Abstract
Background
The shortage of benzathine penicillin G (BPG) worldwide presents a major challenge in the treatment of syphilis. Its availability for syphilis treatment has not been adequately evaluated in China.
Methods
Two surveys were conducted among hospitals providing sexually transmitted infection clinical services in Shandong Province in 2012 and 2018. Data on the basic information and BPG availability of the surveyed hospitals and related factors were collected and analyzed using SPSS 17.0.
Results
A total of 433 and 515 hospitals were surveyed in 2012 and 2018, respectively. A significant difference in BPG availability was observed among different levels and types of hospitals both in 2012 (X2 = 9.747, p = 0.008; X2 = 37.167, p = 0.000) and 2018 (X2 = 11.775, p = 0.003; X2 = 28.331, p = 0.000). The BPG availability among surveyed hospitals increased from 45.0% in 2012 to 56.4% in 2018 (X2 = 11.131, p = 0.001). The BPG availability was higher in 2018 than in 2012 among county-level hospitals (52.0% vs. 40.8%, X2 = 7.783, p = 0.005), general western medicine hospitals (62.1% vs. 50.0%, X2 = 6.742, p = 0.009), maternal and child health hospitals (57.1% vs. 26.9%, X2 = 13.906, p = 0.000), and public hospitals (56.8% vs. 45.0%, X2 = 11.361, p = 0.001). However, the county-level availability of BPG (at least one hospital has BPG in a county-level unit) has not improved between 2012 and 2018 (65.93% vs. 70.34%; X2 = 0.563, p = 0.453). The absences of clinical needs, restriction of clinical antibacterial drugs, and lack of qualifications for providing syphilis treatment were the major reasons for the low BPG availability of hospitals.
Conclusions
BPG availability for syphilis treatment in Shandong Province remains low and presents disparities among different levels and types of hospitals, although it has been improved in recent years. The low availability of BPG for syphilis treatment in China is related to its clinical use by doctors rather than the market supply. Health care reforms should further improve the availability and accessibility of health services.
Similar content being viewed by others
Background
Syphilis is a chronic, multistage disease caused by Treponema pallidum (TP), with a global burden of 17.7 million cases and 5.6 million new infections per year [1]. One-third of untreated syphilis cases progress to late stage, resulting in profound morbidity and even death [2]. Untreated maternal syphilis can lead to serious complications, with an estimated 930,000 maternal syphilis infections that caused 350,000 adverse pregnancy outcomes in 2012 worldwide [3]. In addition, syphilis can increase the risk of acquiring HIV infection [4].
Syphilis is a unique sexually transmitted infection (STI) that remains curable with a single dose of long-acting benzathine penicillin G (BPG) without documented risk of resistance [5]. Although doxycycline, azithromycin, and ceftriaxone have the advantages of obtaining an equivalent efficacy in the treatment of early syphilis as penicillin, treating other coexisting STIs and penicillin-allergic patients, these regimens require multiple daily doses and are more cumbersome and expensive than a single dose of BPG [6,7,8]. Furthermore, tetracyclines are contraindicated during pregnancy [9]. Azithromycin is not recommended for the treatment of syphilis-infected fetus because it does not cross the placenta [10]. The emergence of azithromycin resistance mutations in TP has resulted in treatment failure and limited its usefulness in many regions [11]. Ceftriaxone can cross the placental barrier, but the optimal dose and duration of therapy for pregnant women are unknown and may increase the risk of kernicterus in newborns [12, 13]. No other antibiotics have superiority over penicillin for the treatment of syphilis [6]. Despite the disparity of type, dose, and duration of treatment among the guidelines across different countries around the world, penicillin is still an essential antibiotic for the treatment and prevention of syphilis [2].
However, the shortage of BPG worldwide presents a major challenge in the treatment of syphilis [14]. The World Health Organization noted that more than 3 million treatments per year globally are needed for syphilis and rheumatic heart disease [15]. Approximately 5.6 million doses of 2.4 million units of BPG are needed annually to treat all syphilis cases globally [1, 16]. Among 95 surveyed countries and territories, 39 reported a shortage of the medicine [17]. BPG shortage has affected the treatment and prevention of syphilis globally and was recognized by the 69th World Health Assembly in 2016 as an essential medicine that has been in short supply for several years [18].
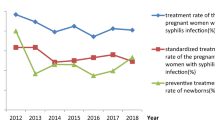
China is the most populous country in the world with high syphilis disease burden. A total of 475,860 new cases of syphilis were reported in China in 2017 [19]. Accordingly, about 1–1.5 million doses of the 2.4 million units of BPG are needed annually for their treatment (2–3 doses of BPG for each case according to Chinese guideline), which may even be approximately 5.2 times more [20]. Approximately 30,882 women diagnosed syphilis during pregnancy and 30,882 live born infants needed treatment in 2012 in China [17]. China is not among the 39 countries with a shortage of BPG. However, the demand for BPG has not been consistently and adequately quantified in China. In 2013, 55.4% of the 15,884 reported pregnant women with syphilis infection in China did not receive treatment or initiated the treatment after 37 gestational weeks, and 14.0% suffered from serious adverse pregnancy outcomes [21]. What has led to the inadequate treatment of syphilis patients in Shandong? How is the availability of BPG for syphilis treatment in Shandong? We conducted a survey in 2012 and 2018 in Shandong Province to evaluate the availability of BPG for syphilis treatment and provide a basis for policy making.
Study setting and methods
Study site
The study was conducted in Shandong Province, China. Shandong, located on the eastern coast of China, is subdivided into 17 prefecture–level cities and 137 county–level units. By 2017, a total of 2450 hospitals had been registered in the province, including 863 public and 1587 private hospitals, where 761 are Class II and above (or county–level and above hospitals), 133 are specialized (including dermatological hospitals), 161 are maternal and child health, and 300 are Chinese medicine hospitals [22].
Study objects
All hospitals providing STI clinical services in Shandong Province meet the criteria of inclusion. The hospitals included in the study were based on the list of those that reported syphilis cases in the past year. Hospitals under county–level, such as township hospitals and health centers, which only provide syphilis screening and referral service, were excluded from this study. Some military and enterprises hospitals were included and classified according to their scale, affiliation, and services they provide.
Data collection
The first survey was conducted in 2012 as a part of baseline assessment for the National Program for Prevention and Control of Syphilis in China (2010–2020) [23]. Contents related to this study were covered, including basic information of the hospitals (level, type, and affiliation), availability of a department of STI services, and provision of BPG. To assess the effectiveness of the program, we conducted the second survey in 2018. In addition to the content of the first survey, related factors to the unavailability of BPG were explored. A questionnaire was used in each survey in data collection. Health staff from the Center for Diseases Control and Prevention at county–level visited each hospital in their respective jurisdictions and filled in the questionnaire (Additional file 1).
Statistical analysis
Data collected were entered into Microsoft Excel for Windows (2012) and analyzed with SPSS 17.0 (IBM, Armonk, NY). The availability of BPG among hospitals according to levels, types, and affiliation was compared. The availability of BPG was considered when BPG was available in a hospital during the survey. Descriptive analysis and Chi–square were used for statistical analysis.
Results
In the 2012 survey, 429 hospitals responded among 471 in 17 prefecture–level cities including 135 county–level units (counties or districts or county–level cities) that reported syphilis cases in the past year, except for 22 township hospitals or health centers. Accordingly, 433 hospitals among 515 were surveyed in 2018 in 15 prefecture–level cities including 118 county–level units, except for 125 township hospitals or health centers.
BPG availability among hospitals at different levels in 2012 and 2018
A significant difference in BPG availability was observed among hospitals at different levels both in 2012 (X2 = 9.747, p = 0.008) and 2018 (X2 = 11.775, p = 0.003). The availability of BPG was significantly higher among provincial hospitals than among county–level hospitals both in 2012 (X2 = 5.613, p = 0.018) and 2018 (X2 = 9.744, p = 0.002). The availability of BPG was significantly higher among provincial hospitals than among municipal hospitals in 2018 (X2 = 4.887, p = 0.028) (Tables 1 and 2).
BPG availability among different types of hospitals in 2012 and 2018
A significant difference in BPG availability was observed among different types of hospitals both in 2012 (X2 = 37.167, p = 0.000) and 2018 (X2 = 28.331, p = 0.000). The availability of BPG among specialized dermatological hospitals was significantly higher than that among general western medicine hospitals (X2 = 12.367, p = 0.000; X2 = 5.159, p = 0.034), maternal and child health hospitals (X2 = 29.824, p = 0.000; X2 = 6.213, p = 0.020), Chinese medicine hospitals (X2 = 19.062, p = 0.000; X2 = 14.053, p = 0.000), and other specialized hospitals (X2 = 18.365, p = 0.000; X2 = 17.348, p = 0.000) both in 2012 and in 2018 (Tables 1 and 2).
In the 2012 survey, the availability of BPG among general western medicine hospitals was significantly higher than that among maternal and child health (X2 = 12.502, p = 0.000), Chinese medicine hospitals (X2 = 4.057, p = 0.044), and other specialized hospitals (X2 = 4.475, p = 0.034). (Table 1) In the 2018 survey, the availability of BPG among general western medicine hospitals was significantly higher than among Chinese medicine hospitals (X2 = 10.504, p = 0.001), and other specialized hospitals (X2 = 12.603, p = 0.000) (Table 2).
BPG availability among hospitals by affiliation in 2012 and 2018
No significant difference of BPG availability was observed between public and private hospitals both in 2012 (X2 = 0.002, p = 0.567) and 2018 (X2 = 0.491, p = 0.306) (Tables 1 and 2).
Changes in BPG availability among hospitals from 2012 to 2018 by level, type, and affiliation
The BPG availability among surveyed hospitals in 2018 was higher than that in 2012 (56.4% vs. 45.0%, X2 = 11.131, p = 0.001). The BPG availability was higher in 2018 than in 2012 among county-level hospitals (52.0% vs. 40.8%, X2 = 7.783, p = 0.005), general western medicine hospitals (62.1% vs. 50.0%, X2 = 6.742, p = 0.009), maternal and child health hospitals (57.1% vs. 26.9%, X2 = 13.906, p = 0.000), and public hospitals (56.8% vs. 45.0%, X2 = 11.361, p = 0.001) (Table 3).
Availability of BPG among county–level units in 2012 and 2018
If BPG was available in at least one hospital in a county-level unit, BPG was considered available in the county-level unit. BPG was available in 65.93% (89/ 135) county-level units in 2012 and 70.34% (83/118) in 2018. No significant difference in BPG availability at county-level was observed between 2012 and 2018 (X2 = 0.563, p = 0.453).
Related factors to BPG availability for syphilis treatment in 2018
In the 2018 survey, we explored the reasons why BPG was unavailable in 189 (43.6%) hospitals. Three major answers were provided by 181 hospitals. The primary reason was the absence of clinical needs (72/181, 38.5%). Second, the clinical use of antibacterial drugs was restricted (37/181, 30.5%). Finally, qualifications lack for providing syphilis treatment (32/181, 27.8%), that is, a qualified department of dermatology & STI and respective doctors are lacking. Among 429 hospitals in the 2012 survey, 197 (45.92%) had a department of dermatology & STI. The availability of BPG among hospitals that have a department of dermatology & STI was significantly higher than those without (66.0% vs. 27.2%, X2 = 64.920, p = 0.000) (Table 1).
Discussion
The Chinese government issued the National Program for Prevention and Control of Syphilis in China (2010–2020) in 2010 [23]. The targets of the program are achievable by 2020 given that BPG can cure most syphilis cases. The availability of BPG for syphilis treatment in Shandong Province has improved in the past 5 years. However, BPG was only available in 56.4% of the hospitals and still had a low availability of 70.3% at the county level in 2018, which was still far from the targets of the Chinese government.
We found a significant difference in BPG availability among different types of hospitals. Specialized dermatological hospitals still play an important role in STI and leprosy prevention and control in China. Maternal and child health hospitals should play a vital role in the prevention and treatment of maternal and congenital syphilis. Although significant change has been observed in the past 5 years, they are still vulnerable in BPG availability.
The low BPG availability among maternal and child health, Chinese medicine, and other specialized hospitals was mostly due to the lack of qualifications for providing syphilis treatment or the lack of a department of dermatology & STI. We found a significant difference in BPG availability between hospitals with and without department of dermatology & STI. For general western medicine hospitals, the major reasons for the lack of BPG are the absence of clinical needs and the restriction of the clinical use of antibacterial drugs.
However, these reasons are untenable. Syphilis has been the third most prevalent disease among the second–class infectious diseases stated by the Infectious Disease Prevention Act of China and is common in general clinical practice [19, 24]. An underlying reason for the absence of clinical needs is that clinical doctors other than dermatologists lack confidence, are reluctant to manage syphilis cases, and would rather refer them to other hospitals if they have not received sufficient training. Second, penicillin has the disadvantage of “high” rate of allergy, which probably prevents doctors to use BPG, considering the great tension in patient-doctor relationships. Although the prevalence of patient–reported penicillin allergy in the general population is as high as 10, 90% of penicillin-allergic patients are able to tolerate penicillin [25]. Although some people are really allergic to penicillin, penicillin therapy may be given to pregnant women with penicillin allergy and serious infections with an acceptable level of safety by using desensitization procedures [9, 26]. Third, many alternative drugs may prevent doctors using BPG. Due to the performance assessment in Chinese hospitals, some doctors prefer second line medicines, such as cephalosporins and macrolides, over BPG, because the low-cost of BPG cannot make profits for hospitals and doctors. A consequence of avoiding the most effective first–line medicines is inducing bacterial resistance [11].
The first version of the National Essential Drugs List was issued by China’s Ministry of Health in 2009 [27]. Until 2012, BPG was excluded from the updated version [28]. Essential drugs should be prepared by all healthcare facilities and are used and sold almost exclusively. However, BPG was still unavailable in many hospitals in Shandong Province. In our 2018 survey, 30.5% of the hospitals lacking BPG refused to purchase it due to the restriction of the clinical use of antibacterial drugs. BPG used to be listed in the restricted antibacterial drugs for clinical use in China. However, the China Ministry of Health excluded it from the list in 2015 in view of its availability [29].
The barriers of BPG unavailability in China were different from those in other countries that suffer from BPG shortage due to market supply [17]. Globally, three companies that still produce the active pharmaceutical ingredient for BPG are located in China. The market supply of BPG is adequate in China. Many hospitals responded to our survey that they can restock BPG at any moment when needed. The implication of our study to other developing countries with shortage of penicillin is that many factor may related to BPG availability beside market supply.
To understand and resolve the dilemma of BPG availability for syphilis treatment in China, the healthcare system reform dated from 1990s should be introspected. Chinese public hospitals are the most important health facilities. Private parties are encouraged to provide medical service and cooperate with public sectors [30]. Hospital reforms aim to maintain the social welfare nature of public hospitals and encourage them to perform public service functions [31]. However, the market-oriented reform distorted the social welfare nature of public hospitals, keeping basic wages low for doctors and encouraging them to make money from prescriptions, which leads to perverse incentives and inequity in healthcare services [32]. The problem may be resolved with the expansion of health system reforms. In 2017, public hospital reforms expanded their focus on eliminating the drug price difference between hospital pharmacies and wholesales [33]. Furthermore, more policy oriented, legal and technical supports should be given to hospitals and clinical doctors to encourage them to restock and use BPG. The 13th Five-Year Plan for Deepening the Medical and Health System Reform states that private parties are encouraged to provide medical service and cooperate with public sectors [31]. In the future, private sectors may contribute more to the availability and accessibility of health services in China.
Limitations of the study
First, the study was conducted in Shandong Province, one of the most economically developed provinces and the second most populous province in China. Although it covers 1/14th of the total population in China, the results of this study may be representative of the coastal economically developed areas in China. Second, this study focused on the availability rather than the accessibility and affordability of BPG. The latter are also important factors for the equity of health care delivery, and need further investigation.
Conclusions
BPG availability for syphilis treatment in Shandong Province remains low and presents disparities among different levels and types of hospitals, although it has been improved in recent years. The low availability of BPG for syphilis treatment in China is related to its clinical use by doctors rather than the market supply. Health care reforms should further improve the availability and accessibility of health services.
Abbreviations
- BPG:
-
benzathine penicillin G
- STI:
-
sexually transmitted infection
- TP:
-
Treponema pallidum
References
Newman L, Rowley J, Vander Hoorn S, Wijesooriya NS, Unemo M, Low N, et al. Global estimates of the prevalence and incidence of four curable sexually transmitted infections in 2012 based on systematic review and global reporting. PLoS One. 2015. https://doi.org/10.1371/journal.pone.0143304.
Clement ME, Okeke NL, Hicks CB. Treatment of syphilis: a systematic review. JAMA. 2014;312:1905–17.
Wijesooriya NS, Rochat RW, Kamb ML, Turlapati P, Temmerman M, Broutet N, et al. Global burden of maternal and congenital syphilis in 2008 and 2012: a health systems modelling study. Lancet Glob Health. 2016;4:525–33.
Hook EW III. Syphilis and HIV infection. J Infect Dis. 1989;160:530–4.
Rd HEW. Syphilis. Lancet. 2017;389:1550–7. https://doi.org/10.1016/S0140-6736(16)32411-4.
Dayan L, Ooi C. Syphilis treatment: old and new. Expert Opin Pharmacother. 2005;6:2271–80.
Xiao H, Liu D, Li Z, Zheng R, Li Z, Hou J, et al. Comparison of doxycycline and Benzathine penicillin G for the treatment of early syphilis. Acta Dermatovenerol Croat. 2017;25:107–11.
Pichichero ME, Casey JR. Safe use of selected cephalosporins in penicillin-allergic patients. Otolaryngol Head Neck Surg. 2007;136:340–7.
Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines. 2015 MMWR Recomm Rep. 2015;64:34–50.
Heikkinen T, Laine K, Neuvonen PJ, Ekblad U. The transplacental transfer of the macrolide antibiotics erythromycin, roxithromycin, and azithromycin. BJOG. 2000;107:770–5.
A2058G Prevalence Workgroup. Prevalence of the 23S rRNA A2058G point mutation and molecular subtypes in Treponema pallidum in the United States, 2007to2009. Sex Transm Dis 2012;39:794–8.
Wendel GD, Sheffield JS, Hollier LM, Hill JB, Ramsey PS, Sanchez PJ. Treatment of syphilis in pregnancy and prevention of congenital syphilis. Clin Infect Dis. 2002;35(Suppl 2):200–9.
Lang R, Shalit I, Segal J, Arbel Y, Markov S, Hass H, et al. Maternal and fetal serum and tissue levels of ceftriaxone following preoperative prophylaxis in emergency cesarean section. Chemotherapy. 1993;39:77–81.
Douglas JM Jr. Penicillin treatment of syphilis: clearing away the shadow on the land. JAMA. 2009;301:769–71.
World Health Organization. Technical consultation on preventing and managing global stock outs of medicines. http://apps.who.int/medicinedocs/documents/s22365en/s22365en.pdf (2015). Accessed 30 Dec 2015.
Taylor MM, Nurse-Findlay S, Zhang X, Hedman L, Kamb ML, Broutet N, et al. Estimating benzathine penicillin need for the treatment of pregnant women diagnosed with syphilis during antenatal care in high-morbidity countries. PLoS One. 2016. https://doi.org/10.1371/journal.pone.0159483.
Nurse-Findlay S, Taylor MM, Savage M, Mello MB, Saliyou S, Lavayen M, et al. Shortages of benzathine penicillin for prevention of mother-to-child transmission of syphilis: an evaluation from multi-country surveys and stakeholder interviews. PLoS Med 2017; https://doi.org/10.1371/journal.pmed 1002473.
69th World Health Assembly closes. News release. Geneva: World Health Organization; 2016. http://www.who.int/mediacentre/news/releases/2016/wha69-28-may-2016/en/. Accessed 28 May 2016.
Chinese Center for Disease Control and Prevention. Epidemic of infectious diseases in China, 2017. http://www.sohu.com/a/224556770_776214 (2018). Accessed 26 Feb 2018.
Jiang N, Gong X, Yue X. Estimation of syphilis epidemic through application of workbook method among populations aged from 15 to 49 years old in China in 2011. Zhonghua Yu Fang Yi Xue Za Zhi. 2014;48:693–8.
Dou L, Wang X, Wang F, Wang Q, Qiao Y, Su M, et al. Epidemic profile of maternal syphilis in China in 2013. Biomed Res Int. 2016. https://doi.org/10.1155/2016/9194805.
Health and Family Planning Commission of Shandong Province. 2017 shandong province health and family planning development statistics bulletin. http://www.sdwsjs.gov.cn/jksd/tjsj_763/zytjbg/201805/t20180515_1312944.html(2018). Accessed 15 May 2018.
China Ministry of Health. Notice of the Ministry of Health on issuing National Program for Prevention and Control of Syphilis in China (2010–2020); http://www.chinacdc.cn/n272442/n272530/n272577/n4020087/38003.html (2010). Accessed 3 June 2010.
National People’s Congress. The Infectious Disease Prevention Act (The 17th Presidential Decree of the People’s Republic of China). https://wenku.baidu.com/view/6289c5492b160b4e767fcfde.html (2004). Accessed 24 Dec 2004.
Gonzalez-Estrada A, Radojicic C. Penicillin allergy: a practical guide for clinicians. Cleve Clin J Med. 2015; dio. https://doi.org/10.3949/ccjm.82a.14111.
Pham MN, Ho HE, Desai M. Penicillin desensitization: treatment of syphilis in pregnancy in penicillin-allergic patients. Ann Allergy Asthma Immunol. 2017;118:537–41.
China's Ministry of Health. Notice on provision of the administration of National Essential Drugs List. http://wsj.yueyang.gov.cn/wsj/11129/11139/content_478952.html (2009). Accessed 18 Aug 2009.
China’s Ministry of Health. National Essential Drugs List (2012 version). http://www.sdadr.gov.cn/WS01/CL0009/1622.html (2013). Accessed 21 Aug 2013.
China Ministry of Health. Notice on further strengthening the management of clinical application of antibacterials; http://wsjsw.qingdao.gov.cn/n28356065/n32563120/n32563122/150914000000666440.html (2015). Accessed 24 Jul 2015.
State Council. The 13th Five-Year Plan for Deepening the Medical and Health System Reform; http://www.gov.cn/zhengce/content/2017-01/09/content_5158053.htm(2016). Accessed 27 Dec 2016.
Barber SL, Borowitz M, Bekedam H, Ma J. The hospital of the future in China: China's reform of public hospitals and trends from industrialized countries. Health Policy Plan. 2014;29:367–78.
Liu YL, Hsiao WC, Eggleston K. Equity in health and health care: the Chinese experience. Soc Sci Med. 1999;(10):1349–56.
State Council. Notice on Universal Expansion of Comprehensive Reforms on Public Hospitals; http://www.gsws.gov.cn/single/11205/75854.html (2017). Accessed 19 April 2017.
Acknowledgments
We thank colleagues from the Center for Diseases Control and Prevention at prefecture and county-level who collected primary data from hospitals in the province.
Funding
This work was supported by the Shandong Provincial Key R&D Plan (2018GSF118062). The funding body was not involved in the collection, analysis and interpretation of data, nor in the writing of manuscripts.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Contributions
DL who is corresponding author obtained funding and designed the study. XC is first authors. DL and XC collected and analyzed the data, drafted the manuscript. GL, YG and TC contributed to the interpretation of the results and critical revision of the manuscript for important intellectual content and approved the final version of the manuscript. All authors have read and approved the final manuscript. DL is the study guarantors.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The objects of this study were hospitals rather than human being or animals. We think that it is not applicable to provide a statement on ethics approval and consent to participate.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
Additional file 1:
Questionnaire on availability of benzathine penicillin G in medical institutions. (DOCX 13 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Chen, X., Li, G., Gan, Y. et al. Availability of benzathine penicillin G for syphilis treatment in Shandong Province, Eastern China. BMC Health Serv Res 19, 188 (2019). https://doi.org/10.1186/s12913-019-4006-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-019-4006-4