Abstract
Background
Published literature suggests that early treatment with natalizumab (“escalation strategy”) is more effective than switch within the same class of immunomodulators (interferons/glatiramer acetate, “switching strategy”) in relapsing-remitting multiple sclerosis (RRMS) patients who failed first-line self-injectable disease-modifying treatment (DMT). The present analysis aims to evaluate the cost-effectiveness profile of escalation strategy vs. switching strategy, adopting the Italian societal perspective.
Methods
A lifetime horizon Markov model was developed to compare early escalation to natalizumab vs. switching among immunomodulators, followed by subsequent escalation to natalizumab. The two compared treatment algorithms were: a) early escalation until progression to Expanded Disability Status Scale (EDSS) = 7.0 vs. b) switching until EDSS = 4.0, followed by escalation until EDSS = 7.0. The model analyzed social costs, quality-adjusted survival and effects of therapies in prolonging time without disability progression and burden of relapses. Clinical data were mainly extracted from a published observational study.
Results
Lifetime costs of early escalation to natalizumab and switching among immunomodulators amounted to €699,700 and €718,600 per patient, respectively. Early escalation was associated with prolonged quality-adjusted survival (11.19 vs. 9.67 QALYs, + 15.8%). A slight overall survival increase was also observed (20.10 vs. 19.67 life years). Both deterministic and probabilistic sensitivity analyses confirmed the robustness of findings.
Conclusions
Adopting the Italian social perspective, early escalation to natalizumab is dominant vs. switching among immunomodulators, in RRMS patients who do not respond adequately to conventional immunomodulators.
Similar content being viewed by others
Background
Multiple Sclerosis (MS) is a chronic condition, affecting young adults in the active working phase, with a significant economic and social burden [1, 2]. In most cases, patients with relapsing-remitting MS (RRMS) suffer from episodes of neurological deterioration (relapses), between periods of complete or partial remission. Transition to secondary progressive multiple sclerosis (SPMS), with or without superimposed relapses, can occur after an initial relapsing-remitting (RR) phase, leading to accumulation of irreversible disability [3]. Optimal treatment strategy then aims to minimize the occurrence of relapses and prolong the time to disability progression. As first-line treatment, RRMS patients can receive self-injectable disease-modifying treatments (DMTs), namely interferon beta (IFN) or glatiramer acetate (GA). However, a significant proportion of patients experience disease activity despite first-line DMT treatment [4]. At this stage, neurologists can decide whether switching treatment to another immunomodulator (i.e. from GA to IFN, or vice versa, or from a lower to a higher dose and/or more frequently administered IFN, hereafter called “switching strategy”) or initiating treatment with second-line therapy (i.e. from GA or IFN, to a high-efficacy DMT such as natalizumab, hereafter called “escalation strategy”) [5]. Several studies have shown that escalating to second-line therapy is more effective than switching [6, 7]. Although this evidence supports escalation from a clinical perspective, prescription of second-line treatment could lead to a relevant increase of therapeutic costs, being second-line options more expensive than first-line immunomodulators. Therefore, the economic investment for escalation should be measured against the incremental clinical benefit over switching. This analysis aims to evaluate cost-effectiveness of early escalation to natalizumab vs. switching among immunomodulators, followed by late escalation to natalizumab, in patients affected by RRMS who have failed first-line treatment with either IFNs or GA [6], adopting the Italian Societal perspective.
Method
Design and parameters
The present analysis is an economic elaboration of a previously published clinical study, conducted by Prosperini et al. [6]. Patients enrolled in this study had > 2 relapses, or 1 relapse associated with sustained disability worsening while receiving first-line DMT for at least 1 year, according to the past Italian Medicine Agency rules for escalation to natalizumab [8, 9]. In the study, patients who failed first-line therapy with one of the available IFNs or GA were split into two groups: patients switching among different IFN formulations, or from IFN to GA, or vice versa (switching strategy, SWI); patients receiving natalizumab (escalation strategy, ESC). Duration of follow-up was 24 months. At the end of the study, a larger proportion of patients were free from relapse (p < 0.0001), disability progression (p = 0.0045), magnetic resonance (MRI) activity (p = 0.0003), and combined activity (p < 0.0001), in the ESC group than in the SWI group.
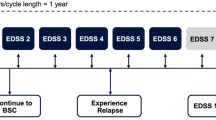
The findings of this study were used to develop a Markov model (Fig. 1) projecting the clinical and economic outcomes of ESC vs. SWI over a lifetime horizon (50 years) and comparing two treatment strategies: i) early escalation (ESC), in which patients were treated with natalizumab until Expanded Disability Status Scale (EDSS) = 7.0 was reached [10]; ii) switching (SWI), in which patients received IFN/GA until EDSS = 4.0, and then were switched to natalizumab (late escalation) and treated until EDSS = 7.0 was reached. No efficacy waning effects were modelled for natalizumab (over time), consistently with the findings of a large real-world, observational, prospective study of patients with RRMS, showing that the risk of disability progression in natalizumab-treated patients was relatively low in the long-term [11, 12]. Patients in both groups did not receive further disease-modifying treatment after EDSS> 7.0 [13,14,15]. The model was developed to measure three main clinical outcomes: disability progression, incidence of relapses and mortality.
Scheme of the Markov model [15]
In the model, pharmacological treatment of RRMS (with either ESC or SWI) reduces both disability progression and incidence of relapses, and improves quality of life, with an indirect impact on life expectancy [16,17,18,19,20]. Over time, EDSS score of each patient could increase (disability progression), decrease (disability regression), or remain stable (disability maintenance). Additionally, patients had a certain probability of progressing to SPMS. It was assumed that: i) treatments did not have any effect in preventing transition from RRMS to SPMS and in delaying disability progression while in the SPMS form; ii) patients affected by SPMS did not receive any DMT.
The model simulates mortality, disability progression (measured through EDSS), relapse occurrence and transition to secondary progressive multiple sclerosis (SPMS). As a consequence, the model provides estimates of overall survival (Life Years, LYs), quality-adjusted survival e (Quality-Adjusted Life Years, QALYs), overall costs, and finally of the incremental cost effectiveness ratio (ICER) per QALY gained.
The Italian Societal perspective was adopted. Outcomes and costs were evaluated over a 50-year time horizon (lifetime horizon) and discounted at 3.50%, in line with technology appraisal best practices, recommended by National Institute for Health and Care Excellence (NICE) [21]. A complete list of the input data used in this analysis is shown in Additional file 1: Table S1-S6.
Clinical data
The cohort of RRMS patients enrolled in the study conducted by Prosperini et al. [6] was used to run the present analysis. The mean age of the cohort was 35.3 years (SD: 8.3 years); 65.8% of patients were females. The mean number of relapses during the year preceding enrolment was 1.7 (SD: 0.7), and the mean patient EDSS score was 2.6 (SD: 1.1). Most patients (85.50%) had EDSS< 4 at the time of enrolment. Patients in the SWI group were mainly treated with high dose beta IFN (IFN beta 1a 44 mcg subcutaneous, 58.4%, or IFN beta 1b, 8.7%) or with GA (32.9%), reflecting quite well the Italian practice on first-line treatment of RRMS.
Data on the incidence of relapses were extracted from a mixed treatment comparison (MTC) used in previous Italian economic evaluations [22,23,24], and then combined with results of Prosperini et al. [6]. In absence of treatment, patients affected by RRMS and SPMS had an annualized relapse rate (ARR) depending on the EDSS score (Table 1). The ARRs for the RRMS form for EDSS scores 0–7 were retrieved from Prosperini et al. [6]. The remaining relapse rate data (RRMS form, EDSS scores 8–10; SPMS, all EDSS scores) were retrieved from multiple sources [25,26,27], due to a lack of data in the Prosperini study [6].
According to the MTC, immunomodulators reduced the risk of ARR of 33–36% in the RRMS cohort [22]. This effect was consistent with the findings observed in the Prosperini study, where the weighted treatment reduction effect observed in the switching group vs. baseline was 0.6574 (− 34%; average treatment effect weighted by treatment distribution [6]). The resulting effect associated with natalizumab on ARR was 0.3024, as escalation to natalizumab reduced the relapse risk by 54% vs. switching [6] (RR: 0.46; IC 95%: 0.31–0.68).
Annual transition probabilities for disability progression (measured through EDSS score) were calculated using patient-level data on EDSS change from enrolment to Month 24 [6]. The annual probability was calculated as the average of the EDSS change between Month 12 vs. baseline, and Month 24 vs. Month 12. These probabilities were used to set transition probabilities in the RRMS state. In the ESC group, probabilities of − 1 point, 0 point, + 1 point, + 2 points, + 3 points of EDSS change vs. baseline were: 0.0236, 0.8727, 0.0849, 0.0189, 0.000, respectively. In the SWI group, probabilities of − 1 point, 0 point, + 1 point, + 2 points, + 3 points of EDSS change vs. baseline were: 0.0000, 0.8199, 0.1553, 0.0217, 0.0031 respectively. The Markov model was finalized using two additional clinical inputs: i) probabilities of transition from the RRMS form to the SPMS form; ii) probabilities of disability progression for SPMS patients. Both sets of data were retrieved from the London Ontario dataset, one of the longest and most complete observational registries on multiple sclerosis, collecting MS data from 1972 and 2000 [28,29,30].
The annual incidence of adverse events (AEs) by treatment was retrieved from a systematic literature review [22, 24, 31]. AEs were also classified as serious and non-serious, to consider their different effect on costs and outcomes. Mortality rates, stratified by age and gender, were retrieved from national registries of the Italian Statistics Institute (ISTAT) [32]. Mortality rates of the general population were adjusted by the additional death risk attributable to multiple sclerosis, depending on both MS form and EDSS level [33].
Quality of life data
Utilities of patients affected by RRMS, stratified by EDSS level, were retrieved from recent pivotal clinical trials [34, 35] measuring quality of life with EuroQoL EQ5D assessments for each EDSS state. Utilities associated with the SPMS form and relapse-related disutilities were determined adjusting the above-mentioned utilities for the RRMS form by negative coefficients retrieved from a survey conducted in the UK, evaluating the QoL deterioration due to disease progression [36]. These disutility factors were − 0.0092 and − 0.0437, for transition to SPMS and relapse occurrence, respectively.
Disutilities associated with treatment-related AEs and relapses were also incorporated in the model. AE-related disutilities depended on type and grade (serious vs. non-serious) of the adverse events and had a temporary, reversible effect on patients’ quality of life (duration range: 1 day - 6 months per year). These values were estimated and validated through clinical expert opinion.
Economic data
This economic analysis was conducted adopting the Italian Societal perspective and considering the cost of disability, treatment acquisition, administration, monitoring, relapses, AEs, productivity loss and non-healthcare direct costs. Disability-related costs were retrieved from the study conducted by Karampampa et al. [1]. Table 2 reports disability-related costs included in the model, expressed in Euro, November 2015 [37].
The economic impact of pharmacological treatment was expressed as net annual cost per patient, using ex-manufacturer price of single drug packs, and subtracting all rebates applied to the Italian National Healthcare System (NHS, Table 3). Administration costs were assumed equal to €0 for all the treatments included in the analysis (as IFNs and GA can be self-administered, subcutaneously or intramuscularly), except for natalizumab (€589.78: weighted average tariff of ambulatory administration [38], 80% of cases, and day-hospital administration [39], 20% of cases). Annual monitoring costs were calculated assuming that the patients would comply with the main recommendations for RRMS. Clinical guidelines issued by the Emilia Romagna Region [40, 41] were used to estimate the cost of follow-up. Table 3 shows monitoring costs, by treatment. To estimate the cost of a relapse, data from Kobelt et al. [2] was used. The relapse management estimated cost (€4000) was adjusted for inflation to November 2015 (€4744). The economic impact of AEs was calculated assuming that mild-to-moderate events would be managed either by the general practitioner (GP) [42] or by the specialist [38], while severe events were managed in day-hospital or through standard hospitalization [39], depending on the event (expert opinion).
Sensitivity analysis
Both univariate deterministic and probabilistic sensitivity analyses were conducted to identify the effects of input variability on the overall results of the analysis. The deterministic sensitivity analysis tested the effect of the following parameters: i) +/− 10% therapy costs; ii) +/− 10% direct disability costs; iii) +/− 10% relapse costs; iv) +/− 10% utility values; v) initiation of natalizumab at EDSS> = 3.0 in the SWI group; vi) initiation of natalizumab at EDSS> = 5.0 in the SWI group. For the probabilistic analysis, the following distributions were used: lognormal for clinical variables (relapse rates, adverse event rates, mortality risk increase due to MS, utilities and disutilities); beta for EDSS transition probabilities (in the switching and escalation groups); gamma for costs. A 10% standard error of the mean value of each variable was used to run probabilistic sensitivity analysis.
Results
Table 4 shows the results of the analysis. Total lifetime social costs amounted to €699,676 and €718,604 in the ESC and SWI groups, respectively. In both groups, treatment costs and indirect costs were the most relevant drivers of expenditure, absorbing 85% of costs in the ESC group and 82% in the SWI group. The higher treatment and administration costs, monitoring costs and AE costs in the ESC group were offset by savings for the reduction of relapse burden and the delaying of disability progression, both reducing direct and indirect costs. The economic burden of AEs was negligible. Early adoption of escalation to natalizumab was more effective than switching among immunomodulators (IFNs and GA), leading to an increase of the discounted quality-adjusted survival (+ 1.52 QALYs; 11.19 in the ESC group, vs. 9.67 in the SWI group). The cost-effectiveness analysis showed that ESC dominated SWI in the societal perspective, being associated with lower costs and longer quality-adjusted survival. Early escalation of RRMS patients determined prolonged survival at a lower level of disability.
This result is shown in Fig. 2: after 15 years of observation, about 60% patients in the ESC group and 70% in the SWI group have an EDSS score greater than 5 (absolute reduction: − 10%). The clinical difference between the two groups reaches its maximum at around Year 30. Then the effect of mortality, similar in the two groups, progressively reduces the benefit. Similarly, the effect of relapse occurrence was reduced in the ESC group. The cumulative analysis conducted on relapses showed that, at the end of the observation, patients in the ESC group experienced fewer episodes than patients in the SWI group (8.84 vs. 12.09, respectively). For all tested scenarios, the results of the univariate sensitivity analysis confirmed early escalation to natalizumab being dominant over switching among IFNs and GA (Additional file 1: Table S7). Finally, probabilistic analysis (N = 1000 simulations) showed that ESC was cost-effective vs. SWI in 85.9% of cases, using a willingness to pay threshold of € 50,000 per QALY gained [51, 52]. In 54.4% of cases, the escalation strategy dominated the switching strategy (Fig. 3).
Discussion
The broad experience achieved with natalizumab in pivotal clinical trials and in observational studies offers obust evidence of its effectiveness in RRMS patients (both naïve or who failed first-line DMT). Recently, the European Medicine Agency (EMA) approved the extension of natalizumab indication in patients with highly active RRMS despite a full and adequate course of treatment with at least one DMT, thus simplifying conditions for escalation [53]. Moreover, the recent review of the benefit-risk profile of natalizumab, conducted by EMA, led to the renewal of the marketing authorization with unlimited validity [54]. The present analysis provides evidence that escalation to natalizumab is a cost-effective option vs. switching among immunomodulators in RRMS patients who failed first-line therapy (IFNs, GA). To our knowledge, this is the first attempt of evaluating economic consequences of early escalation vs. switching in Italy. The clinical data used to conduct the present analysis were mainly derived from an observational analysis conducted in Italy. Each economic assessment is a dynamic process because: i) clinical efficacy data must be confirmed in real practice; ii) certain input data, such as prices of treatments, can change over time; iii) new technologies become available for patients. With this cost-utility analysis we were able to capture two relevant outcomes of the health technology assessment: costs and quality of life. Results of the analysis show that pharmacological expenditure is a relevant cost for healthcare services, but there are other non-negligible costs contributing to healthcare and social economic impact. In fact, although acquisition costs with natalizumab were substantially higher than IFNs and GA in our analysis, early escalation produced savings which entirely offset the investment with natalizumab, thus making escalation a dominant (i.e. less expensive and more effective) alternative vs. switching. Moreover, early escalation led to improved patient quality of life, prolonged survival with lower disability and slightly prolonged overall survival. Finally, these findings were confirmed in all tested scenarios (base-case, one-way sensitivity analysis, probabilistic analysis). In our base case analysis, we decided to adopt a societal perspective, as we aimed to capture the significant economic burden of multiple sclerosis, beyond costs sustained by our healthcare service. Indeed, in their Italian cost-of-illness assessment, Kobelt et al. [2] showed that direct healthcare costs of MS accounted for 28.6% of total per-patient costs, with total direct non-medical costs and productivity loss costs contributing for the remaining 42.3 and 29.1%, respectively.
Despite long-term modelling of costs and clinical consequences can be affected by some methodological limitations (iteration of clinical efficacy results, typically adopted in Markov models, provides a “proxy” of the real evolution of the disease) we believe this analysis is robust enough in terms of clinical efficacy model inputs (most of them were retrieved from published literature) and cost assumptions (retrieved from published literature and consistent with previous Italian publications on RRMS). Likely, the main limitation of this analysis concerns the use of data from a general RRMS population to estimate the natural history of the disease of a highly active RRMS population. Of course, the use of more specific data on highly active RRMS patients would have allowed a more accurate estimate of the clinical outcomes. Unfortunately, to our knowledge, such data are not available. However, we believe this bias disfavoured the option of escalating to natalizumab. Intuitively, the clinical benefits of a therapy reducing disability should be even more evident in a cohort of patients with highly active disease, characterized by faster disability progression. A second limitation of the study was that we did not use EDSS-dependant transition probabilities to model disease progression in the RRMS disease state. We adopted this approach as we did not have adequate sample size in the original study to calculate disability progression rates by EDSS state. Nevertheless, we believe that the benefit of using “real-data” on this specific target population would exceed the drawback of the lack of EDSS-dependant transition probabilities. Moreover, we tested the variability of this parameter in our sensitivity analyses, to get confirmation that the uncertainty associated with this variable would not determine a significant modification of the ICER estimates. Considering all these factors, we acknowledge that the present economic analysis does not represent a conclusive guidance for early treatment of natalizumab, which depends on several clinical factors. The findings of this analysis should be rather considered as a proof of the fact that the current economic evidence supports the escalation of natalizumab in the Italian setting, when this approach is considered appropriate from a clinical perspective. Furthermore, this economic analysis is adopting the Italian societal perspective. Therefore, caution should be taken around the validity of such conclusions in other countries.
Conclusions
The results of this study showed that early escalation to natalizumab in RRMS patients who do not respond adequately to conventional immunomodulators (IFNs, GA) led to both clinical and economic benefits, compared to switching among immunomodulators (IFNs, GA). Overall, the escalation approach: i) improved quality of life, ii) prolonged survival with lower disability, and iii) slightly prolonged overall survival. Although natalizumab acquisition costs were substantially higher than IFNs and GA, early escalation produced savings. Taking together, our findings showed that early escalation to natalizumab was a dominant option for the treatment of RRMS patients who do not respond adequately to conventional immunomodulators (IFNs, GA).
Availability of data and materials
The main data source of this analysis is the study Prosperini et al., Mult Scler 2012 (available at: https://doi.org/10.1177/1352458511417481).
Abbreviations
- AEs:
-
Adverse events
- ARR:
-
Annualised relapse rate
- DMT:
-
Disease modify therapy
- EDSS:
-
Expanded Disability Status
- EMA:
-
European Medicine Agency
- ESC:
-
Patients receiving natalizumab
- GA:
-
Glatiramer acetate
- ICER:
-
Incremental cost effectiveness ratio
- IFN:
-
Interferon beta
- ISTAT:
-
Italian Statistics Institute
- MS:
-
Multiple Sclerosis
- MTC:
-
Mixed treatment comparison
- NHS:
-
National Healthcare System
- NICE:
-
National Institute of Health and Care Excellence
- QALYs:
-
Quality-adjusted survival
- RR:
-
Relapsing-remitting
- RRMS:
-
Relapsing-remitting multiple sclerosis
- SPMS:
-
Secondary progressive multiple sclerosis
- SWI:
-
Patients switching among different IFN formulations, or from IFN to GA, or vice versa
References
Karampampa K, Gustavsson A, Miltenburger C, Teruzzi C, Fattore G. Treatment experience, burden and unmet needs (TRIBUNE) in MS study: results from Italy. Mult Scler J. 2012;18(2_suppl):29–34. https://doi.org/10.1177/1352458512441566c.
Kobelt G, Berg J, Lindgren P, Battaglia M, Lucioni C, Uccelli A. Costs and quality of life of multiple sclerosis in Italy. Eur J Health Econ. 2006;7:45–54. https://doi.org/10.1007/s10198-006-0385-7.
Lublin FD, Reingold SC, Cohen JA, Cutter GR, Sørensen PS, Thompson AJ, et al. Defining the clinical course of multiple sclerosis: the 2013 revisions. Neurology. 2014;83:278–86. https://doi.org/10.1212/WNL.0000000000000560.
Rudick RA, Polman CH. Current approaches to the identification and management of breakthrough disease in patients with multiple sclerosis. Lancet Neurol. 2009;8:545–59. https://doi.org/10.1016/s1474-4422(09)70082-1.
Dörr J, Paul F. The transition from first-line to second-line therapy in multiple sclerosis. Curr Treat Options Neurol. 2015;17:354. https://doi.org/10.1007/s11940-015-0354-5.
Prosperini L, Giannì C, Leonardi L, De Giglio L, Borriello G, Galgani S, et al. Escalation to natalizumab or switching among immunomodulators in relapsing multiple sclerosis. Mult Scler J. 2012;18:64–71. https://doi.org/10.1177/1352458511417481.
Spelman T, Kalincik T, Zhang A, Pellegrini F, Wiendl H, Kappos L, et al. Comparative efficacy of switching to natalizumab in active multiple sclerosis. Ann Clin Transl Neurol. 2015;2:373–87. https://doi.org/10.1002/acn3.180.
Mancardi GL, Tedeschi G, Amato MP, D’Alessandro R, Drago F, Milanese C, et al. Three years of experience: the Italian registry and safety data update. Neurol Sci. 2011;31(Suppl 3):295–7. https://doi.org/10.1007/s10072-010-0356-8.
Italian Medicines Agency (AIFA). Reimbursement and price regimen of Tysabri. Gazette n. 292; December 16, 2006.
Kurtzke JF. A new scale for evaluating disability in multiple sclerosis. Neurology. 1955;5:580–3.
Butzkueven H, Kappos L, Pellegrini F, Trojano M, Wiendl H, Patel RN, et al. Efficacy and safety of natalizumab in multiple sclerosis: interim observational programme results. J Neurol Neurosurg Psychiatry. 2014;85:1190–7. https://doi.org/10.1136/jnnp-2013-306936.
Trojano M, Butzkueven H, Kappos L, Wiendl H, Spelman T, Pellegrini F, et al. Natalizumab treatment shows low cumulative probabilities of confirmed disability worsening to EDSS milestones in the long-term setting. Mult Scler Relat Disord. 2018;24:11–9. https://doi.org/10.1016/j.msard.2018.04.020.
National Institute for Health and Clinical Excellence (NICE). Natalizumab for the treatment of adults with highly active relapsing-remitting multiple sclerosis. NICE Technol Apprais Guid 127. 2007; August:21. https://www.nice.org.uk/guidance/ta127/resources/natalizumab-for-the-treatment-of-adults-with-highly-active-relapsingremitting-multiple-sclerosis-pdf-82598138383813. Accessed 19 Dec 2018.
Battaglia M, Kobelt G, Ponzio M, Berg J, Capsa D, Dalén J, et al. New insights into the burden and costs of multiple sclerosis in Europe: results for Italy. Mult Scler. 2017;23(2_suppl):104–16. https://doi.org/10.1177/1352458517708176.
Gani R, Giovannoni G, Bates D, Kemball B, Hughes S, Kerrigan J. Cost-effectiveness analyses of Natalizumab (Tysabri®) compared with other disease-modifying therapies for people with highly active relapsing-remitting multiple sclerosis in the UK. Pharmacoeconomics. 2008;26:617–27. https://doi.org/10.2165/00019053-200826070-00008.
Jacobs LD, Cookfair DL, Rudick RA, Herndon RM, Richert JR, Salazar AM, et al. Intramuscular interferon beta-1a for disease progression in relapsing multiple sclerosis.PRISMS (prevention of relapses and disability by interferon beta-1a subcutaneously in multiple sclerosis) study group. Ann Neurol. 1996;39:285–94. https://doi.org/10.1002/ana.410390304.
Interferon beta-1b in the treatment of multiple sclerosis: final outcome of the randomized controlled trial. The IFNB Multiple Sclerosis Study Group and The University of British Columbia MS/MRI Analysis Group. Neurology. 1995;45:1277–85. doi:https://doi.org/10.1212/WNL.45.7.1277.
Jacobs LD, Cookfair DL, R a R, Herndon RM, Richert JR, Salazar AM, et al. Intramuscular interferon beta-1a for disease progression in relapsing multiple sclerosis. The multiple sclerosis collaborative research group (MSCRG). Ann Neurol. 1996;39:285–94. https://doi.org/10.1002/ana.410390304.
Ebers GC. Randomised double-blind placebo-controlled study of interferon beta-1a in relapsing/remitting multiple sclerosis. PRISMS (prevention of relapses and disability by interferon beta-1a subcutaneously in multiple sclerosis) study group. Lancet. 1998;352:1498–504. https://doi.org/10.1016/S0140-6736(98)03334-0.
Polman CH, O’Connor PW, Havrdova E, Hutchinson M, Kappos L, Miller DH, et al. A randomized, placebo-controlled trial of Natalizumab for relapsing multiple sclerosis. N Engl J Med. 2006;354:899–910. https://doi.org/10.1056/NEJMoa044397.
National Institute for Health and Clinical Excellence (NICE). Guide to the methods of technology appraisal 2013. NICE; 2013. doi:https://doi.org/10.2165/00019053-200826090-00002.
Hutchinson M, Fox RJ, Havrdova E, Kurukulasuriya NC, Sarda SP, Agarwal S, et al. Efficacy and safety of BG-12 (dimethyl fumarate) and other disease-modifying therapies for the treatment of relapsing–remitting multiple sclerosis: a systematic review and mixed treatment comparison. Curr Med Res Opin. 2013;30:613–27. https://doi.org/10.1185/03007995.2013.863755.
Furneri G, Marchesi C, Santoni L. Budget impact analysis of delayed-release Dimethylfumarate in the treatment of relapsing-remitting multiple sclerosis in Italy. Value Heal. 2015;18:A700–1. https://doi.org/10.1016/j.jval.2015.09.2619.
Furneri G, Santoni L, Marchesi C, Iannazzo S, Cortesi PA, Caputi AP, et al. Cost-effectiveness analysis of delayed-release dimethyl-fumarate in the treatment of relapsing-remitting multiple sclerosis in Italy. Farmeconomia Heal Econ Ther pathways. 2016;17:67. https://doi.org/10.7175/fe.v17i2.1251.
Calabresi PA, Kieseier BC, Arnold DL, Balcer LJ, Boyko A, Pelletier J, et al. Pegylated interferon beta-1a for relapsing-remitting multiple sclerosis (ADVANCE): a randomised, phase 3, double-blind study. Lancet Neurol. 2014;13:657–65. https://doi.org/10.1016/s1474-4422(14)70068-7.
Orme M, Kerrigan J, Tyas D, Russell N, Nixon R. The effect of disease, functional status, and relapses on the utility of people with multiple sclerosis in the UK. Value Heal. 2007;10:54–60. https://doi.org/10.1111/j.1524-4733.2006.00144.x.
Patzold U, Pocklington PR. Course of multiple sclerosis. Acta Neurol Scand. 1982;65:248–66. https://doi.org/10.1111/j.1600-0404.1982.tb03084.x.
Weinshenker BG, Bass B, Rice GP, Noseworthy J, Carriere W, Baskerville J, et al. The natural history of multiple sclerosis: a geographically based study. 2. Predictive value of the early clinical course. Brain. 1989;112 ( Pt 6):1419–1428. http://www.ncbi.nlm.nih.gov/pubmed/2597989. Accessed 11 Dec 2017.
Cottrell DA, Kremenchutzky M, Rice GP, Koopman WJ, Hader W, Baskerville J, et al. The natural history of multiple sclerosis: a geographically based study. 5. The clinical features and natural history of primary progressive multiple sclerosis. Brain. 1999;122 ( Pt 4):625–639. http://www.ncbi.nlm.nih.gov/pubmed/10219776. Accessed 11 Dec 2017.
Kremenchutzky M, Rice GPA, Baskerville J, Wingerchuk DM, Ebers GC. The natural history of multiple sclerosis: a geographically based study 9: observations on the progressive phase of the disease. Brain. 2006;129(Pt 3):584–94. https://doi.org/10.1093/brain/awh721.
Biogen. Natalizumab post marketing surveillance. 2014.
National Institute of Statistics (ISTAT). Mortality tables 2014. http://demo.istat.it/unitav2012/index.html?lingua=ita. Accessed 28 Jan 2013.
Pokorski RJ. Long-term survival experience of patients with multiple sclerosis. J Insur Med 1997;29:101–106. http://www.ncbi.nlm.nih.gov/pubmed/10169627. Accessed 23 Feb 2017.
Gold R, Kappos L, Arnold DL, Bar-Or A, Giovannoni G, Selmaj K, et al. Placebo-controlled phase 3 study of Oral BG-12 for relapsing multiple sclerosis. N Engl J Med. 2012;367:1098–107. https://doi.org/10.1056/nejmoa1114287.
Fox RJ, Miller DH, Phillips JT, Hutchinson M, Havrdova E, Kita M, et al. Placebo-controlled phase 3 study of Oral BG-12 or Glatiramer in multiple sclerosis. N Engl J Med. 2012;367:1087–97. https://doi.org/10.1056/nejmoa1206328.
UK Multiple Sclerosis Survey. Patient demographics, regression model on EDSS, relapse, type of MS and other variables on utility derived from EQ-5D. 2007.
National Institute of Statistics (ISTAT). Calculation of inflation rates. National Institute of Statistics (ISTAT). http://rivaluta.istat.it/Rivaluta/. Accessed 5 Aug 2016.
Ministry of Health. Outpatient care tariffs. Gazette n. 23, Supplement n. 8; January 28, 2013.
Ministry of Health. Hospitalization tariffs. Gazette n. 23, Supplement n. 8; January 28, 2013.
Emilia-Romagna Region. Department of Health Policies. Regional diagnosis and treatment pathway for multiple sclerosis. May 2011. 2011. www.saluter.it/documentazione/ptr/elaborati/128_sclerosi_multipla.pdf.
Region., Friuli Venezia Giulia D of HP. Outpatient care tariffs. 2015. https://www.regione.fvg.it/rafvg/export/sites/default/RAFVG/salute-sociale/sistema-sociale-sanitario/FOGLIA51/allegati/27022015_specialistica_sito.pdf.
Garattini L, Castelnuovo E, Lanzeni D, Viscarra C, Gruppo di studio DYSCO VISITE DV. Durata e costo delle visite in medicina generale: il progetto DYSCO. Farmeconomia Heal Econ Ther pathways. 2003;4:109. https://doi.org/10.7175/fe.v4i2.773.
Italian Medicines Agency (AIFA). Reimbursement and price regimen of Tysabri. Gazette n. 139; June 10, 2006.
Italian Medicines Agency (AIFA). Measures related with certain medicinal products for human use. Gazette n. 196, Supplement n. 154; August 25, 2009.
Italian Medicines Agency (AIFA). Reimbursement and price regimen of Rebif. Gazette n. 274; November 24, 2011.
Italian Medicines Agency (AIFA). Reimbursement and price regimen of Betaferon. Gazette n. 127; June 2, 2000.
Italian Medicines Agency (AIFA). Reimbursement and price regimen of Betaferon. Gazette n. 279, Supplement n. 250; November 30, 2007.
Italian Medicines Agency (AIFA). Marketing authorization for the product for human use Copaxone. Gazette n. 106; May 9, 2005.
Italian Medicines Agency (AIFA). Reimbursement and price regimen of Avonex. Gazette n. 11; January 15, 2004.
Italian Medicines Agency (AIFA). Reimbursement and price regimen of Avonex. Gazette n. 272; November 8, 2011.
Messori A, Santarlasci B, Trippoli S, Vaiani M. Controvalore economico del farmaco e beneficio clinico: stato dell’arte della metodologia e applicazione di un algoritmo farmacoeconomico. PharmacoEconomics Ital Res Artic. 2003;5:53–67. https://doi.org/10.1007/BF03320605.
Neumann PJ, Cohen JT, Weinstein MC. Updating cost-effectiveness — the curious resilience of the $50,000-per-QALY threshold. N Engl J Med. 2014;371:796–7. https://doi.org/10.1056/NEJMp1405158.
European Medicine Agency (EMA). Natalizumab: Summary of Product Characteristics. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/000603/WC500044686.pdf. Accessed 1 Mar 2017.
European Commission. Renewing and amending the marketing authorisation for the medicinal product for human use "Tysabri - Natalizumab" granted by Decision C (2006). http://ec.europa.eu/health/documents/community-register/2016/20160418134501/dec_134501_en.pdf. Accessed 1 Mar 2017.
Acknowledgements
We would like to thank all the people involved in the preparation of the abstract: Furneri G, Santoni L, Ricella C, Prosperini L. Cost-Effectiveness of Escalating to Natalizumab or Switching Among Immunomodulators In Relapsing-Remitting Multiple Sclerosis In Italy. Value in Health. 2015 Nov 1;18(7):A695., used to support the poster presentation at ISPOR 18th Annual European Congress, 2015 Milan.
Funding
This analysis was financially supported by Biogen Italy (Milan, Italy). Biogen reviewed and approved the content of the economic analysis, was involved in writing the manuscript and in reviewing the final content of the manuscript.
Author information
Authors and Affiliations
Contributions
LP conceptualized the study. All authors contributed to modelling design. LP and GF analysed data and developed the economic model. LS and CR reviewed the content of the economic analysis and approved it. LP, LS and GF wrote the manuscript for scientific publication. LS and CR reviewed the final content of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The original data used in this study are from Prosperini et al., Mult Scler 2012 (available at: https://doi.org/10.1177/1352458511417481). Since this study was classified as post-marketing observation, Ethical Committee of Sapienza University, viale del policlinico 1, 00185, Rome, Italy, president prof Aldo Isidori provided exemption of approval and consent to conduct the study.
Consent for publication
Not applicable.
Competing interests
Furneri G.: consulting fees from Biogen Italy for analysis conduction; Santoni L. and Ricella C.: employees of Biogen Italy; Prosperini L.: in the last 2 years, received consulting fees from Biogen and Novartis, and speaking honoraria and travel grants from Biogen, Genzyme, Novartis and Teva.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
Additional file 1:
Description of data: inputs used in cost-effectiveness model. (DOCX 48 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Furneri, G., Santoni, L., Ricella, C. et al. Cost-effectiveness analysis of escalating to natalizumab or switching among immunomodulators in relapsing-remitting multiple sclerosis in Italy. BMC Health Serv Res 19, 436 (2019). https://doi.org/10.1186/s12913-019-4264-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-019-4264-1