Abstract
Background
The demand for organ transplants, both globally and in South Korea, substantially exceeds the supply, a situation that might have been aggravated by the enactment of the Life-Sustaining Treatment Decision Act (LSTDA) in February 2018. This legislation may influence emergency medical procedures and the availability of organs from brain-dead donors. This study aimed to assess LSTDA’s impact, introduced in February 2018, on organ donation status in out-of-hospital cardiac arrest (OHCA) patients in a metropolitan city and identified related factors.
Methods
We conducted a retrospective analysis of a regional cardiac arrest registry. This study included patients aged 16 or older with cardiac arrest and a cerebral performance category (CPC) score of 5 from January 2015 to December 2022. The exclusion criteria were CPC scores of 1–4, patients under 16 years, and patients declared dead or transferred from emergency departments. Logistic regression analysis was used to analyse factors affecting organ donation.
Results
Of the 751 patients included in this study, 47 were organ donors, with a median age of 47 years. Before the LSTDA, there were 30 organ donations, which declined to 17 after its implementation. In the organ donation group, the causes of cardiac arrest included medical (34%), hanging (46.8%), and trauma (19.2%). The adjusted odds ratio for organ donation before the LSTDA implementation was 6.12 (95% CI 3.09–12.12), with non-medical aetiology as associated factors.
Conclusion
The enactment of the LSTDA in 2018 in South Korea may be linked to reduced organ donations among patients with OHCA, underscoring the need to re-evaluate the medical and legal aspects of organ donation, especially considering end-of-life care decisions.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
The discrepancy between the number of patients on organ donation waiting lists and the availability of donors continues to increase, posing a significant challenge both in South Korea and globally. For instance, in the European Union, the incidence of transplantation for solid organs increased, and 60,000 patients were registered on the waiting list for organ donation in 2008 [1]. In South Korea, 48,472 people were waiting for organ transplants in 2021, but the number of organ transplants performed was only 5,839. Organ donation from brain-dead donors increased until 2016 but subsequently declined, dropping from 515 in 2017 to 442 in 2021 [2].
The Life-Sustaining Treatment Decision Act (LSTDA), enacted in South Korea in February 2018, aimed to mitigate the prolonged suffering of terminally ill patients by legally allowing the withdrawal of Life-Sustaining Treatment (LST), such as cardiopulmonary resuscitation (CPR) and mechanical ventilation [3]. The LSTDA seeks to reduce the burden on patients and their families by enabling accurate end-of-life (EOL) decisions and reducing unnecessary medical interventions. This legislation has potentially altered the dynamics of organ donation, as the decision to withdraw LST may limit opportunities for organ recovery.
Emergency physicians play a critical role in treating severely ill patients, often encountering cases with poor prognosis, including anticipated brain death. Despite the importance of their role in identifying potential organ donors, there is significant variability in the process of organ donation. This variability is largely influenced by the physicians’ knowledge, attitudes, and experiences with EOL care decisions [4, 5]. After the enforcement of the LSTDA, the number of cases involving target temperature management (TTM), potential brain death, and notification of brain death decreased, potentially leading to fewer opportunities to consider organ donation from potential brain-dead donors [6].
This study aimed to provide a comprehensive analysis of the impact of the LSTDA on organ donation status among patients with out-of-hospital cardiac arrest (OHCA) in a metropolitan city. By examining the trends and outcomes after the implementation of the LSTDA, this study seeks to contribute to the understanding of how legislative changes can affect critical aspects of medical practice, such as organ donation.
Methods
Study setting, design, and participants
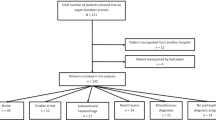
This retrospective, observational study used data from the Regional Cardiac Arrest Registry of Daegu Metropolitan City [7, 8]. As of January 2023, Daegu Metropolitan City had a population of 2.4 million and covered an area of 883.51 km2. The city has 2 level one regional emergency departments (ED) and 4 level two local EDs. These EDs provide the highest level of emergency care services in the region, catering to approximately 217,000 patients annually, which accounts for 54.5% of all ED visits in Daegu [9]. Participants included individuals aged ≥ 16 who experienced OHCA in Daegu between January 2015 and December 2022. The exclusion criteria were as follows: patients younger than 16 years (n = 149), OHCAs with a cerebral performance category (CPC) score of < 5 (n = 716), deceased upon arrival (n = 378), discharged against medical advice or considered a hopeless discharge (n = 25), and insufficient information on hospital outcomes because of transfer to another hospital in the ED (n = 147). Additionally, patients who died in the ED (n = 7,671) were also excluded (Fig. 1).
Legislative implementation and organ donation in Korea
In 2018, Korea implemented the “Act on Decisions on Life-Sustaining Treatment for Patients in Hospice and Palliative Care or at the End of Life”, commonly referred to as the LST Decision Act [3]. This legislation was enacted to emphasis the dignity and worth of individuals nearing the end of their lives, aspects that have been historically undervalued, as well as the importance of advance care planning and considerations surrounding LSTs in EOL care.
This legislation applies to patients in hospice care or in the process of dying. LST is defined as treatment that only prolongs the period of dying without any curative effect, and includes interventions, such as CPR, mechanical ventilation, renal dialysis, chemotherapy, and transfusion [3]. The LSTDA does not specifically mention organ donation.
Under the LSTDA, life-sustaining treatment can be withdrawn upon confirmation of the patient’s intention or consent from the family. This confirmation process requires documentation of the patient’s prior intention or a statement from two or more family members inferring the patient’s intention. Advance directives are documents in which individuals aged 19 or older express their decisions to discontinue LST and their intentions regarding hospice care. The LSTDA recognizes these directives to confirm the patient’s wishes regarding LST. If the patient is unable to express their intention or if their intention cannot be assumed, the consent of all family members is required particularly among patients who have experienced OHCA and subsequently received CPR. Although CPR is considered a life-sustaining treatment, the decision to withdraw LST following the return of spontaneous circulation involves the patient’s guardians or family members. If they decide to withhold LST after hospital admission, the process of documenting and legalizing this decision still affects the patient even if they had previously received CPR.
In South Korea, the Act on Transplantation of Organs stipulates that organ donation should be performed following brain death, with donation after circulatory death being performed only in limited situations within Maastricht category IV [10, 11]. Suspected brain-dead patients must be reported to the organ procurement organization [10]. If brain death is confirmed, the family decides whether to donate the patient’s organs, often without prior consideration during the LST decision-making process.
Data variables and definition
We used the regional OHCA registry, which includes all OHCA cases in level 1 and 2 hospitals in Daegu Metropolitan City [7, 8, 12]. We analysed demographic information, including age, sex, and insurance status; arrest characteristics, such as cause of arrest, witness status, bystander CPR, location of arrest, and initial electrocardiogram (ECG) rhythm; comorbidities, including hypertension, diabetes mellitus, heart disease, and cerebrovascular accidents; hospital treatments, including TTM and extracorporeal membrane oxygenation (ECMO); and length of hospital stay. The causes of arrest were classified as medical or non-medical. Non-medical aetiologies included trauma, hanging, drowning, and intoxication. The cut-off date of 3rd February 2018 was defined and divided into groups before and after the implementation of the LSTDA.
Outcome measures
The primary outcome measured was organ donation, specifically brain-dead organ donation. Outcomes were assessed based on hospital records and data from the organ donation centres of the participating hospitals.
Statistical analysis
Demographic characteristics, other variables and organ donation status were compared between the periods before and after the implementation of the LSTDA. For continuous variables, descriptive statistics were presented as medians with interquartile ranges (25th and 75th percentiles). Categorical variables were reported as counts and percentages. The significance of differences between groups was evaluated using the Mann–Whitney U test for continuous variables and Fisher’s exact test for categorical variables. Temporal trends were analysed using the Cochran–Armitage test.
Associations between variables and organ donation outcomes were examined using stepwise logistic regression analysis. This included demographic factors (i.e. sex, age, and comorbidities), arrest characteristics (i.e. witness status, bystander CPR, primary ECG rhythm, location of arrest), and post-resuscitation hospital management (i.e. TTM and ECMO), in addition to the length of hospital stay and LSTDA implementation grouping. The results are expressed as adjusted odds ratios (AOR) and 95% confidence intervals (CIs). All statistical analyses were performed using SAS software version 9.4 (SAS Institute Inc., Cary, NC, USA). Based on a two-sided test, p < 0.05 was considered statistically significant.
Results
A total of 9,741 patients experienced OHCA between 2015 and 2022 in Daegu, 751 of whom were eligible for this study. Among these, 47 patients chose to donate organs: 30 before and 17 after the implementation of the LSTDA (Fig. 1).
The general characteristics of the patients before and after the implementation of the LSTDA are shown in Table 1. In both groups, approximately 80% of the patients who donated organs were aged < 65 years. The most common cause of arrest was medical in both groups, whereas hanging was the most common cause of arrest among those who donated organs. (43.3% before and 52.9% after the LSTDA), respectively.
Among the 751 patients, 47 (30 before the LSTDA and 17 after the LSTDA) underwent organ donation. The median age was significantly lower in the organ donation group at 47 years compared to that in the no organ donation group, which had a median age of 63 years (p < 0.001). The most common cause of arrest in the organ donation group was hanging (22 patients, 46.8%), followed by medical aetiology (34%) and trauma (19.2%). Regarding hospital treatments, TTM was provided to 18 patients (38.3%) in the organ donation group, compared to 172 patients (24.4%) in the no organ donation group (Table 2).
The AOR for organ donation before the LSTDA implementation was 6.12 (95% CI 3.09–12.12). Regarding the cause of arrest, the AOR for organ donation in the non-medical aetiology group compared to that for the medical aetiology group was 8.51 (95% CI 4.19–17.28). The AORs for organ donation in the age groups 40–64 years and 16–39 years compared to that of those ≥ 65 years were 1.58 (95% CI 0.68–3.67) and 3.22 (95% CI 1.24–8.36), respectively (Table 3).
Figure 2 shows the trend of an annual decrease in the number of organ donations (p < 0.001).
Discussion
This study evaluated organ donation status and associated factors in patients with out-of-hospital cardiac arrest. Only 5% of patients donated their organs, and the enforcement of the LSTDA was associated with a reduction in organ donation. In our study, the factors related to organ donation were non-medical causes of cardiac arrest and the implementation of the LSTDA. This study is significant in analysing the current status of organ donation among patients with OHCA in a metropolitan city and identifying related factors after the implementation of the LSTDA, which has not been previously reported in South Korea or globally.
Our findings revealed that the number of organ donors among patients with OHCA was low prior to the implementation of the LSTDA and declined further after the legislation was enacted. There has been an increase in the number of patients choosing EOL and palliative care while refusing LST, which may have led to a decrease in the number of potential organ donors. Baik et al. [13] reported that 39.5% of patients who decided to discontinue LST treatment met the organ donation criteria. This is compounded by the fact that once LST is withheld, maintaining the physiological stability required for organ donation becomes challenging, further limiting opportunities for organ recovery. After the enactment of the LSTDA, potential brain death cases were reported to the Korea Organ Donation Agency, and 193 of these patients signed to withdraw LST. Among them, 156 patients met the brain death criteria and were eligible for organ donation, but only 16 people (12.6%) agreed to organ donation, a percentage much lower than that of the group that did not withdraw LST (38.9%) [14]. The lack of consideration of organ donation before LST determination was proposed as the reason for the low percentage of organ donation. To mitigate the negative impact of the LSTDA on organ donation rates while respecting EOL decisions, several measures can be considered. Creating more flexible guidelines that respect both EOL decisions and organ donation opportunities, enhancing communication between healthcare providers and families, and improving public awareness about the importance of organ donation are crucial. Developing integrated protocols to ensure organ donation is considered after LST decision-making can bridge the gap between EOL care and organ donation [15].
The demand for organ donation and the potential brain death encountered in the ED is increasing [16, 17], highlighting the necessity of emergency physicians’ knowledge and awareness of organ donation [18]. In South Korea, among notifiers of potential brain death, emergency physicians accounted for 5% (114 out of 2,215) in 2021, representing the second largest proportion among physicians [2]. The number of potential brain deaths in South Korea, as notified by emergency physicians, increased from 100 in 2017 to 144 in 2019 and 114 in 2021. Akkas et al. reported that negative attitudes and lack of knowledge about organ donation in society, religious beliefs, and inadequate knowledge of emergency physicians were barriers that hindered organ donation in the ED [19] while Da Silva et al. argued that national and global standardisation of brain death criteria could improve donation [20]. Some studies have reported high knowledge and positive attitudes toward organ donation among emergency physicians [21,22,23]. To improve knowledge and awareness about organ donation, the introduction of standardized education modules and e-learning programmes in training or supplementary training courses, as is done in other countries, should be considered [24,25,26]. Comprehensive education covering the importance of organ donation, the definition and criteria of brain death and circulatory death, recognition of potential donors, and the notification system should be included in these modules. They should also cover legal knowledge, medical knowledge for donor care, and communication skills for discussing organ donation with families. Online e-learning programmes can ensure that education on organ donation is accessible and standardized across different hospitals.
High rates of organ donation are associated with non-cardiac aetiology as a cause of arrest, brain death as a cause of death, and longer arrest times in the USA [27]. Similarly, in our study, organ donation was associated with a non-medical aetiology of cardiac arrest. The non-medical aetiology group was observed to have a high incidence of hypoxic brain injury, and, consistent with previous studies, hypoxic damage was considered a factor related to organ donation [28]. TTM is associated with good neurological recovery, and even in cases of deterioration, it could present an opportunity for organ donation. ECMO is associated with good neurological outcomes in cardiac arrest [29] and a high rate of organ donation. Smalcova et al. reported a correlation between the application of extracorporeal CPR and increased organ donorship [30]. However, in our study, TTM and ECMO were excluded as associated factors through stepwise multiple logistic analysis, which differed from the findings of the previous study.
According to the actual number of deceased organ donors per million population worldwide in the International Registry on Organ Donation and Transplantation in 2021, the USA accounted for 41.6, Spain for 40.8, but South Korea had a much lower rate at 8.56 [31]. The number of patients with cardiac arrest who donated their organs was small; only 47 patients (5%) donated their organs in our study. The International Liaison Committee on Resuscitation Scientific Statement and Katie et al. proposed that organ donation should be managed as an outcome variable for cardiac arrest [1, 32]. Similarly, in South Korea, organ donations should be collected and managed as key outcome variables. Spain significantly increased its donation rate by promoting the identification and early referral of potential donors, actively implementing donations from expanded donor criteria, and facilitating donations after circulatory death [33]. To adapt these practices to fit South Korea’s context and legal framework, it is essential to consider cultural and legal aspects. Additionally, discussions and systems for facilitating donations after circulatory death should be carefully considered, as currently only donation after brain death and limited cases of circulatory death donation are authorized in South Korea.
This study has several limitations. First, this was a retrospective observational study; therefore, there is the possibility of selection bias. Furthermore, the retrospective design limited our ability to directly analyse barriers to organ donation among patients with cardiac arrest and the challenges potentially introduced following the implementation of the LSTDA. Second, organ donation processes and laws pertaining to LST vary internationally. Therefore, generalising these findings across countries with diverse legal frameworks, organ donation procedures, and healthcare systems is challenging. Finally, the inclusion of the COVID-19 pandemic period could have biased the results. Restrictions on hospital visits and prolonged decision-making processes for LST or organ donation during this period, along with the exclusion of COVID-19 infected patients from potential organ donation, may have affected our findings.
Conclusion
After the enactment of the LSTDA in South Korea in 2018, a reduction in organ donation was observed. While the law does not specifically address organ donation, its implementation may have inadvertently affected donation rates by influencing EOL care decisions. We suggest that efforts to improve the perception of organ donation, along with integrating organ donation considerations into the LST decision-making process and managing organ donation as a key variable in OHCA, are necessary.
Data availability
The datasets generated or analysed during the current study are not publicly available because they contain the privacy of each patient but are available from the corresponding author upon reasonable request.
Abbreviations
- AOR:
-
Adjusted odds ratios
- CPC:
-
Cerebral performance category
- CPR:
-
Cardiopulmonary resuscitation
- CI:
-
Confidence Interval
- ECMO:
-
Extracorporeal membrane oxygenation
- EoL:
-
End of Life
- ED:
-
Emergency department
- ECG:
-
Electrocardiogram
- LST:
-
Life-Sustaining Treatment
- LSTDA:
-
Life-Sustaining Treatment Decision Act
- OHCA:
-
Out-of-hospital cardiac arrest
- TTM:
-
Target temperature management
References
Morrison LJ, Sandroni C, Grunau B, Parr M, Macneil F, Perkins GD, et al. Organ donation after out-of-hospital cardiac arrest: a scientific statement from the international liaison committee on resuscitation. Resuscitation. 2023;190:109864.
Korea Organ Donation Agency. KODA Annual Report 2022. Korea Organ Donation Agency. https://www.koda1458.kr/newPr/eBook.do?num=24&idx=23. Accessed 31 July 2024.
Korea Law Information Center. Act on hospice and palliative care and decisions on life-sustaining treatment for patients at the end of life. Korea Law Information Center. https://www.law.go.kr/LSW/eng/engLsSc.do?menuId=2&query=ACT%20ON%20HOSPICE%20AND%20PALLIATIVE%20CARE%20AND%20DECISIONS%20ON%20LIFE-SUSTAINING%20TREATMENT%20FOR%20PATIENTS%20AT%20THE%20END%20OF%20LIFE#liBgcolor0. Accessed 31 July 2024.
Lee DE, Kim H, Park KH, Park SY, Park SM, Jung YH, et al. Analysis of factors affecting emergency physicians’ attitudes toward deceased Organ & tissue donation. J Korean Med Sci. 2021;36:e329.
Akeely YY, Al Otaibi MM, Alesa SA, Bokhari NN, Alghamdi TA, Alahmari MS, et al. Organ donation in the emergency department: awareness and opportunities. Cureus. 2023;15:e49746.
Park SY, Kim H, Park KH, Park SM, Lee DE, Jung YH, et al. Exploring the experiences and perspectives of emergency physicians on brain death organ tissue donation after the life-sustaining treatment decision act. Korean J Transpl. 2022;36:29–36.
Lee DE, Ryoo HW, Moon S, Park JH, Shin SD. Effect of citywide enhancement of the chain of survival on good neurologic outcomes after out-of-hospital cardiac arrest from 2008 to 2017. PLoS ONE. 2020;15:e0241804.
Ahn JY, Ryoo HW, Moon S, Jung H, Park J, Lee WK, et al. Prehospital factors associated with out-of-hospital cardiac arrest outcomes in a metropolitan city: a 4-year multicenter study. BMC Emerg Med. 2023;23:125.
Emergency medical statistics yearbook. National Emergency Medical Center of Korea. https://e-medis.nemc.or.kr/portal/compose/publicationPage.do. Accessed 31 July 2024.
Korea Law Information Center. Organs Transplant Act. Korea Law Information Center. https://www.law.go.kr/LSW/eng/engLsSc.do?menuId=2§ion=lawNm&query=ORGANS+TRANSPLANT+ACT&x=0&y=0#liBgcolor1. Accessed 31 July 2024.
Park H, Jung ES, Oh JS, Lee YM, Lee JM. Organ donation after controlled circulatory death (maastricht classification III) following the withdrawal of life-sustaining treatment in Korea: a suggested guideline. Korean J Transpl. 2021;35:71–6.
Min C, Lee DE, Ryoo HW, Jung H, Cho JW, Kim YJ, et al. Neurologic outcomes of prehospital mechanical chest compression device use during transportation of out-of-hospital cardiac arrest patients: a multicenter observational study. Clin Exp Emerg Med. 2022;9:207–15.
Baik SM, Park J, Kim TY, Lee JH, Hong KS. The future direction of the organ donation system after legislation of the life-sustaining treatment decision act. Ann Transpl. 2021;26:e934345.
Cho WH. Organ donation in Korea in 2018 and an introduction of the Korea national organ donation system. Korean J Transpl. 2019;33:83–97.
Shemie SD, Robertson A, Beitel J, Chandler J, Ferre E, Evans J, et al. End-of-life conversations with families of potential donors: leading practices in offering the opportunity for organ donation. Transplantation. 2017;101(5S Suppl 1):S17–26.
Michael GE, O’Connor RE. The importance of emergency medicine in organ donation: successful donation is more likely when potential donors are referred from the emergency department. Acad Emerg Med. 2009;16:850–8.
Reed MJ, Lua SBH. Uncontrolled organ donation after circulatory death: potential donors in the emergency department. Emerg Med J. 2014;31:741–4.
Lazzeri C, Manuela B, Peris A. Out of hospital cardiac arrest and organ donation: the innovative approach for emergency physicians. Eur J Emerg Med. 2024;31:5–6.
Akkas M, Demir MC. Barriers to brain death notifications from emergency departments. Transpl Proc. 2019;51:2171–5.
Da Silva IRF, Frontera JA. Worldwide barriers to organ donation. JAMA Neurol. 2015;72:112–8.
Kondori J, Ghafouri RR, Zamanzadeh V, Attari AMA, Large SR, Sheikhalipour Z. Emergency medical staffs’ knowledge and attitude about organ donation after circulatory determined death (DCD) and its related factors. BMC Emerg Med. 2021;21:91.
Hickey M, Yadav K, Abdulaziz KE, Taljaard M, Hickey C, Hartwick M, et al. Attitudes and acceptability of organ and tissue donation registration in the emergency department: a national survey of emergency physicians. CJEM. 2022;24:293–9.
Urquhart R, Kureshi N, Dirk J, Weiss M, Beed S. Family and emergency physicians’ knowledge and attitudes toward organ donation and deemed consent: human organ and tissue donation act in Nova Scotia. Can Fam Physician. 2024;70:e20–7.
Coe TM, Chirban AM, McBroom TJ, Cloonan DJ, Brownlee SA, Moses J, et al. Virtual student-transplant patient interactions empower patients and enhance student transplantation knowledge. Am J Surg. 2021;222:1120–5.
Coe TM, McBroom TJ, Brownlee SA, Regan K, Bartels S, Saillant N, et al. Medical students and patients benefit from virtual non-medical interactions due to COVID-19. J Med Educ Curric Dev. 2021;8:23821205211028343.
Hancock J, Shemie SD, Lotherington K, Appleby A, Hall R. Development of a Canadian deceased donation education program for health professionals: a needs assessment survey. Can J Anaesth. 2017;64:1037–47.
Elmer J, Molyneaux BJ, Shutterly K, Stuart SA, Callaway CW, Darby JM, et al. Organ donation after resuscitation from cardiac arrest. Resuscitation. 2019;145:63–9.
Kramer AH, Hornby K, Doig CJ, Armstrong D, Grantham L, Kashuba S, et al. Deceased organ donation potential in Canada: a review of consecutive deaths in Alberta. Can J Anaesth. 2019;66:1347–55.
Lunz D, Calabrò L, Belliato M, Contri E, Broman LM, Scandroglio AM, et al. Extracorporeal membrane oxygenation for refractory cardiac arrest: a retrospective multicenter study. Intensive Care Med. 2020;46:973–82.
Smalcova J, Havranek S, Pokorna E, Franek O, Huptych M, Kavalkova P, et al. Extracorporeal cardiopulmonary resuscitation-based approach to refractory out-of-hospital cardiac arrest: a focus on organ donation, a secondary analysis of a Prague OHCA randomized study. Resuscitation. 2023;193:109993.
International registry in. organ donation and transplantation: IRODaT(international registry on organ donation and transplantation). https://www.irodat.org/?p=database. Accessed 31 July 2024.
Love KM, Brown JB, Harbrecht BG, Muldoon SB, Miller KR, Benns MV, et al. Organ donation as an outcome of traumatic cardiopulmonary arrest: a cost evaluation. J Trauma Acute Care Surg. 2016;80:792–8.
Matesanz R, Domínguez-Gil B, Coll E, Mahíllo B, Marazuela R. How Spain reached 40 deceased organ donors per million population. Am J Transpl. 2017;17:1447–54.
Funding
There was no financial support for this study.
Author information
Authors and Affiliations
Contributions
TCJ, JHK, HJ, S-HL, JP, IHY, and HWR contributed to the data acquisition. DK and DEL contributed to data analysis. HWR, JKK, and DEL contributed to the data interpretation. MJK drafted the manuscript. MJK, JKK and DEL critically revised the manuscript. All authors made substantial contributions to the conception and design of the study, approved the final manuscript for publication, and agreed to be accountable for all aspects of the study, ensuring that any questions related to the accuracy or integrity of any part of the work were appropriately investigated and resolved.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was reviewed and approved by the Institutional Review Board of Kyungpook National University Chilgok Hospital (approval no: 2019-01-008), which waived the need for individual consent. The study adheres to the ethical guidelines of the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Kim, M.J., Lee, D.E., Kim, J.K. et al. Impact of the life-sustaining treatment decision act on organ donation in out-of-hospital cardiac arrests in South Korea: a multi-centre retrospective study. BMC Med Ethics 25, 93 (2024). https://doi.org/10.1186/s12910-024-01090-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12910-024-01090-4