Abstract
Background
As amyotrophic lateral sclerosis/motor neuron disease (ALS/MND) is a fatal progressive neurodegenerative disorder, patients experience severe impairments, with patients and family caregivers facing emotional distress and exhaustion. Several psychosocial interventions are aimed at providing tailored support for ALS/MND patients and caregivers. The aim of this study was to conduct a scoping review and present a comprehensive overview of psychosocial interventions designed for individuals and families affected by ALS/MND, while also pinpointing research gaps.
Methods
This scoping review utilized Arksey and O'Malley's methodological framework to investigate psychosocial interventions designed for individuals with ALS/MND and their families. The study adhered to the PRISMA-ScR checklist for reporting.
Results
A total of 27 articles describing 25 interventions met the inclusion criteria. The predominant interventions observed in the research encompassed education-related strategies, closely followed by behavior therapy, counseling, social support interventions, and psychotherapy interventions. Across the majority of the studies, findings indicated promising feasibility and acceptability of these interventions. Notably, a significant proportion of quantitative investigations yielded one or more statistically significant effects, while qualitative studies consistently reported favorable outcomes, including enhancements in well-being and heightened awareness of individual circumstances.
Conclusions
Given the progressive and debilitating nature of this condition, coupled with the absence of a cure, the adoption of a psychosocial approach can prove beneficial for both ALS/MND patients and their families. However, high-quality RCTs with a large sample size are recommended to examine and confirm the effectiveness.
Similar content being viewed by others
Background
Amyotrophic lateral sclerosis/motor neuron disease (ALS/MND), commonly known as Lou Gehrig's disease, is a progressive and devastating neurodegenerative disorder affecting motor neurons in the brain and spinal cord [1]. This disease results in the gradual degeneration of motor neurons, leading to muscle weakness, atrophy, and eventual paralysis [1]. As the disease advances, patients face increasingly severe consequences, including difficulties with basic tasks such as walking, talking, and swallowing. Respiratory muscles may also become compromised, necessitating ventilatory support. Ultimately, ALS/MND can lead to complete paralysis, making patients entirely dependent on caregivers for their daily needs [2]. The gradual loss of motor function for those with ALS/MND significantly impacts their quality of life. Findings from previous studies underscore the importance of tailored interventions to enhance the overall well-being of individuals with ALS/MND. Such interventions encompass multidisciplinary care, psychological support, and the incorporation of assistive technologies [3, 4]. Addressing the multidimensional aspects of well-being is crucial for providing comprehensive care and support for individuals facing this debilitating neurodegenerative disease.
Family members often become the primary caregivers for ALS/MND patients, assuming the responsibility for their daily care and well-being. The complex and progressive nature of ALS/MND can have a profound impact on both the physical and psychosocial well-being of both patients and their caregivers [5,6,7]. Caregivers may witness their loved ones' gradual deterioration, causing emotional distress. Additionally, the demands of caregiving can lead to physical and mental exhaustion, often resulting in caregiver burnout [8,9,10]. This impact extends to the caregiver's health and well-being, potentially jeopardizing their ability to provide effective care and affecting family dynamics [7]. Caregivers also face immense stress and burden as they take on caregiving responsibilities, navigate the healthcare system, and cope with the emotional toll of witnessing the progression of this disease [11, 12].
Psychosocial intervention refers to any attempt to provide solutions to the challenges individuals may encounter in terms of their psychological well‐being when interacting with any element of the social environment [13]. Psychosocial care includes a spectrum of services and therapies, spanning from educational interventions that systematically provide information to intensive one-on-one counseling sessions [14]. Psychosocial intervention has emerged as a therapeutic strategy designed to address the multifaceted challenges faced by ALS/MND patients and their caregivers [15,16,17]. Over the years, several psychosocial interventions have been developed and implemented to assist ALS/MND patients and their families to cope with the challenges posed by the disease [9, 18, 19]. Psychosocial interventions often combine multiple components to tailor the approach to the specific needs of each individual and their family. However, these studies were conducted with a heterogenous research design and content and used different measurements for testing effect, which make it difficult to obtain a comprehensive picture of psychosocial interventions both for people with ALS/MND and caregivers.
A prior scoping review focused on psychological interventions for people with MND [20] conducted a detailed and comprehensive analysis. However, it had a limited focus, centering on interventions only for patients and interventions primary with a psychological focus. Furthermore, several recent studies have been published since the completion of this scoping review. Therefore, the purpose of this scoping review is to provide a comprehensive overview of the existing literature on psychosocial interventions for people with ALS/MND and their caregivers, while also pinpointing research gaps. This review aims to inform healthcare practitioners, researchers, and policymakers about the current state of psychosocial interventions for ALS/MND, facilitating the development of more targeted and effective support programs for this vulnerable population.
Method
A scoping review is a study used to summarize and evaluate research results prior to conducting a systematic literature review. It serves as a useful way to map the types, data, and key concepts of evidence in a specific topic or study, helping to identify differences between studies and find answers to a wide range of research questions [21]. This scoping review aims to provide a comprehensive overview of current studies on psychosocial interventions conducted for people with ALS/MND and their families. The study was conducted in accordance with the framework developed by Arksey and O'Malley [21], and the results were reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis extension for Scoping Reviews checklist (Additional File 1).
Stage 1: identifying the research question
The research questions were as follows:
-
What psychosocial interventions have been performed and studied for people with ALS/MND and their caregivers?
-
What are the characteristics of the studies (research design, participants, outcome variables) and interventions (contents, methods)?
-
What are the significant effects of the interventions?
-
What are areas or aspects of a topic that have not yet been sufficiently explained?
Stage 2. Identifying relevant studies
The data search encompassed journal papers published since 2000 and utilized four databases: PubMed, Cochrane Central, EMBASE, and CINAHL. Keywords such as (amyotrophic lateral sclerosis OR motor neuron disease OR Lou Gehrig’s disease) AND (psychoeducation OR counseling OR psychotherapy OR behavioral therapy OR cognitive therapy OR education* OR information* OR training* OR teaching OR social support* OR self-care OR self-management) AND (intervention OR trial OR program OR programme OR RCT) were combined using Boolean operators 'AND' and 'OR.' Table 1 and Additional File 2 present the details of the electronic. Furthermore, we examined references from reference lists and manually searched key journals; however, none were included as they duplicated the findings from the earlier electronic database searches.
Stage 3. Study selection
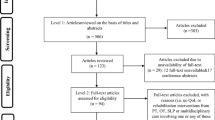
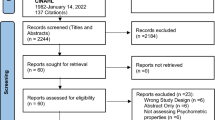
Duplicate articles were removed using the ‘find duplicates’ function in EndNote (Thomson Reuters; Carlsbad, CA, USA), and the selection criteria were applied to identify relevant studies. Articles were included if they met the following criteria: (1) a study of patients with ALS/MND or their families, (2) studies that provided interventions that fit the definition of psychosocial intervention [13, 14], (3) quantitative, qualitative, or mixed methods study design, (4) written in English, and (5) published since 2000. Academic conference posters, abstracts, protocols, commentaries, perspectives, or opinion papers were excluded (Fig. 1).
Stage 4. Charting the data
The following data were extracted and summarized using Microsoft Excel:
-
Publication information: author, year, country
-
Research information: aim of the study, research design (mixed-method research, RCT, quasi-experiment, one-group pre-post study, case study, and qualitative studies), participants for data collection, measurements, key findings.
-
Intervention information: contents (education, counseling, behavioral therapy, social support, or psychotherapy), target for the intervention (patients, caregivers, or both), delivery mode (individual or group-based / in-person or online or other methods), instructive approach (person who provided the intervention), average time per session, frequency, and duration
Results
Study selection
The initial search strategy identified 2,525 studies and after removing 470 duplicated studies, there remained 2,055 studies. After screening titles and abstracts, 2,008 were excluded, resulting in 47 potentially relevant studies. After excluding two duplicated studies, 45 studies were assessed for the eligibility with full-text, and finally 27 studies met the inclusion criteria (Fig. 1).
Study characteristics
A total of 27 studies were analyzed and general characteristics summarized, including authorship, publication year, research country, and research design in Table 2. As visualized in Fig. 2, one study [22] was published in 2010, 11 studies [7, 8, 23,24,25,26,27,28,29] were published between 2011 and 2015, seven studies [5, 6, 9, 10, 19, 30,31,32,33] were published between 2016 and 2020, and eight studies [18, 34,35,36,37,38,39,40] were published after 2021. Most studies were conducted in Italy (n = 9), Australia (n = 5), the Netherlands (n = 4), and USA (n = 3). Denmark, Iran, Japan, Russia, Spain, and Uruguay each published one study. In terms of study design, one group pre-post design [8, 22, 23, 25, 29, 32] and RCT [7, 9, 19, 24, 35, 38] were the most common with six studies, followed by five qualitative studies [6, 10, 18, 30, 31] and four quasi-experimental studies [5, 28, 34, 39], and three each for mixed methods [33, 36, 40] and case studies [26, 27, 37].
Participant characteristics
The range of sample sizes used in data collection varied widely from one [26, 27, 37] to a maximum of 148 [9]. Most of the studies involved less than 50 participants, two studies [5, 38] 50–100 participants, one study [9] had over 100 participants. Eleven studies [5, 19, 22, 24,25,26,27, 34, 35, 37, 39] collected data from people with ALS/MND, six studies [8, 30,31,32,33, 40] from family members, and ten studies [6, 7, 9, 10, 18, 23, 28, 29, 36, 38] from both persons with ALS/MND and also family members.
Intervention characteristics
Content, targets, delivery mode, instructive approach, and frequencies of psychosocial interventions of the reviewed studies are summarized in Table 2. In terms of content, a diverse range was observed (Fig. 3). When an intervention included multiple components of a content category, each was counted individually. When interventions [8, 9, 25, 31] were published in two separate papers, we counted each intervention only once. Among the various interventions, education-related interventions were the most prevalent, totaling 9. This was followed by behavior therapy, counseling, and social support interventions, each comprising 7, and psychotherapy interventions, totaling 6. Education-related interventions included programs such as providing information regarding disease [39], skill training [32], teaching coping skills and problem solving [33], and nutrition education and counseling [34]. Behavior therapy interventions encompassed programs like expressive disclosure exercise [24] and music therapy [19, 22, 36], while counseling interventions included dignity therapy [8, 23] and supportive counseling [39]. Social support interventions included programs such as a mutual support group program [6, 30], and psychotherapy interventions featured treatment such as hypnosis treatment [28, 29], eye movement desensitization and reprocessing [37], and meditation [10].
The number of interventions provided to people with ALS/MND was 12 [19, 22, 24,25,26,27,28,29, 34, 35, 37, 39], while provided to family members was five [9, 30, 32, 33, 40], and including both persons with ALS/MND and family members was eight [5,6,7,8, 10, 18, 23, 38]. Eighteen interventions were provided individually and remaining interventions [6, 10, 18, 30, 32, 33, 40] were administered in a group setting. Most interventions were conducted in face-to-face settings. The remaining interventions included two delivered online [38, 40], one employing a blended approach (combining face-to-face contact and online modules) [9], and one utilizing a webapp-based chatbot [34]. Health professionals, such as psychologists, therapists, and nurses, predominantly led the majority of interventions. However, a subset of interventions was facilitated through alternative means, including email [38] or chatbots [34]. The duration of interventions per session varied, ranging from less than 10 min [38] to half a day [6]. The total intervention periods also exhibited diversity, spanning from one week [24] to nine months [18].
Intervention outcomes
In the majority of the studies, the outcomes related to feasibility aspects, including retention, adherence, and tolerance, largely indicated the feasibility of the interventions. Dropout rates were various, but several studies were high at up to 48% [38], those dropouts were primarily attributable to factors such as the deterioration of patients' health, mobility limitations, and the time constraints faced by family members [9, 31]. The majority of the studies reported favorable acceptability results, such as high levels of participant satisfaction and perceived benefits. Nevertheless, a few studies identified specific limitations arising from challenges such as patients' communication difficulties, mobility issues, participants' prior knowledge levels, and the heterogeneity in disease severity [18, 31].
Table 3 presents the results of studies that examined intervention effectiveness. Among these, six studies employed a single-group pre-post design without a control group, while in the remaining studies, the control groups received a routine rehabilitation program [35], routine monitoring [40], drug treatment [5] or usual care only [7], or wait-list control [9, 38]. Various concepts were used as outcome variables to evaluate study effectiveness. In terms of physical aspects, these included functional status, fatigue, anthropometric measurements, pain, lung function, blood test results, etc. For psychosocial aspects, the variables included depression and anxiety, hope, resilience, health-related quality of life, and overall quality of life. Spiritual variables such as dignity and spiritual well-being were also used as outcome variables. The most frequently measured variables for the people with ALS/MND were quality of life (n = 11), followed by depression and anxiety (n = 8), and functional status (n = 5). For family members, the most frequently measured variables included depression and anxiety (n = 7), caregiver burden (n = 6), and quality of life (n = 4).
In terms of experimental study effectiveness, more than half (n = 13) of the studies demonstrated one or more statistically significant effects. However, in seven studies, the intervention did not show statistically significant effects [8, 9, 22, 23, 25, 33, 40]. When focusing on RCT studies, Averill et al. [24] found that the expressive disclosure exercise intervention resulted in higher well-being for the intervention group compared to the control group at three-months post-intervention, but not at six months. In De Wit's study [9], Acceptance and Commitment Therapy did not reduce distress in patients and caregivers, but it appeared to empower caregivers by enhancing their sense of control in challenging situations. Fateh et al. [35] reported that an energy conservative program led to short- and mid-term improvements in fatigue and occupational performance, but did not enhance quality of life. Pagnini et al. [38] observed that participants who engaged in the online mindfulness intervention experienced improvements in their quality of life and psychological well-being compared to the control group. Raglio et al. [19] found that the active music therapy group showed significant improvements in global scores on the McGill Quality of Life questionnaire, while van Groenestijin et al. [7] identified a significant intervention effect on the mental quality of life of patients and caregivers as well as caregiver burden.
In qualitative research, the majority of studies analyzed needs of people with ALS/MND and their families during the disease course [18, 30], explored the positive and negative aspects of interventions [18, 30], and examined a range of effects in various domains. These effects encompassed improvements in mental and physical well-being [10], heightened positive emotions, and increased self-assurance in coping strategies [31], along with greater awareness of their individual circumstances [6, 30, 31]. Notably, group interventions frequently highlighted peer interactions, resulting in the provision of emotional support [6, 18, 30, 33].
Discussion
The objectives of this study were to conduct a scoping review and present a comprehensive overview of psychosocial interventions designed for individuals and families affected by ALS/MND, while also pinpointing research gaps. This investigation scrutinized 25 psychosocial interventions from a total of 27 articles, aiming to discern the attributes and impacts of these interventions. To the best of our understanding, this scoping review is the inaugural attempt to comprehensively analyze psychosocial interventions offered to both people with ALS/MND and their families.
All of these studies were published after 2010 and no study before 2009, and the number of studies have been gradually increasing over time. However, the majority of the research is conducted in European and American countries, which may limit the generalization of these findings to patients and families in other regions. Due to cultural, social, and healthcare system differences, intervention effects may vary, highlighting the need for research in diverse regions and various cultural contexts.
In the categorization of psychosocial interventions, educational interventions were the most frequently implemented, which aligns with previous research among cancer survivors [41]. Particularly, ALS/MND patients and their families face various challenges due to the rarity of the disease, and providing information and education could enhance patient's self-care abilities and improve family caregiving skills [42]. While the interventions primarily targeted patients, there were also several interventions targeting both patients and families, as well as interventions focusing solely on families. Furthermore, some studies provided interventions to patients or families while simultaneously evaluating research outcomes from both patients and families. These findings are based on previous research indicating that ALS/MND is a condition where family support is essential, and family knowledge and mental health can directly impact patient health outcomes [2]. As patient and family health outcomes are interdependent, recent research in other chronic conditions [43, 44] has increasingly focused on interventions targeting both patients and families as a single unit, also known as a dyadic. Therefore, dyadic interventions for ALS/MND should be developed and implemented in further studies.
Most interventions were conducted in a face-to-face format, with limited research regarding online or smartphone-based interventions. After the COVID-19 pandemic, online interventions have become increasingly prevalent. Online interventions offer users the flexibility to engage in programs at their preferred times and locations, potentially reducing time and spatial constraints and increasing satisfaction [31]. However, some participants preferred 'hands-on' direct support and highlight technical issues associated with online-based interventions [31, 32]. Therefore, it is important to consider demographic characteristics and intervention content when choosing intervention mode. Moreover, participants in group interventions reported benefits such as sharing experiences and receiving emotional support beyond knowledge enhancement and improved mental health. Consequently, depending on the intervention content, group interventions may be considered as a method to enhance participant satisfaction and cost-effectiveness.
The heterogeneity of methodologies and characteristics among the analyzed studies posed challenges for direct comparisons, making it difficult to assess the overall effectiveness of psychosocial interventions. Most studies reported positive findings in terms of the feasibility and acceptability of interventions, and the qualitative interview mostly reported benefits of the interventions. While many studies presented positive effects of interventions quantitatively, some did not report statistically significant effects. However, one reason for the inconsistent results is the limited sample sizes. Most studies were conducted with less than 50 participants and only a few interventions targeted over 100 participants. Furthermore, high dropout rate could result in insufficient power to statistically test study hypothesis. Studies with long term follow ups (about 6 months after intervention completed) or administered online or at a distance, had dropout rates that were relatively high. Given that most studies were conducted with small sample sizes, even if there were actual effects, statistically significant results might not have been obtained. Furthermore, most studies reported only short-term effects, highlighting the importance of investigating the long-term effects of interventions.
Research gaps
We identified several research gaps among the studies. The research designs of the included studies had some limitations, including small sample sizes, high dropout rates, non-randomized controlled trials, issues with measurement tools, and were limited to short-term outcomes. ALS/MND is not only a rare disease, but also one that affects various aspects of the body and progresses rapidly, making participant recruitment and reservation challenging. However, in order to analyze research results more rigorously, there is a need to improve research designs in terms of sample size and study design. While most studies employed validated measurements, there are some concerns. For instance, Hospital Anxiety and Depression Scale is widely used in various studies, however, its validity may be compromised when applied to ALS/MND patients, who have specific disease-related characteristics [45], or non-patient family members. This potentially could lead to a failure to detect the effects of interventions. Furthermore, the promising outcomes from most qualitative studies, including improvements in well-being and increased awareness of individual circumstances, suggest that the integration of mixed methods could enhance our understanding of interventions for ALS/MND.
Secondly, most interventions primarily targeted patients in at early or mid-stages of the disease. For families, the majority of studies focused on spouses. To account for demographic diversity and disease stage, it is essential to consider diversifying the target participant groups. Moreover, most quantitative studies concentrated on evaluating the effectiveness of interventions with respect to depression, anxiety, and quality of life. Consequently, future research endeavors should strive to comprehensively investigate a broader spectrum of outcomes.
This study had some limitations. Firstly, due to the inconsistent research designs, we could not perform a meta-analysis, making it challenging to assess the effects of interventions definitively. Secondly, our inclusion criteria were limited to studies published in English, potentially reducing the generalizability of the findings. Additionally, by focusing solely on original articles and case studies, we omitted gray literature and ongoing research, thus our analysis did not encompass all interventions for ALS/MND patients and their families.
Conclusions
In conclusion, this review highlights the availability of a range of psychosocial programs tailored for people with ALS/MND and their families. These programs exhibit promising potential as supportive interventions throughout the ALS/MND care journey. While the definitive effectiveness of psychosocial interventions remains somewhat unclear in this study, a significant body of research reports favorable outcomes. Furthermore, the majority of these interventions are deemed feasible and applicable. These findings can serve as valuable guidance for clinicians, professionals, and policymakers involved in crafting and implementing interventions for individuals with ALS/MND and their families. Given the progressive and debilitating nature of this condition, coupled with the absence of a cure, the adoption of a psychosocial approach can prove beneficial for both ALS/MND patients and their families. Providing thorough education and counseling at ALS/MND clinics, as well as fostering connections with other patients' families, can positively impact the health outcomes of both patients and their families. Additionally, while there is limited research in this review, various behavioral therapies such as expressive therapy, music therapy, and psychological treatments including hypnotherapy and mindfulness are showing promising results. Therefore, further research is needed, but these interventions are worth actively considering for implementation in ALS/MND clinics.
As mentioned earlier in this review, it is challenging to draw definitive conclusions about the effectiveness of psychosocial interventions applied to ALS/MND patients and their families. Specifically, high-quality RCTs with a large sample size are recommended to examine and confirm intervention effectiveness. Due to the observed high dropout rate in this study, it is necessary to increase the sample size by recruiting participants from multiple sites. Simultaneously, actively utilizing human resources is essential when implementing online interventions to minimize research participant attrition. The integration of mixed methods research may offer valuable insights into the multifaceted nature of intervention strategies. Additionally, there is a pressing need to diversify intervention delivery methods, target populations, and content to better cater to the unique needs of individuals affected by ALS/MND.
Availability of data and materials
All the data are available from the corresponding author up on a reasonable request.
Abbreviations
- ALS/MND:
-
Amyotrophic lateral sclerosis/motor neuron disease
- CINAHL:
-
Cumulative Index of Nursing and Allied Health
- PRISMA-ScR:
-
Preferred Reporting Items for Systematic Reviews and Meta-analyses
- RCT:
-
Randomized controlled trial
- USA:
-
United States of America
References
Brown RH, Al-Chalabi A. Amyotrophic Lateral Sclerosis. N Engl J Med. 2017;377(2):162–72.
Oh J, Kim JA. Supportive care needs of patients with amyotrophic lateral sclerosis/motor neuron disease and their caregivers: A scoping review. J Clin Nurs. 2017;26(23–24):4129–52.
de Almeida FEO, do Carmo Santana AK, de Carvalho FO. Multidisciplinary care in Amyotrophic Lateral Sclerosis: a systematic review and meta-analysis. Neurol Sci. 2021;42(3):911–23.
Rosa Silva JP, et al. Quality of life and functional independence in amyotrophic lateral sclerosis: A systematic review. Neurosci Biobehav Rev. 2020;111:1–11.
Díaz JL, et al. Effect of a short-term psychological intervention on the anxiety and depression of amyotrophic lateral sclerosis patients. J Health Psychol. 2016;21(7):1426–35.
Madsen LS, Jeppesen J, Handberg C, “Understanding my ALS.” Experiences and reflections of persons with amyotrophic lateral sclerosis and relatives on participation in peer group rehabilitation. Disabil Rehabil. 2019;41(12):1410–8.
van Groenestijn AC, et al. Cognitive behavioural therapy and quality of life in psychologically distressed patients with amyotrophic lateral sclerosis and their caregivers: Results of a prematurely stopped randomized controlled trial. Amyotroph Lateral Scler Frontotemporal Degener. 2015;16(5–6):309–15.
Bentley B, et al. Feasibility, acceptability and potential effectiveness of dignity therapy for family carers of people with motor neurone disease. BMC Palliative Care. 2014;13(1):12.
De Wit J, et al. Blended psychosocial support for partners of patients with ALS and PMA: results of a randomized controlled trial. Amyotroph Lateral Scler Frontotemporal Degener. 2020;21(5–6):344–54.
Marconi A, et al. The experience of meditation for people with amyotrophic lateral sclerosis and their caregivers – a qualitative analysis. Psychol Health Med. 2016;21(6):762–8.
Caga J, Kiernan MC, Piguet O. A Systematic Review of Caregiver Coping Strategies in Amyotrophic Lateral Sclerosis and Frontotemporal Dementia. J Geriatr Psychiatry Neurol. 2022;35(6):763–77.
Oh J, Kim JA. Factor analysis of the Zarit Burden Interview in family caregivers of patients with amyotrophic lateral sclerosis. Amyotroph Lateral Scler Frontotemporal Degener. 2018;19(1–2):50–6.
Semple C, et al. Psychosocial interventions for patients with head and neck cancer. Cochrane Database Syst Rev. 2013;7:Cd009441.
Teo I, Krishnan A, Lee GL. Psychosocial interventions for advanced cancer patients: A systematic review. Psychooncology. 2019;28(7):1394–407.
Cheng Q, et al. Effectiveness of psychoeducational interventions among caregivers of patients with cancer: A systematic review and meta-analysis. Int J Nurs Stud. 2022;127:104162.
Setyowibowo H, et al. Psychoeducation for breast cancer: A systematic review and meta-analysis. Breast. 2022;62:36–51.
Yu Y, et al. The Experiences of Informal Caregivers of People With Dementia in Web-Based Psychoeducation Programs: Systematic Review and Metasynthesis. JMIR Aging. 2023;6:e47152.
Bilenchi VA, et al. Psychoeducational groups for people with Amyotrophic Lateral Sclerosis and their caregiver: a qualitative study. Neurol Sci. 2022;43(7):4239–55.
Raglio A, et al. Active music therapy approach in amyotrophic lateral sclerosis: a randomized-controlled trial. Int J Rehabil Res. 2016;39(4):365–7.
Zarotti N, et al. Psychological interventions for people with motor neuron disease: a scoping review. Amyotroph Lateral Scler Frontotemporal Degener. 2021;22(1–2):1–11.
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32.
Horne-Thompson A, Bolger K. An investigation comparing the effectiveness of a live music therapy session and recorded music in reducing anxiety for patients with amyotrophic lateral sclerosis/motor neurone disease. Aust J Music Ther. 2010;21:23–38.
Aoun SM, Chochinov HM, Kristjanson LJ. Dignity therapy for people with motor neuron disease and their family caregivers: a feasibility study. J Palliat Med. 2015;18(1):31–7.
Averill AJ, Kasarskis EJ, Segerstrom SC. Expressive disclosure to improve well-being in patients with amyotrophic lateral sclerosis: a randomised, controlled trial. Psychol Health. 2013;28(6):701–13.
Bentley B, et al. Feasibility, acceptability, and potential effectiveness of dignity therapy for people with motor neurone disease. PLoS One. 2014;9(5):e96888.
García Pérez AI, Dapueto JJ. Case report of a computer-assisted psychotherapy of a patient with ALS. Int J Psychiatry Med. 2014;48(3):229–33.
Jikumaru K. Psychotherapeutic nursing for a patient with amyotrophic lateral sclerosis. J Nara Med Assoc. 2011;62(1–2):21–33.
Kleinbub JR, et al. Hypnosis-based psychodynamic treatment in ALS: a longitudinal study on patients and their caregivers. Front Psychol. 2015;6:822.
Palmieri A, et al. Efficacy of hypnosis-based treatment in amyotrophic lateral sclerosis: a pilot study. Front Psychol. 2012;3:465.
Cipolletta S, et al. Mutual support groups for family caregivers of people with amyotrophic lateral sclerosis in Italy: A pilot study. Health Soc Care Community. 2018;26(4):556–63.
de Wit J, et al. User perspectives on a psychosocial blended support program for partners of patients with amyotrophic lateral sclerosis and progressive muscular atrophy: a qualitative study. BMC Psychol. 2019;7(1):35.
Kavanaugh MS, et al. Skill, confidence and support: conceptual elements of a child/youth caregiver training program in amyotrophic lateral sclerosis – the YCare protocol. Neurodegener Dis Manag. 2020;10(4):231–41.
Ugalde A, et al. A self-care, problem-solving and mindfulness intervention for informal caregivers of people with motor neurone disease: A pilot study. Palliat Med. 2018;32(4):726–32.
De Marchi F, et al. A Telehealth Intervention for Nutritional Counseling in Amyotrophic Lateral Sclerosis Patients. J Clin Med. 2022;11(15):4286.
Fateh HR, et al. The effect of energy conservation strategies on fatigue, function, and quality of life in adults with motor neuron disease: randomized controlled trial. Curr J Neurol. 2022;21(2):83–90.
Kolomeytseva ATA, et al. Home-Based Music Therapy to Support Bulbar and Respiratory Functions of Persons with Early and Mid-Stage Amyotrophic Lateral Sclerosis—Protocol and Results from a Feasibility Study. Brain Sci. 2022;12(4):494.
Oudman E, Baert JCM. Eye movement desensitization and reprocessing (EMDR) and mediative behavioral therapy for the treatment of suffocation related post-traumatic stress disorder (PTSD) in amyotrophic lateral sclerosis (ALS): A case report. Palliat Support Care. 2022;21(1):1–3.
Pagnini F, et al. An online non-meditative mindfulness intervention for people with ALS and their caregivers: a randomized controlled trial. Amyotroph Lateral Scler Frontotemporal Degener. 2022;23(1–2):116–27.
Palmieri A, et al. Empathy-based supportive treatment in amyotrophic lateral sclerosis: A pragmatic study. Am J Clin Hypn. 2021;63(3):202–16.
Sharbafshaaer M, et al. Psychological Support for Family Caregivers of Patients With Amyotrophic Lateral Sclerosis at the Time of the Coronavirus Disease 2019 Pandemic: A Pilot Study Using a Telemedicine Approach. Front Psychiat. 2022;13(13):904841.
Park JH, Bae SH. Effects of Psychoeducational Intervention for Cancer Survivors: A Systematic Review and Meta-Analysis. J Korean Acad Nurs. 2017;47(2):143–63.
Chu HS, Oh J. Information Needs and Preferences of Family Caregivers of Patients With Amyotrophic Lateral Sclerosis. J Neurosci Nurs. 2020;52(5):207–13.
Ghosh M, Dunham M, O’Connell B. Systematic review of dyadic psychoeducational programs for persons with dementia and their family caregivers. J Clin Nurs. 2023;32(15–16):4228–48.
Mou H, Wong MS, Chien WTP. Effectiveness of dyadic psychoeducational intervention for stroke survivors and family caregivers on functional and psychosocial health: A systematic review and meta-analysis. Int J Nurs Stud. 2021;120:103969.
Carvalho TL, et al. Depression and anxiety in individuals with amyotrophic lateral sclerosis: a systematic review. Trends Psychiatry Psychother. 2016;38(1):1–5.
Acknowledgements
None.
Funding
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIT) (No. 2022R1F1A1064038).
Author information
Authors and Affiliations
Contributions
Jo, JA, KP, and YP conceptualized the research question and the design of the study. JO and JA conducted the literature searching and data extraction, Jo, JA, KP, and YP conducted data analysis. JO and YP drafted the first version of the manuscript, JA and KP contributed to the completion of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) Checklist.
Additional file 2.
Documenting the search.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Oh, J., An, J., Park, K. et al. Psychosocial interventions for people with amyotrophic lateral sclerosis and motor neuron disease and their caregivers: a scoping review. BMC Nurs 23, 75 (2024). https://doi.org/10.1186/s12912-024-01721-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12912-024-01721-6