Abstract
Background
Many countries implementing pro-poor reforms to expand subsidized health care, especially for the poor, recognize that high-quality healthcare, and not just access alone, is necessary to meet the Sustainable Development Goals. As the poor are more likely to use low quality health services, measures to improve access to health care need to emphasise quality as the cornerstone to achieving equity goals. Current methods to evaluate health systems financing equity fail to take into account measures of quality. This paper aims to provide a worked example of how to adapt a popular quantitative approach, Benefit Incidence Analysis (BIA), to incorporate a quality weighting into the computation of public subsidies for health care.
Methods
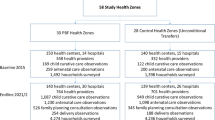
We used a dataset consisting of a sample of households surveyed in 10 provinces of Indonesia in early-2018. In parallel, a survey of public health facilities was conducted in the same geographical areas, and information about health facility infrastructure and basic equipment was collected. In each facility, an index of service readiness was computed as a measure of quality. Individuals who reported visiting a primary health care facility in the month before the interview were matched to their chosen facility. Standard BIA and an extended BIA that adjusts for service quality were conducted.
Results
Quality scores were relatively high across all facilities, with an average of 82%. Scores for basic equipment were highest, with an average score of 99% compared to essential medicines with an average score of 60%. Our findings from the quality-weighted BIA show that the distribution of subsidies for public primary health care facilities became less ‘pro-poor’ while private clinics became more ‘pro-rich’ after accounting for quality of care. Overall the distribution of subsidies became significantly pro-rich (CI = 0.037).
Conclusions
Routine collection of quality indicators that can be linked to individuals is needed to enable a comprehensive understanding of individuals’ pathways of care. From a policy perspective, accounting for quality of care in health financing assessment is crucial in a context where quality of care is a nationwide issue. In such a context, any health financing performance assessment is likely to be biased if quality is not accounted for.
Similar content being viewed by others
Background
Almost without exception, health systems worldwide provide health services that vary in terms of quality and access in ways that invariably favour higher income groups [1]. This occurs even in countries which have ostensibly achieved universal health coverage (UHC) and against a background of longstanding recognition of this type of disparity, countries are urged to ‘aim for affordable UHC and access for all citizens on the basis of equity and solidarity’ [2]. Nonetheless many low- and middle-income countries (LMICs) are implementing reforms to promote equity in health financing and delivery as a pathway towards UHC [3]. Measuring the distributional impact of these reforms is a high priority for these countries [4].
‘Benefit Incidence Analysis’, or BIA, is the traditional approach to estimating the distributional impact of government spending on health care [5]. It uses information on costs and the utilisation of health services to estimate the distribution of public spending across different socio-economic groups. BIA seeks to answer the question: who benefits from public expenditures on health care and by how much? Put differently, BIA measures by how much the income of a household would have to be raised if the household had to pay for the subsidized health services at full cost [6]. In practice, BIA studies estimate “benefits” or “public subsidies” to service users, who are typically ranked by socioeconomic status or some other variable of interest including geographical area, ethnic group or gender [7]. While BIA has traditionally focused on distribution of public sector subsidies, the analysis is increasing being extended to the private sector because of the growing and important role of the private health sector.
A key strength of a BIA is that it can provide a simple and transparent approach to assessing the extent to which public health spending benefits the poor. The approach, however, is not without its limitations. A key one that has been flagged by analysts is the failure to take account of variations in the quality of health services received by different individuals, leading to a potential under/over-estimation of the subsidy [8]. Increased evidence that the poorest segments of the population receive poorer quality of care [9], means that failing to take account of the quality of care in BIA could lead to a biased picture of who benefits most from government health spending.
Recently, Asante et al. attempted to address this critical methodological gap by introducing a quality score into the computation of BIA [8]. They developed a proxy measure for quality using area level deprivation indicators (availability of water, electricity, energy source for cooking, education, etc.). One limitation of their approach (acknowledged by the authors) is the use of deprivation indicators that are not directly related to health care quality. Second, they used area-level indicators by averaging the quality measures at the district level; this could not only mask variations in the quality of health services at the sub-district level, but most importantly across facilities used by individuals with varying socio-economic status (SES). In this paper, we address this important issue using data from linked household and primary health care facility surveys in Indonesia. We aim to provide a worked example of how to apply the quality-weighted BIA methodology using facility-level quality measures linked to individual utilization data.
Methods
Study setting
In 2014, Indonesia took a significant step towards UHC by implementing a comprehensive national social health insurance scheme, known as the Jaminan Kesehatan Nasional (JKN), to make health care available to its entire population [10]. The JKN brings together all major existing health insurance schemes under a single agency - the Social Security Agency for Health (BPJS-Health) - and was made mandatory for all Indonesians. Since the introduction of the JKN, Indonesia has made significant progress, moving from 46.5% of the population covered in 2014 to 83% as of May 2019 [11]. This makes the Indonesian Social Health Insurance (SHI) scheme one of the biggest single payer system in the world. Under the JKN, members must register with a contracted public and private primary care provider. The BPJS-Health pays these providers by capitation for outpatient services [11], and the capitation amount differs based on the total number of practitioners, the ratio of practitioners to beneficiaries, and operating hours.
Utilisation data
We used data from a cross-sectional household survey (ENHANCE Survey) of 7500 households conducted in 10 provinces of Indonesia at the beginning of 2018. Details of the sampling methodology have been published elsewhere (https://equityhealthj.biomedcentral.com). Individuals were asked about their health seeking behaviour, including the name of the private or public outpatient facilities they have visited in the previous month, their socio-economic background, as well as their health insurance status. Those who reported being enrolled in health insurance could fall into either of these categories: individuals considered poor whose insurance contribution is fully subsidised (JKN-PBI group), individuals who need to contribute either via their payroll or to self-enrol and pay premium contributions (JKN non-PBI group) and those enrolled in insurance schemes administered by the local government (Jamkesda group).
Health facility data
The sampling frame for the health facility survey was drawn from information provided by households in the ENHANCE Survey on the name of the primary health care facilities they visited in the previous month. Due to limited time and budget constraints, we could not collect information from all the facilities mentioned in the ENHANCE Survey. Instead, in each sub-district, we selected up to three facilities that were most frequently mentioned by respondents. All the facilities selected were under contract with BPJS-Health and receiving public subsidies (in the form of capitation payments) to provide services to JKN patients. These were either public health centres (Puskesmas), or private clinics. In each facility, the person in-charge was interviewed about general characteristics, infrastructure, and availability of supplies, equipment and drugs.
Cost data
To estimate the unit cost of health services, we used the JKN claims data for 2018 obtained from BPJS-Health and data on capitation payments made to primary health care facilities for the same year. We estimated that the unit cost of one visit in a public health centre was Rp 40,000 (~US$2.8), while a visit in a private clinic was Rp 60,000 (~US$4.2). Out-of-pocket (OOP) payments were derived from the household survey, where individuals were asked about the amount they spent during their last outpatient visit.
Measures of socio-economic status
We developed a standard asset-based measure of socio-economic status, using data on the ownership of a range of durable assets (e.g. car, refrigerator and television), housing characteristics (e.g. material of dwelling floor, roof and walls and main cooking fuel) and access to basic services (e.g. electricity supply, source of drinking water and sanitation facilities) [12]. While income and consumption are the most direct measures of socio-economic status, we used an asset-index in this study for its ease of data collection, ease of computation and applicability to the Indonesian context, where the size of the informal sector is high. Principal component analysis (PCA) was used to estimate wealth levels using the asset indicators [12, 13]. The basic idea of PCA is to replace a set of correlated variables with a set of uncorrelated “principal components” which represent unobserved characteristics of the population. The principal components are linear combinations of the original variables and the weights are derived from the correlation or covariance matrix (depending on whether the data have been standardised) [12]. It is assumed that the first principal component, which explains the most variance among the data, represents household wealth.
Measure of health care quality
Donabedian’s framework for assessing quality of care describes healthcare service delivery as a continuum that includes structure, process and outcomes [14]. According to Donabedian, structural quality consists of human and key material resources such as infrastructure, equipment, drugs, medical supplies, communication, and transport. Process quality assesses whether what is known to be “good” medical care has been applied. Evidence-based care includes systematic patient assessment, accurate diagnosis, provision of appropriate treatment and technical competence in the provisions of diagnostic and therapeutic procedures, continuity of care, and appropriate patient counselling. Health outcomes refer to the ultimate improvement of health in terms of recovery, restoration of functions and survival.
In this study, we measured structural quality through the use of a supply-side readiness (SSR) index. The indicators of SSR were derived from the Service Availability and Readiness Assessment (SARA) tool [15]. Among the many indicators collected as part of the SARA survey, the “general service readiness” section collects information on the potential of health facilities to provide basic health care interventions. Following the SARA methodology, indicators were classified into five general service readiness domains (basic amenities, basic equipment, infection prevention, essential medicines and diagnostic capacity) (Table 1) and coded as binary variables, 1 indicating the presence of the indicator as reported by the provider, and 0 indicating non-availability. Each domain was associated with a score based on the percentage of items available. For each facility, an overall SSR score comprised between 0 and 1 was calculated based on the mean score across the five domains.
Quality-weighted BIA
In this analysis, we restricted our sample to the individuals who could be linked to their health facility of choice, in which facility data was collected. The various steps and data required to conduct a BIA have been described in detail elsewhere [16, 17]. In traditional BIA, the unit subsidy received by each individual is represented by the unit cost incurred by the provider in delivering the service minus any fees paid by the user to the provider in using the service, that is:
Where Si is the subsidy captured by individual i at the facility visited, Ci is the unit cost incurred by the provider at the facility in providing the services to individual i, Fi is the total fee paid by individual i to the provider, qi is the quantity of services consumed within a month and ci, fi, si are the unit cost, fee and subsidy, respectively [18]. In cases where the computation of individual subsidies yielded negative figures, the values were set to zero. As unit costs vary between public and private facilities, individual subsidies must first be computed separately, and then the total subsidy computed as the sum of the subsidies for public and private health visits. Total subsidies were annualised by multiplying the monthly figures by 12. We first ran standard BIA using unadjusted subsidies by ranking households according to their level of wealth, and by estimating the distribution of the subsidies across income groups. Concentration curves (CCs) and concentration indices (CIs) were used to summarise the degree of inequality in the distribution of public health subsidies. Sampling weights have been applied to reflect the probability of each individual being sampled within each province, district, sub-district and village.
According to the Asante et al. framework, the quality-adjusted subsidies WSi can be expressed in the following way:
Where xi is the SSR score of the facility that individual i visited, and Si is the unadjusted subsidy from (1). The quality-weighted BIA was run using the quality-adjusted subsidies as above, and results were compared with the standard BIA approach.
Comparison with level of need
In traditional BIA, the distribution of public subsidies for health services is usually compared with the distribution of the need for health care in order to have a more complete picture of the degree of equity in the system [17]. Several national surveys in LMICs include questions on self-assessed health (SAH) that can be used to proxy health care need [19]. We therefore used a similar approach. In the ENHANCE survey, individuals were asked to rate their general health status. A four-point scale was developed with the following response options: “very good”, “good”, “bad” and “very bad”. Anyone who rated his/her health as ‘bad’ or ‘very bad’ was considered to be in need of health care. The distribution of unadjusted and quality-adjusted subsidies was then compared with the distribution of the need for health care, using SAH as a proxy for need.
Results
Table 2 describes the basic characteristics of individuals in our sample. In total, we managed to link 784 individuals with 51 health facilities they visited, which represents about 19% of all the individuals in the sample who reported seeking primary health care in the previous month. Table 3 describes the health facilities surveyed: 84% were public health centres, and 16% private clinics. 37% offered inpatient services, and about half were open 24 hours a day. The average catchment of a health facility was 35,000 persons. All facilities were contracted with the BPJS-Health and therefore provided subsidised services to JKN patients. Quality scores were relatively high across all facilities, with an average of 82%. Scores for basic equipment were highest, with an average score of 99% (range 60 to 100%) compared to essential medicines with an average score of 60% (range 20 to 85%).
Table 4 presents the distribution of unadjusted and quality-adjusted subsidies. For the unadjusted subsidies, we found that the distribution of subsidies in the public sector was pro-poor (CI = − 0.04), while the distribution of subsidies in the private sector was significantly pro-rich (CI = 0.37). The overall distribution of subsidies was slightly pro-rich, but the CI was not statistically significant (0.032). When adjusting for quality, we found that the distribution of subsidies in the public sector became slightly less pro-poor (CI = − 0.03), while the distribution of subsidies in the private sector became more pro-rich (CI = 0.48). Overall the pro-rich distribution of total subsidies became statistically significant (CI = 0.037).
Figure 1 compares the mean level of need with the distribution of subsidies across wealth quintiles. The level of need was highest among the poorest quintiles, and the distribution of public subsidies was not proportional to the distribution of the need for health care. In other words, the poorest groups in our sample did not receive their fair share of public subsidies when considering their level of need. The level of inequality was slightly higher when using quality-adjusted subsidies, but the magnitude was small.
Discussion
This study provides a worked example of how to apply a quality-weighted BIA methodology, and we summarise the main steps in Table 5 below. Our findings from Indonesia show that the distribution of subsidies for public primary health care facilities became less ‘pro-poor’ and subsidies for private primary health care facilities became more pro-rich after accounting for quality of care. The magnitude or the difference between the distributions of quality-adjusted and unadjusted subsidies was not large, and we believe that the gap between the two distributions is likely to be underestimated. As our measures of quality remain limited to structural indicators and do not include process or outcomes measures, we did not find large variations in quality across study sites though availability of essential medicines has the lowest score. More sensitive measures of quality and/or the inclusion of higher-level facilities such as tertiary care hospitals would have provided a more realistic picture of quality-adjusted subsidies in Indonesia, and potentially greater differences in quality-adjusted and unadjusted subsidies. Additionally, recent efforts to increase quality of care in Indonesia, such as accreditation of primary health care facilities, have certainly led to a standardisation of the basic level of infrastructure and equipment However, this study is aimed at illustrating in practice how to apply quality weights in BIA studies rather than producing precise quantitative estimates.
Indonesia has been the focus of few BIA studies [19]. The first study, published over 30 years ago, showed that primary health care was mildly progressive but hospital care was disproportionately used by the better-off [20]. Similar results were reported in 2001 [21]. A comparative analysis of Asian countries found that in Indonesia, the richest 20% of the population received more than 30% of the total subsidies, and that the distribution of health care utilisation was more pro-poor than the subsidy distribution [22]. The fourth study examined the marginal effects of decentralized public health spending on the benefit incidence, when the authority to manage public spending for health and other sectors was devolved to the district level [23]. This study found that increased public spending at the district level improved the targeting of public funds to the poor by increasing their utilisation of services and also their share of public expenditure. However, the authors concluded that effort to increase the use of health services by the poor was necessary, and that demand-side interventions, such as price subsidies or social health insurance, were needed.
To our knowledge, none of these studies took into account the quality of care that patients received. More recently, Sambodo et al. measured the benefit incidence of healthcare funding under JKN, taking into account regional variation in unit costs across districts [24]. As both primary and secondary care providers are paid prospectively and proportionally to the intensity of their activity under the JKN system, better-equipped service providers are more likely to receive larger provider payments. Sambodo et al. found that the distribution of benefits favoured the wealthier groups, but most importantly that standard BIA using national unit costs underestimates regional disparities in healthcare funding, and therefore underestimates the inequality in the benefit distribution. If one assumes that the variation in unit costs reflects the variations in quality of care (especially availability of basic amenities, basic medical equipment, essential medicines and diagnostic tools), then our findings are consistent with theirs in the sense that the level of inequality in the benefit distribution is underestimated if quality is not accounted for. However, this assumption is unlikely to hold if higher provider payments are not correlated with higher quality, but instead are reflective of higher level of inefficiency; hence the need to account for quality using robust measures.
A major strength of our analysis lies in the fact that we were able to link individuals with the facilities they visited. In most studies, data linkage is not possible at the individual level, since conducting a facility survey alongside a household survey can be resource-intensive. Some limitations should also be acknowledged. Due to time and budget constraints, only 51 primary healthcare facilities could be surveyed, and therefore data on quality was collected in only a fraction of health facilities that individuals in our survey visited in the previous month, making the picture incomplete. However, this study represents a methodological advancement by introducing quality weights into the BIA framework and we hope future studies will be able to validate these results with larger datasets. Another limitation is the use of supply-side readiness scores as a proxy for quality which do not take into account e.g. health systems responsiveness and people’s expectations [25]. Careful interpretation is needed since the concept of quality of care is considerably broader and more complex than the measure used here [26]. Inputs such as infrastructure, equipment, medicines, and diagnostic tests, are just one element or prerequisite to the provision of good quality care [27]. Finally, while concerns have been raised about the use of subjective measures of health care need, they tend to be more readily available to researchers than objective measures and have been validated in the analyses of inequalities in health [28].
From a methodological perspective, one of the challenges of accounting for quality of care in BIA is the lack of adequate data from LMIC settings or standardized measurement of quality, since incomplete and unreliable quality data are common, and they often poorly capture process and outcome measures of care [29]. Researchers often rely on secondary datasets made available through global agencies such as the WHO, World Bank or United States Agency for International Development. The Indonesian Family Life Survey, for example, conducts health facility surveys that incorporate various indicators, including structural and process indicators, which can be used to assess quality of care. However, quality data is collected in only a fraction of health facilities that individuals visited in the previous month, making the picture incomplete. Routine collection of quality indicators that can be linked to individuals are needed to enable a more comprehensive understanding of individuals’ pathways of care, including the quality of services they receive.
The implications of this study go beyond the methodological aspect. From a policy perspective, accounting for quality of care in health financing assessment is crucial in a context where quality of care is a nationwide issue. Recently, the World Bank conducted an assessment of a nationally representative sample of 686 Indonesian public and private primary health care facilities. Their report highlights significant gaps in the readiness of primary health care facilities to deliver a basic level of quality of care [30]. Additionally, large geographical inequalities in the quality of care were detected. In such a context, any health financing performance assessment is likely to be biased if quality is not accounted for.
Conclusion
Through this analysis, we have shown that accounting for quality in BIA studies may provide a more accurate picture of the level of inequality, since poor households may have no choice except to visit the lower quality health facilities in their communities. We recommend that future analysis looking at the level of inequality in the distribution of public health care subsidies should incorporate quality of care in order to get the most accurate picture of the health financing system. Table 5 provides ‘how to’ for future assessment of quality-adjusted BIA. Improvement of the method will lie in the scope of measurement (structural, process or outcomes) of quality of care using standardized indicators, as well as in the accuracy of linking individuals to the very facilities they reported visiting to avoid using area-level information. Policy should focus on strengthening and equalizing quality of care across all primary healthcare facilities, as recommended by the World Bank (World Bank Group, 2020).
Availability of data and materials
The datasets analysed during the current study are not publicly available since the data is still being analysed by the research team but are available from the corresponding author on reasonable request.
Abbreviations
- BIA:
-
Benefit-incidence analysis
- UHC:
-
Universal Health Coverage
- LMICs:
-
Low-and middle-income countries
- SES:
-
Socio-economic status
- JKN:
-
Jaminan Kesehatan Nasional
- SHI:
-
Social Health Insurance
- OOP:
-
Out-of-pocket
- PCA:
-
Principal component analysis
- SSR:
-
Supply-side readiness
- SARA:
-
Service Availability and Readiness Assessment
- CI:
-
Concentration index
- CC:
-
Concentration curve
- SAH:
-
Self-assessed health
- WHO:
-
World Health Organisation
References
Gwatkin DR, Bhuiya A, Victora CG. Making health systems more equitable. Lancet. 2004;364(9441):1273–80.
World Health Organization. Health systems financing: the path to universal coverage. Geneva: WHO; 2010.
Reich MR, Harris J, Ikegami N, Maeda A, Cashin C, Araujo EC, et al. Moving towards universal health coverage: lessons from 11 country studies. Lancet. 2016;387(10020):811–6. https://doi.org/10.1016/S0140-6736(15)60002-2.
Wiseman V, Asante A, Price J, Hayen A, Irava W, Martins J, et al. Ten best resources for conducting financing and benefit incidence analysis in resource-poor settings. Health Policy Plan. 2015;30(8):1053–8.
Selowsky M. Who benefits from government expenditures? A case study of colombia: Oxford Univ Press; 1979.
Martinez-vazguez J. The impact of budgets on the Poor: tax and benefit incidence. 2001.
Van de Walle D. Assessing the welfare impacts of public spending; 1998.
Asante A, Man N, Wiseman V. Evaluating equity in health financing using benefit incidence analysis: a framework for accounting for quality of care. Appl Health Econ Health Policy. 2020. https://doi.org/10.1007/s40258-020-00597-2.
Kruk ME, Gage AD, Arsenault C, Jordan K, Leslie HH, Roder-DeWan S, et al. High-quality health systems in the sustainable development goals era: time for a revolution. Lancet Glob Health. 2018;6:1196–252 Available from: https://linkinghub.elsevier.com/retrieve/pii/S2214109X18303863.
National Team for the Acceleration of Poverty Reduction. The Road to National Health Insurance (JKN). 2015.
Agustina R, Dartanto T, Sitompul R, Susiloretni KA, Achadi EL, Taher A, et al. Review Universal health coverage in Indonesia : concept , progress , and challenges. Lancet. 2019;393:75–102.
Filmer D, Pritchett LH. Estimating wealth effects without expenditure data-or tears: an application to educational enrollments in states of India. Demography. 2001;38(1):115–32. https://doi.org/10.2307/3088292 Available from: http://www.jstor.org/stable/3088292.
Vyas S, Kumaranayake L. Constructing socio-economic status indices: how to use principal components analysis. Health Policy Plan. 2006;21(6):459–68.
Donabedian A. Evaluating the Quality of Medical Care, vol. 83; 1966. p. 691–729.
World Health Organization. Service availability and readiness assessment (SARA) an annual monitoring system for service delivery: Implementation Guide, version 2.2. 2005.
O’Donnell O, van Doorslaer E, Wagstaff A, Lindelow M. Analyzing health equity using household survey data: The World Bank; 2008.
McIntyre D, Ataguba JE. How to do (or not to do) ... a benefit incidence analysis. Health Policy Plan. 2011;26(2):174–82. https://doi.org/10.1093/heapol/czq031 Epub 2010 Aug 4. PMID: 20688764.
Wagstaff A. Benefit incidence analysis: are government health expenditures more pro-rich than we think? Health Econ. 2010;21:351–66.
Asante A, Price J, Hayen A, Jan S, Wiseman V. Equity in health care financing in low- and middle-income Countries : a systematic review of evidence from studies using benefit and financing incidence analyses. PLoS One. 2016;11:1–20.
Van de Walle D, Nead K. Public spending and the poor – theory and evidence: The Johns Hopkins University Press; 1995.
Lanjouw P, Pradhan M, Saadah F, Sayed H, Sparrow R. Poverty , Education , and Health in Indonesia Who Benefits from Public Spending? 2001.
O’Donnell O, van Doorslaer E, Rannan-eliya RP, Somanathan A, Adhikari SR, Harbianto D, et al. The incidence of public spending on Healthcare: comparative evidence from Asia. World Bank Econ Rev. 2007;21:93–123.
Kruse I, Pradhan M, Sparrow R. Marginal benefit incidence of public health spending : evidence from Indonesian sub-national data. J Health Econ. 2012;31(1):147–57. https://doi.org/10.1016/j.jhealeco.2011.09.003.
Sambodo NP, Van Doorslaer E, Pradhan M, Sparrow R. Does geographic spending variation exacerbate healthcare benefit inequality? A benefit incidence analysis for Indonesia. Health Policy Plan. 2021;36(7):1129–39. https://doi.org/10.1093/heapol/czab015.
Mirzoev T, Kane S. What is health systems responsiveness? Review of existing knowledge and proposed conceptual framework. BMJ Glob Health. 2017;2(4):e000486.
Hanefeld J, Powell-Jackson T, Balabanova D. Understanding and measuring quality of care: dealing with complexity. Bull World Health Organ. 2017;95(5):368–74. https://doi.org/10.2471/BLT.16.179309 Epub 2017 Mar 20. PMID: 28479638; PMCID: PMC5418826.
Leslie HH, Sun Z, Kruk ME. Association between infrastructure and observed quality of care in 4 healthcare services : A cross-sectional study of 4 , 300 facilities in 8 countries. PLoS Med. 2017;(14):1–16.
Gerdtham UG, Johannesson M, Lundberg L, Isacson D. A note on validating Wagstaft and van Doorslaer’s health measure in the analysis of inequalities in health. J Health Econ. 1999;18(1):117–24.
Akachi Y, Kruk ME. Quality of care: measuring a neglected driver of improved health. Bull World Health Organ. 2017;95(6):465–72.
World Bank Group. Is Indonesia Ready to Serve? 2020.
Acknowledgements
The ENHANCE Study (Equity and Health Care Financing in Indonesia) was supported through the Health Systems Research Initiative in the UK, and is jointly funded by the Department of International Development, the Economic and Social Research Council, the Medical Research Council and the Wellcome Trust. The funders of this research were not involved in the study. The research would not have been possible without the time and support of all the families and field workers that took part in our household surveys, to them we are very grateful.
Funding
This research is supported by a grant from the Health Systems Research Initiative jointly funded by the Department of International Development, the Economic and Social Research Council, the Medical Research Council and the Wellcome Trust (MR/P013996/1).
Author information
Authors and Affiliations
Contributions
All authors, including AA, DS, AS, RF, QC, SK, DN, GP, EA, AH, LG, AM, VT, SK, HT, VW and MH contributed to the design of the study. MH analysed the data, drafted the manuscript which all authors commented on. All authors, including AA, DS, AS, RF, QC, SK, DN, GP, EA, AH, LG, AM, VT, SK, HT and VW read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Informed written consent was obtained from all subjects and ethical support has been granted by all relevant bodies: the University of Indonesia (Reference: 503/H2.F10/PPM.00.02/2017); London School of Hygiene & Tropical Medicine (Reference: 13773); and the University of New South Wales (Reference: HC17709).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Haemmerli, M., Asante, A., Susilo, D. et al. Using measures of quality of care to assess equity in health care funding for primary care: analysis of Indonesian household data. BMC Health Serv Res 22, 1349 (2022). https://doi.org/10.1186/s12913-022-08739-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-022-08739-z