Abstract
Background
Rehabilitation services depend on competent professionals who collaborate effectively. Well-functioning interprofessional teams are expected to positively impact continuity of care. Key factors in continuity of care are communication and collaboration among health care professionals in a team and their patients. This study assessed the associations between team functioning and patient-reported benefits and continuity of care in somatic rehabilitation centres.
Methods
This prospective cohort study uses survey data from 984 patients and from health care professionals in 15 teams in seven somatic rehabilitation centres in Western Norway. Linear mixed effect models were used to investigate associations between the interprofessional team communication and relationship scores (measured by the Relational Coordination [RC] Survey and patient-reported benefit and personal-, team- and cross-boundary continuity of care. Patient-reported continuity of care was measured using the Norwegian version of the Nijmegen Continuity Questionnaire.
Results
The mean communication score for healthcare teams was 3.9 (standard deviation [SD] = 0.63, 95% confidence interval [CI] = 3.78, 4.00), and the mean relationship score was 4.1 (SD = 0.56, 95% CI = 3.97, 4.18). Communication scores in rehabilitation teams varied from 3.4–4.3 and relationship scores from 3.6–4.5. Patients treated by teams with higher relationship scores experienced better continuity between health care professionals in the team at the rehabilitation centre (b = 0.36, 95% CI = 0.05, 0.68; p = 0.024). There was a positive association between RC communication in the team the patient was treated by and patient-reported activities of daily living benefit score; all other associations between RC scores and rehabilitation benefit scores were not significant.
Conclusion
Team function is associated with better patient-reported continuity of care and higher ADL-benefit scores among patients after rehabilitation. These findings indicate that interprofessional teams’ RC scores may predict rehabilitation outcomes, but further studies are needed before RC scores can be used as a quality indicator in somatic rehabilitation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Interprofessional teamwork is recognised as a cornerstone for both the philosophy and practice of somatic rehabilitation [1]. It emphasises how teams comprising different health care professionals use a shared strategy to work together towards common aims [2]. The need for interprofessional teamwork stems from the complex nature of patients’ health problems and care needs, with teamwork success dependent on collaboration of health care professionals in teams [3,4,5,6]. Well-functioning interprofessional teams are expected to have an impact on continuity of care [4]. However, more research is needed to clarify the association between team functioning and outcomes at patient- and system-levels.
Assessing interprofessional team function is a new and challenging task. Relational Coordination (RC) theory is a framework for assessing teamwork that focuses on communication and relationships among health care professionals in a team [7]. Communication in teams depend on the teams’ underlying relationships [8, 9]. RC is defined as a ‘mutually reinforcing process of interaction between communication and relationships carried out for the purpose of task integration [10]. The RC theory argues that for a team to be effectively coordinated, there is a need for shared knowledge and understanding in teams, as well as relationships built on shared goals and mutual respect [9].
Improved continuity of care has been shown to improve health outcomes, efficiency of care and patient satisfaction [11,12,13,14]. Most existing research has focused on aspects of personal continuity of care from the care providers’ perspective; for example, the importance of having a care provider that sees the patient over a time period [15,16,17]. Information exchange between care providers and care management is also important to ensure continuity [11]. However, continuity of care is a complicated concept, as multiple health care providers in teams care for patients with their own expectations and needs [18, 19]. Therefore, it is important to consider the perspective of the patient when investigating aspects of continuity of care in rehabilitation service delivery. Ideally, improved RC in teams should lead to better continuity of care and increased rehabilitation benefits for the patients involved. Currently, there is a gap in knowledge regarding how collaboration among care providers in a team affects continuity of care [19,20,21,22]. To gather patient perspectives on continuity of care from a population representing a broad range of diagnostic groups, it is recommended that the generic Nijmegen Continuity Questionnaire (NCQ) is used [23, 24]. The NCQ captures personal continuity as well as continuity within teams and across services [22], and has recently been translated to Norwegian health care settings (NCQ-N) [25].
To our knowledge, no previous studies have investigated the associations between RC in interprofessional teams and patient-reported benefit and experienced continuity of care. Therefore, we assessed associations between communication and relationships in a range of interprofessional teams and patient-reported benefit and continuity of care in somatic rehabilitation centres in Western Norway.
Aims
The aims of this study were threefold: to measure RC scores in interprofessional teams in seven rehabilitation centres in Western Norway; assess patient-reported benefit and continuity of rehabilitation care, and investigate associations between RC scores and patient-reported benefit and continuity of care.
Methods
Study design
This prospective cohort study used data from two surveys of patients in all seven somatic rehabilitation centres in Western Norway. Baseline data were collected from January 2015 to June 2015, with follow-up data collection 1 year later. All patients had a 3–4 week stay at one of the rehabilitation centres in the period between these patient surveys. Patient treatment at the rehabilitation centres is organised in teams and all patients were linked to their treating team. Health care professionals in the rehabilitation centres were surveyed from January 2016 to March 2016.
Interprofessional rehabilitation team survey
In cooperation with the leaders of the rehabilitation centres, all health professionals (N = 167) engaged in working with patients in the centres were invited to participate in the survey. These centres deliver services via interprofessional teams; we identified 16 teams, which were the unit of interest in the present study, according to RC theory [9]. Some healthcare professionals were members of more than one team in the centre in which they worked; these professionals were asked to respond to the survey for each team they worked with. Most healthcare professionals were affiliated with only one team (n = 121), 25 had roles in two teams, 13 in three teams and eight worked in four teams. This gave a possible 121 team member responses from healthcare professionals affiliated with more than one team. Therefore, a total of 242 team member responses were invited. Team members were recruited via an e-mail that included information about the project and a link to the RC Survey in Corporater Surveyor version 3.3 (Corporater Inc.). Responses were received from 124 team members (52%), representing 94 different healthcare professionals in 15 interprofessional rehabilitation teams (56% of all employees). Of the responses; 30 were from 19 team members affiliated with two teams, five from members of three teams and six with roles in four teams. One team was missing as no team members responded to the survey and only three patients responded to the questionnaire. The submission of a completed survey was considered provision of consent to participate.
RC survey
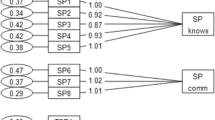
The RC Survey is based on RC theory and is used in both hospital and primary health care settings [14, 26,27,28,29]. The survey has been translated into Norwegian language and validated for Norwegian health care settings in a previous study [30]. The survey comprises seven items evaluating interprofessional team function divided into two sub-scales: four communication items (frequency, accuracy, timeliness and problem solving) and three relationship items (shared goals, shared knowledge and mutual respect) [9]. Each item represents a question (e.g. ‘Do health care professionals in this group communicate frequently with you about rehabilitation patients?’), with responses on a five point Likert scale (1 = never, 2 = rarely, 3 = occasionally, 4 = often, and 5 = always). A higher score indicates better communication or relationships in the interprofessional team. RC survey communication and relationship subscale scores are derived by calculating the mean scores for each subscale [31]. RC focuses on communication and relationships between roles in the team, rather than between unique individuals [9].
Patient surveys
Participants
Patients aged over 18 years who were accepted for admission to a rehabilitation centre in Western Norway between January and July 2015 were invited to participate in this study (N = 2863). In total, 984 patients (34% response rate) accepted the invitation and returned a completed and written consent to participate [32, 33]. The recruitment of patients for the baseline study is fully described in Moen et al. [33]. A 1-year follow-up survey was sent to the 984 participating patients and 705 (25% of those invited at baseline) responded. We excluded 46 patients because of missing The World Health Organisation Disability Assessment Schedule (WHODAS 2.0) data, and four cases that education level was not registered. Finally, 655 patients were included in the analyses (Table 1). Eighteen of the 279 patients who did not respond had died.
Data sources
The WHODAS 2.0 global score as reported in the baseline survey was used as an adjustment variable. This is a 36-item generic patient-reported instrument that measures health and disability [34]. The scale gives subscores for patient self-perceived disability in six functional domains: cognition, mobility, self-care, getting along, life activities, and participation [33, 34]. The WHODAS 2.0 global score ranges from 0 to 100 where 5–24 reflects mild functional loss, 25–49 moderate functional loss, 50–95 severe functional loss and 96–100 total functional loss.
Information about whether the patient was referred by a general practitioner (GP) or a hospital physician was collected from the referral letter at baseline, along with referral diagnoses based on the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10). Additionally, Statistics Norway provided data concerning patient education level. We also included questions from the follow-up survey regarding rehabilitation benefits extracted from the PasOpp Survey [35], developed for the Norwegian Institute of Public Health. Patients were asked to assess how their stay in a rehabilitation centre benefitted their overall health, physical health, mental health, management of activities of daily living (ADL) and participation in social activities.
In addition, we used the NCQ-N which covers three aspects of continuity: personal, team and cross-boundary continuity [19, 25, 36]. These domains are closely related to informational, management and relational continuity of care [11, 37]. The original NCQ has been used for patients receiving care from multiple providers in both hospital and primary health care settings [12, 15, 38, 39], but this study is the first to use the NCQ-N [25]. The NCQ-N comprises of 28 items that are positively formulated statements concerning different aspects of continuity of care (e.g. personal continuity: care provider knows me well, ‘This care provider knows my medical history very well’), scored using a five-point Likert (1 = strongly disagree, 2 = disagree, 3 = neutral, 4 = agree, 5 = strongly agree). A ‘don’t know’ option was also provided, and set as ‘missing’. Subscales for personal continuity (‘the most important health care professional in the rehabilitation centre knows me’) comprising five items and ‘the most important health care professional in the rehabilitation centre shows commitment’ (three items) were derived using the mean scores of the included items. Furthermore, subscales covering team continuity (four items) within the rehabilitation team and cross-boundary continuity (four items) between the rehabilitation centre and the patients’ regular GP were also used. NCQ-N subscales with fewer than two missing items were included in the analyses.
Outcome variables
Five items from the PasOpp Survey were used as outcome variables: overall rehabilitation benefits, physical health benefits, mental health benefits, ADL benefits and social participation benefits. Responses were on a five point Likert scale (1 = not at all, 2 = to a lesser extent, 3 = to some extent, 4 = to large extent, 5 = to great extent), with an additional “not applicable” option (set as ‘missing’).
Four NCQ-N subscales were used as outcome variables with a continuous scale, ranging from 1 to 5 (5 = best):
-
Personal continuity: the most important health care professional in the rehabilitation centre knows me
-
Personal continuity: the most important health care professional in the rehabilitation centre shows commitment
-
Team continuity: collaboration among health care professionals in teams within somatic rehabilitation centres
-
Cross-boundary continuity: collaboration among health care professionals in teams within somatic rehabilitation centres and GPs in the municipality.
Explanatory variables
The main explanatory variables in this study were the RC communication and relationships scores, which were calculated for each team and used as continuous variables, from 1(lowest) to 5 (highest).
Statistical analysis
Descriptive methods were used to analyse sample characteristics. Given the possible intra- cluster correlation between responses from patients treated by the same team, linear mixed effect models were used to investigate associations between patient-reported rehabilitation benefit items (overall rehabilitation benefit, physical benefit, mental health benefit, ADL benefit and social participation benefit) and NCQ-N personal, team and cross-boundary continuity of care items (as outcome variables). The teams’ RC communication and relationship scores were used as explanatory variables. Team allocation was set as the random effect in all models.
For each of the nine outcome variables listed above, four models were estimated using the RC communication subscale as main explanatory variable. First, an unadjusted model (Model 0) containing only the explanatory variable, RC communication subscale and the outcome variables, rehabilitation benefit item scores and NCQ-N subscale scores. Model 1 was adjusted for referral diagnosis (ICD-10) code grouped as: neoplasms, diseases in the nervous system, diseases in the musculoskeletal system, diseases in the circulatory system and others. Model 2 was adjusted for WHODAS 2.0 global score and referral diagnosis. Model 3 was adjusted for WHODAS 2.0 global score, referral diagnosis, sex, age group at the 1 year follow-up (categorised as: < 20, 21–30, 31–40, 41–50, 51–60, 61–70, and > 71), origin of referral (referred by hospital physician or GP) and level of education (categorised as: elementary school, high school, university/college). Similar analyses were repeated with RC relationship scores as the main explanatory variable.
Because of the use of an electronic version of the RC Survey for healthcare professionals, the data retrieved contained no missing values. The level of statistical significance was set as 0.05. All statistical analyses were performed with IBM SPSS for Windows version 23 (IBM Corp., Armonk, NY) [40] and STATA 14 (StataCorp., College Station, TX) [41].
Results
RC scores for rehabilitation teams
The mean communication score among healthcare team respondents was 3.9 (standard deviation [SD] = 0.63, 95% confidence interval [CI] = 3.78, 4.00) and the mean relationship score was 4.1 (SD = 0.56, 95% CI = 3.97, 4.18). The communication scores for the rehabilitation teams ranged from 3.4–4.3, and the relationship scores ranged from 3.6–4.5. Table 2 shows an overview of the 15 teams. The rehabilitation centres varied in size, with 5–17 members in each team.
Patient-reported benefit and continuity of care
The mean overall benefit, physical health and ADL scores were 3.8 (SD = 0.97, 95% CI = 3.73, 3.88), 3.5 (SD = 1.00, 95% CI = 3.45, 3.60) and 3.2 (SD = 1.05, 95% CI = 3.15, 3.32), respectively (Table 3). Team continuity, representing collaboration among rehabilitation team members, had a mean score of 3.7 (SD = 0.82, 95% CI = 3.61, 3.76). Personal continuity mean scores, for the ‘knows me’ and ‘shows commitment’ subscales were 3.0 (SD = 0.86, 95% CI = 2.96, 3.11) and 2.9 (SD = 0.96, 95% CI = 2.76, 2.94), respectively. The cross-boundary continuity mean score for collaboration between the rehabilitation centre and patients’ GPs, was 2.9 (SD = 0.97, 95% CI = 2.81, 3.02).
Associations between team RC scores and patient-reported benefit and continuity of care
The results presented in Table 4 are derived from the univariate model because adjustments in the models did not lead to improvement of Model 0. Results from the fully adjusted models are shown in the table in the Additional file 1.
There was a significant association between RC communication in the team the patient was treated by and ADL benefit (b = 0.29, 95% CI = 0.01, 0.58; p = 0.044). All other associations between RC scores and patient-reported rehabilitation benefit scores were non-significant, but these showed positive coefficients and most had CIs crossing zero with small margins. Associations of team communication and relationships with patient benefit variables were also tested across sex, age groups, referral diagnosis, and education level (not tabulated); however, no significant group differences were found. There was a positive association between team relationship scores and patient-reported team continuity (b = 0.36, 95% CI 0.05, 0.68; p = 0.024), but no significant associations were found regarding communication. Inverse associations were found between communication and relationship scores in teams and both patient-reported personal continuity scales (‘knows me’ and ‘shows commitment’) (Table 4). In addition, there was an inverse association between relationship in teams and cross-boundary continuity (b = − 0.42, 95% CI − 0.80, − 0.04; p = 0.030), whereas no associations were found between communication in teams and cross-boundary continuity of care.
Discussion
This is the first study to investigate prospective associations between communication and relationships in interprofessional teams (measured with the RC Survey), and patient-reported benefit of the rehabilitation stay and experience of continuity of rehabilitation care. Patients treated by teams with higher relationship scores experienced better continuity in the healthcare services they received. However, this study also found that patients reported lower personal continuity of care when treated by teams with higher communication and relationship scores. High relationship scores were associated with lower cross-boundary continuity of care between the rehabilitation centre and the patients’ GPs, as perceived by the patient.
Communication and relationship skills among healthcare professionals are essential for the quality of healthcare delivery [4,5,6]. Further, strong relationships in teams are expected to contribute to effective service delivery and improved patient health outcomes [42]. Gittell indicated that team functions are strong when the reported RC scores are ≥4 on a five-point scale, which was found for nine of the 15 teams included in this study [10]. An earlier study investigating RC in 23 teams from six somatic hospitals and six psychiatric units in Western Norway found that 14 of 23 teams had a RC score below 3.4, which was the lowest score for rehabilitation teams in the present study [30]. Further, in this previous study, half of the teams showed relationship scores below 3.8, compared with only one rehabilitation team in the present study [30]. The RC scores in this study were also high compared with previous international studies, indicating strong team functions for interprofessional teams in rehabilitation centre in Western Norway [8, 26, 29, 43, 44]. A reason why communication and relationship skills were higher in the present study than in previous studies may be that working in teams is crucial for well-functioning rehabilitation services, and the present study suggests this was implemented as the working environment in these rehabilitation centres.
The patient-reported rehabilitation benefit was moderate in our study, with the highest scores for overall benefit and physical health. Only a significant association between benefit and team functions (as measured by RC score) was found. This contrasted with previous studies that showed positive associations between RC scores and outcomes [8, 14, 26, 27]. However, we observed consistent (but non-significant) associations between patient-reported rehabilitation benefit scores and RC scores. The relatively small variance of RC scores between teams in this study may explain why these associations did not reach statistical significance. Another reason for the lack of significant association between RC scores and benefit outcomes may be that the RC scores did not capture the medical content of the rehabilitation programmes, which may vary independent of team function. Future studies should supplement the RC score with measures of programme content.
An important finding of this study was the association between team relationship skills and patient-reported team continuity. Good relationships among health care professionals develop shared knowledge and skills in teams, and impact continuity of care [3]. Research has also found that strong relationships among team members impacted building rapport with patients treated by the team, and increased patient satisfaction [8, 38, 44]. Our study confirmed that patient experienced increased satisfaction with care when there was shared knowledge, shared goals and mutual respect among team members.
The associations between RC scores and team continuity in this study suggest that patients experienced better relational treatment from the whole team rather than from a single healthcare professional. Several studies have found that personal continuity impacted on patients’ experienced benefit of care [18, 45,46,47,48,49]. However, previous studies also found positive associations between team continuity and improved patient outcomes [16], which is consistent with the finding of this study. Therefore, an inverse association between RC and personal continuity could be considered as a natural consequence of a well-functioning team. However, evaluation of the potential negative effect of reduced personal continuity is a topic for further research.
Seamless transitions between service levels increase patient satisfaction [46,47,48,49,50]. Our finding that better team functioning was associated with lower patient scores for continuity between the rehabilitation centres and primary care was unexpected. The expectation was that strong team functions in rehabilitation services would increase the emphasis on seamless transitions between the centres and the primary care. An explanation for our finding could be that patient respondents tended to over-report negative experiences with cross-boundary continuity, as these were easier to remember (recall bias). Therefore, cross-boundary continuity resulting in seamless transitions might have been overlooked. Another explanation could be that patients who experienced well-functioning teams had higher expectations for cross-boundary continuity, therefore, the inverse association between team RC and patient rating of cross-boundary continuity might be attributable to patients’ disappointment. However, this finding should be interpreted with caution, as the response rate for this subscale was lower than for the other continuity of care subscales (Table 3). Further, more studies are needed to investigate this research question.
Study strengths and limitations
Strengths of this study included the prospective longitudinal design and the large and comprehensive study population including patients in rehabilitation centres in Western Norway. A main limitation was the low response rate among patients (34%), which might have resulted in selection bias. Although a high response rate was accomplished from baseline to follow-up (73%), only 25% of the total number of patients invited at baseline responded at follow-up, increasing the problem of representability. Unfortunately, there was no information available regarding non-respondents.
The investigation of associations across multiple health care problems and the use of generic survey instruments were further strengths of this study. However, large numbers of ‘don’t know’ for some NCQ-N items meant that these cases were not included in the analysis and might have caused less certain results. Team members responding for more than one team might also have increased the risk for recall bias. In addition, the response rate for the healthcare professionals was relatively low, which might have introduced selection bias. Healthcare professionals with more than one team might also have experienced difficulties in accurately differentiating communication and relationship patterns for their different rehabilitation teams; if so, this would reduce the differences between teams found in RC scores. However, the response rate for team members affiliated with more than one team was relatively low (24%). In general, the RC survey scores did not vary greatly between the teams, reducing the possibility of detecting weaker associations with the outcomes. Further studies are needed to verify these findings.
Conclusion
Communication and relationships in rehabilitation teams as measured by RC were higher than in comparable studies. This suggests team functioning is a high priority for somatic rehabilitation centres in Western Norway. This study found a positive association between RC relationship in the team the patients were treated by and team continuity reported by patients. However, we did not show that stronger RC team functions in rehabilitation centres predicted better patient outcomes, with the exception of a significant positive association with improved ADL. The negative associations found between team function within rehabilitation centres and cooperation with primary care should be further studied, as further rehabilitation benefits depend on follow-up in primary care.
Abbreviations
- ADL:
-
Activity of daily living
- CI:
-
Confidence interval.
- GP:
-
General practitioner
- NCQ:
-
Nijmegen Continuity Questionnaire
- NCQ-N:
-
Norwegian version of the Nijmegen Continuity Questionnaire
- RC:
-
Relational coordination
- SD:
-
Standard deviation
- WHODAS 2.0:
-
World Health Organization Disability Assessment Schedule 2.0
References
Strasser DC, Falconer JA, Martino-Saltzmann D. The rehabilitation team: staff perceptions of the hospital environment, the interdisciplinary team environment, and interprofessional relations. Arch Phys Med Rehabil. 1994;75(2):177–82.
Dean SG, Siegert RJ, Taylor WJ. Interprofessional rehabilitation: a person-centred approach. Hoboken: Blackwell Wiley; 2012.
Sinclair LB, Lingard LA, Mohabeer RN. What’s so great about rehabilitation teams? An ethnographic study of interprofessional collaboration in a rehabilitation unit. Arch Phys Med Rehabil. 2009;90(7):1196–201.
Momsen AM, Rasmussen JO, Nielsen CV, Iversen MD, Lund H. Multidisciplinary team care in rehabilitation: an overview of reviews. J Rehabil Med. 2012;44(11):901–12.
Reeves S, Pelone F, Harrison R, Goldman J, Zwarenstein M. Interprofessional collaboration to improve professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2017;6.
Martin JS, Ummenhofer W, Manser T, Spirig R. Interprofessional collaboration among nurses and physicians: making a difference in patient outcome. Swiss Med Wkly. 2010;140.
Gittell JH. New directions for relational coordination theory. In: Cameroon KS, Spreitzer GM, editors. The Oxford handbook of positive organizational. scholarship ed. New York: Oxford University Press; 2012. p. 400–11.
Gittell JH, Fairfield KM, Bierbaum B, Head W, Jackson R, Kelly M, et al. Impact of relational coordination on quality of care, postoperative pain and functioning, and length of stay: a nine-hospital study of surgical patients. Med Care. 2000;38(8):807–19.
Gittell JH. Relational coordination: guidelines for theory, mearsurement and analysis. Heller School, Brandeis University. USA: Relational coordination research collaboration; 2012.
Gittell JH. Coordinating mechanisms in care provider groups: relational coordination as a mediator and input uncertainty as a moderator of performance effects. Manag Sci. 2002;48(11):1408–26.
Haggerty JL, Reid RJ, Freeman GK, Starfield BH, Adair CE, McKendry R. Continuity of care: a multidisciplinary review. BMJ (Clinical Research ed). 2003;327(7425):1219–21.
Uijen AA, Bischoff EW, Schellevis FG, Bor HH, van den Bosch WJ, Schers HJ. Continuity in different care modes and its relationship to quality of life: a randomised controlled trial in patients with COPD. Br J Gen Pract. 2012;62(599):422–8.
van Walraven C, Oake N, Jennings A, Forster AJ. The association between continuity of care and outcomes: a systematic and critical review. J Eval Clin Pract. 2010;16(5):947–56.
Hartgerink JM, Cramm JM, Bakker TJ, van Eijsden RA, Mackenbach JP, Nieboer AP. The importance of relational coordination for integrated care delivery to older patients in the hospital. J Nurs Manag. 2014;22(2):248–56.
Hetlevik Ø, Gjesdal S. Personal continuity of care in Norwegian general practice: a national cross-sectional study. Scan J Prim Health Care. 2012;30(4):214–21.
Saultz JW, Lochner J. Interpersonal continuity of care and care outcomes: a critical review. Ann Fam Med. 2005;3(2):159–66.
Schers H, van den Hoogen H, Bor H, Grol R, van den Bosch W. Familiarity with a GP and patients’ evaluations of care. A cross-sectional study. Fam Pract. 2005;22(1):15–9.
Uijen AA. Continuity of care perspectives of the patient with chronic illness. Netherland: Radboud University Nijmegen Medical Centre; 2012.
Uijen AA, Schers HJ, van Weel C. Continuity of care preferably measured from the patients’ perspective. J Clin Epidemiol. 2010;63(9):998–9.
Reid RJ, Haggerty J, McKendry R. Canadian Institute for Health Information, Advisory Committee on Health Services (Canada), Canadian Health Services Research. Defusing the confusion: Concepts and measures of continuity of health care. Canada; Canadian Health Services Research Foundation:2002.
Waibel S, Henao D, Aller MB, Vargas I, Vazquez ML. What do we know about patients’ perceptions of continuity of care? A meta-synthesis of qualitative studies. Int J Qual Health Care. 2012;24(1):39–48.
Uijen AA, Schers HJ, Schellevis FG, Mokkink HG, van Weel C, van den Bosch WJ. Measuring continuity of care: psychometric properties of the Nijmegen continuity questionnaire. Br J Gen Pract. 2012;62(600):949–57.
Uijen AA, Heinst CW, Schellevis FG, van den Bosch WJHM, van de Laar FA, Terwee CB, et al. Measurement properties of questionnaires measuring continuity of care: a systematic review. PLoS One. 2012;7(7):e42256.
Uijen AA, Shers HJ. Letters to editor. J Clin Epidemiol. 2012;65:577–9.
Hetlevik O, Hustoft M, Uijen A, Assmus J, Gjesdal S. Patient perspectives on continuity of care: adaption and preliminary psychometric assessment of a Norwegian version of the Nijmegen continuity questionnaire (NCQ-N). BMC Health Serv Res. 2017;17(1):760.
Cramm JM, Hoeijmakers M, Nieboer AP. Relational coordination between community health nurses and other professionals in delivering care to community-dwelling frail people. J Nurs Manag. 2014;22(2):170–6.
Gittell JH, Godfrey M, Thistlethwaite J. Interprofessional collaborative practice and relational coordination: improving healthcare through relationships. J Interprof Care. 2013;27(3):210–3.
Hartgerink JM, Cramm JM, Bakker TJEM, van Eijsden AM, Mackenbach JP, Nieboer AP. The importance of multidisciplinary teamwork and team climate for relational coordination among teams delivering care to older patients. J Adv Nurs. 2013;70(4):791–9.
Havens DS, Vasey J, Gittell JH, Lin WT. Relational coordination among nurses and other providers: impact on the quality of patient care. J Nurs Manag. 2010;18(8):926–37.
Hustoft M, Hetlevik Ø, Asmus J, Størkson S, Gjesdal S, Biringer E. Communication and relational ties in interprofessional teams in Norwegian specialized health care: a multicentre study of relational coordination. Int J Integr care. 2018;18(2):9. https://doi.org/10.5334/ijic.3432.
Gittell JH, Seidner R, Wimbush J. A relational model of high performance work systems work. Organized Science. 2010;21(2):490–506.
Moen VP, Drageset J, Eide GE, Klokkerud M, Gjesdal S. Validation of World Health Organization assessment schedule 2.0 in specialized somatic rehabilitation services in Norway. Qual Life Res. 2017;26(2):505–14.
Moen VP, Drageset J, Eide GE, Gjesdal S. Dimensions and predictors of disability- a baseline study of patients entering somatic rehabilitation in secondary care. PLoS One. 2018;13(3):e0193761.
Federici S, Bracalenti M, Meloni F, Luciano JV. World Health Organization disability assessment schedule 2.0: an international systematic review. Disabil Rehabil. 2017;39(23):2347–80.
Holmboe O. Patient experiences in rehabilitation institutions. Results from a pilot study. In. Norwegian Institute of Public Health. Oslo; 2009. Available at http://www.fhi.no/en . Accessed 5 Jan 2018.
Uijen AA, Schellevis FG, van den Bosch WJ, Mokkink HG, van Weel C, Schers HJ. Nijmegen continuity questionnaire: development and testing of a questionnaire that measures continuity of care. J Clin Epidemiol. 2011;64(12):1391–9.
Freeman GK. Progress with relationship continuity 2012, a British perspective. Int J Integr Care. 2012;12:e128.
Uijen AA, Schers HJ, Schene AH, Schellevis FG, Lucassen P, van den Bosch WJ. Experienced continuity of care in patients at risk for depression in primary care. Eur J Gen Pract. 2014;20(3):161–6.
Uijen AA, Bosch M, van den Bosch WJ, Bor H, Wensing M, Schers HJ. Heart failure patients’ experiences with continuity of care and its relation to medication adherence: a cross-sectional study. BMC Fam Pract. 2012;13:86.
IBM Corp. IBM SPSS statistics for windows, version 24.0: released 2016. Armonk: NY: IBM Corp.
StataCorp. Stata Statistical Software: Release 14. College Station: TX: StataCorp LP; 2015.
Gittell JH. Relationships between service providers and their impact on customers. J Serv Res. 2002;4(4):299–311.
Lee CT. Social capital and relational coordination in outpatient clinics: an interprofessional analysis. J Interprof Care. 2013;27(1):81–7.
Lee CT, Doran DM, Tourangeau AE, Fleshner NE. Perceived quality of interprofessional interactions between physicians and nurses in oncology outpatient clinics. Eur J Oncol Nurs. 2014;18(6):619–25.
Krogstad U, Hofoss D, Hjortdahl P. Continuity of hospital care: beyond the question of personal contact. BMJ (Clinical Research ed). 2002;324(7328):36–8.
Yeager S. Interdisciplinary collaboration: the heart and soul of health care. Crit Care Nurs Clin North Am. 2005;17(2):143–8.
Medina-Mirapeix F, Oliveira-Sousa S, Sobral-Ferreira M, Del Bano-Aledo ME, Escolar-Reina P, Montilla-Herrador J, et al. Continuity of rehabilitation services in post-acute care from the ambulatory outpatients’ perspective: a qualitative study. J Rehabil Med. 2011;43(1):58–64.
Medina-Mirapeix F, Oliveira-Sousa SL, Escolar-Reina P, Sobral-Ferreira M, Lillo-Navarro MC, Collins SM. Continuity of care in hospital rehabilitation services: a qualitative insight from inpatients’ experience. Rev Bras Fisioter. 2017;21(2):85–91.
Cowie L, Morgan M, White P, Gulliford M. Experience of continuity of care of patients with multiple long-term conditions in England. J Health Serv Res Policy. 2009;14(2):82–7.
Mendes FR, Gemito ML, Caldeira ED, Serra ID, Casas-Novas MV. Continuity of care from the perspective of users. Ciencia & Saude Coletiva. 2017;22(2):841–53.
Acknowledgements
We thank all personnel at rehabilitation centres in Western Norway for recruiting patients and for participating in this study. We thank Edanz Group (www.edanzediting.com/ac) for editing a draft of this manuscript.
Funding
No external funding was received for this research project.
Availability of data and materials
The raw data are property of the research unit in the Bergen Health Authority (Helse Bergen) and are available on reasonable request.
Author information
Authors and Affiliations
Contributions
MH, ØH, SG and EB developed the project idea and contributed to writing the paper. MH, ØH and JA performed the statistical analysis and interpreted the results. All authors have approved the final version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures were in accordance with the ethical standards of the regional research committees and the Declaration of Helsinki 1964 and its later amendments. This study was approved by the Regional Committees for Medical and Health Research Ethics in 2015 (2014/1636/REK vest). Written consent was obtained from all participating patients. Return of the electronic RC Survey questionnaire by healthcare professionals was considered provision of consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
Additional file 1:
Linear mixed effect models, fully adjusted. (DOCX 24 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Hustoft, M., Biringer, E., Gjesdal, S. et al. Relational coordination in interprofessional teams and its effect on patient-reported benefit and continuity of care: a prospective cohort study from rehabilitation centres in Western Norway. BMC Health Serv Res 18, 719 (2018). https://doi.org/10.1186/s12913-018-3536-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-018-3536-5