Abstract
Background
Skilled health care is essential for the mother's and newborn's health and well-being during pregnancy, labor, and the postpartum period. This study aimed to analyze women's knowledge, attitudes, and practices while requesting competent assistance for maternity healthcare in Gesha District, Southwest Region of Ethiopia.
Methods
A community-based cross-sectional study design was conducted from September 20, 2021 to October 19, 2021. A total of 424 mothers participated in this study and a systematic sampling technique was used to select the respondents. The data were collected using a pretested and structured questionnaire. Statistical software SPSS-20 and R-4.1.2 were used to enter and analyze the data respectively. The factors associated with the prevalence of Knowledge, Attitude, and Practice in seeking Skilled Maternal Healthcare Services were identified using descriptive analysis and a binary logistic regression model.
Results
This study result revealed that the overall proportions of good knowledge, positive attitude, and good practice in seeking skilled maternal health care services were 39.15%, 37.5%, and 34.67% respectively. Estimated odds of having knowledge, attitude, and practice were as follows: for having age between 20–24 years at first pregnancy 1.859, 1.86, and 1.799; having a plan for pregnancy 2.74,2.315 and 2.579; mothers attended elementary education 2.337, 2.565 and 3.312; having maternal age 20–24 years 4.336,4.989 and 5.870; maternal age 25–29 years 2.917, 3.794 and 4.017; maternal age 35–49 years 2.837, 2.991 and 3.412; having husbands who had attended elementary education level 2.736, 2.542 and 2.134; secondary and above education 3.464, 3.360 and 2.508; rich mothers 2.261, 1.995 and 2.452; having antenatal care 4 times and above 2.606, 2.570, 2.682; having transportation access 1.921, 1.956 and 2.404; having media access 1.979, 2.171 and 2.715 respectively. The odds of having attitude and practice respectively were as follows: married 1.762, and 2.208; having medium wealth index 1.933 and 2.424. The odds of having previous pregnancy complications was 2.147 which significantly affect the practice of seeking skilled maternal care assistance.
Conclusions
This study discovered that the study participants' knowledge, attitude, and practice of skilled maternal health care are low. Associated factors included age at first pregnancy, planned pregnancy, maternal education level, husband’s education level, maternal age, antenatal care service visits, transport access, and access to media were found to significantly affect the knowledge, attitude, and practice of the respondents in seeking skilled maternal care assistance in common. The household wealth index was also associated with attitude. Pregnancy complications, current marital status, and household wealth index also significantly affect the practice of seeking skilled maternal care assistance. As a result of the findings, initiatives to increase women's knowledge, attitudes, and use of expert maternal health services in the research area are needed for women residing in rural areas.
Similar content being viewed by others
Background
The term "skilled maternal health services" refers to the medical care given to women before, during, and after childbirth which is given by a health professional with midwifery skills that can be provided at different levels (home, health centers, hospitals, and private sectors) [1, 2]. Access to skilled maternal health care services during pregnancy, labor, and the postpartum period is critical to the mother's and newborn's health and well-being. Maternal mortality and morbidity, on the other hand, continue to be major concerns [2]. Approximately 303,000 mothers died worldwide as a result of maternal causes during pregnancy, childbirth, and postpartum [3]. The developing world accounted for 99 percent (302,000) of maternal deaths worldwide, with Sub-Saharan Africa accounting for two-thirds (201,000) [4]. Ethiopia is one of the countries in Sub-Saharan Africa with one of the worst maternal death rates (MMR). MMR is 420 per 100,000 live births, according to the Ethiopian demographic health survey (EDHS) 2016 report [5].
Sustainable development goal (SDG) 3.1 aims to reduce maternal mortality to under 70 deaths per 100,000 live births by 2030 [6]. Only half of women in poor countries, on the other hand, get the healthcare they require. The Ethiopian government has made significant headway in lowering maternal death rates. According to the Ethiopian Demographic Health Survey, the maternal death rate has decreased from 676 per 100,000 live births in 2011 to 412 in 2016 [7]. Despite advancements in maternal healthcare, considerable barriers to access and low usage of maternal health services still exist. Only 62 percent, 28 percent, and 17 percent of Ethiopian women receiving competent antenatal care, skilled birth attendants, and postnatal care, respectively, received skilled antenatal care, skilled birth attendants, and postnatal care [7]. Maternal healthcare services are clearly the most critical interventions for preventing mother morbidity and mortality, yet simply having access to care is insufficient to enhance maternal health outcomes. In low- and middle-income nations, poor infrastructure, poor quality care, and inequality significantly hinder efforts to expand maternity services [8].
Maternal education and awareness of trained providers are constant determinants of prenatal care at the individual level [8,9,10,11,12,13]. Unplanned pregnancies and women who gave birth multiple times (multiparous) were less likely to seek antenatal care [14]. At the structural level, a lack of essential infrastructures such as transportation and telecommunications networks hampered access to antenatal care services [15,16,17]. Past research in Sub-Saharan Africa has found that education, primiparous women, previous antenatal care visits, and awareness of trained providers are all important predictors of skillful delivery [8,9,10,11,12, 18,19,20,21]. Other research, on the other hand, shows that multiparous has a favorable impact on institutional delivery [22, 23]. Furthermore, evidence suggests that antenatal care attendance, desired pregnancy, and birth difficulties are all important predictors of postnatal care service use [20, 24,25,26].
The Ethiopian government intends to reduce maternal mortality, infant mortality, and morbidity by strengthening maternal healthcare system interventions, which include increasing birth attendants, meeting unmet family planning needs, improving childbirth care quality, and increasing health system financing, but maternal mortality remains an unfinished issue that requires further investigation [27]. Even though several types of research have been undertaken in Ethiopia on the consumption of maternal health services [9,10,11, 18, 21, 28], few have addressed the women's level of awareness and attitude toward skilled maternity health care. As a result, the purpose of this study was to evaluate women's knowledge, attitude, and practice of skilled maternity care, as well as the factors that influence them, in a remote area in Gesha district, South West Regional State.
Description of the study area
Gesha is a district in the South West Region of Ethiopia. Part of the Keffa Zone, Gesha is bordered on the south by Bita, on the west by the Sheka Zone, on the north by the Oromia Region and Sayilem, and on the east by Gewata. Towns in Gesha include Deka. The northern part of Gesha was separated to create Sayilem district, the eastern part was added to Gewata district, and the southern part to Bita district. Based on the 2007 Census conducted by the CSA, this district has a total population of 85,104, of whom 41,441 are men and 43,663 women; 81,671 or 96% of its population are rural dwellers. The majority of the inhabitants were Protestants, with 44.62% of the population reporting that belief, 41.02% practicing Ethiopian Orthodox Christianity, and 13.25% of the population were Muslim.
Study design and setting
A community-based cross-sectional study was conducted with a quantitative data collection technique to assess knowledge, attitude, and practice on seeking skill assistance for maternal healthcare services and associated factors among women in rural parts of Gesha woreda. The actual data collection process was carried out from September 20, 2021 to October 19, 2021 (a one-month survey). All women who gave live birth or stillbirth in the last 2 years in rural parts of Gesha woreda were the study participants. The analytical Method of data analysis was used to combine the power of the scientific methods with the use of formal processes to solve the problems related to seeking skill assistance for maternal healthcare services.
Eligibility criteria
Women between 15–49 years of age, women with 2 years of post-delivery or stillbirth, Women, who were mentally and physically capable of being interviewed, and Women who were permanent residents were included in the study.
Women who were critically ill, could not talk or listen, and women who were caregivers but not the actual mother of the baby were excluded from the study.
The sample size determination
The required sample for this study was determined by using a single population proportion sample size calculation formula considering the following assumptions. 95% confidence interval (CI), 5% margin of error, and due to no prior studies done in the study area, the researcher took the maximum proportion which equals 50%.
α = 0.05 (level of significance) with 95% confidence interval.
P = estimated prevalence rate = 0.5
q = 1-p = 1–0.5 = 0.5
d = margin of error of 0.05
n = the sample size
Thus the sample size for this study was \(\mathrm{n}=\frac{{[1.96]}^{2}0.5[0.5]}{{0.05}^{2}}=384.16\approx 385\) with Contingency for non-response and incompleteness = 10%.
Therefore, the final sample size for this study was \(385+38.5=423.5\approx 424\)
Sampling procedures
Gesha woreda’s rural parts were selected purposely to find out factors related to maternal health care service and due to the accessibility of the service might be low compared to the counterparts who were from urban areas. For selecting respondents from the sampling frame of 424 eligible households, a systematic sampling technique was used. Systematic Sampling is a type of probability sampling method where random starting points with fixed intervals are used to select members from a larger population. The household in the direction of the tip of the pen was started with a nearby first. After a successful interview of each household, the interviewer continued to the immediate nearby household of the eligible woman until the required sample size was achieved in the study area. When two eligible women existed in one household, the one with recent birth was selected.
Measuring instruments
A questionnaire was adopted from previous similar studies [29] and also partly developed from various literature reviews that could address the objectives of the study [30]. The questions and statements were grouped and arranged according to the particular that they can address. After extensive revision, the final version of the English questionnaire was developed. An individual who was a graduate of English and knows the local language which is called “kafinoonoo” translated the English version to “kafinoonoo”. Another individual of similar ability then re-translated the final or the agreed “kafinoonoo” version of the questionnaire back to the English with the first to check for any inconsistencies or distortion in the meaning of words in the content of the instrument.
Operational definitions
Skilled assistance: refers to maternity services (antenatal care, Delivery care, and postnatal care) by a health professional with midwifery skills that can be provided at different levels (home, health centers, hospitals, private sector) by a skilled care provider [1, 31].
Skilled care providers: are health professionals (midwives, nurses, and doctors) who have been effectively educated and trained in the skills needed to manage normal (uncomplicated) pregnancies as well as in the identification, management, or referral of complications [1, 31].
Non-skilled providers include health extension workers (HEWs), traditional birth attendants (TBAs), and relatives or family members who cannot fulfill the definition of a skilled provider [1, 31].
Good knowledge and poor knowledge: Women who scored above the mean on knowledge assessment questions were judged to have good knowledge, while those who scored below the mean were considered to have poor knowledge about skilled maternal health services [30].
Positive and negative attitude: Attitude was measured by using the Likert scale (1 = strongly agree, 2 = agree, 3 = disagree, and 4 = strongly disagree). Participants with a positive attitude scored above the mean on the attitude evaluation questions, whereas those with a negative attitude scored below the mean. Practice (antenatal care, skilled delivery, and postnatal care utilization) was measured such that participants who respond above the mean of the practice assessment question were considered as having a good practice, and if below the mean they were considered as having poor practice [30].
Antenatal care (ANC): is a maternal healthcare service provided by skilled healthcare professionals to pregnant women which are provided throughout pregnancy to ensure the best health outcomes for both the mother and the newborn [32].
Postnatal care (PNC): is the care given to the mother and her newborn baby immediately after the birth and for the first six weeks of life [33]
Study variables
The outcome variables for this study were knowledge, attitude, and practice each of which has two categories (dichotomous). The outcome variables are denoted as \({\mathrm{Y}}_{\mathrm{i}}, {\mathrm{w}}_{\mathrm{i}},\mathrm{ and }{\mathrm{Z}}_{\mathrm{i}}\) for knowledge, attitude, and practice respectively.
where, \(\mathrm{i}=\mathrm{1,2},3\dots . 424\) which indicates the \({\mathrm{i}}^{\mathrm{th}}\) individual mother.
Explanatory variables for this study were Socio-demographic variables (maternal age, mother’s education level, marital status, husband’s education level, household wealth index, women occupation, and the number of children ever born); obstetric variables(age at first pregnancy, plan about the last pregnancy, previous pregnancy complication, and antenatal care follow up) and structural variables(transportation access and media access).
Data processing and analysis
After validating the data, the investigator entered the data using SPSS version 20 and exported it to R version 4.1.2 statistical software packages for data cleaning and analysis. Computer frequencies and summary statistics were used to describe the study population by variables of interest. Any errors identified at this time were corrected after revision of the original data using the code numbers and statistical commands. By including all significant factors from the univariate analysis with a significance level of 25%, a multivariable logistic regression analysis was performed [34, 35]. The degree of association between independent and dependent variables was analyzed by a multivariable logistic regression model using binary analysis with 95% CI.
Binary logistic regression is often applicable in a situation where the dependent variable is dichotomous such as the presence or absence of a particular event and the explanatory variables are of any type. The Bernoulli distribution for Bernoulli trial specifies probabilities P (Y = 1) = π and P(Y = 0) = 1- π, for which E (Y) = π.
The general model for binary logistic regression is as follows:
where: \({\mathrm{x}}_{\mathrm{i}}\) is an independent variable in the model, π: the probability of success, 1-π: the Probability of failure, \({\beta }_{o}\)is constant terms, \({\beta }_{i}\)is the coefficients/slope of the independent variable in the model.
Parameter estimation
The maximum likelihood and Wald tests were used for parameter estimation methods in fitting the logistic regression model [36].
The maximum likelihood estimates of the parameters could be obtained by maximizing the log-likelihood function form which is given by:
Since observing values of \(\mathrm{Y}\) say, \({\mathrm{Y}}_{\mathrm{i}}\mathrm{^{\prime}}\mathrm{s }(\mathrm{i}=1, 2\dots \mathrm{n})\) are independently distributed as Bernoulli, the maximum likelihood function of Y is given by:
The Wald test statistic
The Wald test is a way of testing the significance of particular explanatory variables in a statistical model [37]. Wald χ2 statistics are used to test the significance of individual coefficients in the model and are calculated as follows:
where se (β) is the standard error of regression coefficient β. W assumes chi-square distribution with one degree of freedom.
Model adequacy checking
The Hosmer and Lemeshow test is commonly used to test for assessing the goodness of fit of the model and allows for any number of explanatory variables [37]. The receiver operating characteristic curve has been considered a statistical tool to evaluate the performance of model adequacy and it is a common technique for judging the accuracy of the fitted binary logistic regression model [38].
Results
The goal of this study was to determine the prevalence of knowledge, attitude and practice, and associated factors among reproductive-aged women who gave birth within the last 2 years from rural Gesha woreda. To determine the prevalence and determinants of knowledge, attitude, and practice, descriptive and inferential analyses were employed.
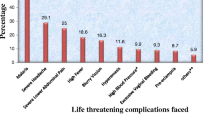
A total of 424 women participated in this study. The overall proportion of good knowledge, positive attitude, and good practice in seeking skilled maternal health care services were 39.15%, 37.5%, and 34.67% respectively with a 100% response rate (Fig. 1).
Among 130 women in the age group 15–19, 27(20.8%), 23(17.7%) and 19(14.6%) of them had good knowledge, positive attitude, and good practice in skilled assistance on maternal health services respectively. Of those mothers who were in the age group 35–49, 23(46.9%), 22(44.9%) and 21(42.9%) of them had good knowledge, positive attitude, and good practice toward skilled assistance in maternal care services respectively.
Among 196 mothers who had no formal education, above one-fourth (28.1%) had good knowledge, about one-fourth (25.5%) had a positive attitude and above one-fifth (21.4%) had good practice towards skilled assistance in maternal health services. Among 178 mothers who were never married, 55(30.9%), 51(28.7%), and about one-fourth 44 (24.7%) of them had good knowledge, positive attitude, and good practice respectively. Of those mothers whose husbands were in secondary and above education level, about half (48%), 35(46.7%), and 30(40%) of the mothers had good knowledge, positive attitude, and good practice of skilled assistance in maternal health service respectively. Regarding the household wealth index, only about one-third (32.9%) of poor mothers had good knowledge and above one-fourth (27.1%) of the respondents had good practice towards skilled assistance on maternal health services (Table 1).
Among 252 women whose first pregnancy was within the age group 15–19, 80(31.7%), 76(30.2), and 69(27.4) of them had good knowledge, positive attitude, and good practice toward skilled assistance in maternal care services respectively, like prenatal care and postnatal care. Of those mothers whose last pregnancy was not planned, above one-third (34.4%) of the respondents had good knowledge, about one-third (32.6%) had a positive attitude and only 29.8% of the respondents had a good practice. Regarding previous pregnancy complications, a total of 197 women had previous pregnancy complications and from which, 49.7%, 44.2%, and 43.7% of the women had good knowledge, positive attitude, and good attitude in seeking skilled assistance on maternal care services respectively. Among those mothers who attended the number of antenatal care service visits less than 4 times, only 29% had good knowledge, above one-fourth (27.4%) had a positive attitude and about one-fourth (24.7%) had good practice in seeking skilled assistance on maternal care service(Table 2).
Among those mothers who had no transport access, about one-third (32.9%) had good knowledge, less than one-third (31.4%) had a positive attitude and above one-fourth (27.9) had a good practice. Regarding media access, among those mothers who had no media access, 74(29.2%) had good knowledge, 27.3% had a positive attitude, and about one-fourth (23.7%) had good practice in seeking skilled assistance on maternal care services (Table 3).
Multivariable binary logistic regression results
Three separate binary logistic regression models were fitted for the three outcome variables such as knowledge, attitude, and practice. Explanatory variables which are significant at a 25% level of significance at a Univariable level were selected for multivariable binary logistic regression. A brief explanation of the results for each model was presented in the following sections.
Factors associated with knowledge in rural parts of Gesha Woreda, Kaffa, Southwest Ethiopia
Based on the multivariable binary logistic analysis, age at first pregnancy, plan for pregnancy, maternal education, Maternal age, Husband’s educational level, Household Wealth index, ANC, Transport access, and Media access were found to be significant factors to know seeking skill assistance of maternal health care service while marital status, pregnancy complication, women occupation and number of children were not significant variables at 5% level of significance.
Mothers whose first pregnancy was at age interval 20–24 were 1.859 times [95% CI: 1.119–3.087] more likely than those mothers whose first pregnancy was at age groups 15–19 to know seeking skilled assistance of maternal health care service. When compared to respondents who had no plan for the pregnancy, those who had a plan were 2.274 times [95% CI: 1.348–3.835] more likely to know the skilled assistance of maternal health care services. Regarding maternal education, mothers who had elementary education were a 2.337 [95% CI: 1.347– 4.052] times higher likelihood of knowing skilled assistance on maternal health care services compared to those who had no formal education. The finding also revealed that mothers in the age group 20–24, 25–29, and 35–49 were 4.336 [95% CI: 2.220–8.472], 2.917[95% CI:1.377–6.179] and 2.835[95% CI:1.186–6.773] times more likely to know the skilled assistance respectively as compared to their counterparts who were in the age group 15–19.
Holding effect other covariates constant, the odds of knowing the skilled maternal assistance for those respondents whose husbands had elementary and secondary &above were 2.736 [95% CI: 1.545–4.846] and 3.464 [95% CI: 1.693–7.089] times greater than those whose husbands had no formal education respectively. Respondents who were in the medium household wealth index were 1.854 [95%CI: 1.048–3.281] times more likely to know skilled health assistance than those who were in the poor household wealth index. According to the findings of this study, respondents who attended the antenatal care service visits four times and above were 2.606 [95% CI: 1.573–4.318] times more likely to know seeking skilled assistance than those who had visited the ANC service less than 4 times. Knowledge was 1.921 [95%CI: 1.154–3.197] times more common among respondents who had transportation access compared with those mothers who had no transportation access. Mothers who had media access were 1.979[95%CI: 1.173–3.339] times more likely to know the skilled maternal care assistance than those who had no media access (Table 4).
Factors associated with attitude in rural parts of Gesha Woreda, Kaffa, Southwest Ethiopia
Those mothers whose first pregnancy at age range 20–24 were 1.806 [95%CI: 1.086–3.005] times more likely to have a positive attitude regarding skilled maternal health care assistance compared to those mothers whose first pregnancy was at age interval 15–19. Women who had a planned pregnancy were 2.315 [95%CI: 1.367–3.922] times more likely to have a positive attitude towards skilled maternal health care assistance than an unplanned pregnancy. Mothers who had elementary education levels were 2.565 [95%CI: 1.472–4.470] times more likely to have a positive attitude in seeking skilled maternal health care assistance compared with those mothers who had no formal education. Married mothers were 1.762 [95%CI: 1.010–3.073] times higher chance to have a positive attitude in seeking skilled maternal care assistance compared to those mothers who were never married. Regarding age group, mothers in the age group 20–24, 25–29, and 35–49 were 4.989, 3.794, and 2.991 times more likely to have a positive attitude in seeking skilled maternal health care assistance than mothers in the age group 15–19 respectively. Husbands’ education level effect has a direct effect to have a positive attitude towards the service. Mothers whose husbands had elementary, and secondary &above education status were 2.542 and 3.360 times more likely to have a positive attitude toward getting skilled maternal care assistance compared to those mothers whose husbands had no formal education respectively. Mothers who had a household wealth index of medium and rich were 1.993 and 1.995 times more likely to have a positive attitude to service compared to their counterparts who were poor respectively. Women having greater than or equal to 4 ANC in their recent pregnancy were twice more likely to have a positive attitude toward skilled assistance as compared with those who visited antenatal care services less than 4 times were 2.570 [95%CI: 1.545–4.275]. Women who had access to transportation were 1.956 times more likely to have a positive attitude in seeking skilled maternal care services than those who had no transportation access 1.956 [95%CI: 1.168–3.275]. Mothers who had media access were 2.171 [95%CI: 1.278–3.687] times more likely to have a positive attitude towards skilled maternal care assistance compared to those mothers who had no access to media (Table 5).
Factors associated with practice in rural parts of Gesha Woreda, Kaffa, Southwest Ethiopia
Age at first pregnancy had a significant effect on practicing skilled maternal care assistance. Mothers whose first pregnancy was in the age range 20–24 were 1.799 [95%CI: 1.799–3.065] times more likely to practice skilled maternal health care service compared to those mothers whose first pregnancy was at age interval 15–19. Mothers who had a planned pregnancy were 2.579 [95%CI: 1.475–4.512] times more likely in practicing skilled maternal health care assistance than an unplanned pregnancy. Mothers who had elementary education levels were 1.840 [95%CI: 1.840–5.960] times more likely to practice skilled maternal health care assistance compared with those mothers who had no formal education. Married mothers were 2.208 [95%CI: 1.222–3.989] times more likely in practicing skilled maternal care assistance compared to those mothers who were never married. Mothers in the age group 20–24, 25–29, and 35–49 were 5.870, 4.017and 3.472 times more likely to practice skilled maternal health care assistance than mothers in the age group 15–19 respectively. Mothers whose husbands had elementary, and secondary &above education status were 2.134 and 2.508 times more likely to practice skilled maternal care service compared to those mothers whose husbands had no formal education respectively. Mothers who had a household wealth index of medium and rich were 2.424 and 2.452 times more likely to practice skilled maternal care services compared to the poor. Women having greater than or equal to 4 ANC in their recent pregnancy were 2.689 times more likely to practice skilled maternal service as compared with those who visited antenatal care service less than 4 times 2.689 [95%CI: 1.571, 4.600]. Women who had access to transportation were 2.404 times more likely to practice skilled maternal care services than those who had no transportation access 2.404 [95%CI: 1.395–4.143]. Mothers who had media access were 2.715 [95%CI: 1.539, 4.787] times more likely to practice skilled maternal care service compared to those mothers who had no access to media (Table 6).
Discussion
One of the primary causes of maternal morbidity and mortality around the globe is a lack of access to maternal health services [39]. This study is one of the first to clarify a prior disagreement between the findings of many studies on knowledge, attitudes, and practice about the use of competent maternity care services. Leaving these tensions unresolved at the individual level might lead to policymakers and program designers missing the target point of intervention. Furthermore, this research paints a clear picture of the problem of low utilization of competent maternal care services as a continuum of care from pregnancy to postpartum. As a result, this study looked into the factors that influence knowledge, attitude, and practice in competent maternal care, focusing on a rural setting. For many years in Ethiopia, skilled mother care services such as prenatal care (ANC), delivery care (DC), and postnatal care (PNC) were mostly available to the rural population [40].
This study enlisted the participation of 424 women from rural areas of Gesha woreda. Knowledge, attitude, and practice of seeking competent assistance were 39.15 percent, 37.75 percent, and 34.67 percent, respectively, indicating that maternity care from skilled providers is underutilized. This research corresponds to a study conducted in Ethiopia's Oromia Region's West Shoa Zone [30]. But this study is low as compared with different studies in different countries [22, 25, 41]. The reasons for this discrepancy could be explained by differences in sample sizes, time intervals, and socioeconomic conditions in the different contexts.
From the influencing factors, age at first pregnancy, planned pregnancy, maternal education level, husband’s education level, maternal age, antenatal care service visits, transport access, and access to media was found to be associated with the knowledge, attitude, and practice in common. The household wealth index was also associated with attitude. Pregnancy complications, current marital status, and household wealth index also significantly affect the practice of seeking skilled maternal care assistance.
Women whose age at first pregnancy ranged from 20 to 24 were more likely to know, have a positive attitude, and practice skilled maternal care assistance such as antenatal care, delivery care, and postnatal care than adolescents and young mothers. Our findings were similar to those of research conducted in rural Bangladesh and Ghana [42, 43]. This could be because teenage girls are trying to hide their pregnancy and are embarrassed to be examined by health care providers.
Women who planned their pregnancy were more probable to know, have a positive attitude, and seek antenatal care, delivery care, and postnatal care than those women who had no plan for the pregnancy. This finding is consistent with research conducted in Ethiopia and the Democratic Republic of the Congo, which found that women who had unplanned pregnancies were less likely to give birth in a health facility than moms who had planned pregnancies [14, 30]. This could be because unwanted pregnancies are connected with discouragement and a lack of pregnancy experience, thus they are less inclined to seek maternity care.
Women’s education was significantly associated with skilled maternal care assistance (antenatal care service, delivery care service, and postnatal care service) utilization. Women with elementary education were more likely to know, have a positive attitude, and practice maternal health care services as compared to women with no education. The findings of this study were in line with other studies in Africa [8, 9, 11, 12, 44, 45] which highlighted that utilization of maternal health services increases consistently as the educational level increases. It is understood that education is likely to enhance women's autonomy and they are near to information and would have good knowledge [46]. The higher use of competent delivery services among well-educated women may be due to their level of understanding, which may lead to women being more worried about their health and disease and seeking appropriate healthcare services.
Lack of husband education had an influential effect on skilled maternal care service in the current study. However, other studies which were done in Bangladesh and Benishangul Gumuz of Ethiopia have disproved this study [47, 48]. The possible disparities might arise from the fact that husbands are more conservative towards their cultural practice of home delivery and women are not autonomous both in Bangladesh and Benishangul Gumuz of Ethiopia regardless of their educational status. This could indicate that education alone may not be enough to influence husbands' behavior unless significant effort is made to modify their attitudes.
Women who had experienced pregnancy complications were found to have a significant association with practicing skilled maternal health care services. Other research in Ethiopia's Oromia area corroborates this conclusion [21]. Mothers who were exposed to media on the importance of skilled maternal healthcare services were more likely to know, have a positive attitude and practice the services. This finding supports the study done in Ethiopia [13]. The number of antenatal care visits tended to increase the utilization of skilled.
delivery. Mothers who had visited the number of ANC services four times and above were more likely to know, have a positive attitude, and practice skilled delivery and postnatal care compared with those who visited less than four times. This finding is consistent with the studies in Ethiopia, Tanzania, South Sudan, and Nepal, respectively [18, 20, 28, 49]. This could be because antenatal care is an important intervention in bringing women into contact with the health system, making skilled birthing more accessible, and providing postnatal care. This means that having frequent antenatal care visits is critical for increasing the use of facility-based delivery services.
The results of this study showed that, to a great extent, women in the rich wealth index group had positive attitudes and practiced ANC, DC, and PNC. Studies done in Ethiopia and Bangladesh Came up with the same results as that in the current study [50, 51]. Even in locations where maternity healthcare is given free of charge, women must pay for transportation and other necessities. As a result, women who couldn't afford these costs found it difficult, if not impossible, to visit health care institutions.
The finding of this study showed that women who had access to transport were more likely to know, have a positive attitude, and practice antenatal care, postnatal care, and delivery care services than those who had no transport access. This finding is in line with a study conducted in Ghana, Kenya, and Malawi, which found that the availability of vehicles such as public transportation and taxis influenced pregnant women's decisions to seek maternity care [17]. This suggests that antenatal care consumption is inextricably linked to basic infrastructure.
Conclusions
The study participants' knowledge, attitude, and practice toward skilled maternal health services are all low, according to the findings. Associated factors included age at first pregnancy, planned pregnancy, maternal education level, husband’s education level, maternal age, antenatal care service visits, transport access, and access to media were found to significantly affect the knowledge, attitude, and practice of the respondents in seeking skilled maternal care assistance in common. The household wealth index was also associated with attitude. Pregnancy complications, current marital status, and household wealth index also significantly affect the practice of seeking skilled maternal care assistance. As a result of the findings of this study, interventions to improve women's knowledge, attitude, and practice of skilled maternal health services in the study area are needed. Furthermore, unexpected pregnancy and a lack of mobility were both linked to a lack of use of maternal health services. As a result, the study recommends that integrated family planning and maternal healthcare services be revisited to help women with unexpected pregnancies access maternal healthcare services, as well as infrastructural improvements to improve access to maternal health services in rural areas of the country. Similarly, the use of competent delivery services is strongly linked to women's education. As a result, this research suggests that promoting equity among the excluded population is important.
Limitations of the study
There are certain limitations to the research. The study employed a cross-sectional study design, which has significant methodological limitations when it comes to determining cause and effect links between factors. Because the information gathered from the participants may be influenced by social desirability due to recall bias, the study seeks to mitigate this by adding only women who had given birth in the previous 2 years.
Availability of data and materials
The datasets used in this study are available upon reasonable request from the corresponding author.
Abbreviations
- ANC:
-
Antenatal care
- DC:
-
Delivery Care
- KAP:
-
Knowledge Attitude and Practice
- PNC:
-
Postnatal Care
- SPSS:
-
Statistical Package for Social Science
References
Carlough M, McCall M. Skilled birth attendance: what does it mean and how can it be measured? A clinical skills assessment of maternal and child health workers in Nepal. Int J Gynecol Obstet. 2005;89:200–8.
Taye BT, Kebede AA, Wondie KY. Intention to use maternal health services and associated factors among women who gave birth at home in rural Sehala Seyemit district: a community-based cross-sectional study. BMC Pregnancy Childbirth. 2022;22:1–12.
Kassebaum NJ, Barber RM, Bhutta ZA, Dandona L, Gething PW, Hay SI, Kinfu Y, Larson HJ, Liang X, Lim SS. Global, regional, and national levels of maternal mortality, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388:1775–812.
Organization WH. Strategies towards ending preventable maternal mortality (EPMM). 2015.
Tsegaye B, Ayalew M. Prevalence and factors associated with antenatal care utilization in Ethiopia: an evidence from demographic health survey 2016. BMC Pregnancy Childbirth. 2020;20:1–9.
Cf O. Transforming our world: the 2030 Agenda for Sustainable Development. NY, USA: United Nations New York; 2015.
Csace I. Ethiopia demographic and health survey 2016, Addis Ababa, Ethiop. Rockville, Maryland, USA: CSA ICF; 2016.
Dimbuene ZT, Amo-Adjei J, Amugsi D, Mumah J, Izugbara CO, Beguy D. Women’s education and utilization of maternal health services in Africa: a multi-country and socioeconomic status analysis. J Biosoc Sci. 2018;50:725–48.
Asfaw S, Assefa T, Tesfaye A, Mamo A. Patterns of skilled birth attendant service utilization and its determinants: a cross sectional study in southern Ethiopia. Sci J Public Heal. 2016;4:415.
Worku AG, Yalew AW, Afework MF. Factors affecting utilization of skilled maternal care in Northwest Ethiopia: a multilevel analysis. BMC Int Health Hum Rights. 2013;13:1–11.
Feyissa TR, Genemo GA. Determinants of institutional delivery among childbearing age women in Western Ethiopia, 2013: unmatched case control study. PLoS One. 2014;9:e97194.
Shigute T, Tejineh S, Tadesse L. Institutional delivery service utilization and associated factors among women of child bearing age at Boset Woreda, Oromia regional state, central Ethiopia. J Women’s Heal Care. 2017;6:420–2167.
BEKELE D, Birhanu A. Point prevalence and factors associated with institutional delivery among married women in reproductive age in Abe Dongoro Woreda, Horro Guduru Wollega zone, Oromia region, Western Ethiopia, Development. 13 (2016).
Ml AN, Dramaix-Wilmet M, Donnen P. Determinants of maternal health services utilization in urban settings of the Democratic Republic of Congo–a case study of Lubumbashi City. BMC Pregnancy Childbirth. 2012;12:1–13.
Ebu NI, Gross J. Factors influencing access to antenatal services and delivery care in sub-Saharan Africa. Afr J Midwifery Womens Health. 2015;9:58–65.
Asundep NN, Carson AP, Turpin CA, Tameru B, Agidi AT, Zhang K, Jolly PE. Determinants of access to antenatal care and birth outcomes in Kumasi, Ghana. J Epidemiol Glob Health. 2013;3:279–88.
Pell C, Meñaca A, Were F, Afrah NA, Chatio S, Manda-Taylor L, Hamel MJ, Hodgson A, Tagbor H, Kalilani L. Factors affecting antenatal care attendance: results from qualitative studies in Ghana, Kenya and Malawi. PLoS One. 2013;8:e53747.
Hagos S, Shaweno D, Assegid M, Mekonnen A, Afework MF, Ahmed S. Utilization of institutional delivery service at Wukro and Butajera districts in the Northern and South Central Ethiopia. BMC Pregnancy Childbirth. 2014;14:1–11.
Asweto CO, Ouma JO, Aluoch JR, Obonyo CO. Women empowerment and skilled attendance/facility delivery in a rural community of western Kenya. 2014.
Kanté AM, Chung CE, Larsen AM, Exavery A, Tani K, Phillips JF. Factors associated with compliance with the recommended frequency of postnatal care services in three rural districts of Tanzania. BMC Pregnancy Childbirth. 2015;15:1–10.
Fikre AA, Demissie M. Prevalence of institutional delivery and associated factors in Dodota Woreda (district), Oromia regional state, Ethiopia, Reprod. Health. 2012;9:1–6.
Dida N, Birhanu Z, Gerbaba M, Tilahun D, Morankar S. Modeling the probability of giving birth at health institutions among pregnant women attending antenatal care in West Shewa Zone, Oromia, Ethiopia: a cross sectional study. Afr Health Sci. 2014;14:288–98.
Dahiru T, Oche OM. "Determinants of antenatal care, institutional delivery and postnatal care services utilization in Nigeria." Pan Afr Med J. 2015;22(1).
Dhakal S, Chapman GN, Simkhada PP, Van Teijlingen ER, Stephens J, Raja AE. Utilisation of postnatal care among rural women in Nepal. BMC Pregnancy Childbirth. 2007;7:1–9.
Mohan D, Gupta S, LeFevre A, Bazant E, Killewo J, Baqui AH. Determinants of postnatal care use at health facilities in rural Tanzania: multilevel analysis of a household survey. BMC Pregnancy Childbirth. 2015;15:1–10.
Somefun OD, Ibisomi L. Determinants of postnatal care non-utilization among women in Nigeria. BMC Res Notes. 2016;9:1–11.
Woldemariam AT, Ababa A, Kwete XJ, Norheim OF, Bergen B, Verguet S. Avoiding premature mortality in Ethiopia 2015–30: a review of national mortality trends and policy recommendations.
Gebeyehu A, Kebede B, Andargie G. Use of previous maternal health services has a limited role in reattendance for skilled institutional delivery: cross-sectional survey in Northwest Ethiopia. Int J Womens Health. 2013;5:79.
Macro O, Hopkins J. Bangladesh Maternal Health Services and Maternal Mortality Survey, 2001, Dhaka, Bangladesh. Natl Inst Popul Res Train. 2003.
Girmaye E, Mamo K, Ejara B, Wondimu F, Mossisa M. Assessment of Knowledge, Attitude, and Practice of Skilled Assistance Seeking Maternal Healthcare Services and Associated Factors among Women in West Shoa Zone, Oromia Region, Ethiopia. Nurs Res Pract. 2021;2021:8888087.
Harvey SA, Ayabaca P, Bucagu M, Djibrina S, Edson WN, Gbangbade S, McCaw-Binns A, Burkhalter BR. Skilled birth attendant competence: an initial assessment in four countries, and implications for the Safe Motherhood movement. Int J Gynecol Obstet. 2004;87:203–10.
Organization WH. WHO recommendations on antenatal care for a positive pregnancy experience, World Health Organization. 2016.
McCauley H, Lowe K, Furtado N, Mangiaterra V, van den Broek N. Essential components of postnatal care–a systematic literature review and development of signal functions to guide monitoring and evaluation. BMC Pregnancy Childbirth. 2022;22:1–16.
Tareke SA, Lelisho ME, Hassen SS, Seid AA, Jemal SS, Teshale BM, et al. The prevalence and predictors of depressive, anxiety, and stress symptoms among Tepi town residents during the COVID-19 pandemic lockdown in Ethiopia. J Racial Ethn Health Disparities. 2022;1–13.
Hosmer DW, Hosmer T, Le Cessie S, Lemeshow S. A comparison of goodness-of-fit tests for the logistic regression model. Stat Med. 1997;16:965–80.
Agresti A. Categorical data analysis. John Wiley & Sons; 2003.
Hosmer DW, Lemeshow S, Sturdivant RX. Applied logistic regression. New York: Wiley; 2000.
Guisan A, Harrell FE. Ordinal response regression models in ecology. J Veg Sci. 2000;11:617–26.
Wang W. Levels and trends in the use of maternal health services in developing countries. ICF Macro, 2011.
Tsegaye B, Shudura E, Yoseph A, Tamiso A. Predictors of skilled maternal health services utilizations: a case of rural women in Ethiopia. PLoS One. 2021;16:e0246237.
Pathak P, Shrestha S, Devkota R, Thapa B. Factors associated with the utilization of institutional delivery service among mothers. J Nepal Health Res Counc. 2017;15:228–34.
Chakraborty N, Islam MA, Chowdhury RI, Bari W, Akhter HH. Determinants of the use of maternal health services in rural Bangladesh. Health Promot Int. 2003;18:327–37.
Addai I. Determinants of use of maternal–child health services in rural Ghana. J Biosoc Sci. 2000;32:1–15.
SulemanHassen S, MulatuTeshale B, Abate Adulo L. Identifying Factors Associated with Barriers in the Number of Antenatal Care Service Visits among Pregnant Women in Rural Parts of Ethiopia. Sci World J. 2021;2021:7146452.
Negero MG, Mitike YB, Worku AG, Abota TL. Skilled delivery service utilization and its association with the establishment of Women’s Health Development Army in Yeky district, South West Ethiopia: a multilevel analysis. BMC Res Notes. 2018;11:1–9.
Raghupathy S. Education and the use of maternal health care in Thailand. Soc Sci Med. 1996;43:459–71.
Weldemariam S, Kiros A, Welday M. Utilization of institutional delivery service and associated factors among mothers in North West Ethiopian. BMC Res Notes. 2018;11:1–6.
Yaya S, Bishwajit G, Ekholuenetale M. Factors associated with the utilization of institutional delivery services in Bangladesh. PLoS One. 2017;12:e0171573.
Mugo NS, Agho KE, Dibley MJ. Risk factors for non-use of skilled birth attendants: analysis of South Sudan household survey, 2010. Matern Child Health J. 2016;20:1266–79.
Mehari K, Wencheko E. Factors affecting maternal health care services utilization in rural Ethiopia: a study based on the 2011 EDHS data. Ethiop J Heal Dev. 2013;27:16–24.
Kamal SMM. Factors affecting utilization of skilled maternity care services among married adolescents in Bangladesh, Asian. Popul Stud. 2009;5:153–70.
Acknowledgements
The authors would like to express their gratitude to the study participants for their cooperation. They assert that Mizan-Tepi University has permitted them. The permission is primarily for the aim of efficient data collection.
Funding
No funding
Author information
Authors and Affiliations
Contributions
SS designed the study, participated in the data extraction, performed analysis interpreted results, and drafted the paper; ME revised the manuscript. Finally, all authors read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical clearance was obtained from the Ethical Review Board of Mizan-Tepi University, formal permission letters were taken from the administration of the Gesha Woreda and the Personal identity of the participants was not used to protect confidentiality. All methods were carried out following Helsinki guidelines and regulations.
Verbal informed consent was obtained from study participants before the start of data collection. The procedure for obtaining verbal informed consent from the participants was ethically approved by the Ethical Review Board of Mizan-Tepi University.
Consent for publication
Not applicable
Competing interests
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Hassen, S.S., Lelisho, M.E. Determining factors associated with the prevalence of knowledge, attitude, and practice in seeking skilled maternal healthcare services among women in a remote area of Gesha district. BMC Health Serv Res 22, 1318 (2022). https://doi.org/10.1186/s12913-022-08710-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-022-08710-y