Abstract
Background
Since the introduction of pharmaceutical care concept by Hepler and Strand in 1990, community pharmacists worldwide have been realigning their roles from being product-focused to patient-orientated to improve patient's quality of life. The objectives of this study were to determine the type of services, with emphasis on the extent of pharmaceutical care services provided by community pharmacists and the barriers in providing such services in Malaysia.
Methods
A cross-sectional observational study was conducted using an online questionnaire. Community pharmacists in Malaysia were invited to participate in the study via emails. The questionnaire was structured based on the Malaysian Community Pharmacy Benchmarking Guidelines, the five practice principles of pharmaceutical care by the American Pharmacists Association and other studies. The online questionnaire was opened for 6 months, from April to September 2018. A reminder to participate was sent via email to the community pharmacists every fortnight.
Results
A total of 420 community pharmacists responded to the online questionnaire. Besides essential services such as treatment for minor illness, medicine dispensing and counselling, most of the respondents were providing health screening and monitoring (99.5%), selection and recommendation of health supplements (90.5%), patient medication review (68.8%), weight management (52.4%) and counselling on smoking cessation (51.0%). More than half (53.3%) of the respondents reported that they were providing pharmaceutical care services to patients with chronic diseases. Based on the practice principles of pharmaceutical care, the respondents were involved in patients' data collection (23.3%), medical information evaluation (18.6%), formulating a drug therapy plan (9.3%), implementing a drug therapy plan (4.5%), and monitoring and modifying the plan (18.3%). Lack of separation between prescribing and dispensing was perceived as the main barrier to the implementation of pharmaceutical care services by a majority of the respondents (84.0%).
Conclusions
The present study found that pharmaceutical care services provided by community pharmacists in Malaysia were inadequate compared to international practice principles. Areas that need improvement included collaboration with patients' other health care providers; more proactive management of patient's medicine regimen; having proper patient monitoring and follow-up mechanisms, and documentation.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
Since the introduction of the pharmaceutical care philosophy by Hepler and Strand in 1990, community pharmacists worldwide have been urged by the respective governments and professional bodies, to shift their roles from being product-focused to patient-orientated, to achieve definite outcomes that improve a patient's quality of life [1]. The American Pharmacists Association (APhA) developed five principles on the practice of pharmaceutical care to ensure positive outcomes for patients. These five principles included: patients’ data collection; medical information evaluation; formulating a drug therapy plan; implementing the plan; monitoring and modifying the plan [2].
Studies on pharmaceutical care services provided by community pharmacists found that such services improved adherence to medications for chronic diseases such as hypertension, osteoporosis and hyperlipidaemia [3,4,5]. The optimisation of medication use had also led to a reduction in health care cost [4, 5]. Patients receiving pharmaceutical care services showed improved health indices such as significant decreases in glycated haemoglobin (HbA1c) level, systolic and diastolic blood pressure [6,7,8,9], better knowledge of the disease and improvement in certain components of health-related quality of life [8], as well as experienced a reduction in length of hospital stay and a lower rate of hospital readmission [10,11,12].
However, various studies had raised concern on the under-utilisation of community pharmacists in Malaysia in providing optimal health care to the general public and contributing to the health care system of the country [13,14,15]. Community pharmacists in Malaysia were mainly involved in supplying medicines and health supplements, providing advice and treatment for minor health problems, and conducting health screening tests [16], although some also provided health promotion services such as counselling on healthy lifestyles, smoking cessation and weight management [13, 17]. Thus far, there is a lack of recent studies on the types of pharmacy services provided by community pharmacists nationwide. Besides, studies specifically on pharmaceutical care services provided by community pharmacists in Malaysia, as well as possible barriers for community pharmacists to practise such services are still lacking. Sam et al. concluded that slightly more than half of the patients were satisfied with the pharmaceutical care services provided by a community pharmacist [18]. Another Malaysian study showed positive clinical outcomes of diabetes patients who went through a community pharmacist-based diabetes management programme [7]. However, both studies were limited to only one community pharmacy in Malaysia. Other local studies on pharmaceutical care focused more on counselling provided by community pharmacists [13, 19, 20]. Although medication counselling is an important element of pharmaceutical care and has been shown to have a positive impact on patient medicine use behaviour and adherence [21], this is only a part of the practice principles for pharmaceutical care by APhA [22].
At the time of the present study, there were more than 2,500 community pharmacies in Malaysia [23]. The health care resources in Malaysia are already stretching to the limit. As community pharmacies are easily accessible by the general public, they should be fully utilised in the development and implementation of the health care system in Malaysia. The question is: Are community pharmacists providing adequate pharmaceutical care services which can contribute to the health care system in Malaysia?
Therefore, the main objectives of the present study were to determine the types of services provided by community pharmacists in Malaysia, with emphasis on the extent of pharmaceutical care services and any barriers associated with the provision of such services, from the pharmacists' perspectives. The findings of this study will enable health care stakeholders in the country to better understand and plan a more comprehensive health care system in Malaysia. This should involve all health care providers including community pharmacists in the partnership or integration between public and private health sectors [24]. This study will also bring awareness to community pharmacists on areas of pharmacy practice which they need to prioritise or improve to provide better health care. In addition, the insights on perceived barriers by the community pharmacists in the implementation of pharmaceutical care will enable related professional bodies to continue engaging with policymakers to develop a better platform for the profession to contribute to the health care system of the country.
Methods
This was a cross-sectional study which used an online, self-administered questionnaire via Survey Monkey®. The target population was community pharmacists who were working in private community pharmacies on a full-time basis in the country. Pharmacists who were working on part-time basis as locum pharmacists, or only in the administration or wholesale department of a community pharmacy, or a community pharmacy located inside a hospital premise, were excluded based on a screening question placed at the beginning of the questionnaire.
Using Raosoft® sample size calculator (http://www.raosoft.com /samplesize.html), with 95% confidence level, 5% margin of errors, a study population size of 2,278 and assuming that the prevalence of pharmaceutical care provision was 50%, the calculated sample size was 329.
A questionnaire was developed based on the Community Pharmacy Benchmarking Guideline [25] as well as the five practice principles of pharmaceutical care [2] and from other studies in the literature [13, 16, 17, 26]. The questionnaire used in this study was developed specifically for this study and provided in the Additional File 1.
The evaluation of pharmaceutical care services provided was based on the five practice principles of pharmaceutical care by the American Pharmacists Association (APhA) [2]: (1) Patients' data collection, (2) Medical information evaluation, (3) Formulating a drug therapy plan, (4) Implementing a drug therapy plan, (5) Monitoring and modifying the plan. These five practice principles were evaluated using 15 sub-questions to best match the definition of each principle by APhA [2].
Ten practising community pharmacists with 10 to 20 years of working experience were consulted on which sub-questions could be used to fulfil each of the pharmaceutical care practice principle by APhA [2]. The response and feedback were analysed and the research team concluded that the community pharmacists needed to carry out all the sub-questions under each of the practice principles to be considered as having fulfilled the practice principle concerned (Additional File 2).
Content validity and clarity of the questionnaire were reviewed and assessed by five practising community pharmacists who have a minimum of 10 years working experience. The questionnaire was modified based on their feedback and uploaded online using Survey Monkey®. A pilot study was conducted on 20 community pharmacists. These community pharmacists consisted of those in Northern (5), Central (6), Southern (3), East Coast (2) regions of Peninsular Malaysia, and from East Malaysia (4). These community pharmacists were requested not to participate in the main study. The results of the pilot study were excluded from the main study.
A list of email contacts of registered community pharmacists in Malaysia was compiled with the help of the Malaysian Pharmaceutical Society (MPS). Community pharmacists were contacted via email to participate in this study. The study was conducted using an online survey. When the invited pharmacists clicked the survey link included in the emails sent to them, they would be connected to the information sheet which contained information about the study, estimated time to complete the survey, participants’ rights to withdraw from the study at any time, including withdrawal of any information provided, and the assurance of their confidentiality. If an invited pharmacist agreed to participate in the study, he/she was required to click a checkbox for consent before he/she could proceed to do the questionnaire. The study had been reviewed and approved by the Human Ethics Committee of Taylor’s University Malaysia (reference number: HEC 2018/002).
The anonymity of the respondents was preserved in the study using the “anonymous responses collector” option from Survey Monkey® so as not to track and store the respondents' information. The “multiple responses” option in Survey Monkey® was turned off to allow only one response per browser or email address, thus minimising multiple responses from a single respondent. The online questionnaire was opened for 6 months, from April to September 2018. During these 6 months, a reminder to participate was sent every fortnight via email to only non-responders or partial responders using a feature in the SurveyMonkey.
Data analysis
All data were entered and analysed using the Statistical Package for the Social Sciences (SPSS) version 21 (IBM Corp, Armonk, New York). Descriptive statistics were performed on all variables. For numeric data, the mean (standard deviation, SD) and median (interquartile range, IQR) were generated. Any possible associations between variables were first tested using univariate chi-square analysis and variables that produced p-value equal to or less than 0.25 were further tested using binary logistic regression under the generalised linear model function [27]. A p-value of less than 0.05 was considered as statistically significant. A small Chi-square value with p > 0.05 from Hosmer-Lemeshow Goodness of Fit test indicates that the model fit is acceptable [28].
Barriers in implementing pharmaceutical care were graded based on a 6-point Likert-like scale, from strongly disagree (1), disagree (2), slightly disagree (3), slightly agree (4), agree (5) to strongly agree (6). Mean score (SD) was calculated for each barrier statement [29]. These responses were then collapsed into three groups: ‘strongly disagree and disagree’, ‘slightly disagree and slightly agree’ and ‘agree and strongly agree’ to ease interpretation of results [29, 30].
Results
From the list of 2,278 community pharmacists, 52 responded that they had stopped practising as community pharmacists while two invalid email addresses were returned, leaving a total of 2,224 community pharmacists. The online questionnaire survey was closed after 6 months with 420 completed questionnaires. This gives a response rate of 18.9% (420/2,224) but meets the minimum required number of 329 from the Raosoft® calculation. Characteristics of the respondents are as shown in Table 1. The proportion of respondents from the various states was similar to the distribution of community pharmacies in each state of Malaysia.
Types of pharmacy services provided
Figure 1 shows the types of pharmacy services provided by the respondents regularly, besides essential services such as response to minor illnesses, medicine dispensing and medication counselling, as stipulated in the Community Pharmacy Benchmarking Guideline [25].
Almost all the respondents (99.5%) were providing at least one type of health screening and monitoring, with measurement of blood pressure (99.3%), blood glucose (97.9%), and cholesterol (74.5%) levels as the most common services.
Among the respondents who offered the selection and recommendation of health supplements for general health, only 15.8% (60) have been certified with Complementary Medicine Education (CMed). Whereas, of the respondents who were providing smoking cessation programme to assist their clients to quit smoking, 53.7% (115) were Certified Smoking Cessation Service Providers (CSCSP).
Factors associated with types of pharmacy services provided
A total of eleven potential factors which might be associated with the types of pharmacy services provided were analysed using binary logistic regression: sex, age group, ethnic group, education level, local or overseas graduate, CSCSP, MyHealth MyWeight, Harm Reduction Programme, Diabetes Medicine Therapy Adherence Clinic (DMTAC) certified or trained, year of practice and type of employment. Only factors that were significantly associated with the types of pharmacy services provided are shown in Table 2.
Provision of pharmaceutical care services
Of the 420 respondents, 53.3% (224) reported that they were providing pharmaceutical care services to their customers with chronic diseases such as diabetes mellitus (91.5%), hypertension (90.6%), hyperlipidaemia (83.0%), asthma (72.3%) and others (10.7%) which included skin problems, hyperuricaemia and gastrointestinal problems. Most of these respondents reported that they provided pharmaceutical care services to less than 20 patients in the recent one month.
Factors associated with the provision of pharmaceutical care
Similar factors were analysed using binary logistic regression mentioned. Only demographic factors that were significantly associated with the provision of pharmaceutical care services are shown in Table 3.
Table 4 summarises the practice of all the five principles of pharmaceutical care by the respondents. Among the 420 respondents, only 0.95% (4) provided all the components in all the five practice principles of pharmaceutical care by APhA.
Table 5 shows the factors associated with the practice of components in the five practice principles of pharmaceutical care.
Barriers and facilitators in providing pharmaceutical care services
Table 6 shows the perceived barriers by the respondents in implementing pharmaceutical care services at their community pharmacies.
Of the 18 statements on barriers, the lack of separation between prescribing and dispensing had the highest mean score (SD) of 5.20 (1.01) as well as the highest percentage of ‘agree and strongly agree’ response (84.0%). This indicates that community pharmacists perceived this as the greatest barrier for providing pharmaceutical care.
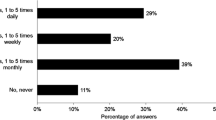
Of the 420 respondents, 274 (65.2%) suggested measures which may facilitate or encourage the provision of pharmaceutical care at their pharmacies (Fig. 2).
The most common facilitator suggested was for the government to implement supportive legislations which included the separation of prescribing and dispensing, mandatory prescriptions by medical doctors, standardization of medicine prices and zoning of community pharmacies. This was followed by increasing public awareness of pharmaceutical care services provided by community pharmacists.
Discussion
The present study found that almost all the respondents (99.5%) were providing some types of health screening and monitoring, mainly the measurement of blood pressure, blood glucose and cholesterol levels. This is higher than from a previous nationwide study (77.1%) by Chua et al [16]. This may be attributed to an increase in awareness and demand by the general public [31] especially by those who could not afford home use medical devices [32]. Nevertheless, future studies should examine the effectiveness of such services in detecting and monitoring the prevalence of non-communicable diseases in the country. This will be in line with the Ministry of Health’s consideration of a public-private partnership in Malaysia [24] which will include the transition of care programme where patients with non-communicable diseases can be referred to community pharmacies to reduce the overload in the public health care system.
Most of the respondents (90.5%) also advised their customers on the selection and use of health supplements for general health. This is similar with a study by Chua et al. [13] which reported that the general public in Malaysia approached community pharmacists mainly to purchase health supplements. However, only 15.8% of the respondents who provided such services were accredited with CMEd. In addition, the odds of providing such service among the community pharmacists with a basic pharmacy degree is almost 5.0 times more than those with a master’s degree. Further studies are required to assess the need for such qualifications for more effective counselling on health supplements. Pharmacy programmes in Malaysia should also include topics on health supplements in their curriculum.
More than two-thirds of the respondents were conducting patient medications reviews in their pharmacies and this was 10 times higher than those who were conducting home medication reviews. This may be due to a shortage of pharmacists or staff which is also mentioned by 63.1% of the respondents in the present study and hence, community pharmacists were not able to leave their pharmacies to conduct home medication reviews. Another reason could be a lack of clinical knowledge and skills in providing home medication review as the odds of providing such service among community pharmacists with a master’s degree were 3.7 times more than those with a basic degree in the present study. Further studies on the processes of medication review in the pharmacies or in the homes are required to determine if these were carried out comprehensively as in Australia [33] or other countries [8, 34] which have incorporated the practice principles for pharmaceutical care in their medication review.
About half of the respondents (51.0%) were providing counselling on smoking cessation. This is similar to the findings by Chua et al. (49.1%) [16]. The war against smoking will continue and the demand for advice to quit smoking may increase in future. In addition, only 53.7% of those who were providing counselling on smoking cessation in the present study had undergone the CSCSP programme while the odds of providing this service among those CSCSP was 8.2 times more than those without such certification. Further studies should also be conducted to determine the effectiveness of such service provided by community pharmacists.
Waste management in community pharmacies involved the collection of expired, damaged, or unused medicines and used needles from customers, for proper disposal. A pilot project was initiated in 2018 by the Malaysian Community Pharmacy Guild to enable community pharmacists to educate and assist the general public on the proper disposal of used needles. This was followed by the Green Pharmacy campaign [35] but the present study found that only 7.9% of community pharmacies were providing waste management service. This is as expected since such service is still relatively new and may need some incentives for the community pharmacies as well as more public awareness campaigns.
Multiple medicine management involves the use of medicine dose administration aid that can be provided by community pharmacists to improve medication adherence. This is beneficial especially for elderly patients who are most susceptible to polypharmacy [36]. With the growing ageing population in Malaysia [37], community pharmacists can play a major role in multiple medicines management but the present study showed that not many respondents (22.1%) were offering such service.
Slightly more than half of the respondents (53.3%) reported that they were providing pharmaceutical care services in their community pharmacies, mainly for patients with diabetes, hypertension, hyperlipidaemia and asthma. However, whether these community pharmacists were familiar with the concept and were practising appropriate pharmaceutical care processes were not captured in this study. A study in Brazil reported that community pharmacists who were providing pharmaceutical care did not have adequate knowledge [38].
The present study found that more than two-thirds of the respondents were not able to access patients' medical information from the patients’ medical doctors. Besides a lack of co-operation from the patients' medical doctors, patients also did not allow community pharmacists to access their medical conditions. These findings are similar to that of studies in other developing countries where the general public has limited knowledge on the roles of community pharmacists [39, 40].
The study also revealed that some of the respondents (14.3%) did not gather medical information from their patients or their caregivers before providing their recommendations. Community pharmacists should be more vigilant in responding to patients’ request for treatment as insufficient patients' medical information may lead to inappropriate treatment recommendation and subsequently, may lead to more harm than good to the patients.
Even though more than 80% of the respondents claimed that they evaluated the safety and effectiveness of the medicines the patients were taking and ensured that their patients understood their current health conditions, most did not document such evaluation and its outcomes. Community pharmacists should be reminded on the importance of documentation which is essential for the effective practice of pharmaceutical care.
Most of the respondents (76.2%) reported that they identified, minimised and prevented potential medicine-related problems while formulating a drug therapy plan. Studies in China (93.1%) and Nigeria (91.1%) also showed that majority of the pharmacists identified medicine-related problems when devising pharmaceutical care plans [40, 41].
Only about 25% of the respondents would recommend changes to the patient's medication regimen when required, compared to 55% of community pharmacists in Nigeria [41]. This may be because community pharmacists in Malaysia do not receive many prescriptions with multiple medications since such prescriptions are usually filled in the hospitals or the clinics of general practitioners. Therefore, community pharmacists are not actively involved in the management of patients' medication regimens and in intervening medication-related problems. Similar situations were also observed in Indonesia [42].
Subsequently, only 10% of the respondents would contact their patients’ medical doctors to discuss the need to change the patients’ medication regimens when appropriate and only half of these respondents documented their interventions. These findings are similar with a study in India where majority of the community pharmacists did not contact the patients’ medical doctors on prescription issues [43]. A previous study in Malaysia also found that almost all (98.9%) the medical doctors in private clinics never had any interactions with community pharmacists [44]. These may be attributed to a poor relationship between the two health care professionals [40], and a lack of awareness or acceptance of pharmacists' roles by the prescribers [44,45,46].
Proper monitoring could be the most important component of pharmaceutical care to detect any undesirable outcomes, but this is usually the least practised [1]. The present study found that less than 20% of the respondents were monitoring and modifying the drug therapy plans for their patients. This finding is similar with studies in Jordan [45] and Saudi Arabia [47].
Community pharmacists in Malaysia rarely document their pharmaceutical care services including the outcomes of their interventions. Poor documentation was also observed in Jordan [45] and Brazil [38]. This may be due to the absence of regulations to keep patients' medical records and also most community pharmacists thought that it was not necessary or were too busy to maintain any documents [48]. Documentation of pharmaceutical services provided should be done for the proper practice of monitoring and modifying of a drug therapy plan.
Ethnicity, employment status and age seemed to determine whether the community pharmacists would conduct the various steps in the practice of pharmaceutical care. Self-employed community pharmacists were more proactive in contacting the patient's other health care providers and recommending changes to the medications. This is as expected since most self-employed individuals will be more enthusiastic and will spend more time with their customers [19]. More in-depth studies such as qualitative studies will be useful to determine how ethnicity affects the provision of pharmaceutical care services.
The present study found that community pharmacists in Malaysia were not providing adequate pharmaceutical care services in the following areas: collaborating with patients' other health care providers to obtain their medical and medication information; managing the patient's medication regimen including the recommendation to change medication when required; having proper patient monitoring and follow-up mechanism; and maintaining documentation of pharmaceutical care services.
The most common barriers that prevented community pharmacists from providing pharmaceutical care services in the present study were government or professional health care policies such as the absence of separation between prescribing and dispensing; government initiative for patients to obtain their prescribed medications from community pharmacies; strict enforcement on the dispensing of prescription-only-medicines with valid prescriptions and lack of standard guidelines on pharmaceutical care services. Lack of supportive health care policies had also been cited as one of the main barriers in other studies [40, 45] including in Malaysia [14] and even in South Korea which practices separation between prescribing and dispensing [29]. The small number of prescriptions received by the community pharmacies in the present study did not provide much opportunity for the provision of pharmaceutical care services to patients with chronic and multiple medications. As suggested by the respondents, the main facilitator for the provision of pharmaceutical care services was having more supportive legislations. The implementation of separation between prescribing and dispensing is a major health care reform which may require political will, time and resources. Perhaps, the authorities concerned can emulate the community pharmacy practice in Thailand where incentives are given to community pharmacists to provide certain services [49].
Another barrier reported was medicine price discrimination by pharmaceutical suppliers. Some medications were not available or were sold to community pharmacies at higher prices [50, 51] and hence, costs of prescribed medications may be higher compared to private hospitals or clinics. This may prevent patients from filling their prescriptions in community pharmacies and consequently less opportunity for prescription screening and for identifying any medication-related problems as well as to provide pharmaceutical care services.
Lack of acceptance by medical doctors for community pharmacists to provide pharmaceutical care services was commonly cited in many developing countries [41, 42, 46]. The present study also found that many respondents (63.6%) reported a lack of acceptance by doctors on recommendation of medication regimens by the pharmacist. This could be due to a lack of doctors’ understanding regarding the clinical knowledge of pharmacists since doctors who had worked closely with community pharmacists trusted these health care professionals [46]. This indicates the importance of open discussion to foster closer collaboration between both health care professionals in providing optimal care to the patients.
Limitations of the study
The first limitation of this study was that the contact list of community pharmacists may not be complete. Therefore, some community pharmacists might have been missed out and did not have the opportunity to participate in the online self-administered questionnaire. In addition, the study was not able to determine if there is any difference in the characteristics of respondents and non-respondents except for the similar distribution among the various states in Malaysia.
Secondly, as this is the first study on pharmaceutical care services provided by community pharmacists in Malaysia based on the five practice principles for pharmaceutical care stipulated by the APhA [2], the components used to verify each principle may not be foolproof. Nevertheless, this did not affect the findings of the present study where the practice of all these principles by community pharmacists in Malaysia were sub-optimal. More importantly, this study showed the areas of pharmaceutical care services that need improvement by community pharmacists. Future studies should also assess the extent or depth of pharmacy programme curricula in Malaysia which cover such services so that appropriate interventions can be planned and implemented.
Conclusions
Most community pharmacies in Malaysia were involved in recommending health supplements, conducting patient medication reviews, weight management and smoking cessation services besides common functions such as treating minor ailments, medication dispensing and counselling. The present study found that community pharmacists in Malaysia were not providing adequate pharmaceutical care services compared to international practice principles. Areas that need improvement included collaboration with patients' other health care providers; more proactive management of patient's medicine regimen; having proper patient monitoring and follow-up mechanisms, and documentation. Programmes for the continuous professional development of community pharmacists should include comprehensive training on the provision of pharmaceutical care. Future studies to assess the effectiveness of services provided by community pharmacists especially on patient medication review and pharmaceutical care should be considered. The current government or professional health care policies were perceived by community pharmacists as the main barrier in providing pharmaceutical care services. Authorities concerned should take this into consideration when planning the health care system of the country.
Availability of data and materials
The datasets used and/or analysed for the present study are available from the corresponding author upon reasonable request.
Abbreviations
- APhA:
-
American Pharmacists Association
- MPS:
-
Malaysian Pharmaceutical Society
- SD:
-
Standard deviation
- IQR:
-
Interquartile range
- CMEd:
-
Complementary medicine education
- CSCSP:
-
Certified smoking cessation service provider
- HRP:
-
Harm reduction programme
- DMTAC:
-
Diabetes medicine therapy adherence clinic
- CI:
-
Confidence interval
- BNF:
-
British national formulary
- MIMS:
-
Monthly index of medical specialities
- OHP:
-
Other health care providers
- PC:
-
Pharmaceutical care
- n.d.:
-
no date
References
Hepler CD, Strand LM. Opportunities and responsibilities in pharmaceutical care. Am J Hosp Pharm. 1990;47(3):533–43. PMID: 2316538.
American Pharmacists Association (APhA). Principles of practice for pharmaceutical care. 1995. Available from http://www.pharmacist.com/principles-practice-pharmaceutical-care. Accessed 2 June 2018.
Fikri-Benbrahim N, Faus MJ, Martínez-Martínez F, Sabater-Hernández D. Impact of a community pharmacists’ hypertension-care service on medication adherence. The AFenPA study. Res Soc Adm Pharm. 2013;9:797–805. https://doi.org/10.1016/j.sapharm.2012.12.006.
Stuurman-Bieze AGG, Hiddink EG, van Boven JFM, Vegter S. Proactive pharmaceutical care interventions improve patients’ adherence to lipid- lowering medication. Ann Pharmacother. 2013;47(11):1448–56. https://doi.org/10.1177/1060028013501146.
Stuurman-Bieze AGG, Hiddink EG, van Boven JFM, Vegter S. Proactive pharmaceutical care interventions decrease patients’ nonadherence to osteoporosis medication. Osteoporos Int. 2014;25:1807–12. https://doi.org/10.1007/s00198-014-2659-8.
Chung WW, Chua SS, Lai PSM, Chan SP. Effects of pharmaceutical care model on medication adherence and glycemic control of people of type 2 diabetes. Patient Preference Adherence. 2014;8:1185–94. https://doi.org/10.2147/PPA.S66619.
Lee YL, Rosnani H, Syed ASS, Syed WG, Yelly OS, Usman H. Impact of a community pharmacist-based diabetes management program on clinical outcomes measures. Int Res J Pharm Pharmacol. 2011;1(3):033–42. Available from https://www.interesjournals.org/articles/impact-of-a-community-pharmacistbased-diabetes-management-program-on-clinical-outcomes-measures.pdf. Accessed 9 Nov 2018.
Pinto SL, Kumar J, Partha G, Bechtol RA. Pharmacist-provided medication therapy management (MTM) program impacts outcomes for employees with diabetes. Popul Health Manage. 2013. https://doi.org/10.1089/pop.2012.0124.
Thavornwattanayong W, Sribundit N. Effects of family pharmacy intervention on clinical outcomes in primary care settings in Thailand. Thai J Pharm Sci. 2016;41(1):35–40. Available from http://www.thaiscience.info/Journals/Article/TJPS/10984266.pdf. Accessed 14 Sept 2019.
Cheen MHH, Goon CP, Ong WC, Lim PS, Wan CN, Leong MY, et al. Evaluation of a care transition program with pharmacist-provided home-based medication review for elderly Singaporeans at high risk of readmissions. Int J Qual Health Care. 2017;29(2):200–5. https://doi.org/10.1093/intqhc/mzw150.
Luder HR, Frede SM, Kirby JA, Epplen K, Cavanaugh T, Martin-Boone JE, et al. TransitionRx: Impact of community pharmacy postdischarge medication therapy management on hospital readmission rate. J Am Pharm Assoc. 2015;55:246–54. https://doi.org/10.1331/JAPhA.2015.14060.
Tommelein E, Mehuys E, Van Hees T, Adriaens E, Van Bortel L, Christiaens T, et al. Effectiveness of pharmaceutical care for patients with chronic obstructive pulmonary disease (PHARMACOP): A randomized controlled trial. Br J Clin Pharmacol. 2013;77(5):756–66. https://doi.org/10.1111/bcp.12242.
Chua SS, Lim KP, Lee HG. Utilisation of community pharmacists by the general public in Malaysia. Int J Pharm Pract. 2013;21:61–9. https://doi.org/10.1111/j.2042-7174.2012.00219.x.
Hassali MA, Li VMS, See OG. Pharmacy practice in Malaysia. J Pharm Pract Res. 2014;44:125–8. https://doi.org/10.1002/jppr.1024.
Loo JSE, Loh MH, Tiong JJL. An evaluation of prescriptions dispensed in Malaysian community pharmacies in the absence of dispensing separation. Indian J Pharm Sci. 2018;80(2):390–5. https://doi.org/10.4172/pharmaceutical-sciences.1000370.
Chua SS, Wong WK, Lee HG, Richard Y, Tan JSH. Implementation of the benchmarking guidelines on community pharmacies in Malaysia. Malaysian J Pharm Sci. 2008;6(1):13–31. Available from http://web.usm.my/mjps/mjps06012008/mjps06012008_2.pdf. Accessed 14 Dec 2017.
Beshir SA, Hamzah NH. Health promotion and health education: Perception, barriers and standard of practices of community pharmacists. Int J Health Promot Educ. 2014;52(4):174–80. https://doi.org/10.1080/14635240.2014.888809.
Sam AT, Jothy TH, Parasuraman S. Assessment of pharmaceutical care services provided by a community pharmacy in Kedah, Malaysia. Pharmacol Toxicol Biol. 2015;1(2):73–80. https://doi.org/10.5530/ptb.1.2.7.
Chua SS, Ramachandran CD, Paraidathathu TT. Response of community pharmacists to the presentation of back pain: a simulated patient study. Int J Pharm Pract. 2006;14:171–8. https://doi.org/10.1211/ijpp.14.3.0003.
Khan TM, Emeka P, Khan AH. Drug Information Activity and Nonprescription Requests Over the Malaysian Counter. Ther Innov Regul Sci. 2013;47(2):198–202. https://doi.org/10.1177/2168479012462214.
Cavaco A. Pharmaceutical care and patient counseling. The Pharmacist Guide to Implementing Pharmaceutical Care. In: da Costa, van Mil JWF, Alvarez-Risco A, editors. Cham: Springer; 2018. p. 33–40. https://doi.org/10.1007/978-3-319-92576-9_4.
International Pharmaceutical Federation (FIP). Counselling, concordance and communication: innovative education for pharmacists. 2nd ed. 2012. EdFIP/IPSF.11-12. Available from https://fip.org/files/fip/HaMIS/fip_ipsf_pce_2nd_2012.pdf. Accessed 5 Apr 2019.
Pharmaceutical Service Division (PSD), Ministry of Health Malaysia. Statistik farmasi 2016. 2017. Available from: https://www.pharmacy.gov.my/v2/sites/default/files/statistic/Statistik%20Farmasi%202016_0.pdf. Accessed 12 Mar 2018.
Ahmad D. Enhancing sustainability in healthcare delivery: A challenge to the New Malaysia. Malaysian J Med Sci. 2019;26(1):1–4. https://doi.org/10.21315/mjms2019.26.1.1.
Pharmaceutical Service Division (PSD), Ministry of Health Malaysia. Community pharmacy benchmarking guideline 2016. 2017. Available from https://www.pharmacy.gov.my/v2/en/documents/community-pharmacy-benchmarking-guideline.html. Accessed 14 Feb 2018.
Hassali MA, Saleem F, Khan TM, Aljadhey H, Farooqui M, Haq NU. Pharmacists’ perception of the sale of non-clinically proven health supplements in Penang, Malaysia. Trop J Pharm Res. 2013;12(3):433–8. https://doi.org/10.4314/tjpr.v12i3.23.
Bursac Z, Gauss CH, Williams DK, Hosmer D. A purposeful selection of variables macro for logistic regression. J Source Code Biol Med. 2007;3(173). Available from https://support.sas.com/resources/papers/proceedings/proceedings/forum2007/173-2007.pdf. Accessed 2 Apr 2019.
IBM. Test of model fit. Available from https://www.ibm.com/support/knowledgecenter/SSLVMB_24.0.0/spss/tutorials/log_loan_fit.html. Accessed 29 Apr 2020.
Sohn HS, Kim SO, Joo KM, Park H, Han E, Ahn HT, et al. Pharmacists’ perceptions of barriers to providing appropriate pharmaceutical services in community pharmacies. Korean J Clin Pharm. 2015;25(2):94–101. ISSN: 1226-6051.
Kelly DV, Bishop L, Young S, Hawboldt J, Phillips L, Keough TM. Pharmacist and physician views on collaborative practice: Findings from the community pharmaceutical care project. Can Pharm J. 2013;146(4):218–26. https://doi.org/10.1177/1715163513492642.
Bahari MB, Ling YW. Factors contributing to customer satisfaction with community pharmacies in Malaysia. J Public Health. 2010;18:35–41. https://doi.org/10.1007/s10389-009-0280-7.
Kho BP, Hassali MA, Lim CJ, Saleem F. A qualitative study exploring professional pharmacy services offered by community pharmacies in the state of Sarawak, Malaysia. J Pharm Health Serv Res. 2017;8(3):201–8. https://doi.org/10.1111/jphs.12181.
Chen TF, Nishtala PS. Pharmaceutical Care in Australia and New Zealand. The Pharmacist Guide to Implementing Pharmaceutical Care. In: da Costa, van Mil JWF, Alvarez-Risco A, editors. Springer, Cham; 2018. p. 173–182. https://doi.org/10.1007/978-3-319-92576-9_15.
Diaz Sierra EC, Melin K. (2014). Clinical and behavioral impact of pharmaceutical care services in community pharmacies in Puerto Rico. J Pharm Care Health Syst. 2014;S1:001. https://doi.org/10.4172/jpchs.1000-S1-001
Malaysian Community Pharmacy Guild (MCPG). Roadmap to advancing community pharmacy unveiled. 2019. Available from http://mcpg.org.my/roadmap-to-advancing-community-pharmacy-unveiled/. Accessed 19 Sept 2019.
Hersberger KE, Boeni F, Arnet I. Dose-dispensing service as an intervention to improve adherence to polymedication. Expert Rev Clin Pharmacol. 2013;6(4):413–21. https://doi.org/10.1586/17512433.2013.811829.
World Health Organization Western Pacific Region (WPRO). Ageing and health: Malaysia. 2014. Available from http://www.wpro.who.int/topics/ageing/ageing_fs_malaysia.pdf. Accessed 13 Dec 2017.
Reis TM, Guidoni CM, Girotto E, Rascado RR, Mastroianni PC, Cruciol JM, et al. Pharmaceutical care in Brazilian community pharmacies: Knowledge and practice. Afr J Pharm Pharmacol. 2015;9(9):287–94. https://doi.org/10.5897/AJPP2014.4239.
El-Dahiyat F, Curley LE, Babar Z. A survey study to measure the practice of patient counselling and other community pharmacy services in Jordan. J Pharm Health Serv Res. 2019;10(1):133–9. https://doi.org/10.1111/jphs.12272.
Fang Y, Yang S, Feng B, Ni Y, Zhang K. Pharmacists’ perception of pharmaceutical care in community pharmacy: a questionnaire survey in Northwest China. Health Soc Care Commun. 2011;19(2):189–97. https://doi.org/10.1111/j.1365-2524.2010.00959.x.
Usman MH, Ilyas OS. Assessment of knowledge, attitude and practice of community pharmacists towards pharmaceutical care in Kaduna state, Nigeria. Int J Pharm Teach Pract. 2014;5(2):972–6. Available from https://www.researchgate.net/publication/264525651_Assessment_of_Knowledge_Attitude_and_Practice_of_Community_Pharmacist_towards_Pharmaceutical_care_in_Kaduna_State_Nigeria. Accessed 14 Feb 2018.
Puspitasari HP, Aslani P, Krass I. Challenges in the management of chronic noncommunicable diseases by Indonesian community pharmacists. Pharm Pract. 2015;13(3):578. https://doi.org/10.18549/PharmPract.2015.03.578.
Deepalakshmi M, Devipriya T, Arun KP, Ponnusankar S. Knowledge, attitude and practice of community pharmacists towards cognitive pharmaceutical care services in Tamil Nadu, India. Indian J Pharm Sci. 2016;8(6):844–9. https://doi.org/10.4172/pharmaceutical-sciences.1000192.
Sarriff A, Nordin N, Hassali MAA. Extending the roles of community pharmacists: Views from general medical practitioners. Med J Malays. 2012;67(6):577–81. Available from https://www.ncbi.nlm.nih.gov/pubmed/23770948. Accessed 16 Dec 2017.
Elayeh E, Akour A, Almadaeen S, AlQhewii T, Basheti IA. Practice of pharmaceutical care in community pharmacies in Jordan. Trop J Pharm Res. 2017;16(2):463–70. https://doi.org/10.4314/tjpr.v16i2.27.
Wibowo Y, Sunderland B, Hughes J. Pharmacist and physician perspectives on diabetes service delivery within community pharmacies in Indonesia: A qualitative study. Int J Pharm Pract. 2016;24:180–8. https://doi.org/10.1111/ijpp.12227.
Ahmed NO, Al-Wahibi NS. Knowledge, attitude and practice towards pharmaceutical care in community pharmacy in Saudi Arabia. Br J Med Med Res. 2016;15(9):1–9. Article no. BJMMR.23920. https://doi.org/10.9734/BJMMR/2016/23920.
Elkalmi RM, Hassali MA, Ibrahim MIM, Liau SY, Awaisu A. A qualitative study exploring barriers and facilitators for reporting of adverse drug reactions (ADRs) among community pharmacists in Malaysia. J Pharm Health Serv Res. 2011;(2):71–8. https://doi.org/10.1111/j.1759-8893.2011.00037.x.
Chaiyakunapruk N, Jones SM, Dhippayom T, Sumpradit N. Pharmacy practice in Thailand. In: Fathelrahman A, Ibrahim M, Wertheimer A, editors. Pharmacy practice in developing countries. 1st ed. London: Academic Press; 2016.
Pharmaceutical Service Division (PSD), Ministry of Health Malaysia. Good pharmaceutical trade practice. 2015. Available from https://www.pharmacy.gov.my/v2/en/documents/good-pharmaceutical-trade-practice.html-0. Accessed 13 Apr 2018.
Pharmaceutical Service Division (PSD), Ministry of Health Malaysia. Medicine prices monitoring in Malaysia. 2018. Available from https://www.pharmacy.gov.my/v2/en/documents/medicine-prices-monitoring-2017.html. Accessed 27 Feb 2019.
Acknowledgements
We wish to thank Dr Sharmini Balashankar and Dr Adam Turner from the Faculty of Science, Nottingham University of Malaysia Campus for their guidance during the early stage of the research. A very special thanks to Ms Rhia Desai, a pharmacy student at University of Nottingham, United Kingdom, for her assistance in setting up the survey questionnaire using the Survey Monkey®. We are also very grateful to the community pharmacists who were involved in validating the questionnaires for this study: Azhar bin Najuddin, Azlie bin Md Yaakub, Bharati a/p Suresh Chand, Che Rahim bin Che Daud, Fauzan bin Mohamed Dzahir, Francis Tan Peng Nam, Goh Chun Kok, Jerry Tan Sze Eng, Lai Jian Chen, Lee Yin Chen, Lim Kean Ping, Merinda Chua Li Chuen, Mohamad Azree bin Jawawi, Naszri bin Abu Samah, Ngu Soon Hieng, Nik Jah bt Nik Ab Kadir, Pang Wee Siang, Ruhani bt Ismail, Salina bt Abdul Wahid, Sally Chuah Sze Yee, Santhanathan a/l S. Rajendram, Siah Kim Meng, Wang Leong Seng, Wan Mohd Hamidi bin Wan Sulaiman, Wong Sie Sing, and Yip Sook Ying. Permission has been obtained from all individuals for their names to be mentioned in this manuscript.
Funding
The authors did not receive any funding or financial support for this research work.
Author information
Authors and Affiliations
Contributions
PL and SSC contributed in the design of the study. PL was responsible for the preparation, data collection and analysis of the study, and also prepared the first draft of the manuscript and edited it. SSC was involved in the data analysis and interpretation as well as editing of the manuscript while MK was involved in checking and interpretation of the results as well as editing the manuscript. All authors read and approved the final manuscript.
Authors' information
PL has just been awarded the Master of Philosophy (Pharmacy) by Taylor's University, Malaysia. SSC is a Professor and the Head, School of Pharmacy, Faculty of Health & Medical Sciences, Taylor's University. MK is a senior lecturer and the Head, Department of Pharmacy Practice, Faculty of Pharmacy, Universiti Teknologi MARA Cawangan Selangor, Puncak Alam Campus, Selangor, Malaysia.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was conducted using an online survey. If the invited pharmacists agreed to participate in the study, they were required to click a checkbox for consent before they could proceed to do the questionnaire.
The study had been reviewed and approved by the Human Ethics Committee of Taylor’s University Malaysia (reference number: HEC 2018/002).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Loh, P., Chua, S.S. & Karuppannan, M. The extent and barriers in providing pharmaceutical care services by community pharmacists in Malaysia: a cross-sectional study. BMC Health Serv Res 21, 822 (2021). https://doi.org/10.1186/s12913-021-06820-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-021-06820-7