Abstract
Purpose
To investigate the prevalence of insomnia among nurses with long COVID-19, analyze the potential risk factors and establish a nomogram model.
Methods
Nurses in Ningbo, China, were recruited for this study. General demographic information and insomnia, burnout, and stress assessment scores were collected through a face-to face questionnaire survey administered at a single center from March to May 2023. We used LASSO regression to identify potential factors contributing to insomnia. Then, a nomogram was plotted based on the model chosen to visualize the results and evaluated by receiver operating characteristic curves and calibration curves.
Results
A total of 437 nurses were recruited. 54% of the nurses had insomnia according to the Insomnia Severity Index (ISI) score. Eleven variables, including family structure, years of work experience, relaxation time, respiratory system sequelae, nervous system sequelae, others sequelae, attitudes toward COVID-19, sleep duration before infection, previous sleep problems, stress, and job burnout, were independently associated with insomnia. The R-squared value was 0.464, and the area under the curve was 0.866. The derived nomogram showed that neurological sequelae, stress, job burnout, sleep duration before infection, and previous sleep problems contributed the most to insomnia. The calibration curves showed significant agreement between the nomogram models and actual observations.
Conclusion
This study focused on insomnia among nurses with long COVID-19 and identified eleven risk factors related to nurses’ insomnia. A nomogram model was established to illustrate and visualize these factors, which will be instrumental in future research for identifying nurses with insomnia amid pandemic normalization and may increase awareness of the health status of healthcare workers with long COVID-19.
Similar content being viewed by others
Introduction
While coronavirus disease 2019 (COVID-19) is predominantly considered an acute self-remitting disease, individuals may experience long-term symptoms that develop after recovery from acute COVID-19 [1]. The World Health Organization (WHO) defines long COVID-19 as the continuation or development of new symptoms 3 months after the initial SARS-CoV-2 infection, with these symptoms lasting for at least 2 months [2]. Fatigue, shortness of breath, and cognitive dysfunction are among the most commonly reported symptoms according to the WHO [3,4,5]. Recent studies have shown that sleep disturbances, including insomnia, are also prominent features of long COVID-19 [6,7,8]. It has been reported that the rate of incident insomnia symptoms is 60.6% for long COVID-19 patients [7], which is higher than the 18-31% prevalence identified in the general population during the COVID-19 pandemic [9].
Insomnia is a common phenomenon among nurses. Previous studies have shown that insomnia in nurses is associated with age [10], marital status [11], education level [12], sex [13], job strain [13] and work shift [13]. Since the COVID-19 pandemic, there has been a significant increase in insomnia in global communities [14, 15], and nurses are at a high risk of insomnia, especially those who have long COVID-19. Long COVID-19 is an often-debilitating illness with sequalae that can impact multiple systems, such as respiratory sequelae, cardiovascular sequelae, neurological sequelae, and other sequelae (psychological and mental effects) [3, 16,17,18]. Moreover, prolonged emotional and interpersonal stress and burnout have been increasingly recognized as hazards, with a high prevalence among medical workers in many countries during the COVID-19 pandemic [19]. A study compared the sleep quality of 287 medical and nursing staff members before infection and during the long COVID-19 period, and reported that the scores on all sleep and psychological scales during the long COVID-19 period were greater (i.e., worse) than those before infection [20].
Compared to the general population, nurses undertake clinical work characterized by articulated work shifts to ensure continuity of care throughout a 24-hour period. It has been reported that shift work is a risk factor for insomnia in nurses [13]. Nurses experienced considerable changes in their work schedules after the start of the COVID-19 pandemic, including longer hours [21], more shift work [13], and general alterations in staff scheduling to minimize interactions between staff members.
Potential insomnia in nurses has been a public health concern because it may degrade the quality of patient care. Insufficient sleep or poor sleep quality due to insomnia leads to fatigue, creating a potentially hazardous environment for patients and negatively effecting on physical health outcomes in medical workers [22]. Lenzer [23] reported a threefold increase in the number of patient deaths from preventable events when nurses had a short sleep duration. Moreover, numerous observational studies have reported that healthcare workers with a short sleep duration and poor sleep quality cannot function to the best of their ability and can make attention-related errors that not only compromise patient care but also put healthcare workers in danger [24,25,26]. For example, studies have shown an increased incidence of self-inflicted needle-stick injuries when nurses are tired. Improving the sleep quality of nurses has become an important social issue that needs to be addressed.
Although insomnia has been identified as a common symptom of long COVID-19, very few studies have quantified the incidence and relative risk of insomnia in nurses with long COVID-19. In this study, we assessed insomnia among nurses with long COVID-19 and investigated the potential relationships between insomnia and variables related to the nursing profession, clinical work, continuous pandemic normalization, and long COVID-19 in nurses. Then, we applied LASSO regression analysis to preliminarily choose the variables for screening, which can determine the degree of influence of a specific characteristic on the target variables. A nomogram is a visualization of a regression equation that can integrate multiple risk factors into a visual diagram so that users can easily interpret results through reading and operation and is used to visualize significant factors. These findings can guide the recognition of insomnia in nurses and other healthcare personnel amid pandemic normalization for future research.
Methods
Participants
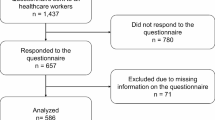
The study was conducted at Ningbo Medical Center LiHuili Hospital in Zhejiang Province, China. A cross-sectional survey was conducted to analyze related variables. The inclusion criteria were as follows: (1) licensed nurses and (2) nurses who had received a COVID-19 diagnosis and whose pathological condition had persisted for at least 2 months [2]. Nurses who were not on duty because of sick leave, maternity leave, or off-site training during the research were excluded from the study. This study was approved by the Ethics Committee of Ningbo Medical Center LiHuili Hospital (2023-C-119). We explained the study to all participants and obtained informed consent.
Procedures
The questionnaires were distributed to clinical nurses via face-to-face contact from March to May 2023. The content includes basic demographic information as well as insomnia, burnout, and stress assessment scores. The data were extracted simultaneously by two reviewers in duplicate and compiled into a preprepared data collection form. Any discrepancies were resolved through consultation with the senior reviewer.
Measures
Demographic information survey
The survey focused on demographic information, including age, gender, family structure, family relationship, education, years of work experience, overtime status, marriage, night shift frequency, technical qualification, relaxation time, department, recovery time, sequelae status, sleep duration before infection, previous sleep problems, exercise, department rotation, and attitudes toward COVID-19.
Insomnia assessment
The Insomnia Severity Index (ISI) includes seven items and is used to assess the nature, severity, and impact of insomnia [27, 28]. Participants reflect on their experiences over the past month by considering aspects such as sleep onset issues, sleep maintenance problems, waking up too early, dissatisfaction with sleep, how sleeping difficulties impact daytime functioning, whether others notice their sleep problems, and the distress caused by these issues. Each item is rated according to a five-point Likert scale, with scores ranging from 0 (no problem) to 4 (very severe). All participants were divided into four subgroups according to their total score, which ranged from 0 to 28. In our study, the designation “sleep 0” indicated the absence of insomnia (0–7), “sleep 1” indicated subthreshold insomnia (8–14), “sleep 2” indicated moderate insomnia (15–21), and “sleep 3” indicated severe insomnia (22–28). Participants with scores ≧ 8 were considered to have insomnia. The reliability of the Chinese version of the scale is 0.65–0.92 [29].
Burnout assessment
The Chinese Maslach Burnout Inventory (CMBI), which assesses the degree of job burnout in workers, was developed by Li et al. [30] based on the Maslach Burnout Inventory (MBI) [31] questionnaire developed by Maslach et al. and is suitable for the Chinese cultural context. It includes three dimensions—emotional exhaustion, personality disintegration, and decreased sense of achievement—with a total of 15 items scored using a seven-point Likert scale. Based on the diagnostic criteria for job burnout and the scores on this scale, job burnout among workers was divided into four levels according to the critical values obtained in the study (emotional exhaustion score ≧ 25 points, personality disintegration score ≧ 11 points, and achievement reduction score ≧ 16 points): none, mild, moderate, and severe. The test’s internal consistency was considered high, with coefficients of 0.667, 0.808, and 0.568, respectively, for the three dimensions [30].
Stress assessment
The stress levels of medical staff were assessed by the Stress Overload Scale (SOS), which was developed by Amirkhan [32]. The scale consists of 22 items organized into two subscales: event load and personal vulnerability. Participants are asked to rate each item on a five-point scale ranging from 1 (never) to 5 (always). The total score is the sum of all responses and ranges from 22 to 110. Higher scores indicated greater stress overload. The Chinese version of the SOS has been validated to be a reliable and valid instrument, with a Cronbach’s coefficient of 0.936, an item content validity index (CVI) of 0.86, and a CVI ranging from 0.80 to 0.86 for each dimension [33].
Data analyses
Statistical analyses were mostly conducted using R Statistical Software version 4.2.1 (http://www.R-project.org). The chi-square test, correlation analysis, and the crosstab function of statistical software version 20.0 (SPSS, Inc., Somers, NY, USA) were used to describe the associations between variables. The LASSO regression technique was adopted to select the most informative features (i.e., family structure, years of work experience, relaxation time, and respiratory system sequelae) from the dataset using the glmnet package (version 4.1-6). Moreover, one-hot encoding was employed to process the data, facilitating an investigation of potential associations between different classes of variables and each class of sleep after LASSO regression. The nomogram was established using the “rms” package (version 6.4-1) to incorporate and visualize significant factors. The receiver operating characteristic (ROC) curve and area under the curve (AUC) were calculated to evaluate the performance of the established nomogram model, and a calibration curve (1000 bootstrap resampling) was used to test the calibration power. A two-tailed p value ≤ 0.05 was considered to indicate statistical significance.
Results
Participant characteristics
The characteristics of the participants are presented in Table 1. A total of 437 nurses were enrolled in this study. Of these nurses, 402 (91.99%) were female, 93.36% had a bachelor’s degree, 46% reported experiencing previous sleep problems and the mean age was 32.2 years [SD 7.15]. Among the nurses surveyed, 46.91% worked in general wards, and 41.88% worked night shifts at least 5 times/month. Regarding family structure, the majority of nurses (49.05%) were from nuclear families. Furthermore, 61.10% of the nurses indicated that they had extremely intimate family relationship. Nurses who participated in the survey exhibited varying levels of stress (mean score 54.536 [SD 16.275]) and job burnout (mean score 57.424 [SD 15.338]).
LASSO regression
LASSO regression analysis involved the selection of 29 categorical variables. The interpretation for 29 categorical variables and the dummy variables were showed in supplemental file- Table 2A. After some coefficients were set to zero (dummy variables in Table 2). The 11 variables, including family structure, years of work experience, relaxation time, respiratory system sequelae, nervous system sequelae, others sequelae, attitudes toward COVID-19, sleep duration before infection, previous sleep problems, stress, and job burnout, were independently associated with insomnia. The results of the LASSO regression after one-hot encoding were as follows: sequela (no nervous system) had the highest weight (w= -0.27), followed by sleep duration before infection 3 (w= -0.221), previous sleep problems 0 (w= -0.182), stress 2 (w = 0.128), job burnout 1 (w= -0.092), and stress 0 (w= -0.076). The R2 value was 0.464. The AUC of the LASSO regression was 0.866.
Factors associated with insomnia in nurses
The factors associated with insomnia in nurses are shown in Fig. 1. According to the correlation analysis, the strongest positive correlations were observed between insomnia and the nervous system sequelae (r = 0.52). Other positive factors for insomnia included stress (r = 0.39), job burnout (r = 0.34), previous sleep problems (r = 0.37), years of work experience (r = 0.10), relaxation time (r = 0.18), respiratory sequelae (r = 0.14), circulatory sequelae (r = 0.16), and others sequelae (r = 0.09). Moreover, negative correlations were detected between sleep outcomes and attitudes toward COVID-19 (r= -0.17) and sleep duration before infection (r= -0.43).
Construction and verification of the nomogram
To further analyze the prognostic value of the risk factors, we established a nomogram model that incorporated all significant factors identified in the LASSO regression (Fig. 2). All the prediction parameters had corresponding accurate values in the nomogram model. The aforementioned values were added together and placed on the total score scale to calculate the risk of insomnia. The ROC curves of the nomogram model showed acceptable values for predicting different degrees of insomnia: sleep 0 (AUC = 0.892), sleep 1 (AUC = 0.772), sleep 2 (AUC = 0.865) , and sleep 3 (AUC = 0.974) (Fig. 3). In addition, calibration curves showed acceptable anticipated and observed probabilities of insomnia (Fig. 4).
An individualized nomogram model to describe the risk of insomnia in nurses
Eleven variables were selected based on the results of the LASSO analysis. The R package “rms” was utilized to construct the prediction model of the post coronavirus insomnia nomogram. The factors with significant differences are indicated by asterisks. Points are assigned for each risk factor by drawing a line upward from the corresponding values to the ‘point’ line. The total points are the sum of the points obtained for the four risk factors and are plotted on the ‘total points’ line. The first row is taken as the observation data; that is, all risk factor points are calculated to have 563 risk scores corresponding to a risk of 3.33
ROC curve of the nomogram model for assessing the quality of sleep in nurses with insomnia
The ROC curve of the models, X-axis: specificity, Y-axis: sensitivity. The AUCs of the models were as follows: sleep score 0 (AUC = 0.892), sleep score 1 (AUC = 0.772), sleep score 2 (AUC = 0.865), and sleep score 3 (AUC = 0.974). This figure was drawn using R software version 4.2.1 http://www.R-project.org
Calibration curve of the nomogram model for predicting insomnia in nurses
The x-axis represents the probability of insomnia (ISI score ≧ 8), and the y-axis represents the actual probability. The 45-degree thick dotted line represents a perfect prediction. The thin dotted line represents the entire cohort (n = 437), and the solid line is bias-corrected by bootstrapping (B = 1000 repetitions), displaying the observed performance of the nomogram
Discussion
The present study is the first to investigate the prevalence of insomnia among nurses with long COVID-19. 54% of the nurses had insomnia, including 1.83% with severe insomnia and 11.44% with moderate insomnia. A meta-analysis that included 401 studies involving 458,754 participants across 58 countries reported that women working in high-risk units and those providing direct care had significantly greater odds of having insomnia during the COVID-19 pandemic [34]. In the present study, 91.99% of the participants were female, and they provided direct care experienced lingering effects of the infection, including respiratory, cardiac, cutaneous, and nervous system sequelae, and had a high risk of insomnia.
Our study also revealed that among the nurses with long COVID-19, 42.56% reported nervous system symptoms, which showed the strongest positive correlation between sleep outcomes and insomnia in this population. Pulmonary dysfunction leading to poor oxygenation of the brain may explain the presence of encephalopathy and sleep disorders in COVID-19 patients [35]. A retrospective study revealed that COVID-19 causes neurological injury and neurogenic diseases, such as fatigue (58%), headache (44%), and attention disorders (27%) [36]. Although several hypotheses have been proposed in the literature, the underlying pathophysiological mechanism of many of these disorders remains unclear. Cough and dyspnea are the most commonly reported pulmonary sequelae of long COVID-19 or persistent COVID-19 after infection [10,11,12], and these symptoms were also observed in the present study. Cough and dyspnea can interrupt continuous sleep states, which has a great impact on sleep quality. Our results highlighted that respiratory complications were an independent risk factor affecting sleep outcomes.
LASSO regression analysis revealed that no stress (w= -0.076) was a protective factor for nurses. In contrast, stress was a risk factor for insomnia. It is widely accepted that higher levels of stress in medical workers directly and significantly reduce their self-efficacy and sleep quality [37]. Previous studies have revealed enormous psychological burdens and psychological barriers among medical staff working in high-stress and high-risk epidemic environments [38]. Stress has the potential to augment the activity of excitatory neural pathways, including the sympathetic nervous system, leading to a persistent state of heightened physiological arousal [39]. This elevated state of arousal may consequently have a detrimental impact on sleep quality, incite inflammatory responses, and potentially disrupt the normal functioning of the nervous system.
The nurses with long COVID-19 in our study had stress(36.38%)and job burnout (98.4%), which is consistent with the high stress and burnout scores of in other studies among medical staff [40]. As the main force in the fight against the pandemic, medical staff, as identified high-risk groups, face significant stress and burnout and may be more prone to physical and mental problems than the general public [41, 42]. Moreover, the majority of the participants were female, and previous studies have highlighted an association between stress and job burnout in women, who are impacted more than men across multiple outcomes, including insomnia [34].
Family structure was another factor included in the nomogram, and an extended family structure can be regarded as a positive factor for sleep outcomes, perhaps due to the additional support that the extended family can provide. When facing health crises, people are likely to turn to their family members for practical and emotional support. Especially in China, the family holds particular significance, and has traditionally occupied a central role in cultural life [43]. During public health crises such as the COVID-19 pandemic, a supportive family environment is particularly crucial because it serves as a psychological buffer against stress and challenges [44]. A study during the pandemic including 150 participants reported that family support among nursing staff did not directly influence rates of sleep disturbances but followed an indirect pathway via stress [45]. Conceivably, in extended families, there are more family members who can provide practical and emotional support or create a supportive family environment for nurses, which may improve their insomnia.
The present study had notable limitations that should be acknowledged. First, the lack of involvement of multiple medical centers could limit the wider applicability of the findings. Including a more diverse sample from various centers would enhance the credibility and relevance of the outcomes. In addition, 91.99% of the participants in this study were female, which is consistent with the proportion of female nurses in China. To enhance the accuracy of the findings, future research should aim to compare the differences between nurses of different genders in the samples studied and focus on incorporating a broader range of healthcare facilities. Second, despite the broad spectrum of parameters analyzed and the acceptable performance of the assessments, we recognize that additional potentially relevant variables, such as pharmacological treatments and depression and anxiety scores, merit future consideration.
Conclusion
Taken together, our study focused on insomnia among nurses with long COVID-19 and we found there are 11 risk factors related. The nomogram model based on LASSO regression was established to illustrate and visualize these factors.
Given the inherent limitations of cross-sectional study, further research are indispensable to verify the causality of this association. Despite several limitations, there is sufficient evidence in this study to show that the nurses suffering from insomnia who underwent the long COVID-19 is high incidence. These findings highlight the need for a targeted measure to improve sleep status of nurses who underwent the long COVID-19.
Data availability
The datasets generated during and analyzed during the current study are not publicly available, but are available from the corresponding author on reasonable request.
References
Raveendran AV, Jayadevan R, Sashidharan S, Long COVID. An overview. Diabetes Metab Syndr. 2021;15(3):869–75.
World Health Organization. Post COVID-19 condition (Long COVID). WHO. 2022. https://www.who.int/europe/news-room/fact-sheets/item/post-COVID-19-condition
Groff D, Sun A, Ssentongo AE, Ba DM, Parsons N, Poudel GR, Parsons N, et al. Short-term and long-term rates of Postacute Sequelae of SARS-CoV-2 infection: a systematic review. JAMA Netw Open. 2021;4(10):e2128568.
Nalbandian A, Sehgal K, Gupta A, Madhavan MV, McGroder C, Stevens JS, Cook JR, et al. Post-acute COVID-19 syndrome. Nat Med. 2021;27(4):601–15.
Del Rio C, Collins LF, Malani P. Long-term Health consequences of COVID-19. JAMA. 2020;324(17):1723–4.
Rouen A, Taïeb J, Caetano G, Pitron V, Elbaz M, Salmon D, Leger D. Polysomnographic parameters in long-COVID chronic insomnia patients. Dialogues Clin Neurosci. 2023;25(1):43–9.
Chen SJ, Morin CM, Ivers H, Wing YK, Partinen M, Merikanto I, Holzinger B, et al. The association of insomnia with long COVID: an international collaborative study (ICOSS-II). Sleep Med. 2023;112:216–22.
Merikanto I, Dauvilliers Y, Chung F, Wing YK, De Gennaro L, Holzinger B, Bjorvatn B, et al. Sleep symptoms are essential features of long-COVID - comparing healthy controls with COVID-19 cases of different severity in the international COVID sleep study (ICOSS-II). J Sleep Res. 2023;32(1):e13754.
Aymerich C, Pedruzo B, Pérez JL, Laborda M, Herrero J, Blanco J, Mancebo G, et al. COVID-19 pandemic effects on health worker’s mental health: systematic review and meta-analysis. Eur Psychiatry. 2022;65(1):e10.
Garg M, Maralakunte M, Garg S, Dhooria S, Sehgal I, Bhalla AS, Vijayvergiya R, et al. The Conundrum of ‘Long-COVID-19’: a narrative review. Int J Gen Med. 2021;14:2491–506.
Carfì A, Bernabei R, Landi F. Persistent symptoms in patients after acute COVID-19. JAMA. 2020;324(6):603–5.
Xiong Q, Xu M, Li J, Liu Y, Zhang J, Xu Y, Dong W. Clinical sequelae of COVID-19 survivors in Wuhan, China: a single-centre longitudinal study. Clin Microbiol Infect. 2021;27(1):89–95.
Caramello V, Gariglio V, Di Salvo G, Maina G, Boccuzzi A. Longitudinal Assessment of Mental Health Consequences of the COVID-19 pandemic long-term exposure on Health Care Workers from a North West Italian Hospital. Disaster Med Public Health Prep. 2023;17:e378.
Morin CM, Bjorvatn B, Chung F, Holzinger B, Partinen M, Penzel T, Ivers H, et al. Insomnia, anxiety, and depression during the COVID-19 pandemic: an international collaborative study. Sleep Med. 2021;87:38–45.
Merikanto I, Kortesoja L, Benedict C, Chung F, Cedernaes J, Espie CA, Morin CM, et al. Evening-types show highest increase of sleep and mental health problems during the COVID-19 pandemic-multinational study on 19 267 adults. Sleep. 2022;45(2):zsab21.
Subramanian A, Nirantharakumar K, Hughes S, Myles P, Williams T, Gokhale KM, Taverner T, et al. Symptoms and risk factors for long COVID in non-hospitalized adults. Nat Med. 2022;28(8):1706–14.
Vargas I, Muench A, Grandner MA, Irwin MR, Perlis ML. Insomnia symptoms predict longer COVID-19 symptom duration. Sleep Med. 2023;101:365–72.
Davis HE, McCorkell L, Vogel JM, Topol EJ. Long COVID: major findings, mechanisms and recommendations. Nat Rev Microbiol. 2023;21(3):133–46.
Jones AM, Clark JS, Mohammad RA. Burnout and secondary traumatic stress in health-system pharmacists during the COVID-19 pandemic. Am J Health Syst Pharm. 2021;78(9):818–24.
Alfonsi V, Scarpelli S, Gorgoni M, Couyoumdjian A, Rosiello F, Sandroni C, Roberto C, et al. Healthcare Workers after two years of COVID-19: the consequences of the pandemic on Psychological Health and Sleep among nurses and Physicians. Int J Environ Res Public Health. 2023;20(2):1410.
Hoedl M, Bauer S, Eglseer D. Influence of nursing staff working hours on stress levels during the COVID-19 pandemic: a cross-sectional online survey. HeilberufeScience. 2021;12(3–4):92–8.
Ghalichi L, Pournik O, Ghaffari M, Vingard E. Sleep quality among health care workers. Arch Iran Med. 2013;16(2):100–3.
Lenzer J. Doctors underwent extreme sleep deprivation in studies of effect on patient deaths. BMJ. 2015;351:h6295.
Parker RS, Parker P. The impact of sleep deprivation in military surgical teams: a systematic review. J R Army Med Corps. 2017;163(3):158–63.
Khajuria A, Khajuria A. Effect of pharmacological enhancement on cognitive and clinical psychomotor performance of sleep-deprived doctors. Int J Surg. 2013;11(10):1143–4.
Sanches I, Teixeira F, dos Santos JM, Ferreira AJ. Effects of Acute Sleep Deprivation resulting from Night Shift Work on Young doctors. Acta Med Port. 2015;28(4):457–62.
Fernandez-Mendoza J, Rodriguez-Muñoz A, Vela-Bueno A, Olavarrieta-Bernardino S, Calhoun SL, Bixler EO, Vgontzas AN. The Spanish version of the Insomnia Severity Index: a confirmatory factor analysis. Sleep Med. 2012;13(2):207–10.
MORIN C. AZRIN N. Social and clinical validation of insomnia treatment outcome; proceedings of the meeting of Association for Advancement of Behavior Therapy, Inc. 72 Spring Street, New York; 1985.
Bai C, JI D, Chen L, Li L, Wang C. Reliability and validity of Insomnia Severity Index in clinical insomnia patients. Chin J Practical Nurs, 2018: 2182–6.
Li YX, Zhang K, Zhao GX. Confirmatory factor analysis of job burnout. Psychol Explor. 2005;25(4):70–3.
Maslach C, Schaufeli WB, Leiter MP. Job burnout. Annu Rev Psychol. 2001;52:397–422.
Amirkhan JH. Stress overload: a new approach to the assessment of stress. Am J Community Psychol. 2012;49:55–71.
Su L, Guo LL. Reliability and validity of the stress overload scale in Chinese nurses. Chin J Nurs. 2014;49:1264–68.
Lee BEC, Ling M, Boyd L, Olsson C, Sheen J. The prevalence of probable mental health disorders among hospital healthcare workers during COVID-19: a systematic review and meta-analysis. J Affect Disord. 2023;330:329–45.
Ahmad SJ, Feigen CM, Vazquez JP, Kobets AJ, Altschul DJ. Neurological sequelae of COVID-19. J Integr Neurosci. 2022;21(3):77.
Carod-Artal FJ, García-Moncó JC. Epidemiology, pathophysiology, and classification of the neurological symptoms of post-COVID-19 syndrome. Neurol Perspect, 2021, 1: S5–15.
Xiao H, Zhang Y, Kong D, Li S, Yang N. The effects of Social Support on Sleep Quality of Medical Staff treating patients with Coronavirus Disease 2019 (COVID-19) in January and February 2020 in China. Med Sci Monit. 2020;26:e923549.
Kisely S, Warren N, McMahon L, Dalais C, Henry I, Siskind D. Occurrence, prevention, and management of the psychological effects of emerging virus outbreaks on healthcare workers: rapid review and meta-analysis. BMJ. 2020;369:m1642.
Yaribeygi H, Panahi Y, Sahraei H, Johnston TP, Sahebkar A. The impact of stress on body function: a review. EXCLI J. 2017;16:1057–72.
Tomaszewska K, Majchrowicz B, Snarska K, Telega D. Stress and Occupational Burnout of nurses Working with COVID-19 patients. Int J Environ Res Public Health. 2022;19(19):12688.
Navinés R, Olive V, Hidalgo-Mazzei D, Langohr K, Vieta E, Martin-Santos R. Burnout in residents during the first wave of the COVID-19 pandemic: a systematic review and meta-analysis. Front Psychiatry. 2023;14:1286101.
Mittermeier I, Merlic D, Braschl S, Sealtiel L, Weilnhammer V, Quartucci C, Weinmann T, et al. Mental health and work-related factors in healthcare workers in a pandemic - meta-analysis. Psychol Health Med. 2023;28(10):3005–51.
Cheung F, Lun VMC, Ngo HY, Fong E, et al. Seeking harmony in Chinese families: a dyadic analysis on Chinese parent–child relations. Asian J Soc Psychol. 2020;23(1):82–90.
Zeng Z, Holtmaat K, Verdonck-de Leeuw IM, Koole SL. Chinese college students’ mental health during the first three months of the COVID-19 pandemic: the protective role of family functioning. Front Public Health. 2024;12:1383399.
Tselebis A, Lekka D, Sikaras C, Tsomaka E, Tassopoulos A, Ilias I, Bratis D. Insomnia, perceived stress, and Family support among nursing staff during the Pandemic Crisis. Healthcare, 2020, 8(4).
Acknowledgements
The authors express our appreciation to the General Research Project of Zhejiang Provincial Department of Education, for funding this project. Additionally, we would like to thank all the participating nurses for their cooperation and assistance.
Funding
This work was supported by the General Research Project of Zhejiang Provincial Department of Education (Y202043652).
Author information
Authors and Affiliations
Contributions
Lingxiao Ye: Research design, Data collection, Writing— Original draft, Resources. Feng Zhang: Research design, Data collection, Data analysis, Writing— original draft and revision. Lili Wang: Funding acquisition, Research design, Data collection, Data analysis, Visualization, Writing— revision. Yufei Chen: Data collection. Jiaran Shi: Conceptualization, Research design, Supervision, Writing— review, revision, and editing. Tingting Cai: Methodology guidance, Research design, Resources, Supervision, Writing— review, revision, and editing. All the authors fully participated in this work and assumed public responsibility for the relevant part of the content. Lingxiao Ye and Feng Zhang contributed equally to this work. We understand that the Corresponding Author is the contact for the editorial process. They are responsible for communicating with the other authors about progress, submitting revisions, and final approval of proofs. All authors agree to the final version of the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Ethics Committee of Ningbo Medical Center LiHuili Hospital (2023-C-119).Written informed consent was obtained from all the participants prior to enrollment in this study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it.The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Ye, L., Zhang, F., Wang, L. et al. Identification of the risk factors for insomnia in nurses with long COVID-19. BMC Nurs 23, 532 (2024). https://doi.org/10.1186/s12912-024-02212-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12912-024-02212-4