Abstract
Background
Evidence indicates that antenatal care (ANC) has both indirect and direct effects on maternal and perinatal morbidity and mortality reduction. In Uganda, the ANC attendance rate stands at 97.3% for one visit, but 59.9% for four or more visits. Given the imminent shift to the eight-contact ANC model in Uganda, combined with a lack of universal coverage for completion of four ANC visits, there is need for research that provides information on the factors that differentiate completers of recommended ANC attendances from non-completers. The aim of this quantitative study was to assess service- level factors affecting completion of ANC attendance defined by completion of four or more visits among women of reproductive age in Iganga district in Uganda.
Methods
Facility assessment scores on the service-level factors of interest for health facilities were obtained using a service level index tool. The relationship between the ANC completion rates of clients sampled from records at the health facilities and facility scores on service-level factors of interest were analyzed. Regression was conducted to determine the predictive relationship between ANC service availability, ANC service content, and ANC service organization, and completion of ANC attendance.
Results
The model was statistically significant, χ2 (6) = 26.118, p ˂ 0.05, and accounted for approximately 17.3% of the variance of ANC attendance completion (R2 = .173). Completion of ANC attendance was primarily predicted by better timing of provision of ANC services, and to a lesser extent by higher levels of availability of medicines and medical supplies.
Conclusions
This study demonstrated that service-level factors have a predictive value for completion of ANC attendance. The findings can be used to improve availability, content, and organization of ANC services with the aim of enhancing positive experiences for clients and motivating them to complete the recommended number of ANC visits.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
Of the 1.5 million babies born in Uganda annually, 38,000 are stillborn [1]. More than half the stillbirths in sub-Saharan Africa are antepartum (occurring during pregnancy before the onset of labor) with the major underlying causes being hypertensive disorders of pregnancy, infections, and placental complications resulting in antepartum hemorrhage [2, 3]. Together, these three conditions account for three quarters of antepartum stillbirths in sub-Saharan Africa for which the cause is known [2]. In Uganda, specifically, hypertensive disorders, anemia, and syphilis are some of the leading maternal conditions associated with stillbirths [4].
Evidence indicates that antenatal care (ANC) has both indirect and direct effects on maternal and perinatal morbidity and mortality reduction [5]. For example, Lawn et al. [6], demonstrated that higher national coverage of ANC is strongly associated with lower antepartum stillbirth rates. Furthermore, 50% of stillbirths and 60% of early neonatal deaths are not linked to specific maternal conditions, underscoring the need for early identification of at-risk pregnancies during the prenatal period [1]. ANC from a skilled provider is a proven intervention aimed at monitoring pregnancy to reduce morbidity and mortality risks for the mother and child that may occur during pregnancy, delivery, and the postnatal period [7]. This is attributed to the opportunity that the ANC platform provides to detect and treat pregnancy-related complications and to ensure early identification and mitigation of risk factors for complications during labor and delivery [5, 8]. In Uganda, the ANC attendance rate stands at 97.3% for one visit but drops to 59.9% for four or more visits [9]. Rural regions in Uganda have rates as low as 58% for four or more visits, indicating noncompletion of up to 42% among pregnant women in rural areas, with the worst performing region in the country having a rate of only 44.5% [9].
Maternal and perinatal survival are currently a high priority for the government of Uganda (GOU). as indicated in the government’s Sharpened Plan and Investment Case for Reproductive, Maternal, Newborn, Child, and Adolescent Health [4]. ANC service provision is part of Cluster 2 of the maternal and child health cluster in the Uganda Minimum Health Care Package for pregnant women in Uganda [10]. While the country is currently implementing a minimum of (at least) four ANC visits, the government has incorporated an eight-contact model into the national sexual and reproductive health policy guideline and in 2018 started initiating activities to support a gradual switch to the eight-contact ANC model recently recommended by WHO for low- and middle-income countries [11]. The eight-contact model emphasizes completion of the first visit as early as possible in the first trimester of pregnancy, with the next visit scheduled at 20 weeks and then repeat visits at 26 weeks, 30 weeks, 34 weeks and then every two weeks until delivery [7]. Given the imminent shift to the eight-contact ANC model of service delivery level in Uganda, combined with a prevailing lack of universal coverage for completion of four ANC visits, there is need for research that provides current information on the factors that differentiate completers of recommended ANC attendances from non-completers, particularly in the rural areas of the country [12].
The most recent national Service Provision Assessment (SPA) survey for Uganda was conducted in 2007 and collected information on overall availability of facility-based services, including ANC services. The 2007 survey data indicated that 70% of health facilities surveyed offered ANC services, but only 20% of health facilities had all the equipment and medical supplies necessary for provision of basic ANC services [13].
Findings from a 2013 survey indicated that 70% of the health facilities visited offered ANC services, but actual provision of discrete components of the recommended ANC service package varied from 69% providing intermittent preventive treatment for malaria in pregnancy to only 12% of health facilities providing advanced distribution of misoprostol to pregnant women [14].
A study conducted in 2018, found that the trend in inconsistent delivery of the comprehensive ANC service content has persisted over a twenty-year period with the lowest overall coverage being having a urine sample taken at 27.9% and the highest overall coverage being having been weighed at 83.6% [12]. Benova et al. [12], also found that only 9.6% of women who completed four or more ANC visits received all eight ANC care components.
Chowfla et al. [15], found that screening, diagnosis, and management of common causes of maternal and neonatal morbidity and mortality during pregnancy was poorly conducted in health facilities surveyed with only three percent of expected cases of pre- eclampsia being diagnosed on a monthly basis.
From the results of the 2007 SPA, 58% of the health facilities provided ANC services for five or more days per week while 37% offered the services for only two days per week. Lower frequency of ANC service provision per week was more likely for primary care facilities than for higher-level and referral facilities such as hospitals [13]. Conrad et al. [16], found gaps in ANC provision in Uganda including ineffective organization of educational sessions, selective omission of certain services, lack of explanation of important clinical and laboratory procedures, failure to link the performed procedures with preventive information, and occasional lack of respect for clients.
Findings from the 2016 DHS in Uganda revealed that 90% of women who gave birth in the five years preceding the survey received ANC from a skilled provider at least once for their last birth [9]. These findings are similar to the National Service Delivery survey data that indicated 97% of women who needed ANC services utilized them [17]. However, nationally only 60% of women received ANC from a skilled provider at least four times [9].
Kawungezi et al. [18] and Bbaale [19], focused mainly on the role of non-facility level factors on ANC utilization. Kawungezi et al. [18], found that individual level factors such as religion, occupation, level of education, and parity influenced place of ANC attendance, number of ANC visits, and ANC booking time in Uganda. Bbaale [19], also found significant associations between individual level factors such as regional disparities, religion, access to media, maternal decision-making autonomy, wealth status, timing of pregnancy, birth histories, birth order, and frequency, and timing of ANC attendance in Uganda [18]. Bbaale [19], strengthened the evidence that women in rural areas of Uganda have lower utilization rates of ANC compared to their urban counterparts.
Studies on ANC service utilization in Uganda have focused on ANC service availability, service content, and to a limited extent service organization. Few studies have focused on the relationship if any, between these factors and ANC service utilization defined by completion of the recommended ANC visits.
Methods
Study design and setting
This was a quantitative study involving investigation of the possible relationship between completion rates of users of ANC services which is the dependent variable and a set of independent variables namely: provider availability, services hours, range of services, and level of service integration. Deductive techniques that are core to quantitative research were used to test the null hypothesis that there is no statistically significant relationship between provider availability, service hours, range of services, the level of service integration, and ANC completion [20].
The setting for the study were selected public and private not for profit health facilities in Iganga district in Eastern Uganda.
Using WHO’s previous standard model of ANC visits, completion of ANC attendance is defined in this study as a client having attended four or more ANC visits during her most recent pregnancy while non-completion is defined as having attended less than four ANC visits [21, 22].
Characteristics of study participants
The study population consisted of all adult clients of reproductive age (18 – 49 years) who attended ANC services in the selected health facilities over a 12-month period prior to the study. The health workers included clinical health facility staff and/or administrative staff directly involved in management of the selected health facilities.
Data collection procedures
The District Health Officer contacted each selected health facility in this study to communicate the research aims and logistics for data collection. The role of the District Health Officer was to provide an additional check with regard to ensuring that ethical review guidelines had been complied with prior to giving clearance for the research in Iganga district. A copy of this letter was presented to the medical officer in-charge at each facility before beginning any data collection.
The study objectives and outline were reviewed with each medical officer/health facility in-charge. Written consent was requested from the medical officer/health facility in-charge and documented as part of the study.
At all selected health facilities ANC attendance records in patient registers from the maternity departments for the twelve months prior to the study were examined. As this was a retrospective data collection process involving analysis of secondary data, the patients whose records were examined were no longer physically at the facility; instead, permission to conduct the patient record abstract data collection was sought from the medical officer in-charge at the facility. No identifiable information, such as the patient’s name, phone number, address, or otherwise was captured. The selected health facility respondents were informed that they could stop the questionnaire at any point in time without any adverse consequences.
Variables and sources of data
The study investigated the relationship between ANC services utilization assessed as completion of four or more visits as the dependent variable and a set of independent variables namely: ANC service availability, ANC service content, and ANC service organization. Data sources included integrated ANC facility registers, summary Health Management Information System (HMIS) reports and health facility manager interviews.
Instrumentation and measures
Data collection involved conducting structured quantitative in-person interviews with facility managers and record reviews using the a Service Level Index (SLI) tool and patient chart abstraction using a patient chart abstract tool.
Service level index tool
Facility assessment scores on the service level factors of interest for selected public and private not for profit health facilities were obtained using the SLI tool which was administered to the health facility in-charges. The indicators proposed for inclusion in the SLI tool are listed in Table 1. Pre-testing of the SLI tool was done as part of Study 1 of this set of studies (Level of Agreement of the SLI tool with the standard SPA tool for measurement of ANC service provision) at a selected health facility in the study district.
Patient chart abstract tool
The patient abstract tool included information on the client’s age and total number of ANC visits completed. No identifiable information, such as the client’s name, phone number, address, or otherwise was captured as part of this module. To maintain client anonymity, each client enrolled in ANC over the 12-month period preceding the study was assigned a unique code/number as part of the data collection process.
At all selected health facilities, handwritten patient registers from the integrated ANC register were examined. The data in the ANC registers included data on ANC users who accessed the static ANC clinic as well as ANC outreach data tallied into the register by the health workers. Electronic health records are rarely available at health facilities in this setting except perhaps for the largest regional referral hospitals. ANC cards or Mother-Baby passports are given directly to the clients to take home and were therefore not available for review. As this was a retrospective data collection process, the patients whose records were examined were no longer physically at the facility, instead, permission to conduct the patient record abstract data collection was sought from each medical officer in-charge of a study facility.
A district that meets nationally approved criteria for classification as high burden for poverty and maternal mortality was purposively selected. Stratified random sampling was used to sample health facilities using a complete list of health facilities in the selected district as the sampling frame compiled in consultation with the District Health Management Team. Stratification ensured increased precision since the stratum are internally homogenous, but each stratum differs from the other [23].
Determination of the sample size for health records in this study was based on a standard formula for calculating an appropriate sample size for estimating magnitude/level of the dependent variable (completion of four or more ANC visits).
Based on the power analysis the study needed a minimum of three hundred seventy-four participants. Systematic random sampling was used to select these client records from the facility registers. This approach is accurate and ensured that every record had the same probability of inclusion [10].
Statistical analysis
Logistic regression was conducted to determine the predictive relationship between ANC service availability, ANC service content, and ANC service organization and completion of ANC attendance [24]. The independent variables were ANC service availability, service content. and service organization. The dependent variable was dichotomized to create a variable with two levels: less than four visits completed, and four or more visits completed. Each of the independent variables were categorized as ordinal variables using the actual values from the SLI scores of health facilities. The regression model contained six variables (range of recommended services provided, timing of services, integration with other services, availability of medical equipment, availability of medicines & medical supplies and availability of trained health provider). Details of categorization of the variables are provided in Table 2.
The relationship between the ANC completion rates of clients sampled from records at the health facilities and facility scores on service level factors of interest were analyzed. Listwise deletion was used to handle missing data. Using this approach, any cases with missing data were excluded and the remaining data were analyzed [25]. Sensitivity analysis was conducted to determine the robustness of the results to the deviations from the missing at random assumption [26]. The multiple R-statistic was used to determine the strength of the relationship between the independent variables and the dependent variable [27].
Results
All eight study sites were public sector facilities under direct management of the government of Uganda. Six study sites offered ANC services 5 days a week, while one site offered these services 6 days a week and one site offered the services only two days a week. Seven study sites were open 24 h for routine service provision, but only one site provided ANC services on a 24-h basis. Table 3 summarizes the general characteristics of the eight study sites.
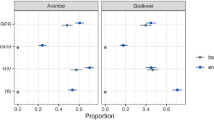
Under the service availability domain, only four percent of ANC completers utilized a facility with a high medical equipment availability score compared to 80% completers utilizing a facility with a low medical equipment score (p = 0.006), 28% of ANC completers utilized a health facility that was assigned a high availability score for medicines and medical supplies compared to 72% of ANC completers utilizing facilities with low scores for availability of medicines and medical supplies at the time the study was conducted (p = 0.01). For the service content domain, the majority of ANC completers (56%) utilized facilities whose range of ANC service provision was fair, but majority of non-completers utilized facilities whose range of service provision was good (p-value = 0.002). For the sub-domain of ANC service organization, 64% and 92% of ANC completers and non-completers respectively utilized health facilities whose timing of service provision was good (p < 0.001) while 24% and 54% of ANC completers and non-completers respectively utilized facilities that were practicing good integration of ANC with other services (p = 0.004). Table 4 summarizes the cross-tabulation findings taking ANC visit completion among ANC service users in the eight study sites between July 2019 and June 2020.
The full model containing all predictors was statistically significant, χ2 (6) = 26.118, p ˂0.05, indicating that the model could distinguish between women who completed four or more ANC visits and those who did not complete four or more ANC visits. The χ2 in the Hosmer- Lemeshow goodness of fit test was 0.732 with a significance level of 0.994 indicating a good model fit. The model as a whole explained 17.3% (Nagelkerke R squared) of the variance in ANC completion and correctly classified 93.4% of respondents. Only two of the independent variables made a unique statistically significant contribution to the model and that was availability of medical supplies and timing of ANC services. As displayed in Table 5, the results indicate that the odds of completing four or more ANC visits decrease by 0.02 for every 1 unit decrease in availability of medical supplies scores and increase by 4.6 for every 1 unit increase in ANC timing score when availability of medical equipment, trained staff, service integration and range of ANC services are controlled for (exp (B) = 0.02, p ˂ 0.05 and exp (B) = 4.6, p ˂ 0.05 respectively).
The prediction model contained two of the six predictors and was reached in five steps. The model was statistically significant, χ2 (2) = 22.752, p < 0.001, and accounted for approximately 15.2% (Nagelkerke R squared) of the variance of ANC attendance completion while correctly classifying 93.4% of study participants. As displayed in Table 6, completion of ANC attendance was primarily predicted by better timing of ANC services, and to a lesser extent by higher levels of availability of medicines and medical supplies. Timing of ANC services was found to be the most important factor for completion of ANC attendance (p value = 0.001). Facilities having timing of ANC service scores higher than 17 were at increased odds (4.5) of having their clients complete ANC attendance compared to those whose timing scores were less than 17. Health facilities having medicines and medical supplies scores higher than 106 which represented low availability of medicines and medical supplies in the SLI tool were at decreased odds (0.1) of having their clients complete ANC attendance compared to those whose scores were less than 106.
Discussion
The study aimed to assess service-level factors possibly affecting completion of ANC attendance defined by completion of four or more visits among women of reproductive age in Iganga district in Uganda. The study investigated whether service level factors independently predict completion of ANC attendance among pregnant women in Uganda. In relation to the research hypothesis, the study demonstrated that there is a statistically significant relationship between ANC service availability, ANC service organization and completion of four or more ANC visits.
A statistically significant predictive relationship was found between timing of ANC services under the service organization domain, and completion of ANC attendance. Women were more likely to complete at least four recommended visits if they received ANC services at a health facility that reported more working hours during the day dedicated to ANC service provision and providing ANC services with higher frequency per week. These results are supported by previous findings that show that provision of ANC services on restricted days of the week presented a barrier to optimal completion of services within the ANC package such as intermittent preventive treatment in pregnancy (IPTp) [28] and the absence of scheduling, increased uncertainty among clients which in turn affected ANC attendance [29]. Timing of provision of ANC services and improved awareness among clients about what specific services in the package to expect on different days of the week has been shown to influence consistent ANC attendance [16, 30]. This finding indicates that timing of ANC services should receive increased consideration through tailored approaches which could potentially include establishment of scheduling and appointment systems for ANC visits all of which contribute to improved planning, time management and certainty from the perspective of ANC service users.
There was also a statistically significant relationship between availability of medicines and medical supplies and completion of ANC attendance. The availability of medicines and medical supplies has emerged in previous studies as a factor that influences ANC attendance. However, Ediau et al. [31], demonstrated that while improved availability of basic medical supplies for ANC service provision led to significant improvements in first ANC visit attendance, by itself this intervention was insufficient to enhance completion of at least four ANC visits. This finding under-scores the need for an increased focus on ensuring availability of medicines and medical supplies as an approach for motivating ANC service users to complete the recommended number of visits.
There was no statistically significant predictive relationship between availability of trained health providers, availability of medical equipment, range of recommended services provided, and integration of ANC services with other services, and completion of ANC attendance. Availability of trained health providers may not influence completion of ANC attendance since it has been demonstrated that provider training by itself is insufficient to improve quality of care and positive ANC experiences for clients [32]. It is plausible that the lack of a predictive relationship between availability of medical equipment, availability of trained health providers, range of recommended services and completion to ANC attendance is explained by client levels of awareness about the recommended ANC package, purpose of medical equipment for ANC and their ability to correctly gauge competence levels of health providers. Afulani et al. [33], found that 30% of ANC service users in Migori county, Kenya did not understand the purposes of tests and medicines received during ANC attendance, but this proportion decreased with increased education levels [7]. This is similar to earlier findings by Pell et al. [34], that demonstrated through qualitative interviews that while women commonly recalled receiving medicines during ANC visits, specific mentions of receipt or non- receipt of HIV and syphilis testing, hemoglobin analysis or blood pressure measurement were rarely mentioned. The authors concluded that understanding of screening / diagnostic procedures and possibly the related importance of medical equipment for these procedures was low. Furthermore, studies have shown that users of ANC services are more likely to be motivated by the perceived quality of interaction with the health provider than by the service provider’s level training and competence [32]. ANC is a platform that can facilitate the provision of multiple health interventions therefore integration with other services is considered a best practice for effective ANC service provision [35]. Some studies have found that integration of ANC services with other services as a component of service organization results in improved user satisfaction but there is limited evidence of a link between integration with other services and completion of recommended ANC visits [36, 37].
Limitations of the study
Although this study generated new insights into the relationship between service level factors and completion of ANC attendance, there are some limitations. The low ANC completion rates in the study population translated into a very small sample size of ANC completers which may have affected the external validity of the study. Data from patient records was reviewed for the period July 2019 to June 2020. Between March 2020 and June 2020, the government of Uganda implemented strict lockdown measures that impacted utilization of routine health services across the country due to restrictions on the use of public transportation. This factor was not controlled for during analysis but may have affected the continued utilization of ANC services among women whose records were reviewed. This limitation as well as the short data period of one year and the focus on only one district may affect generalizability of the results.
Conclusions
This study has demonstrated that service level factors have a predictive value for completion of ANC attendance. The findings can be used to improve availability, content, and organization of ANC services with the aim of enhancing positive experiences for clients and motivating them to complete the recommended number of visits. Timing of ANC service provision, as well as the availability of medicines and medical supplies for ANC service provision, should be prioritized by managers at different levels of the health system. Further research is needed to improve measurement of service level factors and how these interact with ANC service completion incorporating perceptions of service users themselves.
Availability of data and materials
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
Abbreviations
- ANC:
-
Antenatal Care
- HMIS:
-
Health Management Information System
- SLI:
-
Service Level Index
- SPA:
-
Service Provision Assessment
- WHO:
-
World Health Organisation
References
Mbonye AK, Sentongo M, Mukasa GK, Byaruhanga R, Sentumbwe-Mugisa O, Waiswa P, et al. Newborn survival in Uganda: a decade of change and future implications. Health Policy Plan. 2012;27:iii104-17.
The Alliance for Maternal and Newborn Health Improvement (AMANHI) Mortality Study Group. Population-based rates, timing, and causes of maternal deaths, stillbirths, and neonatal deaths in south Asia and sub-Saharan Africa: a multi-country prospective cohort study. Lancet Glob Health. 2018;6:e1297-308.
Hirst JE, Villar J, Victora CG, Papageorghiou AT, Finkton D, Barros FC, et al. The antepartum stillbirth syndrome: risk factors and pregnancy conditions identified from the INTERGROWTH-21(st) project. BJOG. 2018;125:1145–53.
Ministry of Health. Uganda reproductive maternal newborn child and adolescent health sharpened plan. Kampala: Ministry of Health; 2016.
Carroli G, Rooney C, Villar J. How effective is antenatal care in preventing maternal mortality and serious morbidity? An overview of the evidence. Paediatr Perinat Epidemiol. 2001;15:1–42.
Lawn JE, Blencowe H, Waiswa P, Amouzou A, Mathers C, Hogan D, et al. Stillbirths: rates, risk factors, and acceleration towards 2030. Lancet. 2016;387:587–603.
WHO. WHO recommendations on antenatal care for a positive pregnancy experience. 2016. http://apps.who.int/iris/bitstream/10665/250796/1/9789241549912-eng.pdf?ua=1. Accessed 15 Nov 2019.
Dinh T-H, Kamb ML, Msimang V, Likibi M, Molebatsi T, Goldman T, et al. Integration of preventing mother-to-child transmission of HIV and syphilis testing and treatment in antenatal care services in the Northern Cape and Gauteng provinces. South Africa Sex Transm Dis. 2013;40:846–51.
Uganda Bureau of Statistics (UBOS) and ICF. Uganda demographic and health survey 2016: key indicators report. Kampala: UBOS, and Rockville, Maryland, USA: UBOS and ICF; 2017.
Ministry of Health. The second national health policy: promoting people’s health to enhance socioeconomic development. Kampala: Ministry of Health; 2010.
Ministry of Health. The national policy and service standards for sexual and reproductive health and rights – antenatal care protocol. Kampala: Ministry of Health; 2018.
Benova L, Dennis ML, Lange IL, Campbell OMR, Waiswa P, Haemmerli M, et al. Two decades of antenatal and delivery care in Uganda: a cross-sectional study using demographic and health surveys. BMC Health Serv Res. 2018;18:758.
Ministry of Health (MOH). [Uganda] and Macro International Inc. Uganda service provision assessment survey 2007. Kampala: Ministry of Health and Macro International Inc.; 2008.
Uganda Ministry of Health. Uganda services availability and readiness assessment. Kampala: Uganda Ministry of Health; 2013.
Chowfla A, Namajji C, Chitashvili T, Hermida J, Karamagi E, Holschneider S. Improving the quality of integrated antenatal care and care for preeclampsia/eclampsia in Jinja, Uganda. Final report. USAID ASSIST project. Chevy Chase, MD: University Research Co., LLC (URC). 2018.
Conrad P, De Allegri M, Moses A, Larsson EC, Neuhann F, Müller O, et al. Antenatal care services in rural Uganda. Qual Health Res. 2012;22:619–29.
Uganda Bureau of Statistics. National service delivery survey - 2015 report. Kampala: Uganda Bureau of Statistics; 2016.
Kawungezi PC, AkiiBua D, Aleni C, Chitayi M, Niwaha A, Kazibwe A, et al. Attendance and utilization of antenatal care (ANC) services: multi-center study in upcountry areas of Uganda. Open J Prev Med. 2015;5:132–42.
Bbaale E. Factors influencing timing and frequency of antenatal care in Uganda. Australas Med J. 2011;4:431–8.
Creswell JW. Research design: qualitative, quantitative and mixed methods approaches. 3rd ed. Thousand Oaks, CA: Sage Publications Inc.; 2009.
Measure Evaluation. Family planning and reproductive health indicators database. n.d. https://www.measureevaluation.org/prh/rh_indicators/womens-health/sm/percent-women-attended-at-least-four-times-for. Accessed 20 Nov 2019.
WHO. Antenatal care randomized trial: manual for the implementation of the new model. Geneva: WHO; 2002.
Cochran WG. Modern methods in the sampling of human populations. Am J Public Health Nation’s Health. 1951;41:647–68.
Turner AG, Angeles G, Tsui AO, Wilkinson M, Magnani R. Sampling manual for facility surveys for population, maternal health, child health and STD programs in developing countries. MEASURE evaluation manual series, no. 3. Chapel Hill: Carolina Population Center MEASURE; 2001.
Pallant J. SPSS survival manual. 5th ed. Berkshire, England: Open University Press, Mcgraw-Hill Education; 2013.
Kang H. The prevention and handling of the missing data. Korean J Anesthesiol. 2013;64:402–6.
Heiman GW. Basic statistics for the behavioral sciences. 6th ed. Belmont: Wadsworth, Cengage Learning; 2011.
Malaria Consortium. Research Brief. Assessing and addressing barriers to IPT2 uptake in uganda. n.d. https://assets.publishing.service.gov.uk/media/5ae3309740f0b631578aef07/Assessing-and-addressing-barriers-to-IPT2-uptake-in-Uganda-policy-brief.pdf. Accessed 5 Nov 2019.
Gong E, Dula J, Alberto C, de Albuquerque A, Steenland M, Fernandes Q, et al. Client experiences with antenatal care waiting times in southern Mozambique. BMC Health Serv Res. 2019;19:538.
Mathole T, Lindmark G, Ahlberg BM. Dilemmas and paradoxes in providing and changing antenatal care: a study of nurses and midwives in rural Zimbabwe. Health Care Women Int. 2005;26:937–56.
Ediau M, Wanyenze RK, Machingaidze S, Otim G, Olwedo A, Iriso R, et al. Trends in antenatal care attendance and health facility delivery following community and health facility systems strengthening interventions in Northern Uganda. BMC Pregnancy Childbirth. 2013;13:189.
Do M, Wang W, Hembling J, Ametepi P. Quality of antenatal care and client satisfaction in Kenya and Namibia. Int J Qual Health Care. 2017;29:183–93.
Afulani PA, Buback L, Essandoh F, Kinyua J, Kirumbi L, Cohen CR. Quality of antenatal care and associated factors in a rural county in Kenya: an assessment of service provision and experience dimensions. BMC Health Serv Res. 2019;19:684.
Pell C, Meñaca A, Were F, Afrah NA, Chatio S, Manda-Taylor L, et al. Factors affecting antenatal care attendance: results from qualitative studies in Ghana. Kenya and Malawi PLoS One. 2013;8:e53747.
Lincetto O, Mothebesoane-Anoh S, Gomez P, Munjanja S. Antenatal care. In: Lawn J, Kerber K, editors. Opportunities for Africa’s newborns: practical data, policy and programmatic support for newborn care in africa. Geneva, Switzerland: World Health Organization; 2006. p. 51–62.
de Jongh TE, Gurol-Urganci I, Allen E, Zhu NJ, Atun R. Integration of antenatal care services with health programmes in low- and middle-income countries: systematic review. J Glob Health. 2016;6:010403.
Munkhuu B, Liabsuetrakul T, Chongsuvivatwong V, McNeil E, Janchiv R. One-stop service for antenatal syphilis screening and prevention of congenital syphilis in ulaanbaatar, mongolia: a cluster randomized trial. Sex Transm Dis. 2009;36:714–20.
Acknowledgements
The authors thank the dissertation committee at Walden University for assistance with review and refinement of the manuscript. The authors thank the district health team of Iganga district in Uganda for assistance with the data access and data collection processes.
Funding
Author states no funding involved.
Author information
Authors and Affiliations
Contributions
Lorna Barungi Muhirwe was the principal investigator, spearheaded development of the research questions, design and implementation of the research, analysis of the results and writing of the manuscript. Magdeline Aagard supervised the research, provided critical feedback and helped shape the analysis and manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval for the study was obtained from the TASO-Uganda Institutional Review.
Board and the Walden University Institutional Review Board.
All protocols for consent to review the secondary data were conducted in accordance with the regulations of the TASO-Uganda Institutional Review Board, the Walden University Institutional Review Board, and the Declaration of Helsinki. The need for informed consent by service users was waived by the TASO-Uganda Institutional Review Board and the Walden University Institutional Review Board.
Administrative clearance to conduct the study in Iganga District was obtained from the District Health Officer. The District Health Officers contacted each selected study site to communicate the study aims. Each data collector presented a copy of the letter from the District Health Office and the Institutional Review Board approval to the medical officer/health facility in-charge at each site before beginning any data collection.
Written informed consent was requested from the medical officer/health facility in-charge and documented as part of the study. Before any data collection or interviews, data collectors carefully reviewed the study outline so that each respondent fully understood what was being requested of them. Respondents were informed that they could refuse to answer or stop the questionnaire at any point in time without any adverse consequences.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Muhirwe, L.B., Aagard, M. Completion of four or more ANC visits among women of reproductive age in Iganga district in Uganda: a quantitative study on the role of service-level factors. BMC Health Serv Res 23, 906 (2023). https://doi.org/10.1186/s12913-023-09913-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-023-09913-7