Abstract
Background
Provision of care to patients with chronic diseases remains a great challenge for modern health care systems. eHealth is indicated as one of the strategies which could improve care delivery to this group of patients. The main objective of this study was to assess determinants of the acceptance of the Internet use for provision of chosen health care services remaining in the scope of current nationwide eHealth initiative in Poland.
Methods
The survey was carried out among patients with diagnosed chronic conditions who were treated in three health care facilities in Krakow, Poland. Survey data was used to develop univariate and multivariate logistic regression models for six outcome variables originating from the items assessing the acceptance of specific types of eHealth applications. The variables used as predictors were related to the sociodemographic characteristics of respondents, burden related to chronic disease, and the use of the Internet and its perceived usefulness in making personal health-related decisions.
Results
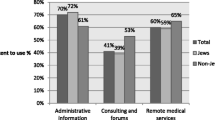
Among 395 respondents, there were 60.3% of Internet users. Univariate logistic regression models developed for six types of eHealth solutions demonstrated their higher acceptance among younger respondents, living in urban areas, who have attained a higher level of education, used the Internet on their own, and were more confident about its usefulness in making health-related decisions. Furthermore, the duration of chronic disease and hospitalization due to chronic disease predicted the acceptance of some of eHealth applications. However, when combined in multivariate models, only the belief in the usefulness of the Internet (five of six models), level of education (four of six models), and previous hospitalization due to chronic disease (three of six models) maintained the effect on the independent variables.
Conclusions
The perception of the usefulness of the Internet in making health-related decision is a key determinant of the acceptance of provision of health care services online among patients with chronic diseases. Among sociodemographic factors, only the level of education demonstrates a consistent impact on the level of acceptance. Interestingly, a greater burden of chronic disease related to previous hospitalizations leads to lower acceptance of eHealth solutions.
Similar content being viewed by others
Background
In recent years, the provision of care to patients with chronic conditions has become one of the greatest challenges faced by health care systems. Patients with chronic diseases require care for prolonged periods. Estimates indicate that in modern societies up to 40% of people suffer from chronic conditions [1]. Furthermore, expenditures related to care provided to patients with chronic diseases are a significant part of health care budgets [2].
Chronic care requires regular interactions between patients and health care systems. Patient involvement in the monitoring and treatment of disease is of crucial importance for the effectiveness of the therapy [3,4]. The growing incidence of chronic diseases can lead to a shortage of health care resources available to patients and their families. All these circumstances trigger intensive searches for new models of care which would enable an adequate and cost-effective support offered to patients with chronic diseases. Development of eHealth environment is frequently indicated as a promising response to challenges associated with chronic care [5-9].
The performance of the health care system in Poland is a continuous source of frustration for patients. A survey conducted among Polish citizens in 2012 revealed that 78% respondents were not satisfied with the health care system. The main complaints were related to patients having a limited access to diagnostic tests and specialty care [10]. A regular nationwide survey “Social Diagnosis” carried out in 2013 also showed that according to 28% of households, the fulfilment of health care needs worsened in last year, and only 2% of respondents declared an improvement of the situation [11]. Reforms of the health care system have lagged behind the political and economic transformation of the early 1990s. More profound changes to the health care system were initiated in the late 1990s. Unfortunately, consecutive governments have not been consistent in maintaining the direction of the reforms. Initially, the responsibility for organizing the provision of health care services was delegated to a network of regional health funds. The next government reversed the regional system of health care funding and, in 2003, introduced a centralized system based on the National Health Fund [12]. Although funding of the health service has increased considerably in the last decade, it remains low in comparison to other EU member states. According to WHO, Polish health expenditure per capita measured in US dollars Purchasing Power Parity (PPP) in 2008 was among the lowest in Europe [13]. Growing expectations of patients and society related to health care services overlap with a general shortage of available resources in the health care system [14,15]. Recent attempts to optimize the health service reimbursement system, the introduction of diagnosis-related group (DRG)-based reimbursement and new rules for setting lists of reimbursed pharmaceuticals have not translated into a better financial standing for health care institutions and patient satisfaction [16]. To sum up, the health care system suffers from many problems, and remedial actions to date have not been fully effective [17]. This has led to a continued search for new strategies which would result in the optimization of care delivery. The use of information and communication technologies (ICT) in health care is perceived as an approach which has a potential to increase efficiency and cost-effectiveness of services.
Indeed, for at least the last two decades there has been a growing trend to increase the implementation of ICT systems in an attempt to support both health care providers and patients. These efforts have been intensified after Poland’s accession to the European Union; a part of the structural funds available to Poland have been directed to the public domain for investing in ICT infrastructure. There are also ambitious plans to develop an advanced information infrastructure in health care [18,19]. Expanding the use of eHealth systems in order to support patients and citizens has become one of key elements of the strategy adopted by the Polish government [20]. The applications enlisted on the priority list include Internet-based medical record, e-prescribing, online access to results of laboratory tests, and making appointments to see physicians [20].
Nowadays, it is obvious that eHealth development is a participatory process and depends strongly on the involvement of all relevant stakeholders [21]. The rationale for developing specific types of eHealth solutions cannot rely on administrative decisions only, but must also address the needs and attitudes of recipients of care services. Thus, plans for the implementation of eHealth applications in chronic care should consider the acceptance and preparedness of patients. Assessing patients’ opinions could provide important information about the acceptance of specific solutions. Additionally, potential factors influencing these opinions should be studied and considered in the process of making decisions about the priorities for eHealth implementation when formulating national level policies.
The acceptance of technology is usually understood as both the intention to use it and its actual use. Strategies of the assessment of eHealth acceptance stem from theories related to behavioural change and technology acceptance. Among them, the technology acceptance model (TAM) [22] and the unified theory of acceptance and use of technology (UTAUT) [23] were most frequently used in relation to eHealth acceptance among health professionals and patients. The TAM model emphasizes two aspects: perceived usefulness and perceived ease of use [24]. In turn, UTAUT is based on four determinants of intention and usage: performance expectancy, effort expectancy, social influence and facilitating conditions. This theory also anticipates behavioural intention and observable use behaviour may be influenced by four moderators including gender, age, experience and voluntariness of use [23].
It also seems that eHealth acceptance among patients has not been addressed so frequently by researchers as its acceptance among professionals. Most reports on eHealth acceptance by physicians published in the last decade applied the two theoretical models mentioned above [25-27].
In their study of patient’s acceptance of provider-delivered eHealth, Wilson et al. used the TAM model and the motivational model [28]. The TAM model was also used in the assessment of the acceptance of an application for Internet-based patient-physician communication [29] and an application designed for patients with HIV/AIDS [30]. The UTAUT theory was used by Beenkens to assess eHealth acceptance among patients with venous thrombosis [31]. This author demonstrated that patient performance and effort expectancies have a strong influence on behavioural intentions to use eHealth technology; additionally a quality of health care measure should be included in the assessment.
Ehealth acceptance is a complex concept related to individual preferences and attitudes. It may be of key importance for the successful implementation of eHealth solutions. Apart from eHealth acceptance, the concept of “eHealth readiness” related to the ability of potential users or health care organizations to benefit from eHealth applications is used by researchers [32-34]. Insights into eHealth readiness may facilitate proceeding efficiently with the development of an eHealth environment.
The main objective of this study was to assess opinions of patients with chronic conditions regarding the feasibility of eHealth to support health care activities in the context of national initiatives focused on the formation of an eHealth environment. The paper presents results of the assessment of patient perception of concrete types of services provided via the Internet. An assessment was also carried out with the intention of yielding guidance for representatives of governmental bodies involved in decision-making in relation to the development of an eHealth domain on the national level. Advanced eHealth tools are not commonly available for end-users in Poland, and patients with chronic diseases may still be perceived as an eHealth-naive population. Thus, the analysis is based on items asking for opinions about the possibility of using the Internet for the provision of health care services rather than their actual use or perceived usefulness originating from real experience. The results of the survey conducted among patients with chronic diseases receiving care from three medical centres in the urban area of Krakow, Poland, form the basis for this analysis.
It was not the aim of this paper to provide a comprehensive view of eHealth acceptance among patients with chronic conditions. Instead, the paper focuses on specific eHealth applications enabling the provision of health services essential in chronic care, in relation with policies developed on the national level. Thus, the term ”acceptance” is used throughout the paper only in relation to concrete types of eHealth solutions. It is applied to designate the respondents’ positive opinion about the possibility of providing of specific health care service online.
Methods
Overview
A cross-sectional survey was performed in a convenience sample of 524 patients with chronic diseases who remained under the care of three medical centres located in Krakow, Poland. The study was conducted from December 2011 to April 2012 until 400 completed questionnaires were returned. The survey focused on the assessment of the opinions of patients suffering from long-term medical conditions about the feasibility of eHealth-based services for care provision. In this paper, the results of the analysis of factors influencing the acceptance of specific eHealth applications relevant to chronic care are presented. The selection of these applications was dictated by their relationship with national policies of eHealth development and current activities in this field in Poland.
Survey questionnaire
The questionnaire developed for the study covered aspects related to the burden of disease, the use of information technologies (IT), health-related use of the Internet, eHealth literacy (eHEALS scale) [35], the acceptance of the use of the Internet and related technologies for the provision of health-related services, and sociodemographic characteristics of the respondents. The key areas covered by the questionnaire stemmed from the review of international references related to the assessment of the eHealth acceptance and use by target audiences. The questionnaire was piloted in a group of 10 patients. As a result, some items were removed as they were deemed to be redundant, or modified to provide a better understanding.
The final version of the questionnaire included 73 items. Questions asking for the respondents’ opinions used the five-point Likert scale (from strongly disagree to strongly agree with neutral in the middle position). The questionnaire also included items assessing the frequency of specific events or activities (relevant frequency scales were assigned) and the respondents’ use of computers and the Internet, also in relation to general and health-related activities with dichotomous (yes/no) response options. For questionnaire items used for the analysis presented in the paper see Additional file 1.
Study setting and participants
The questionnaires were distributed to patients admitted to hospital or attending an ambulatory visit in three healthcare facilities in the Krakow area: the Department of Metabolic Diseases and the Department of Pulmonology, both part of the Jagiellonian University Medical College, and the Jozef Dietl Municipal Hospital in Krakow. The survey was carried out among patients suffering from medical conditions requiring long-term support from the health care system. Thus, only patients with an established diagnosis of a chronic disease with an established treatment were recruited to the survey. Patients who were hospitalized or admitted to polyclinics for diagnosis of new symptoms were not included in the study, unless they had previously been diagnosed with a chronic disease.
Study protocol
The respondents were first informed about the objectives and scope of the survey, and asked for their consent to be included in the study and for processing of the data included in the questionnaire. Questionnaires were distributed to the respondents by interviewers employed and trained for the study, recruited from the medical personnel of the health care centres participating in the study. The study protocol was approved by the Bioethical Committee at the Jagiellonian University (decision No. KBET/107/B/2011 dated 30 June 2011).
Measures
Sociodemographic characteristics
The respondents were asked to provide information about their gender, age, education level, and place of residence. The item asking about the respondents’ education included 9 options from basic to university level, specific to the Polish education system. Nine levels of education included in the questionnaire were collapsed into three categories: (1) education level lower than upper secondary according to the International Standard Classification of Education (ISCED) [36], (2) education level including upper secondary to post-secondary non-tertiary according to ISCED, and (3) education level covering all levels according to ISCED higher than post-secondary non-tertiary. The place of residence was initially assigned five options: rural, urban with <10 000, urban 10 000 – 100 000, urban 100 000 – 500 000, and urban with >500 000 inhabitants. Initial five categories were collapsed to three categories included in the logistic regression models.
Burden of chronic disease
Items included in the survey questionnaires related to the burden of chronic disease for the respondent included duration of chronic disease, hospitalizations resulting from its course, and number of chronic diseases.
Internet use
Respondents were asked about their Internet use and their opinions about the usefulness of the Internet in making decision about their own health. They could select one of three response options in relation to Internet use: independent use of the Internet, use of the Internet with help from others, and no use of the Internet at all. The item asking about the usefulness of the Internet (item 1 from the eHealth literacy scale according to Norman and Skinner) was assigned five response options: from not useful at all to very useful, with the neutral option in the middle [35].
Attitudes toward the use of the Internet for provision of services
The survey questionnaire included items asking about the acceptance of the use of specific eHealth applications. In this paper, the acceptance of the provision of the following online services was analysed: 1) accessing patient medical record, 2) making appointments to see physicians, 3) renewing prescriptions, 4) accessing results of laboratory tests, 5) accessing educational resources, and 6) consulting physicians. The relevant questionnaire items were formulated as “Do you think this service may be provided via the Internet?”, where the service means one of the six types of eHealth applications listed above. The responses to these items could be provided according to the five-point Likert scale from strongly agree to strongly disagree, with the neutral response in the middle position. Initial responses expressed with the five-point Likert scale were collapsed into two categories: ‘0’ – if the respondent selected “Strongly disagree”, “Rather disagree” or “Not sure/Don’t know”, and ‘1’ – if the respondent selected “Strongly agree” or “Rather agree”.
Statistical analysis
Statistical analysis was performed using IBM SPSS v.21 (Armonk, NY, USA). Descriptive analysis was performed for the variables described in the paper. If not stated otherwise, the frequency of responses to specific items was given as a percentage of all valid responses excluding missing responses. The assessment of determinants of the acceptance of eHealth services was conducted with univariate and multivariate logistic regression models. The problem of missing data was addressed with the multiple imputation procedure. The p level below 0.05 was treated as significant.
Missing values
Multiple imputation was performed on the initial data set to account for missing values, according to fully conditional specification procedure available in the SPSS v.21 package. All independent and dependent variables were included in the procedure [37]. The percentage of missing values was 9.9 %. The frequencies of missing values in the variables included in logistic regression models ranged from 0% to 22.9% (see Table 1). Given the high percentage of missing values in some variables, the imputation was repeated twenty times [38].
Logistic regression modelling
The outcome variables were derived from items related to the acceptance of the provision of specific activities online. The predictors included in the model were gender, age, place of residence, education level, number of chronic diseases, duration of the chronic disease, hospitalization related to the chronic disease, Internet use, and opinion about the usefulness of the Internet for making personal health-related decisions. First, the influence of predictors on outcome variables was assessed with univariate logistic regression models. Then, the multivariate models were developed including all nine predictors used for the univariate models.
Multivariate logistic regression was preceded by multicollinearity diagnostic analysis with a calculation of variance inflation factor (VIF) values for independent variables. No concerns were raised, since all VIF values were below 2.0 (Table 2).
Multivariate logistic regression was conducted by the forward method available in the SPSS v.21 package. The odds ratios (OR) and 95% confidence intervals (95%CI) were calculated for predictor variables both in univariate and multivariate logistic regression models. Sensitivity analysis was performed using a nonimputed data set for multiple regression modelling (see Additional file 2) for OR and 95%CI). The results were not contradictory in relation to the pooled results of logistic regression modelling on 20 imputed data sets. Statistical significance changed only in case of a few independent variables when pooled results of multiple logistic regressions carried out on multiply-imputed data set were compared to the results on nonimputed data set.
Results
Characteristics of respondents
Questionnaires were completed by 400 patients from 524 approached by canvassers asking them to join the survey (response rate 76.3%). Following quality checks, five questionnaires were excluded from the analysis because of missing sociodemographic data. Women made up 64.2% of the respondents. The mean age of the respondents (SD) was 47.9 (17.7) years, with 46.6 (17.9) years for women and 50.2 (17.4) years for men. The median age was 50 years, with 31 as the lower quartile and 61 as the higher quartile. The percentage of Internet users (respondents who access the Internet on their own without help from other people) was 60.3% in the study group. More than one chronic disease was diagnosed in 46.3% of respondents. At least one hospitalization due to chronic disease was reported by 71.4% of respondents. Median chronic disease duration was 10 years, with lower and upper quartiles at 5 and 18 years respectively. Detailed information on the frequencies of gender, age categories, level of education, place of residence of respondents, the variables showing the burden of disease, prevalence of chronic diseases, Internet use and opinion about the usefulness of the Internet for making decision about the patient’s own health is shown in Table 3.
Determinants of opinions about the use of the Internet for the provision of health care services
Accessing medical record
The frequency of responses accepting the use of the Internet for accessing patient medical record was 60.7%. Higher acceptance was related to younger age, inhabitance in urban areas, higher education level, only one chronic disease in respondent, no previous hospitalizations caused by the chronic disease, the use of the Internet, and a higher conviction that the Internet is useful for making personal health-related decisions. Respondents with the chronic disease lasting 5–10 years were less prone to accept Internet-based access that those with duration of disease not surpassing 5 years. OR and 95%CI for specific determinants are presented in Table 4. When combined in the multivariate logistic regression model (Table 4), a statistically significant effect was maintained by the level of education (highest education level in relation to reference level of education; OR 2.52; 95%CI 1.12-5.67), previous hospitalization due to chronic disease (no hospitalization vs. at least one hospitalization, OR 0.44, 95%CI 0.22-0.85), and opinion about the usefulness of the Internet for making personal health-related decisions (OR for comparison between the lowest conviction about the usefulness and higher levels; from 3.80 to 6.02 with no difference in relation to the middle response). The odds that respondents with the highest level of education will accept accessing medical documentation online were 2.52 times greater than for respondents from the group with the lowest level of education. The respondents who were highly convinced about the usefulness of the Internet in making health-related decision had 6 times higher odds that they will accept such access than those who believed that the Internet was not useful at all.
Making appointment to see physician
Among services provided with eHealth, making appointments with physician received the highest acceptance from respondents (77.4%). The predictors which demonstrated a statistically significant influence on the acceptance in the univariate model included age, education, number of chronic diseases, duration of chronic disease, use of the Internet, and opinion about the usefulness of the Internet in making personal health-related decisions. In the multivariate logistic regression model, the only independent variable which maintained a significant influence was the opinion about Internet usefulness (OR and 95%CI for comparison between options “not useful at all” and “unsure”, “useful” and “very useful” were 3.56, 1.25-10.18; 6.94, 2.13-22.59 and 11.06, 2.49-49.01, respectively). The odds that respondents convinced about a high usefulness of the Internet for making health-related decisions have a positive opinion about the possibility of using the Internet for making appointment to see physician were 11 times higher when compared with respondents who believed that the Internet was not useful at all for making such decisions. The results of both models are presented in Table 5.
Renewing prescriptions
The acceptance of eHealth application for renewing prescriptions reached 60.2%. The variable which predicted the acceptance in univariate logistic regression models included age, place of residence, education, duration of chronic disease, use of the Internet, and the opinion about the usefulness of the Internet in making personal health-related decisions. The only predictor in the multivariate model was the use of the Internet (OR and 95%CI for comparison of users with non-users 3.23, 1.56-6.69). This means that Internet users were 3.23 times more likely to accept renewing prescriptions online than nonusers. Detailed results of both univariate and multivariate logistic regression models are presented in Table 6.
Accessing results of laboratory tests
The acceptance of using the Internet for accessing laboratory test results was 63.8%. The predictors of the acceptance in univariate logistic regression models included age, place of residence, education, admission to hospital due to chronic disease, the use of the Internet, and the opinion about the usefulness of the Internet in making personal health-related decisions. In the multivariate model, a statistically significant impact was maintained by education (OR and 95%CI for comparison between the lowest and the highest levels of education: 2.56 and 1.12-5.86, respectively), admission to hospital due to chronic disease (OR and 95%CI for comparison between no admission and at least one admission: 0.52 and 0.27-0.98, respectively) and the opinion about the usefulness of the Internet in making health-related decisions (OR and 95% for comparison between response option “not useful at all” and more favourable opinions about the usefulness: 4.43, 1.21-16.29; 3.26, 1.09-9.79; 6.64, 2.28-19.30 and 4.81, 1.45-15.96, respectively). The results show that respondents, who have been admitted to hospital due to chronic disease at least once, were 0.52 times less likely to accept accessing results of laboratory tests results online than respondents who have not been hospitalized. Respondents with the highest education level showed 2.56 higher odds of accepting online provision of this service when compared to individuals with the lowest education level. Detailed results of both models are included in Table 7.
Accessing educational resources for patients
Online access to education resources for patients was accepted by 66.9% respondents. Independent variables predicting the acceptance of this application in univariate logistic regression models were education, place of residence, education, duration of chronic disease, hospitalization due to chronic disease, the use of the Internet and the opinion about the usefulness of the Internet in making personal health-related decisions. In the multivariate model, a statistically significant impact was maintained by education (OR and 95%CI for comparison between the highest and lowest levels of education: 2.51, 1.09-5.74), hospitalization due to chronic disease (OR and 95%CI for comparison between no admission and at least one admission to hospital due to chronic disease: 0.51, 0.27-0.96), duration of chronic disease (OR and 95%CI for comparison between respondents with the disease lasting ≤5 and those with the disease lasting >5 to 10 years: 0.30, 0.14-0.64) and the opinion about the usefulness of the Internet in making personal health-related decisions. For the last independent variable, OR and 95%CI for comparison between the response option “not useful at all” and options “not useful”, “useful” and “very useful” were 4.17, 1.15-14.21; 7.56, 2.29-24.95, and 11.38, 2.73-47.47, respectively. All results of logistic regression modelling in relation to accessing education resources online as an independent variable are shown in Table 8.
Consulting physician
The acceptance of using the Internet for consulting physician was the lowest among independent variables (51.6%). Independent variables with a statistical significance in univariate and multivariate logistic regression models were education, duration of chronic disease and the opinion about the usefulness of the Internet in making personal health-related decisions (Table 9). The values of OR and 95%CI for comparison between respondents with the lowest and highest level of education were 2.33 and 1.31-4.12, respectively. As for duration of the chronic disease, the only significant difference was between respondents with the chronic disease lasting not longer than 5 years and those with the disease lasting more than 10 years and not longer than 18 years (OR and 95%CI: 2.48, 1.22-5.03). This means that the odds of accepting online consultations with physicians by patients with the shortest duration of chronic disease were 2.48 times lower than the odds of patients with the diseases lasting more than 10 years and not longer than 18 years. However, higher approval levels for this type of online service were not seen among respondents suffering from chronic diseases for longer periods. As for the opinion about the usefulness of the Internet for making personal health-related decisions, the differences were statistically significant for comparison between the option “not useful at all” and options “useful” and “very useful” (OR and 95%CI for these comparisons: 3.39, 1.34-8.57 and 4.60, 1.51-13.98, respectively).
Discussion
Principal results
Poland’s accession to the European Union stimulated activities focused on the development of information systems supporting public administration, and the provision of services to citizens, including health care applications. Target areas for development in relation to health care services encompass solutions including patient medical records accessible online, applications for booking appointments with physicians, e-prescribing system, and applications providing access to laboratory test results [39,40]. Using information systems for interactions between patients and health care providers and enhancing the support of patients with access to educational resources was also considered. Implementing eHealth solutions involving patients as end-users requires careful planning and anticipating potential reactions and compliance. This study assessed the acceptance of specific eHealth solutions forming priority areas for national strategies among patients with chronic diseases.
Results of univariate models applied to six types of eHealth solutions consistently revealed that sociodemographic variables had a significant impact on their acceptance. Most eHealth solutions were more accepted by respondents of younger age, higher education level, and urban place of residence with above 100,000 inhabitants. Furthermore, patients using the Internet on their own, and expressing a positive opinion about the usefulness of the Internet in making personal health-related decisions were more likely to accept most of the eHealth solutions included in the analysis. These finding are in line with results of studies performed in various patient groups in other countries [41-51]. The same determinants were also reported for health-related Internet use or acceptance in general populations [52-56]. It is worth noting that our study did not reveal an effect of gender on the acceptance of eHealth systems. Many other studies have reported higher health-related Internet use among women [53,55-59].
Variables related to the burden of disease (number of chronic diseases, duration of chronic disease and hospitalization due to chronic disease) also showed a significant effect on the acceptance of specific applications. Hospitalization due to chronic disease and multiple chronic diseases diagnosed in a patient were both associated with a lower acceptance of three of the six eHealth applications included in the logistic regression models. As for the duration of chronic disease, the acceptance of four of the six eHealth applications was significantly lower among patients with the disease lasting from above 5 to 10 years in comparison to patients with disease duration ≤5 years. Interestingly, the comparison between patients with the shortest disease duration and two categories with the longest duration did not show statistically significant differences. The use of the Internet for consulting physician was more accepted by patients with disease duration from above 10 to 18 years in comparison with the category with the shortest disease duration. There have been some studies indicating a lower use or acceptance of using the Internet for health-related purposes among respondents with a higher disease burden [60,61]. A study on data from a nationwide survey of households in Poland revealed that the hospitalization of a member of a household did not have a significant impact on the acceptance of Internet-based health care services, and recent use of health care services was related only to the acceptance of a limited form of health service online [62]. Other studies have reported a higher acceptance or use of the Internet for health-related purposes among people with previous or existing medical conditions [57,58,63-65].
It should be noted that a longer duration of disease or more than one chronic condition occurring in the same patient are frequently correlated to his or her older age, which in turn is generally associated with lower Internet use, also in the context of health care services.
When included in the multivariate model, the significant effect on the acceptance of specific eHealth solutions was maintained consistently by variables indicating the respondent’s opinion on the usefulness of the Internet for making decisions on personal health, and their education level. The variable related to the respondent’s view on the usefulness of the Internet had a significant impact on all but one independent variable. Education level remained a significant predictor of the acceptance of four types of eHealth solutions analysed except making appointment to see physician and renewing prescriptions. From other independent variables, the hospitalization due to the chronic disease was related to lower acceptance of types of eHealth services and Internet use to higher acceptance of renewing prescriptions online. The impact of duration of the chronic disease was observed in two types of eHealth services.
Our results suggest that the respondents’ views on the usefulness of the Internet for making personal health-related decisions could serve as a universal predictor of patient attitudes towards the implementation and use of eHealth solutions. In five out of six multivariate logistic regression models, it maintained its effect on the acceptance of eHealth solutions. In relation to the acceptance of making appointment with physician online, it appeared to be the only predictor.
In the multivariate logistic regression models, the independent effects of age and place of residence on the acceptance vanished. This is likely due to the fact that the opinion about the usefulness of the Internet for personal health combines the effects stemming from the respondent’s sociodemographic background, especially age and place of residence.
E-prescription was the only application with the acceptance significantly influenced by using the Internet rather than by a positive opinion about the usefulness of the Internet for making personal health-related decisions. For the remaining four applications, the effect of Internet use was overridden by the opinion about its usefulness. This finding may serve as an important indication that Internet use as such is not a sufficient determinant of the acceptance of eHealth services.
Limitations
The study suffered from several limitations. First of all, the group of respondents was limited to patients obtaining care from selected health care facilities in one large city located in southern Poland. Thus, broader extrapolation of the results of the study should be made with caution. On the other hand, the percentage of patients living in rural areas was sufficiently high to provide feedback on their opinions. Two of the three medical departments providing care to respondents serve as referral centres in their specialty areas, which could have an impact on both the characteristics of the patients and their perceived needs for additional or alternative ways of support including eHealth. Another weakness was the high frequency of missing values, especially in relation to variables related to the acceptance of specific forms of eHealth services. To remedy this, the multiple imputation procedure was employed. The comparison of the results of multiple regression modelling performed on the non-imputed data set and pooled results of the analysis on data sets resulting from multiple imputation did not show essential differences. There were only a few discrepancies in terms of predictors having a statistically significant impact on independent variables. Finally, respondents included in the survey should be treated as an eHealth-naive population. Most patients in Poland have only a limited access to advanced eHealth systems. Their opinions about the feasibility of eHealth applications do not come from direct experience, but are likely influenced mainly by their experience of general Internet use, also in health-related context, and the use of electronic public administration applications in some cases.
Conclusions
The study demonstrates that the acceptance of specific eHealth solutions among patients with chronic conditions depends on their general attitude toward the usefulness of the Internet for personal health. Two other important predictors of the acceptance included the patient’s education and previous hospitalizations due to the chronic disease. The effects of sociodemographic factors such as age or place of residence as well as Internet use were not maintained as statistically significant predictors in multivariate models. These observations may lead to the conclusion that implementation of eHealth applications addressed to chronic patients should be preceded with interventions focused on increasing their understanding and acceptance of the eHealth domain. Without appropriate preparation of target audiences, the group of active users may be limited to younger, better educated patients from highly populated urban areas. Furthermore, the use of the Internet is in itself not sufficient to improve the acceptance of eHealth solutions.
References
Anderson G, Horvath J. The growing burden of chronic disease in America. Public Health Rep. 2004;119:263–70.
DeVol R, Bedroussian A. An unhealthy America: the economic burden of chronic disease. Milken Institute: October; 2007 [http://assets1b.milkeninstitute.org/assets/Publication/ResearchReport/PDF/chronic_disease_report.pdf]
Kennedy A, Rogers A, Bower P. Support for self-care for patients with chronic disease. BMJ. 2007;335:968–70.
Greenhalgh T. Chronic illness: beyond the expert patient. BMJ. 2009;338:b49.
Forkner-Dunn J. Internet-based patient self-care: the next generation of health care delivery. J Med Internet Res. 2003;5, e8.
Oh H, Rizo C, Enkin M, Jadad A. What is eHealth (3): a systematic review of published definitions. J Med Internet Res. 2005;7, e1.
Harrison JP, Lee A. The role of E-Health in the changing health care environment. Nurs Econ. 2006;24:283–8.
Coye MJ, Haselkorn A, DeMello S. Remote patient management: technology-enabled innovation and evolving business models for chronic disease care. Health Aff. 2009;28:126–35.
Black AD, Car J, Pagliari C, Anandan C, Cresswell K, Bokun T, et al. The impact of eHealth on the quality and safety of health care: a systematic overview. PLoS Med. 2011;8, e1000387.
Centrum Badania Opinii Społecznej (CBOS). Opinie o funkcjonowaniu systemu opieki zdrowotnej. (Opinions about functioning of health care system). Report from research. BS/34/2012, Warszawa, March 2012. [http://cbos.pl/SPISKOM.POL/2012/K_034_12.PDF]
Czapiński J, Panek T. Social diagnosis 2013. Objective and subjective quality of life in Poland. Contemporary Economics. Warsaw: Quarterly of University of Finance and Management in Warsaw; 2013. 7 (Special Issue):109–18.
Skawińska M. The analysis of the functioning of health care systems in chosen European Union countries (examples of Sweden, Great Britain, Poland and Germany). (Polish). In: Stanisław G, editor. Medical Studies. Kielce: Wydawnictwo Uniwersytetu Jana Kochanowskiego; 2009. 13:69–78.
Sagan A, Panteli D, Borkowski W, Dmowski M, Domanski F, Czyzewski M, et al. Poland. Health system overview. Health systems in transition. European Observatory on Health Systems and Policies. 2011;13:56. [http://www.euro.who.int/__data/assets/pdf_file/0018/163053/e96443.pdf]
Siwczyńska D, Minko M. The functioning of health systems in Poland and the Netherlands in patients’ opinions. Med Biol Sc. 2012;26:115–20.
Rutkowska-Podolowska M, Poplawski L, Zaleska-Tsitini M. Health care policy in Poland and in selected European union countries: attempts at reducing fast increasing medical care costs. The Malopolska School of Economics in Tarnow Research Papers Collection. 2011;19:131–9. http://zn.mwse.edu.pl/ebooki/19/131-139.pdf.
Kolwitz M. The polish healthcare system perspectives and possibilities for adoption of healthcare systems from other countries of the European union. Ann Acad Med Stetin. 2010;56:131–43. http://212.14.41.9/Content/21747/Roczniki_56_3_2010.pdf#page=133.
Boulhol H, Sowa A, Golinowska S, Sicari P. Improving the Health-Care System in Poland. OECD Economics Department Working Papers, No. 957, OECD Publishing. [http://dx.doi.org/10.1787/5k9b7bn5qzvd-en]
Gomez-Barroso JL, Feijo C. Are Central and Eastern European Countries managing to develop the information society? Transformations in Business & Economics. 2010;9:18–41. http://oa.upm.es/8819/1/INVE_MEM_2010_87332.pdf.
Reggi L, Scicchitano S. European Regions Financing Public e-Services: The case of EU Structural Funds. Working Papers Series in Economics, Mathematics and Statistics, WP-EMS 2011/10. [http://www.econ.uniurb.it/RePEc/urb/wpaper/WP_11_10.pdf]
Centrum Systemów Informacyjnych w Ochronie Zdrowia. Kierunki informatyzacji “e-Zdrowie Polska” na lata 2011–2015. (Directions of informatization “e-Health Poland” for years 2011–2015) (Polish). Warszawa 2009. [http://www.csioz.gov.pl/file.php?s=cD81Ng]
van Gemert-Pijnen JE, Nijland N, van Limburg M, Ossebaard HC, Kelders SM, Eysenbach G, et al. A holistic framework to improve the uptake and impact of eHealth technologies. JMIR. 2011;13, e111.
Davis F. User acceptance of information technology: system characteristics, user perceptions and behavioral impacts. Int J Man–machine Studies. 1993;38:475–87.
Venkatesh V, Morris MG, Davis GB, Davis FD. User acceptance of information technology: toward a unified view. MIS Q. 2003;27:425–78.
Davis FD. Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Q. 1989;13:319–40.
Hu PJ, Chau PYK, Sheng ORL, Tam KY. Examining technology acceptance model using physician acceptance of telemedicine technology. J Manage Inf Syst. 1999;16:91–112.
Chau PYK, Hu PJH. Investigating healthcare profesionals’ decisions to accept telemedicine technology: an empirical test of competing theories. Inform Manage. 2002;39:297–311.
Dünnebeil S, Sunayaev A, Blohm I, Leimester JM, Krcmar H. Determinants of physicians’ technology acceptance for e-health in ambulatory care. Int J Med Inform. 2012;81:746–60.
Wilson EV, Lankton NK. Modeling patients’ acceptance of provider-delivered E-health. J Am Med Inform Assoc. 2004;11:241–8.
Klein R. Internet-Based Patient-Physician Electronic Communication Applications: Patient Acceptance and Trust. e-Service J. 2007;5(2) Special Issue: Research in e-Health (Winter 2007):27–52. [http://www.jstor.org/stable/10.2979/ESJ.2007.5.2.27]
Lai TY, Larson EL, Rockoff ML, Bakken S. User acceptance of HIV TIDES-Tailored Interventions for Management of Depressive Symptoms in persons living with HIV/AIDS. J Am Med Inform Assoc. 2008;15:217–26.
Beenkens FHC. Acceptance of e-Health Technology: a patient perspective. PhD Thesis. Delft University of Technology 2011. [http://repository.tudelft.nl/assets/uuid:43537f2b-eab1-4707-ab7e-59e3864b3e12/111201-Beenkens.FHC-Thesis.Complete.pdf]
Khoja S, Scott RE, Casebeer AL, Mohsin M, Ishaq AFM, Gilani S. e-Health readiness assessment tools for healthcare institutions in developing countries. Telemed J E Health. 2007;13:425–32.
Legare E, Vincent C, Lehoux P, Anderson D, Kairy D, Gagnon MP, et al. Developing and validating the French-Canadian version of the practitioner and organization telehealth readiness assessment tools. J Telemed Telecare. 2010;16:140–6.
Tamburis O, Mangia M, Contenti M, Mercurio G, Rossi Mori A. The LITIS conceptual framework: measuring eHealth readiness and adoption dynamics across the Healthcare Organizations. Health Technol. 2012;2:97–112.
Norman CD, Skinner HW. eHEALS: the eHealth literacy scale. JMIR. 2006;8, e27.
United Nations Educational, Scientific and Cultural Organization. Revision of the International Standard Classification of Education (ISCED). 2011. [http://unesdoc.unesco.org/images/0021/002116/211619e.pdf]
Sterne JAC, White IR, Carlin JB, Spratt M, Royston P, Kenward MG, et al. Multiple imputation for missing data in epidemiological and clinical research: potential and pitfalls. BMJ. 2009;338:b2393.
Newgard CD, Haukoos JS. Advanced statistics: missing data in clinical research – part 2: multiple imputation. Acad Emerg Med. 2007;14:669–78.
Ernst & Young. Summary of feasibility study of the project: electronic platform for collection, analysis and sharing of digital Medical Records. Version EU 1.0 EN. Warsaw, December 17th, 2009. [http://p1.csioz.gov.pl/pliki/file/Summary%20of%20Feasibility%20Study%20P1%20-%20EU.pdf]
Centrum Systemów Informacyjnych Ochrony Zdrowia. “Internet-based patient record” project. [http://ikp.gov.pl]
Fogel J, Albert SM, Schnabel F, Ditkoff BA, Neugut AI. Use of the internet by women with breast cancer. J Med Internet Res. 2002;4, e9.
Peterson MW, Fretz PC. Patient use of the internet for information in a lung cancer clinic. Chest. 2003;123:452–7.
Kalichman SC, Benotsch EG, Weinhardt L, Austin J, Luke W, Cherry C. Health-related internet use, coping, social support, and health indicators in people living HIV/AIDS: preliminary results from a community survey. Psychol. 2003;22:111–6.
Dickerson S, Reinhart AM, Feeley TH, Bidani R, Rich E, Garg VK, et al. Patient internet use for health information at three urban primary care clinics. J Am Med Inform Assoc. 2004;11:499–504.
Sabel MS, Strecher VJ, Schwartz JL, Wang TS, Karimipour DJ, Orringer JS, et al. Patterns of internet use and impact on patients with melanoma. J Am Acad Dermat. 2005;52:779–85.
Bass SB, Ruzek SB, Gordon TF, Fleisher L, McKeown-Conn N, Moore D. Relationship of Internet health information use with patient behavior and self-efficacy: experience of newly diagnosed cancer patients who contact the National Cancer Institute’s Cancer Information Service. J Health Commun. 2006;11:219–36.
Mancini J, Nogues C, Adenis C, Berthet P, Banadona V, Chompret A, et al. Patient’s characteristics and rate of Internet use to obtain cancer information. J Pub Health. 2006;28:235–7.
Cima RR, Anderson KJ, Larson DW, Dozois EJ, Hassan I, Sandborn WJ, et al. Internet use by patients in an inflammatory bowel disease specialty clinic. Inflamm Bowel Dis. 2007;13:1266–70.
Buntrock S, Hopfgarten T, Adolfsson J, Oneloy E, Steineck G. The Internet and prostate cancer patients. Searching and finding information. Scand J Urol Nephrol. 2007;41:367–74.
van de Poll-Franse LV, van Eenbergen MC. Internet use by cancer survivors: current use and future wishes. Support Care Cancer. 2008;16:1189–95.
van Uden-Kraan CF, Drossaert CHC, Taal E, Smit WM, Moens HJB, Siesling S, et al. Health-related internet use by patients with somatic diseases: frequency of use and characteristics of users. Inform Health Soc Care. 2009;34:18–29.
Atkinson NL, Saperstein SL, Pleis J. Using the internet for health-related activities: findings from a national probability sample. J Med Internet Res. 2009;11, e4.
Siliquini R, Ceruti M, Lovato E, Bert F, Bruno S, De Vito E, et al. Surfing the internet for health information: an Italian survey on use and population choices. BMC Med Inform Decis Mak. 2011;11:21.
Takahashi Y, Ohura T, Ishizaki T, Okamoto S, Miki K, Naito M, et al. Internet use for health-related information via personal computers and cell phones in Japan: a cross-sectional population-based survey. J Med Internet Res. 2011;13, e110.
Kontos E, Blake KD, Chou WYS, Prestin A. Predictors of eHealth usage: insights on the digital divide from the health information national trends survey 2012. J Med Internet Res. 2014;16, e172.
Beck F, Richard JB, Nguyen-Thanh V, Montagni I, Parizot I, Renahy E. Use of the internet as a health information resource among French young adults: results from a nationally representative survey. JMIR. 2014;16, e128.
Rice RE. Influences, usage, and outcomes of internet health information searching: multivariate results from the Pew surveys. Int J Med Inform. 2006;75:8–28.
Beckjord EB, Rutten LJF, Squiers L, Arora NK, Volckmann L, Moser RP, et al. Use of the internet to communicate with health care providers in the United States: estimates from the 2003 and 2005 Health Information National Trends Surveys (HINTS). J Med Internet Res. 2007;9, e20.
Renahy E, Parizot I. Internet and health: lessons learned from the French national survey on households living conditions in 2005. [French] Rev Epidemiol Sante Publique. 2008;56:117–25.
Gracia E, Herrero J. Internet use and self-rated health among older people: a national survey. J Med Internet Res. 2009;11, e49.
Wang JY, Bennet K, Probst J. Subdividing the digital divide: differences in internet access and use among rural residents with medical limitations. J Med Internet Res. 2011;13, e25.
Duplaga M. Acceptance of internet-based health care services among households in Poland: secondary analysis of a population-based survey. J Med Internet Res. 2012;14, e164.
Hsu J, Huan J, Kinsman J, Fireman B, Miller R, Selby J, et al. Use of e-Health services between 1999 and 2002: a growing digital divide. J Am Med Inform Assoc. 2005;12:164–71.
Renahy E, Parizot I, Chauvin P. Health information seeking on the Internet: a double divide? Results from a representative survey in the Paris metropolitan area, France, 2005–2006. BMC Public Health. 2008;8:69.
Choi NG, DiNitto DM. Internet use among older adults: association with health needs, psychological capital, and social capital. J Med Internet Res. 2013;15, e97.
Acknowledgments
The author would like to thank Prof. Maciej Małecki, MD, PhD, Head of the Department of Metabolic Diseases, Prof. Ewa Niżankowska-Mogilnicka, MD, PhD, former Head of the Department of Pulmonology, Jagiellonian University Medical College, Krakow, Poland, and Dr Andrzej Kosiniak-Kamysz, Director of the Jozef Dietl Hospital in Krakow, for the support and consent to perform the survey among the patients remaining under the care of the Departments and Hospital. The author also acknowledges the help of Elżbieta Brzezicka, M.Sc. and Michał Witkowski, M.Sc. in the survey data entry. Finally, the author extends thanks to Katarzyna Kruczak, MD, PhD, Mirosława Dzikowska, M.Nurs., Anna Andrychiewicz, M.Nurs., Monika Rucka, M.Nurs. and Bartłomiej Matejko for help in distributing the questionnaire to potential respondents.
Funding
This research was supported by the resources of the project No K/ZDS/003685 at the Jagiellonian University Medical College.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that he has no competing interests.
Additional files
Additional file 1:
Questionnaire items used for the analysis presented in the paper (English and Polish versions).
Additional file 2:
The results of multiple logistic regression modelling on nonimputed data set.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Duplaga, M. A cross-sectional study assessing determinants of the attitude to the introduction of eHealth services among patients suffering from chronic conditions. BMC Med Inform Decis Mak 15, 33 (2015). https://doi.org/10.1186/s12911-015-0157-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12911-015-0157-3