiographers, although sustained annual investment in the long term is required to sustain the reporting radiographer workforce.
There was a notable lack of patient and public involvement (PPI) and contribution in the research and evidence surrounding radiology reporting and the reporting radiographer role. Specifically from active involvement as either advising, co-designing, data collection or, of provision of first-hand experience of the service in case studies and reports. The inclusion of PPI perspectives of reporting delays, workforce shortages, and skills mix working may provide valuable insight to factors that shape the service that have not be identified from the existing literature.
Culture
Assumptions and attitudes without evidence have historically inhibited professional culture (meso-level) from adopting interdisciplinary skills mix roles that overlap traditional boundaries, and instead preference monopolies and turfs [295] (meso-level professional bodies [108, 195, 213, 286]) with less acceptance of collaboration or acceptance of individual qualifications, abilities and competencies that enhance patient outcomes. One such historical argument was the 'gold standard' [296] of reporting, a historical medical term applied by radiologists to describe their performance ability in reporting. Although, based primarily on opinion with little evidence of the rigorous threshold of accuracy beyond training assessment [297], which was seemingly at odds with the threshold of clinical error reported [298,299,300]. Current literature terminology now refer to terms ‘reference standard’ which can be applied to any profession reporting, or ‘ground truth’ collaborated by multi-professional diagnostic tests (blood reports, histology results, surgical findings, etc.). Arguments and debates around reporting accuracy and abilities for medical (radiologist) versus non-medical (radiographer) training have now subsided with interprofessional body consensus and acceptance (Kingdon’s policy window [290]) of radiographer reporting training and competency [142, 182, 272, 277]. Supported by evidence of radiographers reporting all patient groups, ages and referral pathways to fully justify the role [200, 218, 219].
The clinical experience within the literature to support the adoption of reporting radiographers can be reflected in the combination of multiple streams [290] of macro [93, 118], meso [74, 108, 142, 180, 189, 196, 198, 203, 211, 214, 220, 223, 224, 226, 235, 236, 239, 243, 254,255,256, 263, 266, 268, 276, 285], and micro-levels through surveys, case studies, and commentaries [86, 104, 111, 144, 194, 249] providing anecdotal reflection and consensus as to the socio, political, and historical impact and importance of embedding the policy agenda of reporting radiographers in healthcare practice to improve local service delivery.
Environment
To implement sustainable adoption of the role nationally has required substantial research to ascertain its value against the environmental backdrop of annual reduced fiscal investment [301] in NHS healthcare services. The evidence (micro-level) to support the advanced practice education and training [38, 42, 46, 158, 174, 234, 251, 277, 279, 284, 302], and the efficacy and ability of radiographers in the role to perform to high standards has been well conceived (Table 6) and designed [37, 39, 105, 106, 112, 120, 303,304,305,306], assessed [38, 43, 44, 46,47,48, 51, 54, 58, 107, 151, 175], and its associated downstream impact on cost [58, 59, 220] and patient treatment and management [53,54,55,56,57, 191, 201, 207, 307] has been critical to the success of the national roll-out and implementation of the role since 1995.
Of note within the literature there is evidence of variance and influence from the different macro, meso, and micro-levels [290] to the uptake and implementation between geographic regions throughout England [111, 164, 200, 209, 217, 249, 262, 279, 283] potentially due to regional access to training programmes [13, 46, 86, 91, 104, 174, 234, 251, 279], and funding [131, 134, 135, 145, 176, 221, 245, 247, 248, 270, 278, 292]. Additionally, the progression of image acquisition technology and display equipment has helped to progress the role.
The move from daylight processing of X-ray hard-copy film in 1995 to contemporary Computed Radiography (CR) and Digital Radiography (DR) systems with storage and display of images on picture archiving and communications systems (PACS) has revolutionised the image quality for reporting subtle findings. Moreover, this has impacted the manner in which reporting sessions now occur [308], from individual radiology department reporting offices in 1995 using light boxes to display individual examinations to modern twenty-first century reporting computer monitors. The role of reporting has adapted to include both on-site (hospital) reporting stations and off-site remote home reporting stations [309] that increase the ability for staff to participate in out of hours (insourcing) reporting which may be beneficial to reduce backlogs.
Furthermore there is a growing body of literature debating and discussing the trialling Artificial Intelligence (AI) software at different macro, meso, and micro-levels [290] to assist and support in the automation of some tasks in the chain of reporting of X-ray examinations [310]. Although, notable advances and trends in the use of AI have been identified [311, 312], the safe integration of AI is as yet more of a second reader assistance and decision support [313] than replacement of radiologists and reporting radiographers.
Leadership
Receptiveness for change borne by governmental agendas and policymaking [290] (macro-level) [172, 197, 216, 227, 232, 233, 237, 244, 246, 252, 259, 260, 287, 314] to improve healthcare services and delivery for modern society, has, at times, encountered meso-level opposition [76, 93, 108, 213]. But strong leadership at the meso-level [6, 74, 75, 117, 123, 162, 165, 315] have helped shape the succession planning and sustainability of the radiographer reporting role over the years to counter alternatives such as outsourcing reporting backlogs to private companies as a quick fix solution that wastes limited NHS finances that could be spent on increasing the reporting workforce capacity [108, 203, 213, 226, 235, 239, 254]. Future progression of the role requires combination [290] of meso-level professional body leadership to shape direction and inclusion within workforce planning to sustain macro-level governmental healthcare proposals to target healthcare priorities such as faster reporting TATs [233, 260], cancer diagnosis [172, 202, 240, 246, 247, 287] and community diagnostic hubs [233, 259, 260].
It was noted from the literature a limiting factor to monitoring the workforce shortages was a lack of verified and accurate data of how many reporting radiographers were embedded in roles within the NHS in England, as often not all NHS trusts returned data so an incomplete picture of the workforce exists [180, 189, 198, 214, 223, 236, 241, 256, 263] which is hinders decisive future workforce planning.
Additionally, considering the wider perspectives and implications of this skills mix practice. Reporting by radiographers is now established in UK clinical practice, and there is growing evidence of future global opportunities for implementing trained radiographer (often termed a radiologic technologist, or medical radiation technologist internationally) reporting in countries [316] with similar drivers around an increasingly unstable equilibrium of patient demand and reporting workforce supply. Already Australia [147], Canada [317], Denmark and Sweden [318], Ghana [319], Mexico [320], Nepal [321], Norway [322], South Africa [323], and Uganda [324] have made tentative steps in radiographer reporting trials to gauge stakeholder acceptance. However, it is noted the individual macro, meso and micro-level barriers and enablers for each country contain large socioeconomical, cultural, political, professional, and healthcare system differences that require exploring before the skills mix clinical practice of reporting by radiographers is fully adopted across each of these countries.
This study acknowledges some limitations in the methodology, specifically with regards to the search strategy used to identify relevant articles. The use of both broad and specific search terms was an attempt to minimise the risk of missing relevant publications, but it is possible that some pertinent articles may have been excluded or missed. This paper should not be considered an exhaustive list of all the publications in this field; but rather highlights some of the most influential papers to date. Likewise there is an acknowledgment of the limitations of quality in detail, transparency, rigour and evidence between professional and governmental policy, guidance, and statements, and clinical practice level studies and research. It's important to consider these limitations when interpreting the findings of the study.
Conclusion
The literature since 1995 has provided a complex interplay of policy professional and practice streams which have been more or less aligned over the years. The literature has reframed the debates on implementation of the radiographer reporting role and has been instrumental in shaping clinical practice. There has been clear influence upon both meso (professional body organisations) and macro-level (governmental/health service) agendas, policies, and guidance that have shaped change at micro-level NHS Trust organisational levels. There is evidence of a shift in culturally intrenched legacy perspectives within and between different meso-level professional bodies around skills mix acceptance and role boundaries. This has helped shape capacity building of the reporting workforce and radiographer skills development.
The enabling evidence provides clarity and definition of the X-ray radiographer reporting role, and its efficacy, utility, and clinical validity, and is seen as beneficial to the healthcare service, particularly in light of mounting patient demand pressures. The enabling drivers found within the evidence included radiographers reporting all patient groups, ages and referral pathways to evidence the role beyond task dependent activities.
Nevertheless, some challenges and barriers at the meso and micro-level were identified, predominately due to professional body slowness to endorsing team working and implement skills mix roles. Workforce shortages remain a consistent barrier and limit the capacity of reporters (both radiology registrars and diagnostic radiographers). With funding and training numbers the main limiting factors halting future growth of the workforce to provide consistent reporting staff to address the increasing demand of patient referrals, which requires addressing at the macro national level to adequate address service delivery shortfalls.
Future work would do well to interweave the patient perspective of reporting delays, workforce and skills mix, which is currently lacking in the published literature. As well as census surveying of reporting radiographers employed within NHS Trusts in England to guide workforce planning and sustainability of the role to support macro-level governmental healthcare priorities.
Availability of data and materials
All data generated or analysed during this study are included in this published article and its supplementary information files.
Abbreviations
- AI:
-
Artificial Intelligence
- BIR:
-
British Institute of Radiology
- BMA:
-
British Medical Association
- CoR:
-
College of Radiographers
- CR:
-
Computed Radiography
- DoH:
-
Department of Health
- DR:
-
Digital Radiography
- GMC:
-
General Medical Council
- JBI:
-
Joanna Briggs Institute
- NHS:
-
National Healthcare System
- MSF:
-
Multiple Streams Framework
- PACS:
-
Picture archiving and communications systems
- PICO:
-
Population, Intervention, Comparison, Outcomes study design
- PPI:
-
Patient and public involvement
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- PRISMA-P:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses Protocols
- PROSPERO:
-
Prospective Register of Systematic Reviews
- RCR:
-
Royal College of Radiologists
- RCT:
-
Randomised Control Trial
- SCoR:
-
Society and College of Radiographers
- SOR:
-
Society of Radiographers
- TATs:
-
Turnaround Times
- UK:
-
United Kingdom
- US:
-
Ultrasound
References
Moodie I. 50 years of history: The Society of Radiographers. 1st ed. London: The Society of Radiographers; 1969.
Anon. Letters, notes and answers to correspondents. Br Med J. 1903;1:831. https://archive.org/details/sim_british-medical-journal_1903_index/page/16/mode/2up.
Anon. Reviews - Radiography and Diagnosis. Br Med J. 1909;1:339. https://archive.org/details/sim_british-medical-journal_1909_1_index/page/30/mode/2up.
Thomas AMK. The first 50 years of military radiology 1895–1945. Eur J Radiol. 2007;63:214–9.
Larkin GV. Occupational Monopoly in Modern Medicine. London: Tavistock; 1983.
Price RC, Paterson OBEAM. The Society of Radiographers 1920 to 2020. Radiography. 2020;26:185–8.
Holland CT. Radiology in clinical medicine and surgery. Br Med J. 1917;1:285. https://doi.org/10.1136/bmj.1.2931.285.
Hernaman-Johnson F. The place of the radiologist and his kindred in the world of medicine. Arch Radiol Electrotherapy. 1919;24:181–7.
British Medical Association. Lay radiographers. Supplement. Br Med J. 1917;2:707–13. https://archive.org/details/sim_british-medical-journal_1917_2_index_0/page/n1/mode/2up?view=theater.
Lay JHE. Radiographers and electro-therapeutics. Br Med J. 1917;2:706. https://doi.org/10.1136/bmj.2.2969.706.
Kempster C. Lay radiographers and electro-therapeutics. Br Med J. 1917;2:778. https://archive.org/details/sim_british-medical-journal_1917_2_index_0/page/n1/mode/2up?view=theater.
Price P. Radiographers and Reporting – The Early Years’, The Invisible Light. J Radiol Hist Heritage Charitable Trust. 2000;14:7–21. Cited 2023 Jan 12. Available from: http://www.bshr.org.uk/journals/IL14.pdf.
Price R. Developing practice in radiography and diagnostic imaging. [Hertfordshire]: University of Hertfordshire; 2006. Cited 2023 Jan 13. Available from: https://uhra.herts.ac.uk/bitstream/handle/2299/1056/Richard+Price.+PhD+Thesis+submitted+OCT+06.pdf?sequence=1.
Aberdour KR. Must Radiologists do all the Reporting? Br J Radiol. 1976;49:573–573.
McLachlan MSF. Must radiologists do all the reporting. Br J Radiol. 1975;48:773–773.
Emrys-Roberts RM. Must radiologists do all the reporting? Br J Radiol. 1975;48:610–610.
College of Radiographers. Articles of Association for Radiographers. London: College of Radiographers; 1977.
Forrest P. Breast cancer screening: report to the Health Ministers of England, Wales. London: Scotland & Northern Ireland; 1986.
Cheyne N, Field-Boden Q, Wilson I, Hall R. The radiographer and the frontline diagnosis. Radiography. 1987;53:114.
College of Radiographers. Code of Professional Conduct. London: College of Radiographers; 1988.
Department of Health. The health of the Nation – a strategy for health in England. London: UK Government; 1992.
Rose JF, Gallivan S. Plain film reporting in the UK. Clin Radiol. 1991;44:192–4.
Saxton HM. Should radiologists report on every film? Clin Radiol. 1992;45:1–3.
Chapman AH. Should radiographers perform barium enemas? Clin Radiol. 1992;46:69.
Loughran CF. Reporting of fracture radiographs by radiographers: the impact of a training programme. Br J Radiol. 1994;67:945–50.
Loughran CF. Radiographer reporting of accident and emergency radiographs: a review of 5000 cases. Br J Radiol. 1996;69:1640–1640.
Wilson J. Radiographers reporting plain films-a project report. Röntgen Centenary Congress Programme and Abstracts. London: British Journal of Radiology; 1995.
College of Radiographers. Code of Professional Conduct. London: College of Radiographers; 1994.
Audit Commission. Improving Your Image - How to Manage Radiology Services More Effectively. London: Audit Commission for Local Authorities and the National Health Service in England; 1995.
Canterbury Christ Church College. Submission for approval of Canterbury Christ Church College of a Proposal for a Postgraduate Certificate Radiography (Clinical Reporting). Canterbury; 1994.
Fineberg H v. Computerized Cranial Tomography. JAMA. 1977;238:224.
Fineberg H. Evaluation of computed tomography: achievement and challenge. Am J Roentgenol. 1978;131:1–4.
Loop J, Lusted L. American College of Radiology Diagnostic Efficacy Studies. Am J Roentgenol. 1978;131:173–9.
Guyatt GH, Tugwell PX, Feeny DH, Haynes RB, Drummond M. A framework for clinical evaluation of diagnostic technologies. CMAJ. 1986;134:587–94.
Fryback DG, Thornbury JR. The Efficacy of Diagnostic Imaging. Med Decis Making. 1991;11:88–94.
Mackenzie R, Dixon AK. Measuring the effects of imaging: An evaluative framework. Clin Radiol. 1995;50:513–8.
Brealey S, Scally AJ, Thomas NB. Methodological standards in radiographer plain film reading performance studies. Br J Radiol. 2002;75:107–13.
Piper KJ, Paterson AM, Godfrey RC. Accuracy of radiographers’ reports in the interpretation of radiographic examinations of the skeletal system: a review of 6796 cases. Radiography. 2005;11:27–34.
Brealey S. An Evaluation of Radiographer Plain Radiograph Reporting. [York]: University of York; 2003. Cited 2023 Jan 13. Available from: https://etheses.whiterose.ac.uk/14062/1/423497.pdf.
Carter S, Manning D. Performance monitoring during postgraduate radiography training in reporting—a case study. Radiography. 1999;5:71–8.
Robinson PJ, Culpan G, Wiggins M. Interpretation of selected accident and emergency radiographic examinations by radiographers: a review of 11000 cases. Br J Radiol. 1999;72:546–51.
Robinson PJA. Plain film reporting by radiographers—a feasibility study. Br J Radiol. 1996;69:1171–4.
Brealey S, Scally A, Hahn S, Thomas N, Godfrey C, Coomarasamy A. Accuracy of radiographer plain radiograph reporting in clinical practice: a meta-analysis. Clin Radiol. 2005;60:232–41.
Brealey S, Hewitt C, Scally A, Hahn S, Godfrey C, Thomas N. Bivariate meta-analysis of sensitivity and specificity of radiographers’ plain radiograph reporting in clinical practice. Br J Radiol. 2009;82:600–4.
Brealey SD, Scuffham PA. The effect of introducing radiographer reporting on the availability of reports for Accident and Emergency and General Practitioner examinations: a time-series analysis. Br J Radiol. 2005;78:538–42.
Piper K. Interpretation of clinical imaging examinations by radiographers: a programme of research [PhD Thesis]. [Canterbury]: Canterbury Christ Church University; 2014. Cited 2023 Jan 13. Available from: https://researchspace.canterbury.ac.uk/file/ff334464401187d27c426fb0c3ce7aece1c86c20a97acf324ef4c1896b1c4592/777885/13316.pdf.
Hardy M, Spencer N, Snaith B. Radiographer emergency department hot reporting: an assessment of service quality and feasibility. Radiography. 2008;14:301–5.
Brealey S, King DG, Crowe MTI, Crawshaw I, Ford L, Warnock NG, et al. Accident and Emergency and General Practitioner plain radiograph reporting by radiographers and radiologists: a quasi-randomized controlled trial. Br J Radiol. 2003;76:57–61.
Brealey SD, King DG, Hahn S, Crowe M, Williams P, Rutter P, et al. Radiographers and radiologists reporting plain radiograph requests from accident and emergency and general practice. Clin Radiol. 2005;60:710–7.
Coleman L, Piper K. Radiographic interpretation of the appendicular skeleton: a comparison between casualty officers, nurse practitioners and radiographers. Radiography. 2009;15:196–202.
Cain G, Pittock LJ, Piper K, Venumbaka MR, Bodoceanu M. Agreement in the reporting of General Practitioner requested musculoskeletal radiographs: reporting radiographers and consultant radiologists compared with an index radiologist. Radiography. 2022;28:288–95.
Buskov L, Abild A, Christensen A, Holm O, Hansen C, Christensen H. Radiographers and trainee radiologists reporting accident radiographs: a comparative plain film-reading performance study. Clin Radiol. 2013;68:55–8.
Snaith BA. Radiographer-led discharge in accident and emergency – The results of a pilot project. Radiography. 2007;13:13–7.
Hardy M, Snaith B, Scally A. The impact of immediate reporting on interpretive discrepancies and patient referral pathways within the emergency department: a randomised controlled trial. Br J Radiol. 2013;86:20120112–20120112.
Henderson D, Gray WK, Booth L. Assessment of a reporting radiographer-led discharge system for minor injuries: a prospective audit over 2 years. Emerg Med J. 2013;30:298–302.
Snaith B, Hardy M. Emergency department image interpretation accuracy: The influence of immediate reporting by radiology. Int Emerg Nurs. 2014;22:63–8.
Shepherd J, Lourida I, Meertens RM. Radiographer-led discharge for emergency care patients, requiring projection radiography of minor musculoskeletal injuries: a scoping review. BMC Emerg Med. 2022;22:70.
Brealey S, King DG, Hahn S, Godfrey C, Crowe MTI, Bloor K, et al. The costs and effects of introducing selectively trained radiographers to an A&E reporting service: a retrospective controlled before and after study. Br J Radiol. 2005;78:499–505.
Hardy M, Hutton J, Snaith B. Is a radiographer led immediate reporting service for emergency department referrals a cost effective initiative? Radiography. 2013;19:23–7.
NHS England. Tabel-3–2022–23-Modality-Provider-Test-to-Report-2022–12–15. London; 2022. Available from: https://www.england.nhs.uk/statistics/wp-content/uploads/sites/2/2022/12/Table-3-2022-23-Modality-Provider-Test-to-Report-2022-12-15-XLSX-162KB.xlsx.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, The PRISMA, et al. statement: an updated guideline for reporting systematic reviews. BMJ. 2020;2021:n71.
Tacconelli E. Systematic reviews: CRD’s guidance for undertaking reviews in health care. Lancet Infect Dis. 2010;10:226.
Jenson KA. 7 Steps to the perfect PICO search. Ipswich; 2018 Nov. Available from: https://www.ebsco.com/sites/g/files/nabnos191/files/acquiadam-assets/7-Steps-to-the-Perfect-PICO-Search-White-Paper_0.pdf.
Sawatzky R, Kwon J-Y, Barclay R, Chauhan C, Frank L, van den Hout WB, et al. Implications of response shift for micro-, meso-, and macro-level healthcare decision-making using results of patient-reported outcome measures. Qual Life Res. 2021;30:3343–57.
Farace DJ. Perspectives on the Design and Transfer of Scientific and Technical Information. Third International Conference on Grey Literature. Luxembourg: GL Conference Series; 1997. p. 3.
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Syst Rev. 2016;5:210.
Elsevier. Mendeley Reference Manager 2.79.0. Elsevier; 2022. Cited 2023 Jan 16. Available from: https://www.mendeley.com/reference-management/reference-manager.
Joanna Briggs Institute. Critical appraisal tools. Joanna Briggs Institute’s Critical appraisal checklists. 2023. Cited 2023 Jan 16. Available from: https://jbi.global/critical-appraisal-tools.
Florczak KL. Meta-Aggregation: Just What Is It? Nurs Sci Q. 2019;32:11–11.
Lockwood C, Munn Z, Porritt K. Qualitative research synthesis. Int J Evid Based Healthc. 2015;13:179–87.
QSR International. NVivo. Burlington: QSR International; 2018.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev. 2021;10:89.
Brady C. Accountability and the role-development radiographer. Radiography. 1995;1:127–33.
Paterson AM. Role development—towards 2000: a survey of role developments in radiography). London: College of Radiographers; 1995.
College of Radiographers. X-ray examination requests by nurse practitioners and radiographic reporting by radiographers. London: College of Radiographers; 1995.
Royal College of Radiologists. Statement on reporting in Departments of Clinical Radiology. London: The Royal College of Radiologists; 1995.
Field-Boden Q, Piper K. Reporting for radiographers. Synergy. 1996:32–4.
Royal College of Radiologists. Advice on Delegation of Tasks in Departments of Clinical Radiology. London; 1996. Available from: https://www.rcr.ac.uk/system/files/publication/field_publication_files/delegation_of_tasks.pdf.
Field-Boden QC, Piper KJ. Do radiologists really need to report on everything? Radiographer. 1996;43:111–3. Cited 2023 Feb 2. Available from: https://search.informit.org/doi/10.3316/informit.557467901906982.
Williams MP. Skill mix for radiologists and radiographers. Br J Radiol. 1996;69:887–8.
Brindle M. Debate intensifies over non radiologists’ roles. Diagnostic Imaging Europe. 1996;11:43–7.
Kletzenbauer SP. Radiographers’ attitudes to skill mix changes. Radiography. 1996;2:289–300. https://doi.org/10.1016/S1078-8174(96)90018-8. (Cited 2023 Feb 2).
Chapman AH. Changing work patterns. Lancet. 1997;350:581–3. https://doi.org/10.1016/S0140-6736(97)07076-1. (Cited 2023 Feb 2).
Cunningham DA. Special interest group in radiographer reporting. Br J Radiol. 1997;70:873–4.
College of Radiographers. Reporting by Radiographers: a Vision Paper. London: College of Radiographers; 1997.
Eyres R, Henderson I, Paterson A, Prime N, Scally A, Wilson J. The implementation of radiographic reporting- a preliminary survey. Br J Radiol. 1997;12:123.
Department of Health. A First-class Service, Quality in the NHS. London; 1998. Available from: https://www.ucl.ac.uk/~ucsarem/docs1/quality.htm.
Robinson PJA. Pattern recognition and radiographer reporting. Radiography. 1998;4:155–7.
College of Radiographers. Interprofessional Roles and Responsibilities in a Radiology Service. London: College of Radiographers; 1998.
Piper K, Paterson A, Ryan C. The implementation of a radiographic reporting service for trauma examinations of the skeletal system in 4 NHS trusts. Canterbury: NHS Executive South Thames funded research project; 1999.
Prime NJ, Paterson AM, Henderson PI. The development of a curriculum—a case study of six centres providing courses in radiographic reporting. Radiography. 1999;5:63–70.
Fernando R. The radiographer reporting debate—the relationship between radiographer reporting, diagnostic ultrasound and other areas of role extension. Radiography. 1999;5:177–9.
Royal College of Radiologists. Skills mix in clinical radiology. London: The Royal College of Radiologists; 1999.
Price R, Miller L, Payne G. Re-Engineering the soft machine: the impact of developing technology and changing practice on diagnostic radiographer skill requirements. Health Serv Manage Res. 2000;13:27–39. https://doi.org/10.1177/09514848000130010. (Cited 2023 Feb 2).
Beecham L. Blair demands reform of the NHS. BMJ. 2000;320:889.
Department of Health. A Health Service for All Talents – Developing the NHS Workforce. London; 2000. Available from: https://wellcomecollection.org/works/cd5c788j/items?canvas=52.
Department of Health. The NHS Plan: a plan for investment, a plan for reform. London; 2000. Available from: https://webarchive.nationalarchives.gov.uk/+/http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_4002960.
NHS Executive. The NHS Plan A plan for investment, A plan for Reform. London: NHS England; 2000.
Tennant D. New tasks for old: a broader view of radiographer reporting. Radiography. 2000;6:149–50.
Department of Health. The NHS Cancer Plan: a plan for investment, a plan for reform. London; 2000 Sep. Available from: https://webarchive.nationalarchives.gov.uk/+/http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_4009609.
Department of Health. Meeting the challenge: a strategy for the allied health professionals. London: Department of Health; 2000.
Brayley N. The need for radiographer reporting: an accident & emergency department (A&E) perspective. Radiography. 2000;6:227–9.
Nixon S. Professionalism in radiography. Radiography. 2001;7:31–5.
Price RC. Radiographer reporting: origins, demise and revival of plain film reporting. Radiography. 2001;7:105–17.
Brealey S. Measuring the Effects of Image Interpretation: An Evaluative Framework. Clin Radiol. 2001;56:341–7.
Brealey S. Quality assurance in radiographic reporting: a proposed framework. Radiography. 2001;7:263–70.
Brealey S, King D, Warnock N. An assessment of different healthcare professionals’ attitudes towards radiographers’ reporting A&E films. Radiography. 2002;8:27–34.
Royal College of Radiologists. Clinical Radiology: Workforce in Crisis BFCR(02)1. London: The Royal College of Radiologists; 2002.
Price RC, Paterson AM. Consultant practitioners in radiography—a discussion paper. Radiography. 2002;8:97–106.
Hayes S. Opinion: radiographer reporting. Synergy Imaging & Therapy Practice. 2002;16. https://www.proquest.com/openview/0b6c3113d65a0131372c2ffdbcdfdacc/1.pdf?pq-origsite=gscholar&cbl=46803.
Price RC, Miller LR, Mellor F. Longitudinal changes in extended roles in radiography. Radiography. 2002;8:223–34.
Brealey S, Scally AJ, Thomas NB. Presence of bias in radiographer plain film reading performance studies. Radiography. 2002;8:203–10.
Morris P, Grieve A, Thomas AMK, Hughes J. The introduction of digital radiography and its implications for radiographer reporting. Synergy: Imaging & Therapy Practice. 2002:4–6.
Reed W. Radiographer reporting-aspects of the UK experience . The Radiographer: The Official Journal of the Australian Institute of Radiography. 2002;49:147–9. Cited 2023 Feb 2. Available from: https://search.informit.org/doi/10.3316/informit.554728855132027.
NHS Modernisation Agency. Radiology A national framework for service improvement. London: NHS England; 2003.
Rudd PD. The development of radiographer reporting 1965–1999. Radiography. 2003;9:7–12.
College of Radiographers. Role development revisited, the research evidence. London; 2003 Apr. Available from: https://www.sor.org/download-file?f=2bc19bf2-5802-41d3-bac2-1ff1e7f2a779&t=m.
Department of Health. Radiography Skills Mix. London; 2003 Jun. Available from: https://webarchive.nationalarchives.gov.uk/+/http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_4007123.
Alderson CJ, Hogg P. Advanced radiographic practice—the legal aspects. Radiography. 2003;9:305–14.
Brealey S. An Evaluation of Radiographer Plain Radiograph Reporting (PhD Thesis). York: University of York.; 2004.
House of Commons. NHS Improvement Plan: Putting people at the heart of public services. London; 2004. Available from: https://parlipapers.proquest.com/parlipapers/docview/t70.d75.2003-109729/usgLogRstClick!!?accountid=9869.
Department of Health. Extending the practice of allied health professionals in the NHS. London; 2004. Available from: https://njl-admin.nihr.ac.uk/document/download/2027419.
Paterson AM, Price RC, Thomas A, Nuttall L. Reporting by radiographers: a policy and practice guide. Radiography. 2004;10:205–12.
Reeves P. Visions of normality? Early experiences of radiographic reporting. Radiography. 2004;10:213–6.
National Audit Office. Improving Emergency Care in England. HC 1075 Session 2003–04. London; 2004. Available from: https://parlipapers.proquest.com/parlipapers/result/pqpresultpage.previewtitle/4?pgId=b71c1dc4-4388-41a5-9001-69e3928fc889&rsId=1852A209C07.
Department of Health. Improving emergency care in England 16th report Session 2004–05. London; 2005. Available from: https://parlipapers.proquest.com/parlipapers/result/pqpresultpage.previewtitle/6?pgId=0e328b87-5f63-4a77-a71b-67472e91a0a0&rsId=18529D912F3.
Jones H. The Introduction of a radiographer-led A&E hot reporting service. Synergy: Imaging & Therapy Practice. 2005:16–8. https://www.proquest.com/openview/617db849ba5025d873b4d1b87d4ebe82/1.pdf?pq-origsite=gscholar&cbl=46803.
Dimond B. Legal Aspects Arising in the Reporting of X‐Rays. Interpreting Trauma Radiographs. Oxford: Wiley; 2005. p. 19–31.
College of Radiographers. Research and the Radiography Profession: A Strategy and five year plan. London; 2005. Available from: https://www.sor.org/download-file?f=bf0977a6-d7df-4720-a673-b370ae4ef30e&t=m.
Radovanovic H, Armfield N. Radiographer reporting in emergency departments - a literature review. Radiographer. 2005;52:32–5.
Health Committee. Public Expenditure on Health and Personal Social Services 2005. Health Committee Evidence Ev 349. London; 2005. Available from: https://parlipapers.proquest.com/parlipapers/result/pqpresultpage.previewtitle/4?pgId=0e328b87-5f63-4a77-a71b-67472e91a0a0&rsId=18529D912F3.
Royal College of Radiologists. Standards for the Reporting and Interpretation of Imaging Investigations. London; 2006. Available from: https://www.rcr.ac.uk/sites/default/files/bfcr061_standardsforreporting.pdf.
Donovan T, Manning DJ. Successful reporting by non-medical practitioners such as radiographers, will always be task-specific and limited in scope. Radiography. 2006;12:7–12.
Health Committee. Workforce planning. First Report of Session 2005–06 HC 10177–11. Volume II: Written evidence from the Society and Co (Ev 225). London; 2005. Available from: https://parlipapers.proquest.com/parlipapers/result/pqpresultpage.previewtitle/3?pgId=0e328b87-5f63-4a77-a71b-67472e91a0a0&rsId=18529D912F3.
Health Committee. Review body for Nursing and other health professions. 21st Report on Nursing and other health professions 2006. London; 2006. Available from: https://parlipapers.proquest.com/parlipapers/result/pqpresultpage.previewtitle/5?pgId=0e328b87-5f63-4a77-a71b-67472e91a0a0&rsId=18529D912F3.
Government Select Committee on Health. Written Evidence submitted by the Royal College of Radiologists (WP 70). London; 2006. Available from: https://publications.parliament.uk/pa/cm200506/cmselect/cmhealth/1077/1077we63.htm.
Department of Health. Department of Health Briefing Paper: extending the practice of allied health professionals in the NHS. London: Department of Health; 2006.
College of Radiographers. Medical Image Interpretation and Clinical Reporting by Non-Radiologists: The Role of the Radiographer. London; 2006. Available from: https://www-sor-org.webpkgcache.com/doc/-/s/www.sor.org/download-file?f=48941def-a913-4575-b456-0fc318ebfdd9&t=m.
Hardy M, Snaith B. Role extension and role advancement – Is there a difference? A discussion paper. Radiography. 2006;12:327–31.
Woodford AJ. An investigation of the impact/potential impact of a four-tier profession on the practice of radiography – A literature review. Radiography. 2006;12:318–26.
Woolford C, Hewitt P. Am I the lowest paid reporting radiographer in the UK?. Canterbury: Synergy News; 2006. p. 14.
Royal College of Radiologists, Society and College of Radiographers. Team working: A contemporary view of skill mix. London; 2007. Available from: https://www-sor-org.webpkgcache.com/doc/-/s/www.sor.org/getmedia/fa61d5fe-a816-47e6-b988-9fc1e0e8c04f/sor_team_working_within_clinical.pdf_1.
NHS National Patient Safety Agency. Safer Practice Notice (NPSA/2007/16). London; 2007. Available from: https://imaging.heartofengland.nhs.uk/wp-content/uploads/2017/02/npsa-16.pdf.
Price RC, Le Masurier SB. Longitudinal changes in extended roles in radiography: A new perspective. Radiography. 2007;13:18–29.
House of Commons. Health Committee. Workforce planning, 4th Report of Session 2006–07 Vol. I. London; 2007 . Available from: https://parlipapers.proquest.com/parlipapers/result/pqpresultpage.previewtitle/9?pgId=1618daef-e5fb-4a22-9f50-a123ddac8840&rsId=1852A1AA60C.
Snaith B, Hardy M. How to achieve advanced practitioner status: a discussion paper. Radiography. 2007;13:142–6.
Smith TN, Baird M. Radiographers’ role in radiological reporting: a model to support future demand. Med J Aust. 2007;186:629–31.
Humphreys A, Johnson S, Richardson J, Stenhouse E, Watkins M. A systematic review and meta-synthesis: evaluating the effectiveness of nurse, midwife/allied health professional consultants. J Clin Nurs. 2007;16:1792–808.
Royal College of Radiologists. Standards for Self-assessment of Performance. London: The Royal College of Radiologists; 2007.
Blakeley C, Hogg P, Heywood J. Effectiveness of UK radiographer image reading. Radiol Technol. 2008;79:221–6. cited 2023 Jan 12. Available from: http://www.radiologictechnology.org/content/79/3/221.short.
Hardy M, Snaith B, Smith T. Radiographer reporting of trauma images: United Kingdom experience and the implications for evolving international practice. Radiographer. 2008;55:16–9.
Jones HC, Manning D. A survey to assess audit mechanisms practised by skeletal reporting radiographers. Radiography. 2008;14:201–5.
Price R, Edwards H, Heasman F, Herbland A, Le Masurier S, Miller L, et al. The scope of radiographic practice 2008. Hertfordshire; 2009. Available from: https://www-sor-org.webpkgcache.com/doc/-/s/www.sor.org/download-file?f=35c3b1cd-3c1c-4349-8040-fd30c9c66092&t=m.
Cowling C. A global overview of the changing roles of radiographers. Radiography. 2008;14:e28-32.
Hardy M, Legg J, Smith T, Ween B, Williams I, Motto J. The concept of advanced radiographic practice: An international perspective. Radiography. 2008;14:e15–9.
Hogg P, Hogg D, Henwood S. Consultant radiographer leadership – A discussion. Radiography. 2008;14:e39-45.
Buttress SJ, Marangon T. Legal issues of extended practice: Where does the responsibility lie? Radiography. 2008;14:e33–8.
Kelly J, Piper K, Nightingale J. Factors influencing the development and implementation of advanced and consultant radiographer practice – A review of the literature. Radiography. 2008;14:e71–8.
Hardy M, Snaith B. Radiographer interpretation of trauma radiographs: Issues for radiography education providers. Radiography. 2009;15:101–5.
Health and Care Professions Council. Standards of proficiency. Health and Care Professions Council. 2013. Cited 2022 Oct 4. Available from: https://www.hcpc-uk.org/globalassets/resources/standards/standards-of-proficiency---radiographers.pdf?v=637106257920000000.
McGee P. Advanced practice in nursing and the allied health professions. 3rd ed. Chichester: Wiley Blackwell; 2009.
College of Radiographers. Consultant radiographers: Succession planning. London; 2009. Available from: https://www-sor-org.webpkgcache.com/doc/-/s/www.sor.org/getmedia/68518ea8-3031-4f47-a49c-e45af2409a1e/Consultant%20Radiographers_%20Succession%20Planning_1.
Yielder J, Davis M. Where radiographers fear to tread: Resistance and apathy in radiography practice. Radiography. 2009;15:345–50.
Smith S, Reeves P. The extension of the role of the diagnostic radiographer in the UK National Health Service over the period 1995–2009. Eur J Radiography. 2009;1:108–14.
College of Radiographers. Education and Professional development strategy: New Directions. London; 2010. Available from: https://www.sor.org/download-file/?f=4961def8-f45c-49a9-ae18-363ec8c4ccc6&t=m.
College of Radiographers. Medical image interpretation by radiographers. Definitive Guidance. London; 2010. Available from: https://www-sor-org.webpkgcache.com/doc/-/s/www.sor.org/download-file?f=7f0ef7a1-2f56-4c4b-b163-24375105cd0c&t=m.
Paterson A. Medical image interpretation: Interprofessional teams or parallel universes. Imaging Onc. 2010;8–13. Cited 2023 Feb 3. Available from: https://www.sor.org/getmedia/30dc1359-508d-4a56-a79c-693514885184/imaonc10webres.pdf_1.
Department of Health. Equity and excellence: liberating the NHS (Vol. 7881). London; 2010. Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/213823/dh_117794.pdf.
Price R. The past is a foreign country. Radiography. 2010;16:169–70.
Forsyth LJ, Maehle V. Consultant radiographers: Profile of the first generation. Radiography. 2010;16:279–85.
Society of Radiographers. More radiographers to report. Stories. 2010. Cited 2023 Feb 3. Available from: http://www.sor.org/stories/more-radiographers-report.
NHS England. Improving Outcomes: A Strategy for Cancer. London; 2011. Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/213785/dh_123394.pdf.
Royal College of Radiologists. Standards and recommendations for the reporting and interpretation of imaging investigations by non-radiologist medically qualified practitioners and teleradiologists - BFCR(11)2 . London; 2011. Available from: https://www.rcr.ac.uk/sites/default/files/publication/BFCR%2811%292_Reporting.pdf.
Miller L, Price R, Vosper M. Training and development for radiographers’ extended roles: a case of ad hoc implementation. Health Serv Manage Res. 2011;24:60–8.
Hardy M, Snaith B. The impact of radiographer immediate reporting on patient outcomes and service delivery within the emergency department: designing a randomised controlled trial. Radiography. 2011;17:275–9.
Health Committee. Education, training and workforce planning. First Report of Session 2012–13. Volume I: Report, together with formal minutes Volume II: Oral and written evidence. Volume III: Additional written evidence from the Royal College of Radiologists (ETWP37). [Incorporating HC 1648-i-v, Session 2010–12]. London; 2011. Available from: https://parlipapers.proquest.com/parlipapers/docview/t70.d75.2012-001008?accountid=9869.
NHS England National Imaging Clinical Advisory Group. Implementing & Day Working in Imaging Departments. London; 2012. Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/213707/dh_132083.pdf.
Department of Health. Liberating the NHS: developing the healthcare workforce from design to delivery. London; 2012. Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/216421/dh_132087.pdf.
Stephenson P, Hannah A, Jones H, Edwards R, Harrington K, Baker S-A, et al. An evidence based protocol for peer review of radiographer musculoskeletal plain film reporting. Radiography. 2012;18:172–8.
Society of Radiographers. Society of Radiographers Scope of radiographic practice survey 2012. London; 2012. Available from: https://www-sor-org.webpkgcache.com/doc/-/s/www.sor.org/download-file?f=ab5a062d-d616-4106-aa2c-e7476be305e3&t=m.
Royal College of Radiologists. Investing in the clinical radiology workforce: the quality and efficiency case. London; 2012. Available from: https://www.rcr.ac.uk/sites/default/files/RCR_CRWorkforce_June2012.pdf.
Royal College of Radiologists, College of Radiographers. Team working in Clinical Imaging. London; 2012. Available from: https://www.rcr.ac.uk/system/files/publication/field_publication_files/BFCR%2812%299_Team.pdf.
Royal College of Radiologists. Standards for the communication of critical, urgent and unexpected significant radiological findings, Second edition - BFCR(12)11. London ; 2012. Available from: https://www.rcr.ac.uk/sites/default/files/publication/BFCR(12)11_urgent.pdf.
Royal College of Radiologists. Clinical radiology workload: guidance on radiologists’ reporting figures Royal College of Radiologists, London BFCR(12)12. London; 2012. Available from: https://www.rcr.ac.uk/sites/default/files/publication/BFCR%2812%2912_workload_0.pdf.
Centre for Workforce Intelligence. Securing the future workforce supply: clinical radiology stocktake. London; 2012. Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/507372/CfWI_Clinical_Radiology_Stocktake_2012.pdf.
Society and College of Radiographers. Education and Career Framework for the Radiography Workforce. London; 2013. Available from: https://www-sor-org.webpkgcache.com/doc/-/s/www.sor.org/getmedia/fe10fddc-19ae-49f6-80d1-3cd2f1dc7dc9/final_society_of_radiographers_career_framework.pdf_1.
Field LJ, Snaith BA. Developing radiographer roles in the context of advanced and consultant practice. J Med Radiat Sci. 2013;60:11–5.
College of Radiographers. Preliminary clinical evaluation and clinical reporting by radiographers: Policy and practice guidance. London; 2013. Available from: https://www.sor.org/getmedia/520af092-cd10-4ae4-8f2f-3625a91b47c3/Preliminary%20Clinical%20Evaluation%20and%20Clinical%20Reporting%20by%20Radiographers_%20Policy%20and%20Practice%20Guidanc_1.
Society of Radiographers. Scope of radiographic practice survey 2013. London; 2013. Available from: https://www-sor-org.webpkgcache.com/doc/-/s/www.sor.org/getmedia/1a65fad8-f227-46c7-b996-47734d241684/The%20Scope%20of%20Practice%202013_3.
Leishman L. Can skeletal image reporting be taught online: Perspectives of experienced reporting radiographers? Radiography. 2013;19:104–12.
Snaith B, Hardy M. The perceived impact of an emergency department immediate reporting service: an exploratory survey. Radiography. 2013;19:92–6.
Woznitza N. Radiographer reporting. J Med Radiat Sci. 2014;61:66–8.
Cox WAS, Price R. What general practitioners require of diagnostic imaging departments: a case study. Radiography. 2014;20:131–6.
Woznitza N, Piper K, Rowe S, West C. Optimizing patient care in radiology through team-working: a case study from the United Kingdom. Radiography. 2014;20:258–63.
Royal College of Radiologists. Radiology in the UK – the case for a new service model. London; 2014. Available from: https://www.rcr.ac.uk/sites/default/files/Radiology_networks_position_paper_published_sept2014_0.pdf.
Royal College of Radiologists. Clinical Radiology UK Workforce Census Report 2012. BFCR(14)14. London: The Royal College of Radiologists; 2014.
NHS England. Five Year Forward View. London; 2014. Available from: https://www.england.nhs.uk/wp-content/uploads/2014/10/5yfv-web.pdf.
Society of Radiographers. Diagnostic radiography UK workforce report 2014. London; 2014. Available from: https://www.sor.org/download-file/?f=cb314bae-e8ae-4a24-9151-cf6aeb1277ca&t=m.
Royal College of Radiologists. How the next Government can improve diagnosis and outcomes for patients RCR(15)2. London; 2015. Available from: https://www.rcr.ac.uk/sites/default/files/RCR(15)2_CR_govtbrief.pdf.
Snaith B, Hardy M, Lewis EF. Radiographer reporting in the UK: A longitudinal analysis. Radiography. 2015;21:119–23.
Barter E. Radiographer-Led discharge. Imag Ther Pract. 2015;5–8. Cited 2023 Feb 3. Available from: https://www.proquest.com/docview/1698044696.
Independent Cancer Taskforce. Achieving world-class cancer outcomes: a strategy for England 2015–2020. London; 2015. Available from: https://www.cancerresearchuk.org/sites/default/files/achieving_world-class_cancer_outcomes_-_a_strategy_for_england_2015-2020.pdf.
Royal College of Radiologists. Clinical Radiology UK Workforce census 2014 report. BFCR(15)3. London; 2015. Available from: https://www.rcr.ac.uk/system/files/publication/field_publication_files/bfcr153_census_20082015.pdf.
Royal College of Radiologists. Standards for providing a seven-day acute care diagnostic radiology service. BFCR(15)14. London; 2015. Available from: https://www.rcr.ac.uk/system/files/publication/field_publication_files/bfcr1514_seven-day_acute.pdf.
Faculty of Clinical Radiology. Diagnostic radiology – our patients are still waiting. London; 2016. Available from: www.rcr.ac.uk/sites/default/backlog_survey_feb_2016.pdf.
Booth L, Henwood S, Miller P. Reflections on the role of consultant radiographers in the UK: What is a consultant radiographer? Radiography. 2016;22:38–43.
Hardy M, Johnson L, Sharples R, Boynes S, Irving D. Does radiography advanced practice improve patient outcomes and health service quality? A systematic review. Br J Radiol. 2016;89:20151066.
Royal College of Radiologists. Standards for the reporting of imaging investigations by non-radiologist medically qualified practitioners. London; 2016. Available from: https://www.rcr.ac.uk/system/files/publication/field_publication_files/bfcr181_standards_for_interpretation_reporting.pdf.
Milner RC, Culpan G, Snaith B. Radiographer reporting in the UK: is the current scope of practice limiting plain-film reporting capacity? Br J Radiol. 2016;89:20160228.
Nightingale J, McNulty J. Advanced practice: maximising the potential of the modern radiographer workforce. Health Management. 2016;16:230–3. Cited 2023 Feb 3. Available from: http://shura.shu.ac.uk/22045/1/NightingaleAdvancedPracticeMaximiseing(VoR).pdf.
Royal College of Radiologists. Clinical Radiology UK Workforce census 2015 report. BFCR(16)6. London; 2016. Available from: https://www.rcr.ac.uk/system/files/publication/field_publication_files/bfcr166_cr_census.pdf.
Snaith B, Milner RC, Harris MA. Beyond image interpretation: Capturing the impact of radiographer advanced practice through activity diaries. Radiography. 2016;22:e233–8.
Royal College of Radiologists. Who shares wins: efficient, collaborative radiology solutions. London; 2016. Available from: https://www.rcr.ac.uk/sites/default/files/who_shares_wins_infographic.pdf.
Society of Radiographers. Diagnostic Radiographers UK workforce report 2016. London; 2016. Available from: https://www.sor.org/download-file/?f=49fb65a3-fa4a-4a74-bdad-d90945e19366&t=m.
NHS Benchmarking Network. National Report Benchmarking NHS Radiology 2016. London: NHS England; 2016.
NHS England. Allied Health Professionals into Action. London; 2017. Available from: https://www.england.nhs.uk/wp-content/uploads/2017/01/ahp-action-transform-hlth.pdf.
Milner RC, Snaith B. Are reporting radiographers fulfilling the role of advanced practitioner? Radiography. 2017;23:48–54.
Lockwood P. Exploring variation and trends in adherence to national occupational standards for reporting radiographers. J Soc Sci Allied Health Prof. 2017;1:20–7. Cited 2023 Feb 3. Available from: https://openresearch.lsbu.ac.uk/download/16544134255f2c319f7ac89f5a00eb2b77cbac69f70866a87a7041d55f8613a2/140141/paper%20as%20published.pdf .
Benwell MJ, Fowler P. The reporting radiographer’s role: a contemporary insight. J Soc Sci Allied Health Prof. 2017;1:6–11. Cited 2023 Feb 3. Available from: https://openresearch.lsbu.ac.uk/item/87026.
British Institute of Radiology, The Society of Radiographers, InHeath. Workforce innovation delivers “prompt, efficient, cost effective and safe clinical imaging services. London; 2017. Available from: https://www.bir.org.uk/media/352283/workforce_innovation_a4.pdf.
Health Education England. National review of radiology academies. London; 2017. Available from: https://www.hee.nhs.uk/sites/default/files/documents/Review%20of%20radiology%20academies%20-%20summary%20FINAL.pdf.
Society of Radiographers. Radiographer reporting: Statement from UK Council of the Society of Radiographers. London; 2017. Available from: https://www.sor.org/news/ezine/radiographer-reporting-statement-from-uk-counc-(2).
Society of Radiographers. Diagnostic Radiography: A Survey of the Scope of Radiographic Practice 2015. London; 2017. Available from: https://www-sor-org.webpkgcache.com/doc/-/s/www.sor.org/getmedia/f672e0df-8bfb-457f-b8e9-2709674519d5/2017-05-17_diagnostic_scope_of_practice_2015_-_final_2.pdf.
Society of Radiographers. Radiographer reporting statement. Canterbury: Synergy News; 2017. p. 1–3.
Kerrney S. There are valid objections, but they should not preclude radiographer reporting. Synergy News . 2017;11–11.
Royal College of Radiologists. Clinical Radiology UK Workforce census 2016 report. BFCR(17)6. London; 2017. Available from: https://www.rcr.ac.uk/system/files/publication/field_publication_files/cr_workforce_census_2016_report_0.pdf.
NHS England. Cancer Workforce Plan Phase 1: Delivering the cancer strategy to 2021. London; 2017. Available from: https://www.hee.nhs.uk/sites/default/files/documents/Cancer%20Workforce%20Plan%20phase%201%20-%20Delivering%20the%20cancer%20strategy%20to%202021.pdf.
NHS Benchmarking. NHS Benchmarking. Projects. Radiology 2017. London; 2017. Available from: https://www.radiograf.no/files/archive/radiograf/pdf/H%C3%B8ringssvar/NHSBN_Radiology_National_Report_2017_-_FINAL.pdf.
Thom SE. Does advanced practice in radiography benefit the healthcare system? A literature review. Radiography. 2018;24:84–9.
Society of Radiographers. Radiographer reporting: For the many, not just the few? Synergy News. Canterbury: Synergy News; 2018. p. 1–3.
Royal College of Radiologists. Standards for interpretation and reporting of imaging investigations. BFCR(18)1. London; 2018. Available from: https://www.rcr.ac.uk/system/files/publication/field_publication_files/bfcr181_standards_for_interpretation_reporting.pdf.
NHS Improvement and NHS England. Allied health professions supporting patient flow: a quick guide. London; 2018. Available from: https://allcatsrgrey.org.uk/wp/download/governance/clinical_governance_2/AHPs_supporting_patient_flow_FINAL_.pdf.
Care Quality Commission. Radiology review. A national review of radiology reporting within the NHS England. London; 2018. Available from: https://www.cqc.org.uk/sites/default/files/20180718-radiology-reporting-review-report-final-for-web.pdf.
Harcus J, Snaith B. The Clinical Academy for Radiographer Reporting (CARR): a new model for training advanced clinical practitioners. J Med Imaging Radiat Sci. 2018;49:S12.
Royal College of Radiologists. Clinical Radiology UK Workforce census 2017 report. London; 2018. Available from: https://www.rcr.ac.uk/publication/clinical-radiologyuk-workforce-census-2017-report.
Society of Radiographers. Diagnostic Radiographers UK workforce report 2017. London; 2018. Available from: https://www.sor.org/download-file/?f=f162bbcf-e734-469c-a9a2-99c725c72455&t=m.
NHS England. NHS long term plan 1.2. London; 2019. Available from: https://www.longtermplan.nhs.uk/wp-content/uploads/2019/08/nhs-long-term-plan-version-1.2.pdf.
Snaith B, Clarke R, Coates A, Field L, McGuinness A, Yunis S. How do consultant radiographers contribute to imaging service delivery and leadership? Br J Healthc Manag. 2019;25:41–7.
Royal College of Radiologists. Clinical Radiology UK Workforce census 2018 report. London; 2019. Available from: https://www.rcr.ac.uk/publication/clinical-radiologyuk-workforce-census-report-2018.
Culpan G, Culpan A-M, Docherty P, Denton E. Radiographer reporting: a literature review to support cancer workforce planning in England. Radiography. 2019;25:155–63.
Society of Radiographers. Diagnostic Radiographers workforce UK census 2018. London; 2019. Available from: https://www.sor.org/getmedia/436353ec-38ca-49c6-907dd7a1ca18393a/diagnostic_workforce_census_2019.pdf.
Royal College of Radiologists. CQC radiology review: where are we now?. London; 2019. Available from: https://www.sor.org/getmedia/0ce575a5-a886-4194-a14d-e8221b702275/rcr-cqc-radiology-review-where-are-we-now_3.pdf.
Society of Radiographers. More reporting radiographers needed to reduce delays . Synergy. 2019. Cited 2023 Feb 3. Available from: https://www.sor.org/news/ezine/more-reporting-radiographers-needed-to-reduce-dela.
NHS England. Interim NHS People Plan. London; 2019. Available from: https://www.longtermplan.nhs.uk/wp-content/uploads/2019/05/Interim-NHS-People-Plan_June2019.pdf.
Health Education England. Annual Report and Accounts 2018–19. London; 2019. Available from: https://www.hee.nhs.uk/sites/default/files/documents/hee-annual-report-2018-to-2019-web-accessible.pdf.
NHS England. Cancer Programme: Faster Diagnosis Framework. London; 2019. Available from: https://www.england.nhs.uk/wp-content/uploads/2019/07/B1332-NHS-Cancer-Programme-Faster-Diagnosis-Framework-v5.pdf.
Health Education England. Progress Update on Phase 1 of the Cancer Workforce Plan. London; 2019. Available from: https://www.hee.nhs.uk/sites/default/files/documents/Cancer%20Workforce%20Plan%20phase%201%20progress%20update%20FINAL.pdf.
Health Education England. Health Education England Business Plan 2019/20. London; 2019. Available from: www.hee.nhs.uk/sites/default/files/documents/HEE%20Business%20Plan%202019-20%20FINAL.pdf.
Stevens BJ. A survey assessment of reporting radiographers’ scope of practice in the West Midlands region of the United Kingdom. Radiography. 2019;25:214–9.
Cuthbertson LM. The journey to advanced practice and skeletal trauma reporting; an Interpretative Phenomenological Analysis of preparation for the role. Radiography. 2019;25:S40–7.
Harcus JW, Snaith B. Expanding training capacity for radiographer reporting using simulation: Evaluation of a pilot academy project. Radiography. 2019;25:288–93.
NHS Improvement. Transforming imaging services in England. A National strategy for imaging networks. London; 2019. Available from: https://webarchive.nationalarchives.gov.uk/20210401201200/https:/improvement.nhs.uk/documents/6119/Transforming_imaging_services.pdf.
Cuthbertson LM. Skeletal trauma reporting; perceptions and experiences of radiographer practitioners exposed to the reporting role. Radiography. 2020;26:35–41.
Royal College of Radiologists. Clinical radiology UK workforce census 2019 report. London; 2020. Available from: https://www.rcr.ac.uk/system/files/publication/field_publication_files/clinical-radiology-uk-workforce-census-2019-report.pdf.
Society of Radiographers. Designing a radiographer reporting service to cope with pressures of Covid-19. London; 2020. Available from: https://www.sor.org/news/reporting/designing-a-radiographer-reporting-service-to-cope.
Society of Radiographers. Diagnostic radiography UK workforce report 2019. London; 2020. Available from: https://www.sor.org/download-file/?f=365ef68a-d681-43bb-9e7e-46ca29a88df2&t=m.
NHS England. We Are The NHS: People Plan 2020/21-action for us all. London; 2020. Available from: https://www.england.nhs.uk/wp-content/uploads/2020/07/We-Are-The-NHS-Action-For-All-Of-Us-FINAL-March-21.pdf.
Woznitza N, Steele R, Groombridge H, Compton E, Gower S, Hussain A, et al. Clinical reporting of radiographs by radiographers: Policy and practice guidance for regional imaging networks. Radiography. 2021;27:645–9.
NHS England. M. Richards Diagnostics: recovery and renewal. Independent Review of Diagnostic Services for NHS England. London; 2020. Available from: https://www.england.nhs.uk/wp-content/uploads/2020/10/BM2025Pu-item-5-diagnostics-recovery-and-renewal.pdf.
Royal National Orthopaedic Hospital NHS Trust, NHS England, NHS Improvement. Getting it right first time: Radiology, GIRFT Programme National Speciality Report. London; 2020. Available from: https://www.gettingitrightfirsttime.co.uk/wp-content/uploads/2020/11/GIRFT-radiology-report.pdf.
Milner RC, Barlow N. General Practitioner satisfaction with a radiographer-led general radiography reporting service at a district general hospital in the UK. Radiography. 2021;27:81–9.
Woznitza N, Steele R, Hussain A, Gower S, Groombridge H, Togher D, et al. Reporting radiographer peer review systems: a cross-sectional survey of London NHS Trusts. Radiography. 2021;27:173–7.
Society of Radiographers. Diagnostic radiography UK workforce report 2020. London; 2021. Available from: https://www.sor.org/download-file?f=c83fbeca-5d8a-4bdc-98a7-526e49da08bb&t=m.
Society of Radiographers. Radiographer reporting grows as NHS struggles with radiology staff shortages. London; 2021. Available from: https://www.sor.org/news/government-nhs/radiographer-reporting-grows-as-nhs-struggles-with.
Royal College of Radiologists ., Society of Radiographers. Institute of Physics & Engineering in Medicine. Diagnostic Imaging Network Implementation Guide. London; 2021. Available from: https://www.england.nhs.uk/wp-content/uploads/2021/04/B0030-Implementation-guide.pdf.
Royal College of Radiologists. Clinical radiology – UK workforce census 2020 report. London; 2021. Available from: https://www.rcr.ac.uk/system/files/publication/field_publication_files/clinical-radiology-uk-workforce-census-2020-report.pdf.
Heales CJ, Mills K, Ladd E. Radiographer advanced and consultant practice and community diagnostic hubs – a vision for the future. Radiography. 2021;27:S28-33.
Society of Radiographers. Survey of Trainee Consultant and Consultant Radiographers 2020. London; 2021. Available from: https://www.sor.org/download-file/?f=865919be-e136-4c21-b062-7cc6a6a4dd64&t=m.
Parliamentary and Health Service Ombudsman. Unlocking Solutions in Imaging: Working together to learn from failings in the NHS. London; 2021. Available from: https://www.ombudsman.org.uk/sites/default/files/Unlocking_Solutions_in_Imaging_working_together_to_learn_from_failings_in_the_NHS%20-%20EMBARGO.pdf.
Health Education England. Annual Report and Accounts 2020–21. London; 2021. Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1003592/Health_Education_England_ARA_2020-21_Web_Accessible.pdf.
Akpan E, Kitundu J, Ekpo E. Public health radiography: a scoping review of benefits, and growth opportunities for radiographers. J Med Imaging Radiat Sci. 2021;52:615–25.
College of Radiographers, Royal College of Radiologists. Quality standards for Imaging. QSI 2021. London; 2021. Available from: https://www.rcr.ac.uk/sites/default/files/quality-standard-for-imaging-qsi.pdf.
Government Select Committee on Health. Written Evidence submitted by the Royal College of Radiologists (RTR0133). London; 2022. Available from: https://committees.parliament.uk/writtenevidence/43057/pdf/.
Wood K. How is the reporting radiographer role portrayed in published studies? A scoping review. Radiography. 2022;28:215–21.
NHS England. Diagnostic imaging network workforce guidance. London; 2022. Available from: https://www.england.nhs.uk/wp-content/uploads/2022/04/B0418_Diagnostic-imaging-network-workforce-guidance_April-2022.pdf.
Royal College of Radiologists. Clinical radiology – UK workforce census 2021 report. London; 2022. Available from: https://www.rcr.ac.uk/sites/default/files/clinical_radiology_census_report_2021.pdf.
Royal College of Radiology, College of Radiographers, British Society of Skeletal Radiologists. Standards for the education and training of reporting practitioners in musculoskeletal plain radiographs. London; 2022. Available from: https://www.rcr.ac.uk/system/files/publication/field_publication_files/standards_for_the_education_and_training_of_reporting_practitioners_in_msk_plain_radiographs_-_printed3.pdf.
Health Education England. HEE Business Plan 2022/23. London; 2022. Available from: https://www.hee.nhs.uk/sites/default/files/HEE%20Business%20Plan%202022-23.pdf.
Sevens T, McGivern T. Reporting radiographer academy training model; an evaluation of the impact for trainees and clinical service. Radiography. 2022;28:798–803.
College of Radiographers. Diagnostic Radiography Workforce Uk Census 2021 Report. London; 2022. Available from: https://www.sor.org/download-file/?f=9dbc9e49-4b03-4e6c-83cf-bade28aef1bb&t=a.
The Kings Fund. Why do diagnostics matter? Maximising the potential of diagnostics services. London; 2022. Available from: https://www.kingsfund.org.uk/sites/default/files/2022-10/Why%20do%20diagnostics%20matter%20online%20version_0.pdf.
Academy of Medical Royal Colleges. Recommendations on alerts and notification of imaging reports. London; 2022. Available from: https://www.rcr.ac.uk/system/files/publication/field_publication_files/alerts_notification_imaging_reports_recommendations_1022_0.pdf.
Murphy L, Nightingale J, Calder P. Difficulties associated with Reporting Radiographer working practices – A narrative evidence synthesis. Radiography. 2022;28:1101–9.
Murphy L, Nightingale J, Calder P. Difficulties associated with access to training and clinical support for Reporting Radiographers – A narrative evidence synthesis. Radiography. 2022;28:1071–9.
Royal College of Radiologists. RCR Clinical radiology census report 2021. London: The Royal College of Radiologists; 2022.
Board of the Faculty of Clinical Radiology. Medical image interpretation by radiographers. Guidance for radiologists and healthcare providers’. London: The Royal College of Radiologists; 2010.
NHS England. Cancer Workforce plan - phase 1: delivering the cancer strategy to 2021. London; 2017. Available from: https://www.hee.nhs.uk/sites/default/files/documents/Cancer%20Workforce%20Plan%20phase%201%20-%20Delivering%20the%20cancer%20strategy%20to%202021.pdf.
Woznitza N. Radiographer reporting. J Med Radiat Sci. 2014;61(2):66.
NHS England. Next steps on the NHS Five Year Forward View. 2017.
Kingdon J, Stano E. Agendas, alternatives, and public policies. Boston: Little, Brown; 1984.
Hoefer R. The multiple streams framework: understanding and applying the problems, policies, and politics approach. J Policy Pract Res. 2022;3:1–5.
Health Education England. 2019 Progress update Update on Phase 1 of the Cancer Workforce Plan. London; 2019. Available from: https://www.hee.nhs.uk/sites/default/files/documents/Cancer%20Workforce%20Plan%20phase%201%20progress%20update%20FINAL.pdf.
NHS England. Diagnostic Imaging Dataset Statistical Release. London: NHS England; 2022.
Department of Health and Social Care. NHS Constitution. London: Department of Health; 2012.
Rao VM, Levin DC. Turf wars in radiology: training in diagnostic imaging: how much is enough? J Am Coll Radiol. 2005;2:1016–8.
Jones DS, Podolsky SH. The history and fate of the gold standard. Lancet. 2015;385:1502–3.
Booth TC, de Martins PRM, McKnight L, Courtney K, Malliwal R. The Fellowship of the Royal College of Radiologists (FRCR) examination: a review of the evidence. Clin Radiol. 2018;73:992.
Berlin L. Radiologic errors, past, present and future. Diagnosis. 2014;1:79–84.
Brady AP. Error and discrepancy in radiology: inevitable or avoidable? Insights Imag. 2017;8:171–82.
Fitzgerald R. Error in Radiology. Clin Radiol. 2001;56:938–46.
Holmes J, Anandaciva S. The comprehensive spending review - what more for health and care spending?. London; 2021. Available from: https://www.kingsfund.org.uk/publications/comprehensive-spending-review-health-and-care-spending.
Piper KJ, Paterson AM, Godfrey RC. Accuracy of radiographers’ reports in the interpretation of radiographic examinations of the skeletal system: a review of 6796 cases. Radiography. 2005;11(1):27–34.
Brealey S. Measuring the effects of image interpretation: An evaluative framework. Clin Radiol. 2001;56(5):341–7.
Brealey S, Scally AJ. Methodological approaches to evaluating the practice of radiographers’ interpretation of images: A review. Radiography. 2008;14:e46–e54.
Scally AJ, Brealey S. Confidence intervals and sample size calculations for studies of film-reading performance. Clin Radiol. 2003;58(3):238–46.
Brealey S, Scally AJ. Bias in plain film reading performance studies. British Journal of Radiology. 2001;74(880):307–16.
Lumsden L, Cosson P. Attitudes of radiographers to radiographer-led discharge: A survey. Radiography. 2015;21(1):61–7.
Mackinnon AD, Billington RA, Adam EJ, Dundas DD, Patel U. Picture archiving and communication systems lead to sustained improvements in reporting times and productivity: results of a 5-year audit. Clin Radiol. 2008;63:796–804.
Crotty M. Imaging informatics: Reporting radiographers and working from home. Synergy. 2021;1–2. Cited 2023 Mar 19. Available from: https://www.sor.org/news/information-management-technology/imaging-informatics-reporting-radiographers-and-wo.
Hughes H, O’Reilly M, McVeigh N, Ryan R. The top 100 most cited articles on artificial intelligence in radiology: a bibliometric analysis. Clin Radiol. 2023;78:99–106.
Sreedharan S, Mian M, Robertson RA, Yang N. The top 100 most cited articles in medical artificial intelligence: a bibliometric analysis. J Med Artif Intell. 2020;3:3–3.
Hosny A, Parmar C, Quackenbush J, Schwartz LH, Aerts HJWL. Artificial intelligence in radiology. Nat Rev Cancer. 2018;18:500–10.
Rainey C, O’Regan T, Matthew J, Skelton E, Woznitza N, Chu K-Y, et al. UK reporting radiographers’ perceptions of AI in radiographic image interpretation – Current perspectives and future developments. Radiography. 2022;28:881–8.
England. Building the nhS of the five Year forward view. 2015;
Paterson A. Consultant radiographers - The point of no return? Radiography. 2009;15:2–5.
Pedersen MRV, Jensen J, Senior C, Gale N, Heales CJ, Woznitza N. Reporting radiographers in Europe survey: An overview of the role within the European Federation of Radiographer Society (EFRS) member countries. Radiography. 2023;29:1100–7.
Talla M, Nakum B, Abdul-Jalil S. Potential Implications of Advanced Practice Radiography on the Canadian Healthcare System from Technologists Perspectives. MICH. 2019;1:1–6. Cited 2023 Sep 20. Available from: https://journals.publicknowledgeproject.org/psychegeloof/index.php/michener-student/article/view/186/111.
Andersson M, Moreno Ourcilleon R. Danish and Swedish Radiographers’ Attitudes towards their Profession and Reporting Radiography-A Qualitative Study. [Lund]: Lund University; 2016. Cited 2023 Sep 20. Available from: https://lup.lub.lu.se/student-papers/search/publication/8778175.
Wuni A-R, Courtier N, Kelly D. Opportunities for radiographer reporting in Ghana and the potential for improved patient care. Radiography. 2020;26:e120–5.
Torres-Mejía G, Smith RA, de la Carranza-Flores ML, Bogart A, Martínez-Matsushita L, Miglioretti DL, et al. Radiographers supporting radiologists in the interpretation of screening mammography: a viable strategy to meet the shortage in the number of radiologists. BMC Cancer. 2015;15:410.
Suraj S, Sabita M, Pradip S, Avinesh S. A picture of radiography education and workforce in Nepal. J Med Imaging Radiat Sci. 2023;54(3):S11–2.
Berntsen A, Myklebust AM, Kjelle E. Reporting radiographers in Norway – A qualitative interview study. Radiography. 2023;29:450–5.
Plessis J du, Pitcher R. Towards task shifting? A comparison of the accuracy of acute trauma-radiograph reporting by medical officers and senior radiographers in an african hospital. Pan Afr Med J. 2015;21.
Bwangu J. Reporting on diagnostic images as role extension in Uganda : radiographers’ experiences and attitudes. [Thesis]. [Johannesburg]: University of Johannesburg; 2022. Cited 2023 Sep 20. Available from: https://ujcontent.uj.ac.za/esploro/outputs/graduate/Reporting-on-diagnostic-images-as-role/9926109607691.
Acknowledgements
Protocol submitted to PROSPERO (CRD42022384191).
Funding
This paper is part of a larger funded study by Health Education England, UK and was supported by Canterbury Christ Church University.
Author information
Authors and Affiliations
Contributions
Authors PL, CB and TS designed the project, PL and CB wrote the main manuscript, PL prepared the figures and tables, CB, TS and NW (all authors), reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable. This manuscript is exempt from institutional research ethics approval as it does not use any human or animal subject data or tissue.
Consent for publication
Not applicable. This manuscript is exempt from institutional research ethics approval as it does not use any human or animal subject data or tissue, thus no requirement for participant consent to publish.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
PRISMA_2020_abstract checklist. Completed PRISMA checklist for abstract.
Additional file 2.
PRISMA_2020_checklist. Completed PRISMA checklist for systematic review’s.
Additional file 3.
Raw Data.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Lockwood, P., Burton, C., Woznitza, N. et al. Assessing the barriers and enablers to the implementation of the diagnostic radiographer musculoskeletal X-ray reporting service within the NHS in England: a systematic literature review. BMC Health Serv Res 23, 1270 (2023). https://doi.org/10.1186/s12913-023-10161-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-023-10161-y