Abstract
Background
Patient experience plays an essential role in improving clinical effectiveness and patient safety. It’s important to identify factors influencing patient experience and to improve quality of healthcare.
Objective
To identify factors that influence patient experience in hospital wards.
Methods
We conducted a systematic review including six databases; they were PubMed, CINAHL, Embase, PsycInfo, ProQuest, and Cochrane. Studies were included if they met the inclusion criteria. The JBI checklist was used to perform quality appraisal. We used 5 domains of the ecological model to organize and synthesize our findings to comprehensively understand the multi-level factors influencing the issue.
Result
A total of 138 studies were included, and 164 factors were identified. These factors were integrated into 6 domains. All domains but one (survey-related factors) could be mapped onto the attributes of the ecological framework: intrapersonal, interpersonal, institutional, community, and public policy level factors. All factors had mixed effect on patient experience. The intrapersonal level refers to individual characteristics of patients. The interpersonal level refers to interactions between patients and healthcare providers, such as the caring time spent by a nurse. The institutional level refers to organizational characteristics, rules and regulations for operations, such as hospital size and accreditation. The community level refers to relationships among organizations, institutions, and informational networks within defined boundaries, such as a hospital located in a larger population area. Public policy level refers to local, state, national, and global laws and policies, including health insurance policies. The sixth domain, survey-related factors, was added to the framework and included factors such as survey response rate and survey response time.
Conclusion
The factors influencing patient experience are comprehensive, ranging from intrapersonal to public policy. Providers should adopt a holistic and integrated perspective to assess patient experience and develop context-specific interventions to improve the quality of care.
PROSPERO registration number CRD42023401066
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Introduction
Patient experience refers to “the sum of all interactions, shaped by an organization’s culture, that influence patient perceptions, across the continuum of care“ [1]. In the course of health care, patients can provide more direct and detailed information, helping providers to be more sensitive and responsive to the specific needs of individual patients, so as to provide personalized and holistic care [2]. Previous studies have indicated that better patient experience is associated with lower mortality rates, hospital-acquired infection rates, medical error rates, as well as improved health status, functional ability, and quality of life [3]. Measuring patient experience, therefore, has become a critical approach to demonstrate real changes in healthcare delivery itself and evaluate the quality of medical services which is an essential component of health service innovation [4]. The report Crossing the Global Quality Chasm in 2018 pointed out that the path to a high-quality future in healthcare needs to integrate elements of person-centered care into healthcare systems and continually improve the experience of patients, families, and communities [5]. Organizations and policy-makers worldwide have begun to measure, report and leverage patient experience data to implement quality improvement strategies [6].
Improving patient experience has become the common goal for global healthcare institutions, and determining the influencing factors is a necessary first step, which could lay the foundation for further intervention. Patient experience can vary in different care settings. Healthcare institutes worldwide have developed the special survey programmes targeted at different healthcare services, for example, Consumer Assessment of Healthcare Providers and Systems (CAHPS) program have released CAHPS Hospital Survey for the inpatient setting [7], and CAHPS Outpatient and Ambulatory Surgery Survey for the outpatient setting [8]. Additionally, National Accident and Emergency (A&E) Department Survey is used in the emergency setting [9]. Among different survey programs, those for the inpatient setting have attracted the most attention, since inpatients have the longest interaction time and most interaction interfaces with healthcare providers during service encounters, and their care experience will largely influence their overall rating of the hospital. Moreover, focusing on this population could contribute to achieving a more holistic and integrated perspective on the influencing factors of patient experience. However, there is no clear understanding of the extent to which various factors influence inpatients’ experience of care. Previous studies have only focused on specific populations, such as cancer patients and emergency patients [10, 11]. A systematic review addressing influencing factors for the inpatient population has been lacking.
Theorical framework
The integration of factors influencing the patient experience was based on the ecological model proposed by McLeroy [12]. The ecological model conceptualizes health broadly, placing an individual’s behaviour in a larger context and considering multiple levels of influence external and internal to the individual, as well as interactions across levels of influence [13]. This model emphasizes five domains of influence on health outcome, ranging from micro to macro level: intrapersonal, interpersonal, institutional, community, and public policy. It is often used in various health promotion programmes because this model assumes that appropriate changes in the social environment will produce changes in individuals, and that the support of individuals is essential for implementing environmental changes.
The key reason for choosing this theory is that our aim is to provide a comprehensive depiction of influencing factors, enabling a deeper understanding of potential intervention points. Upon reviewing existing literature, we found that the influencing factors on patient experience span multiple domains, ranging from individual characteristics to policy changes. Commonly used theoretical models in patient experience research, such as Donabedian’s Structure Process-Outcome Model [14] and the Institute of Medicine’s Framework of healthcare quality [15], predominantly focus on the quality of services provided by hospitals. However, these models do not offer an intuitive and comprehensive understanding of all factors influencing patient experience.
In summary, this systematic review aims to identify influencing factors of patient experience in hospital wards within the multiple levels of McLeroy et al.‘s ecological model.
Methods
This review was reported according to “The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 statement“ [16]. We have registered our protocol in PROSPERO previously, the registered number is CRD42023401066.
Search strategy
The retrieval period spans from the establishment of each of the databases to August 23, 2022 by two independent authors TG and XC. A total of six databases were searched, including PubMed, CINAHL, Embase, PsycInfo, ProQuest, and Cochrane. In addition, we supplemented the included studies by searching for citations. Search terms included Mesh terms, free-text synonyms, and controlled vocabulary for “patient experience”, “patient perception of care”, and “inpatient” to locate relevant research published. A search filter was used to limit to the English language, and there was no publication data limitation. See Additional file 1 for the detailed search strategy.
Eligible criteria
Operational definition of patient experience
Although we chose articles that explicitly contained the terms “patient experience” and “patient perception of care”, the terms patient experience and patient satisfaction are often used interchangeably, with the potential to cause confusion and misunderstanding. Therefore, we carefully re-examined the articles to determine the concept of patient experience and formulated detailed criteria before reviewing the factors.
Patient experience is “feedback from patients on ‘what actually happened’ in the course of receiving care or treatment, capturing both the objective facts and their subjective views of it”. This places the focus for patient experience firmly both on what happens to patients, and how they report that experience [1, 2]. On the other hand, patient satisfaction focuses on the subjective evaluation of patients, mainly reflecting whether the care provideds meet their needs and expectations [17]. It is more an outcome variable than patient experience. Therefore, questionnaires on experience will focus on what happened and what patients felt, so the scoring method will be more objective and detailed, such as “always” and “no” rather than responses like “very satisfied” and “dissatisfied“ [2].
Based on the nature and definition of patient experience, we established the following criteria and considered a variable to be patient experience if it met all the following conditions: (1) Measurement instruments should consist of scales or questionnaires that have undergone a formal development process and have been tested for reliability or validity. (2) Likert scoring method contains frequency (never to always), agreement (disagree to agree), and degree (not at all to a very high degree), and studies with the Likert scoring method using satisfied/excellent would be excluded. (3)We focused on the studies that measured patient experience by overall scores or specific dimensions of the patient experience scale, and excluded studies that only evaluate dependent variables with specific items, global scores, and recommendation levels.
Inclusion and exclusion criteria
Hence, these studies would be included: (1) the population was adult hospitalized patients, (2) the outcome was patient experience, (3) the theme was examining factors associated with patient experience, (4) the study design was an observational study, (5) the article type was primary research, (6) the language was English. And studies would be excluded: (1) the research setting was in specific health facilities (pediatrics and adolescence, psychiatry, ICU, emergency, outpatient, operating room, obstetrics), (2) The study did not have any statistically significant results (P ≥ 0.05), (3) the full text was not available.
Screening and data extraction
All retrieved articles were exported into Endnote X9, and duplicates were removed. Then two authors independently reviewed the studies and a consensus would be reached through discussion. The process of screening was strictly carried out according to the PRISMA flowchart [18]. The data extracted from the remaining studies included: author, date, location, sample, number of centers, design, theory framework, statistical analysis methods, outcome, outcome measurements, and factors.
Quality evaluation
The JBI checklists for cross-sectional, cohort, and case-control studies were used to assess the methodological quality of each study [19]. Two authors (TG and JL) evaluated the study independently. If there was disagreement between the two parties, the issue would be decided by the third author (YZ). We scored yes/no/unclear/not applicated for each question, “Yes” answer scored one point, “no and unclear” scored zero point, and “not applicated” wasn’t counted. The quality score is calculated by the actual score as a percentage of the total score. Studies would be classified into the following categories: excellent (> 80%), some limitations (50–80%), and several limitations (< 50%) [20,21,22]. The quality appraisal wouldn’t be used as the basis for the exclusion of studies, but only for having a better understanding of the quality of the literature in the field.
Data synthesis
We placed the collated determinants into different domain and subdomains based on the ecological model [12]. The intrapersonal level refers to individual characteristics of individuals, we divided this domain into three subdomains: patient characteristics and traits, patient health-related, and patient medical experience based on reviewed factors. The interpersonal level refers to interactions between patients and nurses, it contained two subdomains, staff’ characteristics, traits, and outcomes, staff behaviours and interactions. The institutional level refers to organizational characteristics, rules and regulations for operations. Factors in this domain were categorized into three subdomains, characteristic of institutional, organizational management model and working climate. The community level refers to relationships among organizations, institutions, and informational networks within defined boundaries. Public policy refers to local, state, national, and global laws and policies. The sixth domain of survey related factors was not part of the model. The full data synthesis process was performed by two authors(TG and XC), and the decision was made by the third author (YZ) in case of disagreement.
Result
Study selection
A total of 25,559 studies were identified from the database, and 13 studies were identified through citation tracking. After the first round of screening 1022 papers were selected. In the second round of screening, 473 were non-observational studies(130 qualitative studies, 187 interventional studies and 156 tool development studies), 188 were not about influences on patient experience, 19 were not original research, 158 had outcomes that were not patient experience, 44 were not about inpatients, 1 was not in English, and 12 did not have any significant influences. Finally, 138 studies were included, with 133 cross-sectional, 3 longitudinal, and 2 cohort studies [23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111,112,113,114,115,116,117,118,119,120,121,122,123,124,125,126,127,128,129,130,131,132,133,134,135,136,137,138,139,140,141,142,143,144,145,146,147,148,149,150,151,152,153,154,155,156,157,158,159,160]. See Fig. 1PRISMA Flowchart for PRISMA results.
Of the total 138 studies, there were 87 studies conducted in the USA, 8 studies in the UK, 7 studies in Norway, 5 studies in China, 4 studies in the Netherlands, 3 studies in Turkey. Two studies each for countries Poland, Finland, Iran, Italy. One study each for other 13 countries, such as Denmark, German, Canada, etc. Three studies were conducted in multiple countries.
Seventy-nine studies were multicenter investigations. Hungary, Jordan, Slovenia, and Thailand had only single-center studies. There was a wide disparity in the sample size of included studies with a minimum of 50 and a maximum of 5,480,308. In addition, 38 studies did not describe the sample size.
A theoretical model was used to find possible related factors of patient experience in 12 of the 138 studies. Eight studies used Donabedian’s Structure Process-Outcome Model. The rest were The Institute of Medicine (IOM)’s Framework of Patient-Centered Care, Klein and Kozlowski’s Multilevel Theory, Andersen’s Behavioral Model, Hospital Organizational Composition, Quality Health Outcomes Model, Resource Dependency Theory. They all appeared only once.
A total of 27 measurements of patient experience were used, eight of which were patient experience of nursing (n = 17). The most frequently used was HCAHPS (n = 86). More detailed information on the characteristics was provided in Additional file 2.
Quality assessment
A total of 133 cross-sectional studies and 3 longitudinal studies, were assessed using a cross-sectional study checklist. Additionally, 2 studies were evaluated using a cohort study checklist. The quality of 74 studies was excellent, 45 studies had some limitations and 19 studies had several limitations. See Table 1 (below).
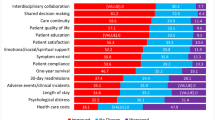
Factors associated with patient experience
A total of 164 factors were identified. There were 138 studies reporting at least one factor significantly related to patient experience. Age (n = 38), education (n = 27), gender (n = 43), and length of stay(n = 27) were commonly examined, but yielded mixed results – showing no influence, positive or a negative influence on patient experience. All factors were sorted into five domains by content analysis: intrapersonal level, interpersonal level, institutional level, community level, policy level, and we add another domain, survey related factors, as this was a factor related to the survey process and could not be included in the model. Tables 2–7 was presented these factors related to patient experience. In these tables, ‘increased’ and ‘decreased’ indicate whether the relationship between this factor and patient experience is positive or negative, respectively. ‘No change’ indicateds that the result is not significant(P ≥ 0.05).
Intrapersonal factors
Eighty-one factors related to intrapersonal experience were examined in 90 studies. Table 2 was presented the factors in intrapersonal level(below). In the patient characteristic and traits subdomain, the effect of most factors was mixed. Older age was positively linked to patient experience in 13 studies [39, 56, 76, 86, 89, 101, 102, 105, 106, 130, 138, 144, 157], negatively linked in 13 studies [25, 31, 37, 48, 59, 60, 68, 76, 80, 109, 143, 152, 157], and showed no change in 25 studies [24, 44, 48, 50, 54, 58, 59, 65, 68, 77, 83,84,85,86, 92, 93, 98, 102, 105, 109, 112, 113, 137, 145, 156]. The impact of factors such as higher income [49, 65, 80, 115, 126] and employed patient [49, 92, 93, 109, 116] on patient experience were inconclusive as well.
In the patient health-related subdomain, good health condition was the most frequent factor positively linked to patient experience in 11 studies [35, 64, 76, 86, 105, 130, 137, 143, 148, 152, 157], negatively associated in 8 studies [39, 56, 83, 84, 100, 118, 137, 138], and no significant in 7 studies [24, 49, 92, 93, 98, 145, 150].Patient experiencing complication [48, 79, 118, 134, 146] and having comorbidity or chronic disease [44, 77, 80, 92, 93, 138, 152, 159] in most studies had been negatively related to patient experience.
In the patient medical experience subdomain, length of stay was the most frequent factor with mixed effect on patient experience [24, 25, 42, 48,49,50, 58, 59, 65, 66, 68, 77, 80, 84,85,86, 92, 93, 98, 105, 110, 125, 129, 142, 143, 145, 153]. Both routine admission and discharge to home were positively associated with patient experience in most related studies [39, 56, 77, 105, 119, 124, 130, 139, 157]. In addition, patient isolation and number of admissions were negatively influencing factor [39, 56, 127, 149].
Interpersonal factors
Eighteen factors related to interpersonal had been found in 23 studies. Table 3 was prestented the factors in interpersonal level(below). In the Staff’ characteristics, traits, and outcomes subdomain, we could find staff’s age [58] and nurses’ wage [108] were negatively associated with patient experience. Conversely, nurses’ education [95] and nurses’ job satisfaction [89] were identified as positive factors. Different doctors’ specialties and nurses’ depersonalizationcan had mixed effect on patient perceptions of medical care [32, 54, 58, 155].
In the Staff behaviors and interactions subdomain, eight factors such as time nurses spent [25, 33] were all related positively to patient experience.Two factors including incorrect treatment [56] and counterproductive caring behaviors [116, 155] were negatively related to patient experience.
* The results of univariate analysis show differences, but the exact positive and negative relationship are unclear.
Institutional level
In the domain institutional factors, 49 factors were exacted from 66 studies. Table 4 was presented the factors in institutional level (below). In the Characteristic of institutional subdomain, larger hospital [24, 27, 43, 44, 56, 67, 74, 80, 82, 105, 108, 133, 138, 157], non-profit ownership [24, 27, 44, 67, 74, 82, 91, 107, 108, 133, 147, 157] and teaching hospital [27, 56, 67, 74, 80, 82, 91, 94, 105, 107, 108, 117, 130, 133, 137, 140, 147, 150, 157] were the most commonly occurring factors. Their impact on patient experience, along with the other ten factors, such as hospital accreditation [29, 36, 90] were mixed. Ten factors, such as physician ownership [27, 34], positively contributed to patient experience. Twelve factors like the number of patients present daily [43, 112] were all negatively related to patient experience.
In the organizational management model subdomain, there are eight factors in total, with six factors such as nursing staffing [24, 33, 44, 45, 80, 89, 95, 97, 108, 121, 158] having mixed effect on patient experience.
In the working climate subdomain, three factors such as staffs receive support from other staffs [66] were all positively related to patient experience. The other three factors have all been shown to play no role in some studies.
Community level
There were six factors related to community exacted from 11 studies. Table 5 was prestented the factors in comunity level(below). A hospital located in larger population area was the most occurring factor, showing a positive effect on patient experience in two studies [67, 80], a negative effect in 7 studies [44, 56, 74, 80, 91, 94, 133], and no effect in one study [24]. Two factors such as the residents education level of patients’ community [86] were positively influencing factors.
Public policy level
The policies influencing patient experience were all related to payment style. Medicaid [24, 76, 80, 94] and Medicare [27, 58, 76, 78, 80] had mixed impact on patient experience. Implementation of Maryland’s global payment model [40] was a positive factor. Table 6 is showing the factors in interpersonal level (below).
Survey related
Four factors were related to the survey process. Telephone survey mode [157] was positively associated with patient experience. Longer survey response time was a negative factor in three studies [39, 77, 83]. Higher survey response rates had positive effect in 2 studies [34, 117], and no effect in one study [66]. Patients with a proxy response tended to report worse patient experiences but no change after controlling for demographic differences [38]. Table 7 is showing the factors in interpersonal level(below).
Discussion
This is the first known systematic review focusing on the factors of patient experience in hospital wards that have been published, and the first systematic review to make a clear distinction between patient experience and patient satisfaction as well. Eventually, we examined a total of 164 factors and integrated them into six domains.
The intrapersonal factor refers to characteristics of the individual, such as knowledge, attitudes, behavior, self-concept, skills and encompass the developmental history of the individual [12]. Our results indicate that the influencing factors of patients’ personal traits and experiential aspects account for almost half of all factors we have reviewed, underscoring their significant role. These factors are typically antecedents to the patient experience, existing before the patient interacts with healthcare services. Patient experience is feedback from patients on ‘what actually happened’ in the course of receiving care or treatment, both the objective facts and their subjective views of it [161]. This suggests that these antecedents greatly shape each patients’ subjective perception of medical experience. In other words, patient individuality is a key reason why patient experience is hard to be controlled [162]. Therefore, understanding these antecedents can help characterize different types of patients’ preferences for medical services, recognize their preferred modes of interaction, and encourage them to co-design the healthcare delivery process, thereby optimizing patient experience [163, 164].
The impact of intrapersonal factors on patient experience is the most controversial part. Some factors exhibit opposite effects in different studies, and even show no significant effects. This highlight the complexity of individual characteristics and their varying influence on patient experiences in different contexts. In addition to methodological differences in study design, sample size, and selection of potential factors, an important reason may be the failure to consider interactions among different intrapersonal factors [165]. For example, Shulman et al.‘s study indicated that the employment status of patients had a negative impact on their overall experience. This result differs from other studies, possibly due to the older age of the patient population under consideration [93].
The interaction between healthcare provider and patients is regarded as a crucial determinant in augmenting the quality of care and patient satisfaction in any specific environment [1]. Our review identified two aspect factors, namely personal characteristics of staff and staff’s behavior and interaction. The staff’s characteristics, emotions, identity can predict healthcare professionals’ intentions and interactive behaviors, which will affect the quality of service directly [166]. A lack of effective communication between patients and physicians can in turn lead to staff burnout, frustration and other negative emotions, which will impair the healthcare provider-patient relationship and patient outcomes [167]. Therefore, to enhance the interactive quality, healthcare leaders or managers should examine how employees interact with patients in a variety of situations and how effective the interactions are. Based on the assessment, appropriate resources like audit and feedback, reminders, and educational outreach should be provided to establish effective touchpoints [168]. Given the importance of the dyadic relationship in the patient experience, it is also another extremely valuable point to explore the mechanisms of patient-provider interaction and value co-creation and to standardize the entire service process [162].
What’s unique about this review is that we also delineate influences at the institutional, community, and policy levels to help us understand the process of shaping the patient experience at a more macro level. Institutional factors can shape the nature of team members’ interaction and influence the intervention’s efficacy [169, 170]. Our review identified three domains of institutional factors, including hospital characteristics, organizational management and working climate. While hospital characteristics maybe immutable, specific mechanisms impacting patient experiences can be addressed through targeted interventions to promote the medical service quality.For example, patients perceive poorer medical staff-patient communication in hospitals with a high proportion of ethnic minority patients [53, 94], which suggests that we can improve the cultural sensitivity of healthcare providers to create a trusting, connected healthcare environment [171].
External environment can have a huge impact on the operation of an entire hospital. Communities are stratified according to dimensions of socio-economic status, which may affect the individual’s health resource and health status [172]. Our review found that community members’ education level, income level, and unemployment rate all have an effect on patient experience. Meanwhile, different external characteristics, such as market competition, social and cultural context, funding environment and policy changing can affect patient experience as well [173]. By focusing on community and policy-related factors, healthcare providers can make effective adjustments and enhance medical care quality. Therefore, hospitals should examine the influencing mechanisms of external factors in a more in-depth manner so as to respond and take strategic actions according to the factors of the surrounding community immediately.
Whether survey data were accurately representative of clinical reality depends upon the patient’s or family’s ability to recall details about the hospitalization experience after discharge. Research indicated the memory of key events in the affective and emotional cognitive realms declines over time, which can result in incomplete or inaccurate responses [174]. Our review showed longer survey response time was related to poor patient experience scores [39, 77, 83]. As recommended by CMS, it is appropriate for survey to be administered between 2 and 42 days after discharge [175]. Survey patterns can affect the patient reported outcome as well [38, 176, 177], thus we suggested valid comparisons of hospital performance require some adjustment for survey patterns and patient mix [178], and future patient experience surveys should include questions of “whether is a patient’s proxy” and “reasons for choosing a proxy”.
Limitation
There are also limitations worth noting. First, we include large number of cross-sectional studies, which is unable to demonstrate a causal relationship between these factors and patient experience directly, only offering hypotheses for future researchers to explore. Second, to ensure the credibility and consistency of the results, we ultimately chose to include only quantitative studies with statistically significant findings and exclude qualitative studies. This approach may make the results we reviewed overlook some factors that are potentially relevant to patient experience. Third, to offer general insights into patient experience factors, our combined results integrated influences from diverse cultural contexts. However, we did not conduct specific analyses for individual cultural contexts, which can lead to some factors not applying or having opposite results in different cultural settings. Besides, the use of ecological theoretical models to guide the interpretation of results may overlook some of the interaction mechanisms between internal and external environments. Finally, the exclusion of non-English literature may result in the omission of relevant literature.
Implication
Our research has revealed that utilizing the operational definition of patient experience we employed can effectively differentiate between these articles. Hence, we strongly recommend that future articles should clearly define patient experience and patient satisfaction to obtain more objective and realistic clinical data, and develop interventions that cater to clinical needs. In addition, this review has integrated and categorized the different domains of factors, which could help researchers gain a better and more comprehensive understanding of patient experience, and provide support in selecting the appropriate list of confounding factors for studies on patient experience. However, the mechanisms of interaction between domains still need to be explored, which is a key part of developing a precise intervention plan. We have listed the possible antecedents, but we have not been able to answer the ‘why’, i.e. why patients with higher levels of education have more negative experiences, and what are the discrepancies between patients’ mental expectations and the actual interactions that lead to good or bad experiences. Understanding these mechanisms can help us target our interventions.
Conclusion
Patient experience has become one of the most important indicators of health service quality evaluation today, identifying influencing factors of patient experience could help healthcare providers to understand and construct targeted interventions. Our review found that patient experience in hospital wards is influenced by six domains: intrapersonal level, interpersonal level, institutional level, community level, public policy level, survey-related factors. Patient age, gender, education level, patient health condition, and teaching hospital are the most frequent factors, but the specific role of these factors on patient experience remains unclear. Future research should explore the causal mechanisms shaping patient experience in specific contexts and target the construction of interventions.
Data availability
The datasets supporting the conclusions of this article are included within the article and its additional files.
References
Wolf JA, Niederhauser V, Marshburn D, et al. Defining patient experience. Patient Experience J. 2014;1(1):7–19.
Larson E, Sharma J, Bohren MA, et al. When the patient is the expert: measuring patient experience and satisfaction with care. Bull World Health Organ. 2019;97(8):563.
Doyle C, Lennox L, Bell D. A systematic review of evidence on the links between patient experience and clinical safety and effectiveness. BMJ open. 2013;3(1):e001570.
Berry LL. Service innovation is urgent in healthcare. AMS Rev. 2019;9(1–2):78–92.
National Academies of Sciences E. Medicine. Crossing the global quality chasm: improving health care worldwide. 2018.
Ahmed F, Burt J, Roland M. Measuring patient experience: concepts and methods. Patient-Patient-Centered Outcomes Res. 2014;7:235–41.
Rockville CAHPS. Hospital Survey: Agency for Healthcare Research and Quality; 2023 [updated November 2023. https://www.ahrq.gov/cahps/surveys-guidance/hospital/index.html.
Rockville CAHPS. Outpatient and Ambulatory Surgery Survey: Agency for Healthcare Research and Quality; 2023 [ https://www.ahrq.gov/cahps/surveys-guidance/oas/index.html.
NHS Patient Surveys Care Quality Commission. 2023 [ https://nhssurveys.org/surveys/.
Alessy SA, Alhajji M, Rawlinson J, et al. Factors influencing cancer patients’ experiences of care in the USA, United Kingdom, and Canada: a systematic review. EClinicalMedicine. 2022;47:101405.
Sonis JD, Aaronson EL, Lee RY, et al. Emergency Department patient experience: a systematic review of the literature. J Patient Experience. 2018;5(2):101–06.
McLeroy KR, Bibeau D, Steckler A, et al. An ecological perspective on health promotion programs. Health Educ Q. 1988;15(4):351–77.
Sallis JF, Owen N, Fisher E. Ecological models of health behavior. Health behavior: Theory, research, and practice. 2015;5(43–64).
Kobayashi H, Takemura Y, Kanda K. Patient perception of nursing service quality; an applied model of Donabedian’s structure-process‐outcome approach theory. Scand J Caring Sci. 2011;25(3):419–25.
America CoQoHCi. Crossing the quality chasm: a new health system for the 21st century. National Academies; 2001.
Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg. 2021;88:105906.
Sitzia J, Wood N. Patient satisfaction: a review of issues and concepts. Soc Sci Med. 1997;45(12):1829–43.
Haddaway NR, Page MJ, Pritchard CC, et al. PRISMA2020: an R package and Shiny app for producing PRISMA 2020-compliant flow diagrams, with interactivity for optimised digital transparency and open synthesis. Campbell Syst Reviews. 2022;18(2):e1230.
Moola S, Munn Z, Tufanaru C, et al. Chapter 7: systematic reviews of etiology and risk. Volume 5. Joanna briggs institute reviewer’s manual The Joanna Briggs Institute; 2017.
Vo M, Thonglor R, Moncatar T, et al. Fear of falling and associated factors among older adults in Southeast Asia: a systematic review. Public Health. 2023;222:215–28.
Spedale V, Luciani M, Attanasio A, et al. Association between sleep quality and self-care in adults with heart failure: a systematic review. Eur J Cardiovasc Nurs. 2021;20(3):192–201.
Mbuzi V, Fulbrook P, Jessup M. Effectiveness of programs to promote cardiovascular health of indigenous australians: a systematic review. Int J Equity Health. 2018;17(1):1–17.
Abdelgadir J, Edmund WO, Abdalla SM, et al. Demographic Factors Associated with patient-reported outcome measures in Pain Management. Pain Physician. 2020;23(1):17–24.
Abrahamson K, Hass Z, Morgan K, et al. The relationship between nurse-reported safety culture and the patient experience. J Nurs Adm. 2016;46(12):662–68.
Ahmad MM, Alasad JA. Predictors of patients’ experiences of nursing care in medical-surgical wards. Int J Nurs Pract (Wiley-Blackwell). 2004;10(5):235–41.
Alaloul F, Myers J, Masterson KM, et al. Patient experience factors and health-related quality of life in hospitalized individuals. Oncol Nurs Forum. 2019;46(2):238–47.
Al-Amin M, Makarem SC. The effects of Hospital-Level factors on patients’ ratings of Physician Communication. J Healthc Manag/Am Coll Healthc Exec. 2016;61(1):28–41.
Al-Jabri Fatma Yaqoob M, Turunen H, Kvist T. Patients’ perceptions of Healthcare Quality at hospitals measured by the revised Humane Caring Scale. J Patient Experience. 2021;8.
Andres EB, Song W, Song W, et al. Can hospital accreditation enhance patient experience? Longitudinal evidence from a Hong Kong hospital patient experience survey. BMC Health Serv Res. 2019;19(1):623.
Bachnick S, Ausserhofer D, Baernholdt M, et al. Patient-centered care, nurse work environment and implicit rationing of nursing care in Swiss acute care hospitals: a cross-sectional multi-center study. Int J Nurs Stud. 2018;81:98–106.
Bahrami F, Hasanvand S, Goudarzi F, et al. Cardiac patients’ perception of a good nursing care: a cross-sectional study. Int Cardiovasc Res J. 2020;14(1):30–5.
Bari V, Hirsch JS, Narvaez J, et al. An approach to predicting patient experience through machine learning and social network analysis. J Am Med Inf Association: JAMIA. 2020;27(12):1834–43.
Barnicot K, Allen K, Hood C, et al. Older adult experience of care and staffing on hospital and community wards: a cross-sectional study. BMC Health Serv Res. 2020;20(1):583.
Bartlett Ellis RJ, Bakoyannis G, Haase JE, et al. Patient perceptions of provider and hospital factors Associated with New Medication Communication. West J Nurs Res. 2016;38(9):1139–54.
Bartlett Ellis RJ, Werskey KL, Stangland RM et al. Using HCAHPS data to model correlates of medication understanding at hospital discharge. Nursing: Research & Reviews. 2017;7:1–7.
Bergholt MD, Falstie-Jensen AM, Brink Valentin J et al. Patients experience more support, information and involvement after first-time hospital accreditation: a before and after study in the Faroe Islands. Int J Qual Health care: J Int Soc Qual Health Care. 2021;33(4).
Biondi EA, Hall M, Leonard MS, et al. Association between resource utilization and patient satisfaction at a tertiary care medical center. J Hosp Med. 2016;11(11):785–91.
Bjertnaes OA. Patient-reported experiences with hospitals: comparison of proxy and patient scores using propensity-score matching. Int J Qual Health care: J Int Soc Qual Health Care. 2014;26(1):34–40.
Bjertnaes OA. The association between survey timing and patient-reported experiences with hospitals: results of a national postal survey. BMC Med Res Methodol. 2012;12:13.
Blanco-Topping R. The impact of Maryland’s global reimbursement system on patient satisfaction: A one-way analysis of variance. ProQuest Information & Learning; 2019.
Bliefnick JM, Ryherd EE, Jackson R. Evaluating hospital soundscapes to improve patient experience. J Acoust Soc Am. 2019;145(2):1117–28.
Bloom DA, Manjunath AK, Gualtieri AP, et al. Patient satisfaction after total hip arthroplasty is not influenced by reductions in Opioid Prescribing. J Arthroplasty. 2021;36(7 Supplement):S250–57.
Bolton LB, Aydin CE, Donaldson N, et al. Nurse staffing and patient perceptions of nursing care. J Nurs Adm. 2003;33(11):607–14.
Brady BM, Zhao B, Niu J, et al. Patient-reported experiences of Dialysis Care within a National Pay-for-performance system. JAMA Intern Med. 2018;178(10):1358–67.
Brooks-Carthon JM, Kutney-Lee A, Sloane DM, et al. Quality of care and patient satisfaction in hospitals with high concentrations of black patients. J Nurs Scholarsh. 2011;43(3):301–10.
Camilleri S, Diebold J. Hospital uncompensated care and patient experience: an instrumental variable approach. Health Serv Res. 2019;54(3):603–12.
Campbell L, Li Y. Are Facebook user ratings associated with hospital cost, quality and patient satisfaction? A cross-sectional analysis of hospitals in New York State. BMJ Qual Saf. 2018;27(2):119–29.
Catalano MA, Hemli JM, Yu PJ et al. Patient Satisfaction Scores After Cardiac Surgery: Should They Be Risk-Adjusted? Seminars in thoracic and cardiovascular surgery. 2022.
Chan SK, Wong IO, Tin KY, et al. Satisfaction with inpatient care in a population-based Hong Kong Chinese sample. Qual Saf Health Care. 2010;19(3):173–81.
Charalambous A, Efstathiou G, Adamakidou T, et al. Adult cancer patients satisfaction of nursing care: a cross-national evaluation of two Southeastern European countries. Int J Health Plann Manage. 2014;29(4):e329–46.
Chatterjee P, Joynt KE, Orav EJ, et al. Patient experience in safety-net hospitals: implications for improving care and value-based purchasing. Arch Intern Med. 2012;172(16):1204–10.
Chen A, Kuhlmann P, Souders C, et al. Assessing the impact of Urology Resident involvement on overall patient satisfaction. J Surg Educ. 2021;78(5):1655–59.
Chen J, Koren ME, Munroe DJ, et al. Is the hospital’s magnet status linked to HCAHPS scores? J Nurs Care Qual. 2014;29(4):327–35.
Chen JG, Zou B, Shuster J. Relationship between patient satisfaction and physician characteristics. J Patient Experience. 2017;4(4):177–84.
Chen LM, Birkmeyer JD, Saint S, et al. Hospitalist staffing and patient satisfaction in the national Medicare population. J Hosp Med. 2013;8(3):126–31.
Danielsen K, Garratt AM, Bjertnaes ØA, et al. Patient experiences in relation to respondent and health service delivery characteristics: a survey of 26,938 patients attending 62 hospitals throughout Norway. Scand J Public Health. 2007;35(1):70–7.
de Vos MS, Hamming JF, Boosman H, et al. The Association between complications, incidents, and patient experience: retrospective linkage of routine patient experience surveys and Safety Data. J Patient Saf. 2021;17(2):e91–7.
Diwan W, Nakonezny PA, Wells J. The effect of length of Hospital stay and patient factors on patient satisfaction in an academic hospital. Orthopedics. 2020;43(6):373–79.
Eftekhary N, Feng JE, Anoushiravani AA, et al. Hospital Consumer Assessment of Healthcare Providers and systems: do patient demographics affect outcomes in total knee arthroplasty? J Arthroplast. 2019;34(8):1570–74.
Elliott MN, Beckett MK, Cohea C et al. The hospital care experiences of older patients compared to younger patients. J Am Geriatr Soc. 2022.
Elliott MN, Lehrman WG, Beckett MK, et al. Gender differences in patients’ perceptions of inpatient care. Health Serv Res. 2012;47(4):1482–501.
Fareed N, MacEwan SR, Vink S, et al. Relationships between patient portal activation and patient satisfaction scores among CG-CAHPS and HCAHPS respondents. Am J Manag Care. 2022;28(1):25–31.
Figueroa JF, Feyman Y, Xiner Z, et al. Hospital-level care coordination strategies associated with better patient experience. BMJ Qual Saf. 2018;27(10):844–51.
Figueroa JF, Zheng J, Orav EJ, et al. Across US Hospitals, Black patients Report comparable or better experiences Than White patients. Health Aff. 2016;35(8):1391–98.
Findik UY, Unsar S, Sut N. Patient satisfaction with nursing care and its relationship with patient characteristics. Nurs Health Sci. 2010;12(2):162–69.
Flott K, Darzi A, Mayer E. Care pathway and organisational features driving patient experience: statistical analysis of large NHS datasets. BMJ open. 2018;8(7):e020411.
Ford EW, Huerta TR, Diana ML, et al. Patient satisfaction scores and their relationship to hospital website quality measures. Health Mark Q. 2013;30(4):334–48.
Frane N, Stapleton EJ, Petrone B et al. Patient satisfaction after Lower Extremity Total Joint Arthroplasty: an analysis of medical comorbidities and patient demographics. J Patient Experience. 2021;8.
Gearhart SF. The relationship between care provider perceptions of safety culture and patient perceptions of care on three hospital units. San Francisco: University of California; 2008.
Goldstein E, Elliott MN, Lehrman WG, et al. Racial/Ethnic differences in patients’ perceptions of Inpatient Care using the HCAHPS Survey: MCRR. Med Care Res Rev. 2010;67(1):74–92.
Groene O, Arah OA, Klazinga NS, et al. Patient experience shows little relationship with Hospital Quality Management Strategies. PLoS ONE. 2015;10(7):e0131805.
Gurland BH, Merlino J, Sobol T, et al. Surgical complications impact patient perception of hospital care. J Am Coll Surg. 2013;217(5):843–49.
Hanson KT, Zalewski NL, Hocker SE et al. At the Intersection of Patient Experience Data, Outcomes Research, and Practice: Analysis of HCAHPS Scores in Neurology Patients. Mayo Clinic proceedings Innovations, quality & outcomes. 2018;2(2):137 – 47.
Herrin J, Mockaitis KG, Hines S. HCAHPS scores and Community factors. Am J Med Quality: Official J Am Coll Med Qual. 2018;33(5):461–71.
Hessels AJ. Impact of health information technology on delivery and quality of patient care. Rutgers The State University of New Jersey - Newark; 2014.
Hicks LS, Ayanian JZ, Orav EJ, et al. Is hospital service associated with racial and ethnic disparities in experiences with hospital care? Am J Med. 2005;118(5):529–35.
Hopkins BS, Patel MR, Yamaguchi JT, et al. Predictors of patient satisfaction and survey participation after spine surgery: a retrospective review of 17,853 consecutive spinal patients from a single academic institution. Part 2: HCAHPS. J Neurosurg Spine. 2019;30(3):389–96.
Indovina KA, Keniston A, Manchala V, et al. Predictors of a top-box patient experience: a retrospective observational study of HCAHPS Data at a Safety Net Institution. J Patient Experience. 2021;8:23743735211034342.
Isaac T, Zaslavsky AM, Cleary PD, et al. The relationship between patients’ perception of care and measures of hospital quality and safety. Health Serv Res. 2010;45(4):1024–40.
Kang YS, Tzeng HM, Zhang T. Rural disparities in Hospital patient satisfaction: Multilevel Analysis of the Massachusetts AHA, SID, and HCAHPS Data. J Patient Experience. 2020;7(4):607–14.
Kazley AS, Diana ML, Ford EW, et al. Is electronic health record use associated with patient satisfaction in hospitals? Health Care Manage Rev. 2012;37(1):23–30.
Kazley AS, Ford EW, Diana M, et al. Market factors related to hospitals’ patient satisfaction ratings. J Hosp Adm. 2015;4(4):40–7.
Kebaish KJ, Mercier MR, Duy PQ, et al. Spine surgery HCAHPS patient satisfaction survey results inversely correlate with Survey Response Time. Spine. 2021;46(18):1264–70.
Köberich S, Feuchtinger J, Farin E. Factors influencing hospitalized patients’ perception of individualized nursing care: a cross-sectional study. BMC Nurs. 2016;15:1–11.
Kózka M, Bodys-Cupak I, Strzelec B, THE NURSING SATISFACTION OF PATIENTS TREATED AT INTERNAL MEDICINE WARDS, et al. Pol Nurs / Pielegniarstwo Polskie. 2019;72(2):121–28.
Kranjac AW, Kranjac D, Fortier MA et al. Surgical Patients’ Hospital Experience Scores: Neighborhood Context Conceptual Framework. Annals of surgery. 2021.
Krol MW, De Boer D, Sixma H, et al. Patient experiences of inpatient hospital care: a department matter and a hospital matter. Int J Qual Health care: J Int Soc Qual Health Care. 2015;27(1):17–25.
Kutney-Lee A, Melendez-Torres GJ, McHugh MD, et al. Distinct enough? A national examination of catholic hospital affiliation and patient perceptions of care. Health Care Manage Rev. 2014;39(2):134.
Kvist T, Voutilainen A, Mäntynen R, et al. The relationship between patients’ perceptions of care quality and three factors: nursing staff job satisfaction, organizational characteristics and patient age. BMC Health Serv Res. 2014;14(1):466–66.
Lam MB, Figueroa JF, Feyman Y, et al. Association between patient outcomes and accreditation in US hospitals: observational study. BMJ (Clinical Res ed). 2018;363:k4011.
Lehrman WG, Elliott MN, Goldstein E, et al. Characteristics of hospitals demonstrating superior performance in patient experience and clinical process measures of care. Med care Res Review: MCRR. 2010;67(1):38–55.
Leonardsen AL, Grøndahl VA, Ghanima W, et al. Evaluating patient experiences in decentralised acute care using the picker patient experience questionnaire; methodological and clinical findings. BMC Health Serv Res. 2017;17(1):685.
Leonardsen AL, Jelsness-Jørgensen LP. Patient experiences and predictors in an acute geriatric ward: a cross-sectional study. J Clin Nurs. 2017;26(23–24):4567–73.
Liu SS, Wen YP, Mohan S, et al. Addressing Medicaid Expansion from the perspective of Patient experience in hospitals. Patient. 2016;9(5):445–55.
Liu X, Zheng J, Liu K, et al. Associations of nurse education level and nurse staffing with patient experiences of hospital care: a cross sectional study in China. Res Nurs Health. 2020;43(1):103–13.
Maher DP, Woo P, Wong W, et al. Perioperative factors associated with Hospital Consumer Assessment of Healthcare Providers and systems responses of total hip arthroplasty patients. J Clin Anesth. 2016;34:232–8.
Martsolf GR, Gibson TB, Benevent R, et al. An examination of Hospital Nurse staffing and patient experience with care: differences between cross-sectional and longitudinal estimates. Health Serv Res. 2016;51(6):2221–41.
Matar RN, Shah NS, Vincent JC, et al. Factors that influence inpatient satisfaction after shoulder arthroplasty. J Shoulder Elbow Surg. 2021;30(4):e165–72.
Mazurenko O, Richter J, Swanson Kazley A, et al. Examination of the relationship between management and clinician perception of patient safety climate and patient satisfaction. Health Care Manage Rev. 2019;44(1):79–89.
Merlino JI, Kestranek C, Bokar D, et al. HCAHPS Survey results: impact of severity of illness on hospitals’ performance on HCAHPS Survey results. J Patient Experience. 2014;1(2):16–21.
Midilli TS, Kirmizioglu T, Kalkim A. Affecting factors and relationship between patients’ attitudes towards the nursing profession and perceptions of nursing care in a university hospital. JPMA J Pakistan Med Association. 2017;67(7):1059–64.
Min R, Li L, Zi C, et al. Evaluation of patient experience in county-level public hospitals in China: a multicentred, cross-sectional study. BMJ open. 2019;9(11):e034225.
Mobolaji-Olajide OM, Adereti SC, Odutayo PO, et al. In-patient satisfaction with nursing care: outcome measurement in a tertiary health facility in Lagos, Nigeria. Int J Afr Nurs Sci. 2020;13:100264.
Mortensen B, Borkowski N, O’Connor Stephen J, et al. The relationship between Hospital Interdepartmental transfers and Patient Experience. J Patient Experience. 2020;7(2):263–69.
Murante AM, Seghieri C, Brown A, et al. How do hospitalization experience and institutional characteristics influence inpatient satisfaction? A multilevel approach. Int J Health Plann Manag. 2014;29(3):e247–60.
Nartey Y, Tata LJ, Khakwani A, et al. Using patient experiences to evaluate care and expectations in lung cancer: analysis of the English Cancer Patient Experience Survey linked with the national cancer registry. Supportive care cancer: Official J Multinational Association Supportive Care Cancer. 2022;30(5):4417–28.
O’Barr GW. Predictability of inpatient satisfaction scores based on hospital characteristics: quantitative analysis of HCAHPS Survey data, 7/1/2013 through 6/30/2014. ProQuest Information & Learning; 2018.
Oppel EM, Young GJ. Nurse staffing patterns and patient experience of care: an empirical analysis of US hospitals. Health Serv Res. 2018;53(3):1799–818.
Ozturk H, Demirsoy N, Sayligil O, et al. Patients’ perceptions of nursing care in a University Hospital. Nurs Sci Q. 2020;33(1):12–8.
Peres-da-Silva A, Kleeman LT, Wellman SS, et al. What factors drive inpatient satisfaction after knee arthroplasty? J Arthroplast. 2017;32(6):1769–72.
Pérotin V, Zamora B, Reeves R, et al. Does hospital ownership affect patient experience? An investigation into public–private sector differences in England. J Health Econ. 2013;32(3):633–46.
Persolja M, Markic M, Blatnik D, et al. Patient satisfaction with nursing care delivered in medical units in posttransitional country: a correlational study. Acta Med Mediterranea. 2018;34(6):2045–54.
Pornsiri P, Kanaungnit P, Doungrut W, et al. Predictors of Perceived Quality of Care in people with heart failure. Pac Rim Int J Nurs Res. 2019;23(1):87–99.
Quigley DD, Elliott MN, Hambarsoomian K, et al. Inpatient care experiences differ by preferred language within racial/ethnic groups. Health Serv Res. 2019;54(1Suppl 1):263–74.
Radwin LE. Cancer patients’ demographic characteristics and ratings of patient-centered nursing care. J Nurs Scholarsh. 2003;35(4):365–70.
Rajabpour S, Rayyani M, Mangolian shahrbabaki P. The relationship between Iranian patients’ perception of holistic care and satisfaction with nursing care. BMC Nurs. 2019;18(1):NPAG–NPAG.
Raleigh VS, Frosini F, Sizmur S, et al. Do some trusts deliver a consistently better experience for patients? An analysis of patient experience across acute care surveys in English NHS trusts. BMJ Qual Saf. 2012;21(5):381–90.
Saarinen IH, Koivisto JM, Kaipia A, et al. Perceived quality of surgical care in association with patient-related factors and correlation to reported postoperative complications in Finland: a cross-sectional study. BMJ open. 2020;10(11):e037708.
Sadrameli SS, Chan TM, Vaziri S, et al. Patient-reported outcomes: quality of care on a neurosurgical Ward. Qual Saf Health Care. 2021;30(3):194–99.
Sammer C, Hauck LD, Jones C, et al. Examining the relationship of an all-cause harm patient safety measure and critical performance measures at the Frontline of Care. J Patient Saf. 2020;16(1):110–16.
Schmidt LA. Patients’ perceptions of nurse staffing, nursing care, adverse events, and overall satisfaction with the hospital experience. Nurs Econ. 2004;22(6):295–306.
Schmocker RK, Holden SE, Vang X, et al. Association of Patient-Reported Readiness for Discharge and Hospital Consumer Assessment of Health Care Providers and systems patient satisfaction scores: a retrospective analysis. J Am Coll Surg. 2015;221(6):1073–82. e1-3.
Schmocker RK, Holden SE, Vang X, et al. The number of inpatient consultations is negatively correlated with patient satisfaction in patients with prolonged hospital stays. Am J Surg. 2016;212(2):282–8.
Shirk JD, Tan HJ, Hu JC, et al. Patient experience and quality of urologic cancer surgery in US hospitals. Cancer. 2016;122(16):2571–78.
Shulman B, Hutzler L, Karia R, et al. The effect of length of Stay and Discharge Disposition on Hospital Consumer Assessment of Healthcare Providers and systems scores in Orthopaedic patients. J Am Acad Orthop Surg. 2019;27(9):e418–22.
Shulman BSMD, Crowe BMD, Hutzler LMPA et al. Socioeconomic Status negatively affects HCAHPS scores in Orthopedic patients: the results of 15,789 patients at a single Institution. Bulletin of the NYU Hospital for Joint diseases. 2018;76(3):216–20.
Siddiqui ZK, Conway SJ, Abusamaan M, et al. Patient isolation for infection control and patient experience. Infect Control Hosp Epidemiol. 2019;40(2):194–99.
Siddiqui ZK, Wu AW, Kurbanova N, et al. Comparison of Hospital Consumer Assessment of Healthcare Providers and systems patient satisfaction scores for specialty hospitals and general medical hospitals: confounding effect of survey response rate. J Hosp Med. 2014;9(9):590–93.
Singer ES, Merritt RE, D’Souza DM, et al. Patient satisfaction after Lung Cancer surgery: do clinical outcomes affect Hospital Consumer Assessment of Health Care providers and systems scores? Ann Thorac Surg. 2019;108(6):1656–63.
Sjetne IS, Veenstra M, Stavem K. The effect of hospital size and teaching status on patient experiences with hospital care: a multilevel analysis. Med Care. 2007;45(3):252–58.
Smirnova A, Arah OA, Stalmeijer RE, et al. The Association between Residency Learning Climate and Inpatient Care Experience in Clinical Teaching Departments in the Netherlands. Acad Medicine: J Association Am Med Colleges. 2019;94(3):419–26.
Sorra J, Khanna K, Dyer N, et al. Exploring relationships between patient safety culture and patients’ assessments of hospital care. J Nurs Adm. 2014;44(10 Suppl):S45–53.
Spaulding A, Tafili A, Dunn A, et al. The Hospital Value-based Purchasing Program: do hospitalists improve health care value. J Hosp Med. 2022;17(7):517–26.
Stein SM, Day M, Karia R, et al. Patients’ perceptions of care are associated with quality of hospital care: a survey of 4605 hospitals. Am J Med Qual. 2015;30(4):382–88.
Stimpfel AW, Sloane DM, Aiken LH. The longer the shifts for hospital nurses, the higher the levels of burnout and patient dissatisfaction. Health Aff. 2012;31(11):2501–09.
Stimpfel AW, Sloane DM, McHugh MD, et al. Hospitals Known for Nursing Excellence Associated with Better Hospital experience for patients. Health Serv Res. 2016;51(3):1120–34.
Suhonen R, Stolt M, Berg A, et al. Cancer patients’ perceptions of quality-of-care attributes-Associations with age, perceived health status, gender and education. Journal of clinical nursing. Volume 27. John Wiley & Sons, Inc; 2018. pp. 306–16. 1–2.
Sullivan P, Bell D. Investigation of the degree of organisational influence on patient experience scores in acute medical admission units in all acute hospitals in England using multilevel hierarchical regression modelling. BMJ open. 2017;7(1):e012133.
Sullivan P, Harris ML, Bell D. The quality of patient experience of short-stay acute medical admissions: findings of the adult Inpatient Survey in England. Clinical medicine (London, England). 2013;13(6):553–56.
Sutak AK, Ryan SP, Hong CS et al. The Effect of Medical Education on patient satisfaction: an Asset or a liability? Orthopedics. 2022:1–5.
Teunissen TAM, Rotink ME, Lagro-Janssen ALM. Gender differences in quality of care experiences during hospital stay: a contribution to patient-centered healthcare for both men and women. Patient Educ Couns. 2016;99(4):631–37.
Tevis SE, Kennedy GD. Patient satisfaction: does surgical volume matter? J Surg Res. 2015;196(1):124–29.
Thiels CA, Hanson KT, Yost KJ, et al. Achieving a 5-star rating: Analysis of Hospital Consumer Assessment of Healthcare Providers and systems (HCAHPS) scores among patients undergoing elective colorectal operations. Surgery. 2016;160(4):902–14.
Thiels CA, Hanson KT, Yost KJ, et al. Effect of Hospital Case Mix on the Hospital Consumer Assessment of Healthcare Providers and systems Star scores: are all stars the same? Ann Surg. 2016;264(4):666–73.
Tonkikh O, Zisberg A, Shadmi E. Association between continuity of nursing care and older adults’ hospitalization outcomes: a retrospective observational study. J Nurs Adm Manag. 2020;28(5):1062–69.
Tzeng HM, Hu HM, Yin CY. Relationship between inpatient pressure ulcer prevalence and patient satisfaction levels based on US Medicare’s hospital compare data. J Clin Nurs (John Wiley Sons Inc). 2015;24(11–12):1730–32.
Tzeng HM, Hu HM, Yin CY, et al. Link between patients’ perceptions of their acute care hospital experience and institutions’ injurious fall rates. J Nurs Care Qual. 2011;26(2):151–60.
Veenstra M, Hofoss D. Patient experiences with information in a hospital setting: a multilevel approach. Med Care. 2003;41(4):490–99.
Vinski J, Bertin M, Sun Z et al. Impact of isolation on hospital consumer assessment of healthcare providers and systems scores: is isolation isolating? Infection control and hospital epidemiology. 2012;33(5):513–16.
Vovos TJ, Ryan SP, Hong CS, et al. Predicting Inpatient Dissatisfaction following total joint arthroplasty: an analysis of 3,593 Hospital Consumer Assessment of Healthcare Providers and systems Survey responses. J Arthroplast. 2019;34(5):824–33.
Weech-Maldonado R, Elliott M, Pradhan R, et al. Can hospital cultural competency reduce disparities in patient experiences with care? Med Care. 2012;50(Suppl0):S48–55.
Wolf A, Olsson L-E, Taft C, et al. Impacts of patient characteristics on hospital care experience in 34,000 Swedish patients. BMC Nurs. 2012;11(1):8–14.
Yalew ZM, Zeleke H, Afenigus AD, et al. Patient experience in Nursing Care and Associated factors among adult admitted patients in Debre Markos and Dessie Referral hospitals, Amhara Region, Ethiopia, 2019. J Patient Experience. 2020;7(6):1391–97.
Younas A, Sundus A. Patients’ experiences and satisfaction about care provided by male nurses in medical surgical units in Islamabad, Pakistan: a pilot study. Nurs Forum. 2018;53(1):12–9.
Zaghini F, Fiorini J, Piredda M et al. The relationship between nurse managers’ leadership style and patients’ perception of the quality of the care provided by nurses: Cross sectional survey. Int J Nurs Stud. 2020;101:N.PAG-N.PAG.
Zarzycka D, Barton E, Mazur A, et al. Socio-demographic and medical factors associated with patients’ satisfaction with nursing careand their perception of pain. Ann Agric Environ Med. 2019;26(2):298–303.
Zhu J. Patient experience with hospital care: examining the factor structure, measurement invariance, predictors, and sources of variation using the HCAHPS survey. ProQuest Information & Learning; 2014.
Zhu J, Dy SM, Wenzel J, et al. Association of Magnet Status and Nurse staffing with improvements in patient experience with Hospital Care, 2008–2015. Med Care. 2018;56(2):111–20.
Zhu L-H, Ying Q-S, Yang M et al. The Impact of Chronic Illness on the Patient Experience: Results From a Cross-Sectional Comparative Study in a Comprehensive Tertiary Hospital in China. Inquiry (00469580). 2022:1–8.
Zrinyi M, Horvath T. Impact on satisfaction, nurse-patient interactions and perceived benefits on health behaviors following a cardiac event. Eur J Cardiovasc Nurs. 2003;2(2):159–66.
Dr Foster. Intelligent board: patient experience. London2010 [ http://drfosterintelligence.co.uk/wp-content/uploads/2011/06/Intelligent-Board-2010.pdf.
Lee D. A model for designing healthcare service based on the patient experience. Int J Healthc Manag. 2019;12(3):180–88.
Domecq JP, Prutsky G, Elraiyah T, et al. Patient engagement in research: a systematic review. BMC Health Serv Res. 2014;14:1–9.
Jackson Y, Janssen E, Fischer R, et al. The evolving role of patient preference studies in health-care decision-making, from clinical drug development to clinical care management. Expert Rev PharmacoEcon Outcomes Res. 2019;19(4):383–96.
Mayer A, Thoemmes F, Rose N, et al. Theory and analysis of total, direct, and indirect causal effects. Multivar Behav Res. 2014;49(5):425–42.
Nilsen P, Potthoff S, Birken SA. Conceptualising Four categories of Behaviours: implications for implementation strategies to achieve Behaviour Change. Front Health Serv. 2021;1:795144.
Back AL, Fromme EK, Meier DE. Training clinicians with communication skills needed to match medical treatments to patient values. J Am Geriatr Soc. 2019;67(S2):S435–41.
Johnson MJ, May CR. Promoting professional behaviour change in healthcare: what interventions work, and why? A theory-led overview of systematic reviews. BMJ open. 2015;5(9):e008592.
Nilsen P, Bernhardsson S. Context matters in implementation science: a scoping review of determinant frameworks that describe contextual determinants for implementation outcomes. BMC Health Serv Res. 2019;19(1):189.
Salas E, Shuffler ML, Thayer AL, et al. Understanding and improving teamwork in organizations: a scientifically based practical guide. Hum Resour Manag. 2015;54(4):599–622.
Debesay J, Kartzow AH, Fougner M. Healthcare professionals’ encounters with ethnic minority patients: the critical incident approach. Nurs Inq. 2022;29(1):e12421.
Boylan JM, Robert SA. Neighborhood SES is particularly important to the cardiovascular health of low SES individuals. Soc Sci Med. 2017;188:60–8.
Kaplan HC, Brady PW, Dritz MC, et al. The influence of context on quality improvement success in health care: a systematic review of the literature. Milbank Q. 2010;88(4):500–59.
Redelmeier DA, Dickinson VM. Determining whether a patient is feeling better: pitfalls from the science of human perception. J Gen Intern Med. 2011;26:900–06.
CMS, Hospital CAHPS. (HCAHPS) https://www.cms.gov/Research-Statistics-Data-and-Systems/Research/CAHPS/HCAHPS12021 [ https://www.cms.gov/Research-Statistics-Data-and-Systems/Research/CAHPS/HCAHPS1.
Perneger TV, Peytremann-Bridevaux I, Combescure C. Patient satisfaction and survey response in 717 hospital surveys in Switzerland: a cross-sectional study. BMC Health Serv Res. 2020;20(1):1–8.
Sinclair M, O’Toole J, Malawaraarachchi M, et al. Comparison of response rates and cost-effectiveness for a community-based survey: postal, internet and telephone modes with generic or personalised recruitment approaches. BMC Med Res Methodol. 2012;12(1):1–8.
Elliott MN, Zaslavsky AM, Goldstein E, et al. Effects of survey mode, patient mix, and nonresponse on CAHPS hospital survey scores. Health Serv Res. 2009;44(2 Pt 1):501–18.
Acknowledgements
The authors wish to thank Dan Shi in The Nethersole School of Nursing, The Chinese University of Hong Kong, for support with the development and tests of search strategies as well as the performance of the database searches.
Funding
This research was supported by the Shanghai “Science and Technology Innovation Action Plan” under Award Number 22692109400.
Author information
Authors and Affiliations
Contributions
Tingyu GUAN: Formal analysis, Data Curation, Writing- Original draft preparation. Xiao CHEN: Formal analysis, Data curation, Writing - Review & Editing. Junfei LI: Formal analysis. Yuxia ZHANG: Conceptualization, Methodology, Writing - Review & Editing, Supervision.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Trial and protocol registration
PROSPERO registration number CRD42023401066.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Guan, T., Chen, X., Li, J. et al. Factors influencing patient experience in hospital wards: a systematic review. BMC Nurs 23, 527 (2024). https://doi.org/10.1186/s12912-024-02054-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12912-024-02054-0