Abstract
Background
Studies in many developing countries have shown that community health workers (CHWs) are valuable for boosting contraceptive knowledge and usage. However, in spite of the evidence, studies in Nigeria have rarely examined whether in the absence of skilled health personnel such as doctors and nurses in rural and remote communities, the health service contacts of non-users with CHWs drive the intention to use modern contraceptives. This study, therefore, examines the extent to which health service contacts with CHWs are associated with the intention to use modern contraceptives among non-users in rural communities of Nigeria.
Methods
This study adopted a descriptive cross-sectional design. Data were extracted from the most recent Nigeria Demographic and Health Survey (NDHS). The study analyzed a weighted sample of 12,140 rural women. The outcome variable was the intention to use modern contraceptives. The main explanatory variable was health service contacts with CHWs. Statistical analyses were performed at three levels with the aid of Stata version 14. Three multivariable regression models were estimated using an adjusted Odds Ratio (aOR) with a 95% confidence interval. Statistical significance was set at p < 0.05.
Results
Findings showed that more than a quarter (29.0%) of women intends to use modern contraceptives. Less than one-fifth (15.9%) of the women had health service contacts with CHWs. In Model 1, women who had health service contacts with CHWs were more likely to intend to use modern contraceptives (aOR =1.430, 95% CI: 1.212–1.687). Likewise, in Model 2, women who had health service contacts with CHWs had a higher likelihood of intending to use modern contraceptives (aOR = 1.358, 95% CI: 1.153–1.599). In Model 3, the odds of intention to use modern contraceptives were higher among women who had health service contacts with CHWs (aOR =1.454, 95% CI: 1.240–1.706).
Conclusion
In rural areas of Nigeria, health service contacts with CHWs are significantly associated with the intention to use modern contraceptives. Family planning programmers should leverage the patronage of CHWs for the purpose of family planning demand generation in rural areas.
Similar content being viewed by others
Background
The intention to use a modern contraceptive indicates the proportion of all women of reproductive age who are not currently using a modern method but have the intent to become modern contraceptive users in the future. This indicator is crucial to family planning programming particularly the family planning demand generation in Nigeria for two reasons. One, it provides information about the current level of non-use of modern contraceptives in the country. Evidence suggests that the non-use of modern contraceptives is not only high in Nigeria but also higher in rural areas [1], as well as in the northern parts of the country [2] compared to the urban and southern parts of the country. Two, it provides information about the extent to which current non-users plan to utilize modern contraceptives in the future. Such information drives the expansion of existing family planning service delivery to levels that anticipates and accommodate future demand for modern contraceptives. It also justifies the need for continued research focusing on the intention to use modern contraceptives among childbearing women.
In Nigeria, modern contraceptive prevalence remained low among young and older women of reproductive age [3, 4] and young and older men [5] though with substantial state and regional variations across the country [6, 7]. For instance, while modern contraceptive use was 12% among currently married women, the use was 28% among unmarried women [7]. Also, the prevalence rate was lower than 10% in northern Nigeria compared to more than 15% in southern Nigeria [2, 3, 8]. Furthermore, modern contraceptive use was 26% among currently married women in urban areas compared to 10% among a similar group of women in rural areas [7]. Evidence also shows that a high level of unmet need for contraception exists in the country [8, 9]. For instance, a recent study found that the unmet need for contraception exceeded 20% in many states of Nigeria. The 2018 Nigeria Demographic and Health Survey reported the unmet need for contraception to be 35% in Cross River State, 33% in Edo State, and 10% each in Anambra and Adamawa states [7].
These pose a significant threat to achieving the national contraceptive prevalence target as declared in the current national policy on population for sustainable development [10]. The policy seeks to increase the modern contraceptive prevalence rate to 27% by 2020, and successively gain an additional 2% increase yearly until 2030. The policy was built on the 2014 national family planning blueprint, which revised the national contraceptive prevalence goal from 36 to 27% by 2024 [11, 12]. The development of the national family planning blueprint was driven with a view to achieving these targets through improve family planning demand generation and service delivery, particularly in the rural areas of the country where the use of modern contraceptives is lower compared to the urban areas.
The family planning blueprint included sets of workable activities intended to generate more demand for family planning. This includes the development of the national family planning communication plan, the rejuvenation of the national health promotion forum, and the launching of the new family planning logo codenamed ‘the Green Dot’. These activities utilized several health and non-health resources such as health communication experts, media organizations, the national orientation agency, faith-based organizations, and existing health agencies. These activities have improved public awareness of family planning in the country [12]. Nevertheless, some health resources that could further enhance the adoption of modern contraceptives by current non-users are still underutilized in the existing framework. One such health resource is the pool of Community Health Workers (CHWs). This refers to individuals who live and work in rural and remote communities to provide basic health services [13, 14]. In Nigeria, there are four cadres of CHWs, namely, community health officers, community health extension workers, junior community health extension workers, and community resource persons [15]. The CHWs received limited health-related training certified by the Community Health Practitioners Registration Board of Nigeria. This enables CHWs to provide recognized specific primary health care both in a health facility and as well as in the community [16, 17], to support the services provided by skilled health personnel such as doctors and nurses/midwives, who in many instances are not readily available in rural and remote communities [18,19,20]. The range of duties performed by CHWs includes but is not limited to supporting maternal and child health [21,22,23,24], helping to control communicable and non-communicable diseases [25], treatment of endemic diseases [26], promoting adequate nutrition [27], providing support during outbreaks of pandemics [17, 28], home visits, referral of patients, and disease surveillance [29].
More importantly, studies in many developing countries have shown that CHWs are valuable for boosting contraceptive usage in rural communities [30,31,32]. In Nigeria, a recent study [33] based on the PMA2020 survey in six states investigated the positive impact of CHWs on modern contraceptive use among childbearing women in rural parts of the country. The study revealed that women visited by CHWs reported higher usage of modern contraceptives which corroborates an earlier finding in India that health workers’ outreach may influence intention to use contraceptives [34]. In recognition of the value of CHWs in boosting contraceptive prevalence in the country, the Nigeria National Council on Health [NCH] (2012) approved that community health extension workers be allowed to provide injectable contraceptives in communities, which is a practice already found to be impactful in other climes [35, 36].
In spite of the evidence of CHWs relevance to contraceptive usage in the country, studies have rarely examined whether in the absence of skilled health personnel such as doctors and nurses in rural and remote communities, the health service contacts of non-users with CHWs drive the intention to use contraceptives. This is important because, in many rural and remote communities of Nigeria, skilled health personnel is not readily available at health facilities in addition to other sundry challenges such as long distances to the facility, lack of essential drugs, and poverty [18, 20]. These challenges discourage the use of essential healthcare services in rural areas. The challenges are now aggravated by widespread insecurity of lives and properties in the country [37, 38] which has led to increasing non-availability of skilled health personnel in rural areas of the country. Some rural dwellers may thus be limited to contacting CHWs for antenatal, delivery, postnatal checks, family planning, and treatment of diverse ailments. Often the health service contacts take place in non-clinical spaces, and sometimes the CHWs visit homes, markets, and farmlands to provide health education and basic services to the people. Hence, if CHWs have sufficient training and education about modern contraceptives, the health service contacts with non-users could be an avenue to talk about family planning, clear misconceptions about family planning, and addresses other family planning concerns of the rural populace. The study, therefore, examines the extent to which health service contacts with CHWs are associated with the intention to use modern contraceptives among non-users in rural communities. Findings will provide further inputs for strengthening the family planning demand generation activities of the family planning blueprint. It will also shed light on how CHWs could contribute to the achievement of the national contraceptive targets sets for 2030 and 2050 in Nigeria.
Methods
Design and Data
This study adopted a descriptive cross-sectional design using a quantitative approach to determine whether the health service contacts of non-users with CHWS are associated with the intention to use contraceptives. The women’s datasets analyzed in the study were extracted from the 2018 Nigeria Demographic and Health Survey (NDHS). The 2018 NDHS is the current (seventh) round of the Demographic and Health Survey (DHS) program implemented in Nigeria by the National Population Commission (NPC) with the collaboration of related national agencies, and the technical support of the Inner-City Fund (ICF) obtained through the DHS Program [7]. The DHSs are conducted across developing countries to build national capacity for the production of demographic and health data, and to provide estimates of demographic and health characteristics required for the monitoring of the Sustainable Development Goals in the participating countries [39, 40]. The 2018 NDHS thus provides internationally comparable demographic and health information that remains valid until the next round of the DHS in 2023. Comprehensive information about the methodology of the 2018 NDHS has been published and made available in the public domain via https://dhsprogram.com/pubs/pdf/FR359/FR359.pdf.
Population and Sample
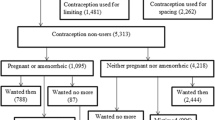
The 2018 NDHS covered 41,821 women of childbearing age. However, some of the women who were not relevant to the current study were excluded. Women excluded include all urban women (16,984), women currently using a method of contraception (8300), infecund women (572), and women who had health service contacts with skilled health personnel such as doctors and nurses/midwives (3121). Thus, the study analyzed a weighted sample of 12,140 women. This represents all women in the 2018 NDHS who were rural dwellers, reported CHWs as the provider of antenatal care, delivery, or postnatal care, and were not currently using a method of contraception. The sample was weighted using the weighting factors available in the dataset.
Research Variables
The outcome variable in the study was the intention to use modern contraceptives. This was derived from responses to the question: “Do you think you will use a contraceptive method to delay or avoid pregnancy at any time in the future?” The responses were in three categories, namely, intend to use later, unsure about future use, and do not intend to use modern contraceptives later. The study focused on women who were sure of their intention to use modern contraceptives later. We, therefore re-grouped the outcome variable into two categories, namely, ‘intend to use’ or ‘otherwise’. This measure was consistent with how the intention to use contraceptives was operationalized in existing studies [41,42,43,44]. The main explanatory variable in the study was health service contacts. This was measured among childbearing women who received antenatal care, delivery care, or postnatal care solely from any of the cadres of CHWs and not from skilled health personnel. The variable was grouped into two categories of ‘health service contact’ or ‘no health service contact’ Three other sets of explanatory variables were included in the analysis for the purpose of making the study findings robust.
One, eight individual demographic and social characteristics were examined. These are maternal age group (15–24, 25–34, and 35 years or older), timing of marriage (early - before 18 years or not early – 18 years or older), maternal education (none, primary, secondary, and higher), parity (primiparity [one child], multiparity [two to four children], and grand multiparity [five or more children]), working status (employed or unemployed), fertility desire (wants within 2 years, wants after 2 years, wants but unsure of timing, undecided, and wants no more) and, mass media exposure (low, moderate, and high). This was derived from the frequency of reading newspapers, listening to the radio, or watching television. A total of nine points was generated and subsequently divided into three equal parts to indicate low, moderate, and high exposure. Also, religion (Christianity, Islam, and others) was examined. Previous studies [42, 43, 45,46,47] have shown that these variables are important correlates of the intention to use contraceptives.
Two, six household characteristics were examined. These are household wealth quintile (poorest, poorer, middle, richer, and richest), partners’ education (none, primary, secondary, and higher), financial autonomy (autonomous or not autonomous), and healthcare autonomy (autonomous or not autonomous). Healthcare and financial autonomy were derived from responses to who had the final say on women’s own health and spending of the respondents’ cash earnings. Women who solely had the final say or jointly with partners were grouped as ‘autonomous’ and ‘not autonomous’ if otherwise. Safer sex negotiation (able to negotiate or unable to negotiate) was also included. Women who reported they could refuse sex from their partners or could ask partners to use a condom during intercourse were categorized as ‘able to negotiate’. The last household factor included was the decision-maker for the non-use of contraceptives (respondent, partner, joint, and others). These variables are included to reveal the power dynamics within the household in patriarchal societies such as Nigeria, which have been established in existing studies as important influencing factors on women’s use or non-use of modern contraceptives [48,49,50,51].
Three, some variables were selected for statistical control in the study. These are attitudes to wife-beating (not acceptable if the respondent did not justify wife-beating in any circumstance or acceptable if the respondent justifies wife-beating in specific circumstances), visitation by a family planning worker in the last 12 months (visited or not visited), pregnancy termination experience (never or ever experienced), and geo-political zone of residence. These variables have been linked to the intention to use modern contraceptives in previous studies [41, 42]. Pregnancy termination experience was included because evidence suggests that women who have experienced induced abortion, may develop an interest in the use of contraceptives especially when such women have been exposed to postabortion care and counselling [52, 53].
Data Analysis
Statistical analyses were performed at three levels with the aid of Stata version 14 [54]. At the first level, descriptive statistics were used to present sample characteristics and the intention to use modern contraceptives. At the second level, the explanatory variables were cross-tabulated with the outcome variable to assess variations in the intention to use contraceptives due to variations in the explanatory variables. Two bivariate analyses were further performed to select variables for inclusion in the final stage of data analysis. Firstly, a binary logistic regression using the unadjusted Odds Ratio (uOR) with a 95% confidence interval was used to assess associations between the explanatory and outcome variables. The control variables were excluded from the assessment. Only variables that reveal significance at p < 0.025 were selected.
Two, a Variance Inflation Factor (VIF) was performed to check the extent of multicollinearity among the variables. Variables were selected into the multivariable model on the basis of either showing significance by the estimates of the uOR or having a VIF score of less than ten. This was done to maintain the statistical principle that a variable with a VIF score of 10 or higher scores signifies the presence of multicollinearity [55]. At the third stage of data analysis, three multivariable regression models were estimated using an adjusted Odds Ratio (aOR) with a 95% confidence interval. Three models were estimated for the purpose of assessing the strength of health service contacts given the introduction of other variables into the successive models. Model 1 controlled for the individual demographic and social characteristics, while Model 2 controlled for the individual characteristics, and household characteristics. Model 3 was the full model which included all the research variables. Statistical significance was set at p < 0.05.
Results
Univariate Results
Table 1 presents the demographic and social profile of the respondents. More than a quarter (29.0%) of the respondents intends to use modern contraceptives later. Less than one-fifth of them (15.9%) had health service contact with CHWs, while the majority had no health service contact with CHWs. The proportions of women in older age groups were higher compared to the proportion in the younger age group of 15–24 years. The majority (71.6%) of the respondents reported early marriage while more than a quarter (28.4%) of the women reported otherwise. The proportion of the respondents with a desire for an additional child was high though those who desired to have another child within 2 years were slightly more than those who desired another child after 2 years. The majority of the women (63.3%) had no formal education. Also, the majority (65.3%) were employed at the time of the survey. More than half of the respondents (55.5%) had low mass media exposure. Likewise, more than one-third of them (37.7%) had moderate mass media exposure. Muslim women were dominant among the respondents. Nearly half (46.5%) of the respondents were grand multiparous.
Most of the women belong to either the poorest or poorer household wealth groups. The majority (62.3%) of respondents’ partners were not formally educated. While the majority (73.7%) of the respondents had no healthcare autonomy, more than half (54.7%) of them had no financial autonomy. Slightly more than two-fifths (42.1%) of the respondents were able to negotiate safer sex with partners. Though the proportion (30.1%) of respondents who were decision-makers for non-use of contraceptives was substantial, the proportion (28.8%) who reported joint decisions with a partner was equally substantial compared to the proportion (18.5%) whose partners decide their contraceptive non-use. The majority of the respondents were not visited by family planning workers in the last 12 months preceding the survey. Though more than half of the women rejected wife-beating under any circumstance more than two-fifths of them justified wife-beating. The majority of the respondents had never experienced a pregnancy termination. Women from the northern region particularly the northwest geo-political zone were preponderant in the sample.
Bivariate Results
Table 2 presents the bivariate findings. Health service contacts were significantly associated with the intention to use modern contraceptives with a higher proportion of the intention to use contraceptives among women who had health service contacts with CHWs compared to women who reported otherwise (38.6% vs. 27.2%). The intention to use contraceptives increased from 34.6 to 35.4% as the maternal age group increased from 15 to 24 years to 25–34 years but decline drastically to 19.5% among women in the advanced age group. The uOR at advanced maternal age (uOR = 0.459; 95% CI: 0.406–0.519) confirms a significant negative association between the maternal age group and the intention to use modern contraceptives. Though the intention to use modern contraceptives was lower among women who reported early marriage compared to those who reported otherwise (28.8% vs. 30.0%), the association was however not significant. Parity and the intention to use modern contraceptives were negatively associated. As women’s parity status was increasing from primiparity to multiparity and to grand multiparity, the intention to use modern contraceptives was declining steadily. With the exclusion of women who wanted no more children, the intention to use modern contraceptives was lower (25.3%) among women who wanted another child within the next 2 years compared to women who either wants after 2 years (38.6%), or were undecided (27.5%) or unsure (36.5%) of the timing of future fertility.
Maternal education was positively associated with the intention to use modern contraceptives with a consistent increase in the intention to use modern contraceptives as educational attainment improves. However, the level of intention to use contraceptives dropped as the educational level reached higher education. Working status was significant (uOR = 1.203; 95% CI: 1.072–1.349) and positively associated with the intention to use modern contraceptives with higher intention among employed compared to unemployed women (30.3% vs. 26.5%). Likewise, mass media exposure and the intention to use modern contraceptives were positively related to a consistent increase in the level of intention as exposure to mass media improves. Christian women reported a higher intention to use modern contraceptives compared to women in other religions. Except for the richest household wealth group, the intention to use modern contraceptives increase progressively as the household wealth group improves. This reveals a positive association. Also, the intention to use modern contraceptives increase with improvement in partners’ education but the level of intention dropped at higher educational attainment. While healthcare autonomy was positively associated with the intention to use a modern contraceptive, financial autonomy was negatively associated with the intention to use modern contraceptives. Safer sex negotiation relates positively to the intention to use modern contraceptives. In contrast, the association between decision-makers for the non-use of contraceptives and the intention to use contraceptives was inconsistent.
Multivariable Results
Table 3 presents further association of health service contacts and other characteristics with the intention to use modern contraceptives. In Model 1 which controlled for the individual demographic and social characteristics, the odds of the intention to use modern contraceptives were higher among women who had health service contacts with CHWs compared to the intention among women who had no health service contacts with CHWs (aOR = 1.430; 95% CI: 1.212–1.687). In the model, the timing of the first marriage was the only individual characteristic with no significant effect on the intention to use modern contraceptives. With the introduction of household characteristics into Model 2, two noticeable changes were observed. One, the odds of the intention to use modern contraceptives reduced from 1.430 in Model 1 to 1.358 in Model 2 though the odds remain higher among women who had health service contacts with CHWs compared to those who had no health service contacts (aOR = 1.358; 95% CI: 1.153–1.599). Two, religion no longer reveals a significant effect on the intention to use modern contraceptives. As also observed in Model 1, the timing of the first marriage did not show a significant effect on the intention to use modern contraceptives. Two of the household characteristics, namely, household wealth and healthcare autonomy had no significant effects on the intention to use modern contraceptives. In the full model (Model 3), health service contacts were strengthened by the inclusion of the control variables. Women who had health service contacts with CHWs were more likely to intend to use modern contraceptives compared to women who had no health service contacts with CHWs (aOR = 1.454; 95% CI: 1.240–1.706).
In the full model, all the individual demographic and social characteristics revealed a significant association with the intention to use modern contraceptives. While maternal age group and religion reduce the odds of the intention to use modern contraceptives, other individual characteristics, namely, the timing of first marriage, parity, fertility desire, maternal education, working status, and exposure to mass media increases the odds of the intention to use modern contraceptives. On one hand, two household characteristics, namely, household wealth and healthcare autonomy remained without statistical significance as observed in the previous model. On the other hand, other household characteristics, namely, partners’ education, financial autonomy, safer sex negotiation, and decision-maker for non-use of contraceptives reveal significant association with the intention to use modern contraceptives. Geo-political zone of residence was the only control variable that showed significant effects on the intention to use modern contraceptives with higher odds in the North-East and North-West compared to lower odds in the three Southern zones.
Discussion
This study examined the extent of the association between health service contacts with CHWs and the intention to use modern contraceptives in settings with limited access to skilled health personnel such as doctors and nurses/midwives. This study builds on existing works that have established the important roles of CHWs in boosting contraceptive prevalence [30,31,32, 36] and was carried out to provide more information on an additional initiative that may boost modern contraceptive usage in rural and remote communities of Nigeria in light of the grossly insufficient numbers of skilled health personnel in such communities [19, 20], which makes the CHWs an important provider of reproductive health services in such communities [13, 23, 24]. This presents an opportunity for family planning programmers to leverage the patronage of CHWs for the purpose of family planning demand generation by encouraging CHWs to use every health service contact with the rural populace to talk about family planning, clear family planning misconceptions, and provide enlightened information about the health concerns of family planning usage. Such initiative will go a long way to reduce the existing disparity not only between the rural and urban areas [1] but also current state and regional disparities [2, 6] in family planning knowledge and use in the country, and also accelerate the achievement of the national contraceptive targets sets for 2030 and 2050 in Nigeria [10].
The study found a 29.0% prevalence of the intention to use modern contraceptives. When compared to findings in existing studies, the prevalence revealed in the current study could be explained in two possible ways. One, the prevalence found is substantially lower than the 52.2, 44.11, and 44.1% respectively reported in three studies conducted outside Nigeria [41, 42, 44] which analyzed similar DHS datasets, and lower than the prevalence found in a Nigerian study [47] that also analyzed the NDHS dataset. It is possible to explain the differences in the prevalence by the group of women analyzed in the studies. While this study focused on rural women who only had health service contacts with CHWs, the other studies conducted outside Nigeria included all childbearing women, and the study conducted in Nigeria included parous women in both urban and rural areas of the country. The prevalence as found in this study may thus be expected to differ from those found in studies that covered larger groups of women. Two, the prevalence found in the current study also differs from the prevalence reported in an existing hospital-based study [43]. Usually, hospital-based studies covered a smaller proportion of childbearing women which often makes the result inconsistent with findings in population-based studies.
Notwithstanding, the prevalence of the intention to use modern contraceptives among non-users as found in this study represents a key opportunity for family planning demand generation in the country. Since CHWs mostly live in the community, they have an understanding of the reproductive norms and culture of the people. This makes them suitable for presenting family planning in a way that is sensitive to the culture, religion, and tradition of the indigenous people, particularly during health service contacts of rural women and may justify higher intention to use modern contraceptives as found among women who had health service contacts with CHWs in the study. The implementation of the family planning blueprint in Nigeria [11, 12] will become more effective by expanding the range of family planning services that CHWs may provide. Incidentally, the existing strategy in the country has empowered CHWs to administer injectable contraceptives [11] but more roles could still be assigned particularly in making resources available for more home visits and family planning outreach programs in rural communities. A recent study in Nigeria [33] confirmed that home visits of CHWs have a strong impact on the uptake of modern contraceptives, which indicates that the strategy is very useful for improving knowledge and the use of modern contraceptives. Though the intention to use modern contraceptives does not automatically translate to future use due to a number of health service factors such as inadequate health services providing contraceptive services, service provision bias, poor private sector participation, and ineffective supply chain management [12], once knowledge is improved, and the intention to use is established, actual use may not face difficult opposition.
Beyond health service contacts with CHWs, this study also found that individual demographic and social characteristics such as age, parity, maternal education, work status, mass media exposure, fertility desire, and religion are important drivers of the intention to use modern contraceptives. This provides support for findings in several existing studies conducted in Nigeria and elsewhere [41, 46, 47]. Also, the study revealed that several relational characteristics such as partners’ education, women’s financial autonomy, safer sex negotiation, and participation in household decisions may have a strong influence on the intention to use modern contraceptives in line with findings in previous studies [42, 43]. The import of these findings is that the socio-demographic context of rural women cannot be exonerated from poor use or non-intention to use modern contraceptives. In most rural communities of Nigeria, the social structure is largely patriarchal which subjugates women’s economic and reproductive lives to male authority. A social transformation of society through improved education and economic empowerment of rural women is a veritable platform for changing the family planning situation in rural and remote communities of Nigeria. This point has been stressed in previous studies [48,49,50,51] that call for increasing women’s empowerment to improve the sexual and reproductive health of women in developing countries.
Strengths and Limitations
The literature search confirms that the focus of this study has rarely been examined across developing countries where CHWs play important role in the provision of primary health care. The study thus expands the frontiers of knowledge about the relevance of CHWs in relation to improvement in modern contraceptive usage in rural communities. The use of the DHS datasets in the study provides a basis for the international comparability of the study methods and findings. The principal investigator will be willing to share the do file with any interested researcher to enhance its replication in other climes. It is also important to draw attention to the few drawbacks of the study. One, the health service contacts recognized in the analysis were limited to contacts for maternal healthcare services such as antenatal care, delivery, postnatal check for mothers, or postnatal check for a child. Health services contacts for other health issues were excluded. This was done to ensure that the women concerned are those susceptible to pregnancy and child delivery concerns which makes family planning a relevant matter to them. The inclusion of other health contacts may moderate the findings. Also, the data analyzed did not capture the possibility of some women contacting both doctors/nurses and CHWs, which may further moderate the findings. In addition, it is important to note that the study did not exclude women based on the recency of last delivery. This is important because the intention to use contraceptives as measured in the study focused on the likely future use of contraceptives and not necessarily the intention to use contraceptives after the last delivery.
Two, the cross-sectional nature of the analyzed data did not permit the establishment of cause and effect between health service contacts and the intention to use modern contraceptives. It, however, provides a significant association between them which is important for understanding how health service contacts relate to the intention to use modern contraceptives. Three, the application of the theory of planned behavior may have improved the study findings, however, the theory could not be applied due to the unavailability of variables that could appropriately measure most of the theoretical constructs. Finally, the study only considered a binary measure of health service contacts. The number of contacts was not captured in the analyses. Follow up studies may thus include the number of health service contacts as another exposure variable that may affect the intention to use contraceptives.
Conclusion
This study examined whether health service contacts with CHWs are significantly associated with the intention to use modern contraceptives among non-users in rural communities of Nigeria. The women’s datasets of the most recent Nigeria Demographic and Health Survey were analyzed based on a sample of 12,140 rural women. Findings from the analysis revealed that more than a quarter of the rural women intend to use modern contraceptives, and the odds of intention to use modern contraceptives were higher among women who had health service contacts with CHWs. In rural areas of Nigeria, health service contacts with CHWs are significantly associated with the intention to use modern contraceptives. This implies that family planning programmers should leverage the patronage of CHWs for the purpose of family planning demand generation in rural areas of Nigeria.
Availability of data and materials
Interested researchers and members of the public could access the dataset online at.
https://dhsprogram.com/data/dataset/Nigeria_Standard-DHS_2018.cfm?flag=1.
Abbreviations
- AOR:
-
Adjusted Odds Ratio
- CHWs:
-
Community Health Workers
- DHS:
-
Demographic and Health Survey
- FMoH:
-
Federal Ministry of Health
- NDHS:
-
Nigeria Demographic and Health Survey
- NPC:
-
National Population Commission
References
Ifeadike CO, Eze PN, Ugwoke U, Nnaji GA. Rural-urban differentials in family planning practices and determinants of use among men in Anambra state. Epidemiol Rep. 2015;3:5. https://doi.org/10.7243/2054-9911-3-5.
Babalola S, Oyenubi O. Factors explaining the North–South differentials in contraceptive use in Nigeria: a nonlinear decomposition analysis. Demogr Res. 2018;38(12):287–308. https://doi.org/10.4054/DemRes.2018.38.12.
Mercer LD, Lu F, Proctor JL. Sub-national levels and trends in contraceptive prevalence, unmet need, and demand for family planning in Nigeria with survey uncertainty. BMC Public Health. 2019;19:1752. https://doi.org/10.1186/s12889-019-8043-z.
Crawford EE, Atchison CJ, Ajayi YP, Doyle AM. Modern contraceptive use among unmarried girls aged 15–19 years in South Western Nigeria: results from a cross-sectional baseline survey for the Adolescent 360 (A360) impact evaluation. Reprod Health. 2021;18:6. https://doi.org/10.1186/s12978-020-01056-w.
Oyedele OJ. Gender, media, and contraceptive use in Nigeria: men need help, not women. J Int Women's Stud. 2021;22(5):266–83.
Lamidi EO. State variations in women’s socioeconomic status and use of modern contraceptives in Nigeria. PLoS One. 2015;10(8):e0135172. https://doi.org/10.1371/journal.pone.0135172.
National Population Commission (NPC) [Nigeria] and ICF. Nigeria Demographic and Health Survey 2018. Abuja, Nigeria, and Rockville: NPC and ICF; 2019. https://www.dhsprogram.com/pubs/pdf/FR359/FR359.pdf
Atchison CJ, Cresswell JA, Kapiga S, Nsanya MK, Crawford EE, Mussa M, et al. Sexuality, fertility and family planning characteristics of married women aged 15 to 19 years in Ethiopia, Nigeria and Tanzania: a comparative analysis of cross-sectional data. Reprod Health. 2019;16:6. https://doi.org/10.1186/s12978-019-0666-0.
Sinai I, Omoluabi E, Jimoh A, Jurczynska K. Unmet need for family planning and barriers to contraceptive use in Kaduna, Nigeria: culture, myths and perceptions. Cult Health Sex. 2020;22(11):1253–68. https://doi.org/10.1080/13691058.2019.1672894.
National Population Commission. National policy on population for sustainable development. Abuja: NPC; 2021.
Federal Ministry of Health. Nigeria Family Planning Blueprint (Scale-Up Plan). Abuja: FMoH; 2014. https://www.healthpolicyproject.com/ns/docs/CIP_Nigeria.pdf
Federal Ministry of Health. Nigeria Family Planning Blueprint (2020–2024). Abuja: FMoH; 2020. https://www.health.gov.ng/doc/Final-2020-Blueprint.pdf
Uzondu CA, Doctor HV, Findley SE, Afenyadu GY, Ager A. Female health workers at the doorstep: a pilot of community-based maternal, newborn, and child health service delivery in Northern Nigeria. Glob Health Sci Pract. 2015;3(1):97–108. https://doi.org/10.9745/GHSP-D-14-00117.
Okereke E, Ishaku SM, Unumeri G, Mohammed B, Ahonsi B. Reducing maternal and newborn mortality in Nigeria - a qualitative study of stakeholders’ perceptions about the performance of community health workers and the introduction of community midwifery at primary healthcare level. Hum Resour Health. 2019;17:102. https://doi.org/10.1186/s12960-019-0430-0.
Okwor T. Community Health Worker Programme in Nigeria. In: Paper presented at Charles Merieux Conference Room, Les Pensieres Center for Global Health, France; 2018. https://www.gtfcc.org/wp-content/uploads/2020/08/gtfcc-case-management-okwor-tochi.pdf.
Okoroafor SC, Ahmat A, Osubor M, Nyoni J, Bassey J, Alemu W. Assessing the staffing needs for primary health care centers in Cross River State, Nigeria: a workload indicators of staffing needs study. Hum Resour Health. 2022;19(Suppl 1):108. https://doi.org/10.1186/s12960-021-00648-2.
Olateju Z, Olufunlayo T, MacArthur C, Leung C, Taylor B. Community health workers experiences and perceptions of working during the COVID-19 pandemic in Lagos, Nigeria - A qualitative study. PLoS One. 2022;17(3):e0265092. https://doi.org/10.1371/journal.pone.0265092.
Aluko-Arowolo S. An exploration of health care delivery in rural areas of South Western Nigeria. KIU JHumanit. 2021;6(1):23–30.
Sayyadi BM, Gajida AU, Garba R, Ibrahim UM. Assessment of maternal health services: a comparative study of urban and rural primary health facilities in Kano State, Northwest Nigeria. Pan Afr Med J. 2021;38(320). https://doi.org/10.11604/pamj.2021.38.320.25214.
Nwankwo ONO, Ugwu CI, Nwankwo GI, Akpoke MA, Anyigor C, Obi-Nwankwo U, et al. A qualitative inquiry of rural-urban inequalities in the distribution and retention of healthcare workers in southern Nigeria. PLoS One. 2022;17(3):e0266159. https://doi.org/10.1371/journal.pone.0266159.
Sotunsa JO, Vidler M, Akeju DO, Osiberu MO, Orenuga EO, Oladapo OT, et al. Community health workers’ knowledge and practice in relation to pre-eclampsia in Ogun State, Nigeria: an essential bridge to maternal survival. Reprod Health. 2016;13(Suppl 2):108. https://doi.org/10.1186/s12978-016-0218-9.
Haver J, Brieger W, Zoungrana J, Ansari N, Kagoma J. Experiences engaging community health workers to provide maternal and newborn health services: Implementation of four programs. Int J Gynecol Obstet. 2015;130:S32–9. https://doi.org/10.1016/j.ijgo.2015.03.006.
Negussie A, Girma G. Is the role of Health Extension Workers in the delivery of maternal and child health care services a significant attribute? The case of Dale district, southern Ethiopia. BMC Health Serv Res. 2017;17:641. https://doi.org/10.1186/s12913-017-2590-8.
Olaniran A, Madaj B, Bar-Zev S, et al. The roles of community health workers who provide maternal and newborn health services: case studies from Africa and Asia. BMJ Glob Health. 2019;4:e001388. https://doi.org/10.1136/bmjgh-2019-001388.
Teshome DF, Balcha SA, Ayele TA, Atnafu A, Sisay M, Asfaw MG, et al. Trained health extension workers correctly identify high blood pressure in rural districts of northwest Ethiopia: a diagnostic accuracy study. BMC Health Serv Res. 2022;22:375. https://doi.org/10.1186/s12913-022-07794-w.
Enguita-Fernàndez C, Alonso Y, Lusengi W, Mayembe A, Manun’Ebo MF, Ranaivontiavina S, et al. Trust, community health workers and delivery of intermittent preventive treatment of malaria in pregnancy: a comparative qualitative analysis of four sub-Saharan countries. Global Public Health. 2021;16(12):1889–903. https://doi.org/10.1080/17441692.2020.1851742.
Adesoro O, Oresanya O, Counihan H, Hamade P, Eguavon D, Emebo C, et al. A feasibility study to assess non-clinical community health workers’ capacity to use simplified protocols and tools to treat severe acute malnutrition in Niger state Nigeria. BMC Health Serv Res. 2021;21:1102. https://doi.org/10.1186/s12913-021-07118-4.
Mickler AK, Carrasco MA, Raney L, Sharma V, May AV, Greaney J. Applications of the High Impact Practices in Family Planning during COVID-19. Sex Reprod Health Matters. 2021;29[1]:1881210. https://doi.org/10.1080/26410397.2021.1881210.
Musoke D, Nyashanu M, Bugembe H, Lubega GB, O’Donovan J, Halage AA, et al. Contested notions of challenges affecting Community Health Workers in low-and middle-income countries informed by the Silences Framework. Hum Resour Health. 2022;20:4. https://doi.org/10.1186/s12960-021-00701-0.
Scott VK, Gottschalk LB, Wright KQ, Twose C, Bohren MA, Schmitt ME, et al. Community Health Workers’ Provision of Family Planning Services in Low- and Middle-Income Countries: a Systematic Review of Effectiveness. Stud Fam Plan. 2015;46(3):241–61. https://doi.org/10.1111/j.1728-4465.2015.00028.x.
Brooks MI, Johns NE, Quinn AK, Boyce SC, Fatouma IA, Oumarou AO, et al. Can community health workers increase modern contraceptive use among young married women? A cross-sectional study in rural Niger. Reprod Health. 2019;16:38. https://doi.org/10.1186/s12978-019-0701-1.
Stephens MJ, Schrumpf LA, Nsarko NE, Baumgartner JN, Ohemeng-Dapaah S, Akosah E, et al. ‘I have a lot of faith in her’: Value of community health workers in addressing family planning in rural Ghana. Global Public Health. 2020;15(10):1509–21. https://doi.org/10.1080/17441692.2020.1762238.
OlaOlorun FM, Tsui AO. Effect of community health workers’ visits on uptake of modern contraception among rural women of reproductive age in Nigeria. Afr J Reprod Health. 2020;24(3):108–17. https://doi.org/10.29063/ajrh2020/v24i3.12.
Kumar A, Jain AK, Ram F, Acharya R, Shukla A, Mozumdar A, et al. Health workers’ outreach and intention to use contraceptives among married women in India. BMC Public Health. 2020;20:1041. https://doi.org/10.1186/s12889-020-09061-1.
Weidert K, Gessessew A, Bell S, Godefay H, Prata N. Community health workers as social marketers of injectable contraceptives: a case study from Ethiopia. Glob Health Sci Pract. 2017;5(1):44–56. https://doi.org/10.9745/GHSP-D-16-00344.
Mir AM, Khan K. Best Bets for Accelerating Family Planning in Pakistan. Brief Islamabad: Population Center Pakistan.
Akanmu AA, Salisu UO, Daramola OP, Ogunsesan AS, Fasina SO, Adejare JA, et al. The COVID-19 pandemic and insecurity: the furiousness in Nigerian communities. Urban Plan Transport Res. 2021;9(1):368–406. https://doi.org/10.1080/21650020.2021.1946420.
Yusuf A, Mohd S. Growth and Fiscal Effects of Insecurity on the Nigerian Economy. Eur J Dev Res. 2022. https://doi.org/10.1057/s41287-022-00531-3.
ICF International. Survey Organization Manual for Demographic and Health Surveys. MEASURE DHS. Calverton: ICF International; 2012.
United States Agency for International Development. The DHS Program and Health Surveys. USA: USAID; 2018.
Tiruneh FN, Chuang K-Y, Ntenda PAM, Chuang Y-C. Factors Associated with Contraceptive Use and Intention to Use Contraceptives among Married Women in Ethiopia. Women Health. 2016;56(1):1–22. https://doi.org/10.1080/03630242.2015.1074640.
Ahuja M, Frimpong E, Okoro J, Wani R, Armel S. Risk and protective factors for intention of contraception use among women in Ghana. Health Psychol Open. 2020;7(2):2055102920975975. https://doi.org/10.1177/205510292097597.
Gebeyehu NA, Lake EA, Gelaw KA, Azeze GA. The Intention on Modern contraceptive use and associated factors among postpartum women in public health institutions of Sodo Town, Southern Ethiopia 2019: an institutional-based cross-sectional study. Biomed Res Int. 2020. https://doi.org/10.1155/2020/9815465.
Gilano G, Hailegebreal S. Assessment of intention to use contraceptive methods with spatial distributions and associated factors among women in Ethiopia: evidence from EDHS 2016. Arch Public Health. 2021;79:109. https://doi.org/10.1186/s13690-021-00631-2.
Tekelab T, Sufa A, Wirtu D. Factors affecting intention to use long acting and permanent contraceptive methods among married women of reproductive age groups in Western Ethiopia: a community based cross sectional study. Fam Med Med Sci Res. 2015;4:158. https://doi.org/10.4172/2327-4972.1000158.
Wuni C, Turpin CA, Dassah ET. Determinants of contraceptive use and future contraceptive intentions of women attending child welfare clinics in urban Ghana. BMC Public Health. 2018;18:79. https://doi.org/10.1186/s12889-017-4641-9.
Solanke BL, Banjo OO, Oyinloye BO, Asa SS. Maternal grand multiparity and intention to use modern contraceptives in Nigeria. BMC Public Health. 2018;18:1207. https://doi.org/10.1186/s12889-018-6130-1.
Asaolu IO, Okafor CT, Ehiri JC, Dreifuss HM, Ehiri JE. Association between measures of women’s empowerment and use of modern contraceptives: an analysis of Nigeria’s demographic and health surveys. Front Public Health. 2017;4:293. https://doi.org/10.3389/fpubh.2016.00293.
Sougou NM, Bassoum O, Faye A, Leye MMM. Women’s autonomy in health decision-making and its effect on access to family planning services in Senegal in 2017: a propensity score analysis. BMC Public Health. 2020;20:872. https://doi.org/10.1186/s12889-020-09003-x.
Some SYM, Pu C, Huang S-L. Empowerment and use of modern contraceptive methods among married women in Burkina Faso: a multilevel analysis. BMC Public Health. 2021;21(1498). https://doi.org/10.1186/s12889-021-11541-x.
MacQuarrie KLD, Aziz A. Women’s decision-making and contraceptive use in Pakistan:an analysis of Demographic and Health Survey data. Sex Reprod Health Matters. 2022;29(2):2020953. https://doi.org/10.1080/26410397.2021.2020953.
Adinma ED, Adinma JIB-D, Eke NO, Iwuoha C, Akiode A, Oji E. Awareness and use of contraception by women seeking termination of pregnancy in south eastern Nigeria. Asian Pac J Trop Dis. 2011:71–5. https://doi.org/10.1016/s2222-1808(11)60018-2.
Borges ALV, OlaOlorun F, Fujimori E, Hoga LAK, Tsui AO. Contraceptive use following spontaneous and induced abortion and its association with family planning services in primary health care: results from a Brazilian longitudinal study. Reprod Health. 2015;12:94. https://doi.org/10.1186/s12978-015-0087-7.
StatCorp. Stata: Release 14. Statistical Software. College Station, TX: StataCorp LP; 2015.
Senaviratna NAMR, Cooray TMJA. Diagnosing Multicollinearity of Logistic Regression Model. Asian Journal of Probability and Statistics. 2019;5[2]:1-9. https://doi.org/10.9734/AJPAS/2019/v5i230132.
Acknowledgments
The authors appreciate MEASURE DHS and the National Population Commission (Nigeria) for granting prompt permission to download and analyze the datasets.
Funding
Not Applicable.
Author information
Authors and Affiliations
Contributions
BLS developed the concept. OOO and OEO modified the concept. BLS, OOO and AFA reviewed literature. BLS, AFA and OEO developed the do file for data analysis. BLS, OOO, and AFA interpreted the results. BLS and OEO discussed the findings. All authors proof-read the manuscript for spelling and grammar. All authors approved the submitted version of the manuscript.
Authors’ Information
BLS is an Associate Professor of Demography and Social Statistics. OOO and OEO are respectively Lecturer I and Senior Lecturer in the Department of Nursing Science. AFA is a doctoral graduand of Demography and Social Statistics.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All methods were performed in accordance with the relevant guidelines and regulations. The study was a secondary analysis of data collected in the 2018 Nigeria Demographic and Health Survey. ICF Review Board approved the survey protocol in the United States (ICF IRB FWA00000845). The National Health Research Ethics Committee of Nigeria also approved the protocol before its implementation in Nigeria (NHREC/01/01/2007). During the survey, participants provided both written and verbal informed consent. In addition, verbal and written informed consent was provided either by the head of household or by the male partner if married where a minor such as age 16 or less were selected for participation in the survey. A brief concept note of the study detailing the research methods was submitted online to Measure DHS for the purpose of getting authorization to download and analyze the data. Measure DHS granted the authorization without delay via a document from ICF. Additional ethical approval was not necessary and was not obtained since the data analyzed is available in the public domain. Analyses did not provide a link to any individual, household, or community.
Consent for publication
Not Applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Solanke, B.L., Oyediran, O.O., Awoleye, A.F. et al. Do health service contacts with community health workers influence the intention to use modern contraceptives among non-users in rural communities? Findings from a cross-sectional study in Nigeria. BMC Health Serv Res 23, 24 (2023). https://doi.org/10.1186/s12913-023-09032-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-023-09032-3