Abstract
Background
Caesarean section (C-section) delivery is an important indicator of access to life-saving essential obstetric care. Yet, there is limited understanding of the costs of utilising C-section delivery care in sub-Saharan Africa. Thus, we estimated the direct and indirect patient cost of accessing C-section in Tanzania.
Methods
Cross-sectional survey data of 2012 was used, which covered 3000 households from 11 districts in three regions. We interviewed women who had given births in the last 12 months before the survey to capture their experience of care. We used a regression model to estimate the effect of C-section on costs, while the degree of inequality on C-section coverage was assessed with a concentration index.
Results
C-section increased the likelihood of paying for health care by 16% compared to normal delivery. The additional cost of C-section compared to normal delivery was 20 USD, but reduced to about 11 USD when restricted to public facilities. Women with C-section delivery spent an extra 2 days at the health facility compared to normal delivery, but this was reduced slightly to 1.9 days in public facilities. The distribution of C-section coverage was significantly in favour of wealthier than poorest women (CI = 0.2052, p < 0.01), and this pro-rich pattern was consistent in rural districts but with unclear pattern in urban districts.
Conclusions
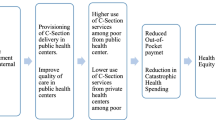
C-section is a life-saving intervention but is associated with significant economic burden especially among the poor families. More health resources are needed for provision of free maternal care, reduce inequality in access and improve birth outcomes in Tanzania.
Similar content being viewed by others
Background
Many country’s health systems are committed to achieve universal health coverage (UHC) goal to ensure healthy lives for all, under the Sustainable Development Goal three [1]. The UHC goal ensures that everyone has access to good quality health care without incurring financial hardship due to health care payment [2]. However, out-of-pocket (OOP) payment is a major means of financing healthcare in low- and middle-income countries (LMICs), which expose high proportion of households into poverty due to catastrophic healthcare expenditure [2,3,4]. Financing health care through direct OOP payments or user fees is typically regressive –i.e., the poorest are paying a relatively higher share of their income than their counterparts [3, 5,6,7]. The cost burden of health care also includes the indirect costs (e.g., time/ opportunity costs) which account for the loss in productivity due to medical illness [4, 8] and can equally limit access to health care as for direct costs [9,10,11].
The chances of incurring economic costs depend on many factors like the opportunity of accessing care, the existence of health financing policies which can ensure financial risk protection, and the nature of the illness. In terms of access, evidence shows that the direct financial costs are major barriers to access health care, which disincentive people to seek care [11,12,13]. Moreover, the health financing system which relies on OOP payments as opposed to prepayment mechanisms (e.g., tax funding and health insurance) often expose a large population, especially the low-income populations, into financial hardship due to medical spending [6, 14]. Similarly, the user fee exemption and waiver policy for the poor and vulnerable groups can potentially offer financial protection [15], but these policies are weakly enforced in many settings due to inadequate budgetary allocation to the health sector [16,17,18] as well as difficulties to identify the eligible clients [19, 20]. Lastly, the nature of illness also influences patients to incur economic costs –e.g., maternal obstetric complications are often unplanned and associated with large financial costs and productivity loss due to hospitalisation [8, 21, 22].
Several studies have examined the economic consequences of illness and associated coping mechanisms in LMICs [4, 23, 24], but not much has been reported in sub-Saharan Africa. For instance, the economic consequences of maternal illness/ obstetric care have been documented in Bangladesh [8, 22, 25,26,27], Nepal [28], Pakistan [29], and Argentina [30]. They generally found that maternal obstetric care (including C-section) was associated with higher direct costs and productivity loss. Knowledge about the economic costs of obstetric care remains limited in sub-Saharan Africa [31], despite the over-reliance on OOP payments for health services. Only a few studies in sub-Saharan Africa (e.g., [7, 17, 32,33,34]) shows that households are still incurring substantial direct costs for C-section delivery care irrespective of the exemption policy in those settings. These studies, however, hardly examined the indirect/ time costs of C-section due to hospitalisation, incremental costs of C-section after adjusting for covariates, and associated equity in C-section coverage.
In this paper, we provided the evidence on the estimates of both direct (OOP payments) and indirect cost (hospitalisation time) of C-section and normal delivery care in the context of free maternal health care in Tanzania. We also estimated incremental costs of C-section compared to normal delivery care and assessed equity in C-section coverage. Estimating costs of C-section in LMICs is preferred because C-section is an important indicator of access to life-saving essential obstetric care [35], and the burden of global maternal deaths is disproportionately higher in LMICs [36]. Both direct and time-related costs should be monitored to better understand the holistic view of cost burdens and barriers, especially in LMICs. Our findings are therefore relevant to inform policy discussions concerning health care financing for improved maternal and neonatal health outcomes and inform the discussions on financial protection towards achieving UHC.
Methods
Study setting
This study was conducted in three regions of Pwani, Morogoro and Lindi, out of 31 regions in Tanzania. These regions were considered because we used data from the evaluation of pay-for-performance (P4P) programme which was implemented in Pwani region, and used four districts from Morogoro and Lindi region for comparison [37, 38]. The population of Pwani region is just above a million, over two million in Morogoro region, and less than a million in Lindi region [39]. All seven districts in Pwani region were included in this study, and three districts from Morogoro and one district from Lindi were sampled. The country has made a lot of progress on child survival, but with little improvement in maternal health, which stands at 556 deaths per 100,000 live births [40, 41]. Access to one antenatal care (ANC) visit is almost universal, but relatively low coverage of institutional delivery (63%) and postnatal care (PNC) (33%) [40]. This reflects a marked imbalance along the continuum of maternal health care as reported elsewhere [42,43,44]. In 2016, the rate of C-section deliveries was 6%, and more likely among women who were wealthier, educated and residing in urban areas [40]. More than 70% of health facilities in Tanzania are publicly owned and are organised in a hierarchical administrative structure (i.e., dispensaries and health centres providing primary health care services, while up the rank there are district, regional, national and specialized hospitals that provide referral care).
The Tanzanian health financing system has multiple funding sources. In 2015/16 for example, the share of financing source to health care included general taxation (34%), donor support (36%), out-of-pocket payments (22%), and health insurance contributions (8%) [45]. In 2018/2019, about 9% of total government expenditure was allocated for health, which is below the Abuja declaration target of 15% [46]. About 34% of Tanzanians are covered by health insurance –i.e. 8% as public servants mainly through National Health Insurance Fund (NHIF), 25% as informal workers through Community Health Fund (CHF), and 1% from private insurance [46]. The coverage of health insurance is still low especially among the poor and informal workers. Tanzania has the exemption and waiver policies to protect the poor and vulnerable groups (e.g., pregnant women, children, and elders) [15, 47], but the enforcement of these policies has been weak such that exempted patients are still paying OOP [16, 48].
Data sources
Data for this study were collected as part of a larger project evaluating the impact of a P4P programme in Pwani region [37, 38]. We specifically used the baseline data of the evaluation study. The survey was done in all seven districts in Pwani region, three districts in Morogoro, and one district in Lindi region. The criteria for selecting the districts are presented elsewhere [38]. A cross-sectional survey of 3000 households was carried out in all 11 districts. Eligible household had a woman aged (15–49 years) who gave birth 12 months before the survey [38]. We included 150 facilities (12 hospitals, 32 health centres and 106 dispensaries) as the primary sampling unit, such that a random sample of 20 eligible households were drawn from each health facility’s catchment population [38]. The household survey was carried out by trained enumerators between January and February 2012. The structured questionnaire was administered to the household head and the eligible woman. The survey tool was designed to capture household background characteristics, and women’s experience of care specific for maternal and child health services, including associated direct and indirect costs. The survey tool was translated in Swahili and all the interviews were conducted in Swahili. A tool was pre-tested for consistency, relevance, and clarity before the actual survey.
Costs of health care
We measured both direct (OOP payments) and indirect costs (hospitalisation time) through the survey tool. Irrespective of the fee exemption policy or insurance coverage, women were asked whether she or anyone else paid for delivery care services received at a health facility. Those who acknowledged paying were asked the following questions: ‘How much did you pay in total excluding the cost of transport to reach the facility? (In Tanzanian shillings, TZS)’ and ‘How long did you spend in the health facility from time of arrival to time of departure? (in hours)’. Thus, through these two questions, we estimated direct and indirect costs, respectively. The direct costs excluded transport costs and were often paid for a consultation fee, drugs, medical supplies, laboratory tests, inpatient costs, informal payment/ gift to the health worker, or operation costs. Time costs were reported in terms of hours and then converted into days; while direct costs were reported in a local currency, Tanzanian shilling (TZS), and then converted into US dollar (USD) using the approximate exchange rate during the survey in 2012 (1 USD equal 1600 TZS).
Statistical analysis
We first performed a descriptive analysis of the costs and background characteristics of respondents by mode of childbirth. Women were classified into two main groups: (i) those with normal delivery, and (ii) those with C-section delivery. The differences in costs and background characteristics by mode of childbirth were computed and tested whether those differences were significantly different from zero by using t-tests. To estimate the effect of C-section on costs, we applied a series of regression models by accounting for various households’ and women characteristics. The following regression model was estimated:
where Yit is the cost incurred by individual i and Di is an indicator dummy for woman delivered by C-section. We controlled for individual and household-level covariates Xi (age, marital status, religion, parity, education level, occupation, insurance status, household size, household wealth status, and place of residence). The error term is εi. We clustered the standard errors at the facility level, or facility catchment area, to account for serial correlation of εi at the facility level. The effect of C-section childbirth on costs is given by β1. The reference group in this analysis is women who had a normal delivery. Our analysis was performed for all women with facility birth (85.8%) as well as for those who delivered in public facilities only (77.3%) (since fee-charging is typical in private facilities).
Given that cost data are typically skewed, with non-normal distribution, we also normalised our data by applying logarithm transformation [49]. We generated a variable using the following formula: In (1 + cost), in order to account for zero payments. Thus, we re-estimated our models using ordinary least-squares (OLS) for logged dependent variables –i.e., ln(Yi).
We further assessed the distribution of C-section coverage and costs across households’ socioeconomic status and place of residence (rural/urban). A wealth index was computed as a measure of household living standard. We used principal component analysis based on 42 items of household characteristics and asset ownership to generate a wealth score for each household (Appendix A1) [50, 51]. Households were then ranked according to the wealth index/ score and categorized into quintiles of equal size, with quintile 1 consisting of the poorest 20% households, while quintile 5 consisted of the least poor 20%. We presented our equity results in three aspects: a bar graph and concentration curve showing the distribution of C-section coverage across quintiles and then computed the corresponding concentration index. The concentration index is defined as twice the area between the 45-degree line of equality and the concentration curve, and it measures the degree of socioeconomic inequality in a variable of interest [52]. A concentration curve plots the cumulative share of C-section coverage (Y-axis) against the cumulative share of the households ranked by socioeconomic status (X-axis). A dominance test was performed to assess whether the concentration curve is statistically different from the line of equality [52]. The concentration curve is then summarised by a concentration index, which ranges between [− 1 and + 1], whereby zero indicate equality across socioeconomic subgroups, while negative and positive values indicate pro-poor and pro-rich access to C-section delivery care, respectively [52]. We also tested whether a concentration index was significantly different from zero. All analyses were performed using STATA version 16.
Results
Descriptive statistics
Table 1 presents a description of the data by mode of delivery. The response rate was almost 96% (n = 2874) out of 3000 eligible women/ households. Out of 2874 women, 86% (n = 2466) had facility-based delivery care, 78% (n = 2229) had normal delivery and 8% (n = 237) had C-section delivery (7.5% of C-section were in public facilities only).
Sampled women were predominantly married, Muslim, educated at least with primary education, farmers, uninsured, and residing in rural district councils. On average, women were aged 26 years old, with almost 3 births, and residing in households with 5 family members. The two groups of women based on the mode of delivery were similar in terms of age, marital status, religion, education, and health insurance status.
Delivery at the health facility was associated with a 20% likelihood of incurring OOP payments. However, as expected, the likelihood of paying OOP almost doubled for C-section compared to normal delivery, i.e., 19% versus 34%. The average amount paid for C-section was almost 12 times that of normal deliveries, while hospitalisation time was 3 times that of normal deliveries. The pattern on cost comparison and hospitalisation time between modes of childbirth did not change even when the analysis was restricted to public facilities only.
Effect of C-section delivery on direct costs
Table 2 shows the incremental chances of paying and the corresponding amount incurred by women who delivered by C-section after accounting for covariates. The C-section delivery care was positively associated with high chances of paying for health care (16 percentage point) and around 18 percentage point in public facilities only. In terms of the odds ratio (data not shown), the likelihood of paying for C-section was higher (OR = 2.43, 95% CI: 1.75–3.35) than normal delivery, and similarly when restricting to public facilities only (OR = 3.19, 95% CI: 2.23–4.57). The incremental cost of giving birth by C-section, compared to normal delivery, was 20 USD on average and almost 11 USD in public facilities only.
Effects of C-section delivery on indirect costs
The effects of C-section on productivity loss after accounting for covariates were presented in Table 3. We found a significant reduction in labour supply/ productivity after C-section delivery. On average, women who delivered by C-section spent 2 days or 51 h more for hospitalisation compared to women with normal delivery (Table 3). The productivity loss slightly reduced to 1.9 days and 47 h when restricting to public facilities only.
Equity in C-section utilisation
As indicated in Fig. 1, the overall coverage of C-section delivery was lowest among women from the poorest households (5.1%) compared to those from the least poor households (14.9%). The corresponding concentration index was positive (CI = 0.2052, p-value< 0.01). All these indicates a pro-rich coverage in C-section care. However, the costs or average amount paid for delivery care were significantly higher among the richest than the poorest women (data not shown). In terms of location, the C-section coverage was higher in urban (12.1%) than in rural districts (7.5%). We further assessed the inequality by wealth status within urban and rural setting separately. While a similar pattern of pro-rich was observed for C-section coverage by socioeconomic quintiles among rural women, there was unclear pattern among women in urban districts since middle groups had the lowest coverage (Figs. 1 and 2). In terms of concentration curves, both curves for rural and urban were below the line of equality indicating a pro-rich utilisation of C-section care. However, the pro-rich inequality in rural areas was significantly different from zero (CI = 0.1786, p < 0.01) than that of urban setting with a borderline significance (CI = 0.2143, p < 0.10). Since the two concentration curves crosses each other, a dominance test was performed to confirm whether the two curves were significantly different. The test confirmed that there was no evidence of dominance, indicating lack of enough evidence that one curve dominating the other. However, the curves in the richest quintiles clearly indicated relatively higher pro-rich inequality in urban than rural, as the curve in urban lies above that of rural. In contrast, the curves in the lowest quintiles were reversed such that the urban curves almost touched the line of equality and lies above the curve for rural, indicating continued pro-rich coverage in rural with unclear pattern for urban.
Discussion
This study found that C-section was significantly associated with higher chances of paying for health care, and had relatively higher direct and indirect costs to patients compared to normal delivery. Women from wealthier and urban households were more likely to access and receive C-section delivery and paid more direct costs on average than their counterpart women.
The prevalence of C-section deliveries was slightly higher (8.3%) than the national average of 6% reported in the 2015/16 Tanzania Demographic and Health Survey [40] and regional average of 7.3% for Africa [53]. The low coverage rate of C-section is typical in developing countries when compared to high-income countries [54, 55]. One of the reasons for low uptake of C-section in developing countries is the inadequate infrastructural and human resource capacity to offer emergency and surgical care [56,57,58]. For instance, only 19–50% of hospitals in sub-Saharan Africa can provide 24-h emergency care. However, as countries reform their health systems and improve health care service utilisation [59,60,61], one would expect the C-section rates would increase over time.
The result of higher patient costs for C-section than normal delivery is consistent with the previous pattern reported elsewhere [7, 8, 17, 22, 25, 31, 33, 62, 63], although the incremental cost of 20 USD that we found was relatively lower. In comparison, the incremental cost for maternal complications/ C-section was 13.6 USD in Mali [7], 55.9 USD in Democratic Republic of Congo [33], and varied by time and measurement in Bangladesh including 86 USD per C-section birth [27], 34 USD per month [8] and around 269 USD from childbirth to six months postpartum [22]. A few studies in a recent review in sub-Saharan Africa reported the costs of C-section delivery ranging from 55.8–377.3 USD [31]. In Pakistan, postpartum mother after C-section incurred 204 USD (79 USD for normal delivery) as total direct and indirect cost including transport and food [29]. These costs incurred by patients and/or relatives suggest that accessing essential obstetric care including C-section can reduce household resources significantly [8, 22] and can reinforce catastrophic health spending [7, 64, 65].
Our study also revealed that C-section delivery was associated with much higher loss in productivity compared to normal delivery. A similar finding, though for maternal complications, was reported in Bangladesh [8, 22] and Ghana [34]. While women in Tanzania were hospitalised for an average of 2 days after C-section, women with maternal complications in Bangladesh lost 2 to 3 days after childbirth [8]. Another study in Bangladesh valued higher productivity loss between 30.1–33.1 USD for severe and less-severe complication than 14.1 USD for normal delivery [25]. Similarly, Ghanaian women with maternal complications spent 3 days on average (2 days median) for hospitalisation, while average productivity loss was estimated to be 8.92 USD [34].
The assessment of equity in health care benefits and payments is an important approach to monitor progress towards UHC [6, 66]. Equity is particularly needed to ensure that households receive health benefits according to their health care need and contributes to the health care according to their ability-to-pay [5, 66]. The available evidence is often in contrast to the above equity principle for UHC [6]. For instance, this study found that C-section delivery was more likely to be accessed by wealthier and urban women, yet inaccessible by their counterparts that may have the greatest health care need. The Tanzania Demographic and Health Survey also reports higher rates of C-section deliveries among the wealthier, educated and urban residing women [40]. This ‘socioeconomic gradient’ in utilising C-section have also been reported elsewhere [54, 55, 67,68,69]. In terms of equity in health care payment, however, the burden of direct payments was significantly higher among the richest as they are more likely to access C-section care than the poorest women. Consistently, the poorest typically spend less on treatment than other income groups due to lack of access, inability to pay, greater use of public services [23].
Fair and timely access to essential life-saving interventions is needed to reduce morbidity and mortality rates globally. For instance, to reduce maternal deaths may need fair and timely access to basic and comprehensive emergency obstetric care [70]. Consequently, many LMICs decided to offer ‘free maternity services’ or implement a user fee exemption policy to reduce the financial barriers [71,72,73,74,75]. Yet, a large body of evidence in these settings shows women are still paying for exempted services and facing financial barrier [16,17,18, 27, 65, 71, 76, 77]. One reason for such weak enforcement of free/ exemption policy is existing disruptions in health systems [71] including an inadequate budget allocation to the health sector [16,17,18] as well as difficulties to identify the eligible clients [19, 20]; which altogether undermines the effectiveness of the policy [78,79,80,81,82].
Our findings have important policy implications. Despite the efforts to reduce the direct medical costs by offering ‘free maternity services’ in many settings including Tanzania (or offering fee exemption for C-section specific in some settings), evidence shows that people are still paying OOP for exempted/ free services. This indicates weak enforcement of the policy and eventually affecting the effort to offer financial protection for UHC. The lack of formal waivers/exemption directives to health workers are considered to undermines the legal basis for effective implementation of free maternity services. It is also well documented that patients may incur costs in relation to informal payment/ gift to the health worker, particularly when supportive supervision is ineffective, health workers having poor working conditions (e.g., drug stockout, inadequate staffing level) and are not renumerated on timely manner (e.g., salaries, benefits) [83]. Access to C-section care is also in favour of the better-off, which reflects the low affordability among the poorest population [7, 64]. It further implies that some women, especially the worse-off, are deterred to access life-saving interventions or losing their lives as they cannot afford C-section delivery care [7, 84]. It is even life-threatening concerning the unaffordability of life-saving interventions such as C-section since this care increases the chance of rehospitalisation [85]. Since C-section is an emergence and life-saving procedure for the mother and the baby, fair and timely access irrespective of women characteristics is necessary. Countries should therefore ensure timely access to effective and affordable basic and comprehensive emergency obstetric care to reduce maternal deaths [35, 86]. Efforts are also needed to improve access to surgical services especially in sub-Saharan Africa [87]. To reduce financial risks especially among the poor in the move to UHC, adequate funding to health facilities through prepayment mechanisms and strong enforcement of the exemption policy or user fee removal would help [2, 66]. Further research is needed to deeply understand the coping mechanisms and main drivers of paying for exempted services in Tanzania.
This study has the following limitations. First, we were unable to incorporate transport costs to access care due to data availability but its significant contribution to catastrophic health spending is well documented [4]. This data was lacking because the main evaluation study was not designed to accommodate this information. Otherwise, the study may have underestimated the actual patient costs associated with seeking C-section services. Second, while the assessment of the affordability of costs regarding C-section is important [7], we did not get data on household income/ expenditure to reflect a household’s ability to pay. Third, we were unable to identify the coping strategies to finance delivery care because of the limited data available. Fourth, the productivity loss was not quantified in monetary values, because of unreliable income or wage rate data for the rural and urban population. Fifth, the information about women’s medical conditions prior to C-section was not collected, while this information could be adjusted and used to explain the findings. Lastly, there is a possibility of a recall bias as we relied on recall data for costs incurred during childbirth in the last 12 months.
Conclusions
Despite the presence of exemption policy for maternal health services in Tanzania, women accessing and utilising delivery care in health facilities are facing substantial direct and indirect costs, and significantly higher costs for obstetric or C-section delivery care. The exemption or user fee removal policy is an important arrangement to address the financial barriers to access essential obstetric care like C-section, but not a sufficient approach to ensure financial protection in poor-resource settings. To achieve the intended policy goal, countries should ensure strong enforcement of exemptions through reduced health system disruptions and timely reimbursement of resources/ budget disbursements to cover the exempted costs. These efforts are needed not only to improve access to obstetric care but also to ensure financial protection for UHC as well as reduce maternal deaths.
Abbreviations
- ANC:
-
Antenatal Care
- C-section:
-
Caesarean Section
- CHF:
-
Community Health Fund
- CI:
-
Concentration Index
- LMICs:
-
Low and Middle-Income Countries
- NHIF:
-
National Health Insurance Fund
- OLS:
-
Ordinary Least Square
- OOP:
-
Out-Of-Pocket
- OR:
-
Odds Ratio
- PNC:
-
Postnatal Care
- TZS:
-
Tanzanian Shillings
- UHC:
-
Universal Health Coverage
- USD:
-
United States Dollar
References
Stenberg K, Hanssen O, Edejer TT, Bertram M, Brindley C, Meshreky A, et al. Financing transformative health systems towards achievement of the health sustainable development goals: a model for projected resource needs in 67 low-income and middle-income countries. Lancet Glob Health. 2017;5(9):e875–87.
WHO: the world health report: health systems financing: the path to universal coverage. In. Edited by Geneva. World Health Organization, Geneva: World Health Organization; 2010.
Xu K, Evans DB, Carrin G, Aguilar-Rivera AM, Musgrove P, Evans T. Protecting households from catastrophic health spending. Health Aff (Millwood). 2007;26(4):972–83.
McIntyre D, Thiede M, Dahlgren G, Whitehead M. What are the economic consequences for households of illness and of paying for health care in low- and middle-income country contexts? Soc Sci Med. 2006;62(4):858–65.
Mills A, Ataguba JE, Akazili J, Borghi J, Garshong B, Makawia S, et al. Equity in financing and use of health care in Ghana, South Africa, and Tanzania: implications for paths to universal coverage. Lancet. 2012;380(9837):126–33.
Asante A, Price J, Hayen A, Jan S, Wiseman V. Equity in health care financing in low- and middle-income countries: a systematic review of evidence from studies using benefit and financing incidence analyses. PLoS One. 2016;11(4):e0152866.
Arsenault C, Fournier P, Philibert A, Sissoko K, Coulibaly A, Tourigny C, et al. Emergency obstetric care in Mali: catastrophic spending and its impoverishing effects on households. Bull World Health Organ. 2013;91(3):207–16.
Powell-Jackson T, Hoque ME. Economic consequences of maternal illness in rural Bangladesh. Health Econ. 2012;21(7):796–810.
McIntyre D, Thiede M, Birch S. Access as a policy-relevant concept in low- and middle-income countries. Health Econ Policy Law. 2009;4(Pt 2):179–93.
Borghi J, Storeng KT, Filippi V. Overview of the costs of obstetric care and the economic and social consequences for households. Reducing financial barriers to obstetric care in low-income countries. 2008.
Ensor T, Cooper S. Overcoming barriers to health service access: influencing the demand side. Health Policy Plan. 2004;19(2):69–79.
O'Donnell O. Access to health care in developing countries: breaking down demand side barriers. Cad Saude Publica. 2007;23(12):2820–34.
Dzakpasu S, Powell-Jackson T, Campbell OM. Impact of user fees on maternal health service utilization and related health outcomes: a systematic review. Health Policy Plan. 2014;29(2):137–50.
Kruk ME, Goldmann E, Galea S. Borrowing and selling to pay for health care in low- and middle-income countries. Health Aff (Millwood). 2009;28(4):1056–66.
Maluka SO. Why are pro-poor exemption policies in Tanzania better implemented in some districts than in others? Int J Equity Health. 2013;12:80.
Kruk ME, Mbaruku G, Rockers PC, Galea S. User fee exemptions are not enough: out-of-pocket payments for 'free' delivery services in rural Tanzania. Tropical Med Int Health. 2008;13(12):1442–51.
Ravit M, Philibert A, Tourigny C, Traore M, Coulibaly A, Dumont A, et al. The hidden costs of a free caesarean section policy in West Africa (Kayes region, Mali). Matern Child Health J. 2015;19(8):1734–43.
Ameur AB, Ridde V, Bado AR, Ingabire M-G, Queuille L. User fee exemptions and excessive household spending for normal delivery in Burkina Faso: the need for careful implementation. BMC Health Serv Res. 2012;12(1):412.
Aryeetey GC, Jehu-Appiah C, Spaan E, D'Exelle B, Agyepong I, Baltussen R. Identification of poor households for premium exemptions in Ghana's National Health Insurance Scheme: empirical analysis of three strategies. Tropical Med Int Health. 2010;15(12):1544–52.
Kuwawenaruwa A, Baraka J, Ramsey K, Manzi F, Bellows B, Borghi J. Poverty identification for a pro-poor health insurance scheme in Tanzania: reliability and multi-level stakeholder perceptions. Int J Equity Health. 2015;14:143.
Wagstaff A. The economic consequences of health shocks: evidence from Vietnam. J Health Econ. 2007;26(1):82–100.
Hoque ME, Powell-Jackson T, Dasgupta SK, Chowdhury ME, Koblinsky M. Costs of maternal health-related complications in Bangladesh. J Health Popul Nutr. 2012;30(2):205–12.
Russell S: The economic burden of illness for households in developing countries: a review of studies focusing on malaria, tuberculosis, and human immunodeficiency virus/acquired immunodeficiency syndrome. The American journal of tropical medicine and hygiene 2004, 71(2_suppl):147–155.
Leive A, Xu K. Coping with out-of-pocket health payments: empirical evidence from 15 African countries. Bull World Health Organ. 2008;86:849–856C.
Borghi J, Sabina N, Blum LS, Hoque ME, Ronsmans C. Household costs of healthcare during pregnancy, delivery, and the postpartum period: a case study from Matlab, Bangladesh. J Health Popul Nutr. 2006;24(4):446–55.
Borghi J, Sabina N, Ronsmans C, Killewo J. Comparison of costs of home and facility-based basic obstetric care in rural Bangladesh. J Health Popul Nutr. 2010;28(3):286–93.
Nahar S, Costello A. The hidden cost of 'free' maternity care in Dhaka, Bangladesh. Health Policy Plan. 1998;13(4):417–22.
Borghi J, Ensor T, Neupane BD, Tiwari S. Financial implications of skilled attendance at delivery in Nepal. Tropical Med Int Health. 2006;11(2):228–37.
Khan A, Zaman S. Costs of vaginal delivery and caesarean section at a tertiary level public hospital in Islamabad, Pakistan. BMC Pregnancy Childbirth. 2010;10:2.
Borghi J, Bastus S, Belizan M, Carroli G, Hutton G, Fox-Rushby J. Costs of publicly provided maternity services in Rosario, Argentina. Salud Publica Mex. 2003;45(1):27–34.
Mori AT, Binyaruka P, Hangoma P, Robberstad B, Sandoy I. Patient and health system costs of managing pregnancy and birth-related complications in sub-Saharan Africa: a systematic review. Health Econ Rev. 2020;10(1):26.
Perkins M, Brazier E, Themmen E, Bassane B, Diallo D, Mutunga A, et al. Out-of-pocket costs for facility-based maternity care in three African countries. Health Policy Plan. 2009;24(4):289–300.
Deboutte D, O'Dempsey T, Mann G, Faragher B. User cost of caesarean section: case study of Bunia, Democratic Republic of Congo. Int J Health Plann Manag. 2015;30(2):88–97.
Dalaba MA, Akweongo P, Aborigo RA, Saronga HP, Williams J, Aninanya GA, et al. Cost to households in treating maternal complications in northern Ghana: a cross sectional study. BMC Health Serv Res. 2015;15(1):34.
Ronsmans C, De Brouwere V, Dubourg D, Dieltiens G. Measuring the need for life-saving obstetric surgery in developing countries. BJOG Int J Obstet Gynaecol. 2004;111(10):1027–30.
Alkema L, Chou D, Hogan D, Zhang S, Moller AB, Gemmill A, et al. Global, regional, and national levels and trends in maternal mortality between 1990 and 2015, with scenario-based projections to 2030: a systematic analysis by the UN maternal mortality estimation inter-agency group. Lancet. 2016;387(10017):462–74.
Binyaruka P, Patouillard E, Powell-Jackson T, Greco G, Maestad O, Borghi J. Effect of paying for performance on utilisation, quality, and user costs of health Services in Tanzania: a controlled before and after study. PLoS One. 2015;10(8):e0135013.
Borghi J, Mayumana I, Mashasi I, Binyaruka P, Patouillard E, Njau I, et al. Protocol for the evaluation of a pay for performance programme in Pwani region in Tanzania: a controlled before and after study. Implement Sci. 2013;8:80.
NBS: Tanzania Population and Housing Census: Population Distribution by Administrative Areas 2012. In. National Bureau of Statistics (NBS): Dar es Salaam; 2013.
TDHS. Tanzania demographic and health survey and malaria Indicator survey 2015–16. In. Dar es Salaam: National Bureau of Statistics (NBS); 2016.
Afnan-Holmes H, Magoma M, John T, Levira F, Msemo G, Armstrong CE, et al. Tanzania's countdown to 2015: an analysis of two decades of progress and gaps for reproductive, maternal, newborn, and child health, to inform priorities for post-2015. Lancet Glob Health. 2015;3(7):e396–409.
Mohan D, LeFevre AE, George A, Mpembeni R, Bazant E, Rusibamayila N, et al. Analysis of dropout across the continuum of maternal health care in Tanzania: findings from a cross-sectional household survey. Health Policy Plan. 2017.
Owili PO, Muga MA, Chou YJ, Hsu YH, Huang N, Chien LY. Associations in the continuum of care for maternal, newborn and child health: a population-based study of 12 sub-Saharan Africa countries. BMC Public Health. 2016;16:414.
Singh K, Story WT, Moran AC. Assessing the continuum of care pathway for maternal health in South Asia and sub-Saharan Africa. Matern Child Health J. 2016;20(2):281–9.
MOHCDGEC: National Health Accounts (NHA) for financial years 2013/14, 2014/15 and 2015/16. In.: Ministry of Health Community development, gender, elderly and children (MoHCDGEC), Tanzania; 2019.
MOHCDGEC: Mid Term Review of the Health Sector Strategic Plan IV 2015–2020: Health Finance Technical Report. . In: Ministry of Health Community Development, Gender, Elderly and Children (MoHCDGEC), Tanzania. Ministry of Health Community Development, Gender, Elderly and Children (MoHCDGEC), Tanzania: Ministry of Health Community Development, Gender, Elderly and Children (MoHCDGEC), Tanzania; 2019.
Mtei G, Makawia S, Masanja H. Monitoring and evaluating progress towards universal health coverage in Tanzania. PLoS Med. 2014;11(9):e1001698.
Manzi F, Schellenberg JA, Adam T, Mshinda H, Victora CG, Bryce J. Out-of-pocket payments for under-five health care in rural southern Tanzania. Health Policy Plan. 2005;20(Suppl 1):i85–93.
Manning WG, Mullahy J. Estimating log models: to transform or not to transform? J Health Econ. 2001;20(4):461–94.
Filmer D, Pritchett LH. Estimating wealth effects without expenditure data--or tears: an application to educational enrollments in states of India. Demography. 2001;38(1):115–32.
Vyas S, Kumaranayake L. Constructing socio-economic status indices: how to use principal components analysis. Health Policy Plan. 2006;21(6):459–68.
O'Donnell O, Doorslaer E, Wagstaff A, Lindelow M. Analyzing health equity using household survey data. A Guide to Techniques and Their Implementation. 2008.
Betrán AP, Ye J, Moller AB, Zhang J, Gülmezoglu AM, Torloni MR. The increasing trend in caesarean section rates: global, regional and National Estimates: 1990-2014. PLoS One. 2016;11(2):e0148343.
Cavallaro FL, Cresswell JA, Franca GV, Victora CG, Barros AJ, Ronsmans C. Trends in caesarean delivery by country and wealth quintile: cross-sectional surveys in southern Asia and sub-Saharan Africa. Bull World Health Organ. 2013;91(12):914–922D.
Ronsmans C, Holtz S, Stanton C. Socioeconomic differentials in caesarean rates in developing countries: a retrospective analysis. Lancet. 2006;368(9546):1516–23.
Hsia RY, Mbembati NA, Macfarlane S, Kruk ME. Access to emergency and surgical care in sub-Saharan Africa: the infrastructure gap. Health Policy Plan. 2011;27(3):234–44.
O'Neill K, Takane M, Sheffel A, Abou-Zahr C, Boerma T. Monitoring service delivery for universal health coverage: the service availability and readiness assessment. Bull World Health Organ. 2013;91(12):923–31.
Dogba M, Fournier P. Human resources and the quality of emergency obstetric care in developing countries: a systematic review of the literature. Hum Resour Health. 2009;7:7.
Lagomarsino G, Garabrant A, Adyas A, Muga R, Otoo N. Moving towards universal health coverage: health insurance reforms in nine developing countries in Africa and Asia. Lancet. 2012;380(9845):933–43.
Gautier L, Ridde V. Health financing policies in sub-Saharan Africa: government ownership or donors' influence? A scoping review of policymaking processes. Glob Health Res Policy. 2017;2:23.
Victora CG, Requejo JH, Barros AJ, Berman P, Bhutta Z, Boerma T, et al. Countdown to 2015: a decade of tracking progress for maternal, newborn, and child survival. Lancet. 2016;387(10032):2049–59.
Borghi J, Hanson K, Acquah CA, Ekanmian G, Filippi V, Ronsmans C, et al. Costs of near-miss obstetric complications for women and their families in Benin and Ghana. Health Policy Plan. 2003;18(4):383–90.
Quayyum Z, Nadjib M, Ensor T, Sucahya PK. Expenditure on obstetric care and the protective effect of insurance on the poor: lessons from two Indonesian districts. Health Policy Plan. 2010;25(3):237–47.
Honda A, Randaoharison PG, Matsui M. Affordability of emergency obstetric and neonatal care at public hospitals in Madagascar. Reprod Health Matters. 2011;19(37):10–20.
Asante F, Chikwama C, Daniels A, Armar-Klemesu M. Evaluating the economic outcomes of the policy of fee exemption for maternal delivery care in Ghana. Ghana Med J. 2007;41(3):110–7.
Kutzin J. Health financing for universal coverage and health system performance: concepts and implications for policy. Bull World Health Organ. 2013;91(8):602–11.
Ravit M, Audibert M, Ridde V, De Loenzien M, Schantz C, Dumont A. Do free caesarean section policies increase inequalities in Benin and Mali? Int J Equity Health. 2018;17(1):71.
Boatin AA, Schlotheuber A, Betran AP, Moller AB, Barros AJD, Boerma T, et al. Within country inequalities in caesarean section rates: observational study of 72 low and middle income countries. Bmj. 2018;360:k55.
Boerma T, Ronsmans C, Melesse DY, Barros AJD, Barros FC, Juan L, et al. Global epidemiology of use of and disparities in caesarean sections. Lancet. 2018;392(10155):1341–8.
WHO: monitoring emergency obstetric care. A handbook. In: Geneva: World Health Organization. 2009.
Ridde V, Robert E, Meessen B. A literature review of the disruptive effects of user fee exemption policies on health systems. BMC Public Health. 2012;12:289.
Meessen B, Hercot D, Noirhomme M, Ridde V, Tibouti A, Tashobya CK, Gilson L: Removing user fees in the health sector: a review of policy processes in six sub-Saharan African countries. Health Policy Plan 2011, 26 Suppl 2:ii16-29.
Hercot D, Meessen B, Ridde V, Gilson L: Removing user fees for health services in low-income countries: a multi-country review framework for assessing the process of policy change. Health Policy Plan 2011, 26 Suppl 2:ii5-15.
Richard F, Witter S, de Brouwere V. Innovative approaches to reducing financial barriers to obstetric care in low-income countries. Am J Public Health. 2010;100(10):1845–52.
Fournier P, Dumont A, Tourigny C, Dunkley G, Dramé S. Improved access to comprehensive emergency obstetric care and its effect on institutional maternal mortality in rural Mali. Bull World Health Organ. 2009;87(1):30–8.
Johnson FA, Frempong-Ainguah F, Padmadas SS. Two decades of maternity care fee exemption policies in Ghana: have they benefited the poor? Health Policy Plan. 2016;31(1):46–55.
Chuma J, Musimbi J, Okungu V, Goodman C, Molyneux C. Reducing user fees for primary health care in Kenya: policy on paper or policy in practice? Int J Equity Health. 2009;8:15.
Witter S, Boukhalfa C, Cresswell JA, Daou Z, Filippi V, Ganaba R, et al. Cost and impact of policies to remove and reduce fees for obstetric care in Benin, Burkina Faso, Mali and Morocco. Int J Equity Health. 2016;15(1):123.
Masiye F, Kaonga O, Kirigia JM. Does user fee removal policy provide financial protection from catastrophic health care payments? Evidence from Zambia. PLoS One. 2016;11(1):e0146508.
Nguyen HT, Zombre D, Ridde V, De Allegri M. The impact of reducing and eliminating user fees on facility-based delivery: a controlled interrupted time series in Burkina Faso. Health Policy Plan. 2018;33(8):948–56.
Lagarde M, Palmer N. The impact of user fees on health service utilization in low- and middle-income countries: how strong is the evidence? Bull World Health Organ. 2008;86(11):839–48.
Fournier P, Dumont A, Tourigny C, Philibert A, Coulibaly A, Traore M. The free caesareans policy in low-income settings: an interrupted time series analysis in Mali (2003-2012). PLoS One. 2014;9(8):e105130.
Binyaruka P, Balabanova D, McKee M, Hutchinson E, Andreoni A, Ramesh M, et al. Supply-side factors influencing informal payment for healthcare services in Tanzania. Health Policy Plan. 2021.
Geleto A, Chojenta C, Musa A, Loxton D. Barriers to access and utilization of emergency obstetric care at health facilities in sub-Saharan Africa: a systematic review of literature. Syst Rev. 2018;7(1):183.
Declercq E, Barger M, Cabral HJ, Evans SR, Kotelchuck M, Simon C, et al. Maternal outcomes associated with planned primary cesarean births compared with planned vaginal births. Obstet Gynecol. 2007;109(3):669–77.
WHO: monitoring emergency obstetric care. A handbook. Geneva: World Health Organization 2009.
Luboga S, Macfarlane SB, von Schreeb J, Kruk ME, Cherian MN, Bergström S, et al. Increasing access to surgical services in sub-saharan Africa: priorities for national and international agencies recommended by the Bellagio essential surgery group. PLoS Med. 2009;6(12):e1000200.
Acknowledgements
We would like to thank all healthcare providers, health managers and all health stakeholders who participated or facilitated to ensure a successfully fieldwork for data collection for P4P evaluation. We also thank the whole P4P evaluation research team, including data collectors and field coordinators. We also acknowledge the support from all field respondents, and various officials such as Regional Medical Officers, District Medical officers, Health facility in-charges, and P4P implementing agency.
Data availability statement
The data have been uploaded into a data repository. The DOI URL for the dataset is: https://doi.org/10.5281/zenodo.21709.
Funding
The Government of Norway funded the data collection for the program evaluation that was used in this paper (grant numbers: TAN-3108 and TAN 13/0005. http://www.norad.no/en/). The funding body had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. All authors had no funding for data analysis and writing of this paper.
Author information
Authors and Affiliations
Contributions
PB conceptualized this sub-study and oversaw data collection. PB analyzed the data and wrote the first draft of the manuscript. ATM together with PB involved in data interpretation, presentation, and revision of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical consideration
Ethical clearance was given for the evaluation of P4P by the Institutional Review Board of the Ifakara Health Institute (approval number: 1BI1IRB/38) and the Ethics Review Board of the London School of Hygiene & Tropical Medicine. Study participants provided written consent to participate in the study. All study participants were given an information sheet explaining the project and the voluntary nature of participation. Informed consent was obtained from all participants and/or their legal guardian(s), and were given a written consent form to sign before proceeding with an interview. The information sheet and consent form were both approved by the ethics committees prior to the start of the research. In addition, all research methods were performed in accordance with the relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors have no competing interests to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Binyaruka, P., Mori, A.T. Economic consequences of caesarean section delivery: evidence from a household survey in Tanzania. BMC Health Serv Res 21, 1367 (2021). https://doi.org/10.1186/s12913-021-07386-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-021-07386-0