Abstract
Background
Medically uninsured groups, many of them migrants, reportedly delay using healthcare services due to costs and often face preventable health consequences. This systematic review sought to assess quantitative evidence on health outcomes, health services use, and health care costs among uninsured migrant populations in Canada.
Methods
OVID MEDLINE, Embase, Global Health, EconLit, and grey literature were searched to identify relevant literature published up until March 2021. The Cochrane Risk of Bias in Non-randomized Studies – of Interventions (ROBINS-I) tool was used to assess the quality of studies.
Results
Ten studies were included. Data showed that there are differences among insured and uninsured groups in reported health outcomes and health services use. No quantitative studies on economic costs were captured.
Conclusions
Our findings indicate a need to review policies regarding accessible and affordable health care for migrants. Increasing funding to community health centers may improve service utilization and health outcomes among this population.
Similar content being viewed by others
Background
Canadian health care
Despite having “universal” medical care coverage for physicians and hospitals in Canada, there are many residents who remain ineligible. The number of uninsured individuals is estimated to be between 200,000 to 500,000 people in Ontario alone [1]. The exact number is unknown given the difficulties in collecting data from this population. The impact of lack of health care insurance on these individuals, who are mainly migrants, is an understudied area in Canada to-date [2,3,4,5,6].
On average, over 300,000 new international migrants come to Canada annually and this number continues to increase [7]. The United Nations Migration Agency defines a migrant as someone who is moving or has moved across an international border or within a state away from their place of birth [8]. From January to March 2019, 82.0% of Canada’s population growth came from international migration [7].
Canada has a publicly funded health care system, Canadian Medicare, which provides residents free access to medically necessary hospital care and physician services [9, 10]. Instead of having a single national plan, Canadian Medicare is comprised of thirteen provincial and territorial health care insurance plans [10]. Residents receive medical coverage from the province or territory that they live in. The Federal government contributes to the financing of provincial/territorial medical health care systems provided that the provinces/territories adhere to the principles of the Canada Health Act (i.e., public administration, comprehensiveness, universality, portability, accessibility). However, there are exceptions—the Interim Federal Health Program (IFHP) offers temporary coverage of basic health services for refugees and asylum seekers, and the Indian Act of 1876 gives the federal government responsibility for the health care of Indigenous Peoples living on reserves. Nevertheless, some individuals are not eligible for provincial medical insurance coverage due to a lack of permanent residence status which according to the Canada Health Act principle of “universality” is a must. As the definition of “resident” is left to the provinces and territories, the eligibility criteria varies across Canada [11]. In Quebec, Ontario, British Columbia, and Manitoba, a three-month waiting period is imposed on new permanent residents before they qualify for provincial medical insurance [12]. This policy was removed in Ontario during the Coronavirus pandemic [13] and it is unclear whether it will be reinstated. Further, undocumented and out-of-status migrants do not qualify for Canadian Medicare and in Ontario, it is estimated that there are approximately 250,000 out-of-status migrants who do not have access to health care coverage [14]. In other words, the uninsured population in Canada is quite heterogenous. At the same time, the migrant population is also heterogenous made up of economic class immigrants, international students, seasonal workers, and refugees, among many others [15]. In Canada, there is a strong relationship between migrant status and being medically uninsured [16].
Lack of insurance coverage can also interact with other determinants of health to influence the health and health care experiences of migrants. For example, without provincial medical coverage, migrants often rely on private insurance or make out-of-pocket payments which can be costly to low-income individuals [17]. Other factors including insufficient knowledge of the Canadian health care system, language barriers, fear of deportation, cultural differences, and discrimination or denial of care also generate barriers and contribute to a decline in health status [3, 5, 18, 19].
Health and health care services use among uninsured
Reduced coverage for migrants may result in an increase in patients seeking emergency care as a last resort for conditions such as uncontrolled diabetes or mental health issues that could have been addressed at earlier stages [20]. Medically uninsured migrants with children often experience delays in surgeries, lack of adequate care for mental health issues, and inability to access support for developmental disabilities [4]. Uninsured pregnant women are also a group of concern as many go without any prenatal care and may experience complications during labour and delivery [4, 21]. These barriers to accessing care can lead to increased complications from untreated or delayed diagnoses of acute or chronic conditions [22]. Lack of insurance coverage among migrants has been associated with lower self-perceived health [23].
Extensive literature from high-income countries including Canada have focused on the “healthy immigrant effect” [24]. It states that immigrants on arrival are healthier than non-immigrants in the receiving country, but with time, their health deteriorates and resembles that of non-migrant residents. The reason why immigrants are healthy on arrival is said to be because of selection at both the individual (individuals who are healthy make the decision to migrate) and institutional (individuals who are healthy and who have high education, professional experience, and show potential to contribute to the Canadian economy are selected by the State) level. The reason why health deteriorates is also said to be because of a number of reasons (e.g., racism, lack of employment), one of which is the lack of health services usage [25, 26]. The strength of the healthy immigrant effect has shown to differ across groups, however [26, 27]. For instance, Lu and Ng (2019), using a Canadian linked dataset, found that the healthy immigrant effect on various health outcomes differed across immigrant categories [27]. It was stronger in economic-class immigrants while among refugees, it was only seen for less severe chronic conditions. Moreover, some studies challenge the healthy immigrant effect and instead provide results for the “sick immigrant effect” which states that immigrants are unhealthier than their native counterparts, even on arrival [28, 29]. This is sometimes the case with refugees who have less-strict guidelines for immigration since the main goal of refugee policies is to help those in dire circumstances.
Financial impact of medical uninsurance
Reductions to IFHP in 2012, which have since been reinstated, were projected to save $50 million per year [22, 30]. However, a study conducted by Evans et al. (2014) found that these costs were ultimately transferred to hospitals, many of which have policies and ethical responsibilities to provide care in emergencies regardless of payment [30]. For example, the University Health Network in Toronto attributed over $800,000 in unpaid service debt to uninsured emergency services as a result of IFHP changes [20]. The three-month waiting period in Ontario was also implemented for cost-cutting purposes and to prevent individuals from entering the country solely for the purpose of utilizing “free” health care [31]. Although its economic and health impact is not clearly known, critics have mentioned that the policy may not be cutting costs as expected [1, 32, 33]. Individuals may be delaying necessary care until the wait period is over. Delaying care can increase health care system costs as people may be using health care services for conditions that have since worsened and are more severe and costly to treat in month four [17]. Hospital costs may also be transferred to community organizations who often provide care to those who do not have medical insurance while lacking the funds that hospitals have. At the individual level, individuals without medical insurance have to pay for primary or hospital care in Canada via private insurance or out-of-pocket. Not only is this a health equity issue, it can lead to these individuals facing financial problems which in turn could affect their health conditions even more. An understanding of what the literature shows in terms of out-of-pocket expenditures for the provincially medically uninsured and the costs to the health care system (public or private) to provide care to the medically uninsured would help evaluate policies targeted towards medically uninsured individuals.
Altogether there is limited understanding of the economic and health impact of Medicare uninsurance among migrants in Canada. Although challenges faced by migrants are widely known in Canada [14], at present there are limited reviews focusing on uninsured migrants and to our knowledge, no systematic reviews examining all migrant populations in Canada such as refugees, undocumented migrants, new permanent residents affected by the three-month waiting period, and international students [3, 5, 33]. Previous Canadian reviews have also focused on qualitative primary studies [5, 33]. As migration and the number of uninsured individuals increase, it is important to gain a comprehensive understanding of health outcomes and health care utilization trends among medically uninsured populations in Canada as well as understand the size of the problem. A systematic analysis of literature can inform where there are gaps in research as well as what the priority needs are. As such, this review sought to synthesize quantitative literature on health outcomes, health care utilization, and out-of-pocket public expenditures and/or costs to the public or private health care system to provide care to medically uninsured populations. Following systematic review methodology, this review also aimed to conduct quality assessment, which is also known as quality appraisal, critical appraisal, and risk of bias assessment. Although systematic reviews are often considered to be the highest level of evidence in the literature, they have their own biases that can lead to some studies having a greater weight in influencing the recommendations made in the review [34,35,36]. To prevent this, the methodological quality and rigor of each of the studies was assessed and reported on.
Methods
Research question and protocol
This systematic review asks: “What health outcomes, health care utilization trends, and health care costs are reported among uninsured migrant populations in Canada?” For the purpose of this review, with the understanding that the uninsured group is quite heterogenous in Canada, uninsured populations were broadly defined as individuals who are provincially medically uninsured (i.e., do not receive health care coverage from their province/territory for medically necessary physician and hospital services). This includes but is not limited to permanent residents waiting for their health card during the three month arrival period in certain provinces, undocumented individuals, asylum seekers who are denied or awaiting their refugee claim, refugees who are refused benefits under the IFHP, temporary foreign workers, visitors, and international students. A systematic review protocol was created a priori to ensure transparency, reproducibility, and consistency.
Search strategy
A comprehensive search algorithm was created and implemented in Ovid MEDLINE, EconLit, Embase, and Global Health on March 9, 2021. The algorithm was created in consultation with a university librarian, after searching “uninsured AND Canada AND health” in MEDLINE and reviewing key words in the title and abstract of relevant papers until saturation was reached. The final search algorithm consisted of key terms related to “uninsured migrant”, “health”, and “Canada” and is further detailed in the supplementary document. To ensure the electronic database search captured all relevant literature, reference lists from all included studies and relevant reviews were also screened. In addition, targeted grey literature was searched on government and research organization websites. The first ten pages of Google Scholar were searched on March 30, 2021 using the following search terms: “uninsured AND Canada AND health”, following guidelines by Haddaway et al. (2015) [37].
Inclusion and exclusion criteria
Articles were included if they a) studied the population of interest (uninsured migrants in Canada), b) examined the intervention of interest (Medicare uninsurance), c) reported at least one outcome of interest (health outcomes, health service utilization, or health care costs), and d) reported primary quantitative data. All reviews were excluded. Other exclusion criteria included notes, editorials, books, news reports, case reports, commentaries, opinions, and letters. Qualitative research was also excluded given that previous reviews have already summarized qualitative literature on this population in Canada [5, 16, 33]. In addition, we were interested in synthesizing the quantitative relationship between medical uninsurance and various outcomes (i.e., health outcomes, health care use, and cost) and understanding the size of the problems affecting the medically uninsured, for which quantitative research was relevant.
Studies were also excluded if they focused on a migrant population residing outside of Canada. Additionally, studies examining the lack of health insurance for services not covered under Canadian Medicare, such as dental or vision care, were excluded. Due to financial and human resource limitations, studies reported in languages other than English were excluded. Lastly, studies examining the IFHP were excluded because this federal program provides comparable health insurance coverage for some medical care services to refugees and refugee claimants (IFHP is intended to be comparable to the provincial medical care insurance programs. It provides coverage for basic health care services as well as supplemental services and prescription drug coverage), and thus does not meet the inclusion criteria [38].
Screenings, extraction and quality assessment
Title and abstracts of papers were screened by two investigators independently using the inclusion and exclusion criteria. Disagreements were discussed and resolved between them. Full-text reviews were conducted for studies that could not be excluded on the basis of title and abstract content. Data extraction and quality assessment were conducted independently by two reviewers, and conflicts were managed by a third reviewer. Some information extracted from the studies included: year of publication, study location, demographic characteristics of the population, study design, uninsured definition, objectives of the study, outcome measures, and main results.
The Cochrane Risk of Bias in Non-randomized Studies – of Interventions (ROBINS-I) tool was used to assess the quality of included studies. The overall ratings for risk of bias were classified as low, moderate, serious, or critical. The tool was selected as it screens studies for different types of biases including selection, performance, detection, attrition, and reporting bias [39]. Utilizing ROBINS-I ensured that conclusions were formed while considering the quality of the studies [39].
Review management
Citations were imported into Covidence, an online systematic review software. The software was used for de-duplication and relevance screening to screen the titles, abstracts, and full-texts of identified articles. Five reviewers took part in the screening process. All studies were screened between March 9, 2021, and March 30, 2021. Data was extracted from relevant papers and recorded in Microsoft Excel which was also used for descriptive analysis and charting. We utilized the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) statement to guide our reporting process [40].
Results
Search results
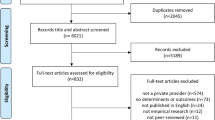
The search yielded 215 articles after deduplication. Of these, 134 were excluded at the title and abstract stage because they were not relevant to the topic of interest. At the full-text review stage, studies failing to meet the inclusion criteria for study design, patient population, intervention, outcomes, comparator group, and setting were excluded. An additional six studies were identified through a grey literature search of Google Scholar, of which one was included. A review of the reference lists of relevant scoping reviews yielded no additional studies. Two studies used the same data but their research questions and results slightly differed, and so were extracted and reported separately [22, 23]. A total of ten articles were included in the review. Figure 1 provides a complete overview of the study selection.
Characteristics of included studies
Table 1 shows the characteristics of included studies. Studies were conducted in the metropolitan cities of Toronto [41,42,43,44,45], Montreal [22, 23, 42, 45, 46], and Vancouver [42] in the provinces of Ontario [45, 47, 48], Quebec [22, 23, 42, 45, 46], and British Columbia [42], respectively. Studies used data from 2002 to 2017, and were published between 2011 and 2020, with the majority being published in 2013 [41,42,43, 45]. Most of the studies used chart reviews or hospital administrative data and conducted retrospective analysis [41, 43,44,45,46,47]. Three cross-sectional studies based on questionnaires were also included [22, 23, 48], as well as one prospective cohort study [42] using a combination of a questionnaire and administrative data. Due to the nature of study designs, longitudinal analysis was not applicable for most studies. The majority of studies used data from hospitals, while three used data from the community [22, 23, 44].
The definition of uninsured varied, but generally was described as individuals living in Canada who were not eligible for public health insurance either through the IFHP or provincial health insurance coverage. One study included not having private insurance as part of the definition of uninsured [23]. Another identified uninsured individuals as those who were billed through the Compassionate Care Program; a program offering free primary care services to uninsured patients [41]. Those who were entitled to health insurance but lacked documentation were also included as uninsured [47, 48]. The studies altogether covered a wide scope of uninsured populations (Table 1).
Studies investigated refugees or refused refugee claimants [22, 42,43,44,45,46], asylum seekers awaiting their refugee claim or those who were denied [22, 42, 43, 46], new permanent residents or immigrants [42, 43, 45, 48], visitors [22, 41, 46], undocumented [43, 45, 46], those with no legal or permanent migrant status [22, 41], foreign students and their dependents [22, 46], temporary foreign workers and their dependents [22], those awaiting sponsorship [46], those who were self-paying and reported a permanent address [48], landed immigrants in the three-month waiting period [41], those with a lost or expired health card [41], those who entered the country through non-regular means [43], and those who did not provide a reason for their uninsured status [41]. Two studies provided less specific definitions for participants such as authorized and unauthorized migrants [23] and insured and uninsured [47]. The number of uninsured individuals studied ranged from 52 uninsured individuals sampled from one hospital in Toronto, Ontario [41] to 140,730 uninsured individuals captured in the National Ambulatory Care Reporting System over a span of nine years [48].
In terms of sex, age, and ethnicity, most studies did not report detailed demographics of the uninsured population. Five studies focused on uninsured females as the objective was to assess perinatal outcomes, service utilization, and cervical cancer screening [42, 44, 46, 47, 49]. One study focused on children exclusively [45] and one study explored differences in outcomes by age [48]. No studies clearly analyzed health outcomes or health services use among medically uninsured older adults over the age of 65. Only one study provided data on ethnicities of uninsured individuals, although it was used for descriptive purposes only [43]. The study reported that the highest number of uninsured individuals were from a Caribbean background (40%) followed by South Asian (10%). An additional three studies, two of which reported on the same population, reported region of origin or birth [19, 20, 28].
Cost
Our search did not produce any results on health care costs among the uninsured population in Canada. There were no quantitative studies that captured the out-of-pocket cost that uninsured individuals may have to pay while accessing physician or hospital services. Two studies discussed cost, however both were excluded at the data extraction stage as they examined the financial effect of the 2012 cuts to the IFHP on refugee claimants and therefore did not meet our inclusion criteria [50, 51]. Moreover, no studies investigated the cost implications of having private insurance in the uninsured populations. This suggests a need for quantitative research on the financial impact of medical uninsurance.
Health service utilization
Nine included studies investigated health services use among uninsured individuals [22, 41,42,43,44,45,46,47,48]. Many of these studies concluded that utilization of health care services such as emergency room and physician visits, and hospital admissions were impeded by a lack of coverage (Table 2). Two studies showed that those without insurance were more likely to be triaged into a severe category upon arrival to the hospital compared to those who were insured, with Rousseau et al. (2013) suggesting this may be attributed in part to a delay in seeking care [31, 34]. Ridde et al. (2020) reported that the reasons for unmet health care needs among uninsured individuals included not having enough money to pay fees (81%), fear of being overcharged (73%), potential negative impact of health consultation on migration status (22%), and fear of rejection by the hospital (7%) [22]. They also mentioned that among those who used health care services, the majority accessed private pharmacies (60%) and community organized health services (43%), while hospitals were used by fewer individuals (14%) [22].
Most studies focused on healthcare services targeted towards females including prenatal and maternal care, midwifery, obstetrician access, and cervical screening. Regarding access to prenatal services, three studies reported reduced utilization among uninsured women compared to insured [43, 46, 47]. These services included prenatal visits, obstetrician services, and prenatal screening such as blood tests, cervical swabs, Pap tests, ultrasounds, and genetic screenings. Wilson-Mitchell & Rummens (2013) found that 6.5% of uninsured women received no antenatal care, whereas 100% of the insured received care [43]. Among uninsured women that received care, only 55% saw an obstetrician, compared to 94% of insured women. Uninsured women were significantly more likely to have sought the services of a midwife (36.0% vs. 4.0%), to have presented at a later gestational age (18.4 weeks vs. 12.7 weeks) and to have delivered their baby at home compared to the insured (28.7% vs. 16.6%) [29, 33]. Those delivering in the hospital had shorter stays compared to insured mothers [43, 47]. Contrary to these findings, Wiedmeyer, Lofters, & Rashid (2012) reported that uninsured women were more likely to have had a Pap test compared to insured women (95.0% vs. 75.0%, odds ratio (OR) = 6.65; p < 0.0001) [44]. However, when the regression was adjusted for variables such as age and English-speaking ability, the strength of the association was not significant (OR = 2.71; 95% confidence interval (CI) = 0.80–9.26). Notably, the sample size for this retrospective chart review was small and the results may not be generalizable since it was from a health care centre that provided care specifically to uninsured individuals and had an established support system for refugees and new immigrants. Jarvis et al. (2011) studied the amount of prenatal and perinatal care accessed by uninsured pregnant women at two primary care centres, one of which provided services free of charge [46]. Uninsured women had fewer prenatal visits than insured women and were more likely to have received inadequate care, which may be due to having started care later in their pregnancy. Jarvis et al. (2011) also conducted a site comparison which revealed uninsured women attended more appointments and were more likely to have received adequate care at the centre providing services free of charge [46]. The results indicate that providing prenatal and perinatal care services free of charge may increase utilization among uninsured women.
The quality assessment of these studies identified limitations with selected study designs (Table 3). As the majority were cross-sectional and retrospective studies, effects of temporality need to be taken into consideration when interpreting results. The reviewed data primarily originated from the emergency room and community health care centres which may not accurately represent the uninsured population in Canada. Since these centres were not randomly selected, extrapolation of the results may be misleading. Another validity concern in most of the studies is that the reported results were not adjusted for known confounders. Rather than running rigorous analytical regressions adjusting for covariates, many studies solely conducted descriptive analysis.
Health outcomes
Table 4 outlines nine studies that discussed health outcomes in the context of Medicare uninsurance among the Canadian migrant population [22, 23, 41,42,43, 45,46,47,48]. Comparing results from across studies, the most common outcome reported among uninsured individuals was poor mental health [22, 23, 41, 45, 48]. Hynie et al. (2016) reported a prevalence of mental and behavioural issues at 10.5% vs. 3.5% in the uninsured and insured, respectively [48]. Likewise, Rousseau et al. (2013) mentioned that compared to refugee children, uninsured children were more likely to access the emergency department for depression, post-traumatic stress disorder, suicidal thoughts, and substance use [45]. Focusing on the uninsured population, Cloos et al. (2020) reported that 26% of their sample had mental distress [23].
Other studies [45, 48] showed an association between uninsured status and adverse health outcomes [48]. For example, Hynie et al. (2016) found that obstetrical complications, resuscitation, and death upon arrival to the emergency room occurred more among uninsured compared to insured individuals at 5.6% vs. 2.7%, 15.6% vs. 11.2%, and 3.7% vs. 2.8%, respectively [48]. Uninsured compared to insured migrant children and youth in Ontario also showed higher diagnosis and prevalence for Ambulatory Care Sensitive Conditions at 4.6% vs. 3.2%. Bunn et al. (2013) also found greater HIV (human immunodeficiency virus) diagnosis among uninsured patients in comparison to insured patients (24% vs. 4%) [41].
Apart from mental health outcomes, there was no clear relationship between one particular health outcome and insurance status. Hynie et al. (2016) reported that while injury, poor mental health, and obstetric outcomes were more frequently reported among the uninsured population, skin disease, eye disease, and respiratory conditions were more frequently reported among the insured [48]. Likewise, Wilson-Mitchell et al. (2013) showed that while gestational diabetes was higher in those uninsured than insured, the opposite was true for hypertension [43]. Both studies however did not test for statistical significance. Rousseau et al. (2013) tested for significance and showed that refugee claimants were significantly more frequently diagnosed with respiratory virus infections, abdominal pain, and appendicitis while uninsured children reported musculoskeletal injuries or lacerations and mental health conditions such as depression, posttraumatic stress disorder, or suicidal thoughts more often (χ2 = 6.97; p = 0.008) [45]. Similar to other studies, Bunn et al. (2013) showed no statistically significant difference between the insured and uninsured groups with respect to many outcomes studied including hypertension, type 2 diabetes, and tuberculosis [41].
Four studies investigated the relationship between Medicare uninsurance and maternal health outcomes including gestational age at birth, type of labour, fetal health, intrapartum and postpartum complications, and preterm birth weight among women [42, 43, 46, 47]. In comparison to their insured counterparts, Darling et al. (2019) found uninsured pregnant women had higher rates of postpartum hemorrhage (3.4% vs. 2.9%), preterm birth (5.0% vs. 4.4%), and babies who were small for gestational age (2.1% vs. 1.7%) [47]. Both Darling et al. (2019) and Jarvis et al. (2011) also reported lower Caesarean section rate (26.3% vs. 35.6%; 13.9% vs. 15.0%) among uninsured compared to insured pregnant women [46, 47]. The most common reason for a Caesarean section among insured and uninsured women was labor dystocia and abnormal fetal heart rate respectively [43]. Gagnon, Merry & Haase (2013) also reported the absence of health insurance as a risk factor for higher emergency Caesarean delivery among migrant women (OR, 2.8; 95% CI: 1.2–6.3) [28]. Uninsured women had babies with lower birth weight than insured women, but the difference was not found to be statistically significant [43, 46]. Also, Wilson-Mitchell & Rummens (2013) reported no significant difference between low birth rate, preterm birth, breastfeeding rates, overall maternal complications, and intrapartum medical interventions among insured and uninsured women [43]. Research by Wilson-Mitchell & Rummens (2013) [29] and Darling et al. (2019) [47] was limited by using a retrospective cohort design. Furthermore, the authors did not address nor adjust for confounding factors. The chart review technique utilized by Wilson-Mitchell & Rummens (2013) also had challenges with accuracy and consistency [43]. Other studies accounted for confounders where possible, however, they were limited by lack of randomization, small sample size, and potential selection bias.
Three studies suggested that the determining factor behind poor health outcomes among uninsured patients was the three-month waiting period to receive health care coverage [41, 45, 48]. However, neither of these studies focused exclusively on the three-month waiting period. These studies received moderate overall bias ratings using the ROBINS-I tool. While Hynie et al. (2016) accounted for age and sex, other confounding variables such as measures of socioeconomic status were not addressed [48]. Rousseau et al. (2013) did not account for confounding variables, nor did the authors address any sources of missing data [45]. Finally, Bunn et al. (2013) had a small sample size which may affect generalizability of their results [41].
Overall quality assessment
The overall risk of bias for the included studies ranged from low to serious (Table 3). Three studies had a low risk of bias rating [22, 23, 47], six studies had a moderate rating [41,42,43,44,45, 48], and one study was rated as serious [46]. Studies with a low risk of bias rating typically controlled for confounders, addressed missing data, and reported all analysis conducted. Reasoning for a moderate rating included small sample sizes, confounders not addressed, and concerns with selection bias due to the sampling methods used. Given that most studies used retrospective databases or medical chart reviews, variables including socio-demographic information were often unavailable and therefore could not be adjusted for. There may have also been inaccuracy and inconsistency in reporting in studies using a retrospective chart review. There were also concerns with selection bias in some of the studies, especially in those sampling from non-randomly selected hospitals or clinics. One study received a serious risk of bias rating as it did not consider important confounders, used medical records that may have changed over time, did not account for missing data, did not compare those who were lost to follow up, and utilized a retrospective chart review [46].
Two included cross sectional studies utilized the same population of migrants in Montreal, Quebec [22, 23]. The studies differed in their purposes as Cloos et al. (2020) focused on the association between precarious migration status and self-perceived health [23] whereas Ridde et al. (2020) examined unmet health care needs and its associated factors among uninsured migrants [22]. Cloos et al. (2020) reported on health outcomes [23] while Ridde et al. (2020) reported on both health outcomes and health service utilization among migrants [22] and thus we felt it necessary to include both studies in the review.
Discussion
This systematic review examined multiple databases and grey literature sources to identify studies exploring the health outcomes, utilization, and cost consequences of Medicare uninsurance among the migrant population in Canada. The results showed that the medically uninsured population is very understudied in Canada. Other Canadian reviews conducted with narrower inclusion criteria have reported a similar number of included studies [3, 6, 42]. Reasons for limited studies on medically uninsured populations include ethical barriers to study this population and limitations of existing data collection methods [52, 53]. Gagnon et al. (2021) who conducted a narrative scoping review on immigration status as a determinant of health, which we see as a complementary study to ours, showed that studies in this area are primarily qualitative in nature [16]. Our search also highlighted that literature is limited by the definition of medically uninsured. Although the inclusion criteria of the review ensured only studies researching provincially medically uninsured populations were captured, the search proved it challenging to make comparisons across all studies because of the differences in how researchers defined uninsured and insured.
Our review demonstrated a gap in Canadian quantitative literature on the medically uninsured population’s out-of-pocket costs when accessing medically necessary services. There are also no economic studies that evaluate the financial impact of medically uninsured populations on the health care system. This restricts policymakers from understanding the scope of the problem. This gap should be addressed given that case studies demonstrate cost as an impeding factor to care. Caulford & D’Andrade (2012) published a case study of an 18-year old female who was told her case was not an emergency when she visited the emergency room for her sickle cell crisis [17]. While waiting in triage, she fainted and was hospitalized for three days, costing her $5,000.
Our results revealed that health services use was low when there was a lack of health insurance. For instance, some uninsured migrant women did not receive any prenatal care whatsoever [43]. This is of particular concern as prenatal care is widely regarded as effective and cost-saving with research suggesting that for every $1 US spent on prenatal care, there are $2 of savings [54]. Consistent with our findings, a scoping review by Magalhaes et al. (2010) found that undocumented migrant workers in Canada had reduced health service utilization due to limited access to health care stemming from fear of deportation, unaffordability of services, lack of knowledge of the health care system, and social isolation [3]. A study conducted by Allen et al. (2017) also reported systemic-level barriers and discrimination as a major factor behind low health care service use [55]. Notably, one study in our review examined a community health centre in Toronto and found the opposite effect [44]. Uninsured refugee women were more likely to receive cervical cancer screening than insured women. While rates of cervical cancer screening are low in the migrant population, this could be because the community clinic model removed barriers to care by providing interpreters, offering settlement services, and providing care to the uninsured free of cost [44]. This health care model could be useful for decision-makers as an example of how to accommodate the needs of this population and provide appropriate care The same trend was observed with the use of midwives when there was a cost associated with visiting physician or hospital services that they could not afford [43]. Physicians or personal social networks may direct women towards midwifery and community health centres that are providing services at little to no cost.
This review did not provide high quality evidence on health outcomes among uninsured populations as half of the studies used descriptive analysis without measures of associations and tests of significance and without adjusting for confounding factors. Our results indicated that uninsured women were at a greater risk of poor obstetric outcomes such as preterm births, emergency Caesarean sections, and postpartum hemorrhages [42, 43] which may be attributed to the absence of health care insurance. Moreover, new permanent residents reported mental distress, poor self-perceived health, and unmet health care needs which suggests the three-month waiting period may contribute to adverse effects on health and wellbeing [45]. This finding is consistent with previous research [6, 56]. A scoping review conducted on new permanent residents in Canada found the mandated three-month waiting period for health insurance created a barrier to accessing necessary care which negatively affected health outcomes [6].
Our review also revealed a greater prevalence of mental health issues such as depression and suicidal thoughts among uninsured migrants compared to their insured counterparts. Uninsured migrants often face poverty, systemic racism, trauma, lack of sufficient support systems, and added pressures when transitioning to a new environment [23, 57]. This exacerbates existing mental health issues as they cannot access services to address their needs [23]. Similar results have been reported in other countries with high numbers of migrants with precarious status [58, 59]. The growing body of qualitative Canadian studies have also reported similar findings [60]. Interviews conducted by Goel et al. (2013) indicated that participants experienced emotional hardship during the three month waiting period including fear, affecting their mental health [32].
Lastly, conducting quality assessment showed the limitations of the current literature including small sample sizes, lack of administrative data, and lack of rigorous analytical methods. The latter could have been because of the limitations of the minimal data that is available on uninsured migrants. In fact, prior to COVID-19, many organizations did not collect data on ethnicity and immigrant status. It is known from the literature that racism and ethnicity/race influence health outcomes and health care use of individuals [61, 62]. As such, racism and/or ethnicity/race may in fact interact with immigrant status to influence outcomes among the uninsured.
This review highlighted that it is impossible to know the current state of health outcomes and health care use among the medically uninsured at a population level if data is not available. It is unclear whether appropriate data is not being collected at the organizational level or whether organizations are not reporting that data. It points to a need to evaluate community and province-level data sources and assess what type of data is being collected and what is missing. At the same time, it becomes important to have a discussion on how best to collect data from uninsured individuals who are often very vulnerable and given that the process can create greater barriers between uninsured groups and the health care system.
There is also a need to create linked administrative datasets that show the services uninsured and insured individuals use over their lifetime. Linked databases will also help address the problem of missing data, especially that from the community. Given the challenges of quantitative data, this review also highlights the need to conduct multi-methods studies that include qualitative research. That being said, strengths of quantitative research should also be mentioned. This review presented the size of the health and health care problems that affect uninsured migrants. It also highlighted statistical differences between insured and uninsured groups for certain conditions and services.
Strengths and limitations
Our review provides a comprehensive analysis of the health outcomes and health services use among medically uninsured migrants in Canada. We utilized the Cochrane ROBINS-1 tool which allowed us to assess the quality of existing studies on the limitations of current literature. Our review also has a few limitations. First, we only included studies with sufficient quantitative data to extract. There are many qualitative studies focused on the uninsured population in Canada that could have provided interesting insights. Qualitative findings may have allowed us to gain a deeper understanding of reported health outcomes and trends in health care service use seen quantitatively in non-insured migrants. It could also further contextualize our findings, help fill the missing quantitative data gaps, especially with respect to cost data, and help policymakers understand the problem in greater depth. Additionally, the heterogeneity of included studies presents a limitation when interpreting results. Each study had a different definition of ‘uninsured’, and while some definitions shared common themes, some studies could have inadvertently included individuals who were not migrants, as chart reviews did not always include the reason for being uninsured or migratory status. Also, given the limited number of studies included, we could not do any sub-group analyses by uninsured group across studies (i.e., undocumented vs. permanent residents within three-month waiting period). We were also unable to make causal claims given the nature of the studies we included. Lastly, the review was restricted to the limits of the questions posed and search terms included a priori. Although we were interested in including and extracting French papers, we did not find any relevant studies in French. This may be because our search terms were in English.
Implications and future research
Our findings can be used to inform policy decisions regarding the provision of health insurance for migrants. Given the observed poor health outcomes, policymakers should consider how providing preventive care to migrants could be beneficial for population health and overall costs. Providing preventive care could help avoid expensive hospitalizations and improve health outcomes among the uninsured. Removing the three-month wait period for health coverage for new permanent residents should be considered as it could improve health by providing more timely care and therefore reduce costs for the government. Further, policymakers may consider increasing funding for community centres as they are commonly utilized by the medically uninsured [44]. Community health centres may also consider expanding their staff to include professionals specializing in mental health, pregnancy, and chronic illnesses as disparities in these areas were frequently reported in our review. An integrated medical system that is universal for all may also be created rather than having a two-tier system in which the uninsured have to rely on community organizations and face barriers in accessing care.
Future research may consider analyzing specific barriers that migrants face when accessing health insurance. Cost as a barrier to seeking care was not discussed in detail. This likely has a large impact on service usage as the cost of care in Canada is expensive for those who do not have medical insurance. Moreover, our literature search revealed a lack of clear data on the older migrant population in Canada. The elderly often experience chronic health conditions and multiple comorbidities. It is important to investigate service utilization in this population as they require additional support from the health care system such as long-term care. Future research may also consider focusing on areas such as specific mental health issues, chronic diseases, and therapy services to better understand the burden of medical uninsurance among migrants. Lastly, included studies were primarily conducted in Ontario and Quebec which reduces generalizability of results to other provinces. British Columbia is home to a very large migrant population and yet there are minimal quantitative studies conducted in this province, and only one study included in our review [7, 42]. As previously mentioned, this could be due to limited relevant data collection and data sources on the health and health care use of medically uninsured migrants. Researching health outcomes and health care services use of medically uninsured populations using linked datasets that include more data from the community as well as sociodemographic data is greatly needed.
Conclusion
This review builds on existing evidence by demonstrating how lack of insurance influences health outcomes, reduces health service utilization, and inhibits access to necessary care. There is a need to provide better access to affordable health care services for the medically uninsured population. We hope our findings can be used to inform policy decisions with the overall goal of improving inequities in health outcomes and service usage for migrants residing in Canada.
Availability of data and materials
All data generated or analyzed during this study are included in this published article [and its supplementary information file].
Abbreviations
- IFHP:
-
Interim Federal Health Program
- ROBINS-I:
-
Risk of Bias in Non-randomized Studies of Interventions
- PRISMA:
-
Preferred Reporting Items for Systematic reviews and Meta-Analyses
- HIV:
-
Human Immunodeficiency Virus
- OR:
-
Odds Ratio
- CI:
-
Confidence Interval
- P:
-
P-value
- X2:
-
Chi-squared statistic
- T:
-
T-statistic
- OHIP:
-
Ontario Health Insurance Plan
- ICD:
-
International Classification of Disease
- RAMQ:
-
Régie de l'assurance maladie du Québec
References
Barnes S. Health Care Access for the Uninsured in Ontario Symposium Report. 2016. Available from: https://www.wellesleyinstitute.com/wp-content/uploads/2017/01/Health-Care-Access-for-the-Uninsured-Symposium-Report.pdf.
Brabant Z, Raynault MF. Health situation of migrants with precarious status: Review of the literature and implications for the Canadian context - Part A. Soc Work Public Health. 2012;27(4):330–44.
Magalhaes L, Carrasco C, Gastaldo D. Undocumented migrants in Canada: A scope literature review on health, access to services, and working conditions. J Immigr Minor Heal. 2010;12(1):132–51.
Rousseau C, Hassan G, Measham T, Lashley M. Prevalence and correlates of conduct disorder and problem behavior in Caribbean and Filipino immigrant adolescents. Eur Child Adolesc Psychiatry. 2008;17(5):264–73.
Salami B, Meharali S, Salami A. The health of temporary foreign workers in Canada: a scoping review. Can J Public Heal. 2015;106(8):e546–54.
Bobadilla A, Orchard T, Magalhães L, Fitzsimmons D. Ontario healthcare coverage eligibility among new permanent residents: a scoping review. J Immigr Refug Stud. 2017;15(4):384–405. https://doi.org/10.1080/15562948.2016.1214993.
Immigration Refugees and Citizenship Canada. 2020 Annual Report to Parliament on Immigration. Immigration, Refug Citizsh Canada. 2020;41. Available from: https://www.canada.ca/en/immigration-refugees-citizenship/corporate/publications-manuals/annual-report-parliament-immigration-2020.html#trprograms%0A; https://www.canada.ca/en/immigration-refugees-citizenship/corporate/publications-manuals/annual-report-par.
United Nations. Migration. [cited 2021 Nov 10]. Available from: https://www.un.org/en/global-issues/migration.
Government of Canada. Canada Health Act R.S.C., 1985, c. C-6. Canada Heal. 1985;R.S.C C-6(2014):18. Available from: http://laws-lois.justice.gc.ca.
The Government of Canada. Canada’s health care system. 2022.
Allin S. Does Equity in Healthcare Use Vary across Canadian Provinces? Heal Policy. 2008;3(4):83–99.
Hutchison B, Levesque J, Strumpf E, Coyle N. Primary Health Care in Canada : Systems in Motion Source : The Milbank Quarterly , Vol . 89 , No . 2 ( June 2011 ), pp . 256–288 Published by : Wiley on behalf of Milbank Memorial Fund Stable URL : http://www.jstor.org/stable/23036216 Your use of the JSTO. 2015;89(2):256–88.
Ministry of Health HSB. COVID-19 Expanding access to OHIP Coverage and Funding Physican and Hospital Services for Uninsured Patients. Info Bulletin. 2020.
Martin D, Miller AP, Quesnel-Vallée A, Caron NR, Vissandjée B, Marchildon GP. Canada’s universal health-care system: achieving its potential. Lancet. 2018;391(10131):1718–35.
Houle R, Maheux H. 150 years of immigration in Canada. Statistics Canada. 2016 Jun 29; Available from: https://www150.statcan.gc.ca/n1/pub/11-630-x/11-630-x2016006-eng.htm.
Gagnon M, Kansal N, Goel R, Gastaldo D. Immigration Status as the Foundational Determinant of Health for People Without Status in Canada: A Scoping Review. J Immigr Minor Heal. 2021(0123456789). Available from: https://doi.org/10.1007/s10903-021-01273-w.
Caulford P, Andrade JD. Health care for Canada’s medically uninsured immigrants and refugees. Can Fam Physician. 2012;58:725–7.
Salami B, Mason A, Salma J, Yohani S, Amin M, Okeke-Ihejirika P, et al. Access to healthcare for immigrant children in Canada. Int J Environ Res Public Health. 2020;17(9):3320.
Hennebry J, McLaughlin J, Preibisch K. Out of the loop: (In)access to health care for migrant workers in Canada. J Int Migr Integr. 2015;17(2):521–38.
Piccininni C, Kwong M. Refugee health care funding in Canada. History, current state, and future directions. UWOMJ. 2019;88(1):40-42.
Khanlou N, Haque N, Mustafa N, Vazquez LM, Mantini A, Weiss J. Access barriers to services by immigrant mothers of children with autism in Canada. Int J Ment Health Addict. 2017;15(2):239–59.
Ridde V, Aho J, Ndao EM, Benoit M, Hanley J, Lagrange S, et al. Unmet healthcare needs among migrants without medical insurance in Montreal. Canada Glob Public Health. 2020;15(11):1603–16. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=med17&NEWS=N&AN=32459571.
Cloos P, Ndao EM, Aho J, Benoit M, Fillol A, Munoz-Bertrand M, et al. The negative self-perceived health of migrants with precarious status in Montreal, Canada: a cross-sectional study. PLoS One. 2020;15(4):1–22.
Beiser M. The health of immigrants and refugees in Canada. Can J Public Heal. 2005;96(SUPPL. 2):S30-44.
Ng E, Quinlan J, Giovinazzo G, Grundy A, Rank C, Syoufi M, et al. All-cause acute care hospitalization rates of immigrants and the Canadian-born population: a linkage study. Heal Rep. 2021;32(9):3–13.
Vang ZM, Sigouin J, Flenon A, Gagnon A. Are immigrants healthier than native-born Canadians? A systematic review of the healthy immigrant effect in Canada. Ethn Heal. 2017;22(3):209–41. https://doi.org/10.1080/13557858.2016.1246518.
Lu C, Ng E. Healthy immigrant effect by immigrant category in Canada. Heal Reports. 2019;30(4):3–11.
Constant AF, García-Muñoz T, Neuman S, Neuman T. A “healthy immigrant effect” or a “sick immigrant effect”? Selection and policies matter. Eur J Heal Econ. 2018;19(1):103–21.
Pinchas-Mizrachi R, Naparstek Y, Nirel R, Kukia E. The, “Sick immigrant” and “Healthy immigrant” phenomenon among Jews migrating from the USSR to Israel. SSM Popul Heal. 2020;12:100694. https://doi.org/10.1016/j.ssmph.2020.100694.
Evans A, Caudarella A, Ratnapalan S, Chan K. The cost and impact of the interim federal health program cuts on child refugees in Canada. PLoS One. 2014;9(5):3–6.
Babies couldn’t wait, mom billed $22K. CBC News. 2011;20; Available from: https://www.cbc.ca/news/canada/toronto/babies-couldn-t-wait-mom-billed-22k-1.1082905.
Goel R, Bloch G, Caulford P. Waiting for care: effects of Ontario’s 3-month waiting period for OHIP on landed immigrants. Can Fam Physician. 2013;59(6):269–75.
Sanchez J, Cheff R, Hassen N, Katakia D. Part one: examining the health status & health care experiences of new permanent residents in the three-month OHIP wait a scoping review of the peer-reviewed literature. 2016. Available from: https://www.wellesleyinstitute.com/wp-content/uploads/2016/07/Examining-Health-in-the-Three-Month-Wait-Part-One.pdf.
Pussegoda K, Turner L, Garritty C, Mayhew A, Skidmore B, Stevens A, et al. Identifying approaches for assessing methodological and reporting quality of systematic reviews: a descriptive study. Syst Rev. 2017;6(1):1–12.
Distiller SR. Quality assessment tools for systematic reviews. 2022.
Tran L, Tam DNH, Elshafay A, Dang T, Hirayama K, Huy NT. Quality assessment tools used in systematic reviews of in vitro studies: a systematic review. BMC Med Res Methodol. 2021;21(1):1–13.
Haddaway NR, Collins AM, Coughlin D, Kirk S. The role of google scholar in evidence reviews and its applicability to grey literature searching. PLoS One. 2015;10(9):1–17.
Government of Canada. Interim Federal Health Program: What is covered. 2022. [cited 2022 Sep 28]. Available from: https://www.canada.ca/en/immigration-refugees-citizenship/services/refugees/help-within-canada/health-care/interim-federal-health-program/coverage-summary.html.
Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:4–10.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, The PRISMA, et al. statement: an updated guideline for reporting systematic reviews. BMJ. 2020;2021:372.
Bunn S, Fleming P, Rzeznikiewiz D, Leung FH. Understanding the demographic characteristics and health of medically uninsured patients. Can Fam Physician. 2013;59(6):e276-81.
Gagnon AJ, Merry L, Haase K. Predictors of emergency cesarean delivery among international migrant women in Canada. Int J Gynecol Obstet. 2013;121(3):270–4. https://doi.org/10.1016/j.ijgo.2012.12.017.
Wilson-Mitchell K, Rummens JA. Perinatal outcomes of uninsured immigrant, refugee and migrant mothers and newborns living in Toronto, Canada. Int J Environ Res Public Health. 2013;10(6):2198–213.
Wiedmeyer ML, Lofters A, Rashid M. Cervical cancer screening among vulnerable women: Factors affecting guideline adherence at a community health centre in Toronto. Ont Can Fam Physician. 2012;58(9):521–6.
Rousseau C, Laurin-Lamothe A, Anneke Rummens J, Meloni F, Steinmetz N, Alvarez F. Uninsured immigrant and refugee children presenting to canadian paediatric emergency departments: disparities in help-seeking and service delivery. Paediatr Child Heal. 2013;18(9):465–9.
Jarvis C, Munoz M, Graves L, Stephenson R, D’Souza V, Jimenez V. Retrospective review of prenatal care and perinatal outcomes in a group of uninsured pregnant women. J Obstet Gynaecol Canada. 2011;33(3):235–43. https://doi.org/10.1016/S1701-2163(16)34824-1.
Darling EK, Bennett N, Burton N, Marquez O. Outcomes of uninsured midwifery clients in Ontario, Canada: a retrospective cohort study. Midwifery. 2019;77:24–31.
Hynie M, Ardern CI, Robertson A. Emergency room visits by uninsured child and adult residents in Ontario, Canada: what diagnoses, severity and visit disposition reveal about the impact of being uninsured. J Immigr Minor Heal. 2016;18(5):948–56.
Mattatall FM. Uninsured maternity patients in calgary: local trends and survey of health care workers. J Obstet Gynaecol Canada. 2017;39(11):1015–20. https://doi.org/10.1016/j.jogc.2017.05.002.
Kandasamy T, Cherniak R, Shah R, Yudin MH, Spitzer R. Obstetric Risks and Outcomes of Refugee Women at a Single Centre in Toronto. J Obstet Gynaecol Canada. 2014;36(4):296–302. https://doi.org/10.1016/S1701-2163(15)30604-6.
Oda A, Tuck A, Agic B, Hynie M, Roche B, McKenzie K. Health care needs and use of health care services among newly arrived Syrian refugees: a cross-sectional study. C Open. 2017;5(2):E354–8.
Campbell-Page RM, Shaw-Ridley M. Managing ethical dilemmas in community-based participatory research with vulnerable populations. Health Promot Pract. 2013;14(4):485–90.
Samuel TJ, White PM, Perreault J. National recording systems and the measurement of international migration in Canada: an assessment. Int Migr Rev. 1987;21(4):1170–211.
Buescher PA, Roth MS, Williams D, Goforth CM. An evaluation of the impact of maternity care coordination on Medicaid birth outcomes in North Carolina. Am J Public Health. 1991;81(12):1625–9.
Allen N, Walker SR, Liberti L, Salek S. Health Technology Assessment (HTA) Case Studies: factors influencing divergent HTA reimbursement recommendations in Australia, Canada, England, and Scotland. Value Health. 2017;20(3):320–8. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=med14&NEWS=N&AN=28292476.
Hamel-Smith Grassby M, Wiedmeyer ML, Lavergne MR, Goldenberg SM. Qualitative evaluation of a mandatory health insurance “wait period” in a publicly funded health system: Understanding health inequities for newcomer im/migrant women. BMJ Open. 2021;11(8):e047597.
Kaltman S, Pauk J, Alter CL. Meeting the mental health needs of low-income immigrants in primary care: a community adaptation of an evidence-based model. Am J Orthopsychiatry. 2011;81(4):543–51.
Wolff H, Stalder H, Epiney M, Walder A, Irion O, Morabia A. Health care and illegality: a survey of undocumented pregnant immigrants in Geneva. Soc Sci Med. 2005;60(9):2149–54.
Gushulak BD, MacPherson DW. Health issues associated with the smuggling and trafficking of migrants. J Immigrant Health. 2000;2:67–78. Available from: http://www.ncbi.nlm.nih.gov/pubmed/16228734.
Campbell RM, Klei AG, Hodges BD, Fisman D, Kitto S. A comparison of health access between permanent residents, undocumented immigrants and refugee claimants in Toronto Canada. J Immigr Minor Heal. 2014;16(1):165–76.
Mahabir DF, O’Campo P, Lofters A, Shankardass K, Salmon C, Muntaner C. Classism and everyday racism as experienced by racialized health care users: a concept mapping study. Int J Heal Serv. 2021;51(3):350–63.
Chiu M. Ethnic differences in mental health and race-based data collection. Healthc Q. 2017;20(3):6–9.
Acknowledgements
We would like to thank Emmanuel Guindon for his guidance on the search strategy and scope of the study as well as his edits to the manuscript.
Review
This manuscript has not been published or submitted elsewhere. An earlier version of the manuscript was released online as a working paper: https://bit.ly/32csjVH .
Funding
This study did not receive a specific grant from any funding agency.
Author information
Authors and Affiliations
Contributions
VB, SC, GP, CA, and EJ participated in the literature search, screening, data extraction, quality assessment, interpretation of findings, and writing and editing of the manuscript. SG was involved in all parts of the project as well as conceptualizing the project and guiding the review and writing process. SG is the corresponding author. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics review was not conducted as this article is a systematic review and the research did not involve human or animal participants.
Consent for publication
Not applicable.
Competing interests
There are no conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Appendices.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Garasia, S., Bishop, V., Clayton, S. et al. Health outcomes, health services utilization, and costs consequences of medicare uninsurance among migrants in Canada: a systematic review. BMC Health Serv Res 23, 427 (2023). https://doi.org/10.1186/s12913-023-09417-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-023-09417-4