Abstract
Background
Herb-drug interactions may result in increased adverse drug reactions or diminished drug efficacy, especially for drugs with a narrow therapeutic index such as warfarin. The current study investigates the effects of sodium ferulate for injection (SFI) on anticoagulation of warfarin from aspects of pharmacodynamics and pharmacokinetics in rats and predicts the risk of the combination use.
Methods
Rats were randomly divided into different groups and administered single- or multiple-dose of warfarin (0.2 mg/kg) with or without SFI of low dose (8.93 mg/kg) or high dose (26.79 mg/kg). Prothrombin time (PT) and activated partial thromboplastin time (APTT) were detected by a blood coagulation analyzer, and international normalized ratio (INR) values were calculated. UPLC-MS/MS was conducted to measure concentrations of warfarin enantiomers and pharmacokinetic parameters were calculated by DAS2.0 software.
Results
The single-dose study demonstrated that SFI alone had no effect on coagulation indices, but significantly decreased PT and INR values of warfarin when the two drugs were co-administered (P < 0.05 or P < 0.01), while APTT values unaffected (P > 0.05). Cmax and AUC of R/S-warfarin decreased but CL increased significantly in presence of SFI (P < 0.01). The multiple-dose study showed that PT, APTT, INR, and concentrations of R/S-warfarin decreased significantly when SFI was co-administered with warfarin (P < 0.01). Warfarin plasma protein binding rate was not significantly changed by SFI (P > 0.05).
Conclusions
The present study implied that SFI could accelerate warfarin metabolism and weaken its anticoagulation intensity in rats.
Similar content being viewed by others
Background
Herbal medicines are widely used as complementary and alternative therapy in clinical practice worldwide. The combined utilization of herbs and drugs is common, but herb-drug interactions may induce unfavorable clinical outcomes, especially for the drugs with a narrow therapeutic index such as warfarin [1, 2].
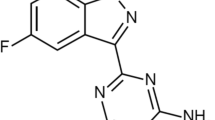
Sodium ferulate injection (SFI) is an important complementary and alternative therapy for patients with vascular diseases including coronary heart diseases, atherosclerosis, cerebrovascular diseases, glomerular diseases, and vasculitis [3,4,5]. Ferulic acid (4-hydroxy-3-methoxy cinnamic acid, FA), an organic monophenolic phytochemical, is the major active ingredient of SFI. FA is present in many herbal medicines such as Ligusticum chuanxiong Hort., Angelica sinensis (Olive.) Diels, Equisetum hyemale L., Cimicifugae heracleifolia Kom., Picrorhiza scrophulariiflora Pennell, Lycium chinense Mill. and Ziziphus jujuba Mill., etc. [5, 6]. Sodium ferulate (Fig. 1), the sodium salt of FA, is mostly used as herbal product due to its high solubility. FA is reported to have a wide range of pharmacological effects including anti-oxidation, anit-hyperlipidemia, anti-atherosclerosis and anti-thrombotic effects [4, 7, 8]. Li et al. explored the influence of sodium ferulate in myocardial ischemic rats by intravenously injecting rats with sodium ferulate. The results showed sodium ferulate can inhibit ischemia reperfusion injury and improve left ventricular remodeling of rats due to its antioxygenation effects and upregulation of miR-133a which has anti-hypertrophy and anti-fibrosis functions [9]. Sodium ferulate can also protect cardiac function of diabetes rats by increasing superoxide dismutase activities and nitric oxide levels and inhibiting oxidative stress both in plasma and myocardium [10]. FA has the potential to prevent and treat liver fibrosis via inhibition of transforming growth factor -β1/Smad pathway in SD rats and human hepatic stellate cell line LX-2 [11]. A study on Institute of Cancer Research mice proved that FA can inhibit platelet aggregation induced by platelet agonists including adenosine diphosphate, thrombin, collagen, and arachidonic acid in a dose-dependent manner [12].
The use of SFI for the treatment of coronary heart disease has been reported in the literatures and presented to be efficient [13,14,15,16]. Moreover, the meta-analysis of 36 studies (with 3207 patients) shows that SFI combined with conventional drugs can improve clinical effectiveness for patients with coronary heart disease [17]. As SFI becomes increasingly used, it is necessary to study its interactions with other drugs, especially in combination with high-risk drugs with narrow therapeutic windows such as warfarin to avoid adverse herb-drug interactions. Warfarin can be prescribed to patients with vascular diseases that increase the likelihood of thromboembolic events. The combined effect of SFI and warfarin has not been studied yet, and the interaction between them remains unknown.
Warfarin has been the most commonly prescribed oral anticoagulants worldwide ever since its first approval in 1954 [18]. Even with the spread of novel oral anticoagulants, warfarin is still irreplaceable in antithrombotic therapy, especially in valvular atrial fibrillation (AF) patients with prosthetic heart valves or with rheumatic mitral stenosis [19, 20]. Warfarin is composed of two optically active isomers, R-warfarin and S-warfarin, which are metabolized by different cytochrome P450 (CYP450) enzymes. S-warfarin is mainly metabolized by CYP2C9 whereas R-warfarin is mainly metabolized by CYP1A2 and CYP3A4 [21, 22]. A major challenge for warfarin usage is its narrow therapeutic window, with an effective concentration range of 1.8–2.6 µg/mL, which is associated with adverse events including bleeding events due to over-anticoagulation or thrombotic disorders due to under-anticoagulation [23,24,25,26]. Warfarin is susceptible to various exogenous factors including concomitant drugs and has the potential to interact with many drugs, medicinal plants and food, which makes close monitoring more necessary [27]. International normalized ratio (INR), which quantifies coagulation activity provides an appropriate way to monitor effectiveness, safety, and anticoagulation management of warfarin. The optimal INR target of warfarin is generally between 2.0 and 3.0. When INR < 2.0, the therapeutic effect may not be effectively achieved, and thrombosis may occur. When INR > 4.0, patients are at increased risk of over-anticoagulation even bleeding [20, 28].
Both SFI and warfarin have anti-thrombotic pharmacological effects and have been widely used in patients with relative vascular diseases. CYP450 isoenzymes involved in warfarin metabolism mainly include CYP1A2, CYP2C9 and CYP3A4, while FA has an inducing effect on the activity of CYP2C9 and CYP3A4 [29]. Therefore, SFI may influence effectiveness of warfarin by affecting its pharmacodynamics (PD) and pharmacokinetics (PK) when co-administered.
Herb-drug interactions call for attention and research for better treatment and preventing potential adverse events. To better understand herb-drug interactions and relative mechanisms, murine experiments are often used in researches. Some researches have been conducted concerning SFI-drugs or herb-warfarin interactions [5, 30]. In streptozotocin-induced diabetic mice, combination of FA with metformin can significantly reduce blood sugar level over either individual treatment [31]. Ginkgo biloba L. extract, a popular herbal ingredient which is widely applied for peripheral arterial diseases and cognitive dysfunction, can decrease warfarin effectiveness via induction of hepatic CYPs by its active ingredient bilobalide in mice [32]. Shenxiong glucose injection is the preparation containing water extracts of Salvia miltiorrhiza Bge. and ligustrazine hydrochloride. Animal studies showed that Shenxiong glucose injection could improve the blood concentration of warfarin by inhibiting CYP2C11 in rats [33]. Herba erigerontis injection could increase prothrombin time (PT) and INR values of rats co-administered with warfarin and decrease plasma protein binding rate of warfarin in rats [34].
This article systematically studied the effect and mechanism of SFI on the anticoagulation of warfarin from the perspectives of PD and PK to clarify whether and how SFI influences the anticoagulation intensity of warfarin, which has not been reported before. The current study would provide a foundation to predict risks for the combined use of SFI and warfarin and thereby improve medical therapeutic effect and safety.
Methods
Chemicals and reagents
SFI was supplied by Harbin Medisan Pharmaceutical Co., Ltd. (Harbin, China). Warfarin was obtained from Shanghai Xinyi Jiufu Co., Ltd (Shanghai, China). Standards of warfarin sodium and methyclothiazide were purchased from National Institutes for Food and Drug Control (Beijing, China). R/S-warfarin were supplied by Toronto Research Chemicals (Toronto, Canada). Reagents of PT and activated partial thromboplastin time (APTT) were provided by Shanghai Sun Biological Technology Co., Ltd (Shanghai, China). Methanol and acetonitrile were chromatographic grade.
Experimental animals
Male Wistar rats weighing 200 ± 20 g were supplied by the Animal Center of the Second Affiliated Hospital of Harbin Medical University (Harbin, China), which was accredited by the Institutional Animal Care and Use Committee (IACUC). All procedures complied with the National Society for Medical Research and Guidelines for the Care and Use of Laboratory Animals. Rats were raised in standard cages under 12:12 h light-dark cycle with sufficient food and water. After the last blood collection procedure, rats were injected sodium pentobarbital (120 mg/kg) by tail vein for euthanasia.
Animal treatment of single-dose warfarin administration
Forty-eight Wistar rats were randomly divided into six groups with eight animals in each group: blank control group, low dose SFI group, high dose SFI group, warfarin control group, warfarin + low dose SFI group, warfarin + high dose SFI group. Rats in the blank control group and warfarin control group were intraperitoneally injected with normal saline for 14 consecutive days, while rats in low dose SFI group, high dose SFI group, warfarin + low dose SFI group and warfarin + high dose SFI group were intraperitoneally injected SFI (8.93 mg/kg or 26.79 mg/kg) for 14 days respectively. On day 8, the rats in the warfarin control group, warfarin + low dose SFI group and warfarin + high dose SFI group were treated with warfarin by oral gavage (0.2 mg/kg), and rats in the blank control group, low dose SFI group and high dose SFI group were given an equal volume of normal saline, respectively.
Animal treatment of multiple-dose warfarin administration
Wistar rats were randomly divided into warfarin control group, warfarin + low dose SFI group, warfarin + high dose SFI group with eight rats in each group and twenty-four rats totally. All rats were given warfarin (0.2 mg/kg) by oral gavage for 8 consecutive days. Rats in warfarin + low dose SFI group and warfarin + high dose SFI group were intraperitoneally injected SFI (8.93 mg/kg, 26.79 mg/kg) for 4 consecutive days from the 5th day, respectively, and rats in the warfarin control group were administrated normal saline with an equal volume by intraperitoneal injection.
Animal treatment of the effects of SFI on warfarin plasma protein binding rate
Thirty-two Wistar rats were randomly divided into the warfarin control group, warfarin + low dose SFI group, warfarin + medium dose SFI group, warfarin + high dose SFI group. For 8 consecutive days, rats in warfarin control group were given an equal dose of normal saline, and rats in warfarin + low dose SFI group, warfarin + medium dose SFI group, warfarin + high dose SFI group were given SFI (8.93 mg/kg, 17.86 mg/kg, 26.79 mg/kg), respectively. On day 8, rats in all groups were given intragastric administration of warfarin (0.2 mg/kg). 1.5 h later, blood was taken from the orbit and subjected to ultrafiltration or other tests. The concentration of warfarin was measured with ultra-high-performance liquid chromatography-tandem mass spectrometry (UPLC–MS/MS).
Pharmacodynamic study
In the single-dose study, blood samples (100 µL) were collected from the retinal venous plexus of the four groups of rats at 0, 4, 8, 12, 24, 36, 48, 72, 96, 120, and 144 h after warfarin administration, respectively. In the multiple-dose study, blood samples (100 µL) of rats from the warfarin control group, warfarin + low dose SFI group and warfarin + high dose SFI group were collected before treatment with warfarin every day. All samples were centrifuged at 3000 r/min for 15 min. PT and APTT values were measured with the automatic blood coagulation analyzer (C2002-2, Precil, Beijing, China). INR = (PTtest/PTnormal)ISI. PTtest and PTnormal are prothrombin time of drug-containing plasma samples and blank plasma samples respectively, and ISI stands for International Sensitivity Index.
Pharmacokinetic study of R/S-warfarin by UPLC-MS-MS
In single-dose study, blood samples (200 µL) were collected from rats in relative groups at the following time points after warfarin administration: 0, 0.5, 1, 1.5, 2, 4, 8, 12, 24, 48, 72, 96, 120 and 144 h. In multiple-dose study, blood samples (200 µL) were collected before each dose of warfarin was given. All the samples were analyzed by UPLC-MS/MS which was performed as described with some modifications [35]. Acetic acid (20 µL) and internal standard (IS) methyclothiazide (50 µL) were added to plasma (100 µL), and vortexed, then ethyl acetate (3 mL) was added and centrifuged (3500 r/min, 5 min). The supernatant was transferred and evaporated under a gentle stream of nitrogen at 40℃. The residue was resuspended with 50% acetonitrile-water solution (100 µL) and filtered. 10 µL aliquot was used for each analysis.
Instrumentations and chromatographic conditions
The chromatographic separation was conducted by Astec CHIROBIOTICTMV chiral columns (5 μm, 2.1 mm × 100 mm) with a mobile phase of 5 mmol/L ammonium acetate (pH 4.02): acetonitrile = 85:15 (v/v) at the flow rate of 0.2 mL/min. 5 µL sample was injected and detected for 12 min for every test at room temperature.
The mass spectrometer was coupled with an electrospray ionization source in positive ion mode for mass spectrometry. Conditions were set as follows: capillary voltage of 0.4 KV, cone voltage of 35 V, and nitrogen flow temperature of 400℃ (flow rate: 650 L/h). Quantification was performed by multiple reaction monitoring mode with parameter setting as follows: (1) warfarin: m/z 307.0→161.0, fragmentation voltage 115 eV, collision energy 20 eV, collision cell acceleration voltage 5 V; (2) IS: m/z 357.8→321.9, fragmentation voltage 100 eV, collision energy 8 eV, collision cell acceleration voltage 5 V. Data were collected and analyzed with G6410A software (Agilent).
Statistical analysis
DAS2.0 software (Chinese Pharmacological Society, Beijing, China) was used to obtain pharmacokinetic parameters including elimination half-life (t1/2), peak concentration (Cmax), area under the concentration-time curve (AUC), and clearance (CL). SPSS 20.0 (IBM CorP. New York, USA) was applied to analyze the pharmacodynamic and pharmacokinetic parameters, and the data are expressed as mean ± SD. Data were compared by independent t test, P < 0.05 was considered significant and P < 0.01 was considered highly significant.
Results
The effect of repeated dosing with SFI on the pharmacodynamics of single-dose of warfarin
Rats were injected with SFI of low dose (8.93 mg/kg) or high dose (26.79 mg/kg) with or without a single dose of warfarin (0.2 mg/kg). Pharmacodynamics parameters including PT and APTT were measured as described above, and INR values were calculated. PT-time curves and INR-time curves are presented in Figs. 2 and 3. APTT values are shown in Table 1. Compared with the blank control group, PT, APTT, and INR values of the low dose or high dose SFI group were not significantly changed (P > 0.05). Compared with the warfarin control group, the PT and INR values of warfarin combined with low dose or high dose SFI group were reduced to varying degrees (P < 0.05 or P < 0.01), while APTT values showed no significant difference (P > 0.05).
The effect of repeated dosing with SFI on the pharmacodynamics of multiple dose of warfarin
Rsts were orally given warfarin (0.2 mg/kg) for 8 consecutive days, in which some were intraperitoneally injected with normal saline, SFI of low dose (8.93 mg/kg) or high dose (26.79 mg/kg) for 3 consecutive days from day 5. To measure PT and APTT, rats’ plasma from different groups were then applied to an automated coagulation analyzer. INR values were calculated accordingly. Figures 4, 5 and 6 present PT-time curves, APTT-time curves, and INR-time curves respectively. According to these results, after the blood concentration of warfarin reaches a steady state, low and high dose SFI can significantly decrease PT, APTT and INR values in rats (P < 0.01).
The effect of repeated dosing with SFI on the pharmacokinetics of a single dose of warfarin
The pharmacokinetic parameters of R-warfarin were shown in Table 2 and corresponding results of S-warfarin were in Table 3. Figures 7 and 8 depicted plasma concentration-time curves of the two configurations of warfarin. Compared with the warfarin control group, the pharmacokinetic parameter Cmax, AUC0 − t and AUC0−∞ of R-warfarin in the warfarin + low dose SFI group reduced by 25.10% (P < 0.01), 42.55% (P < 0.01), 41.29% (P < 0.01), CL increased by 43.33% (P < 0.01), and t1/2 shortened by 29.67% (P < 0.01). The pharmacokinetic parameters Cmax, AUC0 − t, AUC0−∞ of R-warfarin in the warfarin + high dose SFI group reduced by 32.45% (P < 0.01), 58.93% (P < 0.01), 59.72% (P < 0.01), CL increased by 86.67% (P < 0.01), t1/2 shortened by 44.31% (P < 0.01) (Table 2). The S-warfarin pharmacokinetic parameters Cmax, AUC0 − t, AUC0−∞ in the warfarin + low dose SFI group decreased by 21.03% (P < 0.01), 30.79% (P < 0.01), 28.49% (P < 0.01), CL increased by 25.00% (P < 0.01), t1/2 shortened by 8.65% (P > 0.05) and S-warfarin pharmacokinetic parameters Cmax, AUC0 − t, AUC0−∞ in the warfarin + high dose SFI group were reduced by 30.28% (P < 0.01), 43.44% (P < 0.01), 41.57% (P < 0.01), CL increased by 42.31% (P < 0.01), t1/2 shortened by 14.05% (P > 0.05) (Table 3). These data elucidated that SFI could accelerate the metabolism of warfarin enantiomers, especially for R-warfarin in the warfarin + high-dose SFI group.
The effect of repeated dosing with SFI on the pharmacokinetics of multiple-dose of warfarin
Plasma concentration-time curves of warfarin enantiomers are shown in Figs. 9 and 10. Compared with warfarin control group, plasma concentrations of R-warfarin decreased by 11.03% (P < 0.01), 16.14% (P < 0.01) and 16.95% (P < 0.01) after low dose SFI was co-administered, or 12.91% (P < 0.01), 17.76% (P < 0.01), 18.67% (P < 0.01) after high dose SFI co-administered at the last three consecutive days (shown as the day of 6, 7, 8 in the Figs. 9 and 10), respectively. Similarly, plasma concentrations of S-warfarin decreased by 9.90% (P < 0.01), 12.07% (P < 0.01), 12.98% (P < 0.01) after low dose SFI was co-administered, and reduced by 12.33% (P < 0.01), 13.62% (P < 0.01), and 15.74% (P < 0.01) after high dose SFI was co-administered. These data indicated that SFI (both low dose and high dose) could promote the metabolism of warfarin in steady-state, mainly manifested by reducing its plasma concentrations.
The effect of SFI on warfarin plasma protein binding rate
Concentrations of total and free warfarin were measured in the different groups and warfarin plasma protein binding rates were calculated accordingly. As shown in Table 4, warfarin plasma protein binding rates in presence of low-, medium-, and high-dose SFI were 98.03%, 97.95%, and 97.63% respectively, and had no statistical changes. These data implied that SFI had no significant effect on warfarin plasma protein binding rate.
Discussion
The current study assessed the effects of SFI, a herbal medicine widely used in cardiovascular and cerebrovascular diseases, on warfarin anticoagulation effects from perspectives of PD and PK, and predict the risk of the concomitant use. To our knowledge, this is the first study exploring the SFI-warfarin interaction. Our results showed that SFI can weaken anticoagulation effect of warfarin in rats in vivo and it’s suggested to avoid co-administration of SFI or drugs containing FA to patients receiving warfarin.
The coagulation pathways in the body mainly include endogenous coagulation pathways reflected by APTT and exogenous coagulation pathways reflected by PT [36, 37]. The INR value is calculated according to PT and ISC values. Close monitoring of INR value is needed for patients on warfarin to avoid adverse events or therapeutic failures [38,39,40]. In this study, APTT, PT and INR were measured to investigate how warfarin’s anticoagulation intensity was impacted by SFI and in which coagulation pathways. The pharmacodynamic results of the single-dose warfarin test showed that compared with the blank control group, PT, APTT, and INR of the rats in the low dose or high dose SFI groups were not significantly different (P > 0.05). It has been reported that SFI has various pharmacological effects including anti-platelet aggregation, reducing blood lipid level, protecting vascular endothelium, antioxidant effect and increasing coronary artery flow, ect [6]. Our study reported for the first time that SFI has no effect on coagulation parameters, suggesting that SFI does not treat cardiovascular diseases by changing coagulation factors. The results further clarifies the pharmacological mechanism of SFI, and provides more reference for the rational use of natural products or preparations containing FA to treat cardiovascular disorders in traditional practice.
However, compared with the warfarin control group, the combination of the low dose and high dose SFI reduced PT and INR values (P < 0.01), while APTT values were not significantly changed (P > 0.05), suggesting that SFI could weaken the anticoagulation of single-dose warfarin in exogenous coagulation pathway. Moreover, pharmacodynamic results of the steady-state warfarin test showed that PT, APTT, and INR values were downregulated (P < 0.01) when warfarin reached a steady state and was combined with low dose or high dose SFI. These results indicated that SFI alone had no effect on the coagulation index, but when co-administrated with warfarin, it could weaken the anticoagulant effect of single-dose and steady-state warfarin in rats. SFI exerts anti-thrombotic effects by inhibiting platelet aggregation and release [41], whereas warfarin acts by inhibiting the synthesis of coagulation factors due to its structural resemblance of vitamin K [42]. Different anti-thrombotic mechanism of both drugs can explain why SFI attenuates the effect of warfarin but keeps its own anti-thrombotic effect when not co-administered with warfarin.
Our single-dose and steady-state warfarin pharmacokinetic studies showed that both low and high doses of SFI could accelerate the metabolism of warfarin enantiomers in vivo and weaken its anticoagulant effect. There has been reported that ferulic acid had an induction effect on both CYP3A4 and CYP2C9 transcription activity [29]. Since CYP3A4 and CYP2C9 are the main metabolic enzymes for R-warfarin and S-warfarin, respectively, it is speculated that SFI enhances the metabolism of warfarin by inducing these two enzymes, thus weakening its anticoagulant effect.
Clinically available warfarin is a racemic mixture composed of R-warfarin and S-warfarin in equal proportions, while S-warfarin holds 3–5 times more anticoagulation potency than R-warfarin. Both enantiomers are eliminated via hepatic metabolism by different CYP450 enzymes, of which R-warfarin is mainly metabolized by CYP1A2 and CYP3A4, and S-warfarin by CYP2C9 [43]. Therefore, examining the concentration of warfarin in specific enantiomers helped identify metabolic enzymes changed when warfarin was co-administrated with SFI. Warfarin has a high plasma protein binding rate of 98 − 99%. When co-administered drugs compete with warfarin for the binding, it will increase free concentration of warfarin and bleeding risk [44,45,46]. Our study showed that the plasma protein binding rate of warfarin did not change significantly after warfarin was combined with low, medium, and high doses of SFI (P > 0.05). The plasma protein binding rate of sodium ferulate is low at only 19.4%, so it is less likely to compete with warfarin for the binding of plasma protein [6, 47]. Therefore, the combination of the two drugs will not cause drug interactions due to plasma protein binding.
With the increasing application of SFI in the treatment of cardiovascular and cerebrovascular diseases, its interaction with other drugs besides warfarin should also be concerned and studied. It should also be pointed out that according to the previous reports [13,14,15,16,17], the quality of evidences for the efficacy of SFI in the treatment of ischemic cardiovascular and cerebrovascular diseases is not high, due to the presence of clinical heterogeneity, and imprecision in partial outcome measures. Standard therapy is mostly established on large-scale randomized controlled trials (RCT) of high quality and meta-analyses based on those trials [48, 49]. For instance of antiplatelet therapy, to explore appropriate dose of aspirin (81 mg vs. 325 mg) in patients with established atherosclerotic cardiovascular disease, Jones et al. conducted a RCT enrolling 15,076 patients with a median follow-up of 26.2 months and got the conclusion after rigorous statistical analysis [50, 51]. Antithrombotic Trialists’ Collaboration included 287 randomized trials involving more than 200,000 participants to determine the effects of antiplatelet therapy among patients at high risk of occlusive vascular events [52]. Baigent et al. undertook meta-analyses based on six primary prevention trials and sixteen secondary prevention trials [53]. However, there have been no large-scale RCTs investigating the efficacy of SFI in the treatment of cardiovascular and cerebrovascular diseases, no meta-analysis based on high quality of data as well. Therefore, more high quality evidences of clinical trials for SFI are still needed to conduct to further confirm its efficacy.
Conclusions
Herb-drug interactions may result in adverse events which is a non negligible health issue demanding extensive recognition and deep research. When SFI is applied for treatment of cardiovascular diseases as a complementary and alternative therapy, it should be noticed the potential interaction with warfarin. Warfarin is widely used in thromboembolic diseases but susceptible to various factors especially drugs, which may limit it to attain therapeutic responses. The results of this study indicate that SFI can weaken the anticoagulant effect of warfarin, which may lead to warfarin therapeutic failure and increase the risk of thrombosis. Therefore, it is suggested that it is necessary to avoid giving preparations with FA to patients taking warfarin. Once co-administrated, more close monitoring is needed, and the dosage of warfarin should be adjusted according to the INR value to ensure the effectiveness of anticoagulant therapy and avoid thromboembolic events. More studies should be conducted to confirm this finding of SFI-warfarin interaction in humans.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- SFI:
-
Sodium ferulate injection
- PT:
-
Prothrombin time
- APTT:
-
Activated partial thromboplastin time
- INR:
-
International normalized ratio
- AF:
-
Atrial fibrillation
- PD:
-
Pharmacodynamics
- PK:
-
Pharmacokinetics
- FA:
-
Ferulic acid
- IS:
-
Internal standard
- RCT:
-
Randomized controlled trials
References
Parvez MK, Rishi V. Herb-drug interactions and hepatotoxicity. Curr Drug Metab. 2019;20:275–82.
Leite PM, Martins MAP, Carvalho MDG, Castilho RO. Mechanisms and interactions in concomitant use of herbs and warfarin therapy: an updated review. Biomed Pharmacother. 2021;143:112103.
Wang CY, Hsiao CY, Tsai KL, Cheng YH. Injectable thermosensitive chitosan-based hydrogel containing ferulic acid for treating peripheral arterial disease. J Tissue Eng Regen Med. 2020;14:1438–48.
Zdunska K, Dana A, Kolodziejczak A, Rotsztejn H. Antioxidant properties of ferulic acid and its possible application. Skin Pharmacol Physiol. 2018;31:332–6.
Zhang X, Gao ZP. Research progress in ferulic acid. Mod Chin Med. 2020;22(1):138–47.
Li D, Rui YX, Guo SD, Luan F, Liu R, Zeng N. Ferulic acid: a review of its pharmacology, pharmacokinetics and derivatives. Life Sci. 2021;284:119921.
Neto-Neves EM, da Silva Maia B, Filho C, Dejani NN, de Sousa DP. Ferulic acid and cardiovascular health: therapeutic and preventive potential. Mini Rev Med Chem. 2021;21:1625–37.
Wu X, Hu Z, Zhou J, Liu J, Ren P, Huang X. Ferulic acid alleviates atherosclerotic plaques by inhibiting VSMC Proliferation through the NO/p21 signaling pathway. J Cardiovasc Transl Res. 2022;15:865–75.
Li G, Huang X. Influence of sodium ferulate on miR-133a and left ventricle remodeling in rats with myocardial infarction. Hum Exp Toxicol. 2021;40:417–24.
Xu X, Xiao H, Zhao J, Zhao T. Cardioprotective effect of sodium ferulate in diabetic rats. Int J Med Sci. 2012;9:291–300.
Mu M, Zuo S, Wu RM, Deng KS, Lu S, Zhu JJ, Zou GL, Yang J, Cheng ML, Zhao XK. Ferulic acid attenuates liver fibrosis and hepatic stellate cell activation via inhibition of TGF-beta/Smad signaling pathway. Drug Des Devel Ther. 2018;12:4107–15.
Hong Q, Ma ZC, Huang H, Wang YG, Tan HL, Xiao CR, Liang QD, Zhang HT, Gao Y. Antithrombotic activities of ferulic acid via intracellular cyclic nucleotide signaling. Eur J Pharmacol. 2016;777:1–8.
Lin Y, Xu JC. Analysis of the clinical value of sodium ferulate in the treatment of coronary heart diseas. Mod Diagn Treat. 2016;27:46–8.
Lv FY. The therapeutic effect of sodium ferulic acid on coronary heart disease and its protective effect on vascular endothelial function. Henan Med Res. 2017;26:3217–8.
Lai XF, Dai HH, Du L. Study on protective effect and mechanism of sodium ferulate on myocardium in patients with acute myocardial infarction undergoing primary PCI. J Mod Med Health. 2019;35:1807–11.
Liu YR. Analysis of the therapeutic effect of sodium ferulic acid on coronary heart diseases and its protective effect on vascular endothelial function. J Contemp Clin Med. 2022;35:10–1.
Shen Z, Wu Y, Zhou L, Wang Q, Tang Y, Sun Y, Zheng FJ, Li YH. The efficacy of sodium ferulate combination therapy in coronary heart disease: a systematic review and meta-analysis. Phytomedicine. 2023;115:154829.
Ritchie LA, Penson PE, Lane DA. Warfarin therapy and improved anticoagulation control by patient self-management. Thromb Haemost. 2019;119:1550–2.
Catterall F, Ames PR, Isles C. Warfarin in patients with mechanical heart valves. BMJ. 2020;371:m3956.
January CT, Wann LS, Calkins H, Chen LY, Cigarroa JE, Cleveland JC Jr., Ellinor PT, Ezekowitz MD, Field ME, Furie KL, et al. 2019 AHA/ACC/HRS focused update of the 2014 AHA/ACC/HRS Guideline for the management of patients with Atrial Fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice guidelines and the heart rhythm society in collaboration with the Society of thoracic surgeons. Circulation. 2019;140:e125–51.
Wang Z, Xiang X, Liu S, Tang Z, Sun H, Parvez M, Ghim JL, Shin JG, Cai W. A physiologically based pharmacokinetic/pharmacodynamic modeling approach for drug-drug interaction evaluation of warfarin enantiomers with sorafenib. Drug Metab Pharmacokinet. 2021;39:100362.
Qayyum A, Najmi MH, Khan AM, Abbas M, Naveed AK, Jameel A. Determination of S- and R-warfarin enantiomers by using modified HPLC method. Pak J Pharm Sci. 2015;28:1315–21.
Wang Z, Wang Z, Wang X, Lv X, Yin H, Jiang L, Xia Y, Li W, Li W, Liu Y. Potential food-drug interaction risk of thymoquinone with warfarin. Chem Biol Interact. 2022;365:110070.
Witt DM, Clark NP, Kaatz S, Schnurr T, Ansell JE. Guidance for the practical management of warfarin therapy in the treatment of venous thromboembolism. J Thromb Thrombolysis. 2016;41:187–205.
Leite PM, Martins MAP, Castilho RO. Review on mechanisms and interactions in concomitant use of herbs and warfarin therapy. Biomed Pharmacother. 2016;83:14–21.
Huang Q, Cao L, Luo N, Qian H, Wei M, Xue L, Zhou Q, Zou B, Tan L, Chu Y, et al. Predicting Range of initial warfarin dose based on pharmacometabolomic and genetic inputs. Clin Pharmacol Ther. 2021;110:1585–94.
Tavares LC, Marcatto LR, Santos P. Genotype-guided warfarin therapy: current status. Pharmacogenomics. 2018;19:667–85.
Kulig CE, Roberts AJ, Rowe AS, Kim H, Dager WE. INR response to Low-Dose Vitamin K in Warfarin patients. Ann Pharmacother. 2021;55:1223–9.
Zhuang XM, Chen L, Tan Y, Yang HY, Lu C, Gao Y, Li H. Identification of human cytochrome P450 and UGT enzymes involved in the metabolism of ferulic acid, a major bioactive component in traditional Chinese medicines. Chin J Nat Med. 2017;15:695–702.
Tan CSS, Lee SWH. Warfarin and food, herbal or dietary supplement interactions: a systematic review. Br J Clin Pharmacol. 2021;87:352–74.
Prabhakar PK, Prasad R, Ali S, Doble M. Synergistic interaction of ferulic acid with commercial hypoglycemic drugs in streptozotocin induced diabetic rats. Phytomedicine. 2013;20:488–94.
Taki Y, Yokotani K, Yamada S, Shinozuka K, Kubota Y, Watanabe Y, Umegaki K. Ginkgo biloba extract attenuates warfarin-mediated anticoagulation through induction of hepatic cytochrome P450 enzymes by bilobalide in mice. Phytomedicine. 2012;19:177–82.
Sun J, Lu Y, Li Y, Pan J, Liu C, Gong Z, Huang J, Zheng J, Zheng L, Li Y, et al. Influence of Shenxiong glucose injection on the activities of six CYP isozymes and metabolism of warfarin in rats assessed using probe cocktail and pharmacokinetic approaches. Molecules. 2017;22:1994.
Shi Y, Zhang W, Jiang M, Huang L, Zhou Y, Chen J, Liu D, Liu G, Dong M. Effects of sulfotanshinone sodium injection on the pharmacokinetics and pharmacodynamics of warfarin in rats in vivo. Xenobiotica. 2020;50:705–12.
Jiang M, Zhou Y, Chen J, Zhang W, Sun Z, Qin M, Liu Y, Liu G. Effects of Herba erigerontis injection on pharmacodynamics and pharmacokinetics of warfarin in rats in vivo. Basic Clin Pharmacol Toxicol. 2021;128:386–93.
Wheeler AP, Gailani D. The intrinsic pathway of Coagulation as a target for antithrombotic therapy. Hematol Oncol Clin North Am. 2016;30:1099–114.
Winter WE, Flax SD, Harris NS. Coagulation testing in the Core Laboratory. Lab Med. 2017;48:295–313.
Dorgalaleh A, Favaloro EJ, Bahraini M, Rad F. Standardization of Prothrombin Time/International Normalized ratio (PT/INR). Int J Lab Hematol. 2021;43:21–8.
Papala M, Gillard D, Hardman J, Romano T, Rein LE. Extending INR testing intervals in warfarin patients at a multi-center anticoagulation clinic. J Thromb Thrombolysis. 2022;53:626–32.
Bontempi M. Semi-empirical anticoagulation model (SAM): INR monitoring during warfarin therapy. J Pharmacokinet Pharmacodyn. 2022;49:271–82.
Choi JH, Park JK, Kim KM, Lee HJ, Kim S. In vitro and in vivo antithrombotic and cytotoxicity effects of ferulic acid. J Biochem Mol Toxicol. 2018;32(1). https://doi.org/10.1002/jbt.22004.
Donaldson CJ, Harrington DJ. Therapeutic warfarin use and the extrahepatic functions of vitamin K-dependent proteins. Br J Biomed Sci. 2017;74:163–9.
Kaminsky LS, Zhang ZY. Human P450 metabolism of warfarin. Pharmacol Ther. 1997;73:67–74.
Xie B, Jiang SQ, Shen XL, Wu HQ, Hu YJ. Pharmacokinetics, plasma protein binding, and metabolism of a potential natural chemosensitizer from Marsdenia tenacissima in rats. J Ethnopharmacol. 2021;281:114544.
Di L. An update on the importance of plasma protein binding in drug discovery and development. Expert Opin Drug Discov. 2021;16:1453–65.
Bai Y, Fan Y, Ge G, Wang F. Advances in chromatography in the study of drug-plasma protein interactions. Se Pu. 2021;39:1077–85.
Yu X, Jiao Q, Jiang Y, Guo S, Zhang W, Liu B. Study on the plasma protein binding rate and compatibility regularity of the constituents migrating to blood of Simiao Yong’an decoction. Curr Drug Metab. 2020;21:979–93.
Virani SS, Newby LK, Arnold SV, Bittner V, Brewer LC, Demeter SH, Dixon DL, Fearon WF, Hess B, Johnsonet HM, AHA/ACC/ACCP/ASPC. /NLA/PCNA Guideline for the Management of Patients With Chronic Coronary Disease: A Report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. Circulation. 2023;148(9):e9-e119.
Schulz-Schüpke S, Byrne RA, Ten Berg JM, Neumann FJ, Han YL, Adriaenssens T, Tölg R, Seyfarth M, Maeng M, Zrenner B, et al. ISAR-SAFE: a randomized, double-blind, placebo-controlled trial of 6 vs. 12 months of clopidogrel therapy after drug-eluting stenting. Eur Heart J. 2015;36(20):1252–63.
Jones WS, Mulder H, Wruck LM, Pencina MJ, Kripalani S, Muñoz D, Crenshaw DL, Effron MB, Re RN, Gupta K, et al. Comparative effectiveness of aspirin dosing in Cardiovascular Disease. N Engl J Med. 2021;384(21):1981–90.
McCarthy L, In ASCVD. 81 mg and 325 mg of aspirin did not differ for CV or bleeding events. Ann Intern Med. 2021;174(10):JC118.
Antithrombotic Trialists’ Collaboration. Collaborative meta-analysis of randomised trials of antiplatelet therapy for prevention of death, myocardial infarction, and stroke in high risk patients. BMJ. 2002;324(7329):71–86.
Antithrombotic Trialists’ Collaboration, Baigent C, Blackwell L, Collins R, Emberson J, Godwin J, Peto R, Buring J, Hennekens C, Kearney P, et al. Aspirin in the primary and secondary prevention of vascular disease: collaborative meta-analysis of individual participant data from randomised trials. Lancet. 2009;373(9678):1849–60.
Funding
This research is funded by Key Research and Development Project of Heilongjiang Province (2022ZX06C12 to G.Liu) and Heilongjiang Postdoctoral Fund (LBH-Z 20167 to Y. Zhao).
Author information
Authors and Affiliations
Contributions
L.G.F. conceived and planned the project, and acquired funding. Z.Y. and Y.C.J. designed experiments, carried out laboratory work, analyzed data. L.Y., Q.M.N. and S.J.H. performed P.K. and P.D. study, contributed to the preparation of the manuscript. Z.Y. drafted the manuscript. L.G.F. revised the manuscript for important intellectual content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Use of animals and all experimental protocols were approved by the Ethic Committees of the Second Affiliated Hospital of Harbin Medical University (SYDW2023-075). All animal experiment methods are reported in accordance with ARRIVE guidelines.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhao, Y., Yang, C., Liu, Y. et al. Effects of sodium ferulate for injection on anticoagulation of warfarin in rats in vivo. BMC Complement Med Ther 24, 87 (2024). https://doi.org/10.1186/s12906-024-04389-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12906-024-04389-2