Abstract
Background
In 2008, the Institut Català de la Salut (ICS, Catalan Health Institute) implemented a prescription decision support system in its electronic clinical workstation (ECW), which automatically generates online alerts for general practitioners when a possible medication-related problem (MRP) is detected. This tool is known as PREFASEG, and at the time of beginning a new treatment, it automatically assesses the suitability of the treatment for the individual patient. This analysis is based on ongoing treatments, demographic characteristics, existing pathologies, and patient biochemical variables. As a result of the assessment, therapeutic recommendations are provided. The objective of this study is to present the PREFASEG tool, analyse the main alerts that it generates, and determine the degree of alert acceptance.
Methods
A cross-sectional descriptive study was carried out to analyse the generation of MRP-related alerts detected by PREFASEG during 2016, 2017, and 2018 in primary care (PC) in Catalonia. The number of MRP alerts generated, the drugs involved, and the acceptance/rejection of the alerts were analysed. An alert was considered "accepted" when the medication that generated the alert was not prescribed, thereby following the recommendation given by the tool. The MRP alerts studied were therapeutic duplications, safety alerts issued by the Spanish Medicines Agency, and drugs not recommended for use in geriatrics. The prescriptions issued by 6411 ICS PC physicians who use the ECW and provide their services to 5.8 million Catalans through 288 PC teams were analysed.
Results
During the 3 years examined, 67.2 million new prescriptions were analysed, for which PREFASEG generated 4,379,866 alerts (1 for every 15 new treatments). A total of 1,222,159 alerts (28%) were accepted. Pharmacological interactions and therapeutic duplications were the most detected alerts, representing 40 and 30% of the total alerts, respectively. The main pharmacological groups involved in the safety alerts were nonsteroidal anti-inflammatory drugs and renin-angiotensin system inhibitors.
Conclusions
During the period analysed, 28% of the prescriptions wherein a toxicity-related PREFASEG alert was generated led to treatment modification, thereby helping to prevent the generation of potential safety MRPs. However, the tool should be further improved to increase alert acceptance and thereby improve patient safety.
Similar content being viewed by others
Background
According to a European Commission report, 3–10% of hospital admissions between 2012 and 2014 were caused by adverse drug events (ADEs), totalling 2.5–8.4 million cases annually. In addition, approximately 2.1–6.5% of hospitalised patients experienced an ADE, corresponding to 1.8–5.5 million annually [1]. Thus, since the late 1990s, patient safety has become a priority of health systems [2, 3], and several initiatives have identified the need for a new culture of safety in the health and policy environment [4,5,6]. To achieve this, and according to the definition of clinical safety, it is essential to define actions to avoid, prevent, and improve adverse effects or injuries from healthcare processes where possible, since it should be acknowledged that some adverse events are inherent in treatment, and cannot always be avoided or minimised.
In this context, the 1999 technical report ‘To err is human’ by the Institute of Medicine (OIM) highlighted the need to develop new information and communications technologies to reduce medical errors [2], and, beyond this, prescriptions which could increase the risk of developing adverse effects. Subsequent reports later affirmed that the electronic record of healthcare activity that is typical of an electronic health record (EHR), together with the integration of clinical decision support systems (CDSSs) into these EHRs, should contribute to guaranteeing quality in the healthcare system [7, 8] by helping to reduce preventable adverse effects.
In the scientific literature we find different definitions of a CDSS [9, 10]. According to Kawamoto et al. [11], a CDSS can be considered any electronic system designed to help clinical decision making, which takes into account the characteristics of the patient to generate a specific evaluation and provide a recommendation to be evaluated by the practicing clinician. The design and functionalities of these CDSSs can be very varied. Some authors consider that CDSSs aimed at the initial prescription phase may have the greatest impact on improving patient safety [12], while others discuss the fact that integration of a CDSS into the HER renders it possible to provide patient histories along with interactive signals that alert professionals to situations of risk for the patient [13]. As a result, the prescription process can be improved and the clinical safety of patients enhanced [12, 14, 15].
CDSSs have been found to bring multiple benefits to patient care [16,17,18,19], wherein it has been reported that they contribute to improving the dosage and selection of drugs, while also encouraging patients to take part in preventive activities, improving test results, decreasing morbidity, and improving the quality of care [20]. In contrast, the main risk of CDSSs is the alert fatigue experienced by physicians who are faced with a multitude of prompts and reminders on-screen, which can lead to important alerts being ignored [21, 22].
The Catalan Health Institute (ICS) is a public entity that provides health services to 80% of the population of Catalonia. In 2008, in line with promoting the clinical safety of the patient, it designed and integrated a CDSS into its primary care electronic clinical workstation (ECW) that made it possible to detect certain medication-related problems (MRPs) online. This CDSS, which is known as PREFASEG (PREscripción FArmacéutica SEGura, i.e., safe pharmaceutical prescription), is a computer tool that acts interactively to alert clinicians to any potential drug use-related problems during the process of deciding the most appropriate treatment for their patient.
To understand the means by which PREFASEG functions, we consider the prescription of a new drug to a specific patient. At the point at which the prescription is requested by the clinician, PREFASEG is activated and performs an assessment of the prescription to verify that it is safe for the patient, and that it does not pose a potential risk to their health. This evaluation is carried out based on the different MRPs detected by the tool, which include: (1) Drug interactions; (2) Therapeutic duplications; (3) Drugs advised against for use in geriatrics; (4) Contraindications with a safety alert published by the Spanish Agency for Medicines and Health Products (AEMPS, Agencia Española del Medicamentos y Productos Sanitarios); (5) Contraindications due to health problems and/or clinical variables; (6) Drugs that are known to be teratogens during pregnancy; (7) Anticholinergic drug combinations; (8) Patient history of hypersensitivity or suspected hypersensitivity reactions (suspected, not confirmed); and (9) Adverse drug events. To carry out this evaluation, a number of factors are taken into account, such as any active prescriptions that the patient already has on their record, other medical diagnoses or active health problems, the presence of any clinical variables with altered values, and the age and/or sex of the patient. In the event of a safety alert being generated following the above evaluation, the corresponding warnings are shown to the clinician (e.g., the risk to the patient and any therapeutic alternatives) so that he can decide whether to continue with the prescription or change the medication. These safety alerts are displayed in a simple manner on a single screen to permit their rapid consultation and understanding, as shown in Fig. 1, which presents an example relating to the prescription of a product that is not recommended for patients over 75 years of age. The information displayed includes the severity icon (two degrees, moderate or severe), the drug or active ingredient causing the alert, the cause of conflict (i.e., medication or active ingredient conflict, patient age, or pre-existing health problem), the risk to the patient, and any therapeutic alternatives. Each MRP alert is classified as either high (red indicator) or medium–low (orange indicator) clinical relevance, according to previously described recommendations [23].
It is also possible that more than one alert is generated by the tool, and in such a case, the clinician is informed of all warnings associated with the different potential safety issues, as can be seen in Fig. 2.
Each alert generated by PREFASEG is recorded as "audit data” along with the information related to whether it has been accepted or whether prescription of the product was continued. The evaluation of these data allows us to determine if certain types of alerts are accepted to a greater degree than others, thereby improving the clinical content definitions to adapt the tool to the healthcare reality. PREFASEG consists of a calculation core in the Oracle PL/SQL, in which the calculations that access the tables of clinical contents have been optimised, and in which there is a minimum visual interface for the communication of safety alerts. This interface was developed using Developer Forms, which is the same technology employed to produce the ECW. As a result, the look and feel of the alert screens are comparable to those of the original ECW, and so maximum integration is achieved.
The contents of the MRP alerts are defined and maintained as described by a multidisciplinary group of expert professionals from the ICS (i.e., primary care (PC) physicians, pharmacists, and clinical pharmacologists) according to previous literature [9, 24]. The MRP alerts are reviewed and updated each year according to the available scientific evidence, and as a result, the clinical content undergoes some changes from 1 year to the next. For example, references to the more current STOPP/START and Beers criteria were included in updates for drugs advised against for use in geriatrics. Importantly, the clinical content can be revised at any time, and are updated from a specific maintenance platform known as 'Know How.'
The purpose of this study is therefore to describe the principal characteristics of the PREFASEG tool, the main safety alerts generated by PREFASEG in the Catalan PC system, the degree of acceptance of these alerts by physicians, and the main pharmacological groups implicated in the alerts. Furthermore, three of the most frequent alerts are also described in greater detail.
Methods
A descriptive, cross-sectional study was designed, which began in January 2016 and continued until December 2018. This study was developed within the scope of the PC system of the ICS, which is the main entity that provides health services in Catalonia, and which covers a population of 5.8 million inhabitants of the different Catalan territories through a network of 288 PC teams and 8 hospitals. The ICS is a public company with a total of 42,374 professionals who provide services to 80% of the population of Catalonia.
Study sample
The sample studied consisted of all prescriptions issued by the 6411 ICS PC physicians who used the EHR during the study period.
Development of PREFASEG
In general terms, to provide the PREFASEG with clinical and pharmacological content, the following methodology was followed during its development:
-
1.
Bibliographic search. Initially a bibliographic search was carried out in the PubMed database for the different MRPs addressed by PREFASEG, wherein national and international articles that were considered to be the most relevant and best adapted to our healthcare environment were reviewed. The safety alerts included in the ICS Clinical Practice Guidelines [25] were also considered.
-
2.
Consensus with a group of experts. Following a literature review, the pharmacological groups to be included were selected and the messages to be presented to the prescribing physicians were defined. Each MRP alert was classified as high (red) or medium-low (orange) clinical relevance, as mentioned above [23]. The red alerts reflected situations of absolute contraindications, while the orange alerts were considered precautionary.
-
3.
Adaptation of the clinical content to the table formats necessary for the PREFASEG computer program. The clinical content was transferred into a computer-readable language from various configuration tables presented in Excel, and for this purpose, it was necessary to code the active ingredients according to the Anatomical Therapeutic Chemical (ATC) classification. Similarly, the various health issues were coded according to the International Classification of Diseases ICD-10 system. To produce the clinical contents, ATC groups or groups of health problems were built. Each alert type was then defined and configured using a combination of various attributes, as outlined in Table 1.
Table 1 Combinable attributes in the configuration of each PREFASEG notice
Variables and indicators
The main variable of the study was the number of MRP alerts generated by PREFASEG. Another of the variables studied was the number of accepted alerts. An alert was considered "accepted" when the medicine that generated the safety alert was not prescribed.
Some PREFASEG alerts are associated with recommendations for clinical follow-ups or dose reductions. Therefore, following these recommendations does not entail the withdrawal of the treatment that has generated the alert. Consequently, these alerts are not considered “accepted” alerts.
Description of the MRPs included in PREFASEG
The various MRPs that are defined in the PREFASEG system were outlined previously in the introduction (see also Table 1). Further details regarding these MRPs can be found in Additional file 1.
The global MRP alerts generated and accepted by PREFASEG were analysed. More specifically, the safety MRPs related to therapeutic duplications, medicines not recommended for use in geriatrics, and safety alerts from the AEMPS were examined in greater detail.
The contents of the MRP alerts were defined and maintained as described by a multidisciplinary group of expert professionals from the ICS according to previous literature [9, 24]. The MRP alerts were reviewed and updated each year according to the available scientific evidence, and as a result, the clinical content underwent some changes from 1 year to the next. Each MRP alert was classified as either high or medium–low clinical relevance, as described above [23].
The MRP alerts corresponding to “therapeutic duplications” detected patients with a non-beneficial prescription of two or more medicines based on the same active ingredient (alone or in combination) and/or with the same pharmacological action (further details can be found in Additional file 1). Duplications of more than 60 different pharmacological groups commonly used in PC were addressed. In each group, “clinically relevant duplications” and “dose adjustments duplications” (combinations sought with a therapeutic objective) were clearly differentiated. Depending on their relevance, alerts marked with different colours were generated, as indicated above.
During the study period, MRP alerts associated with “AEMPS safety alerts” reported contraindications for the “Triple Whammy,” COXIBS, diclofenac, aceclofenac, cilostazol, ivabradine, agomelatine, escitalopram, citalopram, trimetazidine, raloxifene/bazedoxifene, strontium ranelate, aliskiren, and canagliflozin (further details can be found in Additional file 1). These alerts were considered to be highly relevant because they were absolute contraindications, in addition to having a specific safety alert originating from the AEMPS, and so they were indicated in red.
The MRP alerts corresponding to “medicines not recommended for use in geriatrics” detected patients ≥ 75 years of age who had been prescribed inappropriate medication that posed a more unfavourable risk–benefit profile due to their age (see Additional file 1). The selection of medications considered inappropriate for this age group was based on the Beers (2015) [26], EU-PIM (European Consensus) [27], STOPP/START [28], and PRISCUS [29] criteria (further details can be found in Additional file 1). These alerts were displayed on-screen as alerts of medium–low relevance (i.e., orange colour) since the literature indicates that they should be administered with caution.
Data collection and analysis
The analysed data were obtained from the ECW that stores the active prescriptions of all patients; however, data from specific patients were not analysed. The study was restricted to drugs prescribed and financed by the National Health System for use in the PC setting.
In January 2016, information began to be extracted regarding the different types of MRP alerts generated by PREFASEG, which were internally identified in the patient's EHR. Thus, the number of advisories for each MRP generated, the medicines involved in each alert, and the acceptance or rejection of the alert were recorded. Each month, the alerts generated by the system and accepted by the clinicians were accumulated in a computer repository. The data set was analysed annually through computerised extractions from the ECW databases. The alert traceability was stored and organised on computer servers according to the organisational structure of the ICS, i.e., with differentiation between the health territories in which the institution is organised.
A descriptive analysis was carried out of the generated and accepted alerts of the different MRPs from January 2016 to December 2018. Initially, the analysis was carried out on an annual basis because the clinical contents changed annually. These content changes occurred for a number of reasons, including the inclusion of new marketed drugs, modifications in the definitions of existing MRP alerts to render them more specific, and the inclusion of additional pharmacological groups. Despite these content changes, the data were accumulated, and a global analysis of the alerts generated and accepted during the 3-year study period was also carried out.
Results
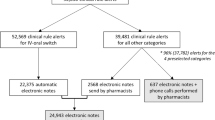
General analysis of the MRP alerts generated by PREFASEG
During the period of study, 22.5, 22.3, and 22.4 million new prescriptions were issued in the ICS PC system in 2016, 2017, and 2018, respectively, while the number of alerts generated by PREFASEG were 1.17 million in 2016, 1.43 million in 2017, and 1.77 million in 2018. Thus, the percentage of MRP alerts generated by the tool with respect to the number of new prescriptions issued were 5% in 2016, 6% in 2017, and 8% in 2018.
The global acceptance of these alerts varied throughout the 3 years studied, ranging from 31% (362,732) in 2016 to 26% (457,976) in 2018 (see Table 2), which corresponds to 69–74% of the MRP alerts generated by PREFASEG during the years of study. Analysis of the accumulated number of alerts issued over the 3-year study period (i.e., 4.38 million alerts) gave a 28% degree of acceptance (i.e., 1.22 million accepted alerts).
When analysing the alerts generated from the different MRPs throughout the study period (2016–2018), it was observed that those related to drug interactions, therapeutic duplications, and drugs advised against for use in geriatrics were the most common. Taking the data collected over the 3 years, 39% (1,691,886) of the 4,379,866 million alerts generated were for drug interactions, 33% (1,436,721) were for therapeutic duplications, and 10% (441,920) were for the use of drugs advised against in geriatrics. Thus, these three types of MRP alerts accounted for more than three-quarters of the PREFASEG alerts (3,570,527; 82%). Of these, 27% were accepted and 73% were ignored. In addition, of the 34,063 alerts related to teratogens in pregnancy, 22,324 (66%) were ignored.
The types of alerts with the highest percentage of acceptance were those related to a history of suspected (unconfirmed) drug hypersensitivity, with 35% (89,279) of these alerts being accepted over the 3 years studied. Detailed analyses indicated that four non-steroidal anti-inflammatory drugs (NSAIDs, i.e., ibuprofen, naproxen, desketoprofen, and diclofenac) represented 45% (113,936) of the suspected hypersensitivity reactions reported by PREFASEG, with ibuprofen generating the highest number of alerts (61,026). In addition, during the study period, the number of suspected hypersensitivity reaction alerts for β-lactam antibiotics alone or in combination fell into the second largest group, with 39,622 alerts and an acceptance level of 63% (25,153).
In contrast, the alerts related to potential teratogenic compounds during pregnancy had a lower degree of acceptance (i.e., 34%, 11,739). It was observed that the active ingredients that generated the most alerts were ibuprofen (10,864) and acetylsalicylic acid (4336) out of a total of 34,063.
Overall, the alerts with the lowest degree of acceptance were those attributed to interactions between treatments, with 25% (423,884) of a total of 1,691,886 being accepted. More specifically, the interactions of NSAIDs with acetylsalicylic acid generated the greatest number of alerts, reaching 220,507 alerts with an acceptance level of 18% (40,227). Table 3 outlines the 10 main interactions at the active ingredient level, which represent 30% (506,082) of all alerts of this type.
Analysis of the PREFASEG alerts related to therapeutic duplication
In the 3 years studied, the four groups of duplications that generated the most alerts were the NSAIDs, paracetamol-type analgesics, renin-angiotensin system (RAS) inhibitors and gastric protectors (see Fig. 3). Out of a total of 65 groups, these 4 duplication groups represented 42% (600,930) of the total alerts generated (1,436,721). Duplications related to analgesics and gastric protectors had the highest levels of acceptance during the study period, reaching 42% (88,435) and 32% (33,245), respectively. In contrast, duplications related to the SSRI antidepressants and the RAS inhibitor antihypertensives had the lowest degrees of acceptance, i.e., 20% (10,753) and 21% (20,940), respectively.
Furthermore, the pairs of active ingredients with the greatest numbers of alerts generated for duplications during the 3 years studied were paracetamol–paracetamol, paracetamol–paracetamol with tramadol, omeprazole–omeprazole, ibuprofen–ibuprofen, and metamizole–metamizole. These 5 pairs represented 22% (317,390) of the duplications, of which 144,450 (46%) were accepted.
Moreover, the duplications related to antibiotics such as amoxicillin generated a considerable number of alerts, i.e., 76,409 over the 3 years studied, and their acceptance rate was relatively low at 23%. Upon the analysis of other groups of potentially dangerous duplications, such as those related to oral anticoagulants, it was observed that PREFASEG generated 14,903 alerts of duplications for this group, of which 42% (6314) were accepted, and the prescriptions were not continued.
Analysis of PREFASEG alerts related to AEMPS safety alerts
It was found that the number of alerts related to AEMPS safety alerts increased throughout the study period, i.e., from 59,146 in 2016 to 84,158 in 2018. This was accompanied by a reduction in the degree of acceptance of these alerts from 31% (18,301) to 22% (18,720), respectively.
Analysing the details of these AEMPS alerts (see Table 4), it was apparent that the Triple Whammy, which considered the concomitant therapy of NSAIDs, diuretics, and RAS inhibitors, generated the highest degree of alerts, representing 85% (195,987) of the total alerts. The degree of acceptance of this type of alert varied, ranging from 30% (13,867) in 2016 to 22% (15,988) in 2018, thereby indicating a decrease in acceptance over this 3-year period. Reviewing the main anti-inflammatory drugs that generated the Triple Whammy alerts, it was observed that in 65% of the cases, the NSAIDs involved were ibuprofen and naproxen.
As indicated in Table 4, the number of alerts generated by diclofenac decreased over time. More specifically, in 2016, diclofenac generated 7288 alerts, while by 2018 this number had reduced to 5137. However, the degree of acceptance also decreased from year to year, dropping from 36% (2588) in 2016 to 29% (1511) in 2018.
The alerts with the highest degree of acceptance were those related to strontium ranelate, raloxifene/bazedoxifene, and aliskiren; however the number of such alerts was low since these are drugs that are being gradually withdrawn from the market, or tend to be unused in daily practice.
Analysis of the PREFASEG alerts related to medicines not recommended for use in geriatrics between January 2016 and December 2018
The alerts generated by PREFASEG that were related to drugs advised against for use in geriatrics increased throughout the study period, i.e., from 108,974 in 2016 to 188,139 in 2018. However, a reduction in the degree of acceptance from 30% (32,345) to 27% (50,299), respectively, was also observed.
The two pharmacological groups that generated the highest number of alerts within this category were the benzodiazepines and the NSAIDs, representing 39% (172,574) and 21% (47,966) of a total of 441,920 alerts in the 3 years studied (see Table 5). More specifically, the alerts related to benzodiazepine usage in geriatrics increased by 55% during the study period, i.e., from 30,662 in 2016 to 68,974 in 2018. Alprazolam represented 44% (65,910) of the alerts generated for benzodiazepines in this group of patients (see Table 6), and overall, the benzodiazepine group showed an acceptance rate of 27% over the 3 years.
Within the NSAID alerts, it was observed that desketoprofen represented 48% (45,293) of the total alerts in this group, and this group showed one of the lowest levels of acceptance (i.e., 22%).
In general, analysis of the degrees of acceptance in this class of alerts shows a significant level of variation (see Table 5), and the pharmacological groups with the highest degree of acceptance (i.e., where no prescription was issued for the corresponding treatment) were the muscle relaxants (41%, 7521) and the peripheral vasodilators (39%, 6621).
Discussion
The main finding of this study was that the PREFASEG system appears to adopt the role of a CDSS that assists in preventing potential safety MRPs for patients by generating online alerts when starting a new treatment. During the period studied, it was observed that 28% of the generated security alerts led to a modification of the prescription (i.e., acceptance of the alert). In absolute terms, between 2016 and 2018, a total of 1,222,159 recommendations were accepted globally, which likely led to the avoidance of numerous potential MRPs in patients. Overall, PREFASEG reported a safety MRP in 1 out of every 15 new prescriptions. The degrees of acceptance of the recommendations were relatively high when compared with a similar study into a different online preventive alert system, where the percentages of acceptance ranged from 12 to 14% [30]. However, the variability between studies was considerable; in a 2009 Cochrane review on the effects of online prompts/reminders, an improvement of only 4.2% was reported [18], while other studies described omissions of recommendations in between 49 and 96% of the cases [31]. In general, subsequent systematic reviews [32, 33] concluded that online notification systems had only a small or moderate effect.
Our study presents a number of characteristics that could explain the relatively high acceptance rate of alerts. For example, the observed degree of acceptance could be accounted for by considering that the tool takes into account the success characteristics of CDSSs described by various authors previously [10, 34]. More specifically, it is integrated into the workflow of clinicians, it generates an alert automatically during the parent consultation and in the context of their medical history, and it provides a specific therapeutic recommendation in each case. In addition, PREFASEG produces different types of safety alerts based the clinical situation of each patient and any medication that they may be taking, and it gives alerts related to the safe prescription of medication for various pathologies. To date, few studies have analysed such a diversity of alerts simultaneously [35,36,37]. It should also be emphasised here that PREFASEG is a tool whose clinical contents are constantly being updated and that has been in use for more than 12 years, during which time it has exhibited a good degree of acceptance by a large number of medical professionals, since it is used by > 6400 PC physicians on a daily basis. Indeed, both ICS pharmacists and PC clinical pharmacologists promote the use of this tool.
Despite the high number of potential MRPs avoided in patients in Catalonia, it should be noted that in the case of safety alerts relating to the use of medicines, it was striking that globally, > 70% of the alerts generated by PREFASEG were ignored, which amounts to 3.16 million over the 3-year study period. However, it must be considered that, on occasions, the recommendations given by PREFASEG did not necessarily imply a change, or the change was not recorded as such. In addition, some recommendations involved a dose reduction or a clinical follow-up of some variable, and therefore the prescription was continued. In such circumstances, the system did not count the recommendation as accepted, even if the dose was lowered or an analysis was requested. If these modifications had been registered, the degree of acceptance would be higher, as the presented acceptance values relate only to cases where the prescription was continued. It should also be considered that not all alerts had the same degree of clinical relevance, with alerts being accompanied by either an orange or a red icon, depending on the importance of the recommendation, as also described in a previous study [23].
Over the course of the 3 years studied, the number of generated alerts increased. This was partly related to the fact that new and updated content was introduced into the PREFASEG system on an annual basis. The existence of a direct relationship between the increased consumption of certain drugs (e.g., the benzodiazepines) was also considered, in addition to the probability that greater numbers of MRP alerts could be generated from such drugs due to their increased use among the population. At the same time, it should be noted that the degree of acceptance of the alerts tended to decrease over time, with practitioners gradually ignoring the recommendations. This decline in acceptance could be partly attributed to alert fatigue; however, it will be necessary to further investigate the reasons behind the rejection of alerts, in addition to separately analysing the high and medium–low relevance alerts, while also considering the cases where the recommendation does not suggest a change of drug. It will also be essential to collect the opinions of the professionals who use the PREFASEG tool. According to various reports, the main reasons for low acceptance by clinicians are the large number of low-relevance alerts they receive and their poor content [21, 22, 38]. To reduce the risk of fatigue, it is therefore necessary to increase the specificity of the alerts, provide clear and concise information, and not impact on the clinician’s workflow.
In relation to the ignored alerts regarding suspicions of a history of hypersensitivity to certain drugs, it is known that general practitioners tend to register cases of hypersensitivity that are reported by patients, despite the fact that such hypersensitivity has not been confirmed, and in many cases, are not real [39,40,41]. To address this issue, a number of hospitals are now working on a project to de-label patients with a supposed hypersensitivity reported in their clinical history unless it is confirmed by the corresponding tests.
Another type of MRP that drew significant attention due to its severity was that of teratogenic drugs, for which 66% of the generated alerts were ignored. However, it must be considered that not all medicines act as teratogens in all trimesters of pregnancy, and PREFASEG is unable to distinguish between such cases. It is also possible that some alerts were generated for women who were no longer pregnant but who, by some registration error, maintained a pregnancy status in their health records.
Regarding the alerts related to therapeutic duplications, it was observed that approximately 70% of these alerts were ignored by clinicians. However, many such alerts were related to adjustment of the daily dose of treatment, and so it was necessary to combine presentations at different doses; this was common in the groups of antihypertensive RAS inhibitors and antidepressants, and in the replacement of amoxicillin with amoxicillin-clavulanate. In terms of the NSAIDs and paracetamol-type analgesics, it was observed that prescriptions were authorised for issuing on demand if necessary, which often generated alerts related to duplication if an attempt was made to prescribe a drug from the same pharmacological group. Another group of duplications that drew attention due to their association with a high risk of serious adverse effects that motivate hospital admissions were the oral anticoagulants [42]. During the 3-year study period, PREFASEG produced 14,903 alerts related to duplications in this group of drugs, which translated to an acceptance of 42% (6314), wherein the prescription was not continued.
In the case of the AEMPS safety alerts, an unexpected low degree of acceptance was recorded considering that these constituted specific alerts from a regulatory agency [43]. In fact, throughout the 3-year study period, the degree of acceptance of the AEMPS safety alerts decreased, and in 2018 they reflected the lowest percentage of acceptance (22%) of all alerts throughout that year. Among these notices, the Triple Whammy, which is associated with a significant increase in the risk of kidney failure [44], represented the largest number of alerts.
Upon examination of the alerts related to the use of drugs advised against in geriatrics, it was observed that the degree of acceptance ranged from 30% in 2016 to 27% in 2018. Despite the fact that this alert category is considered of low clinical relevance, wherein use of a specific drug may not be recommended in older patients but is not totally contraindicated, it produced similar or even superior acceptance results compared to the AEMPS safety alerts. It was therefore considered that this level of acceptance was due to physicians being somewhat more sensitive to safety alerts related to elderly patients. However, we must not lose sight of the fact that > 70% of these alerts were discarded and the corresponding prescriptions was generated, which could lead to potential adverse reactions in patients. In this context, it is estimated that drug-associated adverse effects produce approximately 6.5% of hospital admissions, of which more than half of these could be prevented [45,46,47,48].
The pharmacological groups that generated the highest number of alerts in geriatric patients were the benzodiazepines and the NSAIDs, which are also widely used drugs throughout the population. The significant increase in the number of alerts for benzodiazepines (i.e., from 30,662 in 2016 to 68,974 in 2018) was particularly surprising, and these were mainly attributed to alprazolam. It is known that both an advanced age, which is linked to metabolic and pharmacokinetic changes, and the number of drug treatments that a patient is receiving, are two of the situations that increase the risk of adverse drug effects to the greatest extent [49,50,51]. In addition, it must be considered that the world population is constantly aging, which is accompanied by a greater degree of pathologies, and an increase in the use of pharmaceuticals [52,53,54].
Analysing the percentages of acceptance for alerts related to the use of drugs advised against in geriatrics, significant variation was observed between the different pharmacological groups. More specifically, muscle relaxants and peripheral vasodilators were the groups with the highest degrees of acceptance. According to a previous study, physicians tend to prioritise alerts that are more clinically relevant, or that can be resolved with the least amount of time or effort [55].
In a classic study looking at hospitalisations caused by adverse effects, it was found that the majority occurred in the elderly, and were due to commonly used drugs with well-known safety profiles [56]. Considering this point, which can likely be extrapolated to other countries, it would be interesting to analyse the situation of patients for whom PREFASEG detected a possible MRP that was not addressed.
In terms of limitations to the current study, it should be noted that the moderate percentage of alert acceptance highlights the need to investigate the causes that lead clinicians to discard such a high number of recommendations. Thus, to maximise the usefulness of PREFASEG and to avoid possible alert fatigue, it will be necessary to carry out a detailed review into the traceability data of the tool to eliminate low-relevance alerts that are generated but not accepted, and to highlight any alerts related to therapeutic orientations while providing one or more alternative active ingredients. The introduction of a block to prevent the continuation of a prescription associated with a severe MRP could also be considered.
On the other hand, essential future work should also focus on analysing the acceptance of MRP alerts based on their clinical relevance and the type of recommendation, which are key aspects to consider in the case of drug interactions. In addition, a satisfaction survey should be carried out to request feedback and suggestions from practitioners with regards to improving the PREFASEG system in terms of its clinical content and technological aspects.
The future development of PREFASEG also involves the inclusion of medicines that can only be prescribed in hospitals and their corresponding contraindications, which will allow the program to be extended to different levels of care. The technological evolution of the tool is also necessary to render it more specific when generating alerts. For example, this could be achieved using the terminology common to all SNOMED CT systems (Systematised Nomenclature of Medicine—Clinical Terms) that determine the active ingredient, the dose, the pharmaceutical form, and the number of packaging units [57,58,59]. To optimise the use of PREFASEG and improve the management of clinical information, intelligent systems such as natural language processing could be applied that would allow the clinician to obtain and interact with the information recorded in text format in the patient's clinical history [60, 61]. An improved follow-up and monitoring of the PREFASEG alerts would also be desirable, wherein details regarding the professional receiving the alert are registered and made visible, in addition to whether this alert is ignored, and the level of care of the corresponding professional.
In summary, PREFASEG appears to be a feasible and efficient strategy to improve some aspects of clinical safety related to the prescription of drugs, and as a result, in the health care received by patients.
Conclusions
Our study demonstrated that the PREFASEG (PREscripción FArmacéutica SEGura, i.e., safe pharmaceutical prescription) clinical decision support system contributes to the prevention of potential safety medicine-related problems in patients. In 28% of the cases in which the tool generated a safety alert, primary care physicians modified their prescriptions by some means. The main drug groups implicated in the PREFASEG alerts were the non-steroidal anti-inflammatory drugs, the benzodiazepines, and the renin-angiotensin system inhibitors; groups that frequently cause adverse effects and motivate hospital admissions.
In future, it will be necessary to study in detail the reasons behind the fact that > 70% of the generated alerts were ignored by physicians. In addition, the possibility of reducing the number of alerts should be assessed to avoid alert fatigue. Moreover, it is evident that strategies must be designed to make the prescriber aware of the importance of patient safety, as well as to technologically improve the tool and render it more robust and specific.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ADE:
-
Adverse drug event
- AEMPS:
-
Spanish Agency for Medicines and Health Products (Agencia Española del Medicamentos y Productos Sanitarios)
- CDSS:
-
Clinical decision support system
- ECW:
-
Electronic clinical workstation
- EHR:
-
Electronic health record
- ICS:
-
Institut Català de la Salut (Catalan Health Institute)
- MRP:
-
Medication-related problem
- NSAIDs:
-
Non-steroidal anti-inflammatory drugs
- PC:
-
Primary care
- PREFASEG:
-
PREscripción FArmacéutica SEGura, i.e., safe pharmaceutical prescription
- RAS:
-
Renin-angiotensin system
References
European Commission. Commission staff working document. Pharmacovigilance related activities of Member States and the European Medicines Agency concerning medicinal products for human use (2012–2014). https://ec.europa.eu/health//sites/health/files/files/pharmacovigilance/pharmacovigilance-report-2012-2014_annexen.pdf. Accessed 19 Oct 2019.
Institute of Medicine (US) Committee on Quality of Health Care in American. In: Kohn LT, Corrigan JM, Donaldson MS, editors. To err is human: building a safer health system. Washington, DC: National Academies Press (US); 1999.
Council of Europe Expert Group on Safe Medication Practices. Creation of a better medication safety culture in Europe: building up safe medication practices. Strasbourg: Council of Europe; 2006.
National Patient Safety Agency. Seven steps to patient safety for primary care. London: National Patient Safety Agency; 2006.
World Health Organization (WHO). World alliance for patient safety. Geneva: World Health Organization; 2007.
Food and Drug Administration. Safe use initiative: collaborating to reduce preventable harm from medications. Geneva: US Department of Health and Human Service, Food and Drug Administration; 2009.
Institute of Medicine (US) Committee on Quality of Health Care in America. Crossing the quality chasm: a new health system for the 21st century. Washington, DC: National Academies Press (US); 2001.
Institute of Medicine (US) Committee on Identifying and Preventing Medication Errors. Quality chasm series. Preventing medication errors. Washington, DC: National Academies Press (US); 2007.
Bates DW, Kuperman GJ, Wang S, Gandhi T, Kittler A, Volk L, et al. Ten commandments for effective clinical decision support: making the practice of evidence-based medicine a reality. J Am Med Inform Assoc. 2003;10(6):523–30.
Payne TH. Computer decision support systems. Chest. 2000;118(2 Suppl.):47S-52S.
Kawamoto K, Houlihan CA, Balas EA, Lobach DF. Improving clinical practice using clinical decision support systems: a systematic review of trials to identify features critical to success. BMJ. 2005;330(7494):765–8.
Bates DW, Cullen DJ, Laird N, Petersen LA, Small SD, Servi D, et al. Incidence of adverse drug events and potential adverse drug events: implications for prevention. JAMA. 1995;274(1):29–34.
McCoy AB, Waitman LR, Lewis JB, Wright JA, Choma DP, Miller RA, et al. A framework for evaluating the appropriateness of clinical decision support alerts and responses. J Am Med Inform Assoc. 2012;19(3):346–52.
Bates DW, Spell N, Cullen DJ, Burdick E, Laird N, Petersen LA, et al. The costs of adverse drug events in hospitalized patients. Adverse Drug Events Prevention Study Group. JAMA. 1997;277(4):307–11.
Bobb A, Gleason K, Husch M, Feinglass J, Yarnold PR, Noskin GA. The epidemiology of prescribing errors: the potential impact of computerized prescriber order entry. Arch Intern Med. 2004;164(7):785–92.
Hunt DL, Haynes RB, Hanna SE, Smith K. Effects of computer-based clinical decision support systems on physician performance and patient outcomes: a systematic review. J Am Med Assoc. 1998;280(15):1339–46.
Wasylewicz ATM, Scheepers-Hoeks AMJW. Clinical decision support systems. In: Kubben P, Dumontier M, Dekker A, editors. Fundamentals of clinical data science. Cham: Springer International Publishing; 2018. p. 153–69.
Shojania KG, Jennings A, Mayhew A, Ramsay CR, Eccles MP, Grimshaw J. The effects of on-screen, point of care computer reminders on processes and outcomes of care. Cochrane Database Syst Rev. 2009;3:CD001096.
Moja L, Kwag KH, Lytras T, Bertizzolo L, Brandt L, Pecoraro V, et al. Effectiveness of computerized decision support systems linked to electronic health records: a systematic review and meta-analysis. Am J Public Health. 2014;104(12):e12-22.
Coma E, Medina M, Méndez L, Hermosilla E, Iglesias M, Olmos C, et al. Effectiveness of electronic point-of-care reminders versus monthly feedback to improve adherence to 10 clinical recommendations in primary care: a cluster randomized clinical trial. BMC Med Inform Decis Mak. 2019;19(1):245.
Judge J, Field TS, DeFlorio M, Laprino J, Auger J, Rochon P, et al. Prescribers’ responses to alerts during medication ordering in the long term care setting. J Am Med Inform Assoc. 2006;13(4):385–90.
van der Sijs H, Mulder A, van Gelder T, Aarts J, Berg M, Vulto A. Drug safety alert generation and overriding in a large Dutch university medical centre. Pharmacoepidemiol Drug Saf. 2009;18(10):941–7.
Paterno MD, Maviglia SM, Gorman PN, Seger DL, Yoshida E, Seger AC, et al. Tiering drug–drug interaction alerts by severity increases compliance rates. J Am Med Inform Assoc. 2009;16(1):40–6.
Sittig DF, Wright A, Osheroff JA, Middleton B, Teich JM, Ash JS, et al. Grand challenges in clinical decision support. J Biomed Inform. 2008;41(2):387–92.
Institut Català de la Salut ICS Clinical Practice Guidelines. http://ics.gencat.cat/ca/assistencia/coneixement-assistencial/guies-de-practica-clinica/. Accessed 28 Oct 2021.
Fick DM, Semla TP, Steinman M, Beizer J, Brandt N, Dombrowski R, et al. American Geriatrics Society 2019 updated AGS Beers Criteria® for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2019;67(4):674–94.
Renom-Guiteras A, Meyer G, Thürmann PA. The EU(7)-PIM list: a list of potentially inappropriate medications for older people consented by experts from seven European countries. Eur J Clin Pharmacol. 2015;71(7):861–75.
O’Mahony D, O’Sullivan D, Byrne S, O’Connor MN, Ryan C, Gallagher P. STOPP/START criteria for potentially inappropriate prescribing in older people: version 2. Age Ageing. 2015;44(2):213–8.
Holt S, Schmiedl S, Thürmann PA. Potentially inappropriate medications in the elderly: the PRISCUS list. Dtsch Arztebl. 2010;107(31–32):543–51.
Dexheimer JW, Talbot TR, Sanders DL, Rosenbloom ST, Aronsky D. Prompting clinicians about preventive care measures: a systematic review of randomized controlled trials. J Am Med Inform Assoc. 2008;15(3):311–20.
Bright TJ, Wong A, Dhurjati R, Bristow E, Bastian L, Coeytaux RR, et al. Effect of clinical decision-support systems: a systematic review. Ann Intern Med. 2012;157(1):29–43.
Cheung A, Weir M, Mayhew A, Kozloff N, Brown K, Grimshaw J. Overview of systematic reviews of the effectiveness of reminders in improving healthcare professional behavior. Syst Rev. 2012;1(1):36–43.
Ivers N, Jamtvedt G, Flottorp S, Young JM, Odgaard-Jensen J, French SD, et al. Audit and feedback: effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2012;6:CD000259.
Osheroff JA. Improving medication use and outcomes with clinical decision support: a step by step guide. Chicago: HIMSS; 2009.
Van Wyk JT, Van Wijk MAM, Sturkenboom MCJM, Mosseveld M, Moorman PW, Van Der Lei J. Electronic alerts versus on-demand decision support to improve dyslipidemia treatment: a cluster randomized controlled trial. Circulation. 2008;117(3):371–8.
Clyne B, Bradley MC, Hughes C, Fahey T, Lapane KL. Electronic prescribing and other forms of technology to reduce inappropriate medication use and polypharmacy in older people: a review of current evidence. Clin Geriatr Med. 2012;28(2):301–22.
Upperman JS, Staley P, Friend K, Neches W, Kazimer D, Benes J, Wiener ES. The impact of hospitalwide computerized physician order entry on medical errors in a pediatric hospital. J Pediatr Surg. 2005;40(1):57–9.
Tamblyn R, Huang A, Taylor L, Kawasumi Y, Bartlett G, Grad R, et al. A randomized trial of the effectiveness of on-demand versus computer-triggered drug decision support in primary care. J Am Med Inform Assoc. 2008;15(4):430–8.
Trubiano JA, Adkinson NF, Phillips EJ. Penicillin allergy is not necessarily forever. JAMA. 2017;318(1):82–3.
van Dijk SM, Gardarsdottir H, Wassenberg MW, Oosterheert JJ, de Groot MC, Rockmann H. The high impact of penicillin allergy registration in hospitalized patients. J Allergy Clin Immunol Pract. 2016;4(5):926–31.
Wilcock M, Powell N. Challenges of delabelling penicillin allergy. Droga Ther Bull. 2021;59(11):163–4.
Gaist D, Wallander MA, González-Pérez A, García-Rodríguez LA. Incidence of hemorrhagic stroke in the general population: validation of data from The Health Improvement Network. Pharmacoepidemiol Drug Saf. 2013;22(2):176–82.
Agencia Española de Medicamentos y Productos Sanitarios. Notas informativas de la AEMPS. Madrid (España): Agencia Española de Medicamentos y Productos Sanitarios (AEMPS). https://www.aemps.gob.es/acciones-informativas/notas-informativas-de-la-aemps/. Accessed 19 Apr 2021.
Lapi F, Azoulay L, Yin H, Nessim SJ, Suissa S. Concurrent use of diuretics, angiotensin converting enzyme inhibitors, and angiotensin receptor blockers with non-steroidal anti-inflammatory drugs and risk of acute kidney injury: nested case-control study. BMJ. 2013;346:e8525.
Aranaz-Andrés JM, Aibar-Remón C, Vitaller-Murillo J, Ruiz-López P, Limón-Ramírez R, Terol-García E. Incidence of adverse events related to health care in Spain: results of the Spanish National Study of Adverse Events. J Epidemiol Community Health. 2008;62(12):1022–9.
Aranaz-Andrés JM, Aibar C, Limón R, Mira JJ, Vitaller J, Agra Y, et al. A study of the prevalence of adverse events in primary healthcare in Spain. Eur J Public Health. 2012;22(6):921–5.
Howard RL, Avery AJ, Slavenburg S, Royal S, Pipe G, Lucassen P, et al. Which drugs cause preventable admissions to hospital? A systematic review. Br J Clin Pharmacol. 2007;63:136–47.
Pirmohamed M, James S, Meakin S, Green C, Scott AK, Walley TJ, et al. Adverse drug reactions as cause of admission to hospital: prospective analysis of 18,820 patients. Br Med J. 2004;329(7456):15–9.
Cullinan S, O’Mahony D, Fleming A, Byrne S. A meta-synthesis of potentially inappropriate prescribing in older patients. Drugs Aging. 2014;31(8):631–8.
Gavilán-Moral E, Villafaina-Barroso A, Jiménez-de Gracia L, del Gómez Santana MC. Ancianos frágiles polimedicados: ¿Es la deprescripción de medicamentos la salida? Rev Esp Geriatr Gerontol. 2012;47(4):162–7.
Page RL, Linnebur SA, Bryant LL, Ruscin JM. Inappropriate prescribing in the hospitalized elderly patient: defining the problem, evaluation tools, and possible solutions. Clin Interv Aging. 2010;5(1):75–87.
Turgeon J, Michaud V, Steffen L. The dangers of polypharmacy in elderly patients. JAMA Intern Med. 2017;177(10):1544.
Onder G, Marengoni A. Polypharmacy. JAMA. 2017;318(17):1728.
Payne RA. The epidemiology of polypharmacy. Clin Med J R Coll Phys Lond. 2016;16(5):465–9.
Loo TS, Davis RB, Lipsitz LA, Irish J, Bates CK, Agarwal K, et al. Electronic medical record reminders and panel management to improve primary care of elderly patients. Arch Intern Med. 2011;171(17):1552–8.
Budnitz DS, Lovegrove MC, Shehab N, Richards CL. Emergency hospitalizations for adverse drug events in older Americans. N Engl J Med. 2011;365(21):2002–12.
Jiang G, Solbrig HR, Chute CG. ADEpedia: a scalable and standardized knowledge base of adverse drug events using semantic web technology. AMIA Annu Symp Proc. 2011;2011:607–16.
Farfán Sedano FJ, Terrón Cuadrado M, García Rebolledo EM, Castellanos Clemente Y, Serrano Balazote P, Gómez DÁ. Implementation of SNOMED CT to the medicines database of a general hospital. Stud Health Technol Inform. 2009;148:123–30.
Guía de Conjuntos de Referencias de SNOMED CT para el SNS. Centro Nacional de Referencia para SNOMED CT: Ministerio de Sanidad, Servicios Sociales e Igualdad; 2016.
Wei WQ, Cronin RM, Xu H, Lasko TA, Bastarache L, Denny JC. Development and evaluation of an ensemble resource linking medications to their indications. J Am Med Inform Assoc. 2013;20(5):954–61.
Fung KW, Jao CS, Demner-Fushman D. Extracting drug indication information from structured product labels using natural language processing. J Am Med Inform Assoc. 2013;20(3):482–8.
Acknowledgements
This study has been prepared within the framework of the Doctorate in Pharmacology at the Universitat Autònoma de Barcelona (UAB). We would like to thank ICS Information Systems for supporting us during acquisition of the information required to conduct this study. We would also like to thank the PREFASEG working group for helping to maintain a useful and up-to-date tool.
Funding
The primary care component of this study was funded by the Institut Universitari d’Investigació en Atenció Primària (IDIAP Jordi Gol) Scholarship to complete a PhD thesis in primary care.
Author information
Authors and Affiliations
Contributions
MAP extracted, analysed, and interpreted the data on the use of the PREFASEG tool. She also wrote the majority of the manuscript. MO helped to interpret the data on the use of the PREFASEG tool, in addition to giving support and making contributions to the writing of the manuscript. AF and ED reviewed the data analysis process, reviewed the various parts of the manuscript, and made the relevant contributions to give clarity and understanding to the study. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable. This manuscript does not report studies involving human participants, human data or human tissue. This manuscript does not report studies involving animals.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Annex Table 1. Description of the types of PREFASEG alerts; Annex Table 2. Groups of pharmacological duplications included in PREFASEG in 2018; Annex Table 3. Definitions of the AEMPS safety alerts included in PREFASEG in 2018; Annex Table 4. List of drugs not recommended for use in geriatrics in 2018.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Pons-Mesquida, M.À., Oms-Arias, M., Diogène-Fadini, E. et al. Safer prescription of drugs: impact of the PREFASEG system to aid clinical decision-making in primary care in Catalonia. BMC Med Inform Decis Mak 21, 349 (2021). https://doi.org/10.1186/s12911-021-01710-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12911-021-01710-8