Abstract
Background
There is growing evidence of variation in treatment for patients with depression, not only across patient characteristics, but also with respect to the organizational and structural framework of general practitioners’ (GPs') practice. However, the reasons for these variations are sparsely examined. This study aimed to investigate associations of practice characteristics with provision of depression care in general practices in Norway.
Methods
A nationwide cohort study of residents aged ≥ 18 years with a new depression episode in general practice during 2009–2015, based on linked registry data. Exposures were characteristics of GP practice: geographical location, practice list size, and duration of GP-patient relationship. Outcomes were talking therapy, antidepressant medication and sick listing provided by GP during 12 months from date of diagnosis. Associations between exposure and outcome were estimated using generalized linear models, adjusted for patients’ age, gender, education and immigrant status, and characteristics of GP practice.
Results
The study population comprised 285 113 patients, mean age 43.5 years, 61.6% women. They were registered with 5 574 GPs. Of the patients, 52.5% received talking therapy, 34.1% antidepressant drugs and 54.1% were sick listed, while 17.3% received none of the above treatments. Patients in rural practices were less likely to receive talking therapy (adjusted relative risk (adj RR) = 0.68; 95% confidence interval (CI) = 0.64–0.73) and more likely to receive antidepressants (adj RR = 1.09; 95% CI = 1.04–1.14) compared to those in urban practices. Patients on short practice lists were more likely to receive medication (adj RR = 1.08; 95% CI = 1.05–1.12) than those on long practice lists. Patients with short GP-patient relationship were more likely to receive talking therapy (adj RR = 1.20; 95% CI = 1.17–1.23) and medication (adj RR = 1.08; 95% CI = 1.04–1.12), and less likely to be sick-listed (RR = 0.88; 95% CI = 0.87–0.89), than patients with long GP-patient relationship.
Conclusions
Provision of GP depression care varied with practice characteristics. Talking therapy was less commonly provided in rural practices and among those with long-lasting GP-patient relationship. These differences may indicate some variation, and therefore, its reasons and clinical consequences need further investigation.
Similar content being viewed by others
Background
Depression is a leading cause of ill health and contributes greatly to years lived with disability [1], at high personal and societal costs. The Norwegian Institute of Public Health estimated that about 10% of the adult population will have a depressive episode over the course of a year [2]. However, there have been conducted no national diagnosis-based population surveys in Norway, yet.
The World Health Organisation (WHO) highlights the resilience of the primary care sector as an effective response to global challenges, including ageing populations, health inequalities, and increase in mental disorders [3]. Many European health authorities share a common vision of a strong, publicly funded primary health care system, with general practice as a cornerstone [4, 5]. To secure equal access and continuity of primary care, countries like Norway, the Netherlands, Denmark, and the UK have established list-based systems, with each citizen contracted to a specific general practitioner (GP) practice, and the GPs having fixed, personalized patient lists, and acting as gatekeepers to specialist health care [6]. Continuity of GP services is considered an important prerequisite for quality of care [7], and has been shown to improve patient outcomes regarding mental health [8].
In Norway, as in many other European countries, GPs are often the first health care professionals to whom depressed patients present, and thus play a key role in diagnosing and treating depression [4]. According to Norwegian and British national guidelines [9, 10], talking therapy by the GP is the first choice of treatment in mild to moderate depression. In moderate to severe depression, talking therapy combined with antidepressant medication should be considered, and GPs can refer patients to specialised mental care. Patient preferences are crucial regarding treatment decisions. A meta-analytic review across different settings yielded a 70% greater patient preference for psychological treatment over pharmacological treatment for depression [11].
Studies have shown that characteristics of GP practices may influence the provision of care. Urban GP practice location was associated with higher antidepressant prescription levels in France [12] and Scotland [13]. In terms of GP practice list size, the latter study showed lower prescription levels in practices with large list size [13], while a study from East London demonstrated the opposite [14]. However, these studies were conducted among GP practice populations without considering depression diagnoses. In Norway as in the rest of Europe, the impact of factors not directly related to patient characteristics or severity of disease on treatment is poorly documented [15]. Such knowledge may inform policy makers’ decisions on how to improve the organization of health care services.
The aim of this nationwide registry-based study was therefore to investigate associations of practice characteristics with provision of depression care in general practices in Norway.
Methods
Setting
In 2013, Norway’s 5.1 million inhabitants lived in 428 municipalities with populations ranging from about 200 to 634 000 people. The municipalities are classified according to Classification of centrality, describing their location in relation to urban settlements of various sizes [16]. Of the municipalities, 16% were urban (the largest cities in Norway), 44% in-between (small towns and larger settlements), and 40% rural (rural and remote rural areas) [17]. Of the Norwegian population, 43% lived in urban municipalities, 44% in in-between municipalities, and 14% in rural municipalities. All inhabitants have equal access to the primary and secondary public health services and prescription drugs (for example antidepressant drugs) covered by the National Insurance Scheme. In 2001, a national list-based system (the Regular GP Scheme) was implemented, giving all residents the right to have a GP, and to change GP twice a year. However, there is limited freedom of choice due to shortage of GPs, especially in rural areas. More than 99% of the population is registered with a specific GP, giving most patients good access to primary mental health care. Although, all GPs in Norway face the same regulations, such as payment systems and constraints, their practice characteristics may vary considerably. GPs are usually required to participate up to one day per week in other clinical or administrative tasks in the municipalities, such as primary care out-of-hours services, preventive health care in school, nursing home and prison. Some GPs are engaged in research and teaching activities, while others work part-time. Treatment in specialist health care by psychologist or psychiatrist requires a referral from the GP and is usually provided to patients with complex conditions, recurrent or severe depression. Access to specialist mental health care is limited and varies across treatment sites, but documentation at the national level shows no variation in waiting lists across urban–rural areas.
Design
We conducted a nationwide registry-based cohort study comprising all individuals with a new depression diagnosis recorded in general practice in 2009–2015. We examined associations between the characteristics of GP practices and the provision of GP depression care for 12 months from the date of the depression diagnosis.
Data sources
Information from national registries for the period 2008 through 2016 was linked at the individual patient- and GP-level, using the (encrypted) unique personal identification number assigned to all residents of Norway. Data was stored and analyzed in a safe server at the University of Bergen, Norway.
The source population comprised all inhabitants of Norway born before 1 January 1996 and alive 1 January 2008 (4,017,989 individuals), drawn from the Population Registry. We obtained information regarding individuals’ gender, year of birth, immigrant status and degree of urbanity, based on place of residence for all citizens. The Regular GP Registry provided information on all participating GPs and their listed patient population. We obtained information on GPs’ list size, i.e., the number of patients registered with the GP. We extracted the date of patients entering their GP’s list, from the start of the Regular GP Scheme in 2001, and eventually the date of patients leaving their GP’s list. The Control and Reimbursement of Health Care Claims (KUHR) database stores data on all fee-for-service claims from public primary care providers. For each contact with a GP during daytime, we obtained information on date of contact, diagnoses recorded according to the International Classification of Primary Care, 2nd version (ICPC-2), and reimbursement code(s) for diagnostic and therapeutic measures, as recorded by the GPs. The Norwegian Prescription Database (NorPD) contains information on all prescription drugs dispensed to individual patients treated in ambulatory care. For each prescription of an antidepressant drug, we extracted date of dispensing, generic drug information (Anatomical Therapeutic Chemical (ATC) code), and reimbursement code (drugs reimbursed by the Norwegian State for the treatment of depression). The National Education Database is based on the International Standard Classification of Education (ISCED 2011). We obtained information on the highest level of completed education.
Study population
The study population was established by first identifying all individuals aged 18 years or above with a depression diagnosis recorded in general practice (GP consultation with the ICPC-2 code P76 Depression in KUHR) during 01.01.2008–31.12.2015 (n = 443 803). Second, to establish a cohort of patients with a new depression diagnosis, we conducted washout of 146 226 patients with a depression diagnosis in general practice (P76 in KUHR) and/or specialist care (ICD-10 codes F32, F33, F34 or F41.2 in NPR) and/or dispensed antidepressant drug (ATC code N06A, referred by the Norwegian State for the treatment for depression in NorPD) during 12-month prior to index date. Only patients’ first depression episode during the study period was included (n = 301 577). Finally, we excluded 16 464 patients with missing information on GP practice characteristics or registered on GP patient lists smaller than 300 patients. We did so because these lists contained only a few patients and were probably created administratively or in start-up phase, with no proper functioning. The final study population comprised 285 113 patients, registered with 5574 GP practices.
Exposure
Exposures studied were characteristics of GP practices; geographical practice location, practice list size and duration of GP-patient relationship. Practice location was categorized as urban (the largest cities in Norway), in-between (small towns and larger settlements), and rural (rural and remote rural areas), with urban practice location as reference. Practice list size was categorized into quintiles (300–848, 849–1075, 1076–1238, 1239–1473, and 1474–2506 patients) based on list length for all GPs in 2012 (in the middle of the study period), with the longest list length as reference. Duration of GP-patient relationship was measured in years, from first date on current GP list until the date of depression diagnosis, categorized into 1–2, 3–4, 5–6, 7–8, 9–14 years, with the longest continuity as reference.
Outcome
Information on GP depression care linked to ICPC-2 code P76 Depression, provided during 12 months from the index date was identified. Types of GP depression care studied were talking therapy, antidepressant drugs, and certification of sickness absence. Talking therapy was recorded by identifying the reimbursement code for this measure in KUHR. The prerequisites for this reimbursement code were changed during the study period. A referral to secondary mental care was a requirement until July 2011, and until July 2014, this code could not be combined with the higher rewarding reimbursement code for a long consultation (> 20 min). From NorPD we included all dispensed antidepressant drugs (ATC code N06A) reimbursed for the treatment of depression prescribed by GPs and other doctors. In a previous study based on similar datasets, drug treatment for depression was initiated by a GP in 86% of cases [18]. Certification of sickness absence was recorded by identifying the reimbursement code for this measure in KUHR, and was only used for patients aged 18–66 years, because usual age at retirement in Norway is 67 years. All outcome variables were binary (yes, no).
Covariates
Gender was recorded as men or women. We recoded patient age into six groups: 18–29, 30–39, 40–49, 50–59, 60–69 and 70 + years. Educational level was recoded from 11 levels into three categories: low (primary school, grades 1–7, and lower-secondary school, grades 8–10, or less); medium (upper-secondary school, grades 11–13); and high (> 13 years, university, and higher education). Immigrant status was recoded into Norwegian-born or born abroad of foreign-born parents.
Statistical analyses
Descriptive statistics were used to examine the distribution of demographic variables in the study population and characteristics of GP practices. The Pearson’s correlation between practice list size and continuity was presented.
The provision of GP depression care during 12 months from date of diagnosis was analyzed as one treatment at the time, because we lack exact knowledge of whether patients receiving more than one treatment option did receive them simultaneously, as overlapping or consecutively. Associations between exposure (practice location, list size and continuity of care) and outcome (talking therapy, antidepressant drugs and sick leave certification) were analyzed with log binomial regression estimating relative risk (RR) with 95% CI. Due to problems with converge in a log binomial regression regarding talking therapy, Poisson regression with robust variance estimates (Zou, 2004), was applied to estimate RR and 95% CI. Crude estimates and estimates adjusted for patient characteristics and GP practice characteristics were presented for talking therapy, antidepressant drug and sick leave certification. In the regression analyses, age is used as a continuous adjustment variable. We decided to present list size and duration of GP-patient relationship in categories because it was easier to interpret the results and it was not obvious that there would be a linear relationship with the outcomes. However, when list size and duration were used as adjustment variables, they were used as continues variables. Since age can be a confounding factor for the association between duration of GP-relationship and talking therapy, age stratified corresponding models were applied in sensitivity analyses. For all statistical analyses, we used α = 0.05 as significant level. The data were analyzed by using STATA/SE version 16.1 (Stata Statistical Software).
Results
The study population comprised 285 113 patients (61,6% women) with a new depression episode in general practice, mean age 43.5 (SD = 16.3) years; the youngest age group (18–29 years) constituted the largest group with 24.2% of the cohort, and the oldest age group (70+) constituted the smallest group with 7.2% (Table 1). Educational attainment was high among 27.0% of the patients, medium among 41.2% and low among 31.8%. 11,7% were born abroad of foreign-born parents.
The patients in the study population were registered on 5 574 unique GP patient lists. GP practice location was distributed as urban (37.9%), in-between (45.5%), or rural (16.6%). GPs’ mean list size was 1 328 (SD = 379) patients and decreased with decreasing degree of urbanity (Table 2). The mean duration of the GP-patient relationship was 70 (SD = 50) months and was slightly shorter among patients in rural practices. Duration of GP-patient relationship increased with increasing list size (correlation coefficient = 0.29, p < 0.000).
Thirty-six percent has had the same GP for 9–14 years at date of depression diagnosis. The proportions among patients 40 years and older were 42% (40–49 years) and 49% (70 + years). Conversely, 27% of the patients younger than 40 years has had the same GP for only 1–2 years, with higher proportions in age groups 18–29 years (38%) and 30–39 years (28.9%) (not tabulated).
Of the patients, 52.5% received talking therapy, 34.1% antidepressant drugs, 54.1% were sick listed, and 17.3% received only GP consultation with none of the above treatment options. 42.3% of them received more than one treatment option during the 12-month follow-up period (Table 3).
In terms of treatment rates (percentage of patients receiving a treatment), talking therapy was more commonly provided to younger compared to older patients, to those with high compared to low educational level, and to immigrants compared to Norwegian-born. Regarding drug treatment, patients being male, older, low or medium educated, or immigrant, were more likely to receive antidepressants compared to their counterparts. Sick leave certification was more commonly provided to patients being female or highly educated (Table 4).
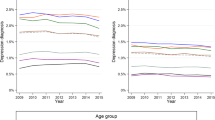
Patients living outside the largest cities in Norway were less likely to receive talking therapy when consulting their GP with a new depression episode (Fig. 1, Supplementary Table 1). This was particularly evident in the most rural parts of Norway [adj RR = 0.68 (0.64–0.72)]. We found a higher likelihood of receiving talking therapy among patients registered with GPs with medium list sizes compared to those on the longest lists. Regarding continuity of care, patients with a relationship to their GP lasting up to 6 years had a higher likelihood of receiving talking therapy compared with those having a long relationship (9–14 years). Adjusted RR for those with the shortest relationship was = 1.20 (1.17–1.23). Adjusting for patient characteristics and other GP list characteristics had limited impact on the likelihood of receiving talking therapy. Age stratified analyses gave similar results for both strata, 18–39 and 40 + years.
Rural practice was associated with a greater likelihood of being prescribed antidepressant drugs [adj RR = 1.09 (1.05–1.13)] compared to urban practice (Fig. 2, Supplementary Table 2). Further, shorter GP list sizes compared to longest list size, and shorter GP-patient relationship compared to longest relationship was associated with a greater likelihood of being prescribed antidepressant drugs.
Among patients at working age, less sick leave certification was associated with shorter GP-patient relationship. Adj RR for those with the shortest relationship (1–2 years) was = 0.88 (0.87–0.89) compared to longest relationship (9–14 years) (Fig. 3, Supplementary Table 3).
Discussion
Summary
In a nationwide cohort of patients with a new depression diagnosis in general practice in 2009–2015, we examined associations between GP practice characteristics and provision of GP depression care. Rural practice location was associated with less provision of talking therapy and more prescription of antidepressant drugs than urban practice location. Short patient lists slightly increased the likelihood of receiving medication compared to long patient lists. Short GP-patient relationship was associated with more talking therapy and antidepressant drugs, and less sick leave certification compared to long GP-patient relationship.
Strengths and limitations
The main strength of this study is the use of national registry data linked at the individual patient and GP level, providing a rich source of information, and eliminating recall bias. The almost complete data sets are another strength; information only regarding educational level was lacking for 1.4% (n = 4108) of the patients, with no expected impact on the results due to small numbers.
GP-registered new depression diagnosis was defined as a GP consultation with the ICPC-2 code P76, after a one-year washout period. The study population was restricted to patients whose depression was identified by a GP and recorded as such. Patients with depression who did not seek help or were not diagnosed with depression by the GP remained beyond the scope. Further, we lack information regarding severity because the ICPC-2 system does not allow for such grading. Consequently, we were not able to examine GPs’ guideline adherence. However, there is no reason to assume that severity of depression is unevenly distributed across the exposure variables. A limitation is that we study reimbursement codes recorded for payment purposes, not a report on what the GPs actually did. The prerequisites for the reimbursement code for talking therapy were changed during the study period. Further, this reimbursement code must be registered manually by the GP, in contrast to the reimbursement code for sick leave certification, which is registered automatically. Although we may have underestimated the prevalence of performed GP talking therapy sessions during the first years of the study period, this would apply for all GPs and cause “non-differential” misclassification. The NorPD contains complete data on prescription drugs dispensed. Although we may have slightly underestimated ‘prescribed’ antidepressants due to primary non-compliance, the use of drug dispensing data is recognized as an acceptable proxy for drug use in epidemiological studies [19]. Another limitation of the Norwegian registries is lack of other information that might explain practice variation, e.g., GPs’ experience and fields of interest, full-time-equivalent working as GP, treatment in specialist health care and/or municipal psychiatric services and waiting lists.
We measured continuity of care as the period from a person was registered on a given GP list to the date of depression diagnosis. Registration of GP-patient relationships in the RGP registry began with the establishment of the RGP scheme in 2001. This means that the study population, regardless of age at date of diagnosis, may have achieved maximum continuity between 9 years (index year 2009) and 14 years (index year 2015). The real continuity may be even longer because many patients chose the GP they previously went to (the "municipal doctor") as their “regular GP” in 2001; however, the possible implications on the study outcomes could not be examined due to lack of data.
We believe that the results of this study that started in 2009 are still valuable, because there haven’t been any healthcare reforms that may have impacted general practice care during this time frame. Whether the results of this study, shedding light on how practice characteristics affect service delivery in Norway, may be transferable to countries with similar organization of primary care and mental healthcare provision, such as UK, Sweden, Denmark, and the Netherlands remains to be clarified.
Interpretation of findings and comparison with existing literature
Geographical practice location
In the present study we found that rural practice location was associated with less provision of talking therapy and somewhat higher prescription of antidepressant drugs compared with urban practice location. These results are not in line with studies from general practice in Scotland [13] and France [12] which found lower levels of antidepressant prescribing for rural practices. However, the Scottish and French studies did not select GP practice populations on basis of depression diagnoses. Several factors may influence the geographical variation in drug prescribing. GP practices in rural areas compared to cities have a higher turnover of GPs [20], and relatively more patient lists are served by substitute/temporary doctors, who may be less experienced or competent in offering talking therapy. Another explanation could be a higher workload in rural practices [21] due to a general shortage of GPs in rural areas, and therefore less opportunity to offer follow-up with talking therapy sessions. Long distance to the GP practice may also contribute to less talking therapy, to the benefit of prescriptions of medication that is readily available. Considering rural populations, studies have found a high rate of barriers related to stigma, which may affect help-seeking behavior more in rural than urban residing patients [22, 23]. Patients postponing the visit to the doctor may become sicker and have a greater need for medication. Differences in behavior and demand between patients in urban and rural areas, as well as the doctors’ attitude, may therefore affect treatment decisions. Nevertheless, the question arises as to whether patients in rural areas in general have less access to talking therapy, reflecting inequity in depression treatment. This is concerning because guidelines emphasize psychological treatment as GPs’ primary tool in depression care [9]. Notably, a meta-analytic review across different settings yielded a 70% greater patient preference for psychological treatment over pharmacological treatment for depression [11].
Practice list size
Surprisingly, there was a slightly greater likelihood of receiving antidepressant treatment among patients on short GP lists, which contradicts the idea of a “high-prescriber” profile due to a greater workload among GPs with long patient lists. Our findings align with two studies from general practice in London [14] and Scotland [13]. However, these studies defined list sizes per full-time equivalent GP, in contrast to our study describing actual list size per GP. Regarding talking therapy, we found a slightly greater likelihood of receiving this treatment option with list size between 849–1473 patients compared to the longest list size, possibly explained by GPs with shorter lists have more time to offer talking therapy. We consider list size an appropriate proxy for GPs’ availability for their patients. In 2015, a list size of 300 patients corresponded to approximately one GP practice day a week. This may possibly explain why the shortest patient lists (300–848) were not associated with more talking therapy.
Continuity of care
Patients with a short GP-relationship had a higher chance of receiving talking therapy. At a national level, Norwegian GPs have increased the provision of talking therapy to patients with new depression over the last decade [21]. This trend is in accordance with recommendations from Norwegian and international guidelines [9, 10]. Nevertheless, findings from the current study give nuances to this picture by pointing to some variation in talking therapy by continuity of GP-patient relationship that is independent of patient characteristics. Regarding antidepressant treatment, patients with the shortest GP-patient relationship had a relatively higher chance of receiving medication. There are plausible explanations for these variations. A long GP-patient relationship requires physicians who remain in their GP practices over time and thereby have an accumulated knowledge and experience with their list patients, and their diseases and individual needs. Possibly, GPs with short GP-patient relationships are newly qualified doctors who are not yet familiar to their patients and, therefore, may be more willing to initiate medication and talking therapy than GPs with longer GP-patient relationships who possibly practice “wait-and-see” more commonly. GPs may not want to jeopardize the GP-patient relationship and be complaisant to patients’ request for a certain treatment, for instance antidepressant medication. However, this probably applies for all GPs and should not contribute to variation across continuity of care. Long GP-patient relationship (9–14 years) was more common among patients 40 years and older, while short GP-patient relationship (1–2 years) was more common among those younger than 40 years. It has been documented that referral rates to specialist health care among older patients in Norway and the UK were lower than for younger patients [24, 25]. Our analysis was adjusted for patients’ age, we also performed stratified analyzes by age, which gave similar estimates in both strata. Although continuity of care is regarded as an aspect of quality, our findings challenge the idea of long continuity being exclusively good for the patients. Long GP-patient relationship can possibly lead to doctors being less engaged to the patients, or, on the contrary, having a long GP-patient relationship and knowing your patients background may be a starting point for supportive talks instead of formalized talking therapy, and can possibly be therapeutic in itself. However, the findings still implicate inequality of opportunity to receive talking therapy across continuity of GP-patient relationship. Our findings as regards to lesser sick leave certification with short GP-patient relationship may possibly be explained by younger doctors being more restrictive with sick leave certification as national guidelines urges GPs to limit sick leave certification.
Conclusion
The Norwegian RGP scheme is considered a successful public service [26], with equitable health services for all inhabitants as a core value. Our findings point at some variation due to organizational and structural factors for patients with a new depression episode presented in general practice. Especially, differential treatment applies to talking therapy being less commonly provided in rural practices, and with long-lasting GP-patient relationship. Potentially poorer access to this core treatment modality may be relevant for the population group affected. Therefore, it should be of particular concern to health authorities and decision-makers, as a goal of securing the quality and equality of care regardless of practice characteristics. Although, the differences found in the present study are relatively small, they are relevant at a population level, given a national health policy aiming to provide equity in health care. Further studies are needed to explore the reasons for the observed differences and the implications for patient outcomes.
Availability of data and materials
The data used in this study are provided by Statistics Norway, the Norwegian Directorate of Health, and the Norwegian Institute of Public Health, with restrictions only to be used under licence for researchers in the current study, and so are not publicly available. However, the registry data used in this study will be available from the authors upon reasonable request and with included permission from Regional Ethical Committee for Medical and Health Research Ethics, Region West, Norwegian Data Protection Authority, Statistics Norway, the Norwegian Directorate of Health, and the Norwegian Institute of Public Health.
Abbreviations
- ATC:
-
Anatomical therapeutic chemical
- CI:
-
Confidence interval
- GLM:
-
Generalized linear model
- GP:
-
General practitioner
- ICD:
-
International classification of diseases
- ICPC:
-
International classification of primary care
- KUHR:
-
Control and reimbursement of primary health care claims database
- NorPD:
-
Norwegian prescription database
- NPR:
-
Norwegian patient registry
- RR:
-
Relative risk
- SD:
-
Standard deviation
- WHO:
-
World health organisation
References
GBD 2019 Mental Disorders Collaborators. Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Psychiatry. 2022;9(2):137–50.
Tesli MS, Handal M, Torvik FA, Knudsen AKS, Odsbu I, Gustavson K, et al. Public Health Report. Mental illness among adults. Folkehelseinstituttet. 2016. https://www.fhi.no/nettpub/hin/psykisk-helse/psykiske-lidelser-voksne/ Accessed 27 May 2022.
World Health Organization. The world health report 2008: primary health care now more than ever. World Health Organization. 2008. https://apps.who.int/iris/handle/10665/43949. Accessed 27 May 2022.
Verhaak PFM, van Dijk CE, Nuijen J, Verheij RA, Schellevis FG. Mental health care as delivered by Dutch general practitioners between 2004 and 2008. Scand J Prim Health Care. 2012;30(3):156–62.
Wang PS, Aguilar-Gaxiola S, Alonso J, Angermeyer MC, Borges G, Bromet EJ, et al. Use of mental health services for anxiety, mood, and substance disorders in 17 countries in the WHO world mental health surveys. Lancet Lond Engl. 2007;370(9590):841–50.
Sripa P, Hayhoe B, Garg P, Majeed A, Greenfield G. Impact of GP gatekeeping on quality of care, and health outcomes, use, and expenditure: a systematic review. Br J Gen Pract. 2019;69(682):e294-303.
Baker R, Freeman GK, Haggerty JL, Bankart MJ, Nockels KH. Primary medical care continuity and patient mortality: a systematic review. Br J Gen Pract. 2020;70(698):e600–11.
Puntis S, Rugkåsa J, Forrest A, Mitchell A, Burns T. Associations between continuity of care and patient outcomes in mental health care: a systematic review. Psychiatr Serv Wash DC. 2015;66(4):354–63.
Norwegian Board of Health. Nasjonale retningslinjer for diagnostisering og behandling av voksne med depresjon i primær- og spesialisthelsetjenesten (IS-1561). Oslo. 2009. [National guidelines for diagnosis and treatment of adults with depression]. https://www.helsebiblioteket.no/retningslinjer/psykisk-helse/depresjon-nasjonale-retningslinjer-for-diagnostisering-og-behandling-av-voksne-med-depresjon-i-primaer-og-spesialisthelsetjenesten?lenkedetaljer=vis. Accessed 27 May 2022.
National Institute for Health and Clinical Excellence (NICE), 2009. Depression in adults: recognition and management. Clinical Guidelince CG90. https://www.nice.org.uk/guidance/cg90. Accessed 27 May 2022.
McHugh RK, Whitton SW, Peckham AD, Welge JA, Otto MW. Patient preference for psychological vs pharmacologic treatment of psychiatric disorders: a meta-analytic review. J Clin Psychiatry. 2013;74(6):595–602.
Mercier A, Benichou J, Auger-Aubin I, Lebeau JP, Houivet E, Van Royen P, et al. How do GP practices and patient characteristics influence the prescription of antidepressants? A cross-sectional study. Ann Gen Psychiatry. 2015;14(1):3.
Morrison J, Anderson MJ, Sutton M, Munoz-Arroyo R, McDonald S, Maxwell M, et al. Factors influencing variation in prescribing of antidepressants by general practices in Scotland. Br J Gen Pract J R Coll Gen Pract. 2009;59(559):e25-31.
Hull SA, Aquino P, Cotter S. Explaining variation in antidepressant prescribing rates in east London: a cross sectional study. Fam Pract. 2005;22(1):37–42.
Lidal IB, Håvelsrud K, Mathisen M, Vist GE, Lidal IB. Listelengde og kvalitet i fastlegeordningen. Nasjonalt kunnskapssenter for helsetjenesten. [List size and quality of care among GPs within the regular general practitioner scheme]. Report from Kunnskapssenteret no. 01−2012. Oslo: Norwegian Knowledge Centre for the Health Services, 2012. http://www.ncbi.nlm.nih.gov/books/NBK464732/ Accessed 27 May 2022.
Andersen E. Classification of centrality. Statistics Norway; 2020. https://www.ssb.no/a/metadata/conceptvariable/vardok/927/en
Høydahl E. Ny sentralitetsindeks for kommunene. [New Index for Urbanization]. Stat Nor. 2017;50. https://www.ssb.no/befolkning/artikler-og-publikasjoner/_attachment/330194?_ts=15fdd63c098. Accessed 27 May 2022.
Hansen AB, Baste V, Hetlevik O, Haukenes I, Smith-Sivertsen T, Ruths S. GPs' drug treatment for depression by patients' educational level: registry-based study. BJGP Open. 2021;5(2):BJGPO-2020-0122.
Beardon PH, McGilchrist MM, McKendrick AD, McDevitt DG, MacDonald TM. Primary non-compliance with prescribed medication in primary care. BMJ. 1993;307(6908):846–8.
Abelsen B, Gaski M, Brandstorp H. Duration of general practitioner contracts. Tidsskr Den Nor Laegeforening Tidsskr Prakt Med Ny Raekke. 2015;135(22):2045–9.
Rebnord IK, Eikeland OJ, Hunskår S, Morken T. Fastlegers tidsbruk [GPs’ time use]. National Centre for Emergency Primary Health Care, Uni Research Helse, Bergen. Report to the Norwegian Board of Health, 2018. https://www.regjeringen.no/contentassets/e65a3259728c4d7a966ae53664c74da6/fastlegers_tidsbruk_180306.pdf. Accessed 27 May 2022.
Aisbett DL, Boyd CP, Francis KJ, Newnham K, Newnham K. Understanding barriers to mental health service utilization for adolescents in rural Australia. Rural Remote Health. 2007;7(1):624.
Fox JC, Blank M, Rovnyak VG, Barnett RY. Barriers to help seeking for mental disorders in a rural impoverished population. Community Ment Health J. 2001;37(5):421–36.
Ruths S, Haukenes I, Hetlevik Ø, Smith-Sivertsen T, Hjørleifsson S, Hansen AB, et al. Trends in treatment for patients with depression in general practice in Norway, 2009–2015: nationwide registry-based cohort study (The Norwegian GP-DEP Study). BMC Health Serv Res. 2021;21(1):697.
Walters K, Falcaro M, Freemantle N, King M, Ben-Shlomo Y. Sociodemographic inequalities in the management of depression in adults aged 55 and over: an analysis of English primary care data. Psychol Med. 2018;48(9):1504–13.
Nonseid J, Eide K. Innbyggerundersøkelsen 2017 - Hva mener brukerne? [Population Survey 2017 - What do the users think?] Difi-rapport 2017:7, ISSN 1890–583. https://dfo.no/sites/default/files/fagomr%C3%A5der/Rapporter/Rapporter-Difi/difi-rapport_2017_7_innbyggerundersokelsen_2017_hva_mener_brukerne_0.pdf. Accessed 27 May 2022.
Acknowledgements
We thank Tatiana Fomina at Biostatistics and Data analysis core facility (BIOS) at the University of Bergen for help in facilitating data.
Funding
Open access funding provided by University of Bergen. Research Council of Norway (Grant number 287884); Norwegian Research Fund for General Practice (PhD grant to SRI).
Author information
Authors and Affiliations
Contributions
SRI, SRU, VB, IH, ØH, and TSS defined the research question, designed the study, and interpreted the results. SRU and IH obtained approvals and acquired data. SRI and VB conducted the statistical analyses. SRI wrote the main manuscript text. SRI prepared all tables and figures. All authors reviewed the manuscript and approved the final version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Regional Committee for Medical and Health Research Ethics, Region West approved the project (2017/934). The Regional Ethical Committee for Medical and Health Research Ethics, Region West also waived the requirement of the informed consent for the study (2017/934/REK vest). The Norwegian Data Protection Authority approved the use of the data for research purposes in this project (17/01372–2/SBO). The register owners, Statistics Norway, the Norwegian Directorate of Health, and the Norwegian Institute of Public Health, approved linkage of registries. The data were pseudo-anonymized by third party (Statistics Norway) and analysed at group level to minimize the risk for backwards identification of individuals. All analyses were carried out, and methods were used in accordance with the relevant guidelines and regulations (declaration of Helsinki).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Supplementary Table 1. Likelihooda (crude and adjusted) of receiving talking therapy from GP (yes/no), among 285 113 patients with a new depression diagnosis in 2009-2015, by characteristics of GP practices. Supplementary Table 2. Likelihooda (crude and adjusted) of receiving antidepressant medication from GP (yes/no) among 285 113 patients with a new depression diagnosis in 2009-2015, by characteristics of GP practices. Supplementary Table 3. Likelihooda (crude and adjusted) of receiving sick leave certification from GP (yes/no), among 257 645b patients at working age with a new depression diagnosis in 2009-2015, by characteristics of GP practices.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Riiser, S., Baste, V., Haukenes, I. et al. Practice characteristics influencing variation in provision of depression care in general practice in Norway; a registry-based cohort study (The Norwegian GP-DEP study). BMC Health Serv Res 22, 1201 (2022). https://doi.org/10.1186/s12913-022-08579-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-022-08579-x