Abstract
Background
Informed consent is a process in which a healthcare provider obtains permission from an individual prior to surgery. Patient satisfaction with the informed consent process is one of the main indicators of healthcare service quality. This study aimed to assess patient satisfaction with surgical informed consent at Jimma Medical Center, Ethiopia, in 2020.
Methods
A facility-based cross-sectional study was conducted from April 1 to June 30, 2020, at Jimma Medical Center. Face-to-face interviews were conducted using structured questionnaires. A systematic sampling technique was used to select the study participants. The collected data were coded, entered into Epi data version 3.1, and analyzed using SPSS version 25. Bivariate and multivariate regression analyses were performed to determine the association between patient satisfaction and socio-demographic and facility-related factors. In multivariate regression, predictors with a P-value of < 0.05 were considered statistically significant.
Results
Totally 372 study participants were interviewed with a response rate of 97.8%. Nearly two-fifths (43%) of patients were satisfied with surgical informed consent. Living in an urban area (AOR: 2.279, 95% CI 1.257–4.131), having current referred history (AOR: 1.856, 95% CI 1.033–3.337), consent form version (AOR: 2.076, 95% CI 1.143–3.773), time spent on the provision of informed consent (AOR: 5.227, 95% CI 2.499–10.936) and having better patient-health providers relationship (AOR: 5.419, 95% CI 3.103–9.464) predictors were positively associated with patient satisfaction.
Conclusion
Patient satisfaction with the surgical informed consent process was relatively low. Therefore, Health care professionals need to emphasize a way of delivering informed consent, patients' needs and obey a standard informed consent to improve patient satisfaction.
Similar content being viewed by others
Introduction
Surgical informed consent is one vital part of preoperative care [1,2,3]. Informed consent is the process by which a healthcare provider obtains permission from an individual before delivering therapy, treatment, or surgery [4]. The process of informed consent involves more than signing a prescribed form [5]. Providing proper surgical informed consent to patients who have undergone surgery makes them satisfied [6,7,8].
Patient satisfaction is a major indicator of quality of healthcare services [9]. Patient satisfaction is the degree to which a patient meets the expectations of ideal care based on their perception of the actual care received [10, 11]. Patient satisfaction during informed consent increases when written informed consent is provided, combined with verbal informed consent during the preoperative period [12]. Satisfied patients are more likely to obey treatment, take an active role in their care, continue using health care services, voluntarily participate in decision making, and stay within a healthcare provider [13].
Previous studies have reported that the level of patient satisfaction with informed consent varies between countries. The studies conducted in Pakistan, Israel, Netherland, and Switzerland showed that patient satisfaction with surgical informed consent ranged from 49 to 95% [14,15,16,17]. In contrast, patient satisfaction with the provision of surgical informed consent in African countries is relatively low. The studies conducted in Rwanda, Botswana, Eritrea, and Hawassa, Ethiopia revealed that the overall patient satisfaction with surgical informed consent ranged 36.9–67.4% [18,19,20,21].
patients who were satisfied with their health care services showed greater adherence to treatment plans, fewer hospital readmissions, and greater intention to keep follow-up appointments; patients treated at the hospital with higher patient satisfaction scores experienced lower rates of postoperative mortality, and death after any complication [22].
Different studies revealed that factors affecting patient satisfaction in preoperative care services include, lack of a standard consent form, lack of readiness to deal with urgent medical conditions, overcrowding of the surgical unit, younger age, low literacy level, Patient knowledge and understanding of surgery, patients who underwent elective surgery, patients who had experience with disease or operation, lack health care provider experience with SIC, heavy workload for health care providers, delay in requesting consent, time spent on informed consent provision and patient-doctor relationship [7, 20, 23,24,25,26,27,28,29,30].
Worldwide, different attempts have been made to increase health care quality by improving patient satisfaction. Recent studies have recognized perioperative surgical home (PSH) as a way of working with patients to optimize their condition before surgery, the intraoperative phase, the immediate postoperative phase, and post-discharge [31]. In Ethiopia, efforts have been made to enhance patient satisfaction through informed consent. The effort included; preparing Medico-legal guidelines, incorporating Medical ethics for doctors in the Curriculum, and provision of Compassionate, Respectful, and Caring health care providers are already commenced [32]. However, it doesn’t provide adequate results to enhance patient satisfaction with the surgical procedures. It has been confirmed; that litigation issues for healthcare providers increase over time [33].
Previous studies in Ethiopia have been limited to patient satisfaction with informed consent. Therefore, this study aimed to assess patient satisfaction with the provision of surgical informed consent at Jimma Medical Center, Jimma, Ethiopia.
Methods
Study design and setting
This cross-sectional study was conducted at Jimma Medical Center, Jimma, Ethiopia. Jimma Medical Center is a referral hospital in Southwest Ethiopia. It is a teaching tertiary hospital with four major clinical departments including internal medicine, surgery, pediatrics, and gynecology/obstetrics; and other clinical departments, dentistry, ophthalmology, Orthopedics, psychiatry, Reproductive health center, dermatology, and Antiretroviral therapy (ART) clinics. The obstetrics and gynecology ward had 76 beds available for postoperative care. Approximately 1,461 and 900 patients underwent obstetric and gynecological-related surgery within the past six months respectively (previous 6-month report). A total of 787 patients underwent surgery within two months. The study period was from April 1 to June 30, 2020.
Study participants
All women who underwent obstetric and gynecological surgeries were included in the study. Women who underwent obstetric and gynecological surgeries during the study period were selected as the study population.
Inclusion and exclusion criteria
Women who underwent Ob-Gyn surgery and those aged ≥ 18 years were included in this study. However, those who were critically ill and had known psychiatric illnesses were excluded.
Sample size determination and technique
The sample size was determined using the single population proportion formula by considering 62% proportion (P) which took from research conducted in Hawassa [21]; with a 95% confidence interval (1.96); α = 0.05 and 5% marginal of error. By adding a non-response rate of 5%, the final sample size was 380. A systematic sampling technique was employed to select study participants from a total of 787 two-month surgical cases after determining the interval (K value). The k-value was determined by dividing the total two-month surgical case (787) by the final sample size (380) which was approximately 2. The first study participant was selected using a simple random technique from the first two individuals and the second participant was chosen every two intervals from the registration book until the final sample size was reached.
Data collection tool and procedure
Data were collected using a structured closed-ended questionnaire. The data collection tool was adapted from different studies developed for similar purposes [2, 15]. The questionnaires have six parts. The first part about general socio-demographic characteristics consists of 8 items, the second part deals with patient-related factors consists of 7 items; the third one about service-related factors consists of 8 items, and the fourth part deals with the patient-healthcare relationship consisting of 9 items, adopted from validation of the patient to doctor relationship questionnaire (PDRQ-9) study conducted in German [34], the fifth part deals with patients’ knowledge of surgical informed consent and the last part deals with satisfaction with informed consent, it measured using 10 items with a five-point Likert scale option (ranging from 1 completely dissatisfied to 5 completely satisfied). Two BSc nurses and one MSc nurse were involved in the data collection and supervision respectively. Data were collected using a face-to-face interview.
Data quality management
The questionnaire was initially prepared in English then translated into the local languages (Afaan Oromo and Amharic) and then translated back into English. Prior to the actual data collection, a pretest was conducted on 5% of the total sample (19 women) at Shenen Gibe Hospital. Appropriate corrections and mandates were made to the questionnaire. The one-day training was provided to the supervisor and data collectors. During the data collection period, the data were checked for completeness and consistency. Any error, ambiguity, incompleteness, or other problems were addressed through communication with data collectors before the beginning of the next day's data collection activities. The reliability of the patient satisfaction tool was confirmed using Cronbach’s Alpha, which was 0.83.
Data analysis procedure
The collected data were coded and entered into Epi data version 3.1 and exported into SPSS version 25. The Hosmer and Lemeshow test was performed to confirm model fitness. Bivariate and multivariate analyses were performed to compare the satisfaction of surgical informed consent with predictors. In bivariate logistic regression, the variables which had a P-value < 0.25 were considered candidate variables for multivariable logistic regression. In multivariable regression, variables with a P-value < 0.05 were considered statistically significant with the outcome variable. Finally, the results were narrated using text, tables, figures, and graphs.
Ethical consideration
Ethical clearance was obtained from Institutional Review Board of Jimma University (IRB Ref No: 000,165/2020). Permission letter was obtained from Jimma Medical Center. The purpose and importance of the study were explained and verbal informed consent was secured. Confidentiality was maintained at all level of the study. Participants’ involvement in the study was on voluntary bases and that they could withdraw at any time if they want. All the information given by the respondents was used for research purposes only.
Results
Socio-demographic characteristics
A total of 372 study participants were involved in the study with a response rate of 97.8%. The majority 310 (83.3%) of study respondents were married and 324 (87.1%) were aged < 35 years. The majority 182 (48.9%) were Muslim, and 267 (70.1%) study participants were Oromo. The majority of 242 (65.1%) participants were living in Urban, 168 (45%) were housewives, 291 (78.2%) were literate and nearly half 47.1% had less than 1500 EB monthly income (Table 1).
Patient-related factors
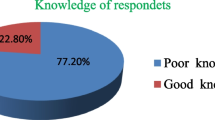
More than half of the respondents (52.2%) were multipara and three-fourths of study participants (74.5%) had undergone an emergency surgical procedure. The majority of study participants 319 (86%) underwent operation with a reason of pregnancy-related cases followed by 20 (5.4%) gynecological cancers, 12(3.2%) gynecological benign tumors, and 11 (3%) pelvic organ disorders. One hundred three (27%) respondents had a previous history of surgery, of which 60 (58.3%) of them had once a surgical history while the remaining 43 (41.7%) patients had more than one surgical history. A majority (77.1%) of women had poor knowledge, and the remaining one-quarter (22.9%) of them had good knowledge of ward surgical informed consent (Table 2).
Service-related factors
Two hundred fifty-eight (69.4%) study participants were referred from other health facilities. Nearly two-thirds, 62.9% of women were responding that the consent form was written in their mother tongue. The majority of 302 (81.2%) study participants reported that surgical informed consent was obtained by GP/resident, followed by obstetrician-gynecologists 44 (11.8%) and nurse/midwives 26 (7%). More than half of 208 (56%) respondents reported that they received informed consent counseling immediately before surgery. The consent form was signed by the patients themselves 352 (94.6%) while the remaining 20 (5.4%) were signed by their relatives (Table 3).
Patient- health provider relationship
Women were asked to assess the patient-healthcare providers’ relationship while they provided informed consent. Out of the total interviewed study participants, 179 (48%) women had a good patient health providers relationship.
Patient satisfaction with surgical informed consent
Women have scored the highest satisfaction value on three satisfaction measurement items; i.e. awareness of the benefit of operation, involvement in the discussion about the operation, and involvement in decision making accounting for 79.1%, 89.5%, and 91.2% respectively (Table 4).
Women were asked to assess their level of satisfaction with the SICs they had received prior to their surgical procedure on a five-point scale. The findings of this study showed that 160 (43%) respondents were satisfied and the remaining 212 (57%) respondents were dissatisfied with the informed consent provision.
Factors associated with Satisfaction of informed consent
In bivariate logistic regression, variables with a P-value less than 0.25 were considered as candidate variables for multivariate logistic analysis. These variables were residence, marital status, occupation, parity, type of surgery, referred history from another health facility, the version of a written consent form, timing of consent, time taken to provide informed consent, the person signing the consent form, profession who request for the operation, knowledge of SIC and patient to healthcare provider relationships (Table 5). However, in the multivariable regression, candidate variables were entered into the regression using the backward elimination method; and only five predictors included:- residence, referred history from another hospital, Version of a written consent form, time spent while providing SIC, and patient-healthcare provider relationship were statistically significant with patient satisfaction (Table 6).
The results of multivariable logistic regression analysis showed that the respondents who came from urban settings were 2.2 times (AOR: 2.279, 95% CI 1.257–4.131) more likely satisfied than those who came from rural residences. Respondents who had no referred history from other health settings were 1.8 times (AOR: 1.806, 95% CI 1.014–3.215) more likely satisfied with the provision of informed consent compared to those who had referred history from another health facility.
Women who received written informed consent with mother tongue were two times (AOR: 2.572, 95% CI 1.422–4.655) more likely satisfied with informed consent than their counterparts. Patients who had received information about surgical informed consent for 10 min duration were 5 times (AOR: 5.726, 95% CI 2.755–11.900) more likely satisfied with the provision of informed consent than patients who have received the information for less than 5 min. Furthermore, women who had a good patient-health care providers relationship were 7 times (AOR: 7.752, 95% CI 4.402–13.652) more likely satisfied with the informed consent process than-their-counterpart.
Discussion
This study reported that women's satisfaction with surgical informed consent was 43% (95% CI 38.2% to 48.7%). The finding of this result is almost similar with studies conducted in Egypt and Eritrea which accounted for 48.4% and 45% of patients satisfied with SIC provision respectively [20, 36]. However, it is lower than studies conducted in the Netherlands, Israel, Hawassa-Ethiopia, Rwanda, and Pakistan on patient satisfaction with informed consent which accounted for 80.8%, 80%, 62.1%, 67.4%, and 48.9% respectively [14, 16, 17, 19, 21]. The discrepancy might be due to variations in health care service quality and patient flow rate.
The findings of this study showed that women from urban residences were two times more likely satisfied with the informed consent than respondents who came from rural residences. This was supported by a study conducted in Eritrea; patients who came from urban settings were more satisfied with informed consent than those who came from a rural setting [20]. This might be because urban living populations have a better chance of receiving health care services promptly and they are nearer to hearing health-related information.
According to this study; patients who hadn’t referred history from other health settings were 1.8 times more likely to be satisfied than those who had referred history from another health facility. A possible reason might be that patients who had a referred history from other health facilities have been worried about their case or diseases because their case was beyond the service provided by the local health facility and they came to seek further investigation and intervention. They also had to be anxious and stressed in the new hospital environment and healthcare providers since they came from another hospital.
Moreover, women's satisfaction with surgical informed consent was statistically significant for the language of written informed consent. Women who received written informed consent with mother tongue were twice more likely to be satisfied than their counterparts. This is supported by a study conducted in Switzerland in which the consent form written in a simple layman's language and wording improves patients' ability to understand the information provided and is strongly associated with patient satisfaction [15]. Simply providing information doesn't guarantee that a patient understands what healthcare providers tell them unless we provide the information within mother tongue because they have different levels of understanding [21].
Furthermore, the duration of time spent during provision surgical informed consent was positively associated with women's satisfaction with surgical informed consent. Patients who had received information about surgical informed consent for longer than 10 min were 5 times more likely to be satisfied than patients who received the information for less than 5 min. This is supported by a study conducted in Nigeria revealed that; time spent explaining surgical procedures and the possible outcome could calm patients and reduce their level of anxiety [37]. This might be due to the adequate time provided to women during the informed consent process allowing them to easily understand the information provided. When health care providers explained the proposed surgery with adequate time, the women coped from anxiety and have been satisfied.
Additionally, women's satisfaction with informed consent was significantly associated with the patient to health care provider relationship. According to this study, the respondents who had a good relationship with health care providers were seven times more likely to be satisfied with the informed consent process than their counterparts. This is supported by a study conducted in the Netherland which reported that a better-perceived patient-to-doctor relationship was related to higher patient satisfaction [26]. Similarly, a study conducted in Australia revealed that the proper delivery of patient-centered health care services with effective communication skills resulted in trust between the patient and healthcare provider and improved patient satisfaction [38].
Strength and Limitation of the study
As strength, new study or investigation for the current study setting and had a high response rate. As a limitation this study was conducted solely on women who underwent obstetrics and gynecology-related procedures, it didn't address major surgery, so it might have a generalizability issue. The social desirability bias is also limitation of this study.
Conclusion
Women's satisfaction with the provision of surgical informed consent was inadequate. Residence, written consent form version, time spent, applied the recommended component of SIC, and patient to healthcare provider relationship were significant predictors of women's satisfaction with informed consent. Healthcare providers need to emphasize following standard informed consent guidelines and give enough time while the provision surgical informed consent to patients. Moreover, all concerned bodies have to work collaboratively to make proper SIC service and enhance patient satisfaction.
Availability of data and materials
The datasets used for this study could be available from the corresponding author upon reasonable request.
Abbreviations
- AOR:
-
Adjusted odd ratio
- COR:
-
Crude odd ratio
- JMC:
-
Jimma medical center
- SIC:
-
Surgical informed consent
References
Leclercq WKG, Keulers BJ, Scheltinga MRM, Spauwen PHM, Van Der Wilt GJ. A review of surgical informed consent: past, present, and future. World J Surg. 2010;34(7):1406–15.
Rogers P, Lloyd S, Shetty D, Newell P, Gay D. Measuring patient satisfaction with the ct consent process: the comrade outcome measure. Imaging Med. 2013;5(6):505–13.
Meaza B. Perception about informed consent for surgical procedures as part of patient safety practice among service providers and patients in Addis Ababa hospitals. 2017
Lovegrove C, Mantori S, Shrotri N. Patient satisfaction with informed consent on the day of surgery. Int J Surg. 2017;2017(47):S96.
Lee AV, Moriarty JP, Borgstrom C, Horwitz LI. What can we learn from patient dissatisfaction? an analysis of dissatisfying events at an academic medical center. J Hosp Med. 2010;5(9):514–20.
Katsafourou PA, Gbolade BA. Informed consent for elective and emergency surgery: questionnaire study [2]. BJOG An Int J Obstet Gynaecol. 2005;112(10):1454.
Siddiqui FG, Shaikh JM, Memon MM. An audit of informed consent in surgical patients at a university hospital. J Ayub Med Coll Abbottabad. 2010;22(1):133–5.
Hallock JL, Rios R, Handa VL. Patient satisfaction and informed consent for surgery. Am J Obstet Gynecol [Internet]. 2017;217(2):181. https://doi.org/10.1016/j.ajog.2017.03.020.
Warner DS, Sc B, Giannaris S, John R. Patient-satisfaction measures in anesthesia. Science. 2013;2:555.
Aragon SJ, Gesell SB. A patient satisfaction theory and its robustness across gender in emergency departments: a multigroup structural equation modeling investigation. Am J Med Qual. 2003;18(6):229–41.
Mira JJ, Tomás O, Virtudes-Pérez M, Nebot C, Rodríguez-Marín J. Predictors of patient satisfaction in surgery. Surgery. 2009;145(5):536–41.
Trinh LN, Fortier MA, Kain ZN. Primer on adult patient satisfaction in perioperative settings. Perioper Med. 2019;8(1):1–13.
Getachew G, Berhe D. Why patients are dissatisfied on nursing care services at menelik hospital, addis ababa. J Innov Assoc. 2016;5(6):850–60.
Abolfotouh MA, Adlan AA. Quality of informed consent for invasive procedures. Int J Gen Med. 2012;5:269–75.
Ghulam AT, Kessler M, Bachmann LM, Haller U, Kessler TM. Patients’ satisfaction with the preoperative informed consent procedure in Switzerland. Mayo Clin Proc. 2006;81(3):307–12.
Bedforth NM, Hardman JG. Patient satisfaction with perioperative care among patients having orthopedic surgery in a university hospital. Science. 2010;3:49–55.
Jawaid M, Farhan M, Masood Z, Husnain SMN. Preoperative informed consent : is it truly informed ? Iran J Publ Heal. 2014;41:25–30.
Ar B, Me H, Vdh H. Patient satisfaction with the quality of care in a primary health care setting in Botswana. Science. 2011;53(2):170–5.
Leóntine I. Dissertation Patients Satisfaction with Perioperative Care at Oshen Fing Faisal Hospital By. 2017
Andemeskel YM, Elsholz T, Gebreyohannes G, Tesfamariam EH. Patient satisfaction with peri-operative anesthesia care and associated factors at two National Referral Hospitals: a cross sectional study in Eritrea. BMC Health Serv Res. 2019;19(1):1–20.
Teshome M, Wolde Z, Gedefaw A, Tariku M, Asefa A. Surgical informed consent in obstetric and gynecologic surgeries: experience from a comprehensive teaching hospital in Southern Ethiopia. BMC Med Ethics. 2018;19(1):1–9.
Sacks GD, Lawson EH, Dawes AJ, Russell MM, Maggard-Gibbons M, Zingmond DS, et al. Relationship between hospital performance on a patient satisfaction survey and surgical quality. JAMA Surg. 2015;150(9):858–64.
Ochieng J, Ibingira C, Buwembo W, Munabi I, Kiryowa H, Kitara D, et al. Informed consent practices for surgical care at university teaching hospitals : a case in a low resource setting. BMC Med Ethics. 2014;15(40):1–5.
San NEM, Gómez-Alonso D, Trigueros JM, Quiroga J, Gualis J, Vaquero C. Readability of surgical informed consent in Spain. Cirugía Española (English Ed). 2014;92(3):201–7.
Gebremedhn EG, Lemma GF. Patient satisfaction with the perioperative surgical services and associated factors. Gondar Pan Afr Med J. 2017;27:1–14.
de Waard CS, Poot AJ, den Elzen WPJ, Wind AW, Caljouw MAA, Gussekloo J. Perceived doctor-patient relationship and satisfaction with general practitioner care in older persons in residential homes. Scand J Prim Health Care [Internet]. 2018;36(2):189–97. https://doi.org/10.1080/02813432.2018.1459229.
Jennifer LH, Rebeca R, Victoria LH. Patient satisfaction and informed consent for surgery. Am J Obstet Gynecol. 2017;2:181.e7.
Aldossari SH, Alfayez SS, Ibrahim R, Mutlaq A, Alturki DI, Khalid A. The relationship between quality of informed consent and perioperative care, and patient satisfaction: a tertiary- care hospital ’ s experience. Science. 2017;3(9):107–12.
Xesfingi S, Vozikis A. Patient satisfaction with the healthcare system: assessing the impact of socio- economic and healthcare provision factors. BMC Health Serv Res. 2016;2:1–7.
Sulaiman A, Ayyuba R, Diggol I, Haruna I. Knowledge, attitude and perception of patients towards informed consent in obstetric surgical procedures at Aminu Kano Teaching Hospital. Niger J Basic Clin Sci. 2015;12(1):45.
Kwon MA. Perioperative surgical home: a new scope for future anesthesiology. Korean J Anesthesiol. 2018;71(3):175–81.
Ethiopian medical association. Medicoethico Legal.Pdf. 2016
Medical Malpractice_Unethical Medical Treatment-Legal Guides-Avvo
Zenger M, Schaefert R, Van Der Feltz-Cornelis C, Brähler E, Häuser W. Validation of the patient-doctor-relationship Questionnaire (PDRQ-9) in a representative cross-sectional German population survey. PLoS ONE. 2014;9(3):1–8.
Nurhusien YAN, B H. Knowledge and perception of surgical informed consent and associated factors among adult surgical patients in Gondar University Comprehensive and Specialized Hospital , Ethiopia. 2018;1–33
Mohamed AM, Ghanem MA, Kassem AA. Knowledge, perceptions and practices towards medical ethics among physician residents of University of Alexandria hospitals, Egypt. East Mediterr Heal J. 2012;18(9):935–45.
Parvin R. & Shahjahan, M. KNowledge, attitude, and practice of E-health among doctors working at selected private hospitals in Dhaka, Bangladesh Rehana Parvin BPT, MPH, Md Shahjahan MCPS, MD. 2016;1–11
Chandra SMM. Trust and communication in a doctor-patient relationship. Healthc Commun. 2018;3(336):1–6.
Acknowledgements
First, we would like to give our special thanks to Jimma University for its contribution to financial support. Secondly, our heartfelt thanks go to Jimma Medical Center staffs, data collectors, and study participants.
Funding
The fund for this research was obtained from Jimma University, Jimma, Ethiopia. The role of the funder was only to provide the fund needed for this study. The funder had no involvement in the study design, data collection, publication decision or manuscript writing.
Author information
Authors and Affiliations
Contributions
TB: Develops proposal, prepared the manuscript, reviewed, edited the manuscript, statistically analyzed and interpreted. AT: Develops proposal, prepared the manuscript, reviewed, and edited the manuscript, analyzed and interpreted the data, discussed the findings of the study, and drafted the manuscript. YB: Develops proposal, prepared the manuscript, reviewed, and edited the manuscript, analyzed and interpreted the data, discussing the findings of the study. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by Institutional Review Board of Jimma University (IRB Ref No: 000,165/2020). Permission letter was obtained from Jimma Medical Center. The purpose and the importance of the study were explained and verbal informed consent was secured. Confidentiality was maintained at all level of the study. Participants’ involvement in the study was on voluntary bases and that they could withdraw at any time if they want. All the information given by the respondents was used for research purposes only. Confidentiality and privacy was maintained by anonymously of the respondents during data collection procedure.
Consent of Publication
Not applicable.
Competing interests
The authors declared that there is no competing interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Biyazin, T., Taye, A. & Belay, Y. Patient satisfaction with surgical informed consent at Jimma Medical Center, Ethiopia. BMC Med Ethics 23, 103 (2022). https://doi.org/10.1186/s12910-022-00841-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12910-022-00841-5